Abstract
We examined (1) differences between controls and patients with social anxiety disorder (SAD) in emotional clarity and attention to emotions; (2) changes in emotional clarity and attention to emotions associated with cognitive-behavioral group therapy (CBGT), mindfulness-based stress reduction (MBSR), or a waitlist (WL) condition; and (3) whether emotional clarity and attention to emotions moderated changes in social anxiety across treatment. Participants were healthy controls (n = 37) and patients with SAD (n=108) who were assigned to CBGT, MBSR, or WL in a randomized controlled trial. At pretreatment, posttreatment, and 12-month follow-up, patients with SAD completed measures of social anxiety, emotional clarity, and attention to emotions. Controls completed measures at baseline only. At pretreatment, patients with SAD had lower levels of emotional clarity than controls. Emotional clarity increased significantly among patients receiving CBGT, and changes were maintained at 12-month follow-up. Emotional clarity at posttreatment did not differ between CBGT and MBSR or between MBSR and WL. Changes in emotional clarity predicted changes in social anxiety, but emotional clarity did not moderate treatment outcome. Analyses of attention to emotions were not significant. Implications for the role of emotional clarity in the treatment of SAD are discussed.
Keywords: emotional clarity, attention, social anxiety, CBT, MBSR
Individuals with social anxiety disorder (SAD) experience pervasive and impairing anxiety in social or performance situations. They fear both negative and positive evaluation by others, which often leads to the tendency to avoid or escape social situations (American Psychiatric Association [APA], 2013; Rapee & Heimberg, 1997; Weeks, Heimberg, Rodebaugh, & Norton, 2008). Recent studies estimate that in a given 12-month period, 7.1% of the United States population meets criteria for SAD, and the lifetime prevalence rate has been estimated at 12.1%; nearly one-third of those cases are classified as severe (Kessler, Berglund, et al., 2005; Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Ruscio et al., 2008). Considering the substantial impairment experienced by individuals with SAD in areas such as work, social and romantic relationships (e.g., Aderka et al., 2012; Rodebaugh, Fernandez, & Levinson, 2012), and overall quality of life (Simon et al., 2002), it is important to elucidate factors which can be targeted through treatment to alleviate social anxiety symptoms and to determine which treatments might best facilitate improvement in these factors.
One factor that may be appropriate to target through treatment for SAD is emotional intelligence. Emotional intelligence refers to an individual’s ability to appraise and regulate emotions in oneself and others and to use emotions to problem-solve and achieve (Salovey & Mayer, 1990). The current study focuses on two specific facets of emotional intelligence: emotional clarity and attention to emotions. Emotional clarity refers to one’s ability to identify the type of emotions (e.g., fear versus anger) one is experiencing, whereas attention to emotions refers to the degree to which an individual attends to his or her emotional experiences (Coffey, Berenbaum, & Kerns, 2003). These two distinct facets emerge when examining emotional intelligence, alexithymia, and emotional awareness, and they have been found to relate differentially to certain personality constructs. For example, emotional clarity was associated with neuroticism but not extroversion, whereas attention to emotions was associated with extroversion but not neuroticism (Coffey et al., 2003).
The Role of Emotional Clarity in SAD and Social Anxiety
Emotional clarity is a key part of emotion regulation, as being able to clearly identify one’s emotions is the first step in determining how to regulate and cope with them. Lower levels of emotional clarity have been linked to poorer psychosocial adjustment (Salguero, Palomera, & Fernandez-Berrocal, 2012). Conversely, greater emotional clarity has been linked to positive coping and greater well-being (Gohm & Clore, 2002). Extremera and Fernández-Berrocal (2005) found that emotional clarity predicted greater life satisfaction, even when accounting for other predictors such as neuroticism and negative mood. These findings suggest that being able to identify and describe one’s own emotions is important for psychosocial adjustment.
Emotional clarity has also been shown to be inversely related to social anxiety (SA). Greater ability to distinguish between moods and emotions (emotional clarity) is associated with lower levels of social anxiety (Salovey, Stroud, Woolery, & Epel, 2002). O’Toole, Hougaard, and Mennin (2013) conducted a meta-analysis of the relationship between social anxiety and emotion knowledge, a broader concept which includes both interpersonal and intrapersonal knowledge of emotions. In studies which used both self-report and behavioral tasks, there was a significant negative relationship between social anxiety and intrapersonal emotional knowledge in both individuals with SAD and in non-clinical socially anxious samples. Also, when compared to a low socially anxious group, highly socially anxious individuals had lower emotional clarity.
Using the Trait Meta Mood Scale (TMMS; Salovey, Mayer, Goldman, Turvey, & Palfai, 1995) clarity of emotions subscale, the Toronto Alexithymia Scale-20 (TAS-20; Bagby, Parker, & Taylor, 1994) difficulty identifying emotions subscale, and the TAS-20 difficulty describing emotions subscale, Turk, Heimberg, Luterek, Mennin, and Fresco (2005) found that those with higher levels of social anxiety had lower emotional clarity and more difficulty identifying their emotions compared to non-anxious controls. Individuals with higher levels of social anxiety also had greater difficulty describing their emotions compared to individuals with higher levels of generalized anxiety and non-anxious controls. Thompson, Boden, and Gotlib (2015) also found that, compared to non-anxious controls, individuals with SAD reported lower levels of emotional clarity. Furthermore, social anxiety, but not depression, was predicted by emotional clarity, which suggests that emotional clarity may play a specific role in social anxiety. Taken together, these findings suggest that individuals with SAD demonstrate lower clarity in identifying their emotions. This relationship is critical given that a lack of emotional clarity in social anxiety may lead to the use of emotional suppression and avoidance strategies, and these strategies tend to increase anxiety (Kashdan, Barrios, Forsyth, & Steger, 2006).
The Role of Attention to Emotions in SAD and SA
Attention to emotions has also been examined in individuals with social anxiety and SAD. Turk and colleagues (2005) found that individuals with higher levels of social anxiety were less attentive to emotions than those with higher levels of generalized anxiety or controls. Socially anxious students reported greater emotional suppression and difficulty attending to emotions (Spokas, Luterek, & Heimberg, 2009), further suggesting that lack of attention to emotion may be maladaptive for individuals with social anxiety. However, Salovey and colleagues (2002) found no relationship between SA and attention to emotions. There is also some research which suggests that elevated attention to emotions is not necessarily beneficial. For example, some studies using community samples have shown that attention to emotions is associated with greater affect instability, affect intensity, and emotional variability, suggesting a potentially deleterious effect of attention to emotions (Thompson, Dizen, & Berenbaum, 2009; Thompson et al., 2011). In a sample of participants with major depressive disorder, those who reported higher levels of attention to emotions during a depressive episode were less likely to be recovered fourteen months later (Thompson et al., 2013). It is possible that greater attention to emotions is most beneficial for those who are more effective at regulating their emotions and less so for those with poorer emotion regulation skills (Lischetzke & Eid, 2003). Further research is needed to clarify the relationship between attention to emotions and SA and to determine whether greater attention to emotions is linked to positive outcomes in the context of SAD.
Influencing Emotional Clarity and Attention to Emotions in SAD
Cognitive-behavioral group therapy (CBGT; Heimberg & Becker, 2002) and mindfulness-based stress reduction (MBSR; Kabat-Zinn & Santorelli, 1993) have both been found to produce significant symptom reduction among individuals with SAD (e.g., Goldin et al., 2016; Koszycki, Benger, Shlik, & Bradwejn, 2007). However, further research is needed to elucidate factors that play a role in determining who benefits most from which treatment (or from psychological treatment more generally). For example, those who pay less attention to emotions at baseline may benefit to a greater degree from MBSR given its focus on attention. One might also posit that those who have higher levels of emotional clarity at baseline may benefit more from CBGT given its focus on the impact of thoughts on physiological symptoms and emotions. However, it is possible that those with higher baseline levels of attention to emotions and emotional clarity may be more successful at attending to, identifying, and engaging with their emotions during treatment, making both CBGT and MBSR effective for them in reducing social anxiety.
Considering the relationship between emotional clarity and psychological well-being (Gohm & Clore, 2002; Salguero et al., 2012), it will also be important to elucidate which treatments produce the greatest increases in emotional clarity. Although there have not been previous investigations in SAD, Chung, Yoon, Park, Yang, and Oh (2013) found that difficulty identifying and describing feelings decreased and emotional clarity increased following CBGT for early psychosis. A few studies have also examined changes across treatment in alexithymia, which is characterized by poor emotional clarity, as well as reduced daydreaming, difficulty expressing feelings, and externally-oriented thinking, a factor highly overlapping with attention to emotions (Taylor, 1984). In a sample of patients with obsessive-compulsive disorder participating in CBT, Rufer et al. (2004) found that alexithymia did not change from pre- to posttreatment. However, Kimball (2000) found decreases in alexithymia from pre- to post-CBT in adult sexual assault survivors. Overall, these findings suggest that CBT may increase emotional clarity and attention to emotions. However, most of these studies examined alexithymia, so further research is needed to determine whether CBT affects emotional clarity and attention to emotions specifically.
More recently mindfulness meditation training programs such as MBSR have been used as interventions for anxiety disorders. MBSR teaches participants to attend fully to the present moment, even when the present experience is inherently painful, and to adopt a nonjudgmental attitude when attending to the present moment (Brantley, 2005). Although MBSR decreases fear of emotions and improves emotion regulation (Goldin & Gross, 2010; Robins, Keng, Ekblad, & Brantley, 2011), to the best of our knowledge, studies have not investigated whether MBSR increases emotional clarity or attention to emotions. However, there are a number of ways that MBSR could modify these emotional factors. It is possible that mindfulness meditation training could increase participants’ attention to emotions by way of increasing attention to the present moment. For example, one proposed mechanism of change in MBSR is interoceptive awareness via the body scan meditation, which involves directing attention to bodily sensations including those related to emotions and is thought to improve emotional awareness (Bechara & Naqvi, 2004; Hölzel, Ott, Hempel, & Stark, 2006). Furthermore, by adopting a nonjudgmental, observer view of the present experience, MBSR could increase emotional clarity by scaffolding a clearer perspective from which to identify specific emotions from moment to moment (Gu, Strauss, Bond, & Cavanagh, 2015).
The Present Study
The present study aimed to: (1) examine differences between individuals with SAD and healthy controls on emotional clarity and attention to emotions, (2) examine whether emotional clarity and attention to emotions change during treatment, whether changes are maintained at 12-month follow-up, and whether CBGT and MBSR exert differential effects on these variables, and (3) investigate whether emotional clarity and attention to emotions (pretreatment, posttreatment, and the change from pre- to posttreatment) moderate the effects of CBGT and MBSR on severity of social anxiety symptoms in adults with SAD.
We predicted that individuals with SAD would have significantly lower levels of pretreatment emotional clarity and attention to emotions compared to healthy controls. We also predicted that emotional clarity and attention to emotions would increase across treatment, regardless of treatment condition, and that improvements would persist at 12-month follow up. We expected those with higher emotional clarity and attention to emotions at pretreatment to experience greater decreases in social anxiety across treatment, and we expected the degree of increase in emotional clarity and attention to emotions from pre- to posttreatment to be associated with the degree of decrease in social anxiety.
Method
Participants
Participants were 108 individuals with generalized SAD based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; APA, 2000) and 37 controls who did not meet criteria for any current or past psychiatric disorders. Diagnostic assessment for all participants was conducted using the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994). To meet criteria for generalized SAD, patients had to endorse greater than moderate social fear in five or more different social situations. Clinicians rated the severity of the diagnosis on a scale from 0 to 8, with a rating of 4 or greater required for diagnosis. Doctoral clinical psychologists and doctoral students reviewed 20% of the cases; there was 100% agreement with the initial diagnosis and rating. To be eligible, patients also had to score greater than 60 on the Liebowitz Social Anxiety Scale-Self-Report (LSAS-SR; Fresco et al., 2001; Liebowitz, 1987). This cutoff score is indicative of generalized SAD, as determined previously by receiver operating characteristics analysis (Rytwinski et al., 2009). For both patients with SAD and controls, further exclusion criteria included: having received or participated in pharmacotherapy or psychotherapy in the past year, CBT for anxiety in the past two years, any MBSR course in the past, long-term meditation retreats or regular meditation practice (defined as 10 minutes at least 3 times weekly), a history of neurological, cardiovascular or thought disorders, or bipolar disorder. Participants were additionally required to be in remission from PTSD or alcohol/substance abuse or dependence for at least one year and to not report on the telephone screen significant symptoms of current major depressive disorder (MDD; 14 or more days of depressed mood in the past month) or obsessive compulsive disorder (OCD), given the likelihood that these symptoms would result in a primary diagnosis of MDD or OCD. However, at the in-person interview, clients with secondary MDD or OCD were permitted to enroll in the study. All participants gave informed consent. This study was approved by the Stanford University Institutional Review Board.
Recruitment took place over a two-year period during which 724 individuals completed the online screening survey. Of those, 307 participated in a telephone screening interview to determine potential eligibility; 173 individuals were potentially eligible and administered the ADIS-IV-L. The final 108 participants were those who met diagnostic and research criteria and completed the baseline assessments. These patients with SAD were randomized to either CBGT (n=36), MBSR (n=36), or WL (n=36) groups. The rate of attrition was low and consistent across conditions (total attrition, n = 8). See the CONSORT diagram in Goldin et al. (2016).
Treatments
Cognitive Behavioral Group Therapy (CBGT)
CBGT consisted of 12 weekly sessions which each lasted 2.5 hours. Therapists followed the Heimberg and Becker (2002) CBGT protocol for SAD. This protocol includes psychoeducation, orientation to CBGT, training in cognitive restructuring skills, graduated exposure to feared social situations, and relapse prevention and termination. Portions of the Hope, Heimberg and Turk (2010) client workbook were used to complement the weekly sessions.
Mindfulness-Based Stress Reduction (MBSR)
The MBSR group was structured so that there were 12 weekly 2.5 hour sessions, which was equivalent to the CBGT condition in amount of time spent in group meetings and number of sessions. The course curriculum largely followed an outline set forth by Kabat-Zinn and Santorelli in 1993, but the original outline included a full day meditation retreat which was not included in this study in order to maintain the same session structure as in CBGT. A Mindfulness Based Stress Reduction Workbook (Stahl & Goldstein, 2010) was also used to supplement the weekly sessions and included exercises and audio files to facilitate patients’ home practice.
Treatment adherence and patient attendance did not differ between CBGT and MBSR. Details are reported in Goldin et al. (2016).
Measures
Emotional clarity and attention to emotions were assessed using a 23-item scale developed by Palmieri, Boden, and Berenbaum (2009). The scale was derived by combining questions from the Clarity and Attention subscales of the TMMS and the Identifying Feelings and Externally Oriented Thinking subscales of the TAS-20. These items comprise two subscales which measure ability to attend to emotions (attention to emotions; 10 items) and ability to identify and understand one’s emotions (emotional clarity; 13 items). The attention to emotions subscale includes items such as “I don’t think it’s worth paying attention to our emotions or moods,” and the emotional clarity subscale includes items like “When I am upset, I don’t know if I am sad, frightened, or angry.” Participants indicated their responses on a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The clarity subscale has shown good internal consistency (α = .89) as has the attention subscale (α = .87), and both subscales demonstrate convergent validity through their correlations with openness to experience (i.e., openness to their own emotional experiences; Palmieri et al., 2009). In the current study, the internal consistency of the emotional clarity and attention to emotions subscales were demonstrated by alpha values of .93 and .79, respectively, in the total sample. In the sample of patients with SAD, the emotional clarity subscale showed excellent internal consistency (pretreatment: α = .92; posttreatment: α = .89; 12-month follow-up: α = .91) and the attention to emotions subscale showed adequate internal consistency (pretreatment: α = .77; posttreatment: α = .61; 12-month follow-up: α = .81).
Social anxiety was assessed using the LSAS-SR (Fresco et al., 2001; Liebowitz, 1987). The scale presents 13 performance situations and 11 social interaction situations and asks participants to rate both the severity of fear and anxiety experienced in a given situation from 0 (none) to 3 (severe) and the degree of avoidance of the situation from 0 (never) to 3 (usually; 68–100%). Scores are summed to create a total scale score of social anxiety severity. The LSAS-SR demonstrates excellent convergent validity as it correlates highly with other commonly used measures of social anxiety and avoidance such as the Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) and the Social Phobia Scale (SPS; Mattick & Clarke, 1998; Fresco et al., 2001). It has demonstrated adequate discriminant validity, as shown by comparisons of correlations between the LSAS-SR and other measures of social anxiety versus measures of depression such as the Beck Depression Inventory (Fresco et al., 2001). The total score has shown test-retest reliability over a 12-week interval (r = .83; Baker, Heinrichs, Kim, & Hofmann, 2002) and demonstrated good internal consistency in a sample of patients with SAD (α = .95) and among controls (α = .94; Fresco et al., 2001). In the current sample, the internal consistency of the LSAS-SR was excellent in the total sample (α = .92) and the sample of patients with SAD (pretreatment: α = .92; posttreatment: α = .92; 12-month follow-up: α = .96).
Procedure
Potential participants were identified through clinician referrals and community listings. Screenings were conducted via telephone followed by an in-person diagnostic interview to determine the participant’s history of Axis I disorders as well as symptom severity. As patients were admitted into the study, groups of six consecutive patients were placed in a group sequence at random, which resulted in six groups each of CBGT, MBSR and waitlist (WL). Patients in the CBGT and MBSR conditions completed self-report assessments at baseline, posttreatment, and 12-month follow-up. Patients in the WL condition completed assessments at baseline, post-WL (corresponding with posttreatment for the CBGT and MBSR conditions), after they had received one of the two treatments (randomly assigned), and 12-month follow-up. Treatment was provided at no cost, and patients received $150 compensation for completing the 12-month follow-up behavioral session. Controls were provided appropriate financial compensation for their time. Informed consent was obtained from all participants.
Results
Sample Demographics
There were no significant differences (all p’s >.05) between CBGT, MBSR, WL, and healthy control groups in terms of gender, age, education, ethnicity, marital status, or income. In patients with SAD, there were no differences between CBGT, MBSR, and WL conditions in terms of age at onset of SAD symptoms and years since onset. Information regarding the characteristics of participants in each condition is presented in Table 1. CBGT, MBSR, and WL also did not differ on current or past Axis I comorbidity. Rates of Axis I comorbidity in the sample are reported in Goldin et al. (2016).
Table 1.
Demographic information by condition
| CBGT (n = 36) | MBSR (n = 36) | WL (n = 36) | HC (n = 37) | |
|---|---|---|---|---|
| Males, n (%) | 16 (44.4%) | 16 (44.4%) | 16 (44.4%) | 15 (40.5%) |
| Age, M (SD) | 34.14 (8.05) | 29.90 (7.61) | 34.06 (7.78) | 32.07 (8.64) |
| Education, years M (SD) | 17.41 (3.29) | 16.22 (1.67) | 16.52 (2.93) | 17.39 (2.76) |
| Race/ethnicity, n (%) | ||||
| Caucasian | 18 (50.0%) | 14 (38.9%) | 15 (41.7%) | 19 (51.4%) |
| Asian | 15 (41.7%) | 13 (36.1%) | 14 (38.9%) | 12 (32.4%) |
| Hispanic/Latino | 2 (5.6%) | 7 (19.4%) | 1 (2.8%) | 3 (8.1%) |
| African American | 0 | 1 (2.8%) | 0 | 0 |
| American Indian/Alaskan Native | 0 | 0 | 1 (2.8%) | 0 |
| More than one race | 1 (2.8%) | 1 (2.8%) | 5 (13.9%) | 3 (8.1%) |
| Marital Status, n (%) | ||||
| Single, never married | 20 (55.6%) | 23 (63.9%) | 18 (50.0%) | 20 (54.1%) |
| Married | 12 (33.3%) | 8 (22.2%) | 16 (44.4%) | 10 (27%) |
| Living with partner | 3 (8.3%) | 5 (13.9%) | 1 (2.8%) | 3 (8.1%) |
| Divorced, separated, widowed | 1 (2.8%) | 0 | 0 | 4 (10.8%) |
| Missing or not reported | 0 | 0 | 1 (2.8%) | 0 |
| Income, n (%) | ||||
| <$10,000 | 3 (8.3%) | 3 (8.3%) | 1 (2.8%) | 1 (2.7%) |
| $10,000-$25,000 | 3 (8.3%) | 2 (5.6%) | 4 (11.1%) | 3 (8.1%) |
| $25,000-$50,000 | 5 (13.9%) | 5 (13.9%) | 5 (13.9%) | 9 (24.3%) |
| $50,000-$75,000 | 6 (16.7%) | 5 (13.9%) | 3 (8.3%) | 9 (24.3%) |
| $75,000-$100,000 | 4 (11.1%) | 3 (8.3%) | 4 (11.1%) | 4 (10.8%) |
| >$100,000 | 9 (25.0%) | 9 (25.0%) | 10 (27.8%) | 8 (21.6%) |
| Missing or not reported | 6 (16.7%) | 9 (25.0%) | 9 (25.0%) | 3 (8.1%) |
Note. Between group t-tests and χ2 tests were all nonsignificant (p > .05). CBGT = Cognitive Behavioral Group Therapy; MBSR = Mindfulness-Based Stress Reduction; WL = Waitlist; HC = Healthy Control Group.
Emotional Clarity and Attention to Emotions at Baseline
Baseline group differences between healthy controls and individuals with SAD on emotional clarity and attention to emotions were examined using a series of independent samples t-tests. Controls reported significantly higher levels of emotional clarity than individuals with SAD at baseline. There were no significant differences in attention to emotions between individuals with SAD and controls (See Table 2).
Table 2.
Means (and standard deviations) of measures at baseline in individuals with SAD and Controls
| Group | t (df) | Cohen’s d | ||
|---|---|---|---|---|
| SAD | Control | |||
| LSAS-SR | 90.69 (17.91) | 14.24 (9.46) | 24.76 (143)*** | 5.34 |
| Emotional Clarity | 42.59 (10.73) | 52.38 (6.84) | −5.19 (142)*** | 1.09 |
| Attention to Emotions | 38.22 (5.56) | 37.75 (5.66) | 0.43 (142) | 0.08 |
Note. LSAS-SR = Liebowitz Social Anxiety Scale - self-report version.
p < .05,
p < .01,
p < .001
At pretreatment for patients with SAD, the bivariate correlations between the LSAS-SR and emotional clarity (r=−.07) and attention to emotions (r=−025) were not significant (p’s>.05). Emotional clarity and attention to emotions were significantly but moderately correlated at baseline, r=.37, p<.01.
Effects of Treatment on Emotional Clarity and Attention to Emotions
We examined whether emotional clarity and attention to emotions changed differentially from pre- to posttreatment as a function of treatment condition. We examined change from pre-to post-treatment/waitlist with the CBGT, MBSR, and WL conditions in the model. We used the MIXED procedure in SPSS (Version 24) to apply linear mixed-effects models (LMMs). Random intercepts were included in the model. Maximum likelihood estimation was used to address missing data at posttreatment/waitlist, so cases with missing data were not excluded. Within-group effect sizes are calculated as Cohen’s d (Cohen, 1988) and used the differences in estimated marginal means divided by the pooled within-group standard deviation (Dunlap, Cortina, Vaslow, & Burke, 1996).
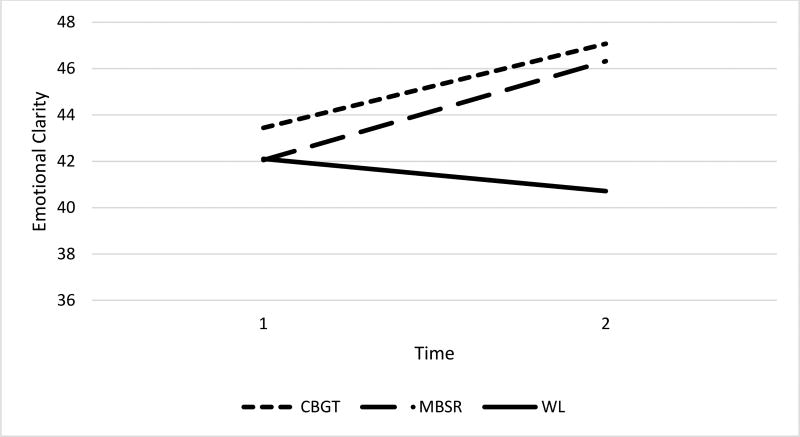
First, we used LMMs to compare emotional clarity from pretreatment to post-treatment/waitlist for the MBSR, CBGT, and WL conditions. See Table 3 for estimated marginal means relevant to this set of LMMs analyses. There was a main effect of Time such that emotional clarity scores increased from pre- to post-treatment/waitlist, F(1, 92.60) = 4.46, p = .037. There was no main effect of Treatment Condition on emotional clarity, F(2, 107.89) = 1.12, p = .33. However, the main effect of Time was qualified by a significant Treatment Condition by Time interaction, F(2, 92.53) = 4.14, p = .019 (see Figure 1). Planned contrasts using estimated marginal means revealed that emotional clarity at post-treatment/waitlist was significantly higher for CBGT versus WL, t(101.98) = 2.22, p = .028, d = 0.26. There were no significant differences in emotional clarity at post-treatment/waitlist between MBSR and CBGT, t(107.19) = 0.57, p = .57, d = 0.07, or between MBSR and WL, t(104.59) = 1.62, p = .11, d = 0.19. To be conservative, the alpha level was controlled at .05 for all post hoc contrasts using Dunn-Sidak.
Table 3.
Estimated marginal means (and standard errors) of emotional clarity and attention to emotions at pretreatment and post-WL by treatment condition.
| CBGT (n = 36) |
MBSR (n = 36) |
WL (n = 36) |
|
|---|---|---|---|
| Emotional Clarity | |||
| Pretreatment | 43.44 (1.78) | 42.06 (1.78) | 42.11 (1.79) |
| Post-WL | 46.58 (1.89) | 45.04 (1.93) | 40.72 (1.84) |
| Attention to Emotions | |||
| Pretreatment | 38.61 (0.91) | 39.03 (0.91) | 36.96 (0.91) |
| Post-WL | 39.07 (0.92) | 39.79 (0.94) | 36.38 (0.89) |
Figure 1.
Trajectory of change in emotional clarity from pretreatment to post-treatment/waitlist for cognitive behavioral group therapy (CBGT), mindfulness-based stress reduction (MBSR), and waitlist (WL) conditions based on estimated marginal means.
Next, we used LMMs to compare emotional clarity at pretreatment, posttreatment, and 12-month follow-up for CBGT and MBSR. For these analyses, waitlist patients’ scores after they participated in treatment were included, and the treatment conditions included in the model were CBGT and MBSR. See Table 4 for estimated marginal means and standard errors for this set of analyses. There was a significant main effect of Time, F(2, 77.81) = 6.96, p = .002. There was no main effect of Treatment Condition and no Time by Treatment Condition interaction, p’s > .05. Planned pairwise contrasts using estimated marginal means revealed that, in the CBGT condition, emotional clarity was significantly higher at posttreatment compared to pretreatment, t(81.16) = 2.43, p = .05, d = 0.25. Emotional clarity remained significantly higher at 12-month follow-up compared to pretreatment in the CBGT condition, t(86.82) = 2.89, p = .014, d =.30. There were no significant differences in scores across time in the MBSR condition (all p’s > .05).
Table 4.
Estimated marginal means (and standard error) of emotional clarity and attention to emotions at pretreatment, posttreatment, and 12-month follow up by treatment condition.
| CBGT (n = 54) |
MBSR (n = 54) |
|
|---|---|---|
| Emotional Clarity | ||
| Pretreatment | 43.10 (1.42) | 42.32 (1.41) |
| Posttreatment | 45.79 (1.43) | 44.19 (1.53) |
| 12-month follow-up | 46.49 (1.49) | 45.03 (1.59) |
| Attention to Emotions | ||
| Pretreatment | 37.71 (0.79) | 38.76 (0.78) |
| Posttreatment | 37.48 (0.77) | 38.81 (0.82) |
| 12-month follow-up | 37.08 (0.85) | 38.03 (0.91) |
We also used LMMs to test whether there were significant differences in the effects of CBGT, MBSR, or WL condition on attention to emotions from pretreatment to post-treatment/waitlist (see Table 3). There was no main effect of Time, F = 0.36, p = .55, or Treatment Condition on attention to emotions, F = 2.84, p = .06. The Treatment Condition by Time interaction was not significant for attention to emotions, F = 1.34, p = .27.
Next, we used LMMs to compare attention to emotions at pretreatment, posttreatment, and 12-month follow-up for CBGT and MBSR (See Table 4). These analyses also included waitlist patients’ scores after receiving treatment. There was no main effect of Time or Treatment Condition, and there was no Time by Treatment Condition interaction, all p’s > .05.
Moderation of Treatment Outcome
To conduct moderation analyses, we used multiple imputation to handle missing data at posttreatment and follow-up time points. Analyses were run in Mplus Version 7.31 (Muthén & Muthén, 2015). Pre- and posttreatment emotional clarity and attention to emotions scores were mean centered. Posttreatment scores include those who were treated after the waitlist, so analyses reflect the entire sample of treated patients with SAD.
Pretreatment emotional clarity did not significantly predict change in LSAS scores from pre- to posttreatment, b = −.24, t(104) = −1.10, p = .27, d = 0.22. Treatment Condition predicted change in LSAS scores from pre- to posttreatment with marginal significance, b = 8.75, t(104) = 1.94, p = .053, d = 0.38. Pretreatment emotional clarity did not interact with treatment group to moderate the degree of change in LSAS total scores from pre- to posttreatment b = .02, t(103) = .04, p = .97, d = 0.007.
The change in emotional clarity from pre- to posttreatment significantly predicted changes in LSAS scores from pre- to posttreatment, b = −.96, t(103) = −2.92, p < .01, d = 0.58. In this analysis, Treatment Condition did not predict pre- to posttreatment changes in LSAS scores, b = 7.75, t(103) = 1.79, p = .07, d = 0.35. Changes in emotional clarity from pre- to posttreatment did not significantly interact with Treatment Condition to moderate changes in LSAS scores from pre- to posttreatment, b = .62, t(103) = 1.00, p = .32, d = 0.20.
The change in emotional clarity from pre- to posttreatment significantly predicted changes in LSAS scores from pretreatment to 12-month follow-up, b = −1.05, t(103) = −2.55, p = .01, d = 0.50. Treatment Condition did not predict changes in LSAS scores from pretreatment to 12-month follow-up, b = 4.33, t(103) = .81, p = .42, d = 0.16. Changes in emotional clarity from pre- to posttreatment did not significantly interact with Treatment Condition to moderate changes in LSAS scores from pretreatment to 12-month follow-up, b = .06, t(103) = .08, p = .93, d = 0.016.
The level of emotional clarity at posttreatment predicted LSAS scores at 12-month follow-up, b = −0.49, t(104) = −2.16, p = .03, d = 0.42. The interaction between emotional clarity at posttreatment and Treatment Condition did not predict 12-month follow-up scores, b = .60, t(104) = 1.39, p = .16, d = 0.27.
Moderation analyses were conducted with attention to emotions as the moderator. All results were non-significant (p>.05) and are included as supplementary material.
Discussion
This study aimed to examine differences in emotional clarity and attention to emotions between healthy controls and patients with SAD, the effects of CBGT and MBSR on emotional clarity and attention to emotions, whether baseline and posttreatment levels of emotional clarity and attention to emotions moderate treatment outcome, and whether changes in emotional clarity and attention to emotions predict changes in SA.
Our hypotheses regarding emotional clarity were partially supported. Those with SAD had lower levels of emotional clarity at baseline compared to healthy controls, corroborating the existing evidence that emotional clarity deficits exist in SAD (O’Toole et al., 2013; Thompson et al., 2015; Turk et al., 2005). Emotional clarity also increased across treatment such that patients who received CBGT had higher levels of emotional clarity at posttreatment compared to patients in the WL condition. At posttreatment, patients who received MBSR did not differ from those who were assigned to either CBGT or WL. These findings suggest that CBGT had an effect on individuals’ ability to identify and describe their emotional experiences, which converges with prior studies which found that emotional clarity (as a component of alexithymia) increases following CBT for other disorders (Chung et al., 2013; Kimball, 2000). Because levels of emotional clarity in the MBSR condition did not differ from the CBGT condition at posttreatment, there is some evidence that both CBGT and MBSR generate change in emotional clarity. However, the lack of statistical difference in emotional clarity in the MBSR and waitlist conditions at posttreatment tempers this conclusion. Further research should focus on clarifying whether emotional clarity is enhanced following MBSR and could examine variables such as amount of meditation practice which may explain the degree of change in emotional clarity.
Changes in emotional clarity from pre- to posttreatment predicted changes in social anxiety from pre- to posttreatment and from pretreatment to 12-month follow-up. This phenomenon may be explained by treatment’s dual effect on both emotional clarity and social anxiety symptoms, but it may also suggest that increases in emotional clarity are tied to decreases in social anxiety. As patients’ ability to identify and describe emotions increases, they may then be able to apply appropriate strategies learned in treatment (e.g., cognitive reappraisal) to effectively regulate emotions. Boden and colleagues (2012) found that high levels of emotional clarity and the use of cognitive reappraisal interact to predict less severe PTSD symptoms and greater positive affect. This aligns with research suggesting that the relationship between poor emotional clarity and social anxiety is mediated by difficulty employing emotion regulation strategies and difficulty accepting emotions (Vine & Aldao, 2014). Emotional clarity may be a necessary prerequisite to the effective use of emotion regulation strategies. Further research is needed to determine whether there is a causal relationship between changes in emotional clarity and changes in social anxiety and could examine whether emotional clarity is a mediator or mechanism of change for treatment of SAD.
Emotional clarity at baseline did not moderate treatment outcome. These findings suggest that baseline levels of emotional clarity do not affect the degree to which an individual will benefit from MBSR or CBGT. This was unexpected given the aforementioned research which found that emotional clarity and cognitive reappraisal interact to predict lower severity of symptoms in a sample of individuals with PTSD (Boden et al., 2012). However, this research was cross-sectional and not in the context of treatment. One possible explanation may be that those who begin treatment with higher emotional clarity are more readily able to benefit from treatment and may respond more quickly to treatment, but individuals with lower emotional clarity at baseline are able to gain emotional clarity through treatment and ultimately benefit to the same degree by the end of treatment. Future research will be needed to determine the nature of the effects of heightened emotional clarity at baseline on changes in social anxiety throughout the course of treatment.
We did not find support for our hypotheses regarding attention to emotions. Attention to emotions did not differ between those with SAD and controls. Similarly, attention to emotions did not change across treatment and was not a moderator of treatment outcome. These results diverge from previous research which suggests that those with SAD pay less attention to emotions (Spokas et al., 2009; Turk et al., 2005). However, similar to our finding, prior research (e.g., Salovey et al., 2002) found no relationship between social anxiety and attention to emotions. One potential reason for the mixed findings regarding attention to emotions may stem from differences in the nature of the attention participants are paying to their emotions. Perhaps prior to treatment, participants are more prone to attend to anxiety and negative emotions, whereas after treatment they may be attending to their emotions in a more positive or non-judgmental way. Furthermore, research suggests that distinguishing between voluntary and involuntary attention to emotions is important, as the two are differentially related to emotional clarity (Huang, Berenbaum, & Chow, 2013). Because the data collected in this study did not tap into the type of the attention or to what participants attended, we were unable to test this potential explanation for our findings. It is also possible that increased attention to emotions may reflect heightened intensity of affect, which would make increases in attention to emotions unlikely to positively impact treatment outcome. Thompson et al. (2011) used experience sampling methods to investigate the relationship between attention to emotions and affect and found that attention to emotions was related to greater intensity of both positive and negative affect in that moment, but predicted later reduction in negative affect. This suggests that attention to emotions is related to emotional intensity, which may be a factor worth targeting in an attempt to enhance treatment outcome. As the current literature on attention to emotions in SAD is mixed, it will be important to continue investigating the impact of increased attention to emotions on anxiety symptoms. Future research should clarify the nature of the attention being paid to emotions in order to fully understand this relationship.
The current study had a number of strengths. Primarily, emotional clarity and attention to emotions were investigated for the first time in the context of treatment for SAD. Because the study included both CBGT and MBSR, we were able to examine whether the treatments differentially impacted emotional clarity and attention to emotions. However, the study is not without limitations. We used a self-report measure of emotional clarity and attention to emotions derived from the TMMS and TAS-20, and although the measure has been validated and used in previous research (Palmieri et al., 2009), it may be particularly useful to look at specific facets of emotional clarity (e.g., source and type clarity) and attention to emotions rather than the broader constructs (Boden & Thompson, 2015). Our findings may be measure-specific, and future research should strive to replicate these findings using other measures of these constructs. Furthermore, future research should focus on the construction and validation of behavioral measures of emotional clarity and attention to emotions so that these constructs can be measured in a multimodal fashion. Finally, due to the exclusionary criteria employed in this study, rates of comorbid MDD were suppressed. Going forward, research should examine how current comorbid MDD affects changes in emotional clarity and attention to emotion during treatment and the effect that these factors have on treatment outcome for SAD.
Our study’s findings are an important basis from which to begin exploring the impact of different treatments on emotional clarity and attention to emotions. Taking into account the association between emotional clarity, psychosocial well-being, and life satisfaction (Extremera & Fernández-Berrocal, 2005; Gohm & Clore, 2002; Salguero et al., 2012), determining which treatments increase emotional clarity to the greatest degree will allow us to treat social anxiety while simultaneously fostering emotional clarity. Treatments which impact both social anxiety and emotional clarity could enhance psychosocial well-being to an even greater degree. Finally, continuing to examine other facets of emotional intelligence such as emotional intensity as potential factors which may impact treatment response will help identify which participants would benefit most from specific treatment options. Ultimately, this research will refine the implementation of evidence-based treatment options by allowing clinicians to make informed decisions about which treatment options would best serve clients based on specific strengths and deficits they present.
Supplementary Material
Highlights.
We examined emotional clarity (EC) and attention to emotion in patients with social anxiety disorder (SAD).
Patients demonstrated lower levels of EC than healthy controls.
Cognitive-behavioral group therapy increased EC more than a waitlist.
Mindfulness-based stress reduction did not increase EC more than a waitlist.
Changes in emotional clarity predicted changes in social anxiety.
Analyses involving attention to emotions were not significant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aderka IM, Hofmann SG, Nickerson A, Hermesh H, Gilboa-Schechtman E, Marom S. Functional impairment in social anxiety disorder. Journal of Anxiety Disorders. 2012;26:393–400. doi: 10.1016/j.janxdis.2012.01.003. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.) Washington, DC: Author; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Press, Inc.; 2013. [Google Scholar]
- Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, Hofmann SG. The Liebowitz Social Anxiety Scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy. 2002;40:701–715. doi: 10.1016/S0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Bechara A, Naqvi N. Listening to your heart: Interoceptive awareness as a gateway to feeling. Nature Neuroscience. 2004;7:102–103. doi: 10.1038/nn0204-102. [DOI] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Kashdan TB, Alvarez J, Gross JJ. The interactive effects of emotional clarity and cognitive reappraisal in posttraumatic stress disorder. Journal of Anxiety Disorders. 2012;26:233–238. doi: 10.1016/j.janxdis.2011.11.007. [DOI] [PubMed] [Google Scholar]
- Boden MT, Thompson RJ. Facets of emotional awareness and associations with emotion regulation and depression. Emotion. 2015;15:399–410. doi: 10.1037/emo0000057. [DOI] [PubMed] [Google Scholar]
- Brantley J. Mindfulness-based stress reduction. In: Orsillo SM, Roemer L, editors. Acceptance and mindfulness-based approaches to anxiety: Conceptualization and treatment. New York, NY: Springer; 2005. pp. 131–145. [DOI] [Google Scholar]
- Chung YC, Yoon KS, Park TW, Yang JC, Oh KY. Group cognitive-behavioral therapy for early psychosis. Cognitive Therapy and Research. 2013;37:403–411. doi: 10.1007/s10608-012-9460-9. [DOI] [Google Scholar]
- Coffey E, Berenbaum H, Kerns JG. The dimensions of emotional intelligence, alexithymia, and mood awareness: Associations with personality and performance on an emotional Stroop task. Cognition and Emotion. 2003;17:671–679. doi: 10.1080/02699930302304. [DOI] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Earlbaum Associates, Inc.; 1988. [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) New York, NY: Oxford University Press; 1994. [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. doi: 10.1037/1082-989X.1.2.170. [DOI] [Google Scholar]
- Extremera N, Fernández-Berrocal P. Perceived emotional intelligence and life satisfaction: Predictive and incremental validity using the Trait Meta-Mood Scale. Personality and Individual Differences. 2005;39:937–948. doi: 10.1016/j.paid.2005.03.012. [DOI] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/S0033291701004056. [DOI] [PubMed] [Google Scholar]
- Gohm CL, Clore GL. Four latent traits of emotional experience and their involvement in well-being, coping, and attributional style. Cognition & Emotion. 2002;16:495–518. doi: 10.1080/02699930143000374. [DOI] [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10:83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2016;84:427–437. doi: 10.1037/ccp0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of meditation studies. Clinical Psychology Review. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York: Guilford Press; 2002. [Google Scholar]
- Hölzel BK, Ott U, Hempel H, Stark R. Wie wirkt Achtsamkeit? Eine Interviewstudie mit erfahrenen Meditierenden (How does mindfulness work? An interview study with experienced meditators); Paper presented at the 24th Symposium of the Section for Clinical Psychology and Psychotherapy of the German Society for Psychology; Würzburg, Germany. 2006. May, [Google Scholar]
- Hope DA, Heimberg RG, Turk CL. Managing social anxiety: A cognitive-behavioral Therapy Approach (Client Workbook, 2nd edition) New York: Oxford University Press; 2010. [Google Scholar]
- Huang S, Berenbaum H, Chow PI. Distinguishing voluntary from involuntary attention to emotion. Personality and Individual Differences. 2013;54:894–898. doi: 10.1016/j.paid.2012.12.025. [DOI] [Google Scholar]
- Kabat-Zinn J, Santorelli S. Mindfulness-based stress reduction professional training resource manual. Center for Mindfulness in Medicine, Health Care and Society; Worchester, MA: 1993. [Google Scholar]
- Kashdan TB, Barrios V, Forsyth JP, Steger MF. Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behaviour Research and Therapy. 2006;44:1301–1320. doi: 10.1016/j.brat.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas K, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimball LA. Alexithymia in survivors of sexual assault: Predicting treatment outcome. Doctoral dissertation. University of Missouri; St. Louis: 2000. [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy. 2007;45:2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Levy RL. Social support and compliance: A selective review and critique of treatment integrity and outcome measurement. Social Science & Medicine. 1983;17:1329–1338. doi: 10.1016/0277-9536(83)90192-2. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Lischetzke T, Eid M. Is attention to feelings beneficial or detrimental to affective well-being? Mood regulation as a moderator variable. Emotion. 2003;3:361–377. doi: 10.1037/1528-3542.3.4.361. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/S0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide, Seventh Edition. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- O’Toole MS, Hougaard E, Mennin D. Social anxiety and emotion knowledge: A meta-analysis. Journal of Anxiety Disorders. 2013;27:98–108. doi: 10.1016/j.janxdis.2012.09.005. [DOI] [PubMed] [Google Scholar]
- Palmieri PA, Boden MT, Berenbaum H. Measuring clarity of and attention to emotions. Journal of Personality Assessment. 2009;91:560–567. doi: 10.1080/00223890903228539. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35:741–756. doi: 10.1016/S0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Robins CJ, Keng SL, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: A randomized controlled trial. Journal of Clinical Psychology. 2012;68:117–131. doi: 10.1002/jclp.20857. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Fernandez KC, Levinson CA. Testing the effects of social anxiety disorder on friendship quality across gender and ethnicity. Cognitive Behaviour Therapy. 2012;41:130–139. doi: 10.1080/16506073.2012.661451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rufer M, Hand I, Braatz A, Alsleben H, Fricke S, Peter H. A prospective study of alexithymia in obsessive-compulsive patients treated with multimodal cognitive-behavioral therapy. Psychotherapy and Psychosomatics. 2004;73:101–106. doi: 10.1159/000075541. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychological Medicine. 2008;38:15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowitz MR, Cissell S, Hofmann SG. Screening for social anxiety disorder with the self-report version of the Liebowitz Social Anxiety Scale. Depression and Anxiety. 2009;26:34–38. doi: 10.1002/da.20503. [DOI] [PubMed] [Google Scholar]
- Simon NM, Otto MW, Korbly NB, Peters PM, Nicolaou DC, Pollack MH. Quality of life in social anxiety disorder compared with panic disorder and the general population. Psychiatric Services. 2002;53:714–718. doi: 10.1176/appi.ps.53.6.714. [DOI] [PubMed] [Google Scholar]
- Salguero JM, Palomera R, Fernández-Berrocal P. Perceived emotional intelligence as predictor of psychological adjustment in adolescents: A 1-year prospective study. European Journal of Psychology of Education. 2012;27:21–34. doi: 10.1007/s10212-011-0063-8. [DOI] [Google Scholar]
- Salovey P, Mayer JD. Emotional intelligence. Imagination, Cognition, and Personality. 1990;9:185–211. [Google Scholar]
- Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional attention, clarity, and repair: Exploring emotional intelligence using the Trait Meta-Mood Scale. In: Pennebaker JW, editor. Emotion, Disclosure, and Health. Washington DC: US: American Psychological Association; 1995. pp. 125–154. [DOI] [Google Scholar]
- Salovey P, Stroud LR, Woolery A, Epel ES. Perceived emotional intelligence, stress reactivity, and symptom reports: Further explorations using the Trait Meta-Mood Scale. Psychology and Health. 2002;17:611–627. doi: 10.1080/08870440290025812. [DOI] [Google Scholar]
- Spokas M, Luterek JA, Heimberg RG. Social anxiety and emotional suppression: The mediating role of beliefs. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:283–291. doi: 10.1016/j.jbtep.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Stahl B, Goldstein E. A mindfulness-based stress reduction workbook. New Harbinger Publications; 2010. [Google Scholar]
- Taylor GJ. Alexithymia: Concept, measurement, and implications for treatment. American Journal of Psychiatry. 1984;141:725–732. doi: 10.1176/ajp.141.6.725. [DOI] [PubMed] [Google Scholar]
- Thompson RJ, Boden MT, Gotlib IH. Emotional variability and clarity in depression and social anxiety. Cognition and Emotion. 2015:1–11. doi: 10.1080/02699931.2015.1084908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RJ, Dizen M, Berenbaum H. The unique relations between emotional awareness and facets of affective instability. Journal of Research in Personality. 2009;43:875–879. doi: 10.1016/j.jrp.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, Gotlib IH. Concurrent and prospective relations between attention to emotion and affect intensity: An experience sampling study. Emotion. 2011;11:1489–1494. doi: 10.1037/a0022822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, Gotlib IH. The role of attention to emotion in recovery from major depressive disorder. Depression Research and Treatment. 2013;2013:1–6. doi: 10.1155/2013/540726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk CL, Heimberg RG, Luterek JA, Mennin DS, Fresco DM. Emotion dysregulation in generalized anxiety disorder: A comparison with social anxiety disorder. Cognitive Therapy and Research. 2005;29:89–106. doi: 10.1007/s10608-005-1651-1. [DOI] [Google Scholar]
- Vine V, Aldao A. Impaired emotional clarity and psychopathology: A transdiagnostic deficit with symptom-specific pathways through emotion regulation. Journal of Social and Clinical Psychology. 2014;33:319–342. doi: 10.1521/jscp.2014.33.4.319. [DOI] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Rodebaugh TL, Norton PJ. Exploring the relationship between fear of positive evaluation and social anxiety. Journal of Anxiety Disorders. 2008;22:386–400. doi: 10.1016/j.janxdis.2007.04.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.