Case Vignette
A 54-year-old man was referred for split-night polysomnography due to snoring and excessive daytime sleepiness. His past medical history was notable for atrial fibrillation and type 2 diabetes mellitus. His physical exam was notable for class 3 obesity, with a body mass index of 51 kg/m2, and Mallampati class 3 airway.
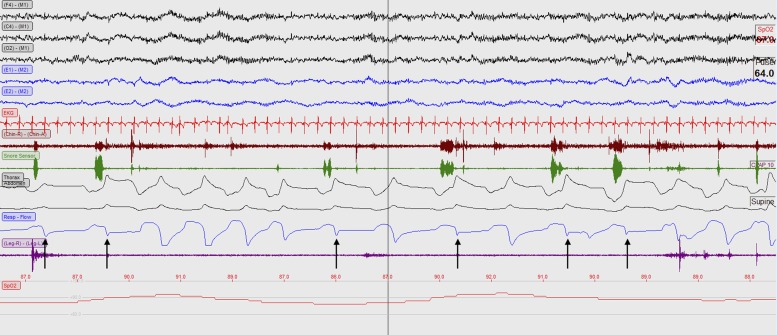
On polysomnography, he met split night criteria after 2 hours of diagnostic sleep time. During the diagnostic portion of the study, the patient displayed very severe obstructive sleep apnea, with a 4% apnea–hypopnea index of 112 events per hour. During continuous positive airway pressure (CPAP) titration using a nasal interface, the epoch depicted in Figure 1 was recorded at a CPAP pressure of 10 cm H2O.
Figure 1.
A 60-second epoch from the titration portion of the study with 10 cm of continuous positive airway pressure using a nasal mask. Breaths of interest are marked with upward black arrows.
Questions
1. What is notable about the expiratory limb of the CPAP airflow waveform, as shown in Figure 1?
2. What are potential remedies that can be employed?
Discussion
During positive airway pressure (PAP) titration, loss of a portion of the expiratory limb of the PAP waveform was seen, resulting in a pattern resembling the square root symbol. The “square root sign” observed in this case occurred because oral leak limited expiratory airflow from reaching the CPAP flow sensor. To appreciate oral leak on flow waveforms, it is essential that one is confident in the accurate orientation of the flow signal relative to inspiration and expiration. This can be achieved by examining biocalibrations, observing characteristics typically seen during inspiration (inspiratory flow limitation and snoring), and noting the steep downslope on expiration seen when flow signal is oriented with inspiration as an upward deflection.
In our experience, the “square root sign” is frequently associated with oral leak. In this case, we were confident that this was oral leak due to the sleep technologist’s observation of oral leak as well as video confirmation of an open mouth. Our experience illustrates that the detection of expiratory leak often requires vigilance and a high degree of suspicion on the part of the technician. A thermistor placed in front of the patient’s mouth may also help detect mouth breathing during CPAP titration with a nasal interface.
Oral leak is a common complication of PAP therapy delivered via a nasal mask for obstructive sleep apnea. It results in diversion of effective pressure, and, in turn, can cause oral dryness, reduce the efficacy of PAP therapy, and disrupt sleep (1). Moreover, failure to recognize oral leak may result in overtitration.
In a population of patients with oral leak, chinstrap use was associated with reduced leak, increased PAP adherence, and reduced frequency of obstructive events (2). The use of an oronasal mask is another option supported by American Academy of Sleep Medicine Practice Parameters (3). Enthusiasm for oronasal masks is tempered somewhat by greater mask leak compared with nasal masks in a randomized cross-over trial (4), and greater adherence to PAP therapy with nasal versus oronasal masks (5). Ultimately, mask selection and chinstrap use is an individualized decision that is best made after taking patient preferences and comfort into account.
There is also a bidirectional relationship between oral leak and increased nasal resistance, with nasal resistance contributing to mouth breathing (6), and oral leak increasing nasal resistance (7). Therefore, efforts to reduce nasal resistance, including nasal dilators and decongestants (6) may be helpful in reducing oral leak.
Answers
-
1. What is notable about the expiratory limb of the CPAP airflow waveform, as shown in Figure 1?
Figure 1 demonstrates a loss of a portion of the expiratory limb of the CPAP airflow waveform, indicating expiratory leak and results in a pattern that approximates the square root symbol.
-
2. What are potential remedies that can be employed?
Mask adjustment or replacement should be considered for expiratory leak originating from the skin–mask interface. In the presence of expiratory leak due to oral leak, a chinstrap can be applied to maintain mouth closure, although the use of an oronasal mask can be a potentially effective alternative.
Follow-Up
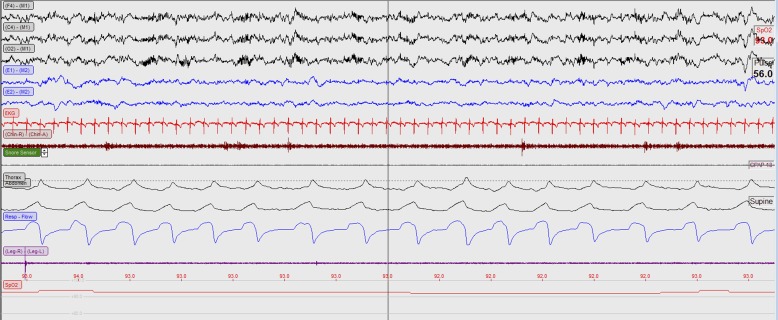
After oral leak was effectively treated, some flow limitation remained, as seen on the inspiratory portion of several breaths in Figure 2. After CPAP was increased from 10 to 18 cm H2O, flow limitation and oxygenation improved (Figure 3).
Figure 2.
A 60-second epoch from the titration portion of the study with 12 cm of continuous positive airway pressure using a nasal mask and chinstrap.
Figure 3.
A 60-second epoch from the titration portion of the study with 18 cm of continuous positive airway pressure using a nasal mask and chinstrap.
Supplementary Material
Footnotes
Supported by U.S. National Institutes of Health grant T32HL007287-38.
The views expressed here are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M. Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J. 1999;14:1251–1257. doi: 10.1183/09031936.99.14612519. [DOI] [PubMed] [Google Scholar]
- 2.Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10:377–383. doi: 10.5664/jcsm.3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, et al. American Academy of Sleep Medicine. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–380. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 4.Bakker JP, Neill AM, Campbell AJ. Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath. 2012;16:709–716. doi: 10.1007/s11325-011-0564-3. [DOI] [PubMed] [Google Scholar]
- 5.Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53:290–292. doi: 10.1136/thx.53.4.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLean HA, Urton AM, Driver HS, Tan AK, Day AG, Munt PW, et al. Effect of treating severe nasal obstruction on the severity of obstructive sleep apnoea. Eur Respir J. 2005;25:521–527. doi: 10.1183/09031936.05.00045004. [DOI] [PubMed] [Google Scholar]
- 7.Richards GN, Cistulli PA, Ungar RG, Berthon-Jones M, Sullivan CE. Mouth leak with nasal continuous positive airway pressure increases nasal airway resistance. Am J Respir Crit Care Med. 1996;154:182–186. doi: 10.1164/ajrccm.154.1.8680678. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.