Abstract
To inform the development of HIV-prevention rectal douches, we reviewed the scientific literature and online instructional videos on rectal douching associated with receptive anal intercourse (RAI). Up to 88% of men who practice RAI ever have douched, while 43–64% have douched recently. Of them, 87–97% douche before RAI and 13–48% afterwards. Water, occasionally mixed with soap or salt, is used most often, although up to 31% of men use commercial products. Douching is more common among individuals reporting substance use, sexually transmitted infections, or being HIV-infected. Scant literature is available on women’s rectal douching practices, but it is apparently less frequent than among men (32% vs. 70%). Videos advise using 2–3 doses of liquid and retaining it for 10–30 seconds before expelling. These findings can inform the development of a safe and acceptable rectal douche for HIV prevention.
Keywords: rectal douche, HIV prevention, men who have sex with men, microbicides, enema
INTRODUCTION
Anal intercourse, which has been documented since antiquity, takes place both in heterosexual and homosexual contexts. Results from a U.S. national probability sample of men and women ages 14–94 show that up to 38% of U.S. men reported at least one occasion of anal intercourse within their lifetime, with 21% reporting at least one instance in the past year, and 6% reporting at least one instance in the past month; 32% percent of U.S. women ages 14–94 reported having engaged in anal intercourse at least once in their lifetime, with 11% reporting at least one instance in the past year and 3% reporting at least one instance in the past month. (1) Focusing specifically on MSM and transgender women (TGW), the scientific literature pays attention to sexual role (insertive or receptive) during anal sex, indicating that between 8% and 29% of MSM report taking predominantly or exclusively an insertive role (“tops”), between 13% and 50% report taking predominantly or exclusively an anal receptive role (“bottoms”) and between 29% and 58% report being versatile. (2–4)
Given that the presence of fecal matter in the rectum during anal intercourse is generally regarded as undesirable, the use of rectal douches (or enemas) has some popularity among individuals who practice receptive anal intercourse (RAI). This is evidenced by the fact that at least one online instructional video about rectal douching reviewed for this study had more than a million views at the time of our research. (5) However, many commonly used household products can lead to damage of rectal epithelial tissue and potentially increase a user’s risk of contracting HIV and STIs (6), which has mobilized scientific researchers and community advocates to stress the need to determine which rectal douches are safe.(7) Conversely, if a safe rectal douche could be formulated to deliver an HIV-prevention agent, this could potentially decrease a user’s risk of contracting HIV and STIs during RAI and become an important alternative prevention strategy.
This article reviews published scientific literature on rectal douching among men and women who practice RAI. It also summarizes the main recommendations on rectal douching posted on online media. We focus mainly on the behavioral aspects of rectal douching, including choice and volume of douches used, douche applicators, subgroups of douche users, douche safety, and acceptability of an HIV prevention douche. Our purpose was to identify gaps in knowledge that need to be addressed as work proceeds for the development of HIV-prevention rectal douches in the Development of a Rectal Enema as Microbicide (DREAM) Program. (8)
METHODS
Literature search
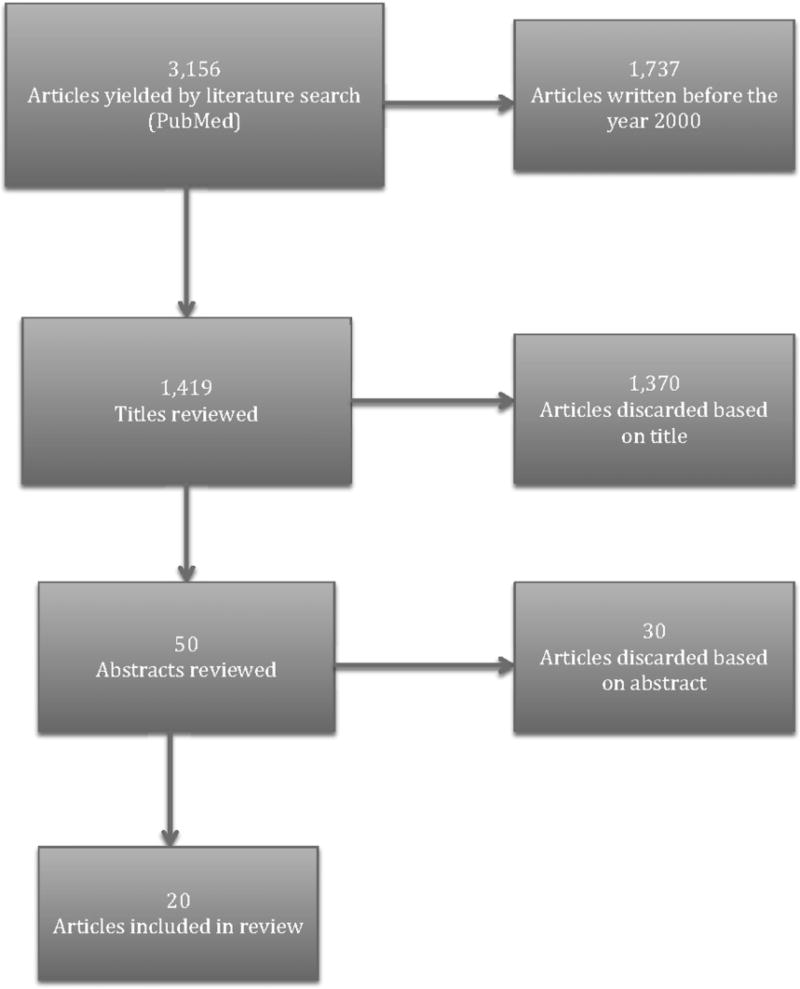
In December of 2016, we conducted a literature review using PubMed to identify articles on rectal douching in association with RAI that were published during or after the year 2000. Keywords included “rectal douching,” “rectal douche,” “rectal enemas,” “rectal douching and anal intercourse,” “rectal douching and anal sex,” “rectal enemas and anal intercourse,” “rectal enemas and anal sex,” and “douching for cleanliness.” Due to the paucity of research on rectal douching performed within a sexual context, all articles that reported findings on this practice among men who have sex with men (MSM), heterosexual women and/or transgender women (TGW) were included. Articles focusing exclusively on vaginal douching or rectal douching outside of a sexual context (e.g., reports on rectal enema use within a medical or surgical context) were excluded. All searches occurred in English. Searches for the abovementioned terms in the PubMed database yielded a total of 3,157 articles. We first reviewed article titles and found 50 potential articles for inclusion. After examining the abstracts to further eliminate unrelated articles, a total of 20 articles met the above inclusion criteria and were included for discussion in this review. Five of the articles included international samples.
Social Media Instructional Videos
To learn more about common rectal douching practices and their level of popularity, we conducted a search for the terms "rectal douching," "douching for cleanliness," "rectal douche how to," “rectal enemas,” “rectal enemas and anal sex,” and "rectal douching and anal sex" on the YouTube social media website. Searches for these terms yielded a total of about 23,220 results. We excluded any videos with titles that indicated they would not provide instructional information about how to properly douche one’s rectum (e.g., videos that served as douche giveaways and comedic videos about heterosexual males’ reactions to rectal douching). As YouTube sorts search findings by order of relevance, we then listened to the remaining videos in order of their appearance, and discarded those that did not provide actual recommendations for how to best practice rectal douching (e.g., videos that simply listed rectal douching as a good way to prepare for anal sex but did not include any procedural recommendations on how to douche). Finally, we summarized recommended practices from each video until reaching redundancy (additional videos ceased to provide new information).
RESULTS
Rectal Douching among MSM
Many MSM use rectal douches to prepare for RAI. In a study of almost 5,000 MSM recruited in 16 U.S. cities through banner advertisements from two of the nation’s largest gay websites, 88% of respondents who practiced RAI reported ever douching for cleansing purposes before RAI. (9) Prevalence estimates for recent rectal douching (defined here as at least one occurrence within the past 12 months) before RAI varied in different studies from 43 to 64% (2, 7, 9–12). This includes one study (7) of 11,766 HIV-uninfected MSM ages 18–87 recruited online in the U.S. Small sample studies (4, 10, 11) have identified the age of onset of rectal douching for cleansing purposes among MSM to be, on average, in their mid to late 20s.
Among MSM who report recently douching within the context of anal intercourse (past 12 months), 87–97% report douching before sex, (2, 9–12) and 13–48% after sex.(2, 9–12) With respect to MSM who report recently douching before an RAI encounter, 41 to 83% always do it and 14 to 37% frequently do it. Reasons for douching before RAI include a desire to maintain personal hygiene (2, 9–11, 13), adhering to a request from a sexual partner (2, 9–11, 13), a belief that douching enhances pleasure during RAI (2, 9, 13), the participant heard friends discussing the practice (10, 11), and a desire to prepare (2) or get excited for RAI.(2, 3, 10, 11) Some men who douche after sex report believing that the practice may help protect them against STIs.(2, 10, 11) Other reasons for douching after RAI include a desire to maintain personal hygiene (2, 10, 11, 13), to transition from sex (2), to adhere to a request from a sexual partner (10, 11, 13), a belief that douching following RAI enhances pleasure (13), and participants hearing their friends talk about the practice (10, 11).
MSM typically report douching a median value of one hour prior to an expected RAI encounter (with a range of 30–120 minutes) (2, 10), and, among those who douche after RAI, a median value of thirty minutes following the sexual encounter (with a range of 15–60 minutes).(2, 10) One Internet survey (2) reports that out of 4,301 respondents who did not douche before anal sex, 26.5% did not know about douching or had not thought about it; these findings are consistent with results from studies with smaller samples, which report that 26.7 to 35% of participants did not douche within the context of RAI because they didn’t know about rectal douches/enemas (9, 13).
Douche choices and volume
Of MSM who douche, 79 to 93% report using non-commercial/homemade substances and solutions.(2, 9, 13) Among them, water is by far most commonly used (64 to 82% of douchers who use non-commercial products), (2, 3, 9, 14) followed by water and soap (11 to 29.6%), (2, 9, 13) and water and salt (4.7 to 10.6%) (2, 9, 13). Between 11 and 31% of MSM who douche rectally report using commercial products (2, 9, 13), with saline-based solutions being the most common (56 to 100% of rectal douchers who use commercial products). (9, 14) Other commonly used products include: sodium phosphate, (32%), mineral oil/glycerin (22%), and laxatives (19%).(9)
Currently, not much research exists regarding ideal douche volumes. One small study (15) found that 125ml of an enema solution was overall well tolerated by study participants (n=9).
Users’ subgroups
Among men and women who report recent RAI (past three months), rectal douching may be more common among individuals who report substance-use with sex than those who do not (74% vs. 46%, respectively) (9), individuals who report having had an STI in the past year (69–94% vs. 57–86%) (2, 9), and individuals who have ever tested HIV-positive (72–95%% vs. 53–86%).(2, 9, 12) With regards to rectal douching and STI transmission, one study conducted with 994 MSM who recently attended an STI outpatient clinic found that the commonly reported positive association between douching and STI positivity disappeared when controlling for sexual position: Excluding all MSM who did not report recently engaging in RAI, as these individuals are at a higher risk for HIV and STI transmission, the authors found no relationship between rectal douching and anorectal chlamydia or gonorrhea. (12)
Research suggests that HIV-positive men may be more likely than HIV-negative men to douche both prior to and following RAI, with estimates as high as 96% and 44%, respectively.(2, 4, 11) HIV-positive men may also be more willing to openly discuss rectal douching than their HIV-negative counterparts.(4) One article (7) specifically surveyed douching practices across racial/ethnic groups in the U.S., finding that between 40% and 53% of respondents reported douching, with no significant differences between groups. Another article (2) comparing douching behavior of men across racial/ethnic groups in the U.S. found that 87–91% of men reported ever having used a rectal douche before RAI with no significant differences by race/ethnicity. However, there were significant differences when comparing douching behavior after RAI; 56% of Hispanic men, 47% of black men, and 43% of men of "other races" reported ever douching after RAI, compared to only 19% of white men.(2)
Douche safety and acceptability of an HIV-prevention douche among MSM
Although many commonly used household products can lead to damage of rectal tissue and potentially increase the user’s risk for HIV and STIs, polyethylene glycol-electrolyte solutions (laxative solutions that increase the amount of water in the intestinal tract to stimulate bowel movements) do not result in tissue damage and are reportedly more comfortable than soap and water (which provoke a stronger defecation stimulus).(6) Available research suggests that iso-osmolar enemas, or those containing concentrations of solutes similar to blood and intracellular fluid, may be good vehicles for an HIV-prevention agent: they have greater anatomic distribution in the colon, they achieve higher drug concentrations in colon fluid and tissue, and, among a small group of MSM participating in a clinical trial, had similar acceptability while being associated with fewer adverse effects than enemas with higher (hyperosmolar) or lower (hypo-osmolar) solute concentrations.(15)
Studies exploring the acceptability of a potential HIV-prevention douche indicate that most MSM believe a deeply penetrating liquid douche would offer greater HIV protection than a microbicide gel.(13) One survey conducted in Peru found that up to 80% of MSM would use a rectal douche containing a microbicide to protect against HIV if such a product were available.(16) Increased familiarity with and exposure to rectal douching practices is one factor that could mediate a man’s willingness to use rectal douches containing microbicides.(16)
Rectal Douching among Women
We found almost no information in the reviewed literature about rectal douching in women. One international survey found that douching is more common among men than women (70% vs. 32%).(9) Another study found that TGW may also perceive deeply penetrating liquid douches to offer greater HIV protection than gels.(13)
Social Media Instructional Videos
Despite the paucity of current research, YouTube videos on how to properly use rectal douches appear to be highly-viewed (at the time of writing, one video registered 45,000 views and another slightly over one million) suggesting that the practice elicits considerable interest.(5, 17, 18) These videos tend to recommend the use of warm water as the enema solution, (5, 17, 18) and advise users to retain the liquid for about ten (18) to thirty (17) seconds before expelling it from the rectum (Table 1). Users are advised to repeat the process two to three times “until the water comes clean” to ensure a sufficient, shallow cleaning.(5, 17, 18) Given that some residual water may be lodged in the intestines, the videos recommend waiting 15–30 minutes after douching to engage in anal intercourse in case more water makes its way to the rectum and needs to be expelled.(17).
Table 1.
YouTube Video Recommendations for Rectal Douching
| Type of Douche | Shallow Douching | Deeper Douchinga |
| Solution | Warm Water | Warm Water |
| Douche Applicator | Commercial Enema Bottle, Plastic Water Bottle, or Rubber Bulb | Hose or Enema Bag Attached to Shower |
| Time to Retain Liquid | 10–30 seconds | As long as possible |
| Time to Wait Before Anal Sex | 15–30 minutes | 30–60 minutes |
Deeper douching is recommended before longer sessions of anal sex or more highly penetrative acts such as receptive anal fisting
The videos also differentiate between recommendations for shallow (see above) and deep douching. A deeper douching is recommended for individuals who might have anal sex for longer periods of time, or who engage in more penetrative acts such as receptive anal fisting.(17) With deeper douching methods, it is advised to retain the water in the rectum for as long as possible before expelling it; due to this deeper penetration, it is also recommended that users wait longer periods of time (30 minutes to an hour) before engaging in anal sex to ensure that residual water has had enough time to travel to the rectum for expulsion.(5, 17)
Douche applicators
Based on the literature, men reported most commonly using enema bottles, plastic or rubber bulbs (whether prepackaged or reusable), (2, 10) hoses attached to a shower (4, 9, 12) or to a sink, (9) or a plastic bottle (such as a water bottle) (3, 9) for rectal douching. Instructional videos recommend commercial enema bottles, (17, 18) a plastic water bottle, (18) plastic or rubber bulbs, (18) or hoses or enema bags attached to a shower. (18)
DISCUSSION
Our review of the existent scientific literature and a cursory observation of the instructional videos available on YouTube show that rectal douching is popular among certain sectors of people who practice RAI. These individuals not only have used douches in association with RAI at some point in their lives, but they also seem to have adopted the practice on a regular basis.
Focusing on douches for cleansing purposes, there is a need to further determine which products are safe. The association of rectal douching with STIs and HIV initially raised some concerns that douches may facilitate the transmission of pathogens by damaging rectal epithelial tissue.(19, 20) Yet, a recent article found that rectal douching or sharing douching equipment were not significantly associated with anorectal chlamydia and/or gonorrhea (12), and another study (15) found that iso-osmolar products did not result in damage to rectal epithelial tissue. It could be that individuals who anticipate prolonged sexual encounters, potentially with more than one partner and involving recreational drug use, do douche thoroughly in preparation for sex; yet, the increase in likelihood of HIV or STI transmission may not be causally and exclusively related to douching. More research is needed on this topic. Further, there is a need to conduct public campaigns advising populations at risk about products that should be avoided.
Focusing on douches for HIV or other disease prevention, it is necessary to determine if the same douche could be used for both cleansing and disease prevention, which would be ideal. Alternatively, after cleansing is accomplished, a different, disease-prevention douche would need to be applied. In either case, there is a need to determine the range of doses that can offer protection without resulting in overdosing, the frequency with which these doses should be applied, the length during which protection can be maintained, optimal solution volumes, procedures to be followed (e.g., minimum retention time to allow quick absorption of the product by the mucosa, which is likely to happen within a few seconds of administration), and the compatibility of disease prevention douches with cleansing douches and rectal lubricants used to facilitate penetration.(21–23) Moreover, if the cleansing douches leave liquid in the intestines that may be flushed out after 15 or 30 minutes, it will be important to determine that this does not wash away the HIV-prevention agent. Once these parameters have been established, it will be important to promote use of safe disease-preventions douches among at-risk individuals. Importantly, up to a quarter of individuals reporting that they had not douched stated that they did not know or had not thought about it. This raises the possibility that educational efforts could increase the number of RAI practitioners who could douche, particularly if they perceive that douches could be safe and bring additional benefits to cleansing, such as disease prevention.
Limitations
All reviewed scientific articles were in English. Although English has become the lingua franca for scientific reports, it is possible that additional information, particularly in the lay media, could complement the findings here reported. Furthermore, most surveys collected information from convenience samples of volunteers, including individuals subscribing to paid online social and sexual networking sites. This may generate biased results. Some large internet surveys were restricted to HIV-negative men or included questions on douching in studies whose main focus was not on douching (e.g., alcohol-related HIV risk behavior). The largest Internet survey included just two questions on douche usage prior to intercourse -- if ever used and number of times used in the prior three months. Finally, there is a dearth of information on women, especially TGW who are likely to engage in RAI.
Considering that anal intercourse and douching in preparation for it are stigmatized behaviors, it is likely that all surveys will result in underestimates. Nevertheless, when large sectors of the population exhibit behaviors that are either problematic or can be tailored towards a healthier outcome, it may not be absolutely necessary to estimate the prevalence of such behaviors in the population at large. The reviewed documentation supports the need to identify non-toxic rectal douching products and to develop rectal douches that could prevent rectally transmitted infections.
Figure 1.
Literature Review Flowchart
Acknowledgments
The study was funded by a U19 grant under the Integrated Preclinical-Clinical Program for HV Topical Microbicides (IPCP-HTM), Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH) (AI113127). This work was also supported by a center grant from the NIMH to the HIV Center for Clinical and Behavioral Studies at New York State Psychiatric Institute and Columbia University [P30-MH43520; PI: Remien, PhD]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Compliance with Ethical Standards:
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest: All authors declare that they have no conflicts of interest.
References
- 1.Herbenick D, Reece M, Schick V, Sanders Sa, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 142013;94. J Sex Med. 2010;7(Suppl 5):255–65. doi: 10.1111/j.1743-6109.2010.02012.x. [DOI] [PubMed] [Google Scholar]
- 2.Noor SW, Simon Rosser BR. Enema use among men who have sex with men: A behavioral epidemiologic study with implications for HIV/STI prevention. Arch Sex Behav. 2014;43(4):755–69. doi: 10.1007/s10508-013-0203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galea JT, Kinsler JJ, McLean S, Calvo G, Sánchez H, Leon SR, et al. Rectal Douching Prevalence and Practices Among Peruvian Men Who have Sex with Men and Transwomen: Implications for Rectal Microbicides. AIDS Behav. 2016;20(11):2555–64. doi: 10.1007/s10461-015-1221-9. [DOI] [PubMed] [Google Scholar]
- 4.Schilder AJ, Orchard TR, Buchner CS, Strathdee SA, Hogg RS. Insert Discourse: Rectal Douching Among Young HIV-Positive and HIV-Negative Men Who Have Sex with Men in Vancouver, Canada. Sex Cult. 2010;14(4):327–43. [Google Scholar]
- 5.How to give yourself an enema/douche/clean inside your butt. https://www.youtube.com/watch?v=BugCpKJvkVQ.
- 6.Schmelzer M, Schiller LR, Meyer R, Rugari SM, Case P. Safety and effectiveness of large-volume enema solutions. Appl Nurs Res. 2004;17(4):265–74. [PubMed] [Google Scholar]
- 7.Calabrese SK, Rosenberger JG, Schick VR, Novak DS, Reece M. An event-level comparison of risk-related sexual practices between black and other-race men who have sex with men: condoms, semen, lubricant, and rectal douching. AIDS Patient Care STDS. 2013 Feb;27(2):77–84. doi: 10.1089/apc.2012.0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Institutes of Health G. Development of a Rectal Enema as Microbicide (DREAM) [cited 2017 May 3];2015 Available from: http://grantome.com/grant/NIH/U19-AI113127-01.
- 9.Javanbakht M, Stahlman S, Pickett J, Leblanc M-A, Gorbach PM. Prevalence and types of rectal douches used for anal intercourse: results from an international survey. BMC Infect Dis. 2014;14:1–8. doi: 10.1186/1471-2334-14-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carballo-Dieguez A, Bauermeister JJ, Ventuneac A, Dolezal C, Mayer K, Carballo-Diéguez A, et al. Why Rectal Douches May Be Acceptable Rectal-Microbicide Delivery Vehicles for Men Who Have Sex With Men. Sex Transm Dis April 2010. 2010;37(4):228–33. doi: 10.1097/OLQ.0b013e3181bf9b2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH. The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: Implications for rectal microbicides. AIDS Behav. 2008 Nov;12(6):860–6. doi: 10.1007/s10461-007-9301-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Achterbergh RCA, van der Helm JJ, van den Boom W, Heijman T, Stolte IG, van Rooijen MS, et al. Is rectal douching and sharing douching equipment associated with anorectal chlamydia and gonorrhoea? A cross-sectional study among men who have sex with men. Sex Transm Infect. 2017 Jan 20; doi: 10.1136/sextrans-2016-052777. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Galea JT, Kinsler JJ, Imrie J, Nureña CR, Sánchez J, Cunningham WE. Rectal douching and implications for rectal microbicides among populations vulnerable to HIV in South America: a qualitative study. Sex Transm Infect. 2014 Aug;90(1):33–5. doi: 10.1136/sextrans-2013-051154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitchell JW, Sophus AI, Lee J-Y, Petroll AE. Anal Douche Practices and Willingness to Use a Rectal Microbicide Enema for HIV Prevention and Associated Factors Among an Internet Sample of HIV-Negative and HIV-Discordant Male Couples in the US. AIDS Behav. 2016;20(11):2578–87. doi: 10.1007/s10461-015-1250-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leyva FJ, Bakshi RP, Fuchs EJ, Li L, Caffo BS, Goldsmith AJ, et al. Isoosmolar Enemas Demonstrate Preferential Gastrointestinal Distribution, Safety, and Acceptability Compared with Hyperosmolar and Hypoosmolar Enemas as a Potential Delivery Vehicle for Rectal Microbicides. AIDS Res Hum Retroviruses. 2013;29(11):1487–95. doi: 10.1089/aid.2013.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kinsler JJ, Galea JT, Lama JR, Segura P, Peinado J, Casapia M, et al. Rectal douching among Peruvian men who have sex with men acceptability of a douche-formulated rectal microbicide to prevent HIV infection. Sex Transm Infect. 2013;89(1):62–62. doi: 10.1136/sextrans-2012-050630. [DOI] [PubMed] [Google Scholar]
- 17.Fleet Before You Meet. https://www.youtube.com/watch?v=Bmp6QHt-zWw.
- 18.Cleaning Out - For Anal Sex. https://www.youtube.com/watch?v=uvloaqN8vgE.
- 19.Coates R, Calzavara L, Read S, Fanning M, Shpherd F, Klein M, et al. Risk factors for HIV infection in male sexual contacts of men with AIDS or an AIDS-related condition. Am J Epidemiol. 1988;128(4):729–39. doi: 10.1093/oxfordjournals.aje.a115026. [DOI] [PubMed] [Google Scholar]
- 20.Moss AR, Osmond D, Bacchetti P, Chermann JC, Barre-Sinoussi F, Carlson J. Risk factors for AIDS and HIV seropositivity in homosexual men. Am J Epidemiol. 1987;125(6):1035–47. doi: 10.1093/oxfordjournals.aje.a114619. [DOI] [PubMed] [Google Scholar]
- 21.Carballo-Diéguez A, Stein Z, Sáez H, Dolezal C, Nieves-Rosa L, Díaz F. Frequent use of lubricants for anal sex among men who have sex with men: The HIV prevention potential of a microbicidal gel. Am J Public Health. 2000;90(7):1117–21. doi: 10.2105/ajph.90.7.1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gorbach PM, Weiss RE, Fuchs E, Jeffries RA, Hezerah M, Brown S, et al. The slippery slope: lubricant use and rectal sexually transmitted infections: a newly identified risk. Sex Transm Dis. 2012;39(1):59–64. doi: 10.1097/OLQ.0b013e318235502b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dezzutti CS, Brown ER, Moncla B, Russo J, Cost M, Wang L, et al. Is Wetter Better? An Evaluation of Over-the-Counter Personal Lubricants for Safety and Anti-HIV-1 Activity. PLoS One. 2012;7(11):e48328. doi: 10.1371/journal.pone.0048328. [DOI] [PMC free article] [PubMed] [Google Scholar]