Abstract
Objective
To determine the feasibility of a randomised controlled trial of an internet intervention for low back pain (LBP) using three arms: (1) usual care, (2) usual care plus an internet intervention or (3) usual care plus an internet intervention with additional physiotherapist telephone support.
Design and setting
A three-armed randomised controlled feasibility trial conducted in 12 general practices in England.
Participants
Primary care patients aged over 18 years, with current LBP, access to the internet and without indicators of serious spinal pathology or systemic illness.
Interventions
The ‘SupportBack’ internet intervention delivers a 6-week, tailored programme, focused on graded goal setting, self-monitoring and provision of tailored feedback to encourage physical activity. Additional physiotherapist telephone support consisted of three brief telephone calls over a 4-week period, to address any concerns and provide reassurance.
Outcomes
The primary outcomes were the feasibility of the trial design including recruitment, adherence and retention at follow-up. Secondary descriptive and exploratory analyses were conducted on clinical outcomes including LBP-related disability at 3 months follow-up.
Results
Primary outcomes: 87 patients with LBP were recruited (target 60–90) over 6 months, and there were 3 withdrawals. Adherence to the intervention was higher in the physiotherapist-supported arm, compared with the stand-alone internet intervention. Trial physiotherapists adhered to the support protocol. Overall follow-up rate on key clinical outcomes at 3 months follow-up was 84%.
Conclusions
This study demonstrated the feasibility of a future definitive randomised controlled trial to determine the clinical and cost-effectiveness of the SupportBack intervention in primary care patients with LBP.
Trial registration number
ISRCTN31034004; Results.
Keywords: low back pain, internet intervention, self-management, primary care
Strengths and limitations of this study.
This is the first pragmatic feasibility trial examining an internet intervention specifically designed for patients with low back pain consulting in general practice.
The feasibility of two methods of delivery was determined; providing the internet intervention with and without telephone physiotherapist support.
Follow-up was relatively short at 3 months; it is unclear whether response rates would remain similar at additional follow-up points necessary for a definitive trial.
Background
Low back pain (LBP) causes more global disability than any other condition,1 and has a lifetime prevalence of up to 85%.2 The economic costs of LBP have been reported at £12.3 billion per annum in the UK alone.3 In those who consult in primary care, pain trajectories often remain stable, with patients who report persistent-mild to persistent-severe pain, often remaining in the same pain grouping at 7-year follow-up.3 Chronic LBP, with a prevalence of 3%–10%,4 is associated with depression, anxiety, deactivation, inability to work and substantial societal costs.2 5
The recently updated National Institute for Health and Care Excellence guidelines for managing LBP continue to state the importance of self-management and advice to remain active.6 Identifying effective means to support behavioural self-management is becoming increasingly important; a recent review questioned the effectiveness of paracetamol for spinal pain,7 8 and concerns continue to grow regarding the adverse effects of prescriptions for opioid-related painkillers.9 In primary care, general practitioners (GPs) are unlikely to have the time or the training to deliver effective self-management support, and access to National Health Service (NHS) such as physiotherapy are often limited, with long waiting times for patients.10 There is a critical need for novel interventions enabling primary care practitioners to provide their patients with LBP immediate access to evidence-based, accessible self-management advice and support.
Internet interventions are automated, structured programmes delivering tailored advice over time through text and audio-visual content.11 They differ from simple health information webpages, which in the case of LBP are abundant and often of low quality.12 Internet interventions may offer a useful resource for primary care practitioners to draw on. Research on internet interventions for LBP is at an early stage: a recent systematic review of nine randomised controlled trials (RCTs) of internet interventions for chronic LBP13 concluded that despite showing some promise, many of the trials were limited by small samples sizes,14 15 comparisons to waiting lists or no treatment controls16 and researchers rarely considered healthcare resource use.13 To our knowledge, there have been no trials of internet interventions developed specifically for patients with LBP consulting in primary care. As primary care practitioners see the full spectrum of patients with LBP, ideal interventions for this context would offer effective self-management advice for those with acute, recurrent and chronic presentations, facilitating simple implementation.
‘SupportBack’ is an internet intervention specifically developed by our team for patients with LBP consulting in primary care using a theory-based, evidence-based and person-based approach.17 Its central focus in enabling people to manage their LBP is to support appropriate engagement in physical activity. It is also designed to contain simple advice and behaviour change support/techniques for a range of clinical presentations (eg, acute or subacute) through effective reassurance for common concerns (such as the misconception, hurt equals harm), as well as providing elements that those with more chronic LBP may find helpful (eg, managing low mood, fear-avoidance, challenges with work and poor sleep). Brief additional human support often improves outcomes when added to internet interventions18 and SupportBack has been designed to be delivered either as a stand-alone intervention, or with additional brief telephone support from a physiotherapist.
In order to determine the effectiveness of digital approaches such as SupportBack, pragmatic trials are required that examine these interventions in addition to, and compared with, usual primary care for LBP. The aim of this study was to determine the feasibility of delivering the SupportBack intervention in addition to usual care to patients with LBP consulting in general practice, with or without brief physiotherapist telephone support, compared with usual care alone. We aimed to determine the feasibility of RCT procedures alongside the acceptability, uptake and use of the interventions, as well as preliminarily exploring key clinical and economic outcomes in order to inform a future full trial.
Method
Design
We conducted a three-parallel arm, single-centre feasibility RCT of the SupportBack internet intervention for LBP in primary care. The full details of the method and interventions can be found in the published trial protocol.17
Participants
Patients were included in the trial if they had current LBP (experienced pain within the last 2 weeks); had access to the internet; had consulted their general practice with LBP within the last 6 months; could read/understand English without assistance. Patients were excluded if they were under 18 years of age; had clinical indicators of (suspected) spinal pathology such as infection, fracture or cancer or had taken part in an earlier study to develop the intervention. Pregnancy was added to the exclusion criteria after the trial had begun.
Recruitment
The local Clinical Research Network (CRN) facilitated recruitment of general practices. Within practices, potentially eligible patients were identified by searching computerised lists of LBP consultations from the last 6 months. The resulting lists were screened by a GP who excluded patients who did not fulfil the eligibility criteria as determined from patients’ notes. Practice staff sent out study packs to the remaining patients containing options for interested patients to contact the research team. Study packs were also provided to practices for opportunistic recruitment within LBP consultations. Interested patients who contacted the research team underwent a secondary telephone screen by a study manager, who asked about their current LBP and screened a list of 12 key symptoms that may indicate serious spinal pathology or systemic illness.17 Patients answering yes to any symptoms were discussed with a clinician in the research team and referred back to their GP where appropriate. Those patients who remained eligible were sent a link to the study website, where they provided online consent, completed all baseline measures and were then randomised to one of the three trial arms. Recruitment opened in February 2015 and closed in September 2015. The follow-up period ended in January 2016.
Interventions
Usual care
Those patients allocated to this arm continued to receive usual care for their LBP over the trial period. This care was unrestricted and could vary substantially; for example, patients who did not reconsult at their general practice may not have received care beyond their initial consultation, whereas others may have accessed a range of treatment including physiotherapy or pain clinics.
Internet intervention plus usual care
Patients allocated to the internet intervention arm continued to receive unrestricted usual care for LBP. In addition, patients received access to SupportBack, a tailored multisession internet intervention designed to support self-management of LBP, developed by our team using LifeGuide software (http://www.lifeguideonline.org). SupportBack has been described in more detail elsewhere.17 In brief, the intervention focuses on self-regulatory processes including goal setting, self-monitoring and tailored feedback to support physical activity. There is also a focus on cognitive reassurance and self-efficacy for activity in the presence of pain throughout; addressing concerns with evidence-based feedback and modelling success through patient activity stories. SupportBack was developed using the person-based approach19 incorporating systematic, in-depth, qualitative research with 22 patients and community volunteers with experience of LBP.
The intervention has six sessions, and it was recommended that patients complete one session per week for 6 weeks. The first session introduces the rationale for physical activity being key in the self-management of LBP and allows patients to select goals for the next week. Goals options, including gentle back exercises or walking, are automatically tailored, based on how patients report their LBP is affecting their functioning at the time. Each of the following five sessions consists of patients reviewing and amending their activity goals for the coming week with automatic feedback. From session 2 onwards, after the goal review, patients have access to one new module per week from the SupportBack menu. The modules on the menu focus on a broad range of LBP-related topics including: mood; managing pain at work; sleep; relieving pain through medication and dealing with flare-ups. The broad aim of the intervention is to support patients to become their own expert in self-managing their LBP, thus strategies learnt (eg, remaining active during fair-ups) could also be used to manage LBP in the future and reduce the severity of recurrences. Patients used SupportBack without support from a health professional in this arm of the trial. They received automated weekly email reminders to log in, and any technical difficulties were addressed by the study manager. Patients were able to access the SupportBack internet intervention at any time over the trial period and from wherever was most convenient.
Internet intervention plus physiotherapist telephone support plus usual care
Patients in this arm continued to receive unrestricted usual care for LBP and had access to the SupportBack intervention as above. In addition, those in this arm received up to a total of 1 hour of physiotherapist telephone support, split into three calls, with approximately 30 min for call 1, and 15 min for calls 2 and 3. The calls were designed to be delivered approximately after week 1, between weeks 2–3 and after week 4. The purpose of the physiotherapists’ calls was to provide support and encouragement to participants to use the SupportBack internet intervention, to address participants’ concerns and provide additional reassurance. Two senior musculoskeletal physiotherapists (male and female, NHS bands 6 and 7) provided the telephone support. They worked through a standardised checklist for each phone call (available on request from the corresponding author), and although they were able to address individual patient concerns, they were asked not to provide additional recommendations beyond the content of the internet intervention. Their fidelity to the study protocol was evaluated by audio-recording a sample of 20 telephone consultations.
Outcomes and measures
The primary outcomes for this trial were descriptive, focusing on the feasibility of the trial design and intervention delivery, including: recruitment of general practices; recruitment of patients within the allocated timeframe of the trial; suitability of eligibility and screening criteria; withdrawals and retention at follow-up at 3 months; usage of the internet intervention and self-reported activity adherence; delivery and uptake of the telephone support along with any significant issues encountered.
The success criteria for the feasibility trial, as published in the protocol,17 are listed below:
Recruiting a minimum of 60 patients with LBP, access to the internet and without indicators of serious spinal pathology from primary care within the allotted recruitment time period for the trial.
Attrition at 3 months follow-up should be equal to or lower than 30% from all trial arms.
By examining the recordings, the telephone support physiotherapists are able to deliver the telephone sessions in line with the protocol, covering approximately two-third of the checklist in each call.
Patients should be able to access the intervention and complete measures, complete session 1 and set goals for future sessions.
Qualitative and quantitative data should indicate that the intervention and trial procedures are acceptable to patients (acceptability referring to completion of questionnaires, retention and appropriate use of the intervention). Qualitative data will be reported elsewhere.
All self-reported measures were collected online using LifeGuide software at baseline. At 3 months postrandomisation, measures were primarily collected online, non-response triggered additional follow-up methods including email reminders, paper questionnaires being posted and a telephone call from a blinded independent research assistant to collect key outcomes only. Demographic data collected included gender, age, education, occupation, income and marital status. A range of LBP-related measures were collected: LBP-related physical disability was measured using the Roland and Morris Disability Questionnaire (RMDQ),20 an outcome likely to be a primary outcome in a future full trial; pain duration was measured by asking about time since the last pain free month21; pain intensity was measured using three numerical rating scales (NRS) measuring current, average and least pain over the last 2 weeks as well as a mean of the three as a pain index22; number of troublesome days in pain over the last month was measured with a single item23; risk of persistent disability was measured using the STarT Back tool22; fear of movement was measured using the Tampa Scale for Kinesiophobia24; catastrophising beliefs were measured using the Pain Catastrophising Scale.25 Self-reported physical activity was measured using the International Physical Activity Questionnaire Short Form (IPAQ-SF),26 and questions about numbers of weeks, and times per week people did specific activities or went walking to help their back pain were asked at 3 months follow-up. Enablement was measured using a modified patient enablement instrument.27
Adherence to the internet intervention was examined by using LifeGuide-generated data on SupportBack sessions started and completed. Psychological process variables including patients’ expectations of positive outcome were measured using a modified brief Credibility and Expectancy Questionnaire (CEQ)28 at baseline across all arms, and the full CEQ was completed after session 1 in the two internet intervention arms. Exercise self-efficacy was also measured after session 1 in the two internet intervention arms.29 30 The Problematic Experiences of Therapy Scale (PETS)31 was used to measure difficulties with adherence to recommended exercises.
To determine the feasibility of collecting health economic measures for a cost-effectiveness analysis in a future full trial, a GP notes review was conducted and health-related quality of life was measured using the EQ-5D 3L.32 Resource use was costed using published sources of unit cost data.33 34 Identified resource use was costed using 2014/2015 UK pound sterling.
Sample size
The target for this trial was to recruit between 60 and 90 patients overall, with 20–30 per arm. Guidance for sample size in feasibility trials varies with numbers ranging from 12 to 30+ per arm.35 36 A sample of not less than 60 overall allowed for the assessment of the primary feasibility outcomes including recruitment, adherence and retention.
Randomisation and blinding
Randomisation was fully automated by the internet intervention software (LifeGuide). The randomisation sequence was generated within the software and concealed from the trial team. An automated algorithm block randomised patients to the three trial arms. Patients were stratified by severity of physical disability (measured by the RMDQ ≥7). Patients were notified of their allocated arm automatically by the LifeGuide software. Due to the behavioural nature of the intervention, it was not possible to blind patients to interventions. The study manager allocated patients to physiotherapists and therefore was not blind to allocation. All telephone outcome data were collected by an independent blinded research assistant. The trial statistician remained blind until the analysis was finalised. More detail on randomisation can be found in the protocol.17
Analysis
The primary analysis for this trial focused on a description of the key feasibility outcomes including numbers of general practices recruited; patient eligibility and recruitment rates; withdrawals; response to follow-up at 3 months. Use of the internet intervention was described by reporting numbers of sessions started and completed per arm. Delivery of physiotherapist telephone support was described in terms of the number of calls successfully made and mean/modal calls per patient. Fidelity of the telephone support was examined by selecting a random sample of 30% of the verbatim transcripts of the calls and physiotherapist completed call check sheets. As detailed in the protocol,17 the check sheets contained recommended topics to be covered in each call, acknowledging that not all topics may be appropriate. AWAG examined the transcript-check sheet pairs examining correspondence of topics covered in each case. Any major deviation was noted.
Descriptive statistics were used to identify any floor or ceiling effects. Means and/or medians, SD and 95% CIs were reported for the measures. Exploratory quantitative analyses were conducted on patients’ clinical, activity and psychological process measures. In addition to analyses reported in the protocol, linear regression models, controlling for baseline covariates (each outcome at baseline, gender, age, marital status, employment status, income, ethnicity and age left education), were used to explore between group differences in continuous outcome measures (eg, RMDQ, numerical pain rating scale). Continuous outcomes were modelled using a linear model if they met the underlying assumptions that the outcome measure and the residuals were normally distributed. Where these assumptions were not met, a non-parametric quantile regression was used.37 As this was a feasibility trial the objective was not hypothesis testing, rather these analyses allowed for preliminary examination of trends in between-group comparisons. The analysis was undertaken on an intention-to-treat basis, analysing participants in the group to which they had been randomised and comprised complete cases only. Proportions of patients achieving a minimal clinically important difference (MCID) was described. In this trial, a MCID was classified as a reduction of 2 points on the RMDQ compared with usual care alone.38 Spearman’s correlations with 95% CIs were used to explore the relationship between psychological process measures such as expectancy and exercise self-efficacy on LBP-related disability and adherence to physical activity.
Health economic analysis at this stage was descriptive. We aimed to report estimates of cost and outcomes measures and baseline and follow-up. The methods of collecting health economics data were similar to the methods that would be used in a future full RCT. NHS-related costs were estimated from computer records in participating general practice. Estimates were made of the cost of making access to SupportBack and the costs of providing nurse support as per protocol. These costs were recorded over the 3-month follow-up period. Resources identified were combined with relevant unit costs.33 34 Outcomes for use within the economics evaluation were change in LBP-related disability (RMDQ) and the quality-adjusted life-year (QALY) evaluated using the EQ-5D 3L.39
Results
Recruitment and retention
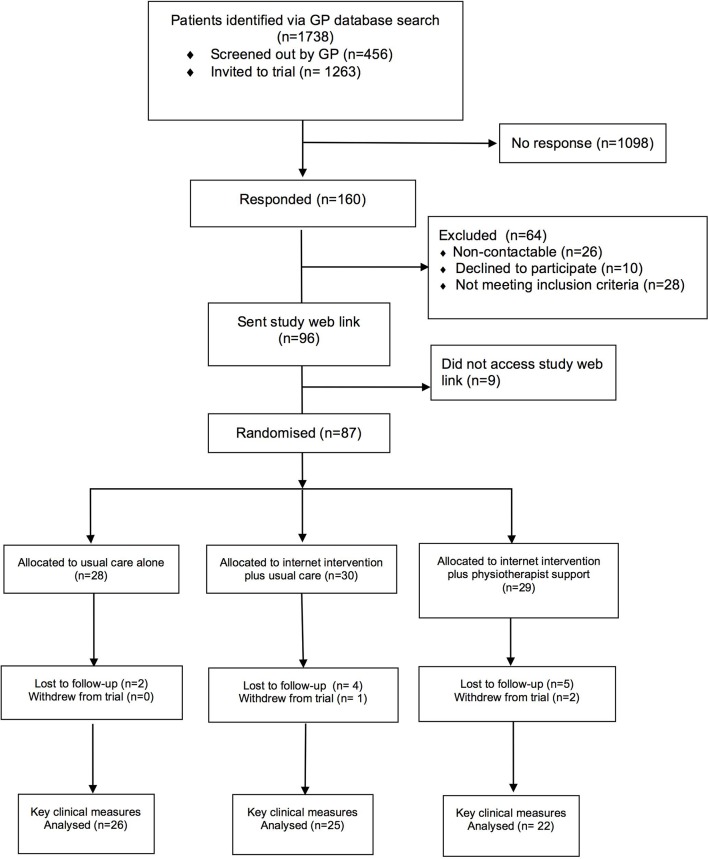
The CRN received expressions of interest to take part in the trial from 27 practices, of which 4 were initially approached and recruited, this was increased to 12 following close monitoring of initial recruitment rates. One thousand two hundred sixty-three trial invitation letters were sent from the 12 participating practices to potentially eligible patients. One hundred sixty responses were received. Of these, 87 patients with LBP met the eligibility criteria after further telephone screening and were randomised over a 6-month period. This translated to a recruitment rate of 14–15 patients per month, and approximately 7 patients randomised per practice over a total of 6 months. Three patients withdrew over the course of the trial: one from the internet intervention plus usual care arm (no reason given), two from the internet intervention plus physiotherapist support arm (due to illness and due to family bereavement). The overall follow-up rate for the key clinical outcomes was 84% (73/87) at 3 months, and varied between arms: usual care=93%, internet intervention plus usual care=83%, internet intervention plus physiotherapist support=76%. See figure 1 for patient flow through the trial.
Figure 1.
SupportBack patient flow diagram. GP, general practitioner.
Patient characteristics
Eighty-four participants provided baseline data. Table 1 shows participant characteristics across the three trial arms. Demographic characteristics were generally similar across the arms, with some exceptions including greater numbers of retired participants in the usual care alone arm. With regard to clinical variables at baseline, LBP-related disability (measured by the RMDQ) was similar across arms. Taken together, the RMDQ, pain numerical rating scales and STarT back scores indicate slightly higher severity in those randomised to the internet intervention plus physiotherapist support arm. Pain duration, measured as time since last pain free month, was similar across arms. Number of troublesome days in pain over the last 4 weeks differed substantially; from a median of 10 in the usual care alone arm to 18 in the internet intervention plus physiotherapist support arm.
Table 1.
Baseline characteristics
| Variable | Usual care (n=27) | Internet intervention plus usual care (n=29) | Internet intervention plus physiotherapist support (n=27) |
| Female | 15 (55.6%) | 19 (65.2%) | 17 (63.0%) |
| Age | 60.3 (16.3) | 54.5 (13.7) | 59.3 (10.4) |
| Marital status | |||
| Married/partner | 23 (85.2%) | 19 (65.5%) | 22 (81.5%) |
| Single | 3 (11.1%) | 4 (13.8%) | 2 (7.4%) |
| Divorced/separated | 0 | 5 (17.2%) | 1 (3.7%) |
| Widow/widower | 1 (3.6%) | 1 (3.6%) | 2 (7.4%) |
| White ethnicity | 27 (100%) | 26 (92.9%) | 27 (100%) |
| Age left education | 17.6 (2.7) | 17.3 (1.7) | 17.6 (2.8) |
| Employment status | |||
| Full time | 7 (25.9%) | 12 (41.8%) | 6 (22.2%) |
| Part time | 2 (7.4%) | 4 (13.8%) | 8 (29.6%) |
| Retired | 13 (48.2%) | 6 (20.7%) | 8 (29.6%) |
| Self-employed | 2 (7.4%) | 3 (10.3%) | 4 (14.8%) |
| Sickness/disability | 2 (7.4%) | 2 (6.9%) | 1 (3.7%) |
| Other | 1 (3.7%) | 2 (6.9%) | 0 |
| Annual income (up to £) | |||
| 10 000 | 2 (7.4%) | 4 (14.3%) | 3 (11.5%) |
| 20 000 | 7 (25.9%) | 6 (21.4%) | 3 (11.5%) |
| 40 000 | 9 (33.3%) | 9 (32.1%) | 10 (38.5%) |
| >40 000 | 9 (33.3%) | 9 (32.1%) | 10 (38.5%) |
| Expected reimprovement in LBP | 5.86 (1.88) | 5.22 (2.06) | 5.74 (2.19) |
| Expected percentage improvement in LBP (item from the CEQ) | 43.21% (25.53) | 41.92% (21.17) | 37.40% (25.50) |
| Median days of pain in the last 4 weeks
(IQR) (item from the CEQ) |
10 (6, 25) | 10 (4, 21) | 18 (5, 28) |
| Time since you had a whole month without pain | |||
| <3 months | 5 (17.2%) | 6 (21.4%) | 5 (19.2%) |
| 3–6 months | 1 (3.5%) | 2 (7.1%) | 4 (15.4%) |
| 7–12 months | 5 (17.2%) | 4 (14.3%) | 6 (23.1%) |
| 1–2 years | 7 (24.1%) | 4 (14.3%) | 5 (19.2%) |
| 3–5 years | 4 (13.8%) | 4 (14.3%) | 3 (11.5%) |
| 6–10 years | 2 (6.9%) | 4 (14.3%) | 3 (11.5%) |
| >10 years | 5 (17.2%) | 4 (14.3%) | 0 |
| LBP-related disability (RMDQ) mean (SD) | 6.8 (4.9) | 6.6 (4.6) | 7.7 (4.7) |
| STarT Back risk group | |||
| Low | 16 (57.1%) | 19 (67.9%) | 14 (51.9%) |
| Medium | 11 (39.3%) | 6 (21.4%) | 12 (44.4%) |
| High | 1 (3.8%) | 3 (10.7%) | 1 (3.7%) |
CEQ, Credibility and Expectancy Questionnaire; LBP, low back pain; RMDQ, Roland and Morris Disability Questionnaire.
Adherence outcomes
Table 2 shows the percentages of participants starting and completing sessions of the SupportBack internet intervention. Both the percentages starting and completing sessions tended to be higher in the internet intervention plus telephone support arm. For all sessions, those starting a session tended to complete it, with the exception of the internet intervention plus usual care arm in session 1. Overall, 11.1% (3/27) of those in the internet intervention plus telephone support arm and 29.6% (8/27) of patients in the internet intervention plus usual care arm partially completed session 1 and did not return to the internet intervention over the duration of the trial.
Table 2.
Percentages starting (Start) and completing (Com.) internet intervention sessions (S)
| Start S1 | Com. S1 | Start S2 | Com. S2 |
Start S3 | Com. S3 |
Start S4 | Com. S4 |
Start S5 | Com. S5 |
Start S6 | Com. S6 |
|
| Internet intervention* | 89% | 54% | 61% | 57% | 54% | 50% | 46% | 43% | 36% | 36% | 32% | 32% |
| Internet intervention+ support† | 82% | 70% | 85% | 70% | 82% | 78% | 59% | 56% | 48% | 48% | 41% | 41% |
*Internet intervention plus usual care.
†Internet intervention plus physiotherapist support.
At follow-up, participants were also asked about activities they engaged with to help their LBP (walking or back exercises). All participants were asked to provide these data, serving as an indication of self-reported activity adherence in the internet intervention arms, and providing data about levels of activity in the usual care alone arm. The responses are tabulated in table 3. Most participants regardless of arm allocation reported spending 9–12 weeks going for walks or doing back exercises and did so regularly (4+ days per week).
Table 3.
Tabulation of self-reported LBP-related activities
| Usual care alone (n=14) | Internet intervention plus usual care (n=16) | Internet intervention plus telephone support (n=19) | |
| How many weeks spent doing back exercises or going for walks? | |||
| Never started | 2 (14.3%) | 0 | 0 |
| 1 week | 0 | 0 | 0 |
| 1–2 weeks | 0 | 1 (6.3%) | 1 (5.3%) |
| 3–5 weeks | 3 (21.4%) | 6 (37.5%) | 4 (21.1%) |
| 6–8 weeks | 1 (7.1%) | 2 (12.5%) | 5 (26.3%) |
| 9–12 weeks | 8 (57.1%) | 7 (43.7%) | 9 (47.4%) |
| How many times a week did you do back exercises or go for walks? | |||
| Never started | 2 (14.3%) | 0 | 0 |
| 1 day | 1 (7.1%) | 2 (12.5%) | 1 (5.3%) |
| 2–3 days | 2 (14.3%) | 5 (31.3%) | 2 (10.5%) |
| 4–5 days | 5 (35.7%) | 4 (25.0%) | 7 (36.8%) |
| Every day | 4 (28.6%) | 5 (31.3%) | 9 (47.4%) |
Numbers are lower as these variables were not part of minimum data collection over the telephone at 3 months follow-up with telephone follow-up.
Physiotherapist telephone support
Support telephone calls were made to 25/29 (86%) participants who were randomised to this arm. For those that did not receive calls, three participants were uncontactable despite multiple call attempts made by the physiotherapists (two of three continued to use the internet intervention alone), and one participant was not allocated a physiotherapist due to an administrative error. This was discovered at the end of the trial through the qualitative interview with this participant. This individual continued to use the internet intervention alone.
For the 25 patients receiving physiotherapist support calls, the mean number of calls made was 2.4 (SD=1.03, mode=3). Mean call durations were 17.3 min (SD=8.5) for call 1, and 11.5 (SD=6.2) and 11.9 (SD=6.2) minutes for calls 2 and 3, respectively. From the 65 connected calls made, a random sample of 20 calls (30%) were selected to examine fidelity using verbatim transcripts of the calls and physiotherapist completed call check sheets. At least two-thirds of the recommended topics were covered in 19 of the calls checked (95%).
Clinical outcomes/measures
Mean physical disability measured by RMDQ score, was 6.9 (SD=5.5) across the trial arms at baseline. From the 84 participants who provided RMDQ data at baseline, 73 (84%) provided a response at 3 months follow-up. Of these, 27 (34.2%) were contacted by telephone or completed a paper questionnaire follow-up pack. Exploratory analysis of RMDQ scores showed, on average, participants in all three arms improved between baseline and follow-up (see table 4). The internet intervention plus usual care arm improved by 0.6 points more than usual care alone, while the internet intervention plus physiotherapist support arm improved by 2.4 points, after controlling for baseline score and covariates. When those with a lower RMDQ at baseline (<4) were excluded, the results remained similar with participants allocated to the internet intervention plus usual care improving by 0.4, and those allocated to internet intervention plus physiotherapist support improving by 2.0 more than usual care alone on the RMDQ. The proportions achieving the MCID were higher in the internet intervention plus physiotherapist support arm (13/22, 59.1%), than the internet intervention plus usual care (8/26, 31.0%) and usual care alone (10/25, 40.0%) arms.
Table 4.
Clinical and physical activity measures at baseline and follow-up, including linear regression analysis (mean difference), and quantile regression analysis (median difference)
| Baseline mean (SD) | 3 months follow-up mean (SD) | Mean difference (95% CI) at follow-up controlling for baseline | Mean difference (95% CI) at follow-up controlling for baseline and other covariates* | |
| LBP-related disability (RMDQ) (n=73) | ||||
| Usual care alone | 6.8 (4.9) | 6.3 (5.1) | ||
| Internet intervention plus usual care | 6.6 (4.6) | 5.8 (4.5) | −0.7 (−2.77 to 1.35) | −0.6 (−3.10 to 1.83) |
| Internet intervention plus physiotherapist support | 7.7 (4.7) | 5.1 (5.1) | −1.3 (−3.49 to 0.81) | −2.4 (−5.00 to 0.25) |
| LBP-related disability (RMDQ)—excluding those with a score below 4 (n=51) | ||||
| Usual care alone | 8.5 (4.3) | 7.3 (5.4) | ||
| Internet intervention plus usual care | 9.0 (3.9) | 7.4 (4.9) | −0.03 (−2.73 to 2.82) | −0.4 (−3.08 to 3.11) |
| Internet intervention plus physiotherapist support | 9.5 (3.6) | 6.4 (5.4) | −0.8 (−3.64 to 1.99) | −2.0 (−4.98 to 0.94) |
| Pain intensity (NRS)—index average (n=72) | ||||
| Usual care alone | 3.8 (2.3) | 3.6 (2.1) | ||
| Internet intervention plus usual care | 3.9 (2.0) | 3.2 (2.2) | −0.8 (−1.60 to 0.07) | −0.5 (−1.47 to 0.49) |
| Internet intervention plus physiotherapist support | 4.2 (2.2) | 3.1 (2.0) | −0.7 (−1.53 to 0.21) | −0.8 (−1.78 to 0.25) |
| Pain intensity (NRS) 1—current (n=72) | ||||
| Usual care alone | 3.6 (3.1) | 4.0 (2.5) | ||
| Internet intervention plus usual care | 4.0 (2.6) | 3.6 (2.5) | −0.9 (−1.86 to 0.16) | −0.6 (−1.82 to 0.56) |
| Internet intervention plus physiotherapist support | 4.5 (2.6) | 3.1 (2.3) | −1.4 (−2.40 to –0.29) | −1.0 (−2.25 to 0.21) |
| Pain intensity (NRS)—least pain last 2 weeks (n=72) | ||||
| Usual care alone | 3.2 (2.5) | 2.8 (2.1) | ||
| Internet intervention plus usual care | 3.1 (2.1) | 2.3 (2.3) | −0.7 (−1.60 to 0.16) | −0.6 (−1.46 to 0.29) |
| Internet intervention plus physiotherapist support | 2.9 (2.7) | 2.3 (2.1) | −0.04 (−0.97, 0.89) | 0.2 (−0.71 to 1.08) |
| Pain intensity (NRS)—average last 2 weeks (n=72) | ||||
| Usual care alone | 4.6 (2.0) | 4.1 (2.1) | ||
| Internet intervention plus usual care | 4.5 (2.1) | 3.6 (2.5) | −0.5 (−1.56 to 0.54) | −0.4 (−1.54 to 0.76) |
| Internet intervention plus physiotherapist support | 5.2 (2.1) | 3.4 (1.7) | −0.9 (−1.96 to 0.25) | −0.8 (−2.07 to 0.44) |
| Fear avoidance (TSK) (n=59) | ||||
| Usual care alone | 37.8 (6.2) | 35.0 (6.4) | ||
| Internet intervention plus usual care | 37.5 (7.4) | 36.1 (8.1) | 0.7 (−2.52 to 3.84) | 0.1 (−3.02 to 3.29) |
| Internet intervention plus physiotherapist support | 35.5 (6.8) | 34.3 (7.5) | 0.8 (−2.30 to 4.02) | −0.6 (−3.65 to 2.53) |
| Negative orientation towards pain (PCS) (n=57) | ||||
| Usual care alone | 13.7 (12.8) | 14.0 (11.4) | ||
| Internet intervention plus usual care | 13.5 (10.0) | 12.8 (9.0) | −1.5 (−6.37 to 3.40) | −3.5 (−9.70 to 2.74) |
| Internet intervention plus physiotherapist support | 13.6 (9.4) | 18.63 (8.5) | 4.2 (−0.58 to 8.90) | 3.7 (−1.78 to 9.27) |
| Modified Enablement Scale (n=58) | ||||
| Usual care alone | 26.5 (8.4) | 27.9 (10.5) | ||
| Internet intervention plus usual care | 25.1 (8.5) | 25.4 (9.7) | −2.0 (−8.51 to 4.55) | −1.3 (−8.69 to 6.01) |
| Internet intervention plus physiotherapist support | 26.1 (7.8) | 28.3 (9.3) | 0.1 (−6.19 to 6.43) | −0.3 (−6.63 to 6.08) |
| Days in pain | Median (Q1, Q3) | Median (Q1, Q3) | Median difference (95% CI) at follow-up controlling for baseline | Median difference (95% CI) at follow-up controlling for baseline and other covariates* |
| Usual care alone | 10 (6, 25) | 6 (2, 20) | ||
| Internet intervention plus usual care | 10 (4,21) | 4 (0, 15) | −0.7 (−9.20 to 7.87) | −1.6 (−10.36 to 7.16) |
| Internet intervention plus physiotherapist support | 18 (5, 28) | 10 (3, 20) | 0.3 (−8.71 to 9.38) | 1.1 (−8.62 to 10.90) |
| Physical activity (IPAQ) | Median (Q1, Q3) | Median (Q1, Q3) | ||
| Usual care alone | 3139.5 (466.1, 5385) | 2277.5 (912, 6105) | ||
| Internet intervention plus usual care | 1178.5 (480, 4131) | 1130.5 (693, 2826) | −64.9 (−2796.15 to 2666.32) | 331.8 (−2360.85 to 3024.50) |
| Internet intervention plus physiotherapist support | 3168 (396, 7413) | 990 (396, 3226.5) | −668.0 (−3347.32 to 2011.25) | −408.0 (−2757.56 to 1941.50) |
*Covariates controlled for were age, gender, marital status, employment status, income, ethnic group and age left education.
IPAQ, International Physical Activity Questionnaire; NRS, Numerical Rating Scale; PCS, Pain Catastrophising Scale; RMDQ, Roland Morris Disability Scale; TSK, Tampa Scale for Kinesiophobia.
Additional pain-related measures are also shown in table 4. There were small reductions in pain intensity (NRS) in all arms from baseline to 3 months, although greater change occurred in the internet intervention plus physiotherapist support arm in comparison with internet intervention plus usual care arm and usual care alone. There were small reductions in fear avoidance beliefs across all arms. With regard to pain catastrophising, there were small increases in the usual care alone arm and unexpectedly, in the internet intervention plus physiotherapist support arm (13.6–18.6). At 3 months, those in the internet intervention plus physiotherapist support arm reported eight less days in pain, internet intervention plus usual care arm reported six less days in pain and those in usual care alone reported two less days in pain over the last 4 weeks. Finally, patient enablement showed small increases across all three arms.
The STarT Back tool22 was used at baseline and 3 months follow-up to describe the proportions of participants at low, medium or high risk of persistent disability (see table 5). There was an increase in the proportion of patients classed as low risk in both the internet intervention plus usual care (60%–70%) and the internet intervention plus physiotherapist support arms (33%–74%). The proportion of patients classified at high risk reduced to zero in the internet intervention plus physiotherapist support arm. There was little change in the risk proportions in the usual care alone arm from baseline to 3 months follow-up.
Table 5.
Number of patients (%) in STarT Back subgroups at baseline and follow-up for all trial arms
| Arm | Baseline | Follow-up | ||||
| Low risk | Medium risk | High risk | Low risk | Medium risk | High risk | |
| Usual care alone | 15 (51.7%) | 11 (37.9%) | 3 (10.3%) | 11 (47.8%) | 10 (43.5%) | 2 (8.7%) |
| Internet intervention plus usual care | 17 (60.7%) | 8 (28.6%) | 3 (10.7%) | 12 (70.6%) | 3 (17.7%) | 2 (11.8%) |
| Internet intervention plus physiotherapist support | 9 (33.3%) | 15 (55.6%) | 3 (11.1%) | 14 (73.7%) | 5 (11.8%) | 0 |
Physical activity
The IPAQ-SF data were converted to MET/min/week and compared using medians with quantile regression, as the distribution of energy expenditure is known to be non-normal in many populations. The median at baseline for the sample was 2343 (IQR=480, 5544). It is important to note that the American Heart Association recommends 450–750 MET/per week or approximately, moderate exercise for 30 min/day, 5 days a week.40 A baseline median of 2343 is unexpected, and brings into question the reliability of this self-report measure of physical activity.
Process variables for the full trial
Thirty seven patients in the internet intervention arms completed the CEQ and the Exercise Self-efficacy Questionnaire (ESE) (66%). The association between the CEQ score and the RMDQ score at follow-up (r=−0.19, 95% CI −0.50 to 0.15) was in the expected direction, as was the association between ESE and number of weeks spent engaging in back-related exercise reported at 3 months (r=0.28, 95% CI −0.08 to 0.58). PETS was completed by 67%18 of patients in the internet intervention plus usual care and 70%19 of the internet intervention plus physiotherapist support arm. PETS is used to explore the relationship between its scores and quantitative adherence (both to the internet intervention and recommended exercises) data in large samples. As the numbers are small our main focus is on completion rates, which suggest PETS is suitable for inclusion in a full trial.
Health economic outcomes
The hosting cost of providing access to SupportBack was assumed to be £12.50 per person, this based on predicted costs of server provision and website maintenance. Physiotherapist support was estimated at £38 per person. This gives a total intervention cost of £12.50 and £50.50 in the internet intervention plus usual care and internet intervention plus physiotherapist support arm, respectively. The total mean cost for all 79 participants was £270, of which £107 (43%) was related to back pain; indicating that use of NHS services were an important cost for this group of patients (see table 6). Our sample showed 66% of total NHS costs and 78% of back pain-related costs occurred in secondary care. Due to delays related to referring and attending secondary care appointments, it is likely that costs would occur after the 3-month period used in this study.
Table 6.
NHS costs (£, mean (SD)) derived from computer records at participating general practices at 3 months follow-up
| Usual care alone (n=26) | Internet intervention plus usual care (n=28) | Internet intervention plus physiotherapist support (n=25) | All (excluding intervention costs) (n=79) | |
| Intervention costs | 0 | 12.5 | 50.5 | |
| All NHS costs | ||||
| Primary care costs* | 96 (142) | 85 (114) | 108 (136) | 96 (130) |
| Secondary care—A&E | – | 14 (42) | 11 (53) | 8 (39) |
| Secondary care—O/P | 116 (279) | 48 (83) | 87 (106) | 83 (178) |
| Secondary care—inpatient | 59 (299) | 129 (564) | 101 (391) | 97 (432) |
| Secondary care—total | 175 (490) | 191 (586) | 198 (483) | 188 (517) |
| Total costs | 271 (492) | 289 (650) | 357 (553) | 284 (564) |
| Back pain costs only | ||||
| Primary care costs—back pain only | 15 (40) | 30 (73) | 35 (75) | 26 (64) |
| Secondary care—A&E | – | – | 11 (53) | 3 (30) |
| Secondary care—O/P | 76 (251) | 25 (62) | 32 (69) | 44 (153) |
| Secondary care—inpatient | 26 (132) | 24 (129) | 101 (391) | 49 (244) |
| Secondary care—total | 102 (325) | 50 (158) | 143 (482) | 96 (340) |
| Total costs—back pain only | 116 (327) | 92 (178) | 228 (535) | 123 (367) |
*Primary care costs refer to GP consultations (at the surgery/home/phone); practice nurse consultations (at the surgery/home/phone); use of other person in surgery (mainly phlebotomist); any other primary care-related costs (walk in centre or phlebotomist) and costs of back pain relevant prescribing.
Two outcomes measures would be used in the economic evaluations alongside any future full trial; change in LBP-related disability (RMDQ) and QALY evaluated using the EQ-5D 3L.39 However, because of the variability in costs any estimates of cost-per point change in these measures would be subject to considerable uncertainty and so are not reported here. The EQ-5D was found to be strongly negatively correlated with RMDQ at both baseline and follow-up, with respective Pearson’s correlations of −0.594 and −0.560 (P<0.01). This provides some support for the use of the EQ-5D in a future full trial of SupportBack for LBP. For QALYs, there were only 57 cases with baseline and follow-up data for the EQ-5D and 54 that also had cost data. This was lower than response rate for RMDQ and other clinical measures. The EQ-5D was one of the last questionnaires participants completed, additionally, it was not part of the minimum dataset collected by telephone at 3 months.
Harms
Six hospital admissions were reported: two (internet intervention plus physiotherapist support arm), two (internet intervention plus usual care), two (usual care alone). One case of suspected cauda equine syndrome was detected towards the end of the trial in the physiotherapist support arm (immediate clinical treatment was received, L5/S1 discectomy performed) and five admissions were identified from patient general practice medical record reviews: one for a facet joint injection, one for a haemoarthrosis, one for lumbar screening and injection, one for an epidural steroid injection and one unrelated serious adverse event. We think it is very unlikely that the gentle activity advice offered by the internet intervention would lead to any of the above, but it is not possible to rule out; all serious adverse reactions were reported to the trials’ Research Ethics Committee.
Discussion
We believe this is the first trial of an internet intervention specifically designed for patients with LBP consulting in general practice. Overall, the trial design was found to be feasible and the success criteria were met17; the target number of patients were recruited within the trial timeframe; the majority of patients were exposed to core active internet intervention content; the telephone support physiotherapists adhered to the protocol and acceptable levels of retention were achieved for the key clinical outcomes at 3 months follow-up. Caution is required when interpreting the exploratory analysis of clinical outcomes as, due to the feasibility aims of this trial, it was not powered to determine effectiveness. The reduction of 2.4 points on the RMDQ for the internet intervention plus physiotherapist support arm compared with usual care alone at 3 months follow-up, provides an indication of the potential importance of remote, brief healthcare professional support for primary care patients with LBP. Reductions in LBP-related disability compared with usual care alone were smaller when the internet intervention was delivered without support.
The trial design had a number of strengths. The internet intervention was provided in addition to and compared with unrestricted usual care. This pragmatic design will enable evaluation of the incremental value of the interventions in addition to the existing full range of LBP healthcare available. Use of outcomes recommended as core outcome domains for LBP41 will enable comparison with other non-digital interventions; previous studies of internet interventions for LBP have used a heterogeneous range of outcome measures.13 To our knowledge, this is the first trial to integrate brief physiotherapist telephone support with an internet intervention specifically designed for LBP patients. Physiotherapists are ideally placed to support LBP interventions with a central focus on physical activity, and this trial demonstrates the feasibility of a guided digital approach for the management of a prevalent musculoskeletal condition in primary care.
We identified some limitations to be addressed in the full trial: encouraging physical activity was a core focus of SupportBack. The high median MET minutes of physical activity reported by patients at baseline on the IPAQ-SF appears to reflect a substantial overestimation, severely limiting the scales potential for detecting change in physical activity over the course of the trial. Despite the IPAQ-SF remaining the most widely used self-report measure of physical activity,42 overestimation is frequently reported.43 Objective measures such as accelerometers can be intrusive, costly when needed in large numbers and there are still questions over accuracy.44 Consequently, for the full trial it may be best to provide additional support for accurate reporting on the IPAQ-SF at baseline (eg, through providing worked examples). Our sample had a lower mean RMDQ score than other trials for LBP in primary care,45 with approximately 30% reporting an RMDQ score of ≥4 at baseline. This may be a function of the 6-month recruitment window from patients’ LBP consultation, our broad inclusion criteria (experience of LBP in the last 2 weeks) and the low intensity nature of the interventions on offer. For the full trial, we will amend our recruitment strategy to recruit patients closer to their consultation at participating practices. We will also amend our recruitment procedure aiming at improving efficiency, working to ensure more of those invited are screened and more of those screened are eligible. Follow-up rates differed between the three arms, with the lowest rates in the internet intervention plus telephone support arm. In the main trial, follow-up rates will be closely monitored to ensure they remain above 80% across all three arms. Finally, the randomisation was unbalanced on some demographic and clinical variables. This was likely a function of the small numbers in each arm, and would be expected to balance out with the numbers required (approximately 200+ per arm) for a full trial. Nevertheless, differences at baseline should be considered when interpreting the exploratory findings with variables including troublesome days in pain and risk of persistent disability.
Health economic evaluations of digital health interventions can be complex. A recent paper has discussed these complexities inherent in costing digital health interventions, such as SupportBack, highlighting the importance of considering ongoing costs and benefits of digital interventions.46 For costing future implementation, it would be important to identify any hosting costs as well as documenting any additional development costs needed and whether any of these would be ongoing (to keep the intervention up to date). We would also propose sensitivity analysis to allow for different assumptions as to the number of people who will use the intervention as this affects the estimate of unit cost. As this was a small-scale feasibility trial, there was considerable uncertainty caused by a small number of high cost items such as inpatient stays. As well as substantially increasing participants, in the full trial the EQ-5D will be collected after the RMDQ and included in the minimum dataset phone calls, and follow-up will occur at regular intervals over a 12-month period. Finally, potential future benefit should be considered and assessed where possible beyond the perspective of the trial timeframe; since LBP tends to be recurrent coping strategies learnt from SupportBack might help prevent or manage back pain recurrence.
To conclude, digital approaches with and without healthcare professional support have the potential to offer an accessible means of effectively supporting behavioural self-management. We have shown that the SupportBack intervention is acceptable to patients with LBP presenting to primary care, and demonstrated the feasibility of a future definitive RCT aimed at determining its clinical and cost-effectiveness.
Supplementary Material
Acknowledgments
The authors would like to thank the Southampton branch of the BackCare charity for their input into the initial idea for this trial and their ongoing feedback.
Footnotes
Contributors: LY, AWAG and PL conceived the idea for the study. AWAG, LY, PL, LCR, NEF, EMH and JCH designed the trial and secured funding. RS and AWAG developed the internet intervention with LY and LR, with further input from NEF, JCH, EMH, PL and LL. LY, AG, LCR, JCH, NEF, developed the physiotherapy telephone support package. RS managed the trial on a day-to-day basis with oversight from AG, PL, LCR, LY and input from NEF, JCH, EMH and LL. BS, DT, WM planned and carried out the statistical and health economic analysis. AWAG drafted the manuscript with input from all authors, AWAG is the guarantor for the data.
Funding: This article presents independent research funded by the National Institute for Health Research (NIHR) Research for Patient Benefit programme (RfPB PB-PG- 1111-26080). NEF and JCH are funded by an NIHR Research Professorship awarded to NEF (NIHR-RP-011-015) and LR is funded by an HEFCE/NIHR Senior Clinical Lectureship (round 3). NEF, EMH and PL are NIHR Senior Investigators.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: NHS Ethics Committee REC Reference 13/SC/020.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The datasets generated during the current study are available from the corresponding author on reasonable request.
References
- 1.Hoy D, March L, Brooks P, et al. . The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968–74. 10.1136/annrheumdis-2013-204428 [DOI] [PubMed] [Google Scholar]
- 2.Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354:581–5. 10.1016/S0140-6736(99)01312-4 [DOI] [PubMed] [Google Scholar]
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95–103. 10.1016/S0304-3959(99)00187-6 [DOI] [PubMed] [Google Scholar]
- 4.Freburger JK, Holmes GM, Agans RP, et al. . The rising prevalence of chronic low back pain. Arch Intern Med 2009;169:251–8. 10.1001/archinternmed.2008.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gore M, Sadosky A, Stacey BR, et al. . The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 2012;37:E668–77. 10.1097/BRS.0b013e318241e5de [DOI] [PubMed] [Google Scholar]
- 6.Excellence NIFHAC. Low back pain: Early management of persistent non-specific low back pain. Clinical Guideline 134. London: Nice 2009. [Google Scholar]
- 7.Machado GC, Maher CG, Ferreira PH, et al. . Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ 2015;350:h1225 10.1136/bmj.h1225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mallen C, Hay E. Managing back pain and osteoarthritis without paracetamol. BMJ 2015;350:h1352 10.1136/bmj.h1352 [DOI] [PubMed] [Google Scholar]
- 9.Crofford LJ. Adverse effects of chronic opioid therapy for chronic musculoskeletal pain. Nat Rev Rheumatol 2010;6:191–7. 10.1038/nrrheum.2010.24 [DOI] [PubMed] [Google Scholar]
- 10.Salisbury C, Foster NE, Hopper C, et al. . A pragmatic randomised controlled trial of the effectiveness and cost-effectiveness of ’PhysioDirect' telephone assessment and advice services for physiotherapy. Health Technol Assess 2013;17:1–157. 10.3310/hta17020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yardley L, Choudhury T, Patrick K, et al. . Current issues and future directions for research into digital behavior change Interventions. Am J Prev Med 2016;51:814 10.1016/j.amepre.2016.07.019 [DOI] [PubMed] [Google Scholar]
- 12.Butler L, Foster NE. Back pain online: a cross-sectional survey of the quality of web-based information on low back pain. Spine 2003;28:395–401. 10.1097/01.BRS.0000048497.38319.D3 [DOI] [PubMed] [Google Scholar]
- 13.Garg S, Garg D, Turin TC, et al. . Web-based interventions for chronic back pain: a systematic review. J Med Internet Res 2016;18:e139 10.2196/jmir.4932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buhrman M, Fältenhag S, Ström L, et al. . Controlled trial of Internet-based treatment with telephone support for chronic back pain. Pain 2004;111:368–77. 10.1016/j.pain.2004.07.021 [DOI] [PubMed] [Google Scholar]
- 15.Buhrman M, Nilsson-Ihrfeldt E, Jannert M, et al. . Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J Rehabil Med 2011;43:500–5. 10.2340/16501977-0805 [DOI] [PubMed] [Google Scholar]
- 16.Carpenter KM, Stoner SA, Mundt JM, et al. . An online self-help CBT intervention for chronic lower back pain. Clin J Pain 2012;28:14–22. 10.1097/AJP.0b013e31822363db [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geraghty AW, Stanford R, Little P, et al. . Using an internet intervention to support self-management of low back pain in primary care: protocol for a randomised controlled feasibility trial (SupportBack). BMJ Open 2015;5:e009524 10.1136/bmjopen-2015-009524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther 2009;38:196–205. 10.1080/16506070903318960 [DOI] [PubMed] [Google Scholar]
- 19.Yardley L, Morrison L, Bradbury K, et al. . The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res 2015;17:e30 10.2196/jmir.4055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roland M, Fairbank J. The Roland-Morris disability questionnaire and the oswestry disability Questionnaire. Spine 2000;25:3115–24. 10.1097/00007632-200012150-00006 [DOI] [PubMed] [Google Scholar]
- 21.Dunn KM, Croft PR. The importance of symptom duration in determining prognosis. Pain 2006;121:126–32. 10.1016/j.pain.2005.12.012 [DOI] [PubMed] [Google Scholar]
- 22.Hill JC, Dunn KM, Lewis M, et al. . A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum 2008;59:632–41. 10.1002/art.23563 [DOI] [PubMed] [Google Scholar]
- 23.Little P, Lewith G, Webley F, et al. . Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain. BMJ 2008;337:a884 10.1136/bmj.a884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goubert L, Crombez G, Van Damme S, et al. . Confirmatory factor analysis of the Tampa Scale for Kinesiophobia: invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain 2004;20:103–10. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan M, Bishop SR, Pivik J. The pain catastrophizing scale: user manual. 2009.
- 26.Craig CL, Marshall AL, Sjöström M, et al. . International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 27.Howie JG, Heaney DJ, Maxwell M, et al. . A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15:165–71. 10.1093/fampra/15.2.165 [DOI] [PubMed] [Google Scholar]
- 28.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 2000;31:73–86. 10.1016/S0005-7916(00)00012-4 [DOI] [PubMed] [Google Scholar]
- 29.Resnick B, Palmer MH, Jenkins LS, et al. . Path analysis of efficacy expectations and exercise behaviour in older adults. J Adv Nurs 2000;31:1309–15. 10.1046/j.1365-2648.2000.01463.x [DOI] [PubMed] [Google Scholar]
- 30.Tijou I, Yardley L, Sedikides C, et al. . Understanding adherence to physiotherapy: findings from an experimental simulation and an observational clinical study. Psychol Health 2010;25:231–47. 10.1080/08870440802372431 [DOI] [PubMed] [Google Scholar]
- 31.Kirby S, Donovan-Hall M, Yardley L. Measuring barriers to adherence: validation of the problematic experiences of therapy scale. Disabil Rehabil 2014;36:1924–9. 10.3109/09638288.2013.876106 [DOI] [PubMed] [Google Scholar]
- 32.Brooks R, Rabin R, De Charro F. The measurement and valuation of health status using EQ-5D: a European perspective: evidence from the EuroQol BIO MED research programme. Berlin: Springer Science & Business Media, 2003. [Google Scholar]
- 33.Curtis L, Burns A. Unit costs of health and social care. 2015.
- 34.Department of Health. NHS Reference costs 2014-15. 2014. Retrieved from https://www.gov.uk/government/publications/nhs-reference-costs-2014-to-2015
- 35.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 2005;4:287–91. 10.1002/pst.185 [DOI] [Google Scholar]
- 36.Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012;65:301–8. 10.1016/j.jclinepi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- 37.Hao L, Naiman DQ. Quantile regression. London: Sage Publications Inc, 2007. [Google Scholar]
- 38.Stratford PW, Binkley JM, Riddle DL, et al. . Sensitivity to change of the Roland-Morris Back Pain Questionnaire: part 1. Phys Ther 1998;78:1186–96. 10.1093/ptj/78.11.1186 [DOI] [PubMed] [Google Scholar]
- 39.Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53–72. 10.1016/0168-8510(96)00822-6 [DOI] [PubMed] [Google Scholar]
- 40.Haskell WL, Lee IM, Pate RR, et al. . Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007;39:1423–34. 10.1249/mss.0b013e3180616b27 [DOI] [PubMed] [Google Scholar]
- 41.Chiarotto A, Deyo RA, Terwee CB, et al. . Core outcome domains for clinical trials in non-specific low back pain. Eur Spine J 2015;24:1127–42. 10.1007/s00586-015-3892-3 [DOI] [PubMed] [Google Scholar]
- 42.Lee PH, Macfarlane DJ, Lam TH, et al. . Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act 2011;8:115 10.1186/1479-5868-8-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hallal PC, Gomez LF, Parra DC, et al. . Lessons learned after 10 years of IPAQ use in Brazil and Colombia. J Phys Act Health 2010;7(Suppl 2):S259–64. 10.1123/jpah.7.s2.s259 [DOI] [PubMed] [Google Scholar]
- 44.Napolitano MA, Borradaile KE, Lewis BA, et al. . Accelerometer use in a physical activity intervention trial. Contemp Clin Trials 2010;31:514–23. 10.1016/j.cct.2010.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hill JC, Whitehurst DG, Lewis M, et al. . Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet 2011;378:1560–71. 10.1016/S0140-6736(11)60937-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McNamee P, Murray E, Kelly MP, et al. . Designing and undertaking a health economics study of digital health interventions. Am J Prev Med 2016;51:852–60. 10.1016/j.amepre.2016.05.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.