Abstract
Background
In 2015, the second cycle of the CONCORD programme established global surveillance of cancer survival, as a metric of the effectiveness of health systems and to inform global policy on cancer control.
Methods
CONCORD-3 updates the world-wide surveillance of cancer survival to 2014, with individual data for 37.5 million patients diagnosed with cancer during the 15-year period 2000–2014. Data were provided by 322 population-based cancer registries in 71 countries and territories, of which 47 provided data with 100% population coverage. The study includes 18 cancers or groups of cancers: oesophagus, stomach, colon, rectum, liver, pancreas, lung, breast (women), cervix, ovary, prostate and melanoma of the skin in adults, and brain tumours, leukaemias and lymphomas in both adults and children. Standardised quality control procedures were applied; errors were rectified by the registry concerned. We estimated five-year net survival. Estimates were age-standardised with the International Cancer Survival Standard weights.
Findings
For most cancers, five-year net survival remains among the highest in the world in the US and Canada, in Australia and New Zealand, and in Finland, Iceland, Norway and Sweden. For many cancers, Denmark is closing the survival gap with the other Nordic countries. Survival trends are generally increasing, even for some of the more lethal cancers: in some countries, survival has increased by up to 5% for cancers of the liver, pancreas and lung. For women diagnosed during 2010–2014, the predicted five-year survival for breast cancer is now close to 90% in the US and in Australia, but international differences remain very wide, with levels as low as 40% in South Africa.
For gastrointestinal cancers, the highest levels of five-year survival are seen in South-East Asia, in Korea for cancers of the stomach (69%), colon (72%) and rectum (71%), in Japan for oesophageal cancer (36%) and in Taiwan for liver cancer (28%). By contrast, in the same world region, survival is generally lower than elsewhere for melanoma of the skin (60% in Korea, 52% in Taiwan, 50% in China), and for both lymphoid malignancies (53% in Korea, 51% in Taiwan, 38% in China) and myeloid malignancies (46% in Korea, 33% in Taiwan, 25% in China). For children diagnosed during 2010–2014, five-year survival for acute lymphoblastic leukaemia ranged from 66% in Thailand to 95% in Finland. Five-year survival from brain tumours in children is higher than for adults, and the global range is very wide (from 45% in Thailand to 80% in Sweden and Denmark).
Interpretation
The CONCORD programme enables timely comparisons of the overall effectiveness of health systems in providing care for 18 cancers that collectively represent 75% of all cancers diagnosed world-wide every year. It contributes to the evidence base for global policy on cancer control. From 2017, the Organisation for Economic Co-operation and Development will use findings from the CONCORD programme as the official benchmark of cancer survival, among their indicators of the quality of health care in 48 countries world-wide. It is crucial for governments to recognise population-based cancer registries as key policy tools that can be used to evaluate both the impact of cancer prevention strategies and the effectiveness of health systems for all patients diagnosed with cancer.
Keywords: population-based cancer registry, net survival, surveillance, global health
Introduction
The incidence of cancer continues to rise, both in high-income countries and, especially, in low- and middle-income countries. Prevention is crucial, but implementation has been slow and incomplete, even in high-income countries. Prevention is a long-term strategy, and not all cancers can be prevented.1 To reduce cancer mortality, it is necessary both to reduce cancer incidence and to improve cancer survival.
Many cancer patients will continue to be diagnosed every year for decades to come: an estimated 14 million patients a year world-wide around 2012,2 with a 50% projected increase to 21.6 million patients a year by 2030.3 Those patients will all need prompt diagnosis and optimal treatment, to improve their survival. Monitoring the effectiveness of national and regional health systems in treating and caring for these patients becomes ever more crucial.
In 2016, the WHO Executive Board recommended strengthening health systems to ensure early diagnosis and accessible, affordable, high-quality care for all cancer patients.3 The World Health Assembly followed up with a resolution on cancer control in May 2017. It included recommendations that national cancer control strategies should aim to reduce late presentation, ensure appropriate treatment and care for potentially curable malignancies such as acute leukaemia in children, “to increase survival, reduce mortality and improve quality of life.”4
President Tabaré Vázquez of Uruguay and WHO Director-General Tedros Ghebreyesus recently called for all countries “to provide universal health coverage, thereby ensuring all people can access needed preventive and curative health-care services, without falling into poverty.”5 Their call relates to all non-communicable diseases, including cancer. Population-based cancer survival is one metric that can help evaluate whether all people have access to effective treatment services.
In 2015, the CONCORD programme established global surveillance of cancer survival for the first time,6 with publication of trends in survival over the 15-year period 1995–2009 among patients diagnosed with cancer in 67 countries that were home to two-thirds (4.8 billion) of the world’s population. In 40 countries, the data had 100% national population coverage. CONCORD-2 incorporated centralised quality control and analysis of individual data for 25,676,887 patients diagnosed with one of 10 common cancers that represented 63% of the global cancer burden in 2009. The 279 population-based registries covered a combined total population of 896 million people.
The US National Cancer Institute, in an invited commentary7 for The Lancet, noted that the global analyses of cancer survival in CONCORD-2 provided insights from countries with successful cancer control initiatives that could be applied in other regions, and that the availability of better data “provides a clearer picture of the effect of cancer control programmes on the ultimate goal of improving survival and reducing the effect of cancer on the social and economic development of countries.”
The US Centers for Disease Control and Prevention (CDC) described CONCORD-2 as the start of global surveillance of cancer survival,a with survival estimates “that can be compared, so scientists can begin to determine why survival differs among countries. This could lead to improvements in cancer control programs.” The results from CONCORD-2 influenced national cancer control strategy in the UK in July 2015.8,9 In September 2015, the International Atomic Energy Agency’s Programme for Action on Cancer Therapy (PACT) used the results to launch a world-wide campaignb to highlight the global divide in cancer survival, and to raise awareness of persistent inequalities in access to life-saving cancer services.10 Further analysis of survival trends and disparities by race and stage at diagnosis in 37 US states are included in a forthcoming supplement to Cancer,11,12 designed to improve cancer control in the US.
CONCORD-3 updates world-wide surveillance of cancer survival trends to include patients diagnosed up to 2014, with follow-up to 31 December 2014. In countries that were already involved, more registries are participating, and 8 more countries have joined the programme. Follow-up for patients diagnosed during 2000–2009 with one of the 10 cancers included in CONCORD-2 has been updated. CONCORD-3 includes data for patients diagnosed during 2000–2014 with one of 18 malignancies that represent 75% of the global cancer burden (Table 1). In addition to information on stage at diagnosis, we have collected data on tumour grade and the first course of treatment. Findings are published within 3 years of the end of follow-up.
Table 1.
Estimated number of patients diagnosed with an index cancer* world-wide each year around 2012: by world region†
| Overall
|
More developed
|
Less developed
|
||||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Oesophagus | 455,784 | 3.2 | 86,144 | 1.4 | 369,640 | 4.6 |
| Stomach | 951,594 | 6.8 | 274,509 | 4.5 | 677,085 | 8.4 |
| Colorectum | 1,360,602 | 9.7 | 736,867 | 12.2 | 623,735 | 7.8 |
|
| ||||||
| Liver | 782,451 | 5.6 | 134,302 | 2.2 | 648,149 | 8.1 |
| Pancreas | 337,872 | 2.4 | 187,465 | 3.1 | 150,407 | 1.9 |
| Lung | 1,824,701 | 13.0 | 758,214 | 12.5 | 1,066,487 | 13.3 |
|
| ||||||
| Melanoma | 232,130 | 1.7 | 191,066 | 3.2 | 41,064 | 0.5 |
| Breast (F) | 1,671,149 | 11.9 | 788,200 | 13.0 | 882,949 | 11.0 |
| Cervix | 527,624 | 3.8 | 83,078 | 1.4 | 444,546 | 5.5 |
|
| ||||||
| Ovary | 238,719 | 1.7 | 99,752 | 1.6 | 138,967 | 1.7 |
| Prostate | 1,094,916 | 7.8 | 741,966 | 12.3 | 352,950 | 4.4 |
| Brain and CNS | 256,213 | 1.8 | 88,967 | 1.5 | 167,246 | 2.1 |
|
| ||||||
| Lymphomas | 451,691 | 3.2 | 219,255 | 3.6 | 232,436 | 2.9 |
| Leukaemias | 351,965 | 2.5 | 141,274 | 2.3 | 210,691 | 2.6 |
| All index cancers‡ | 10,537,411 | 74.9 | 4,531,059 | 74.8 | 6,006,352 | 74.9 |
|
| ||||||
| All cancers | 14,067,894 | 100.0 | 6,053,621 | 100.0 | 8,014,273 | 100.0 |
Source: Globocan 201213
Index cancer: cancer or group of malignancies included in CONCORD-3.
“More developed”: Northern America, Europe, Australia, New Zealand and Japan; “Less developed”: other countries and regions.13 These are UN designations intended for statistical convenience and do not reflect a judgement about the stage reached by a particular country or area in the development process.24
All cancers except non-melanoma skin cancer
Methods
Cancer registries
We contacted 412 cancer registries in 85 countries: 20 in Africa (13 countries), 45 in Central and South America (15 countries), 68 in North America (2 countries), 80 in Asia (20 countries), 189 in Europe (33 countries) and 10 in Oceania (2 countries).
When the data call for CONCORD-3 was issued in May 2016, 12 of the 279 cancer registries that had participated in CONCORD-2 were no longer operational. The registry in Benghazi (Libya) was disrupted by war, the registry in Macerata (Italy) ceased operating, the Department of Health ceased funding the UK National Registry of Childhood Tumours in 2013, and the 9 English regional cancer registries were replaced by a single cancer registry for England in 2013. Of the 267 remaining registries, nine could no longer provide up-to-date follow-up of all registered patients, while 13 did not reply to repeated approaches. Data from the Tirol (Austria) registry are no longer reported separately from the Austrian national estimates. In all, 244 (87%) of the 279 registries (63 of the 67 countries) that participated in CONCORD-2 submitted data.
Of the 133 registries that had not previously participated in the CONCORD programme, 108 agreed to do so. Of these, 85 (78%) registries in 12 countries submitted data, while 11 were unable to complete follow-up of registered cancer patients for their vital status, 9 made no further contact, and 3 signed up too late.
Of the 329 registries that submitted data, 7 were excluded because their data were not compliant with the protocol and could not be rectified in time. These exclusions affected the only participating registry or registries from several countries: Tunisia (Central Region), Bosnia Herzegovina (Republika Srpska), Saudi Arabia and Serbia (Central Region and Vojvodina). We analysed data provided by 322 cancer registries (81% of the 400 operational registries invited) in 71 countries and territories (text-figure 1), for patients diagnosed with cancer during the 15-year period 2000–2014, with data on their vital status at least five years after diagnosis, or at 31 December 2014.
Text-figure 1. Recruitment of cancer registries.
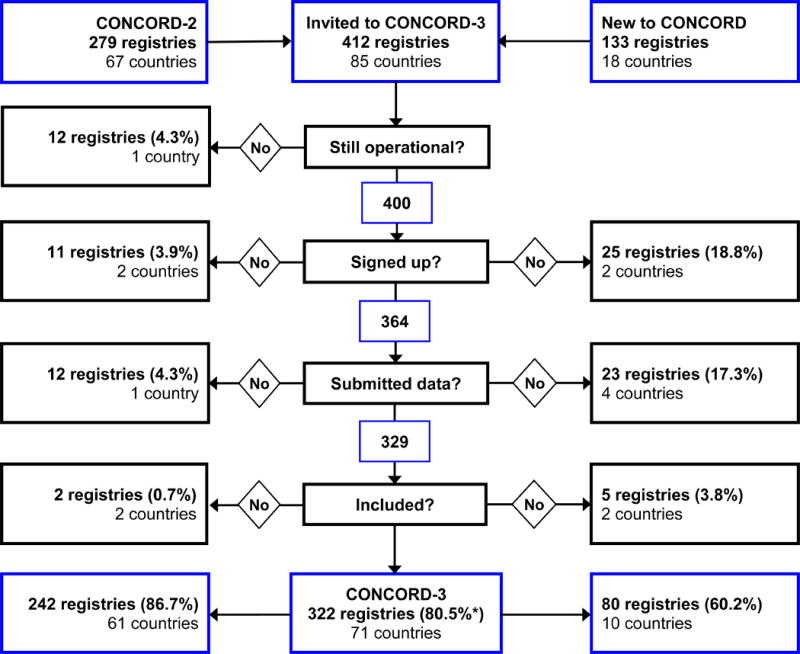
*Of the 400 operational registries invited; all other percentages refer to the number of registries at the top of each column. The number of countries excluded (black boxes) refers to those for which exclusions affected the only participating cancer registry or registries.
Eight countries are participating in the global surveillance of cancer survival for the first time: Africa: Morocco; Central and South America: Costa Rica (national), Mexico (children, national), and Peru; Asia: Iran, Kuwait (national) and Singapore (national), and Europe: Greece (children, national).
Protocol
The CONCORD-3 protocol defining the data structure, file transmission procedures and statistical analyses was expanded and updated from the CONCORD-2 protocol, with the addition of variables on five additional cancers or groups of malignancies, tumour grade, and the modality and date of the first course of treatment by surgery, radiotherapy or systemic therapy.
In a study of this scale, adherence to protocol is critical. The protocol and analytic approaches were discussed with CONCORD Working Group members from 27 countries at a one-day meeting in Marrakech, Morocco, in October 2016. The protocol was also discussed at workshops in China, the Russian Federation, Romania, Singapore and the USA (for North America), and in conference calls with Costa Rica, Hong Kong, Malaysia, Mauritius, Mexico and Mongolia.
English is still a barrier to communication in many countries, so the CONCORD-3 protocol was translated into eight other languages: Arabic, Chinese (Mandarin), French, Italian, Japanese, Portuguese, Russian and Spanish. Translations were done by native speakers in the CONCORD Central Analytic Team in London or the wider CONCORD Working Group, and checked against the English original by other native speakers. The protocol was made available to participants in all nine languages on the CONCORD web-site. The Central Analytic Team communicates with participants in six languages.
We examined survival for 18 cancers or groups of malignancies (“index cancers”): oesophagus, stomach, colon, rectum, liver, pancreas, lung, melanoma of the skin, breast (women), cervix, ovary and prostate in adults (15–99 years); brain tumours, myeloid and lymphoid malignancies in adults, and brain tumours, acute lymphoblastic leukaemia (ALL) and lymphomas in children (0–14 years). Collectively, these cancers accounted for about 75% of the estimated number of patients diagnosed with cancer world-wide each year around 2012 (10,537,411 of 14,067,894, excluding non-melanoma skin cancer; Table 1).13 The overall proportion is very similar in Northern America, Europe, Australia, New Zealand and Japan (“developed countries”) and in other world regions (“developing countries”), but it varies widely between cancers: prostate cancer is proportionately three times more common in developed countries, and cervical cancer four times more common in developing countries.
Solid tumours were defined by anatomic site (topography), and the leukaemias, lymphomas and melanoma of the skin by morphology (Table 2). Topography and morphology were coded to the International Classification of Diseases for Oncology (third edition, ICD-O-3),14 including its first revision.15 We restricted estimation of survival for melanomas to those arising in the skin, including the skin of the labia majora, vulva, penis and scrotum (ICD-O-3 C51.0, C51.9, C60.9, C63.2). Melanomas arising in internal organs were included with all other malignancies in those organs. For ovarian cancer, we included the fallopian tube, uterine ligaments and adnexa, as well as the peritoneum and retroperitoneum, where high-grade serous ovarian carcinomas are often detected.16 Registries were not asked to select cancers by sex, although some did so. Where data sets did include records for breast cancer in men, the proportion was consistently around 0.7%; these records were excluded. We also excluded small numbers of retroperitoneal malignancies in men, as well as Kaposi sarcoma, and tumours in solid organs with haematopoietic morphology.
Table 2.
Definition of malignancies, and number of contributing countries and registries*, by calendar period of diagnosis
| Malignancy | Topography and/or morphology codes† | Description | Contributing countries and registries*
|
||||
|---|---|---|---|---|---|---|---|
| Any period | |||||||
| 2000–2004 | 2005–2009 | 2010–2014 | 2000–2014 | ||||
| Oesophagus | C15.0–C15.5; C15.8–C15.9 | Oesophagus | Countries | 55 | 59 | 58 | 60 |
| Registries | 249 | 287 | 273 | 290 | |||
|
| |||||||
| Stomach | C16.0–C16.6; C16.8–C16.9 | Stomach | Countries | 57 | 62 | 60 | 62 |
| Registries | 252 | 293 | 277 | 294 | |||
|
| |||||||
| Colon | C18.0–C18.9; C19.9 | Colon and rectosigmoid junction | Countries | 57 | 64 | 64 | 65 |
| Registries | 251 | 294 | 280 | 296 | |||
|
| |||||||
| Rectum | C20.9; C21.0–C21.2; C21.8 | Rectum, anus and anal canal | Countries | 56 | 63 | 63 | 64 |
| Registries | 250 | 292 | 278 | 294 | |||
|
| |||||||
| Liver | C22.0–C22.1 | Liver and intrahepatic bile ducts | Countries | 56 | 60 | 60 | 61 |
| Registries | 250 | 289 | 275 | 291 | |||
|
| |||||||
| Pancreas | C25.0–C25.4; C25.7–C25.9 | Pancreas | Countries | 55 | 58 | 58 | 59 |
| Registries | 249 | 288 | 274 | 290 | |||
|
| |||||||
| Lung | C34.0–C34.3; C34.8–C34.9 | Lung and bronchus | Countries | 57 | 61 | 61 | 61 |
| Registries | 250 | 289 | 275 | 290 | |||
|
| |||||||
| Melanoma of the skin | 8720–8790 provided topography was C44.0– C44.9, C51.0, C51.9, C60.9 or C63.2 | Melanoma of the skin, including skin of labia majora, vulva, penis and scrotum | Countries | 55 | 58 | 59 | 59 |
| Registries | 239 | 278 | 266 | 281 | |||
|
| |||||||
| Breast (women) | C50.0–C50.6; C50.8–C50.9 | Breast | Countries | 59 | 64 | 65 | 66 |
| Registries | 255 | 295 | 282 | 298 | |||
|
| |||||||
| Cervix | C53.0–C53.1; C53.8–C53.9 | Cervix uteri | Countries | 57 | 63 | 62 | 64 |
| Registries | 253 | 293 | 277 | 295 | |||
|
| |||||||
| Ovary | C48.0–C48.2; C56.9; C57.0–C57.4; C57.7–C57.9 | Ovary, fallopian tube and uterine ligaments, other and unspecified female genital organs, peritoneum and retroperitoneum | Countries | 56 | 61 | 59 | 61 |
| Registries | 249 | 288 | 272 | 289 | |||
|
| |||||||
| Prostate | C61.9 | Prostate gland | Countries | 58 | 62 | 62 | 62 |
| Registries | 249 | 289 | 275 | 290 | |||
|
| |||||||
| Brain | C71.0–C71.9 | Brain (adults) | Countries | 55 | 58 | 58 | 59 |
| Registries | 247 | 283 | 269 | 286 | |||
| Brain (children) | Countries | 54 | 58 | 60 | 60 | ||
| Registries | 219 | 257 | 245 | 260 | |||
|
| |||||||
| Myeloid (adults)ǂ | 9740; 9741; 9742; 9800; 9801; 9805; 9806; 9807; 9808; 9809; 9840; 9860; 9861; 9863; 9865; 9866; 9867; 9869; 9870; 9871; 9872; 9873; 9874; 9875; 9876; 9891; 9895; 9896; 9897; 9898; 9910; 9911; 9920; 9930; 9931; 9945; 9946; 9950; 9960; 9961; 9962; 9963; 9964; 9975; 9980; 9982; 9983; 9984; 9985; 9986; 9987; 9989; 9991; 9992 | All myeloid malignancies | Countries Registries |
56 249 |
59 280 |
60 268 |
61 286 |
|
| |||||||
| Lymphoid (adults)ǂ | 9590; 9591; 9596; 9597; 9650–9655; 9659; 9661– 9665; 9667; 9670; 9671; 9673; 9675; 9678; 9679; 9680; 9684; 9687–9691; 9695; 9698; 9699; 9700–9702; 9705; 9708; 9709; 9712; 9714; 9716– 9719; 9725–9729; 9731–9735; 9737; 9738; 9760– 9762; 9764; 9811–9818; 9820; 9823; 9826; 9827; 9831–9837; 9940; 9948 | All lymphoid malignancies | Countries Registries |
57 250 |
60 284 |
61 271 |
62 289 |
|
| |||||||
| Acute lymphoblastic leukaemia (children)¶ | 9835–9837; plus 9811–9818 provided topography was C42.0, C42.1, C42.3, C42.4 or C80.9 | Precursor-cell acute lymphoblastic leukaemia (ALL) | Countries Registries |
56 214 |
60 247 |
61 233 |
61 254 |
|
| |||||||
| Lymphoma (children)¶ | 9590; 9591; 9596; 9597; 9650–9655; 9659; 9661– 9665; 9667; 9670; 9671; 9673; 9675; 9678–9680; 9684; 9687–9691; 9695; 9698–9702; 9705; 9708; 9709; 9712; 9714; 9716–9719; 9725–9729; 9731– 9735; 9737; 9738; 9740–9742; 9750–9762; 9764– 9769; 9970; 9971; plus 9811–9818 provided topography was not C42.0, C42.1, C42.3, C42.4 or C80.9 | All lymphomas | Countries Registries |
55 214 |
60 253 |
62 235 |
62 257 |
Some registries contributed data for selected cancers and/or calendar periods, so the number of participating countries also varies by cancer and calendar period. The number of countries and registries that contributed data at some point during 2000–2014 (last column) is thus greater than or equal to the number in any five-year period.
Lymphoid malignancies were defined by HAEMACARE17 groups 1–19 and myeloid malignancies by HAEMACARE groups 20–25, incorporating morphology codes from the first revision of ICD-O-3 (see text).
Registries provided data for all haematopoietic malignancies (ICD-O-3 morphology codes in the range 9590–9992) in adults and children, to minimise differences in the spectrum of leukaemias and lymphomas submitted for analysis. In consultation with specialists in the HAEMACARE17 and InterLymph18,19 groups, we agreed to analyse survival for adults in two broad groups: lymphoid malignancies (HAEMACARE groups 1–19) and myeloid malignancies (groups 20–25; Table 2, web-table 1).
For children, we agreed to present survival estimates separately for ALL and lymphomas, based on ICD-O-3 codes, grouped according to the third edition of the International Classification of Childhood Cancer (ICCC-3).20 The first revision of ICD-O-3, published in 2013,15 introduced eight new entities for acute lymphoblastic leukaemia/lymphoma (morphology codes 9811–9818). These new entities were not used at all by registries in 42 of the 58 countries that submitted data for children diagnosed with ALL during 2010–2014, and very rarely in eight countries (combined number of children coded to a new entity below 100), but the proportions ranged from 11% to 89% in large data sets from Australia, Belgium, Canada, the Netherlands, Puerto Rico, Singapore, Taiwan and the US. The overall proportion for all 58 countries combined during 2010–2014 was 29% (10,679 of 36,867 children). We therefore included the new entities in all analyses. They were included among the acute lymphoblastic leukaemias if the anatomic site was coded as blood, bone marrow, reticulo-endothelial or haematopoietic systems (not otherwise specified) (C42.0–42.1, C42.3–42.4), or unknown primary site (C80.9). Otherwise such malignancies were included with the lymphomas (web-table 1).
Survival analyses include only primary, invasive malignancies (ICD-O-3 behaviour code 3), except for the brain, where benign tumours (behaviour code 0) are also included. To facilitate quality control and comparison of the intensity of early diagnostic and screening activity, registries were asked to provide data for all registered malignancies at each index site, including those that were benign, of uncertain or borderline malignancy (1), in situ (2), metastatic (6) or uncertain whether primary or metastatic (9).
Registries were asked to provide full dates (day, month, year) of birth, diagnosis and death or last known vital status, both for quality control and to enable comparable estimation of survival.21 Where the day or month of birth, or the day of the date of diagnosis, or the day or month of the date of last known vital status was missing, we used an algorithm (details on request) to standardise the imputation of missing dates for all populations.
Participating registries completed a questionnaire on their methods of operation, including data definitions, data collection procedures, coding of anatomic site, morphology and behaviour, the tracing of registered cancer patients to ascertain their vital status, and how tumour records are linked with data on vital status.
Patients diagnosed with two or more primary cancers at different index sites during 2000–2014 were included in the analyses for each cancer, e.g. colon cancer in 2005 followed by a breast cancer in 2010. Survival was measured from the date of diagnosis until death, loss to follow-up or censoring. We retained the most complete record for patients with synchronous primary cancers in the same organ. If a patient was registered with two or more primary malignancies in the same index site during 2000–2014 (metachronous primaries), only the first was included in analyses.
North American registries define multiple primary cancers under the rules of the Surveillance Epidemiology and End Results (SEER) programme.22 Those rules accept more cancers as new primary cancers than the rules of the International Association of Cancer Registries (IACR),23 which are used by most cancer registries in other continents. The North American Association of Central Cancer Registries (NAACCR) kindly updated the program developed for CONCORD-2 to enable all North American registries to recode their entire incidence databases to the IACR multiple primary rules, before their data sets for 2000–2014 were extracted for CONCORD-3.
Countries and territories were defined by their UN name, continent and code as of 2015.24 The names of jurisdictions used in the text, tables, graphics, maps and web-appendix are those used for statistical purposes by the Statistics Division of the UN Secretariat; similarly, we use “national coverage” to contrast with “regional coverage” for statistical purposes. These designations and the presentation of data here do not imply any assumption regarding the political affiliation of countries or territories, or the expression of any opinion whatsoever on the part of the CONCORD programme concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Some names have been shortened for convenience (e.g. Korea for the Republic of Korea, Russia for Russian Federation): this does not carry any political significance.
Cyprus is a Member State of the European Union, but it is part of Asia. Costa Rica, Cuba, Guadeloupe, Martinique, Mexico and Puerto Rico (Caribbean and Central America) were grouped with South America as America (Central and South). World maps and 29 regional maps were prepared in ArcGIS® Release 10.3,25 using digital boundaries (shapefiles) from the Database of Global Administrative Areas (GADM 2.8).26
The population coverage of the data from participating registries is given as the proportion of the country or jurisdiction’s population, taken from the UN Population Division database for 2014,27 or from the authorities for Australia, Guadeloupe, Hong Kong, Poland, Portugal and Taiwan or the registries concerned. Belarus, Greece and Mexico provided data only for childhood cancers, so the populations used were for children (0–14 years), and Mali, Mongolia and Morocco only provided cancer data for women, so the female populations were used.
Quality control
As for the previous cycle of the CONCORD programme,6 we performed data quality checks in three phases: protocol adherence, exclusions, and editorial checks. After each phase, a detailed report was sent to each cancer registry for discussion, and correction of data where required.
First, registries were sent a report showing the percentage compliance with the protocol for each of 51 variables in each cancer file. Compliance less than 100% required correction and/or re-submission of data.
Next, we checked for logical inconsistencies between the variables in each tumour record. Exclusion criteria were defined a priori, based on experience from CONCORD-2, and extended to cover features of some of the five additional cancers such as Ann Arbor stage for the lymphomas, and 14 additional variables on tumour grade and treatment. The variables in each record were checked for logical coherence against 20 sets of criteria, including eligibility (e.g. age, tumour behaviour), definite errors (e.g. sex-site errors, invalid dates, impossible date sequence, missing vital status) and possible errors, including a wide range of inconsistencies between age, tumour site and morphology.6,28 Registries were sent ‘exclusion reports’ for each index cancer and each calendar period, summarising the number of tumour records with each type of definite or possible error, the number registered from a death certificate only (DCO) or detected at autopsy, and the number and proportion of eligible patients whose data could be included in survival analyses. Registries were invited to request details of tumour records in which errors had been detected. Many registries used this information to update their databases. Where errors in classification, coding or pathological assignment were identified, registries were asked to correct and re-submit their data.
Finally, we examined the proportion of tumour records with morphological verification of the diagnosis, whether from histology of a biopsy or surgical specimen, cytology of a smear or bone marrow aspirate, or from imaging or biomarkers, including tumours with a specific morphology code. We also examined the proportion of cases with non-specific morphology, the distributions of the day and month of the dates of birth, diagnosis and last known vital status, and the proportion of patients who died within 30 days, were lost to follow-up, or were censored within 5 years of diagnosis.
Follow-up for vital status
Cancer registries use various methods to determine the vital status (alive, dead, emigrated, lost to follow-up) of registered cancer patients.6 Among 243 registries that provided specific information on follow-up procedures, 242 (99%) determine the vital status of registered cancer patients using passive follow-up techniques, in which tumour registration records are regularly linked to a regional or national index of all death registrations, regardless of the cause of death. Linkages are usually based on a national identity or social security number that is stored in both records. Such linkages are increasingly done electronically, but manual scrutiny of printed lists is still required in places. Tumour records that match to a death record are updated with the date of death. Some registries routinely receive paper or electronic death certificates for their territory, but this is insufficient on its own, since death certificates that do not mention cancer are rarely included. Transcription errors can arise with identity numbers, so variables such as the name, sex and date of birth are often used to improve the probability of an accurate match between a cancer record and a death registration.
Many registries use electoral registers, hospital records or official databases, such as social insurance, health insurance and driving licences, to determine the date on which a patient was last known or believed to have been alive. Patients recorded as having migrated beyond the registry’s jurisdiction, or to another country, may be recorded as lost to follow-up, because the patient’s eventual death is unlikely to be recorded: they are censored from survival analysis on that date.
Active follow-up techniques are also used by 124 (51.0%) registries, which routinely contact the treating physician, GP or hospital administration to determine the vital status for each registered patient, often on a quarterly or annual basis. Some registries also determine the vital status by contact with the patient’s family, by telephone or home visit, or with the village administration.
Registries were asked to submit data with follow-up for at least 5 years or, for patients diagnosed during 2010–2014, until 31 December 2014. Registration and follow-up for patients diagnosed in 2000–2009 was updated, and new data sets were submitted.
Patients registered solely from a death certificate or diagnosed at autopsy were excluded from analyses, because their survival time is unknown.
Statistical methods
Most registries submitted data for patients diagnosed from 2000 to 2014, with follow-up to 2014, although some registries only began operation after 2000, or provided data for less than 15 years. The study design for examining survival trends among patients diagnosed in three consecutive five-year periods was cohort, cohort, period. This design was also used for CONCORD-2,6 so it enables us to examine global trends in survival over a 20-year period, by including the estimates for patients diagnosed during 1995–1999.
The cohort approach is considered the gold standard,29,30 because it provides a survival estimate for a group of patients who were diagnosed during the same year or period, are likely to have been treated in similar fashion, and who have all been followed up for at least the duration of survival required, such as 5 years. This approach to the estimation of survival is easy to interpret, but other approaches are required when some patients have been followed up for less than 5 years.
We used the cohort approach for patients diagnosed in 2000–2004 and 2005–2009, because in most data sets, all patients had been followed up for at least five years. We used the period approach31 for patients diagnosed during 2010–2014, because five years of follow-up data were not available for all patients. This combination of cohort and period approaches facilitates monitoring of cancer survival trends over an extended time span, from the earliest to the most recent years of cancer registration for which follow-up data are available (web-annex 1).32
To ensure comparability of survival trends from 1995,6 we estimated net survival up to five years after diagnosis for both adults and children. Net survival is the cumulative probability of surviving up to a given time since diagnosis (e.g. 5 years) after correcting for other causes of death (background mortality). We used the Pohar Perme estimator,33 which takes unbiased account of the higher competing risks of death in the elderly, implemented with the algorithm stns34 in Stata (version 14).35
To control for the wide differences in background mortality between participating jurisdictions and over time, we produced 8,790 life tables of all-cause mortality for each calendar year during 2000–2014 in the general population of each country or registry territory, by single year of age and sex, and by race/ethnicity in Australia (Northern Territory: Indigenous, non-Indigenous), Israel (Arab, Jewish), New Zealand (Māori, non-Māori) and Singapore (Chinese, Malay, Indian).
For 120 registries, we obtained complete life tables that did not require interpolation or smoothing, for each calendar year 2000–2014.
For 207 registries, the method of life table construction depended on whether we received raw data (numbers of deaths and populations) or mortality rates, and on whether the raw data or the mortality rates were by single year of age (“complete”) or by five-year age group (“abridged”).
For 109 registries, we obtained death and population counts from the registry, or the relevant national statistical authority. We derived life tables for 2001 and 2013 if possible, each centred on three calendar years of data (e.g. 2000–2002, 2012–2014) to increase the robustness of the rates. We constructed raw mortality rates from the death and population counts using a Poisson regression model with flexible functions,36 then smoothed and extended the rates to obtain complete life tables by sex and single year of age up to age 99 years. Life tables for each calendar year 2002–2012 were created by linear interpolation between the 2001 and 2010 life tables.37 Rather than extrapolate, we used the life table centred on 2001 for 2000, and the life table centred on 2013 for 2014.
For 64 registries that provided abridged mortality rates, or complete mortality rates that were not smoothed, we used the Ewbank relational model38 with 3 or 4 parameters to interpolate (if abridged) and smooth the mortality rates for the registry territory against a high-quality smooth life table for a country with a similar pattern of mortality by age.39
Each set of life tables was checked with a standardised statistical summary on the earliest and latest year of available data, showing the data source and the method of construction and smoothing. For each sex and, where relevant, each race or ethnicity, the reports show the life expectancy at birth, the probability of death in the age bands 15–59, 60–84 and 85–99 years, and semi-log plots of the age-mortality rates, showing both the raw data points and the final smoothed life-table curve, and the model residuals by age group (web-annex 2).
Collection of authoritative raw data on the numbers of deaths and populations by age, sex and calendar year or period in participating jurisdictions proved more difficult than in 2013–2014. For 34 registries, no reliable data on all-cause mortality could be obtained for the registry territory. We took national life tables published by the UN Population Division,27 and interpolated and extended them to age 99 years with the Elandt-Johnson method.40
For the 42 participating states in the US, we used life tables by state, race and socioeconomic status, provided by the US National Cancer Institute (Mariotto A, NCI, personal communication, 26 January 2016).
For each country, registry and calendar period, we present age-standardised net survival estimates for each cancer at five years after diagnosis. For adults, we used the International Cancer Survival Standard (ICSS) weights,41 in which age at diagnosis is categorised into 5 groups: 15–44, 45–54, 55–64, 65–74 and 75–99 years and, for prostate cancer, 15–54, 55–64, 65–74, 75–84 and 85–99 years. Of the three sets of ICSS weights, we used group 2 (cancers for which incidence does not increase steeply with age) for melanoma of the skin, cervix uteri and brain (adults), and group 1 (cancers for which incidence does increase steeply with age) for oesophagus, stomach, colon, rectum, liver, pancreas, lung, breast, ovary and prostate, and both groups of haematopoietic malignancies. For children, we estimated survival for the age groups 0–4, 5–9 and 10–14 years; age-standardised estimates were obtained by assigning equal weights to the three age-specific estimates.41,42
Cumulative survival probabilities in the range 0–1 are presented for convenience as percentages in the range 0–100%. 95% confidence intervals for both unstandardised and age-standardised survival estimates were derived assuming a Normal distribution, truncated to the range 0–100. Standard errors to construct the confidence intervals were derived with the Greenwood method.43 If no death or censoring occurred within 5 years, or if all patients died within five years (survival probability 1 or zero) we obtained a binomial approximation for the lower and upper bound, respectively, of the confidence interval.29
Survival was not estimated if fewer than 10 patients were available for analysis. If 10–49 patients were available for analysis in a given calendar period, we only estimated survival for all ages combined. If 50 or more patients were available, we attempted survival estimation for each age group. If a single age-specific estimate could not be obtained, we merged the data for adjacent age groups and assigned the combined estimate to both age groups before standardisation for age. If two or more age-specific estimates could not be obtained, we present only the unstandardised estimate for all ages combined. We did not merge data between consecutive calendar periods.
The pooled estimates for countries with more than one registry do not include data from registries for which the estimates were less reliable. Less reliable estimates are reported with a flag when they are the only available information from a given country or territory.
Ethical approvals and confidentiality
We maintain approvals from the Ethics and Confidentiality Committee of the UK’s statutory Health Research Authority (HRA) (reference ECC 3–04(i)/2011, last update 3 March 2017) the National Health Service Research Ethics Service (11/LO/0331, 21 February 2017) and the London School of Hygiene and Tropical Medicine (12171, 6 September 2017). The HRA also approves the Cancer Survival Group’s System-Level Security Policy, governing data security. One investigator (MPC) maintains triennial certification with the Collaborative Institutional Training Initiative in Human Subjects Research for Biomedical Investigators (https://www.citiprogram.org, ID3327653, 2 May 2016). We maintain statutory and/or ethical approvals and data sharing agreements, usually with annual renewal, in 85 other jurisdictions participating in the CONCORD programme. Registries in all other jurisdictions obtain local approval. The data belong to the participating registries and are only used for purposes agreed in the CONCORD protocol.
Participants transmit data via a specially configured file transmission utility with 256-bit Advanced Encryption Security. The utility automatically generates a random, strong, one-time password for each data file at the time of transmission, and emails it to a different address. Neither the password nor the address are seen by the sender. This avoids the need for confirmation of passwords by email or telephone. Tumour records are effectively anonymised: they do not contain the patient’s name, address, postcode, or any national identity or social security number. All variables are numeric or alphanumeric codes. Each registry is sent a set of unique codes that must be used in naming each cancer data file, including distinct filenames for any re-transmission. The codes have no meaning outside the study. Data files thus contain no information that could be used to identify a person or a cancer registry, and neither the name nor the content of the file indicates that it even contains cancer data. This enhances security, as well as facilitating efficient handling of thousands of data files.
Role of the funding sources
The funding sources played no part in the design, data collection, quality control, analysis, interpretation of the findings, writing of the manuscript, or the decision to submit for publication. The corresponding author had full access to all data and responsibility for submission for publication.
Results
The CONCORD database 2000–2014
Data were analysed for 322 cancer registries in 71 countries in Africa (8 registries, 6 countries), Central and South America (33 registries, 13 countries), North America (57 registries, 2 countries), Asia (66 registries, 17 countries), Europe (149 registries, 31 countries) and Oceania (9 registries, 2 countries) (Figure 1).
Figure 1. Participating countries and regions: world (adults).
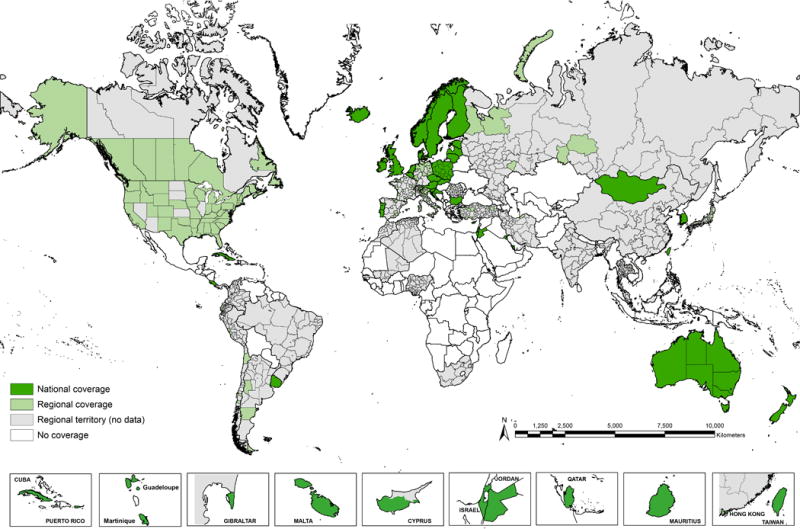
Registries in smaller countries are shown in boxes, at different scales.
See web-figures 1.1–1.29 for regional maps, and web-figure 1.30 for world map for childhood cancers.
For 47 countries, data were provided with 100% coverage of the national population: 41 for both adults and children, and 6 for children only (Argentina, Belarus, France, Greece, Mexico and Switzerland) (Table 3). In the other countries, population coverage varied from less than 1% in India to 86% in the US. More than 80 cancer registries joined the CONCORD programme for the first time. The 322 participating registries cover a combined population of almost one billion people around 2014 (989,082,244; Table 4). Detailed maps of participating jurisdictions are shown in web-figures 1.1–1.30.
Table 3.
Data quality indicators, patients diagnosed during 2000–2014, by continent and country
| Calendar period |
Patients submitted |
Ineligible (%)¶
|
Eligible patients |
Excluded (%)‖‖
|
Patients included |
Data quality indicators (%) ††
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incomplete dates |
In situ | Other | DCO | Other | MV | Non-specific morphology |
Lost to follow-up |
Censored | |||||
| AFRICA | 46,627 | 9.6 | 0.4 | 1.1 | 41,447 | 0.9 | 2.1 | 40,197 | 91.6 | 14.1 | 7.6 | 37.7 | |
|
| |||||||||||||
| Algerian registries | 2000–2014 | 18,157 | 7.6 | 0.1 | 1.8 | 16,434 | 1.8 | 3.3 | 15,602 | 98.4 | 10.2 | 0.0 | 31.5 |
| Mali (Bamako) | 2010–2012 | 104 | 41.3 | 0.0 | 0.0 | 61 | 0.0 | 1.6 | 60 | 100.0 | 20.0 | 0.0 | 0.0 |
| Mauritius* | 2005–2012 | 4,125 | 0.0 | 0.0 | 0.4 | 4,109 | 0.0 | 3.7 | 3,959 | 96.7 | 19.8 | 0.0 | 2.3 |
| Morocco (Casablanca) | 2008–2012 | 4,840 | 1.4 | 0.0 | 0.1 | 4,769 | 0.0 | 1.8 | 4,683 | 100.0 | 2.4 | 33.0 | 35.6 |
| Nigeria (Ibadan) | 2003–2014 | 11,726 | 25.4 | 1.4 | 1.2 | 8,443 | 0.9 | 1.1 | 8,274 | 98.7 | 2.0 | 0.0 | 65.3 |
| South Africa (Eastern Cape) | 2000–2014 | 7,675 | 0.0 | 0.0 | 0.6 | 7,631 | 0.0 | 0.2 | 7,619 | 62.3 | 39.5 | 19.7 | 40.2 |
|
| |||||||||||||
| AMERICA (Central and South) | 906,076 | 5.4 | 3.1 | 0.7 | 822,687 | 13.7 | 1.1 | 700,946 | 92.4 | 8.0 | 5.2 | 3.7 | |
|
| |||||||||||||
| Argentinian registries† | 2000–2014 | 75,167 | 1.7 | 1.5 | 0.5 | 72,366 | 10.8 | 0.6 | 64,151 | 96.5 | 5.7 | 0.0 | 2.3 |
| Brazilian registries | 2000–2014 | 191,344 | 18.5 | 3.9 | 0.5 | 147,622 | 8.0 | 0.9 | 134,597 | 90.0 | 10.6 | 22.9 | 0.3 |
| Chilean registries | 2000–2012 | 28,987 | 0.0 | 0.8 | 0.7 | 28,555 | 7.6 | 0.1 | 26,363 | 86.2 | 12.0 | 0.0 | 13.6 |
| Colombian registries | 2000–2014 | 63,402 | 3.1 | 1.5 | 1.2 | 59,740 | 5.0 | 0.9 | 56,245 | 89.9 | 11.3 | 0.0 | 21.0 |
| Costa Rica* | 2002–2014 | 72,900 | 0.0 | 4.1 | 1.4 | 68,900 | 8.4 | 0.8 | 62,536 | 90.1 | 13.0 | 0.0 | 0.0 |
| Cuba* | 2000–2012 | 193,196 | 0.0 | 0.0 | 0.2 | 192,755 | 32.3 | 2.5 | 125,696 | 91.8 | 5.1 | 2.6 | 0.0 |
| Ecuadorian registries | 2000–2014 | 71,798 | 7.7 | 8.2 | 0.8 | 59,892 | 9.8 | 1.6 | 53,043 | 92.0 | 9.9 | 0.3 | 2.7 |
| Guadeloupe* | 2008–2013 | 8,896 | 0.0 | 12.0 | 0.3 | 7,802 | 0.0 | 0.2 | 7,787 | 99.1 | 2.1 | 0.0 | 57.7 |
| Martinique* | 2000–2012 | 16,066 | 0.0 | 0.0 | 0.1 | 16,053 | 0.0 | 1.7 | 15,779 | 97.3 | 0.7 | 7.3 | 0.1 |
| Mexico (Childhood)† | 2008–2014 | 9,749 | 5.8 | 0.0 | 9.7 | 8,236 | 0.0 | 0.5 | 8,194 | 99.8 | 3.9 | 9.3 | 7.6 |
| Peru (Lima) | 2010–2012 | 19,078 | 0.1 | 0.0 | 0.7 | 18,929 | 8.9 | 0.1 | 17,226 | 93.9 | 2.9 | 0.0 | 10.2 |
| Puerto Rico* | 2000–2011 | 118,877 | 3.7 | 3.9 | 0.7 | 109,001 | 6.4 | 0.3 | 101,613 | 98.4 | 3.4 | 0.0 | 0.0 |
| Uruguay* | 2008–2012 | 36,616 | 0.0 | 9.6 | 0.7 | 32,836 | 15.5 | 0.1 | 27,716 | 85.0 | 15.9 | 0.0 | 0.0 |
|
| |||||||||||||
| AMERICA (North) | 15,925,870 | 0.7 | 6.8 | 0.7 | 14,622,183 | 1.8 | 0.3 | 14,320,034 | 97.7 | 3.0 | 1.4 | 0.0 | |
|
| |||||||||||||
| Canadian registries | 2000–2014 | 1,519,461 | 0.1 | 4.9 | 0.7 | 1,431,975 | 1.2 | 0.4 | 1,409,413 | 94.8 | 5.5 | 0.0 | 0.0 |
| US registries | 2000–2014 | 14,406,409 | 0.7 | 7.0 | 0.7 | 13,190,208 | 1.8 | 0.3 | 12,910,621 | 98.0 | 2.8 | 1.5 | 0.0 |
|
| |||||||||||||
| ASIA | 6,595,363 | 0.6 | 3.4 | 0.4 | 6,298,518 | 4.7 | 0.4 | 5,976,959 | 88.6 | 11.5 | 0.4 | 1.0 | |
|
| |||||||||||||
| Chinese registries | 2003–2013 | 610,729 | 0.8 | 0.2 | 0.2 | 603,861 | 1.4 | 0.1 | 594,533 | 66.2 | 41.8 | 3.2 | 0.1 |
| Cyprus* | 2004–2014 | 25,086 | 1.4 | 2.6 | 0.8 | 23,880 | 9.0 | 0.5 | 21,610 | 98.9 | 1.8 | 0.0 | 34.8 |
| Hong Kong* | 2005–2014 | 78,127 | 3.8 | 0.0 | 0.0 | 75,146 | 0.4 | 0.2 | 74,721 | 96.6 | 0.0 | 5.5 | 0.0 |
| Indian registries | 2000–2014 | 5,048 | 3.2 | 0.0 | 0.0 | 4,882 | 1.7 | 0.6 | 4,774 | 82.1 | 25.1 | 1.8 | 0.1 |
| Iran (Golestan) | 2006–2008 | 1,187 | 0.0 | 0.0 | 0.5 | 1,181 | 8.9 | 3.1 | 1,039 | 82.1 | 17.9 | 8.9 | 0.0 |
| Israel* | 2000–2013 | 282,191 | 0.0 | 7.3 | 2.2 | 255,359 | 4.8 | 0.4 | 241,881 | 96.8 | 4.2 | 0.0 | 0.0 |
| Japanese registries | 2000–2014 | 2,237,861 | 1.0 | 4.8 | 0.5 | 2,096,697 | 12.4 | 0.1 | 1,834,894 | 91.4 | 11.3 | 0.0 | 1.7 |
| Jordan* | 2000–2014 | 43,442 | 0.2 | 1.2 | 1.5 | 42,179 | 0.2 | 1.6 | 41,433 | 99.1 | 3.0 | 5.9 | 0.0 |
| Korea*‡ | 2000–2014 | 1,770,463 | 0.5 | 0.0 | 0.0 | 1,762,176 | 0.0 | 0.1 | 1,760,804 | 93.1 | 7.8 | 0.0 | 0.0 |
| Kuwait* | 2000–2013 | 8,931 | 0.0 | 1.4 | 1.1 | 8,710 | 2.3 | 0.3 | 8,484 | 99.8 | 0.4 | 1.2 | 0.0 |
| Malaysia (Penang) | 2000–2013 | 19,612 | 0.3 | 0.0 | 0.1 | 19,527 | 1.6 | 2.1 | 18,805 | 94.2 | 9.5 | 0.0 | 13.0 |
| Mongolia* | 2003–2014 | 1,025 | 0.0 | 1.1 | 0.0 | 1,014 | 0.3 | 1.2 | 999 | 77.0 | 4.1 | 7.6 | 0.0 |
| Qatar* | 2000–2014 | 7,940 | 0.0 | 1.0 | 1.0 | 7,778 | 1.0 | 0.7 | 7,642 | 95.4 | 6.3 | 0.0 | 51.0 |
| Singapore* | 2000–2014 | 122,461 | 0.0 | 7.0 | 1.9 | 111,495 | 1.1 | 0.3 | 109,992 | 91.7 | 1.9 | 0.0 | 0.0 |
| Taiwan* | 2000–2014 | 941,313 | 0.1 | 8.6 | 0.1 | 859,169 | 0.0 | 0.1 | 858,683 | 86.6 | 0.5 | 0.0 | 0.0 |
| Thai registries | 2000–2014 | 183,776 | 0.0 | 0.3 | 0.5 | 182,455 | 3.8 | 8.7 | 159,528 | 68.6 | 34.0 | 0.0 | 3.0 |
| Turkish registries | 2000–2013 | 256,171 | 1.5 | 2.7 | 0.9 | 243,009 | 1.9 | 0.5 | 237,137 | 94.7 | 7.9 | 0.2 | 3.8 |
|
| |||||||||||||
| EUROPE | 17,057,088 | 0.1 | 7.0 | 2.1 | 15,481,564 | 2.8 | 0.3 | 14,991,316 | 94.0 | 3.9 | 0.9 | 2.1 | |
|
| |||||||||||||
| Austria* | 2000–2014 | 486,379 | 0.0 | 7.4 | 1.2 | 444,735 | 6.1 | 1.1 | 412,683 | 98.0 | 4.9 | 0.0 | 0.0 |
| Belarus (Childhood)† | 2000–2014 | 1,740 | 0.0 | 0.0 | 0.0 | 1,740 | 0.6 | 2.5 | 1,687 | 97.9 | 2.5 | 1.5 | 0.0 |
| Belgium* | 2004–2014 | 616,737 | 0.0 | 11.4 | 0.2 | 545,373 | 0.0 | 0.2 | 544,110 | 98.4 | 2.0 | 1.1 | 0.0 |
| Bulgaria* | 2000–2014 | 299,563 | 0.0 | 0.0 | 0.1 | 299,333 | 8.5 | 0.0 | 273,868 | 89.2 | 1.4 | 0.1 | 0.0 |
| Croatia* | 2000–2014 | 246,883 | 0.0 | 3.5 | 0.2 | 237,793 | 6.2 | 0.1 | 222,776 | 82.9 | 0.5 | 0.0 | 0.0 |
| Czech Republic* | 2000–2014 | 640,594 | 0.0 | 7.5 | 1.6 | 582,748 | 1.3 | 0.4 | 572,368 | 90.3 | 1.5 | 0.0 | 0.0 |
| Denmark* | 2000–2014 | 366,310 | 0.0 | 0.0 | 0.2 | 365,525 | 0.0 | 0.1 | 365,105 | 96.3 | 6.8 | 0.2 | 0.0 |
| Estonia* | 2000–2012 | 64,038 | 0.0 | 1.8 | 0.7 | 62,396 | 3.9 | 0.2 | 59,848 | 89.2 | 2.0 | 0.3 | 0.0 |
| Finland* | 2000–2014 | 328,513 | 0.6 | 5.4 | 0.9 | 306,077 | 3.8 | 0.1 | 294,268 | 95.8 | 3.2 | 0.1 | 0.0 |
| French registries† | 2000–2012 | 466,020 | 0.2 | 0.0 | 0.3 | 463,588 | 0.0 | 0.6 | 460,927 | 96.1 | 0.6 | 1.8 | 0.1 |
| German registries | 2000–2014 | 1,925,070 | 0.4 | 4.5 | 1.0 | 1,811,465 | 10.3 | 0.2 | 1,621,312 | 97.5 | 0.7 | 0.3 | 17.7 |
| Gibraltar* | 2000–2010 | 732 | 13.0 | 11.7 | 1.1 | 543 | 0.2 | 1.7 | 533 | 99.6 | 0.8 | 0.0 | 41.7 |
| Greece (National Paediatric)† | 2000–2014 | 1,743 | 0.6 | 0.0 | 0.0 | 1,733 | 0.0 | 0.4 | 1,726 | 99.9 | 0.1 | 0.8 | 0.2 |
| Iceland* | 2000–2014 | 15,245 | 0.0 | 1.4 | 0.8 | 14,918 | 0.8 | 0.1 | 14,782 | 96.5 | 3.9 | 0.0 | 0.0 |
| Ireland* | 2000–2013 | 240,962 | 0.0 | 16.3 | 0.9 | 199,552 | 1.5 | 0.2 | 196,331 | 92.2 | 1.7 | 0.0 | 0.0 |
| Italian registries | 2000–2014 | 1,452,003 | 0.0 | 1.8 | 0.8 | 1,414,476 | 0.7 | 0.3 | 1,400,117 | 87.5 | 14.1 | 0.7 | 0.8 |
| Latvia* | 2000–2014 | 97,852 | 0.0 | 0.1 | 26.8 | 71,511 | 0.0 | 0.6 | 71,082 | 99.8 | 1.1 | 0.0 | 0.0 |
| Lithuania* | 2000–2012 | 154,857 | 0.0 | 4.1 | 1.1 | 146,896 | 4.9 | 0.2 | 139,475 | 87.6 | 1.5 | 0.0 | 0.3 |
| Malta* | 2000–2013 | 17,625 | 0.0 | 6.9 | 1.8 | 16,091 | 3.1 | 0.4 | 15,518 | 92.4 | 8.9 | 0.0 | 0.0 |
| Netherlands* | 2000–2014 | 1,047,456 | 0.0 | 3.8 | 1.2 | 994,826 | 0.2 | 0.6 | 987,029 | 96.2 | 4.0 | 0.5 | 0.0 |
| Norway* | 2000–2014 | 488,733 | 0.0 | 10.3 | 32.5 | 279,696 | 0.5 | 0.1 | 277,991 | 99.8 | 0.4 | 0.2 | 0.0 |
| Poland* | 2000–2014 | 1,389,978 | 0.0 | 0.1 | 0.3 | 1,383,780 | 2.5 | 0.3 | 1,344,837 | 91.4 | 1.3 | 0.0 | 0.0 |
| Portugal* | 2000–2014 | 408,523 | 0.7 | 2.7 | 1.5 | 388,199 | 0.1 | 0.2 | 386,853 | 96.7 | 2.7 | 1.7 | 0.0 |
| Romania (Cluj) | 2006–2012 | 17,740 | 0.0 | 3.1 | 1.7 | 16,894 | 16.6 | 0.2 | 14,060 | 90.1 | 10.7 | 0.0 | 0.0 |
| Russian registries‡ | 2000–2014 | 252,171 | 0.0 | 0.5 | 0.4 | 249,928 | 0.8 | 1.0 | 245,591 | 85.4 | 4.1 | 2.0 | 1.3 |
| Slovakia* | 2000–2010 | 180,029 | 0.0 | 4.1 | 1.3 | 170,269 | 8.2 | 0.1 | 156,122 | 94.0 | 6.7 | 0.0 | 0.0 |
| Slovenia* | 2000–2013 | 124,213 | 0.0 | 13.0 | 2.4 | 105,052 | 2.0 | 0.0 | 102,970 | 93.5 | 0.3 | 0.1 | 0.0 |
| Spanish registries | 2000–2014 | 417,865 | 0.3 | 6.8 | 0.9 | 384,586 | 1.9 | 0.2 | 376,759 | 91.7 | 2.2 | 0.5 | 0.5 |
| Sweden* | 2000–2014 | 676,693 | 0.0 | 15.4 | 3.0 | 551,717 | 1.1 | 0.2 | 544,531 | 98.6 | 2.2 | 0.2 | 0.0 |
| Swiss registries† | 2000–2014 | 241,610 | 0.0 | 7.9 | 2.5 | 216,439 | 1.2 | 0.5 | 212,695 | 95.9 | 2.4 | 4.6 | 3.9 |
| United Kingdom* | 2000–2014 | 4,389,211 | 0.1 | 13.0 | 1.4 | 3,753,685 | 1.8 | 0.3 | 3,673,362 | 94.9 | 4.5 | 1.9 | 0.0 |
|
| |||||||||||||
| OCEANIA | 1,691,153 | 0.3 | 9.7 | 0.7 | 1,510,866 | 1.6 | 0.2 | 1,483,573 | 96.5 | 3.6 | 0.0 | 0.0 | |
|
| |||||||||||||
| Australia* | 2000–2014 | 1,443,620 | 0.3 | 11.3 | 0.8 | 1,263,961 | 1.4 | 0.2 | 1,244,350 | 97.0 | 3.0 | 0.0 | 0.0 |
| New Zealand* | 2000–2014 | 247,533 | 0.0 | 0.0 | 0.3 | 246,905 | 2.9 | 0.2 | 239,223 | 94.3 | 6.3 | 0.0 | 0.0 |
|
| |||||||||||||
| Total | 42,222,177 | 0.5 | 6.4 | 1.2 | 38,777,265 | 2.9 | 0.3 | 37,513,025 | 94.6 | 4.9 | 1.0 | 1.1 | |
Data with 100% coverage of the national population.
Data with 100% coverage of the national population for childhood malignancies only.
Korea: Republic of Korea; Russia: Russian Federation.
Incomplete dates: records in which the year of birth is unknown; or the month and/or year of diagnosis is unknown; or the year of last known vital status is unknown. In situ malignancy (ICD-O-3 behaviour code 2): some registries do not register in situ cancers; other registries did not submit them. Other: records with incomplete data, or for tumours that are benign (behaviour code 0, except brain tumours), of uncertain behaviour (1), metastatic from another organ (6), or unknown if primary or metastatic (9); or for patients with age outside the range 0–14 years (children) or 15–99 years (adults); or other conditions (see text).
DCO: tumours registered from a death certificate only (DCO), or detected solely at autopsy. Sweden does not register DCOs; autopsy-detected cases were not submitted for CONCORD-2, but have been submitted for CONCORD-3. Other: vital status or sex unknown; invalid date or sequence of dates; inconsistency of sex-site, site-morphology, age-site, age-morphology, or age-site-morphology.
MV: microscopically verified. Non-specific morphology (solid tumours only): ICD-O-314,15 morphology code in the range 8000–8005. Censored: patients whose last known vital status is “alive” and who were censored within five years of diagnosis or, if diagnosed in 2010 or later, before 31 December 2014.
Table 4.
Population covered by participating registries (number of persons and % of national population) and number of patients diagnosed during 2000–2014 who were included in survival analyses, by continent and country
| Population covered¶ |
% of national |
Oesophagus | Stomach | Colon | Rectum | Liver | Pancreas | Lung | Melanoma of skin |
Breast (women) |
Cervix | Ovary | Prostate | Brain (adults) |
Brain (children) |
Myeloid (adults) |
Lymphoid (adults) |
ALL (children) |
Lymphoma (children) |
Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AFRICA | 10,533,762 | 3.4 | 3,057 | 1,731 | 2,172 | 1,487 | 869 | 379 | 2,734 | 368 | 15,117 | 5,017 | 1,010 | 2,726 | 592 | 179 | 425 | 2,042 | 64 | 228 | 40,197 |
|
| |||||||||||||||||||||
| Algerian registries | 2,447,075 | 6.3 | 104 | 1,129 | 1,331 | 827 | 244 | 272 | 1,852 | 248 | 5,196 | 885 | 423 | 764 | 392 | 109 | 290 | 1,376 | 45 | 115 | 15,602 |
| Mali (Bamako) | 764,245 | 9.0 | – | – | – | – | – | – | – | – | 60 | – | – | – | – | – | – | – | – | – | 60 |
| Mauritius* | 1,268,567 | 100.0 | 59 | 494 | 494 | 289 | 27 | 45 | 584 | 4 | 483 | 436 | 244 | 628 | 36 | 3 | 42 | 86 | – | 5 | 3,959 |
| Morocco (Casablanca) | 2,178,083 | 12.7 | – | – | – | – | – | – | – | – | 4,683 | – | – | – | – | – | – | – | – | – | 4,683 |
| Nigeria (Ibadan) | 2,797,220 | 1.6 | – | – | 230 | 266 | 333 | – | – | 69 | 3,962 | 1,578 | 225 | 833 | 148 | 45 | 76 | 412 | 12 | 85 | 8,274 |
| South Africa (Eastern Cape) | 1,078,572 | 2.0 | 2,894 | 108 | 117 | 105 | 265 | 62 | 298 | 47 | 733 | 2,118 | 118 | 501 | 16 | 22 | 17 | 168 | 7 | 23 | 7,619 |
|
| |||||||||||||||||||||
| AMERICA (Central and South) | 99,818,363 | 23.7 | 13,528 | 60,643 | 82,843 | 26,424 | 9,019 | 15,731 | 53,959 | 8,202 | 159,976 | 49,067 | 16,023 | 115,102 | 8,547 | 4,936 | 10,842 | 47,740 | 13,299 | 5,065 | 700,946 |
|
| |||||||||||||||||||||
| Argentinian registries | 3,973,922 | 9.2 | 1,152 | 2,686 | 6,076 | 1,959 | 968 | 1,657 | 5,195 | 1,084 | 15,282 | 2,467 | 1,688 | 7,115 | 1,217 | 2,662 | 1,588 | 4,281 | 5,119 | 1,955 | 64,151 |
| Brazilian registries | 15,882,624 | 7.7 | 6,678 | 15,567 | 21,984 | 10,354 | 858 | 5,520 | 4,884 | 1,424 | 49,811 | 3,083 | 1,201 | 7,556 | 1,011 | 168 | 852 | 3,270 | 233 | 143 | 134,597 |
| Chilean registries | 2,459,133 | 13.8 | 918 | 4,423 | 1,949 | 824 | 525 | 793 | 2,166 | 554 | 3,717 | 1,564 | 698 | 4,816 | 475 | 83 | 652 | 1,968 | 171 | 67 | 26,363 |
| Colombian registries | 4,277,369 | 9.0 | 642 | 7,988 | 3,874 | 1,990 | 1,129 | 1,303 | 3,965 | 1,373 | 9,609 | 5,124 | 1,759 | 8,722 | 1,601 | 243 | 1,476 | 5,004 | 306 | 137 | 56,245 |
| Costa Rica* | 4,757,606 | 100.0 | 528 | 8,577 | 5,438 | 1,926 | 1,239 | 1,188 | 2,688 | 1,432 | 12,019 | 7,466 | 1,408 | 11,345 | 1,067 | 153 | 857 | 4,646 | 456 | 103 | 62,536 |
| Cuba* | 11,379,111 | 100.0 | – | 6,664 | 15,047 | – | – | – | 19,344 | – | 33,313 | 16,396 | 4,560 | 21,358 | – | – | – | 8,451 | – | 563 | 125,696 |
| Ecuadorian registries | 6,398,546 | 40.2 | 486 | 7,210 | 3,203 | 1,622 | 1,502 | 1,069 | 2,641 | 1,080 | 8,283 | 5,453 | 1,732 | 7,939 | 1,481 | 324 | 1,489 | 6,330 | 859 | 340 | 53,043 |
| Guadeloupe* | 450,273 | 100.0 | 119 | 521 | 724 | 210 | 82 | 167 | 308 | 52 | 1,266 | 160 | 110 | 3,389 | 55 | 14 | 115 | 480 | 9 | 6 | 7,787 |
| Martinique* | 396,425 | 100.0 | 213 | 973 | 1,305 | 423 | 206 | 473 | 693 | 164 | 2,279 | 399 | 191 | 6,480 | 182 | 20 | 482 | 1,257 | 29 | 10 | 15,779 |
| Mexico (Childhood)† | 35,188,624 | 100.0 | – | – | – | – | – | – | – | – | – | – | – | – | – | 1,047 | – | – | 5,647 | 1,500 | 8,194 |
| Peru (Lima) | 7,548,697 | 24.4 | – | – | 2,803 | 992 | – | – | – | – | 5,590 | 2,917 | – | – | – | – | 891 | 3,653 | 268 | 112 | 17,226 |
| Puerto Rico* | 3,686,517 | 100.0 | 1,743 | 3,900 | 14,594 | 3,882 | 2,202 | 1,984 | 6,570 | 1,039 | 18,807 | 2,458 | 1,728 | 29,855 | 1,458 | 222 | 2,440 | 8,400 | 202 | 129 | 101,613 |
| Uruguay* | 3,419,516 | 100.0 | 1,049 | 2,134 | 5,846 | 2,242 | 308 | 1,577 | 5,505 | – | – | 1,580 | 948 | 6,527 | – | – | – | – | – | – | 27,716 |
|
| |||||||||||||||||||||
| AMERICA (North) | 301,237,785 | 84.8 | 195,255 | 283,566 | 1,471,548 | 461,707 | 246,966 | 462,187 | 2,564,507 | 678,206 | 2,587,798 | 163,517 | 312,954 | 2,703,952 | 251,888 | 27,157 | 508,562 | 1,356,829 | 29,995 | 13,440 | 14,320,034 |
|
| |||||||||||||||||||||
| Canadian registries | 27,213,277 | 76.5 | 18,788 | 33,889 | 166,760 | 60,958 | 20,858 | 41,908 | 236,434 | 65,235 | 237,321 | 16,054 | 31,395 | 256,736 | 28,186 | 2,196 | 49,474 | 139,370 | 2,712 | 1,139 | 1,409,413 |
| US registries | 274,024,508 | 85.8 | 176,467 | 249,677 | 1,304,788 | 400,749 | 226,108 | 420,279 | 2,328,073 | 612,971 | 2,350,477 | 147,463 | 281,559 | 2,447,216 | 223,702 | 24,961 | 459,088 | 1,217,459 | 27,283 | 12,301 | 12,910,621 |
|
| |||||||||||||||||||||
| ASIA | 227,771,765 | 7.2 | 206,254 | 971,935 | 703,081 | 361,987 | 617,479 | 205,345 | 950,362 | 31,314 | 726,968 | 161,620 | 109,998 | 397,673 | 73,306 | 8,513 | 140,066 | 293,307 | 11,371 | 6,380 | 5,976,959 |
|
| |||||||||||||||||||||
| Chinese registries | 31,755,347 | 2.3 | 72,714 | 92,578 | 35,001 | 31,498 | 74,295 | 19,110 | 133,932 | 1,449 | 53,791 | 13,131 | 10,517 | 12,380 | 11,341 | 526 | 12,171 | 19,388 | 498 | 213 | 594,533 |
| Cyprus* | 1,153,658 | 100.0 | 81 | 802 | 2,665 | 788 | 247 | 534 | 2,489 | 589 | 5,069 | 321 | 553 | 4,088 | 394 | 14 | 555 | 2,326 | 56 | 39 | 21,610 |
| Hong Kong* | 7,241,700 | 100.0 | – | – | 28,797 | 12,856 | – | – | – | – | 28,956 | 4,112 | – | – | – | – | – | – | – | – | 74,721 |
| Indian registries | 1,005,294 | 0.1 | 269 | 303 | 199 | 191 | 230 | 134 | 850 | 29 | 812 | 753 | 172 | 183 | 162 | 18 | 153 | 272 | 32 | 12 | 4,774 |
| Iran (Golestan) | 1,893,646 | 2.4 | 412 | 353 | 216 | 58 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1,039 |
| Israel* | 7,939,483 | 100.0 | 1,691 | 9,737 | 33,938 | 9,401 | 2,310 | 8,083 | 25,347 | 12,265 | 51,125 | 2,942 | 5,663 | 32,503 | 5,235 | 843 | 8,375 | 30,911 | 754 | 758 | 241,881 |
| Japanese registries | 51,445,407 | 40.6 | 63,631 | 381,457 | 247,682 | 102,776 | 122,792 | 79,636 | 276,444 | 4,018 | 184,372 | 30,606 | 31,244 | 168,505 | 15,007 | 1,293 | 37,845 | 85,640 | 1,438 | 508 | 1,834,894 |
| Jordan* | 7,416,083 | 100.0 | 352 | 1,955 | 5,116 | 1,775 | 606 | 952 | 4,282 | 214 | 11,584 | 579 | – | 2,457 | 1,483 | 489 | 1,917 | 6,511 | 681 | 480 | 41,433 |
| Korea*‡ | 50,074,400 | 100.0 | 30,627 | 396,213 | 187,078 | 121,053 | 214,821 | 59,357 | 257,345 | 5,771 | 179,520 | 58,663 | 28,076 | 83,892 | 17,701 | 2,333 | 42,322 | 70,594 | 3,389 | 2,049 | 1,760,804 |
| Kuwait* | 3,753,121 | 100.0 | 90 | 207 | 908 | 330 | 261 | 240 | 559 | 18 | 2,568 | 163 | 221 | 509 | 230 | 49 | 346 | 1,405 | 251 | 129 | 8,484 |
| Malaysia (Penang) | 1,543,500 | 5.2 | 290 | 1,061 | 2,285 | 1,126 | 927 | 539 | 2,863 | – | 4,606 | 1,046 | 805 | 915 | 289 | 84 | 504 | 1,244 | 156 | 65 | 18,805 |
| Mongolia* | 1,468,823 | 100.0 | – | – | – | – | – | – | – | – | 999 | – | – | – | – | – | – | – | – | – | 999 |
| Qatar* | 2,172,065 | 100.0 | 98 | 361 | 784 | 283 | 438 | 186 | 587 | 55 | 1,861 | 196 | 214 | 586 | 287 | 33 | 489 | 1,042 | 71 | 71 | 7,642 |
| Singapore* | 3,870,700 | 100.0 | 1,434 | 6,822 | 17,225 | 6,241 | 7,101 | 3,481 | 17,921 | 367 | 22,473 | 2,943 | 3,514 | 7,991 | 1,202 | 196 | 3,339 | 7,187 | 388 | 167 | 109,992 |
| Taiwan* | 23,123,866 | 100.0 | 27,680 | 54,983 | 108,844 | 57,163 | 158,157 | 22,283 | 141,108 | 2,988 | 116,929 | 29,214 | 16,872 | 52,681 | 8,410 | 1,211 | 17,813 | 39,704 | 1,811 | 832 | 858,683 |
| Thai registries | 13,738,188 | 20.3 | 3,344 | 5,321 | 13,801 | 6,679 | 30,814 | 3,284 | 28,865 | 695 | 25,001 | 12,737 | 5,469 | 5,869 | 2,779 | 385 | 5,177 | 8,486 | 605 | 217 | 159,528 |
| Turkish registries | 18,176,484 | 23.4 | 3,541 | 19,782 | 18,542 | 9,769 | 4,480 | 7,526 | 57,770 | 2,856 | 37,302 | 4,214 | 6,678 | 25,114 | 8,786 | 1,039 | 9,060 | 18,597 | 1,241 | 840 | 237,137 |
|
| |||||||||||||||||||||
| EUROPE | 321,767,598 | 50.1 | 294,606 | 668,096 | 1,764,170 | 801,387 | 283,720 | 506,723 | 2,317,434 | 647,507 | 2,700,348 | 267,986 | 399,675 | 2,355,249 | 297,032 | 24,316 | 436,684 | 1,182,009 | 29,544 | 14,830 | 14,991,316 |
|
| |||||||||||||||||||||
| Austria* | 8,516,916 | 100.0 | 5,324 | 19,308 | 46,127 | 23,360 | 10,570 | 18,371 | 56,130 | 19,150 | 74,818 | 6,455 | 11,567 | 75,082 | 7,615 | – | 7,223 | 31,583 | – | – | 412,683 |
| Belarus (Childhood)† | 1,498,163 | 100.0 | – | – | – | – | – | – | – | – | – | – | – | – | – | 580 | – | – | 740 | 367 | 1,687 |
| Belgium* | 11,226,322 | 100.0 | 10,191 | 15,222 | 63,540 | 27,614 | 7,026 | 15,015 | 83,551 | 21,905 | 111,685 | 6,929 | 10,447 | 97,316 | 9,057 | 781 | 19,790 | 42,772 | 720 | 549 | 544,110 |
| Bulgaria* | 7,201,308 | 100.0 | – | 21,404 | 37,854 | 22,511 | 5,704 | – | 50,210 | 5,875 | 53,605 | 16,329 | 12,206 | 26,190 | – | – | 6,226 | 14,919 | 537 | 298 | 273,868 |
| Croatia* | 4,255,853 | 100.0 | 3,007 | 14,589 | 27,382 | 15,309 | 5,456 | 8,596 | 41,744 | 7,848 | 35,323 | 5,279 | 7,138 | 22,066 | 7,515 | 403 | 5,026 | 15,421 | 443 | 231 | 222,776 |
| Czech Republic* | 10,542,666 | 100.0 | 7,764 | 24,157 | 83,481 | 34,838 | 12,056 | 27,622 | 93,241 | 27,800 | 89,989 | 14,950 | 18,875 | 78,581 | 11,007 | 489 | 9,734 | 36,974 | 531 | 279 | 572,368 |
| Denmark* | 5,646,899 | 100.0 | 6,556 | 8,022 | 40,495 | 22,384 | 4,708 | 13,279 | 62,402 | 24,630 | 65,840 | 5,755 | 9,024 | 55,052 | 8,951 | 493 | 8,951 | 27,756 | 574 | 233 | 365,105 |
| Estonia* | 1,316,203 | 100.0 | 786 | 5,212 | 6,523 | 3,062 | 903 | 2,698 | 9,201 | 1,983 | 8,149 | 2,232 | 2,122 | 9,734 | 1,295 | 103 | 1,512 | 4,193 | 93 | 47 | 59,848 |
| Finland* | 5,479,660 | 100.0 | 3,686 | 9,871 | 25,374 | 12,847 | 5,096 | 12,851 | 31,950 | 14,949 | 62,282 | 2,318 | 8,101 | 66,706 | 5,953 | 503 | 5,573 | 25,395 | 572 | 241 | 294,268 |
| French registries | 13,891,552 | 21.7 | 9,958 | 13,770 | 53,149 | 20,018 | 14,818 | 15,328 | 51,989 | 13,677 | 82,538 | 5,125 | 8,658 | 91,806 | 7,532 | 4,477 | 18,897 | 41,784 | 4,830 | 2,573 | 460,927 |
| German registries | 29,655,933 | 36.8 | 27,208 | 75,378 | 191,396 | 99,791 | 28,301 | 57,498 | 212,897 | 78,713 | 300,626 | 24,302 | 38,064 | 284,771 | 27,683 | 691 | 45,934 | 126,594 | 1,019 | 446 | 1,621,312 |
| Gibraltar* | 31,997 | 100.0 | 12 | 29 | 81 | 21 | 5 | 13 | 63 | 31 | 169 | 10 | 14 | 62 | 11 | – | 4 | 8 | – | – | 533 |
| Greece (National Paediatric)† | 1,610,335 | 100.0 | – | – | – | – | – | – | – | – | – | – | – | – | – | 237 | – | – | 1,092 | 397 | 1,726 |
| Iceland* | 327,318 | 100.0 | 271 | 473 | 1,433 | 580 | 165 | 481 | 2,314 | 713 | 2,743 | 225 | 276 | 3,083 | 348 | 35 | 433 | 1,167 | 31 | 11 | 14,782 |
| Ireland* | 4,675,164 | 100.0 | 4,899 | 6,801 | 21,724 | 9,085 | 2,178 | 5,931 | 26,838 | 9,470 | 34,632 | 3,573 | 4,952 | 37,536 | 4,605 | 396 | 6,250 | 16,806 | 461 | 194 | 196,331 |
| Italian registries | 34,881,955 | 58.3 | 12,219 | 80,686 | 188,983 | 53,226 | 63,084 | 56,698 | 203,548 | 46,607 | 250,204 | 13,394 | 31,025 | 196,256 | 28,325 | 1,613 | 49,653 | 121,301 | 2,022 | 1,273 | 1,400,117 |
| Latvia* | 1,989,354 | 100.0 | 1,294 | 6,878 | 7,658 | 4,748 | 464 | 1,072 | 9,691 | 2,503 | 13,020 | 3,148 | 3,842 | 10,674 | 1,415 | 100 | 1,749 | 2,679 | 147 | – | 71,082 |
| Lithuania* | 2,916,798 | 100.0 | 2,130 | 11,840 | 11,148 | 7,694 | 1,776 | 5,421 | 18,499 | 3,317 | 17,699 | 6,318 | 5,452 | 30,156 | 2,942 | 136 | 4,850 | 9,741 | 250 | 106 | 139,475 |
| Malta* | 417,723 | 100.0 | 184 | 656 | 1,908 | 781 | 152 | 709 | 2,043 | 541 | 3,523 | 136 | 547 | 2,069 | 315 | 24 | 492 | 1,383 | 35 | 20 | 15,518 |
| Netherlands* | 16,868,020 | 100.0 | 25,342 | 29,585 | 126,237 | 51,839 | 6,397 | 28,717 | 159,895 | 59,088 | 198,074 | 10,317 | 19,252 | 142,578 | 17,261 | 1,428 | 30,256 | 78,420 | 1,588 | 755 | 987,029 |
| Norway* | 5,147,970 | 100.0 | 3,021 | 7,548 | 36,646 | 16,306 | 1,916 | 6,671 | 33,558 | 19,994 | 43,349 | 4,458 | 7,207 | 57,657 | 5,647 | 484 | 8,374 | 24,389 | 511 | 255 | 277,991 |
| Poland* | 38,483,957 | 100.0 | 18,959 | 79,466 | 140,075 | 83,669 | 20,764 | 47,635 | 306,136 | 35,834 | 220,036 | 48,857 | 53,462 | 131,099 | 37,794 | 2,071 | 21,008 | 94,159 | 2,505 | 1,308 | 1,344,837 |
| Portugal* | 10,566,132 | 100.0 | 6,122 | 33,865 | 57,219 | 25,989 | 5,107 | 8,303 | 40,422 | 9,358 | 69,599 | 9,013 | 6,532 | 64,886 | 7,348 | 549 | 9,414 | 32,024 | 627 | 476 | 386,853 |
| Romania (Cluj) | 983,525 | 5.0 | 216 | 1,201 | 1,552 | 657 | 547 | 563 | 2,126 | 436 | 2,205 | 1,004 | 460 | 1,301 | 291 | 19 | 482 | 969 | 21 | 10 | 14,060 |
| Russian registries‡ | 8,081,400 | 5.6 | 6,000 | 31,711 | 28,946 | 16,305 | 3,757 | 10,048 | 42,434 | 4,914 | 41,903 | 10,897 | 10,628 | 20,346 | 4,449 | 327 | 3,190 | 9,209 | 320 | 207 | 245,591 |
| Slovakia* | 5,422,861 | 100.0 | 2,794 | 9,604 | 23,694 | 11,066 | 2,741 | 6,624 | 22,971 | 6,389 | 23,698 | 6,170 | 5,207 | 14,376 | 3,695 | 323 | 4,466 | 11,821 | 304 | 179 | 156,122 |
| Slovenia* | 2,066,068 | 100.0 | 1,202 | 6,443 | 12,376 | 6,682 | 1,964 | 4,073 | 16,051 | 5,603 | 15,822 | 2,281 | 2,750 | 14,932 | 1,943 | 114 | 3,026 | 7,498 | 122 | 88 | 102,970 |
| Spanish registries | 9,396,745 | 20.3 | 5,637 | 17,844 | 54,250 | 18,245 | 11,848 | 12,438 | 54,237 | 11,028 | 56,759 | 5,023 | 7,710 | 63,237 | 8,685 | 1,521 | 13,483 | 31,782 | 1,917 | 1,115 | 376,759 |
| Sweden* | 9,703,247 | 100.0 | 6,233 | 13,463 | 55,664 | 29,777 | 7,242 | 14,240 | 51,122 | 36,921 | 102,483 | 6,816 | 12,132 | 139,051 | 9,327 | 761 | 14,280 | 43,784 | 926 | 309 | 544,531 |
| Swiss registries | 4,368,854 | 53.2 | 3,583 | 6,135 | 21,137 | 8,633 | 5,070 | 7,694 | 27,116 | 14,893 | 39,262 | 1,858 | 4,964 | 40,528 | 4,102 | 565 | 7,175 | 18,923 | 733 | 324 | 212,695 |
| United Kingdom* | 64,596,700 | 100.0 | 120,008 | 116,935 | 398,118 | 174,350 | 53,905 | 118,134 | 605,055 | 163,337 | 680,313 | 44,814 | 97,061 | 578,118 | 71,921 | 5,093 | 129,233 | 308,555 | 5,873 | 2,539 | 3,673,362 |
|
| |||||||||||||||||||||
| OCEANIA | 27,952,971 | 100.0 | 21,728 | 33,411 | 174,823 | 67,496 | 20,311 | 39,014 | 162,266 | 187,512 | 232,346 | 13,537 | 25,841 | 290,176 | 25,294 | 1,713 | 54,647 | 129,127 | 3,078 | 1,253 | 1,483,573 |
|
| |||||||||||||||||||||
| Australia* | 23,457,489 | 100.0 | 17,877 | 27,952 | 144,382 | 56,260 | 17,281 | 33,319 | 136,318 | 156,302 | 193,134 | 11,065 | 21,124 | 247,000 | 21,569 | 1,484 | 46,955 | 108,727 | 2,565 | 1,036 | 1,244,350 |
| New Zealand* | 4,495,482 | 100.0 | 3,851 | 5,459 | 30,441 | 11,236 | 3,030 | 5,695 | 25,948 | 31,210 | 39,212 | 2,472 | 4,717 | 43,176 | 3,725 | 229 | 7,692 | 20,400 | 513 | 217 | 239,223 |
|
| |||||||||||||||||||||
| Total | 989,082,244 | 20.2 | 734,428 | 2,019,382 | 4,198,637 | 1,720,488 | 1,178,364 | 1,229,379 | 6,051,262 | 1,553,109 | 6,422,553 | 660,744 | 865,501 | 5,864,878 | 656,659 | 66,814 | 1,151,226 | 3,011,054 | 87,351 | 41,196 | 37,513,025 |
Populations in 2014 or nearest available year (see text).
Data with 100% coverage of the national population.
Data with 100% coverage of the national population for childhood malignancies only.
Korea: Republic of Korea; Russia: Russian Federation.
Populations for 2014 are from the UN Population Division,27 or national authorities in Australia, Guadeloupe, Hong Kong, Poland, Portugal and Taiwan (2010). Sub-national populations were provided by the registry concerned. Belarus, Greece and Mexico only provided data for childhood cancers: national populations shown are for children (0–14 years). Mali, Mongolia and Morocco only provided cancer data for women: national populations shown are for women. Population shown for France excludes Guadeloupe and Martinique.
Coverage is now national in Australia, and contributions from additional registries increased the population coverage in another 14 of the 25 countries that participated in CONCORD-2 with sub-national coverage: Africa: Algeria (from 1.6% to 6.0%); Central and South America: Brazil (5.7%, 7.7%), Chile (5.5%, 13.8%), Colombia (6.9%, 9.0%), Ecuador (33.8%, 40.2%); North America: the USA (83.2%, 85.8%); Asia: Japan (29.2%, 40.6%), Thailand (5.9%, 20.3%), Turkey (5.4%, 23.4%); Europe: France (18.4%, 21.7%), Italy (38.6%, 58.3%), Romania (3.1%, 5.0%), Russia (0.9%, 5.6%), Switzerland (47.4%, 54.7%); Oceania: Australia (90.8%, 100%). International coverage has been reduced by the loss of data from Indonesia (Jakarta) and from four countries in Africa: Gambia, Lesotho, Libya and Tunisia.
Three of the Polish registries that participated in CONCORD-2 now use a different or anglicised name, changing the alphabetical order in web-tables: Holy Cross (formerly Kielce), Lower Silesia (Wrocław) and Subcarpathia (Podkarpackie). All 16 voivodships of Poland are now included.
Four registries submitted data with wider territorial coverage than before. The Burgundy (Digestive) registry in France submitted data for both the Saône-et-Loire and the Côte-d’Or départements; the Biella registry (Italy) now covers the Provincia di Vercelli as well as Biella; the Milano (Italy) registry now covers Provincia di Milano and Lodi as well as the city of Milan, and the Cluj (Romania) registry expanded coverage from Cluj county to include Bistrița-Năsăud county.
We received more than 4,700 data sets.
We examined individual cancer registrations for 42,218,671 patients diagnosed with an index cancer during the period 2000–2014 (Table 3). Of these, 2,701,998 (6.4%) were for an in situ cancer, mostly of the cervix (54.6% of 1,708,084 women), breast (10.6% of 7,377,462 women), colon (4.4% of 4,619,536 adults) or prostate (0.6% of 6,069,630 men) (web-table 2). The proportions of in situ cancer are not directly comparable between countries, because some registries still do not record in situ malignancies, while others did not submit data for cancers where in situ malignancy is common. The variation between continents is still of interest: for cervical cancer, it ranged from 2.3% in African registries to 24% in Central and South American registries, 37.4% in Asian registries and 82% in Oceania; US registries did not submit data for in situ cervical cancers, and only three Canadian provinces did so. The proportion of in situ breast cancers varied from 0.3% in African registries to 4–6% in Asia, Europe and Oceania and 17% in North America.
Patients with in situ cancer were not included in survival analyses. We excluded a further 506,625 (1.7%) patients because the year of birth, the month or year of diagnosis, or the year of last vital status was unknown, or because the tumour was not a primary, invasive malignancy (behaviour code 3), or the morphology was that of Kaposi sarcoma or lymphoma in a solid organ, or for other reasons (Table 3). The proportion of records excluded for these reasons is shown for each cancer and each cancer registry in web-table 2.
Of the 38,771,959 patients otherwise eligible for inclusion in survival analyses, the records for 1,124,388 (2.9%) were excluded because the cancer was registered only from a death certificate or discovered at autopsy (Table 3), and 116,316 (0.3%) for other reasons. These included definite errors (unknown vital status, unknown sex, sex-site error, invalid date(s) or sequence of dates) and possible errors, such as apparent inconsistencies between age, cancer site and morphology (details on request). For example, we excluded hepatoblastomas in children older than 6 years, and multiple myeloma in persons aged less than 20 years, unless the record was confirmed as correct by the registry concerned.
Among the 37,507,799 patients available for survival analyses for all cancers combined (97% of those eligible for inclusion), pathological evidence of malignancy (histology, cytology or haematology) was available for 35,482,420 (94.6%) (Table 3). This proportion ranged from 88.6% in Asia, 90.1% in Africa and 92.4% in Central and South America, up to 94–98% in Europe, Oceania and North America. Continental variation was much wider for some cancers (web-table 2).
Countries marked in the text with an asterisk are those for which survival estimates are based on data with national population coverage (100%). Survival estimates that are considered less reliable are flagged (§) in tables and graphics. These are data sets in which 15% or more of patients were lost to follow-up or censored alive within five years of diagnosis. For patients diagnosed in 2010 or later, this criterion was applied for patients censored alive before 31 December 2014, the study closure date. Estimates are also flagged as less reliable if 15% or more of patients were registered only from a death certificate or at autopsy and excluded from analysis, since their survival is unknown. Finally, estimates are also flagged if 15% or more of patients were excluded from analysis because one or more dates was incomplete: unknown year of birth, unknown month or year of diagnosis, or unknown year of last vital status.
In what follows, we present results in a similar structure for each group of cancers. Where possible, we also present graphics of national trends in cancer survival over the 20-year period 1995–2014. Estimates for patients diagnosed during 1995–99 are for countries that provided data for one of the 10 cancers included in CONCORD-2.6
Gastrointestinal cancers
Oesophagus
Results are available for 734,428 adults from 290 registries in 60 countries (Tables 2 and 4).
In 2010–2014, 5-year age-standardised net survival was in the range 10–30% in most countries, with a much wider range in Asia (web-figure 4). Most survival estimates were considered reliable (Table 5, web-table 4).
Table 5.
Five-year age-standardised net survival (NS, %): adults (15–99 years) diagnosed with one of 15 common malignancies and children (0–14 years) diagnosed with one of 3 common malignancies by calendar period of diagnosis (2000–2004, 2005–2009, 2010–2014)
| Period of diagnosis |
Oesophagus
|
Stomach
|
Colon
|
Rectum
|
Liver
|
Pancreas
|
Lung
|
Melanoma of the skin
|
Breast
|
Cervix
|
Ovary
|
Prostate
|
Brain (adults)
|
Brain (children)
|
Myeloid (adults)
|
Lymphoid (adults)
|
ALL (children)
|
Lymphoma (children)
|
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | NS (%) | 95% CI | ||
|
AFRICA
| |||||||||||||||||||||||||||||||||||||
| Algeria (3 registries) |
2000–2004 | – | 20.7§ | 14.3 – 27.1 | 88.1§ | 80.1 – 96.0 | 63.4§ | 48.3 – 78.5 | 6.2§ | 0.0 – 13.7 | 8.3§ | 0.0 – 20.3 | 18.0§ | 14.0 – 22.0 | 6.9§ | 0.0 – 18.5 | 38.9§ | 29.1 – 48.7 | 61.1§ | 55.5 – 66.7 | 50.7§ | 35.6 – 65.8 | 89.9§ | 77.8 – 100.0 | – | – | 21.1§ | 6.0 – 36.2 | 23.3§ | 13.8 – 32.8 | 30.9§ | 10.1 – 51.6 | 6.0§ | 0.0 – 15.1 | |||
| 2005–2009 | 554§ | 36.4 – 74.5 | 42.4§ | 36.4 – 48.4 | 76.7§ | 69.6 – 83.9 | 64.5§ | 56.4 – 72.7 | 13.9§ | 8.6 – 19.2 | 30.2§ | 21.3 – 39.2 | 30.2§ | 25.7 – 34.8 | 63.4§ | 59.4 – 67.3 | 55.6§ | 47.4 – 63.8 | 70.7§ | 64.5 – 77.0 | 54.3§ | 44.7 – 63.8 | 50.3§ | 41.0 – 59.6 | 51.9§ | 43.4 – 60.4 | 43.3§ | 29.4 – 57.2 | 17.1§ | 0.1 – 34.1 | 47.8§ | 39.9 – 55.8 | 100.0§ | 100.0 – 100.0 | 78.9§ | 62.5 – 95.3 | |
| 2010–2014 | 37.3§ | 23.4 – 51.1 | 41.6§ | 35.5 – 47.7 | 74.2§ | 65.7 – 82.7 | 67.3§ | 58.0 – 76.5 | 13.5§ | 6.9 – 20.1 | 29.8§ | 18.7 – 40.9 | 33.7§ | 28.5 – 38.9 | 54.9§ | 47.3 – 62.6 | 77.0§ | 68.5 – 85.6 | 72.4§ | 66.0 – 78.7 | 66.5§ | 53.5 – 79.5 | 64.1§ | 56.6 – 71.6 | 46.5§ | 37.5 – 55.5 | 54.1§ | 39.2 – 69.0 | 17.9§ | 5.3 – 30.6 | 59.1§ | 49.9 – 68.3 | – | 77.5§ | 65.4 – 89.7 | ||
|
| |||||||||||||||||||||||||||||||||||||
| Mali (Bamako) | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |||||||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | 0.0§ | 0.0 – 0.0 | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Mauritius* | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | 44.3 | 36.8 – 51.7 | 65.9 | 56.7 – 75.1 | 83.6§ | 75.0 – 92.1 | – | – | 31.7 | 25.9 – 37.6 | – | 83.6 | 75.9 – 91.3 | 80.8 | 76.0 – 85.6 | 79.7 | 69.6 – 89.8 | 61.8 | 54.1 – 69.4 | – | – | – | – | – | – | |||||||||||
| 2010–2014 | 28.1 | 14.6 – 41.5 | 25.7 | 18.0 – 33.3 | 57.9 | 48.5 – 67.2 | 72.9§ | 62.7 – 83.0 | 17.0 | 2.6 – 31.3 | 24.5 | 11.4 – 37.6 | 20.4 | 13.2 – 27.7 | – | – | – | – | 63.5 | 54.7 – 72.4 | 43.7 | 25.5 – 61.9 | – | 50.1 | 34.4 – 65.8 | 65.9 | 53.4 – 78.4 | – | – | ||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Morocco (Casablanca) | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | 86.7§ | 71.7 – 100.0 | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | 99.7§ | 95.8 – 100.0 | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Nigeria (Ibadan) | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | 41.2§ | 16.9 – 65.6 | 25.9§ | 0.0 – 53.7 | – | – | – | 100.0§ | 100.0 – 100.0 | 98.8§ | 95.6 – 100.0 | 58.6§ | 46.5 – 70.7 | 59.4§ | 24.9 – 93.9 | 73.9§ | 50.2 – 97.6 | 88.6§ | 60.4 – 100.0 | – | 57.4§ | 29.0 – 85.8 | 86.8§ | 54.9 – 100.0 | – | 51.0§ | 31.5 – 70.6 | ||||||||
| 2010–2014 | – | – | 17.4§ | 0.1 – 34.8 | 16.9§ | 0.0 – 37.8 | – | – | – | 97.7§ | 74.6 – 100.0 | 97.5§ | 89.9 – 100.0 | 49.8§ | 36.5 – 63.1 | 49.1§ | 33.8 – 64.4 | 58.7§ | 40.1 – 77.2 | 54.9§ | 19.7 – 90.0 | – | 28.4§ | 3.0 – 53.7 | 56.4§ | 32.2 – 80.5 | – | 6.0§ | 0.0 – 13.6 | ||||||||
|
| |||||||||||||||||||||||||||||||||||||
| South Africa (Eastern Cape) | 2000–2004 | 12.1§ | 0.0 – 27.0 | – | – | – | 27.1§ | 0.0 – 57.1 | – | – | – | 53.0§ | 23.4 – 82.7 | 70.7§ | 56.7 – 84.7 | 82.5§ | 42.5 – 100.0 | 77.6§ | 55.0 – 100.0 | – | – | – | – | – | – | ||||||||||||
| 2005–2009 | 19.2§ | 12.0 – 26.4 | 25.0§ | 6.1 – 44.0 | 31.9§ | 10.7 – 53.1 | 19.9§ | 0.0 – 46.4 | – | – | 16.7§ | 0.8 – 32.5 | – | 32.0§ | 23.3 – 40.7 | 40.2§ | 32.2 – 48.1 | 81.0§ | 58.8 – 100.0 | 38.6§ | 25.1 – 52.0 | – | – | – | 29.5§ | 10.8 – 48.2 | – | – | |||||||||
| 2010–2014 | 18.0§ | 12.6 – 23.4 | 25.6§ | 7.2 – 43.9 | 12.3§ | 4.3 – 20.2 | 9.1§ | 0.0 – 21.5 | 0.0§ | 0.0 – 0.0 | 21.8§ | 0.0 – 49.5 | 15.0§ | 6.1 – 24.0 | 16.7§ | 0.0 – 41.0 | 40.1§ | 30.7 – 49.6 | 37.1§ | 31.4 – 42.9 | 67.8§ | 47.4 – 88.2 | 37.8§ | 25.5 – 50.1 | 51.6§ | 0.6 – 100.0 | – | – | 47.7§ | 31.1 – 64.4 | – | – | |||||
|
AMERICA (CENTRAL AND SOUTH) | |||||||||||||||||||||||||||||||||||||
| Argentina† | 2000–2004 | 18.7§ | 12.7 – 24.8 | 21.7§ | 17.1 – 26.2 | 54.2§ | 49.7 – 58.7 | 48.9 | 41.5 – 56.3 | 14.1§ | 6.0 – 22.1 | 9.6§ | 5.5 – 13.6 | 19.5§ | 15.5 – 23.5 | 68.4 | 60.6 – 76.3 | 82.3 | 79.4 – 85.2 | 58.3 | 52.6 – 64.0 | 40.4 | 32.4 – 48.4 | 83.5 | 78.5 – 88.6 | 29.8§ | 22.6 – 37.0 | 45.1 | 41.8 – 48.3 | 47.9 | 39.4 – 56.3 | 54.5 | 49.1 – 59.8 | 65.0 | 62.7 – 67.3 | 79.9 | 76.7 – 83.0 |
| (5 registries) | 2005–2009 | 15.0§ | 11.4 –18.6 | 19.3§ | 16.9 – 21.7 | 51.2§ | 49.0 – 53.5 | 47.5 | 43.3 – 51.7 | 11.4§ | 8.2 – 14.5 | 8.3§ | 6.0 – 10.7 | 12.4§ | 10.9 – 14.0 | 68.1 | 63.4 – 72.9 | 82.0 | 80.4 – 83.6 | 55.6 | 52.0 – 59.1 | 43.2 | 38.6 – 47.9 | 83.6 | 81.2 – 86.0 | 27.7§ | 24.4 – 31.0 | 56.1 | 52.9 – 59.3 | 39.5 | 34.5 – 44.6 | 48.8 | 45.9 – 51.6 | 72.0 | 69.7 – 74.2 | 76.9 | 73.5 – 80.3 |
| 2010–2014 | 16.4§ | 11.9 – 21.0 | 21.5§ | 18.5 – 24.4 | 54.4§ | 51.8 – 57.1 | 49.9 | 45.3 – 54.4 | 12.6§ | 8.7 – 16.6 | 11.4§ | 8.1 – 14.6 | 13.1§ | 11.2 – 15.1 | 71.0 | 65.6 – 76.4 | 84.4 | 82.6 – 86.2 | 52.7 | 48.7 – 56.7 | 38.6 | 34.3 – 42.9 | 87.6 | 84.9 – 90.4 | 30.7§ | 26.8 – 34.6 | 62.9§ | 59.4 – 66.4 | 37.4 | 32.1 – 42.6 | 48.2 | 45.0 – 51.5 | 76.1§ | 73.7 – 78.4 | 83.4 | 80.1 – 86.6 | |
|
| |||||||||||||||||||||||||||||||||||||
| Brazil | 2000–2004 | 10.7§ | 9.0 – 12.4 | 19.1§ | 17.9 – 20.3 | 44.5§ | 42.9 – 46.0 | 37.7§ | 35.7 – 39.6 | 15.4§ | 10.4 – 20.5 | 3.9§ | 3.0 – 4.9 | 10.7 | 8.3 – 13.1 | 76.7 | 71.5 – 81.8 | 68.7§ | 67.5 – 69.8 | 69.3 | 66.1 – 72.6 | 42.1 | 36.0 – 48.1 | 90.0 | 87.2 – 92.8 | 31.3§ | 26.2 – 36.4 | 55.7 | 44.7 – 66.6 | 31.1 | 7.3 – 54.9 | 48.2 | 43.7 – 52.6 | 67.7 | 57.8 – 77.6 | 69.2 | 57.3 – 81.1 |
| (6 registries) | 2005–2009 | 12.5§ | 10.6 – 14.5 | 24.7§ | 23.2 – 26.2 | 50.6§ | 49.3 – 52.0 | 45.7§ | 43.7 – 47.8 | 9.6§ | 6.5 – 12.8 | 9.1§ | 7.3 – 10.9 | 7.8 | 5.8 – 9.8 | 75.9 | 71.7 – 80.1 | 76.9§ | 75.7 – 78.0 | 63.2 | 59.9 – 66.5 | 34.1 | 29.4 – 38.9 | 92.5 | 90.2 – 94.8 | 28.2§ | 24.4 – 32.1 | 34.7 | 21.9 – 47.5 | 41.6 | 31.4 – 51.8 | 49.4 | 45.6 – 53.2 | 69.8 | 60.0 – 79.6 | 86.3 | 77.1 – 95.5 |
| 2010–2014 | 9.7§ | 7.9 – 11.4 | 20.6§ | 18.9 – 22.2 | 48.3§ | 46.7 – 49.9 | 42.4§ | 40.1 – 44.6 | 11.2§ | 7.6 – 14.7 | 9.5§ | 7.4 – 11.5 | 8.5 | 5.3 – 11.6 | 70.0 | 65.4 – 74.7 | 75.2§ | 73.9 – 76.5 | 60.3 | 56.3 – 64.3 | 34.9 | 29.5 – 40.3 | 91.6 | 89.1 – 94.1 | 28.1§ | 23.7 – 32.6 | 28.9 | 15.8 – 41.9 | 39.1 | 28.7 – 49.5 | 46.2 | 42.2 – 50.2 | 66.0 | 53.3 – 78.8 | 88.2 | 78.2 – 98.3 | |
|
| |||||||||||||||||||||||||||||||||||||
| Chile | 2000–2004 | 7.0 | 3.1 – 10.9 | 14.5 | 11.7 – 17.4 | 35.5 | 28.6 – 42.3 | 35.9 | 26.3 – 45.5 | 3.6§ | 0.0 – 7.4 | 2.2 | 0.2 – 4.2 | 7.1§ | 4.4 – 9.8 | 57.4 | 46.6 – 68.1 | 74.6 | 68.2 – 81.1 | 58.2 | 52.3 – 64.0 | 25.8 | 18.5 – 33.1 | 82.6 | 77.2 – 88.0 | 12.4 | 0.0 – 26.7 | 46.7 | 22.7 – 70.7 | 29.1 | 19.1 – 39.1 | 28.9 | 23.4 – 34.3 | 76.7 | 65.6 – 87.7 | 70.1 | 43.3 – 96.9 |
| (4 registries) | 2005–2009 | 10.8 | 7.5 – 14.1 | 16.3 | 14.7 – 18.0 | 47.1 | 43.1 – 51.0 | 39.5 | 33.9 – 45.0 | 2.7§ | 1.0 – 4.4 | 3.6 | 1.9 – 5.4 | 6.3§ | 4.7 – 7.8 | 64.4 | 54.4 – 74.4 | 73.5 | 68.4 – 78.6 | 57.2 | 51.6 – 62.9 | 29.0 | 23.3 – 34.7 | 84.4 | 80.7 – 88.1 | 21.8 | 14.3 – 29.3 | 56.7 | 37.0 – 76.4 | 25.8 | 20.8 – 30.8 | 37.1 | 33.7 – 40.5 | 67.4 | 57.3 – 77.4 | 69.7 | 51.4 – 88.0 |
| 2010–2014 | 8.7 | 0.3 – 17.0 | 16.7 | 14.2 – 19.3 | 43.9§ | 39.3 – 48.5 | 32.7§ | 26.6 – 38.8 | 3.7§ | 0.7 – 6.8 | 4.4 | 1.0 – 7.8 | 4.6§ | 3.0 – 6.2 | 59.7§ | 49.4 – 69.9 | 75.5§ | 69.4 – 81.5 | 56.7§ | 50.0 – 63.4 | 28.0§ | 21.3 – 34.7 | 82.0§ | 78.4 – 85.5 | 24.2 | 15.2 – 33.2 | – | 16.5 | 11.4 –21.6 | 32.5 | 23.8 – 41.2 | 63.9 | 48.5 – 79.3 | – | |||
|
| |||||||||||||||||||||||||||||||||||||
| Colombia | 2000–2004 | 10.7§ | 5.6 – 15.8 | 18.4 | 16.0 – 20.9 | 45.0 | 40.6 – 49.4 | 38.3 | 32.9 – 43.7 | 4.8§ | 1.8 – 7.9 | 6.4§ | 3.5 – 9.4 | 9.4 | 7.2 – 11.5 | 63.1§ | 57.0 – 69.1 | 72.3 | 68.9 – 75.7 | 56.6§ | 53.5 – 59.8 | 33.5 | 28.0 – 39.0 | 83.6 | 80.7 – 86.5 | 23.8 | 20.1 – 27.5 | 44.9§ | 32.9 – 57.0 | 16.3 | 11.4 –21.2 | 37.2 | 33.4 – 40.9 | 52.3 | 43.5 – 61.2 | 68.4§ | 55.3 – 81.6 |
| (4 registries) | 2005–2009 | 9.5 | 4.6 – 14.4 | 17.7 | 16.2 – 19.3 | 41.3 | 37.9 – 44.7 | 37.2 | 32.7 – 41.7 | 5.4 | 3.1 – 7.7 | 3.4 | 1.6 – 5.2 | 10.5 | 8.5 – 12.5 | 71.3§ | 66.2 – 76.5 | 79.1 | 76.1 – 82.0 | 55.4 | 52.6 – 58.1 | 35.4 | 30.3 – 40.6 | 87.8 | 85.4 – 90.3 | 27.4 | 23.5 – 31.4 | 33.9§ | 23.4 – 44.5 | 30.7 | 25.7 – 35.7 | 42.3 | 39.2 – 45.4 | 57.3 | 47.8 – 66.9 | 85.0§ | 76.1 – 93.9 |
| 2010–2014 | 10.5§ | 3.9 – 17.1 | 17.1§ | 15.4 – 18.8 | 34.5§ | 31.2 – 37.9 | 38.0§ | 33.2 – 42.8 | 5.2§ | 2.7 – 7.8 | 5.3§ | 2.8 – 7.8 | 8.7§ | 6.7 – 10.6 | 65.1§ | 59.2 – 71.1 | 72.1§ | 69.0 – 75.2 | 49.4§ | 46.5 – 52.3 | 33.3§ | 28.2 – 38.4 | 80.3§ | 77.6 – 83.1 | 20.8§ | 17.1 – 24.4 | 46.9§ | 35.9 – 57.9 | 31.8§ | 26.6 – 37.1 | 40.3§ | 37.0 – 43.6 | 68.9 | 51.6 – 86.3 | – | ||
|
| |||||||||||||||||||||||||||||||||||||
| Costa Rica* | 2000–2004 | 35.7§ | 26.3 – 45.1 | 48.4 | 45.5 – 51.2 | 63.8 | 59.5 – 68.1 | 48.4 | 41.3 – 55.6 | 39.0§ | 32.4 – 45.6 | 38.1§ | 31.3 – 44.8 | 36.2§ | 31.0 – 41.5 | 82.6 | 77.2 – 88.1 | 87.0 | 83.6 – 90.3 | 84.9§ | 81.2 – 88.6 | 54.3 | 43.7 – 64.9 | 94.0 | 92.0 – 96.1 | 30.8§ | 24.9 – 36.7 | 77.1 | 55.1 – 99.0 | 35.0 | 25.4 – 44.6 | 50.0 | 45.2 – 54.8 | 97.8 | 93.2 – 100.0 | – | |
| 2005–2009 | 19.2§ | 11.3 – 27.1 | 38.4 | 36.3 – 40.5 | 55.1 | 52.2 – 58.0 | 50.2 | 45.2 – 55.2 | 23.6§ | 18.5 – 28.7 | 23.8§ | 19.1 – 28.6 | 22.0§ | 19.0 – 25.1 | 76.2 | 71.5 – 80.8 | 86.4 | 84.0 – 88.7 | 78.3§ | 75.3 – 81.3 | 47.1 | 40.5 – 53.7 | 92.6 | 90.9 – 94.2 | 18.9§ | 15.1 – 22.8 | 71.2 | 61.2 – 81.3 | 21.2 | 15.7 – 26.7 | 50.4 | 46.9 – 53.9 | 87.4 | 82.8 – 91.9 | 93.0 | 86.7 – 99.3 | |
| 2010–2014 | 20.9§ | 14.3 – 27.6 | 40.6 | 38.5 – 42.7 | 60.1 | 57.4 – 62.8 | 53.9 | 49.2 – 58.5 | 24.1§ | 19.7 – 28.5 | 24.5§ | 19.5 – 29.5 | 20.1§ | 17.1 – 23.1 | 77.2 | 72.7 – 81.7 | 86.7 | 84.6 – 88.9 | 78.0§ | 74.8 – 81.2 | 56.9 | 49.1 – 64.7 | 93.2 | 91.5 – 94.9 | 21.5§ | 17.5 – 25.6 | 69.8 | 57.8 – 81.8 | 29.4 | 23.3 – 35.4 | 52.4 | 49.1 – 55.7 | 80.0 | 69.3 – 90.7 | 93.5 | 86.2 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Cuba* | 2000–2004 | – | 17.2§ | 15.7 – 18.7 | 39.8§ | 38.3 – 41.2 | – | – | – | 4.5§ | 3.8 – 5.1 | – | 73.7 | 72.2 – 75.1 | 64.1 | 62.3 – 65.9 | 29.5 | 26.7 – 32.3 | 26.1§ | 24.6 – 27.6 | – | – | – | 44.0§ | 41.6 – 46.5 | – | 72.4§ | 67.1 – 77.8 | |||||||||
| 2005–2009 | – | 25.6§ | 23.6 – 27.5 | 48.5§ | 46.9 – 50.1 | – | – | – | 23.2§ | 22.1 – 24.2 | – | 81.8 | 80.5 – 83.0 | 68.8 | 67.0 – 70.7 | 38.4 | 35.6 – 41.3 | 53.8§ | 52.1 – 55.6 | – | – | – | 49.4§ | 46.7 – 52.0 | – | 77.4§ | 71.5 – 83.3 | ||||||||||
| 2010–2014 | – | 35.7§ | 32.8 – 38.6 | 63.9§ | 61.6 – 66.2 | – | – | – | 30.1§ | 28.4 – 31.8 | – | 75.1 | 73.7 – 76.5 | 72.9 | 70.5 – 75.2 | 49.3§ | 45.0 – 53.5 | 71.4§ | 68.9 – 74.0 | – | – | – | 60.1§ | 56.3 – 63.8 | – | 78.5§ | 70.5 – 86.6 | ||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Ecuador | 2000–2004 | 20.9 | 9.9 – 31.9 | 17.8 | 12.3 – 23.3 | 47.7 | 41.0 – 54.4 | 38.7 | 30.4 – 47.1 | 8.1§ | 4.6 – 11.5 | 8.4§ | 4.7 – 12.2 | 10.1§ | 7.2 – 13.0 | 59.0 | 50.9 – 67.1 | 72.1 | 67.3 – 76.9 | 47.4 | 44.1 – 50.7 | 34.5 | 26.5 – 42.5 | 85.7 | 82.0 – 89.5 | 24.2 | 19.4 – 28.9 | 48.0§ | 35.2 – 60.8 | 20.5 | 12.6 – 28.4 | 33.1 | 29.1 – 37.0 | 48.3§ | 40.3 – 56.4 | 73.4§ | 62.7 – 84.1 |
| (5 registries) | 2005–2009 | 7.7 | 3.5 – 11.9 | 17.4 | 12.0 – 22.7 | 46.7 | 42.9 – 50.5 | 43.5 | 38.8 – 48.2 | 6.3§ | 4.1 – 8.6 | 9.0§ | 6.2 – 11.8 | 10.5§ | 8.5 – 12.4 | 60.5 | 54.5 – 66.5 | 75.7 | 72.7 – 78.7 | 50.4 | 47.8 – 52.9 | 38.8 | 33.1 – 44.5 | 80.7 | 78.0 – 83.5 | 20.9 | 17.6 – 24.2 | 31.2 | 20.9 – 41.5 | 20.3 | 15.5 – 25.0 | 39.4 | 36.7 – 42.0 | 51.5 | 44.9 – 58.0 | 72.2 | 63.7 – 80.7 |
| 2010–2014 | 12.7 | 6.7 – 18.7 | 19.1 | 13.1 – 25.1 | 47.8 | 43.9 – 51.6 | 44.5 | 39.2 – 49.8 | 5.9§ | 3.9 – 7.8 | 8.4§ | 5.7 – 11.2 | 12.2§ | 10.0 – 14.4 | 57.9 | 51.6 – 64.1 | 75.5 | 72.4 – 78.7 | 52.0 | 49.3 – 54.7 | 37.9 | 32.1 – 43.7 | 82.2 | 79.4 – 85.0 | 25.8 | 22.0 – 29.6 | 48.2 | 35.9 – 60.5 | 24.4 | 18.9 – 29.9 | 40.1 | 37.4 – 42.8 | 49.8 | 42.7 – 56.9 | 67.3 | 57.4 – 77.2 | |
|
| |||||||||||||||||||||||||||||||||||||
| Guadeloupe* | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | 0.0 | 0.0 – 0.1 | 11.7§ | 5.7 – 17.7 | 30.9§ | 23.1 – 38.7 | 21.3§ | 8.8 – 33.8 | 9.5§ | 0.0 – 20.3 | 11.2§ | 1.7 – 20.8 | 6.8 | 2.3 – 11.2 | 86.2§ | 53.0 – 100.0 | 69.8§ | 60.0 – 79.7 | 20.9§ | 3.3 – 38.5 | 24.2§ | 8.9 – 39.5 | 82.8§ | 78.2 – 87.5 | 0.2§ | 0.0 – 0.6 | – | 37.5§ | 9.8 – 65.3 | 25.7§ | 17.3 – 34.0 | – | – | ||||
| 2010–2014 | – | 11.7§ | 6.8 – 16.6 | 26.8§ | 19.5 – 34.0 | 35.6§ | 22.4 – 48.8 | 3.7§ | 0.0 – 9.2 | – | 4.0§ | 0.2 – 7.7 | 14.1§ | 0.0 – 36.7 | 50.2§ | 39.6 – 60.8 | 19.4§ | 9.0 – 29.9 | 29.5§ | 13.8 – 45.2 | 71.4§ | 65.5 – 77.2 | 9.6§ | 0.0 – 19.5 | – | 32.3§ | 21.4 – 43.2 | 36.0§ | 27.3 – 44.6 | – | – | ||||||
|
| |||||||||||||||||||||||||||||||||||||
| Martinique* | 2000–2004 | 4.2 | 0.4 – 8.1 | 29.7 | 24.2 – 35.2 | 57.0 | 50.4 – 63.6 | 44.1 | 35.1 – 53.1 | 12.0 | 5.6 – 18.4 | 13.4 | 7.8 – 19.1 | 12.5 | 7.6 – 17.4 | 81.8§ | 68.5 – 95.1 | 78.9 | 73.5 – 84.3 | 69.7 | 62.5 – 76.9 | 29.5 | 17.8 – 41.1 | 93.2 | 90.5 – 95.8 | 32.6 | 22.4 – 42.8 | – | 46.2 | 36.8 – 55.6 | 49.8 | 44.1 – 55.5 | 77.5 | 55.9 – 99.2 | – | ||
| 2005–2009 | 4.9 | 1.1 – 8.7 | 33.0 | 27.5 – 38.5 | 54.9 | 49.5 – 60.3 | 54.0 | 46.0 – 62.1 | 12.4 | 5.6 – 19.1 | 6.9 | 3.2 – 10.5 | 14.7 | 10.4 – 18.9 | 86.4§ | 74.7 – 98.2 | 87.8 | 83.5 – 92.1 | 57.6 | 48.9 – 66.3 | 34.0 | 24.6 – 43.4 | 97.8 | 95.7 – 99.9 | 28.1 | 19.9 – 36.2 | – | 49.7 | 41.8 – 57.6 | 48.7 | 43.9 – 53.6 | – | – | ||||
| 2010–2014 | 4.0 | 1.8 – 6.3 | 32.1 | 24.5 – 39.6 | 53.6 | 46.9 – 60.3 | 52.0 | 42.2 – 61.7 | 15.6 | 7.2 – 23.9 | 11.9 | 6.5 – 17.3 | 11.8 | 6.4 – 17.2 | 77.8§ | 61.3 – 94.3 | 89.8 | 84.5 – 95.1 | 57.5 | 46.2 – 68.8 | 35.7§ | 23.4 – 48.0 | 97.9 | 95.1 – 100.0 | 35.8 | 26.4 – 45.3 | – | 47.9 | 39.4 – 56.5 | 49.4 | 43.3 – 55.4 | – | – | ||||
|
| |||||||||||||||||||||||||||||||||||||
| Mexico (Childhood)† | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | – | – | – | – | – | 41.2 | 35.1 – 47.4 | – | – | 52.5 | 49.8 – 55.2 | 75.1§ | 70.7 – 79.5 | ||||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | – | – | – | – | – | 36.5 | 30.0 – 43.0 | – | – | 52.7 | 49.4 – 56.1 | 72.0§ | 66.4 – 77.7 | ||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Peru (Lima) | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |||||||||||||||||||
| 2010–2014 | – | – | 59.0 | 55.8 – 62.1 | 54.8 | 50.0 – 59.5 | – | – | – | – | 84.0 | 81.4 – 86.7 | 57.2 | 54.8 – 59.6 | – | – | – | – | 36.3§ | 29.5 – 43.0 | 46.2§ | 42.9 – 49.6 | 60.4 | 53.4 – 67.3 | 73.4§ | 64.8 – 82.1 | |||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Puerto Rico* | 2000–2004 | 10.9 | 8.5 – 13.4 | 26.6 | 24.1 – 29.1 | 60.9 | 59.3 – 62.5 | 53.9 | 50.9 – 57.0 | 11.8§ | 9.0 – 14.6 | 8.8§ | 6.3 – 11.2 | 14.7§ | 13.1 – 16.3 | 73.3 | 68.2 – 78.4 | 83.4 | 81.9 – 84.9 | 60.6 | 56.9 – 64.4 | 34.9 | 30.8 – 39.0 | 98.7 | 97.6 – 99.7 | 31.7§ | 28.0 – 35.4 | 71.2 | 62.1 – 80.3 | 25.6§ | 21.4 – 29.8 | 49.1 | 46.8 – 51.4 | 79.3 | 70.2 – 88.4 | 94.5 | 90.1 – 98.8 |
| 2005–2009 | 13.0 | 10.1 – 15.9 | 29.9 | 27.3 – 32.5 | 62.1 | 60.6 – 63.5 | 59.4 | 56.6 – 62.3 | 8.7§ | 6.9 – 10.5 | 9.0§ | 6.9 – 11.1 | 16.0 | 14.5 – 17.5 | 75.4 | 70.6 – 80.1 | 83.0 | 81.6 – 84.4 | 58.8 | 55.3 – 62.4 | 37.2 | 33.4 – 41.0 | 99.0 | 98.1 – 99.9 | 34.8 | 31.5 – 38.0 | 76.1 | 67.6 – 84.6 | 38.8 | 35.6 – 42.0 | 53.5 | 51.6 – 55.4 | 86.2 | 78.1 – 94.4 | 90.9 | 83.1 – 98.7 | |
| 2010–2014 | 20.4 | 14.8 – 25.9 | 34.6 | 30.3 – 39.0 | 63.4 | 61.1 – 65.7 | 59.0 | 54.6 – 63.4 | 14.2§ | 10.4 – 18.0 | 10.2§ | 7.1 – 13.3 | 17.6 | 14.9 – 20.3 | 75.1 | 68.2 – 81.9 | 84.1 | 82.0 – 86.3 | 63.5 | 57.9 – 69.1 | 37.3 | 32.0 – 42.6 | 98.4 | 97.0 – 99.8 | 36.3 | 31.2 – 41.4 | 70.5 | 56.3 – 84.7 | 44.9 | 39.6 – 50.1 | 60.3 | 57.2 – 63.4 | 93.1 | 83.6 – 100.0 | 96.3 | 89.9 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Uruguay* | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | 12.0§ | 8.4 – 15.6 | 20.5 | 17.5 – 23.5 | 57.7 | 55.0 – 60.4 | 50.5 | 46.3 – 54.6 | 12.0§ | 4.4 – 19.7 | 4.3§ | 2.3 – 6.3 | 9.9§ | 8.3 – 11.5 | – | – | 55.7 | 51.6 – 59.8 | 37.4 | 31.9 – 42.8 | 84.7 | 82.1 – 87.3 | – | – | – | – | – | – | |||||||||
| 2010–2014 | 8.0§ | 5.3 – 10.7 | 18.5§ | 15.4 – 21.5 | 53.5 | 49.2 – 57.7 | 50.1 | 44.8 – 55.4 | 14.3§ | 8.0 – 20.6 | 4.4§ | 3.0 – 5.8 | 9.0§ | 7.4 – 10.6 | – | – | 56.5 | 51.8 – 61.1 | 37.4§ | 31.4 – 43.4 | 86.5 | 83.7 – 89.3 | – | – | – | – | – | – | |||||||||
|
| |||||||||||||||||||||||||||||||||||||
| AMERICA (NORTH) | |||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Canada | 2000–2004 | 14.5 | 13.4 – 15.6 | 25.1 | 24.2 – 26.0 | 61.6 | 61.1 – 62.1 | 61.9 | 61.1 – 62.8 | 17.4 | 16.2 – 18.5 | 7.9 | 7.3 – 8.5 | 16.3 | 15.9 – 16.6 | 87.9 | 87.3 – 88.6 | 85.9 | 85.5 – 86.4 | 67.9 | 66.4 – 69.5 | 37.6 | 36.6 – 38.6 | 93.0 | 92.6 – 93.3 | 24.7 | 23.4 – 26.0 | 73.3 | 68.2 – 78.4 | 47.5 | 46.1 – 48.8 | 60.1 | 59.5 – 60.7 | 91.0 | 88.8 – 93.3 | 89.4 | 85.9 – 92.9 |
| (9 registries) | 2005–2009 | 14.7 | 13.7 – 15.7 | 26.6 | 25.7 – 27.5 | 65.7 | 65.2 – 66.2 | 65.5 | 64.7 – 66.3 | 19.2 | 18.2 – 20.2 | 9.4 | 8.8 – 10.0 | 18.5 | 18.1 – 18.8 | 88.5 | 88.0 – 89.1 | 87.6 | 87.2 – 88.0 | 66.9 | 65.3 – 68.5 | 41.0 | 40.0 – 42.0 | 94.2 | 93.9 – 94.5 | 29.8 | 28.5 – 31.1 | 72.5 | 67.7 – 77.2 | 49.2 | 47.9 – 50.5 | 66.0 | 65.4 – 66.5 | 92.1 | 90.0 – 94.3 | 88.5 | 84.4 – 92.5 |
| 2010–2014 | 16.1 | 15.1 – 17.1 | 29.6 | 28.6 – 30.5 | 67.0 | 66.5 – 67.5 | 66.8 | 66.0 – 67.5 | 18.7 | 17.8 – 19.7 | 10.8 | 10.2 – 11.4 | 20.6 | 20.2 – 20.9 | 89.1 | 88.6 – 89.6 | 88.2 | 87.8 – 88.6 | 66.6 | 65.1 – 68.1 | 40.9 | 39.9 – 41.8 | 93.6 | 93.3 – 94.0 | 29.9 | 28.6 – 31.1 | 72.7 | 68.0 – 77.4 | 50.4 | 49.2 – 51.6 | 68.6 | 68.1 – 69.1 | 92.6 | 90.7 – 94.6 | 92.3 | 89.1 – 95.6 | |
|
| |||||||||||||||||||||||||||||||||||||
| United States | 2000–2004 | 16.5 | 16.1 – 16.8 | 26.2 | 25.8 – 26.5 | 64.7 | 64.5 – 64.9 | 63.9 | 63.5 – 64.2 | 12.5 | 12.2 – 12.8 | 7.2 | 7.0 – 7.4 | 17.0 | 16.9 – 17.1 | 88.9 | 88.7 – 89.1 | 88.9 | 88.7 – 89.0 | 64.3 | 63.7 – 64.8 | 40.4 | 40.0 – 40.7 | 97.5 | 97.3 – 97.6 | 26.8 | 26.5 – 27.1 | 72.1 | 71.1 – 73.2 | 41.0 | 40.7 – 41.3 | 61.2 | 61.0 – 61.4 | 86.7 | 85.8 – 87.5 | 88.5 | 87.4 – 89.6 |
| (48 registries) | 2005–2009 | 18.7 | 18.4 – 19.1 | 30.1 | 29.7 – 30.4 | 65.5 | 65.3 – 65.7 | 64.5 | 64.1 – 64.8 | 15.6 | 15.3 – 15.9 | 8.9 | 8.7 – 9.1 | 19.4 | 19.3 – 19.5 | 90.4 | 90.2 – 90.6 | 89.8 | 89.6 – 89.9 | 63.0 | 62.5 – 63.5 | 42.0 | 41.7 – 42.4 | 98.1 | 98.0 – 98.2 | 35.1 | 34.8 – 35.4 | 76.8 | 75.9 – 77.7 | 45.9 | 45.6 – 46.2 | 66.1 | 66.0 – 66.3 | 88.1 | 87.3 – 88.9 | 90.2 | 89.2 – 91.3 |
| 2010–2014 | 20.0 | 19.6 – 20.4 | 33.1 | 32.7 – 33.4 | 64.9 | 64.7 – 65.1 | 64.1 | 63.7 – 64.4 | 17.4 | 17.1 – 17.7 | 11.5 | 11.3 – 11.7 | 21.2 | 21.1 – 21.3 | 90.8 | 90.6 – 91.0 | 90.2 | 90.1 – 90.4 | 62.6 | 62.0 – 63.1 | 43.4 | 43.1 – 43.8 | 97.4 | 97.3 – 97.5 | 36.5 | 36.1 – 36.8 | 78.2 | 77.3 – 79.2 | 46.7 | 46.4 – 47.0 | 68.1 | 67.9 – 68.3 | 89.5 | 88.8 – 90.3 | 94.3 | 93.6 – 95.1 | |
|
| |||||||||||||||||||||||||||||||||||||
| ASIA | |||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| China | 2000–2004 | 22.9 | 22.0 – 23.9 | 30.2 | 29.3 – 31.1 | 51.4 | 49.6 – 53.3 | 49.5 | 47.5 – 51.4 | 11.7 | 10.9 – 12.5 | 14.4 | 12.8 – 16.0 | 18.7 | 18.0 – 19.4 | 35.6 | 25.8 – 45.4 | 75.9 | 70.9 – 80.9 | 53.3 | 48.1 – 58.5 | 42.4 | 38.2 – 46.6 | 57.7 | 52.3 – 63.0 | 22.7 | 20.5 – 25.0 | 32.7 | 21.0 – 44.4 | 18.6 | 15.8 – 21.5 | 33.9 | 31.6 – 36.2 | 61.8 | 46.5 – 77.2 | 44.2 | 29.7 – 58.8 |
| (21 registries) | 2005–2009 | 27.1 | 26.5 – 27.7 | 33.2 | 32.7 – 33.7 | 55.6 | 54.6 – 56.5 | 52.5 | 51.5 – 53.6 | 11.6 | 11.1 – 12.0 | 10.2 | 9.4 – 11.0 | 17.7 | 17.4 – 18.1 | 45.5 | 40.8 – 50.2 | 80.4 | 79.3 – 81.5 | 63.0 | 61.2 – 64.9 | 40.6 | 38.8 – 42.5 | 62.5 | 59.9 – 65.1 | 26.4 | 25.2 – 27.7 | 39.1 | 31.2 – 47.0 | 20.1 | 18.7 – 21.4 | 35.4 | 34.2 – 36.6 | 53.5 | 44.6 – 62.4 | 52.3 | 39.5 – 65.0 |
| 2010–2014 | 29.7 | 29.0 – 30.4 | 35.9 | 35.3 – 36.5 | 57.6 | 56.6 – 58.6 | 56.9 | 55.8 – 58.0 | 14.1 | 13.6 – 14.7 | 9.9 | 9.1 – 10.7 | 19.8 | 19.4 – 20.2 | 49.6 | 44.5 – 54.6 | 83.2 | 82.1 – 84.3 | 67.6 | 65.8 – 69.5 | 41.8 | 39.8 – 43.7 | 69.2 | 66.4 – 72.0 | 32.0 | 30.6 – 33.5 | 41.1 | 32.0 – 50.1 | 24.8 | 23.2 – 26.4 | 38.3 | 37.0 – 39.5 | 57.7 | 46.6 – 68.7 | 61.1 | 47.5 – 74.8 | |
|
| |||||||||||||||||||||||||||||||||||||
| Cyprus* | 2000–2004 | – | 36.6 | 22.2 – 51.1 | 70.7§ | 61.8 – 79.6 | 61.9§ | 43.0 – 80.8 | 8.4§ | 0.0 – 21.0 | 12.8§ | 1.7 – 23.9 | 18.3 | 12.2 – 24.3 | 89.0§ | 73.6 – 100.0 | 89.3§ | 80.8 – 97.8 | 60.4§ | 41.0 – 79.8 | 42.6§ | 24.6 – 60.6 | 91.0§ | 84.0 – 97.9 | 32.1§ | 13.4 – 50.8 | – | 60.0§ | 39.1 – 80.9 | 61.4§ | 52.2 – 70.6 | – | – | ||||
| 2005–2009 | 47.2§ | 30.5 – 63.8 | 28.1§ | 22.9 – 33.3 | 67.6§ | 63.9 – 71.4 | 78.3§ | 71.3 – 85.4 | 13.3§ | 6.3 – 20.2 | 8.0§ | 4.5 – 11.6 | 18.2 | 15.6 – 20.8 | 82.1§ | 75.8 – 88.4 | 92.0§ | 88.7 – 95.4 | 66.9§ | 60.0 – 73.8 | 46.2§ | 39.9 – 52.4 | 98.3§ | 95.4 – 100.0 | 24.6§ | 18.6 – 30.7 | – | 39.8§ | 33.3 – 46.2 | 69.4§ | 65.1 – 73.7 | 85.2§ | 72.1 – 98.3 | 100.0§ | 86.3 – 100.0 | ||
| 2010–2014 | 39.0§ | 21.8 – 56.3 | 35.6§ | 30.0 – 41.2 | 72.1§ | 68.5 – 75.8 | 75.9§ | 69.6 – 82.2 | 10.6§ | 5.8 – 15.5 | 11.6§ | 7.7 – 15.5 | 18.7 | 16.2 – 21.2 | 79.0§ | 73.1 – 85.0 | 92.8§ | 89.7 – 95.9 | 73.3§ | 65.1 – 81.6 | 46.4§ | 40.0 – 52.7 | 99.2§ | 96.4 – 100.0 | 25.2§ | 19.5 – 31.0 | – | 36.0§ | 30.2 – 41.9 | 65.7§ | 61.8 – 69.6 | 86.6§ | 78.2 – 95.0 | – | |||
|
| |||||||||||||||||||||||||||||||||||||
| Hong Kong* | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | 56.1 | 55.1 – 57.1 | 57.3 | 55.8 – 58.7 | – | – | – | – | 82.2 | 80.9 – 83.5 | 66.7 | 64.5 – 69.0 | – | – | – | – | – | – | – | – | |||||||||||||||
| 2010–2014 | – | – | 56.4 | 55.4 – 57.3 | 58.0 | 56.6 – 59.4 | – | – | – | – | 83.3 | 82.1 – 84.6 | 65.8 | 63.6 – 68.1 | – | – | – | – | – | – | – | – | |||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| India | 2000–2004 | 2.9 | 0.0 – 6.4 | 6.4 | 2.5 – 10.3 | 46.9 | 31.9 – 61.8 | 36.9 | 16.1 – 57.8 | 2.4 | 0.0 – 6.0 | 4.2 | 0.0 – 10.5 | 6.9 | 2.3 – 11.5 | – | 57.6 | 48.1 – 67.1 | 45.2 | 34.8 – 55.6 | 25.6 | 12.2 – 39.1 | 24.8 | 6.3 – 43.3 | 22.4§ | 8.3 – 36.5 | – | 19.7 | 6.3 – 33.1 | 40.6 | 28.1 – 53.1 | 54.0 | 28.3 – 79.8 | – | |||
| (2 registries) | 2005–2009 | 3.4 | 0.7 – 6.0 | 9.8 | 3.4 – 16.3 | 33.8 | 21.1 – 46.4 | 33.6 | 20.8 – 46.3 | 3.7 | 0.0 – 7.7 | 5.3 | 0.0 – 11.4 | 3.5 | 1.4 –5.7 | – | 59.1 | 46.6 – 71.6 | 51.6 | 40.5 – 62.6 | 13.2 | 7.7 – 18.7 | 33.2 | 16.3 – 50.0 | 16.7 | 10.4 – 23.0 | – | 6.1 | 2.5 – 9.6 | 45.4 | 34.2 – 56.6 | 75.5 | 52.1 – 99.0 | – | |||
| 2010–2014 | 4.1 | 0.0 – 8.5 | 8.9 | 4.0 – 13.9 | 38.9 | 24.6 – 53.3 | 30.0 | 20.5 – 39.5 | 6.3 | 0.6 – 11.9 | 5.6 | 0.0 – 11.6 | 3.7 | 1.6 –5.7 | 61.5 | 27.3 – 95.8 | 66.1 | 51.5 – 80.8 | 59.0 | 47.5 – 70.5 | 15.6 | 10.2 – 21.1 | 44.3 | 32.1 – 56.6 | 30.0 | 17.5 – 42.6 | – | 29.0 | 16.8 – 41.3 | 45.6 | 33.0 – 58.1 | – | – | ||||
|
| |||||||||||||||||||||||||||||||||||||
| Iran (Golestan) | 2000–2004 | –- | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | 7.4 | 4.8 – 10.0 | 5.7 | 3.3 – 8.0 | 29.1 | 20.2 – 38.0 | 26.2 | 14.1 – 38.3 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Israel* | 2000–2004 | 17.9 | 14.3 – 21.5 | 29.3 | 27.6 – 31.1 | 66.5 | 65.4 – 67.6 | 62.7 | 60.6 – 64.7 | 15.1§ | 12.2 – 17.9 | 7.6§ | 6.4 – 8.8 | 20.8 | 19.8 – 21.8 | 85.6 | 84.2 – 87.0 | 85.1 | 84.2 – 86.1 | 65.0 | 61.6 – 68.5 | 40.1 | 37.8 – 42.4 | 92.5 | 91.4 – 93.6 | 29.7 | 27.8 – 31.7 | 74.5 | 69.3 – 79.6 | 51.3 | 49.1 – 53.5 | 63.7 | 62.5 – 64.9 | 86.4 | 81.6 – 91.2 | 89.1 | 84.6 – 93.5 |
| 2005–2009 | 22.4 | 18.6 – 26.2 | 29.8 | 28.1 – 31.5 | 71.4 | 70.3 – 72.4 | 67.3 | 65.3 – 69.3 | 15.6§ | 13.1 – 18.2 | 9.2§ | 8.0 – 10.5 | 23.8 | 22.8 – 24.8 | 88.4 | 87.2 – 89.7 | 87.8 | 86.8 – 88.7 | 65.9 | 62.7 – 69.1 | 43.5 | 41.1 – 45.9 | 95.7 | 94.7 – 96.6 | 32.3 | 30.4 – 34.3 | 72.0 | 67.2 – 76.9 | 43.9 | 41.9 – 46.0 | 65.2 | 64.1 – 66.3 | 86.7 | 82.2 – 91.2 | 90.8 | 87.3 – 94.3 | |
| 2010–2014 | 25.8 | 21.4 – 30.2 | 32.3 | 30.4 – 34.3 | 71.7 | 70.6 – 72.9 | 67.8 | 65.6 – 70.0 | 18.9§ | 15.6 – 22.2 | 12.4§ | 10.8 – 14.0 | 26.6 | 25.4 – 27.7 | 87.4 | 86.1 – 88.8 | 88.0 | 87.0 – 89.0 | 66.6 | 63.2 – 70.1 | 45.0 | 42.3 – 47.7 | 95.6 | 94.5 – 96.7 | 32.8 | 30.6 – 34.9 | 77.6 | 72.6 – 82.6 | 39.7 | 37.6 – 41.9 | 65.5 | 64.2 – 66.7 | 87.9 | 83.1 – 92.6 | 92.3 | 89.0 – 95.6 | |
|
| |||||||||||||||||||||||||||||||||||||
| Japan (16 registries) | 2000–2004 | 27.7 | 26.4 – 29.0 | 50.5 | 50.0 – 50.9 | 63.4 | 62.7 – 64.0 | 58.6 | 57.6 – 59.5 | 25.7§ | 25.1 – 26.3 | 6.9§ | 6.4 – 7.4 | 29.3 | 28.1 – 30.5 | 68.9 | 65.1 – 72.8 | 85.9 | 85.2 – 86.6 | 67.5 | 66.3 – 68.7 | 35.5 | 33.8 – 37.2 | 85.9 | 84.9 – 87.0 | 27.9§ | 26.3 – 29.5 | 65.3 | 59.2 – 71.5 | 24.8 | 23.4 – 26.1 | 47.5 | 46.3 – 48.7 | 79.7 | 74.9 – 84.4 | 86.0 | 80.2 – 91.7 |
| 2005–2009 | 33.3 | 32.3 – 34.2 | 57.6 | 57.3 – 57.9 | 66.8 | 66.3 – 67.3 | 64.0 | 63.3 – 64.6 | 28.6§ | 28.1 – 29.1 | 7.6§ | 7.2 – 7.9 | 29.3 | 28.9 – 29.7 | 68.3 | 65.6 – 71.0 | 88.9 | 88.4 – 89.3 | 69.2 | 68.3 – 70.1 | 43.9 | 42.8 – 45.1 | 91.4 | 90.8 – 92.0 | 38.5§ | 37.2 – 39.7 | 62.5 | 58.1 – 66.8 | 27.5 | 26.7 – 28.3 | 52.0 | 51.4 – 52.6 | 83.7 | 80.6 – 86.9 | 84.7 | 79.5 – 89.9 | |
| 2010–2014 | 36.0 | 34.8 – 37.3 | 60.3 | 59.9 – 60.7 | 67.8 | 67.3 – 68.4 | 64.8 | 64.0 – 65.7 | 30.1§ | 29.5 – 30.6 | 8.3§ | 7.8 – 8.7 | 32.9 | 32.3 – 33.4 | 69.0 | 66.0 – 72.0 | 89.4 | 88.9 – 89.9 | 71.4 | 70.4 – 72.3 | 46.3 | 44.9 – 47.7 | 93.0 | 92.4 – 93.6 | 46.3§ | 44.9 – 47.7 | 69.6 | 64.4 – 74.7 | 33.3 | 32.4 – 34.3 | 57.3 | 56.5 – 58.0 | 87.6 | 84.2 – 91.0 | 89.6 | 84.2 – 95.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Jordan* | 2000–2004 | 52.6§ | 41.3 – 63.9 | 76.1§ | 69.7 – 82.5 | 86.0§ | 81.6 – 90.5 | 79.9§ | 71.1 – 88.8 | 71.5§ | 58.1 – 84.9 | 66.9§ | 52.0 – 81.8 | 42.9§ | 38.3 – 47.4 | 68.5§ | 56.4 – 80.6 | 87.6§ | 83.5 – 91.7 | 75.6§ | 66.8 – 84.3 | – | 88.5§ | 83.7 – 93.3 | 55.8§ | 49.0 – 62.6 | 73.5§ | 65.7 – 81.3 | 57.1§ | 48.1 – 66.1 | 76.0§ | 69.4 – 82.6 | 75.4§ | 69.7 – 81.2 | 92.4§ | 88.1 – 96.6 | |
| 2005–2009 | 53.9§ | 43.0 – 64.8 | 64.8§ | 58.4 – 71.3 | 80.8§ | 77.0 – 84.7 | 76.2§ | 67.1 – 85.3 | 64.3§ | 54.5 – 74.1 | 32.5§ | 25.6 – 39.4 | 44.1§ | 39.4 – 48.7 | 63.1§ | 49.3 – 76.9 | 86.6§ | 83.2 – 90.0 | 70.6§ | 63.9 – 77.4 | – | 88.6§ | 83.3 – 93.9 | 46.7§ | 41.1 – 52.4 | 66.0§ | 58.6 – 73.3 | 56.5§ | 46.9 – 66.1 | 74.6§ | 68.3 – 80.9 | 89.2§ | 84.8 – 93.6 | 91.1§ | 86.4 – 95.8 | ||
| 2010–2014 | 41.1§ | 30.4 – 51.9 | 55.7§ | 48.7 – 62.6 | 76.1§ | 72.1 – 80.1 | 73.2§ | 65.0 – 81.4 | 40.0§ | 28.6 – 51.3 | 24.0§ | 18.7 – 29.3 | 28.3§ | 24.9 – 31.6 | 55.9§ | 41.5 – 70.4 | 84.4§ | 80.9 – 88.0 | 56.4§ | 48.2 – 64.6 | – | 86.1§ | 81.1 – 91.0 | 32.9§ | 26.8 – 39.0 | 57.3§ | 49.9 – 64.8 | 42.5§ | 35.3 – 49.6 | 65.1§ | 60.3 – 69.9 | 88.0§ | 83.1 – 92.8 | 87.0§ | 81.4 – 92.6 | ||
|
| |||||||||||||||||||||||||||||||||||||
| Korea* | 2000–2004 | 18.6 | 17.6 – 19.6 | 48.6 | 48.2 – 48.9 | 60.5 | 59.9 – 61.2 | 60.8 | 60.0 – 61.6 | 15.3 | 15.0 – 15.7 | 7.6 | 7.2 – 8.1 | 15.3 | 15.0 – 15.6 | 51.4 | 48.3 – 54.4 | 79.5 | 78.0 – 81.0 | 76.0 | 75.3 – 76.7 | 43.0 | 41.2 – 44.7 | 76.0 | 74.6 – 77.5 | 27.6 | 26.4 – 28.9 | 54.2 | 50.8 – 57.6 | 31.7 | 30.4 – 33.0 | 39.8 | 38.8 – 40.8 | 73.1 | 70.4 – 75.8 | 82.4 | 79.3 – 85.4 |
| 2005–2009 | 26.9 | 25.8 – 28.0 | 61.1 | 60.8 – 61.5 | 68.1 | 67.6 – 68.6 | 68.1 | 67.5 – 68.7 | 22.4 | 22.1 – 22.8 | 8.4 | 8.0 – 8.9 | 19.9 | 19.6 – 20.2 | 55.3 | 52.8 – 57.7 | 84.0 | 83.0 – 85.0 | 77.0 | 76.4 – 77.7 | 44.1 | 42.7 – 45.5 | 87.3 | 86.5 – 88.1 | 31.9 | 30.8 – 33.0 | 61.4 | 58.1 – 64.7 | 41.5 | 40.5 – 42.5 | 47.5 | 46.7 – 48.4 | 78.6 | 76.1 – 81.0 | 83.0 | 80.0 – 85.9 | |
| 2010–2014 | 31.3 | 30.3 – 32.4 | 68.9 | 68.6 – 69.2 | 71.8 | 71.4 – 72.2 | 71.1 | 70.6 – 71.7 | 27.2 | 26.8 – 27.6 | 10.5 | 10.0 – 10.9 | 25.1 | 24.8 – 25.4 | 59.9 | 57.5 – 62.2 | 86.6 | 85.8 – 87.5 | 77.3 | 76.6 – 78.0 | 47.5 | 46.2 – 48.9 | 89.9 | 89.2 – 90.5 | 33.7 | 32.6 – 34.7 | 60.3 | 56.9 – 63.8 | 45.9 | 44.9 – 46.8 | 52.5 | 51.8 – 53.3 | 84.4 | 82.1 – 86.7 | 91.0 | 88.9 – 93.1 | |
|
| |||||||||||||||||||||||||||||||||||||
| Kuwait* | 2000–2004 | 17.6§ | 2.9 – 32.4 | 15.0 | 7.1 – 22.9 | 64.8 | 53.1 – 76.5 | 59.3 | 48.1 – 70.4 | 11.4§ | 3.5 – 19.2 | 11.2§ | 3.1 – 19.3 | 13.3 | 8.9 – 17.7 | – | 68.3 | 58.0 – 78.7 | 54.8 | 45.2 – 64.3 | 38.9 | 26.3 – 51.5 | 78.8 | 66.7 – 90.9 | 30.3§ | 19.1 –41.5 | 47.1 | 24.4 – 69.8 | 38.6 | 27.1 – 50.0 | 52.1 | 42.9 – 61.2 | 76.1§ | 65.7 – 86.5 | 93.0 | 86.2 – 99.8 | |
| 2005–2009 | 9.5 | 0.0 – 20.6 | 13.4 | 7.1 – 19.7 | 50.2 | 42.7 – 57.7 | 53.3 | 42.4 – 64.2 | 12.4 | 5.8 – 19.1 | 7.0 | 3.0 – 11.0 | 16.3 | 11.1 –21.5 | – | 71.0 | 63.8 – 78.2 | 73.8 | 61.7 – 86.0 | 35.4 | 25.2 – 45.6 | 71.9 | 63.7 – 80.0 | 24.9 | 17.3 – 32.6 | 59.2 | 39.2 – 79.1 | 24.0 | 15.9 – 32.0 | 63.2 | 55.8 – 70.7 | 74.9 | 65.6 – 84.1 | 90.7 | 83.2 – 98.2 | ||
| 2010–2014 | 25.4 | 10.5 – 40.4 | 22.4 | 12.6 – 32.3 | 58.5 | 49.4 – 67.7 | 58.2 | 48.5 – 67.9 | 18.6 | 9.8 – 27.3 | 23.6 | 12.0 – 35.2 | 13.4 | 8.8 – 18.0 | – | 75.2 | 66.4 – 83.9 | 56.6 | 44.2 – 69.0 | 35.1 | 25.6 – 44.7 | 84.0 | 74.1 – 94.0 | 31.8 | 23.2 – 40.4 | – | 25.6 | 17.7 – 33.6 | 68.2 | 59.5 – 76.9 | 88.4 | 80.6 – 96.2 | 96.3 | 91.4 – 100.0 | |||
|
| |||||||||||||||||||||||||||||||||||||
| Malaysia (Penang) | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | 13.2 | 6.5 – 19.9 | 23.2 | 17.5 – 29.0 | 54.9 | 49.2 – 60.6 | 37.3 | 30.1 – 44.5 | 6.4 | 3.7 – 9.1 | 8.9 | 4.5 – 13.3 | 6.8 | 4.9 – 8.7 | – | 74.4§ | 66.3 – 82.4 | 56.3§ | 49.5 – 63.0 | 36.4§ | 27.3 – 45.6 | 74.9 | 67.5 – 82.3 | 20.5 | 10.7 – 30.4 | 41.3§ | 19.0 – 63.6 | 20.3 | 11.5 –29.1 | 31.4 | 24.7 – 38.1 | 72.8§ | 62.4 – 83.3 | 95.3§ | 89.2 – 100.0 | ||
| 2010–2014 | 13.7 | 3.8 – 23.6 | 30.0 | 22.9 – 37.0 | 55.9 | 46.1 – 65.8 | 58.0 | 46.6 – 69.4 | 9.6 | 3.9 – 15.2 | 19.0 | 12.0 – 26.0 | 10.1 | 7.1 – 13.2 | – | 65.0§ | 52.1 – 78.0 | 57.1§ | 48.3 – 65.9 | 46.8§ | 34.5 – 59.0 | 87.7 | 80.8 – 94.5 | 28.3 | 14.7 – 42.0 | 63.4§ | 45.7 – 81.2 | 29.6 | 21.2 – 38.0 | 51.3 | 39.6 – 63.1 | 82.3§ | 72.0 – 92.5 | 85.0§ | 66.2 – 100.0 | ||
|
| |||||||||||||||||||||||||||||||||||||
| Mongolia* | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | 76.7 | 60.0 – 93.4 | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | 76.1 | 63.8 – 88.4 | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Qatar* | 2000–2004 | 36.1§ | 10.3 – 61.9 | 15.0§ | 2.0 – 28.0 | 62.1§ | 50.1 – 74.1 | 67.8§ | 48.7 – 86.9 | 7.1§ | 2.6 – 11.5 | 9.9§ | 0.0 – 21.2 | 7.4§ | 0.8 – 14.1 | 77.5§ | 48.0 – 100.0 | 59.2§ | 48.7 – 69.7 | 83.9§ | 68.5 – 99.2 | 47.1§ | 25.1 – 69.0 | 81.5§ | 60.7 – 100.0 | 52.9§ | 34.0 – 71.9 | 11.1§ | 0.0 – 27.1 | 63.8§ | 49.8 – 77.7 | 46.5§ | 34.5 – 58.4 | 67.3§ | 44.3 – 90.3 | 69.0§ | 52.6 – 85.4 |
| 2005–2009 | 33.4§ | 9.4 – 57.5 | 22.0§ | 12.2 – 31.7 | 64.3§ | 47.6 – 80.9 | 60.5§ | 46.7 – 74.3 | 10.3§ | 3.2 – 17.3 | 4.2§ | 0.0 – 10.4 | 14.3§ | 7.4 – 21.2 | 30.1§ | 0.0 – 65.3 | 73.3§ | 63.0 – 83.7 | 55.6§ | 35.3 – 76.0 | 62.6§ | 47.5 – 77.6 | 98.2§ | 87.1 – 100.0 | 32.4§ | 19.0 – 45.8 | – | 52.1§ | 39.7 – 64.6 | 60.3§ | 45.9 – 74.7 | 82.6§ | 61.2 – 100.0 | 88.5§ | 73.8 – 100.0 | ||
| 2010–2014 | 42.2§ | 9.4 – 75.0 | 17.5§ | 9.7 – 25.3 | 63.5§ | 51.7 – 75.2 | 43.6§ | 31.2 – 56.1 | 27.2§ | 12.9 – 41.5 | 16.6§ | 7.2 – 26.1 | 17.2§ | 10.3 – 24.2 | 99.7§ | 84.7 – 100.0 | 71.9§ | 58.4 – 85.5 | 63.5§ | 44.2 – 82.8 | 39.2§ | 26.3 – 52.1 | 89.6§ | 79.0 – 100.0 | 36.1§ | 20.5 – 51.7 | 65.5§ | 34.5 – 96.5 | 56.9§ | 42.0 – 71.9 | 75.0§ | 58.8 – 91.2 | 100.0§ | 100.0 – 100.0 | 95.3§ | 87.3 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Singapore* | 2000–2004 | 9.0 | 6.2 – 11.8 | 25.4 | 23.3 – 27.4 | 56.1 | 54.4 – 57.8 | 51.4 | 48.5 – 54.2 | 13.2 | 11.6 – 14.9 | 5.3 | 3.6 – 7.0 | 10.3 | 9.4 – 11.2 | 62.8 | 51.0 – 74.6 | 76.3 | 73.9 – 78.7 | 68.3 | 65.2 – 71.5 | 42.5 | 37.9 – 47.0 | 83.4 | 80.3 – 86.5 | 26.2 | 21.5 – 30.9 | 60.9 | 48.0 – 73.8 | 39.2 | 35.1 – 43.3 | 46.0 | 43.0 – 48.9 | 79.8 | 72.3 – 87.2 | 86.9 | 77.5 – 96.3 |
| 2005–2009 | 10.5 | 7.4 – 13.5 | 27.1 | 25.0 – 29.2 | 60.3 | 58.7 – 61.8 | 59.0 | 56.3 – 61.8 | 20.4 | 18.6 – 22.2 | 6.7 | 5.1 – 8.3 | 13.0 | 12.0 – 13.9 | 59.0 | 50.5 – 67.5 | 80.3 | 78.3 – 82.3 | 63.3 | 60.1 – 66.6 | 46.8 | 42.8 – 50.7 | 86.7 | 84.5 – 88.9 | 30.3 | 26.2 – 34.4 | 57.5 | 45.9 – 69.0 | 43.7 | 40.1 – 47.4 | 55.3 | 52.7 – 57.9 | 90.4 | 84.2 – 96.6 | 73.8 | 61.6 – 86.0 | |
| 2010–2014 | 14.8 | 11.1 – 18.4 | 30.3 | 28.2 – 32.4 | 61.7 | 60.2 – 63.2 | 60.5 | 58.0 – 63.0 | 24.7 | 22.8 – 26.6 | 9.4 | 7.6 – 11.2 | 15.5 | 14.5 – 16.5 | 60.0 | 51.7 – 68.2 | 80.3 | 78.4 – 82.2 | 63.4 | 60.2 – 66.6 | 43.9 | 40.7 – 47.0 | 87.8 | 85.8 – 89.8 | 34.4 | 30.6 – 38.2 | 62.0 | 51.4 – 72.5 | 44.1 | 41.1 – 47.1 | 58.7 | 56.4 – 61.1 | 88.6 | 81.8 – 95.4 | 92.1 | 85.2 – 99.1 | |
|
| |||||||||||||||||||||||||||||||||||||
| Taiwan* | 2000–2004 | 13.0 | 12.0 – 13.9 | 35.6 | 34.8 – 36.4 | 56.8 | 56.0 – 57.5 | 57.7 | 56.8 – 58.7 | 19.5 | 19.1 – 19.9 | 7.0 | 6.3 – 7.7 | 11.6 | 11.2 –12.0 | 48.6 | 44.6 – 52.6 | 80.2 | 78.9 – 81.6 | 74.3 | 73.4 – 75.2 | 44.1 | 41.8 – 46.4 | 75.5 | 73.8 – 77.2 | 26.5 | 24.8 – 28.1 | 57.1 | 52.4 – 61.8 | 23.1 | 21.6 – 24.6 | 40.3 | 39.2 – 41.4 | 72.1 | 68.2 – 75.9 | 80.1 | 75.6 – 84.7 |
| 2005–2009 | 13.2 | 12.3 – 14.1 | 36.7 | 35.9 – 37.5 | 60.4 | 59.8 – 61.0 | 61.5 | 60.6 – 62.3 | 24.4 | 24.0 – 24.8 | 6.5 | 5.9 – 7.1 | 16.0 | 15.6 – 16.4 | 53.3 | 49.7 – 56.9 | 82.2 | 81.2 – 83.2 | 73.2 | 72.2 – 74.2 | 47.5 | 45.5 – 49.5 | 79.8 | 78.7 – 81.0 | 27.6 | 26.0 – 29.2 | 58.8 | 54.1 – 63.5 | 30.4 | 29.1 – 31.7 | 46.8 | 45.8 – 47.8 | 78.8 | 75.3 – 82.3 | 84.0 | 79.6 – 88.4 | |
| 2010–2014 | 15.5 | 14.6 – 16.4 | 38.6 | 37.8 – 39.4 | 62.6 | 62.0 – 63.1 | 62.5 | 61.7 – 63.3 | 27.9 | 27.5 – 28.4 | 7.7 | 7.0 – 8.3 | 20.6 | 20.2 – 21.0 | 52.1 | 48.5 – 55.6 | 84.2 | 83.3 – 85.1 | 70.0 | 68.9 – 71.1 | 48.8 | 46.9 – 50.8 | 83.0 | 81.9 – 84.0 | 28.4 | 26.9 – 29.9 | 54.8 | 49.9 – 59.6 | 33.4 | 32.2 – 34.6 | 50.5 | 49.6 – 51.5 | 76.5 | 72.8 – 80.1 | 86.7 | 82.5 – 90.8 | |
|
| |||||||||||||||||||||||||||||||||||||
| Thailand (6 registries) | 2000–2004 | 8.8§ | 6.6 – 11.1 | 22.3§ | 18.7 – 25.8 | 39.8§ | 37.2 – 42.5 | 43.0§ | 38.5 – 47.4 | 7.7§ | 6.9 – 8.6 | 6.9§ | 5.1 – 8.7 | 10.2§ | 9.3 – 11.1 | 44.7§ | 34.4 – 55.0 | 56.6§ | 52.0 – 61.3 | 53.5§ | 51.3 – 55.7 | 41.8§ | 34.8 – 48.7 | 52.1§ | 46.6 – 57.6 | 11.7§ | 9.2 – 14.3 | 23.4§ | 15.2 – 31.5 | 9.4§ | 7.2 – 11.6 | 30.3§ | 26.7 – 34.0 | 54.5§ | 46.7 – 62.4 | 43.9§ | 27.1 – 60.8 |
| 2005–2009 | 7.8 | 5.9 – 9.7 | 16.1 | 13.9 – 18.3 | 42.8 | 41.1 – 44.6 | 38.6 | 36.0 – 41.1 | 7.9 | 7.3 – 8.6 | 9.6 | 7.7 – 11.5 | 10.3 | 9.6 – 11.1 | 37.9§ | 30.6 – 45.2 | 64.8§ | 62.5 – 67.0 | 55.8§ | 54.0 – 57.7 | 35.8 | 32.3 – 39.3 | 71.8 | 69.0 – 74.7 | 17.6 | 15.2 – 20.0 | 38.4 | 30.6 – 46.3 | 18.2 | 16.0 – 20.4 | 36.1 | 33.7 – 38.4 | 60.6 | 54.2 – 67.1 | 63.7§ | 52.3 – 75.0 | |
| 2010–2014 | 7.1 | 5.1 – 9.1 | 12.5 | 10.7 – 14.3 | 47.0 | 45.2 – 48.8 | 44.4 | 41.8 – 47.1 | 6.9 | 6.3 – 7.5 | 6.8 | 5.3 – 8.2 | 8.6 | 7.9 – 9.2 | 29.9§ | 23.7 – 36.1 | 68.7§ | 66.6 – 70.8 | 53.9§ | 52.1 – 55.8 | 37.2 | 34.0 – 40.5 | 68.0 | 65.2 – 70.8 | 14.7 | 12.6 – 16.9 | 44.5§ | 35.9 – 53.1 | 25.4 | 22.8 – 28.0 | 35.0 | 32.8 – 37.1 | 65.9§ | 59.2 – 72.6 | 73.9§ | 65.0 – 82.7 | |
|
| |||||||||||||||||||||||||||||||||||||
| Turkey | 2000–2004 | 14.8§ | 9.2 – 20.4 | 21.9§ | 18.5 – 25.4 | 52.9§ | 49.1 – 56.7 | 48.5 | 43.9 – 53.0 | 20.1§ | 15.0 – 25.2 | 10.9§ | 7.8 – 14.1 | 11.9§ | 10.6 – 13.3 | 60.9§ | 53.2 – 68.6 | 84.8 | 81.5 – 88.0 | 64.8 | 59.7 – 69.9 | 46.1§ | 38.3 – 53.8 | 83.4§ | 79.3 – 87.5 | 32.1§ | 27.9 – 36.2 | 56.8 | 46.3 – 67.2 | 35.9§ | 30.6 – 41.2 | 54.3§ | 49.6 – 58.9 | 72.4 | 64.3 – 80.6 | 79.9 | 70.9 – 88.9 |
| (9 registries) | 2005–2009 | 14.7 | 12.9 – 16.5 | 21.4 | 20.3 – 22.4 | 52.7 | 51.3 – 54.2 | 49.3 | 47.3 – 51.3 | 14.9 | 12.9 – 17.0 | 9.5 | 8.4 – 10.7 | 12.7 | 12.2 – 13.2 | 57.7 | 54.6 – 60.9 | 80.6 | 79.2 – 82.1 | 59.2 | 56.5 – 61.9 | 40.0 | 37.4 – 42.6 | 81.2 | 79.9 – 82.6 | 34.0 | 32.4 – 35.6 | 61.1 | 56.2 – 66.0 | 49.0 | 46.8 – 51.2 | 50.3 | 48.7 – 51.8 | 78.7 | 74.9 – 82.6 | 85.0 | 81.4 – 88.7 |
| 2010–2014 | 19.0 | 16.9 – 21.1 | 24.6 | 23.6 – 25.6 | 55.2 | 53.8 – 56.6 | 52.6 | 50.6 – 54.5 | 15.9 | 14.0 – 17.8 | 10.4 | 9.3 – 11.5 | 14.9 | 14.3 – 15.4 | 60.7 | 57.6 – 63.7 | 82.1 | 80.7 – 83.5 | 60.7 | 58.1 – 63.3 | 39.7 | 37.3 – 42.0 | 83.8 | 82.5 – 85.1 | 35.6 | 34.1 – 37.0 | 62.5 | 58.4 – 66.7 | 54.0 | 51.8 – 56.1 | 54.5 | 53.0 – 56.1 | 80.9 | 77.2 – 84.6 | 82.9 | 79.1 – 86.7 | |
|
EUROPE | |||||||||||||||||||||||||||||||||||||
| Austria* | |||||||||||||||||||||||||||||||||||||
| 2000–2004 | 16.2 | 14.2 – 18.3 | 30.0 | 28.7 – 31.3 | 60.7 | 59.7 – 61.7 | 60.2 | 58.9 – 61.5 | 11.2 | 10.0 – 12.4 | 6.7§ | 5.9 – 7.5 | 15.4 | 14.8 – 16.0 | 83.4 | 82.2 – 84.7 | 81.7 | 80.9 – 82.4 | 65.4 | 63.4 – 67.4 | 40.9 | 39.4 – 42.5 | 90.1 | 89.3 – 90.8 | 24.2 | 22.6 – 25.9 | – | 25.0 | 23.1 – 26.8 | 57.6 | 56.5 – 58.7 | – | – | ||||
| 2005–2009 | 16.8 | 15.0 – 18.7 | 34.2 | 32.9 – 35.6 | 63.5 | 62.5 – 64.4 | 63.5 | 62.2 – 64.8 | 14.2§ | 12.9 – 15.6 | 8.5 | 7.7 – 9.4 | 18.0 | 17.4 – 18.6 | 84.6 | 83.5 – 85.8 | 83.9 | 83.2 – 84.6 | 66.0 | 63.7 – 68.2 | 41.2 | 39.6 – 42.8 | 90.8 | 90.1 – 91.5 | 28.5 | 26.9 – 30.1 | – | 29.6 | 27.7 – 31.5 | 62.2 | 61.1 – 63.3 | – | – | ||||
| 2010–2014 | 18.6 | 16.6 – 20.6 | 35.4 | 34.0 – 36.9 | 63.7 | 62.7 – 64.7 | 64.2 | 62.9 – 65.6 | 14.8§ | 13.4 – 16.2 | 10.5§ | 9.5 – 11.4 | 19.7 | 19.1 – 20.4 | 87.8 | 86.7 – 88.8 | 84.8 | 84.1 – 85.5 | 63.9 | 61.6 – 66.2 | 41.0 | 39.4 – 42.7 | 90.2 | 89.5 – 90.9 | 26.3 | 24.7 – 27.9 | – | 32.0 | 30.1 – 34.0 | 63.3 | 62.3 – 64.4 | – | – | ||||
|
| |||||||||||||||||||||||||||||||||||||
| Belarus (Childhood)† | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | 66.1 | 59.8 – 72.3 | – | – | 78.5 | 73.0 – 83.9 | 86.5 | 80.7 – 92.3 | |||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | – | – | – | – | – | 70.4 | 64.0 – 76.8 | – | – | 87.0 | 81.9 – 92.2 | 84.6 | 77.0 – 92.2 | ||||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | – | – | – | – | – | 68.5 | 61.6 – 75.5 | – | – | 86.6 | 81.7 – 91.5 | 85.2 | 78.0 – 92.4 | ||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Belgium* | 2000–2004 | 16.6 | 13.8 – 19.4 | 29.3 | 26.4 – 32.2 | 64.3 | 62.7 – 66.0 | 62.9 | 60.4 – 65.4 | 21.3 | 16.8 – 25.8 | 8.9 | 6.9 – 10.8 | 15.4 | 14.4 – 16.4 | 86.3 | 83.9 – 88.7 | 84.8 | 83.5 – 86.0 | 65.1 | 61.1 – 69.0 | 42.7 | 39.4 – 45.9 | 92.1 | 90.8 – 93.4 | 31.5 | 28.5 – 34.5 | 84.1 | 75.6 – 92.6 | 49.7 | 46.7 – 52.7 | 65.5 | 63.6 – 67.4 | 80.4 | 69.8 – 91.0 | 94.2 | 87.9 – 100.0 |
| 2005–2009 | 23.2 | 21.7 – 24.7 | 35.8 | 34.4 – 37.1 | 65.0 | 64.3 – 65.7 | 65.3 | 64.3 – 66.4 | 20.6 | 19.0 – 22.3 | 10.5 | 9.6 – 11.4 | 17.0 | 16.5 – 17.4 | 88.9 | 87.9 – 89.8 | 85.3 | 84.7 – 85.8 | 65.7 | 63.8 – 67.6 | 42.8 | 41.3 – 44.3 | 93.2 | 92.6 – 93.7 | 31.9 | 30.6 – 33.2 | 75.2 | 70.3 – 80.1 | 53.2 | 51.9 – 54.5 | 68.0 | 67.2 – 68.8 | 90.5 | 87.0 – 94.1 | 95.6 | 92.9 – 98.2 | |
| 2010–2014 | 23.6 | 22.1 – 25.0 | 37.5 | 36.2 – 38.9 | 67.9 | 67.2 – 68.6 | 66.6 | 65.6 – 67.6 | 20.7 | 19.2 – 22.2 | 12.4 | 11.4 –13.3 | 18.2 | 17.7 – 18.6 | 91.0 | 90.1 – 91.8 | 86.4 | 85.9 – 86.9 | 65.4 | 63.5 – 67.2 | 43.1 | 41.6 – 44.6 | 93.8 | 93.2 – 94.3 | 31.2 | 29.9 – 32.5 | 74.5 | 70.2 – 78.9 | 55.4 | 54.2 – 56.5 | 70.6 | 69.8 – 71.4 | 90.8 | 87.3 – 94.3 | 95.4 | 92.7 – 98.1 | |
|
| |||||||||||||||||||||||||||||||||||||
| Bulgaria* | 2000–2004 | – | 11.2§ | 10.3 – 12.0 | 43.9 | 42.7 – 45.2 | 37.0 | 35.6 – 38.4 | 4.0§ | 2.9 – 5.1 | – | 5.8 | 5.3 – 6.3 | 50.8 | 47.9 – 53.8 | 70.9 | 69.7 – 72.1 | 49.2 | 47.6 – 50.7 | 32.9 | 30.9 – 34.9 | 49.4 | 47.1 – 51.7 | – | – | 29.9§ | 27.2 – 32.6 | 38.1 | 36.1 – 40.0 | 63.5 | 55.5 – 71.5 | 70.7 | 62.2 – 79.2 | ||||
| 2005–2009 | – | 13.9 | 13.0 – 14.9 | 48.5 | 47.4 – 49.6 | 42.1 | 40.7 – 43.5 | 4.6§ | 3.5 – 5.6 | – | 7.0 | 6.5 – 7.6 | 56.0 | 53.3 – 58.6 | 75.9 | 74.8 – 77.0 | 53.2 | 51.7 – 54.7 | 33.9 | 32.2 – 35.5 | 54.8 | 52.7 – 56.9 | – | – | 40.1 | 37.6 – 42.6 | 39.9 | 38.1 – 41.6 | 74.8 | 68.4 – 81.1 | 74.3 | 64.9 – 83.7 | |||||
| 2010–2014 | – | 16.0 | 14.9 – 17.0 | 52.4 | 51.3 – 53.6 | 45.9 | 44.4 – 47.4 | 6.5§ | 5.1 – 7.9 | – | 7.7 | 7.1 – 8.2 | 61.2 | 58.8 – 63.7 | 78.3 | 77.2 – 79.4 | 54.8 | 53.3 – 56.3 | 37.3 | 35.4 – 39.1 | 68.3 | 66.2 – 70.5 | – | – | 41.6§ | 39.2 – 44.1 | 43.5 | 41.8 – 45.2 | 78.3 | 71.7 – 84.9 | 87.7 | 80.6 – 94.9 | |||||
|
| |||||||||||||||||||||||||||||||||||||
| Croatia* | 2000–2004 | 6.8 | 4.9 – 8.7 | 19.7 | 18.4 – 20.9 | 47.3 | 45.9 – 48.7 | 44.4 | 42.7 – 46.1 | 9.2§ | 7.6 – 10.7 | 9.1 | 7.9 – 10.4 | 11.2 | 10.5 – 11.9 | 66.4 | 64.0 – 68.8 | 73.6 | 72.2 – 75.0 | 63.2 | 60.6 – 65.8 | 36.9 | 34.6 – 39.2 | 65.7 | 63.6 – 67.9 | 37.0 | 35.1 – 38.8 | 65.7 | 58.3 – 73.1 | 31.1 | 28.6 – 33.6 | 42.7 | 41.0 – 44.4 | 81.7 | 74.3 – 89.1 | 76.6 | 66.8 – 86.3 |
| 2005–2009 | 9.1 | 6.9 – 11.2 | 18.9 | 17.6 – 20.2 | 49.5 | 48.2 – 50.8 | 47.1 | 45.5 – 48.7 | 9.2§ | 7.7 – 10.8 | 8.2 | 7.0 – 9.4 | 10.6 | 10.0 – 11.3 | 74.7 | 72.7 – 76.7 | 78.2 | 77.0 – 79.4 | 64.3 | 61.9 – 66.7 | 33.4 | 31.3 – 35.5 | 78.3 | 76.7 – 79.9 | 39.6 | 37.8 – 41.5 | 75.2 | 67.9 – 82.5 | 29.2 | 26.8 – 31.6 | 51.0 | 49.3 – 52.6 | 86.7 | 81.1 – 92.3 | 84.6 | 76.2 – 93.0 | |
| 2010–2014 | 8.7 | 6.6 – 10.8 | 20.0 | 18.6 – 21.3 | 51.1 | 49.9 – 52.4 | 48.2 | 46.5 – 49.8 | 9.3§ | 7.7 – 10.9 | 8.4§ | 7.1 – 9.7 | 10.0 | 9.3 – 10.6 | 77.2 | 75.3 – 79.1 | 78.6 | 77.4 – 79.7 | 63.2 | 60.8 – 65.6 | 36.0 | 33.9 – 38.2 | 80.9 | 79.3 – 82.4 | 42.2 | 40.4 – 44.0 | 73.4 | 65.6 – 81.3 | 32.2 | 29.7 – 34.7 | 52.7 | 51.1 – 54.3 | 85.2 | 79.1 – 91.3 | 94.5 | 89.1 – 99.9 | |
|
| |||||||||||||||||||||||||||||||||||||
| Czech Republic* | 2000–2004 | 7.3 | 6.0 – 8.6 | 18.7 | 17.7 – 19.7 | 48.0 | 47.3 – 48.8 | 43.8 | 42.6 – 44.9 | 3.0 | 2.3 – 3.6 | 3.6 | 3.0 – 4.1 | 8.6 | 8.2 – 9.0 | 80.7 | 79.5 – 81.8 | 75.7 | 74.8 – 76.5 | 60.4 | 58.9 – 61.9 | 34.3 | 33.0 – 35.5 | 71.0 | 69.9 – 72.2 | 19.5 | 18.2 – 20.8 | 55.6 | 47.9 – 63.3 | 19.9 | 18.2 – 21.7 | 49.9 | 48.8 – 51.0 | 88.0 | 82.9 – 93.1 | 89.0 | 82.7 – 95.3 |
| 2005–2009 | 9.0 | 7.5 – 10.5 | 19.3 | 18.3 – 20.3 | 52.0 | 51.3 – 52.7 | 47.9 | 46.8 – 49.0 | 5.3 | 4.5 – 6.2 | 4.7 | 4.1 – 5.3 | 9.8 | 9.4 – 10.3 | 84.6 | 83.7 – 85.6 | 79.1 | 78.4 – 79.9 | 62.7 | 61.2 – 64.1 | 35.3 | 34.0 – 36.5 | 81.5 | 80.7 – 82.3 | 22.1 | 20.8 – 23.4 | 64.3 | 57.4 – 71.3 | 33.5 | 31.8 – 35.1 | 53.2 | 52.2 – 54.3 | 90.3 | 85.6 – 95.0 | 82.9 | 73.2 – 92.5 | |
| 2010–2014 | 9.8 | 8.3 – 11.4 | 20.6 | 19.6 – 21.6 | 56.1 | 55.4 – 56.9 | 52.3 | 51.2 – 53.4 | 6.7 | 5.6 – 7.7 | 6.1 | 5.4 – 6.7 | 10.6 | 10.2 – 11.1 | 85.7 | 84.8 – 86.6 | 81.4 | 80.7 – 82.1 | 61.0 | 59.5 – 62.4 | 36.5 | 35.2 – 37.8 | 85.3 | 84.6 – 86.0 | 21.4 | 20.1 – 22.7 | 69.7 | 63.2 – 76.2 | 36.8 | 35.2 – 38.5 | 57.2 | 56.1 – 58.2 | 88.2 | 82.1 – 94.3 | 89.6 | 82.5 – 96.6 | |
|
| |||||||||||||||||||||||||||||||||||||
| Denmark* | 2000–2004 | 8.4 | 6.9 – 9.8 | 14.7 | 13.2 – 16.3 | 51.5 | 50.4 – 52.6 | 53.2 | 51.7 – 54.7 | 4.4 | 3.1 – 5.8 | 3.8 | 3.0 – 4.5 | 9.5 | 9.0 – 10.1 | 87.3 | 86.0 – 88.5 | 80.3 | 79.4 – 81.2 | 63.0 | 60.6 – 65.4 | 33.1 | 31.4 – 34.8 | 63.6 | 62.1 – 65.1 | 30.5 | 28.8 – 32.2 | 68.8 | 62.1 – 75.5 | 35.7 | 33.6 – 37.8 | 57.7 | 56.4 – 59.0 | 84.3 | 78.6 – 90.0 | 90.2 | 82.2 – 98.2 |
| 2005–2009 | 10.4 | 8.9 – 11.9 | 15.4 | 13.9 – 16.9 | 56.5 | 55.5 – 57.6 | 59.8 | 58.4 – 61.1 | 5.6 | 4.2 – 7.0 | 5.6 | 4.7 – 6.4 | 12.3 | 11.7 –12.8 | 89.1 | 88.1 – 90.0 | 84.0 | 83.2 – 84.8 | 66.7 | 64.3 – 69.1 | 37.4 | 35.7 – 39.2 | 82.5 | 81.6 – 83.4 | 35.1 | 33.4 – 36.7 | 79.4 | 72.9 – 85.8 | 45.0 | 43.0 – 47.0 | 66.9 | 65.7 – 68.0 | 93.1 | 88.4 – 97.7 | 90.0 | 83.1 – 97.0 | |
| 2010–2014 | 13.7 | 12.0 – 15.4 | 19.9 | 18.1 – 21.6 | 61.6 | 60.6 – 62.7 | 64.8 | 63.4 – 66.1 | 7.5 | 5.9 – 9.1 | 8.0 | 7.0 – 9.1 | 16.6 | 16.0 – 17.3 | 91.1 | 90.2 – 91.9 | 86.1 | 85.4 – 86.9 | 69.5 | 67.0 – 72.0 | 39.7 | 37.8 – 41.6 | 85.6 | 84.7 – 86.4 | 38.9 | 37.3 – 40.6 | 79.5 | 73.3 – 85.6 | 47.6 | 45.7 – 49.6 | 70.9 | 69.8 – 72.1 | 94.0 | 90.1 – 97.9 | 93.8 | 89.0 – 98.7 | |
|
| |||||||||||||||||||||||||||||||||||||
| Estonia* | 2000–2004 | 5.7 | 2.8 – 8.6 | 22.3 | 20.2 – 24.4 | 48.9 | 46.2 – 51.5 | 46.4 | 42.9 – 49.9 | 5.5§ | 2.8 – 8.3 | 4.8 | 3.2 – 6.5 | 10.8 | 9.5 – 12.2 | 71.4 | 67.0 – 75.8 | 70.9 | 68.2 – 73.6 | 62.3 | 58.5 – 66.1 | 31.2 | 27.7 – 34.6 | 67.9 | 64.5 – 71.3 | 25.2 | 21.4 – 29.0 | 81.2 | 69.9 – 92.5 | 36.6 | 31.6 – 41.6 | 48.8 | 45.6 – 52.0 | 63.7 | 51.0 – 76.4 | 88.3 | 73.4 – 100.0 |
| 2005–2009 | 6.0 | 3.5 – 8.5 | 24.2 | 22.1 – 26.4 | 53.8 | 51.3 – 56.3 | 50.5 | 46.9 – 54.1 | 6.5 | 3.9 – 9.2 | 5.4 | 3.8 – 7.0 | 14.3 | 12.6 – 15.9 | 75.2 | 71.7 – 78.8 | 75.4 | 73.1 – 77.6 | 66.9 | 63.4 – 70.4 | 37.2 | 33.8 – 40.7 | 83.2 | 80.9 – 85.6 | 26.1 | 22.6 – 29.6 | 72.3 | 57.9 – 86.7 | 42.4 | 38.1 – 46.8 | 53.5 | 50.6 – 56.4 | 85.4 | 73.6 – 97.1 | 85.8 | 68.1 – 100.0 | |
| 2010–2014 | 5.4 | 2.3 – 8.5 | 29.2 | 26.1 – 32.3 | 58.4 | 55.2 – 61.6 | 54.8 | 50.1 – 59.5 | 4.2 | 1.8 –6.6 | 10.2 | 7.0 – 13.4 | 16.9 | 14.9 – 19.0 | 81.8 | 77.6 – 86.0 | 76.6 | 73.8 – 79.3 | 66.5 | 62.2 – 70.7 | 42.3 | 37.4 – 47.1 | 86.3 | 83.5 – 89.0 | 31.0 | 26.1 – 36.0 | 64.5 | 47.3 – 81.8 | 37.8 | 32.1 – 43.5 | 53.8 | 50.2 – 57.4 | 87.7 | 76.4 – 98.9 | 88.0 | 73.1 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Finland* | 2000–2004 | 11.8 | 9.5 – 14.1 | 26.0 | 24.3 – 27.6 | 61.3 | 59.9 – 62.8 | 59.9 | 58.0 – 61.9 | 7.1 | 5.5 – 8.8 | 4.1 | 3.2 – 4.9 | 11.9 | 11.0 –12.7 | 84.8 | 83.3 – 86.4 | 86.5 | 85.5 – 87.5 | 67.8 | 64.3 – 71.3 | 41.2 | 39.2 – 43.1 | 90.0 | 89.1 – 90.9 | 35.4 | 33.5 – 37.4 | 78.5 | 72.5 – 84.6 | 40.1§ | 37.4 – 42.8 | 56.8 | 55.5 – 58.1 | 84.7 | 78.0 – 91.4 | 90.5 | 84.3 – 96.7 |
| 2005–2009 | 12.8 | 10.6 – 15.0 | 25.1 | 23.4 – 26.8 | 63.2 | 61.9 – 64.5 | 63.8 | 62.0 – 65.6 | 9.1§ | 7.3 – 10.8 | 7.3 | 6.2 – 8.5 | 12.1 | 11.3 –13.0 | 87.4 | 86.2 – 88.6 | 87.7 | 86.9 – 88.5 | 65.2 | 61.4 – 69.0 | 44.2 | 42.2 – 46.2 | 93.4 | 92.6 – 94.1 | 35.8 | 34.0 – 37.6 | 78.0 | 71.5 – 84.5 | 41.6§ | 39.2 – 44.0 | 62.5 | 61.2 – 63.7 | 88.1 | 83.2 – 92.9 | 92.0 | 84.5 – 99.6 | |
| 2010–2014 | 12.4 | 10.5 – 14.4 | 25.7 | 23.9 – 27.5 | 64.9 | 63.7 – 66.2 | 64.4 | 62.6 – 66.1 | 10.4§ | 8.5 – 12.2 | 7.4§ | 6.3 – 8.4 | 13.0 | 12.1 – 13.9 | 88.7 | 87.6 – 89.8 | 88.5 | 87.7 – 89.3 | 67.4 | 63.8 – 71.1 | 41.1 | 39.2 – 43.0 | 93.2 | 92.4 – 93.9 | 37.6 | 35.7 – 39.4 | 75.6 | 69.0 – 82.2 | 47.2§ | 44.7 – 49.6 | 64.4 | 63.2 – 65.5 | 95.2 | 91.5 – 98.9 | 91.2 | 84.3 – 98.1 | |
|
| |||||||||||||||||||||||||||||||||||||
| France† (23 registries) | 2000–2004 | 13.0 | 11.8 –14.2 | 26.3 | 24.9 – 27.7 | 60.7 | 59.8 – 61.5 | 58.3 | 56.9 – 59.6 | 14.0 | 12.9 – 15.1 | 7.8 | 6.9 – 8.7 | 14.1 | 13.5 – 14.6 | 89.7 | 88.5 – 90.9 | 86.8 | 86.1 – 87.4 | 61.7 | 59.4 – 64.0 | 41.6 | 39.8 – 43.3 | 90.1 | 89.4 – 90.8 | 21.8 | 20.3 – 23.3 | 67.2 | 65.0 – 69.5 | 53.3 | 51.9 – 54.7 | 64.4 | 63.6 – 65.3 | 88.1 | 86.4 – 89.8 | 92.7 | 90.8 – 94.6 |
| 2005–2009 | 14.9 | 13.6 – 16.1 | 27.1 | 25.8 – 28.4 | 63.6 | 62.8 – 64.3 | 60.7 | 59.5 – 61.9 | 16.5 | 15.4 – 17.6 | 9.0 | 8.2 – 9.8 | 16.2 | 15.7 – 16.7 | 90.9 | 89.9 – 91.9 | 87.2 | 86.6 – 87.8 | 62.1 | 60.0 – 64.2 | 42.1 | 40.4 – 43.7 | 93.6 | 93.1 – 94.1 | 27.2 | 25.8 – 28.7 | 70.8 | 68.6 – 73.0 | 54.6 | 53.3 – 55.8 | 69.9 | 69.1 – 70.7 | 90.0 | 88.4 – 91.6 | 92.6 | 90.6 – 94.6 | |
| 2010–2014 | 13.9 | 11.4 –16.4 | 26.7 | 23.9 – 29.6 | 63.7 | 62.2 – 65.3 | 60.9 | 58.4 – 63.4 | 18.3 | 16.0 – 20.5 | 8.6 | 7.0 – 10.2 | 17.3 | 16.1 – 18.5 | 90.8 | 88.7 – 92.9 | 86.7 | 85.5 – 88.0 | 65.0 | 60.3 – 69.7 | 43.5 | 40.0 – 46.9 | 93.1 | 91.9 – 94.2 | 27.2 | 24.2 – 30.3 | 70.8 | 68.1 – 73.5 | 57.5 | 54.9 – 60.1 | 69.6 | 67.9 – 71.3 | 88.6 | 86.5 – 90.8 | 94.2 | 92.0 – 96.4 | |
|
| |||||||||||||||||||||||||||||||||||||
| Germany (10 registries) | 2000–2004 | 16.6 | 15.3 – 17.8 | 31.8 | 30.0 – 33.5 | 62.0 | 61.2 – 62.8 | 60.9 | 60.2 – 61.6 | 12.5§ | 11.6 –13.4 | 8.0§ | 7.5 – 8.6 | 14.9 | 14.3 – 15.4 | 91.0 | 90.4 – 91.6 | 83.9 | 83.4 – 84.4 | 64.9 | 63.8 – 66.1 | 40.8 | 39.3 – 42.2 | 90.4 | 89.9 – 90.9 | 29.1 | 24.8 – 33.3 | 63.1 | 56.0 – 70.2 | 46.0 | 43.9 – 48.1 | 61.2 | 60.4 – 62.0 | 94.0 | 90.7 – 97.3 | 90.4 | 84.2 – 96.5 |
| 2005–2009 | 19.7 | 18.8 – 20.6 | 31.4 | 30.8 – 32.0 | 64.9 | 64.4 – 65.3 | 62.2 | 61.6 – 62.8 | 12.9 | 11.3 –14.5 | 9.3 | 8.4 – 10.2 | 16.9 | 16.5 – 17.4 | 92.0 | 91.5 – 92.6 | 85.6 | 85.2 – 85.9 | 65.7 | 64.6 – 66.8 | 40.6 | 39.6 – 41.6 | 91.8 | 91.3 – 92.2 | 27.3 | 26.2 – 28.5 | 67.8 | 61.1 – 74.6 | 51.9 | 50.7 – 53.1 | 65.7 | 65.1 – 66.3 | 92.1 | 89.2 – 95.0 | 93.8 | 88.9 – 98.8 | |
| 2010–2014 | 20.8 | 19.8 – 21.8 | 33.5 | 32.8 – 34.2 | 64.8 | 64.3 – 65.3 | 62.3 | 61.6 – 62.9 | 13.0 | 10.5 – 15.5 | 10.7 | 9.6 – 11.8 | 18.3 | 17.9 – 18.8 | 93.1 | 92.6 – 93.6 | 86.0 | 85.7 – 86.4 | 65.2 | 64.0 – 66.4 | 41.2 | 40.2 – 42.2 | 91.6 | 91.2 – 92.0 | 29.6 | 28.3 – 30.9 | 69.5 | 61.8 – 77.2 | 54.9 | 53.5 – 56.3 | 67.9 | 67.3 – 68.6 | 91.1 | 87.4 – 94.8 | 96.9 | 94.2 – 99.6 | |
|
| |||||||||||||||||||||||||||||||||||||
| Gibraltar* | 2000–2004 | – | 8.0 | 0.0 – 19.9 | 38.8 | 17.7 – 59.9 | – | – | – | 21.7§ | 0.0 – 44.9 | 65.4 | 37.6 – 93.3 | 79.3§ | 66.5 – 92.1 | – | – | 62.5§ | 31.5 – 93.5 | – | – | – | – | – | – | ||||||||||||
| 2005–2009 | – | 39.2§ | 12.8 – 65.5 | 52.3§ | 24.3 – 80.4 | 39.3§ | 7.6 – 70.9 | – | 0.6§ | 0.0 – 1.9 | 19.6§ | 8.0 – 31.1 | 100.0§ | 88.5 – 100.0 | 72.1§ | 56.8 – 87.4 | – | – | 42.3§ | 9.1 – 75.6 | – | – | – | – | – | – | |||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Greek National Paediatric† | 2000–2004 | –– | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 80.3 | 75.3 – 85.4 | 89.2 | 82.6 – 95.8 | ||||||||||||||||
| 2005–2009 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 84.8 | 80.4 – 89.3 | 84.9 | 78.3 – 91.6 | |||||||||||||||||
| 2010–2014 | – | – | – | – | – | – | – | – | – | – | – | – | – | 68.9 | 60.3 – 77.4 | – | – | 84.2 | 80.0 – 88.3 | 87.5 | 81.5 – 93.5 | ||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||
| Iceland* | 2000–2004 | 13.1 | 3.8 – 22.4 | 32.9 | 24.9 – 40.9 | 61.4 | 55.4 – 67.4 | 71.0 | 63.0 – 79.0 | 3.9 | 0.0 – 10.0 | 4.8 | 1.4 –8.1 | 14.1 | 11.2 –16.9 | 84.5 | 77.7 – 91.3 | 87.4 | 82.9 – 91.8 | 81.8 | 72.8 – 90.8 | 39.6 | 30.9 – 48.3 | 80.1 | 75.5 – 84.7 | 24.1 | 19.5 – 28.6 | 80.0 | 56.6 – 100.0 | 48.2 | 38.3 – 58.1 | 66.6 | 60.4 – 72.8 | – | – | ||
| 2005–2009 | 19.1 | 10.4 – 27.8 | 30.3 | 21.9 – 38.6 | 64.0 | 58.8 – 69.1 | 66.3 | 58.2 – 74.5 | 16.0 | 6.0 – 26.1 | 0.0 | 0.0 – 0.1 | 16.0 | 12.9 – 19.1 | 85.4 | 79.5 – 91.3 | 85.8 | 81.4 – 90.2 | 87.6 | 79.5 – 95.7 | 40.9 | 31.3 – 50.5 | 89.7 | 86.5 – 92.9 | 21.0 | 14.3 – 27.6 | 73.4 | 51.8 – 94.9 | 47.9 | 39.7 – 56.1 | 67.9 | 62.6 – 73.1 | – | – | |||
| 2010–2014 | 17.7 | 10.5 – 24.8 | 28.1 | 20.2 – 36.1 | 68.2 | 63.2 – 73.1 | 63.0 | 55.5 – 70.5 | 14.3 | 6.9 – 21.7 | 0.0 | 0.0 – 0.0 | 20.2 | 16.9 – 23.4 | 87.5 | 82.1 – 92.9 | 89.1 | 85.1 – 93.1 | 80.1 | 71.2 – 89.1 | 40.3 | 31.2 – 49.4 | 90.8 | 87.7 – 93.9 | 29.2 | 20.8 – 37.7 | 90.1 | 72.4 – 100.0 | 43.4 | 35.8 – 50.9 | 71.5 | 66.3 – 76.6 | 92.4 | 78.4 – 100.0 | – | ||
|
| |||||||||||||||||||||||||||||||||||||
| Ireland* | 2000–2004 | 12.9 | 11.0 –14.7 | 18.6 | 16.7 – 20.4 | 53.3 | 51.8 – 54.7 | 51.1 | 48.9 – 53.2 | 11.6 | 8.7 – 14.6 | 5.7 | 4.4 – 7.0 | 10.1 | 9.3 – 10.9 | 85.5 | 83.6 – 87.4 | 77.2 | 75.8 – 78.5 | 57.8 | 54.1 – 61.6 | 29.4 | 27.2 – 31.7 | 83.7 | 82.5 – 84.9 | 26.9 | 24.9 – 29.0 | 67.8 | 60.0 – 75.6 | 47.6 | 44.9 – 50.2 | 55.4 | 53.8 – 57.0 | 82.9 | 76.6 – 89.2 | 97.4 | 94.6 – 100.0 |
| 2005–2009 | 17.2 | 15.2 – 19.1 | 22.2 | 20.4 – 24.1 | 58.4 | 57.1 – 59.7 | 57.1 | 55.0 – 59.1 | 11.8 | 9.4 – 14.2 | 6.9 | 5.6 – 8.2 | 13.5 | 12.7 – 14.3 | 86.6 | 85.1 – 88.1 | 81.4 | 80.2 – 82.6 | 58.7 | 55.5 – 61.9 | 31.2 | 28.9 – 33.4 | 89.7 | 88.7 – 90.7 | 30.8 | 28.7 – 33.0 | 68.6 | 61.1 – 76.1 | 52.5 | 50.1 – 55.0 | 64.2 | 62.7 – 65.7 | 87.1 | 80.9 – 93.4 | 96.2 | 92.0 – 100.0 | |
| 2010–2014 | 20.3 | 18.0 – 22.7 | 27.6 | 25.4 – 29.8 | 60.5 | 59.1 – 62.0 | 61.7 | 59.4 – 64.0 | 14.2 | 11.2 –17.2 | 9.6 | 7.9 – 11.4 | 17.5 | 16.5 – 18.5 | 89.2 | 87.7 – 90.7 | 82.0 | 80.7 – 83.3 | 63.6 | 60.1 – 67.2 | 32.8 | 30.3 – 35.3 | 91.1 | 90.1 – 92.2 | 34.5 | 32.0 – 36.9 | 74.0 | 66.4 – 81.5 | 53.1 | 50.5 – 55.8 | 66.9 | 65.3 – 68.5 | 88.3 | 82.4 – 94.3 | 95.3 | 89.6 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Italy (45 registries) | 2000–2004 | 11.5 | 10.5 – 12.6 | 31.6 | 30.9 – 32.2 | 59.0 | 58.6 – 59.5 | 55.8 | 54.9 – 56.6 | 15.9 | 15.2 – 16.5 | 6.8 | 6.3 – 7.3 | 14.0 | 13.7 – 14.3 | 84.1 | 83.3 – 84.8 | 84.2 | 83.8 – 84.5 | 67.3 | 66.0 – 68.7 | 37.7 | 36.8 – 38.6 | 87.2 | 86.7 – 87.7 | 24.1 | 23.2 – 25.1 | 68.5 | 64.5 – 72.5 | 46.4 | 45.5 – 47.3 | 58.5 | 57.9 – 59.0 | 82.6 | 79.2 – 86.0 | 88.3 | 84.9 – 91.8 |
| 2005–2009 | 12.9 | 11.9 –14.0 | 31.1 | 30.5 – 31.7 | 64.3 | 63.9 – 64.7 | 61.1 | 60.4 – 61.8 | 20.0 | 19.4 – 20.6 | 7.9 | 7.5 – 8.3 | 15.5 | 15.2 – 15.8 | 86.0 | 85.5 – 86.6 | 85.9 | 85.5 – 86.2 | 67.7 | 66.5 – 68.9 | 39.3 | 38.5 – 40.1 | 89.6 | 89.2 – 90.0 | 27.0 | 26.2 – 27.8 | 75.5 | 72.3 – 78.8 | 49.2 | 48.5 – 49.9 | 61.9 | 61.5 – 62.4 | 89.2 | 86.8 – 91.6 | 89.4 | 86.5 – 92.4 | |
| 2010–2014 | 13.8 | 12.3 – 15.3 | 30.5 | 29.7 – 31.3 | 64.2 | 63.6 – 64.7 | 61.3 | 60.3 – 62.2 | 20.3 | 19.6 – 21.1 | 9.2 | 8.5 – 9.8 | 15.9 | 15.5 – 16.3 | 85.7 | 85.0 – 86.5 | 86.0 | 85.5 – 86.4 | 66.8 | 65.1 – 68.5 | 39.4 | 38.3 – 40.5 | 89.5 | 89.0 – 89.9 | 28.8 | 27.8 – 29.9 | 74.8 | 70.4 – 79.2 | 49.2 | 48.2 – 50.2 | 62.6 | 61.9 – 63.2 | 87.8 | 84.4 – 91.2 | 91.6 | 87.4 – 95.7 | |
|
| |||||||||||||||||||||||||||||||||||||
| Latvia* | 2000–2004 | 6.9 | 3.4 – 10.3 | 24.2 | 22.2 – 26.3 | 50.5 | 47.8 – 53.3 | 39.4 | 36.3 – 42.5 | 12.0 | 3.8 – 20.3 | 8.8 | 5.4 – 12.1 | 17.3 | 15.3 – 19.3 | 66.3 | 62.0 – 70.6 | 79.7 | 77.1 – 82.2 | 52.8 | 49.0 – 56.6 | 40.3 | 36.6 – 44.0 | 69.9 | 66.5 – 73.3 | 22.2 | 18.8 – 25.7 | 79.7 | 67.1 – 92.2 | 22.2 | 18.7 – 25.7 | 59.8 | 54.9 – 64.8 | 80.5 | 70.0 – 91.0 | – | |
| 2005–2009 | 10.8 | 7.3 – 14.2 | 26.7 | 24.6 – 28.9 | 54.0 | 51.4 – 56.5 | 46.6 | 43.4 – 49.7 | 7.8 | 3.8 – 11.7 | 11.2 | 7.5 – 14.8 | 19.5 | 17.7 – 21.2 | 65.1 | 61.1 – 69.1 | 79.9 | 77.8 – 82.1 | 57.7 | 54.2 – 61.2 | 39.8 | 36.5 – 43.1 | 88.8 | 86.0 – 91.6 | 23.9 | 20.8 – 27.0 | 72.3 | 52.2 – 92.3 | 17.9 | 14.4 – 21.4 | 64.7 | 60.5 – 68.9 | 77.0 | 66.4 – 87.7 | – | ||
| 2010–2014 | 6.1 | 3.6 – 8.6 | 28.0 | 25.7 – 30.3 | 56.5 | 54.0 – 58.9 | 53.3 | 50.2 – 56.5 | 12.9 | 7.7 – 18.0 | 13.7 | 9.3 – 18.1 | 20.4 | 18.7 – 22.1 | 72.1 | 68.3 – 75.8 | 82.2 | 80.3 – 84.2 | 56.0 | 52.6 – 59.5 | 45.5 | 41.9 – 49.0 | 90.4 | 87.6 – 93.2 | 26.1 | 22.7 – 29.5 | 67.1 | 51.2 – 83.1 | 21.4 | 17.9 – 25.0 | 71.6 | 67.8 – 75.4 | 84.1 | 73.2 – 94.9 | – | ||
|
| |||||||||||||||||||||||||||||||||||||
| Lithuania* | 2000–2004 | 4.7 | 2.9 – 6.4 | 22.0 | 20.7 – 23.3 | 44.5 | 42.6 – 46.3 | 40.6 | 38.4 – 42.8 | 7.9 | 5.6 – 10.2 | 6.5 | 5.3 – 7.7 | 8.8 | 8.0 – 9.6 | 67.2 | 63.9 – 70.6 | 64.6 | 62.9 – 66.4 | 53.8 | 51.6 – 56.0 | 30.2 | 28.1 – 32.3 | 75.8 | 73.7 – 77.9 | 19.4 | 17.2 – 21.6 | 47.5 | 36.2 – 58.8 | 25.4 | 22.5 – 28.3 | 43.5 | 41.5 – 45.5 | 74.3 | 65.2 – 83.3 | 86.1 | 77.2 – 95.0 |
| 2005–2009 | 6.2 | 4.2 – 8.1 | 24.9 | 23.4 – 26.4 | 51.1 | 49.2 – 53.0 | 48.8 | 46.6 – 51.1 | 8.3§ | 5.9 – 10.7 | 5.4§ | 4.3 – 6.5 | 8.8 | 8.0 – 9.7 | 70.6 | 67.6 – 73.7 | 71.3 | 69.6 – 73.1 | 59.1 | 56.9 – 61.3 | 31.6 | 29.5 – 33.8 | 93.8 | 92.6 – 95.1 | 22.0 | 19.7 – 24.3 | 66.6 | 53.4 – 79.8 | 47.5 | 45.1 – 49.9 | 50.8 | 48.9 – 52.7 | 67.7 | 56.5 – 78.8 | 79.6 | 67.1 – 92.1 | |
| 2010–2014 | 5.6 | 3.3 – 7.8 | 27.0 | 24.9 – 29.0 | 56.9 | 54.4 – 59.4 | 52.7 | 49.7 – 55.7 | 8.0§ | 5.3 – 10.7 | 7.0§ | 5.2 – 8.8 | 9.9 | 8.7 – 11.0 | 75.3 | 71.8 – 78.9 | 73.5 | 71.3 – 75.7 | 59.2 | 56.4 – 62.0 | 35.0 | 32.0 – 37.9 | 94.3 | 92.7 – 95.8 | 23.4§ | 20.4 – 26.4 | 61.8 | 44.7 – 78.9 | 52.8 | 49.7 – 56.0 | 56.7 | 54.0 – 59.3 | 74.7 | 62.8 – 86.5 | 93.7 | 85.9 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Malta* | 2000–2004 | 7.8 | 0.0 – 15.6 | 19.9 | 14.6 – 25.2 | 57.0 | 51.9 – 62.2 | 55.1 | 47.7 – 62.5 | 4.2 | 0.0 – 10.5 | 5.9 | 3.0 – 8.7 | 9.2 | 6.5 – 12.0 | 87.3 | 80.0 – 94.7 | 79.7 | 75.6 – 83.8 | 46.4 | 30.8 – 62.0 | 39.6 | 31.6 – 47.5 | 81.9 | 76.6 – 87.2 | 22.3 | 15.2 – 29.3 | 60.1 | 31.7 – 88.6 | 32.7 | 24.6 – 40.8 | 43.4 | 37.8 – 49.0 | 87.5 | 71.8 – 100.0 | – | |
| 2005–2009 | 6.1 | 0.5 – 11.8 | 24.8 | 19.3 – 30.3 | 52.9 | 48.5 – 57.4 | 53.8 | 47.2 – 60.5 | 0.0§ | 0.0 – 0.0 | 2.2§ | 0.5 – 4.0 | 11.4 | 8.7 – 14.1 | 81.6 | 75.2 – 88.1 | 84.8 | 81.3 – 88.2 | 65.1 | 51.4 – 78.9 | 27.5 | 22.0 – 33.0 | 86.4 | 81.9 – 91.0 | 20.1 | 14.0 – 26.1 | – | 25.4§ | 18.0 – 32.8 | 52.4 | 47.3 – 57.6 | 93.8 | 82.3 – 100.0 | – | |||
| 2010–2014 | 11.2 | 1.6 – 20.8 | 23.8 | 17.5 – 30.0 | 57.5 | 52.6 – 62.3 | 56.1 | 49.2 – 62.9 | 0.0§ | 0.0 – 0.0 | 5.5§ | 2.7 – 8.3 | 14.9 | 11.5 –18.2 | 81.9 | 75.6 – 88.3 | 86.9 | 83.1 – 90.6 | 57.4 | 46.8 – 68.1 | 28.0 | 21.4 – 34.6 | 88.2 | 83.9 – 92.5 | 28.0 | 19.7 – 36.2 | – | 46.3§ | 38.3 – 54.3 | 61.9 | 55.8 – 68.0 | – | – | ||||
|
| |||||||||||||||||||||||||||||||||||||
| Netherlands* | 2000–2004 | 12.1 | 11.2 –13.0 | 19.7 | 18.8 – 20.6 | 58.1 | 57.4 – 58.7 | 58.0 | 57.0 – 59.1 | 10.1 | 8.6 – 11.7 | 3.7 | 3.2 – 4.2 | 12.4 | 12.1 – 12.7 | 88.4 | 87.6 – 89.2 | 83.9 | 83.4 – 84.4 | 66.1 | 64.1 – 68.0 | 36.3 | 35.1 – 37.6 | 83.4 | 82.7 – 84.1 | 21.4 | 20.4 – 22.5 | 62.7 | 58.4 – 67.0 | 39.4 | 38.2 – 40.6 | 54.7 | 53.9 – 55.4 | 84.1 | 80.7 – 87.4 | 86.5 | 81.9 – 91.2 |
| 2005–2009 | 16.8 | 15.8 – 17.7 | 22.9 | 22.0 – 23.9 | 60.9 | 60.3 – 61.5 | 63.1 | 62.2 – 64.0 | 13.4 | 11.8 –14.9 | 5.5 | 5.0 – 6.1 | 15.7 | 15.3 – 16.0 | 89.8 | 89.1 – 90.4 | 85.8 | 85.3 – 86.3 | 65.5 | 63.6 – 67.3 | 37.2 | 36.0 – 38.5 | 87.5 | 86.9 – 88.1 | 26.3 | 25.2 – 27.3 | 66.0 | 61.9 – 70.1 | 49.9 | 48.8 – 51.0 | 63.7 | 63.0 – 64.4 | 89.8 | 86.9 – 92.6 | 86.5 | 82.3 – 90.8 | |
| 2010–2014 | 21.0 | 20.0 – 22.0 | 25.0 | 24.0 – 26.0 | 63.1 | 62.5 – 63.7 | 65.3 | 64.5 – 66.2 | 15.8 | 14.2 – 17.4 | 7.4 | 6.8 – 8.1 | 17.3 | 16.9 – 17.6 | 91.0 | 90.4 – 91.6 | 86.6 | 86.1 – 87.1 | 67.5 | 65.6 – 69.3 | 37.5 | 36.2 – 38.7 | 88.5 | 87.9 – 89.0 | 28.2 | 27.2 – 29.3 | 69.1 | 65.1 – 73.1 | 52.2 | 51.2 – 53.2 | 66.4 | 65.8 – 67.1 | 90.4 | 87.5 – 93.3 | 87.9 | 83.5 – 92.2 | |
|
| |||||||||||||||||||||||||||||||||||||
| Norway* | 2000–2004 | 9.0 | 6.7 – 11.3 | 22.4 | 20.5 – 24.2 | 60.0 | 58.8 – 61.2 | 62.4 | 60.8 – 64.1 | 7.9 | 5.4 – 10.3 | 5.0 | 3.9 – 6.0 | 12.3 | 11.5 –13.1 | 86.4 | 85.1 – 87.6 | 84.7 | 83.7 – 85.8 | 70.9 | 68.0 – 73.7 | 41.4 | 39.3 – 43.6 | 83.8 | 82.8 – 84.9 | 32.4 | 30.5 – 34.3 | 79.7 | 73.8 – 85.5 | 41.5 | 39.2 – 43.8 | 57.5 | 56.1 – 58.8 | 87.7 | 82.4 – 93.1 | 93.3 | 87.2 – 99.4 |
| 2005–2009 | 13.3 | 10.8 – 15.8 | 25.3 | 23.3 – 27.4 | 64.3 | 63.2 – 65.4 | 66.8 | 65.1 – 68.4 | 14.2 | 11.2 –17.2 | 6.1 | 5.0 – 7.2 | 15.9 | 15.1 – 16.8 | 87.3 | 86.2 – 88.3 | 87.2 | 86.1 – 88.3 | 70.7 | 67.8 – 73.6 | 42.8 | 40.7 – 45.0 | 90.3 | 89.5 – 91.1 | 36.7 | 34.9 – 38.5 | 75.9 | 69.7 – 82.1 | 50.9 | 48.8 – 53.0 | 64.9 | 63.7 – 66.2 | 84.9 | 78.2 – 91.6 | 90.9 | 84.3 – 97.5 | |
| 2010–2014 | 16.5 | 14.0 – 19.0 | 26.5 | 24.4 – 28.6 | 66.7 | 65.6 – 67.8 | 69.2 | 67.6 – 70.8 | 18.7 | 15.5 – 22.0 | 9.5 | 8.0 – 11.0 | 19.0 | 18.1 – 19.8 | 89.3 | 88.3 – 90.3 | 87.7 | 86.6 – 88.8 | 73.3 | 70.3 – 76.3 | 45.5 | 43.3 – 47.7 | 92.9 | 92.2 – 93.7 | 36.8 | 34.9 – 38.7 | 74.3 | 67.6 – 81.0 | 52.7 | 50.7 – 54.7 | 68.4 | 67.2 – 69.6 | 83.0 | 76.5 – 89.5 | 95.2 | 90.9 – 99.4 | |
|
| |||||||||||||||||||||||||||||||||||||
| Poland* (16 registries) | 2000–2004 | 7.2 | 6.3 – 8.1 | 15.9 | 15.2 – 16.5 | 45.3 | 44.6 – 45.9 | 42.5 | 41.8 – 43.3 | 9.5 | 8.5 – 10.5 | 8.2 | 7.6 – 8.8 | 12.1 | 11.8 –12.4 | 63.2 | 62.0 – 64.4 | 71.3 | 70.7 – 71.9 | 51.6 | 50.8 – 52.5 | 32.7 | 31.9 – 33.6 | 68.8 | 67.9 – 69.7 | 26.6 | 25.6 – 27.7 | 62.6 | 59.2 – 66.0 | 18.9 | 17.9 – 19.9 | 40.3 | 39.6 – 41.0 | 79.6 | 76.3 – 82.9 | 81.7 | 77.8 – 85.6 |
| 2005–2009 | 8.9 | 7.9 – 9.8 | 19.9 | 19.3 – 20.4 | 51.1 | 50.5 – 51.6 | 47.6 | 46.9 – 48.3 | 10.7 | 9.8 – 11.7 | 9.7 | 9.2 – 10.3 | 14.1 | 13.8 – 14.4 | 67.1 | 66.2 – 68.1 | 74.7 | 74.2 – 75.2 | 54.4 | 53.6 – 55.3 | 35.4 | 34.6 – 36.2 | 75.0 | 74.4 – 75.7 | 29.0 | 28.2 – 29.8 | 61.7 | 58.1 – 65.3 | 26.3 | 25.2 – 27.5 | 47.8 | 47.2 – 48.5 | 84.4 | 81.7 – 87.0 | 89.4 | 86.4 – 92.4 | |
| 2010–2014 | 9.1 | 8.1 – 10.1 | 20.9 | 20.3 – 21.4 | 52.9 | 52.3 – 53.4 | 48.4 | 47.7 – 49.1 | 10.8 | 9.9 – 11.8 | 8.0 | 7.5 – 8.5 | 14.4 | 14.1 – 14.7 | 69.8 | 68.9 – 70.7 | 76.5 | 76.1 – 77.0 | 55.1 | 54.2 – 55.9 | 37.5 | 36.7 – 38.3 | 78.1 | 77.5 – 78.7 | 28.2 | 27.4 – 28.9 | 62.5 | 58.7 – 66.4 | 27.3 | 26.2 – 28.4 | 52.1 | 51.4 – 52.8 | 86.9 | 84.1 – 89.7 | 92.6 | 89.7 – 95.5 | |
|
| |||||||||||||||||||||||||||||||||||||
| Portugal* (4 registries) | 2000–2004 | 10.2 | 8.6 – 11.7 | 29.8 | 28.9 – 30.8 | 56.5 | 55.6 – 57.4 | 54.4 | 53.1 – 55.7 | 13.6 | 11.8 –15.5 | 8.0 | 6.7 – 9.2 | 10.6 | 10.0 – 11.2 | 78.8 | 76.8 – 80.7 | 81.6 | 80.7 – 82.5 | 60.4 | 58.6 – 62.2 | 39.9 | 37.7 – 42.1 | 87.2 | 86.2 – 88.1 | 22.9 | 21.3 – 24.6 | 62.0 | 55.0 – 69.1 | 43.7 | 41.6 – 45.8 | 51.3 | 50.1 – 52.6 | 80.8 | 75.3 – 86.4 | 86.2 | 81.0 – 91.4 |
| 2005–2009 | 12.5 | 11.0 –14.1 | 32.4 | 31.5 – 33.3 | 61.1 | 60.4 – 61.9 | 59.8 | 58.7 – 60.9 | 15.3 | 13.6 – 17.0 | 10.3 | 9.1 – 11.4 | 14.1 | 13.5 – 14.7 | 81.7 | 80.2 – 83.2 | 86.1 | 85.3 – 86.9 | 65.3 | 63.6 – 67.0 | 41.8 | 39.7 – 44.0 | 90.0 | 89.3 – 90.8 | 23.8 | 22.4 – 25.3 | 63.1 | 56.5 – 69.7 | 49.0 | 47.1 – 50.9 | 58.2 | 57.1 – 59.2 | 84.1 | 78.8 – 89.5 | 94.0 | 90.1 – 97.9 | |
| 2010–2014 | 16.1 | 12.0 – 20.2 | 32.2 | 30.2 – 34.2 | 60.9 | 59.2 – 62.6 | 59.6 | 57.1 – 62.1 | 18.7 | 14.5 – 22.9 | 10.7 | 8.2 – 13.1 | 15.7 | 14.3 – 17.1 | 83.7 | 80.4 – 87.0 | 87.6 | 85.9 – 89.3 | 66.2 | 62.6 – 69.8 | 43.6 | 38.7 – 48.4 | 90.9 | 89.1 – 92.6 | 22.7 | 19.7 – 25.8 | 70.5 | 57.0 – 84.1 | 49.8 | 45.4 – 54.2 | 59.7 | 57.3 – 62.1 | 89.8 | 80.7 – 98.9 | 94.7 | 88.9 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Romania (Cluj) | 2000–2004 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||||||||||
| 2005–2009 | 10.2§ | 4.4 – 16.0 | 19.3§ | 16.0 – 22.7 | 53.5§ | 48.9 – 58.0 | 44.8 | 38.9 – 50.8 | 4.1§ | 1.8 –6.4 | 4.5§ | 2.2 – 6.7 | 7.9§ | 6.1 – 9.6 | 68.4 | 61.5 – 75.3 | 74.8 | 70.4 – 79.3 | 61.7 | 57.0 – 66.5 | 28.9§ | 22.3 – 35.6 | 78.2 | 72.5 – 83.8 | 20.4§ | 14.0 – 26.7 | – | 44.9 | 37.2 – 52.5 | 47.3 | 42.0 – 52.5 | – | – | ||||
| 2010–2014 | 0.0§ | 0.0 – 0.1 | 26.0§ | 21.5 – 30.5 | 52.2§ | 46.0 – 58.4 | 58.4 | 49.8 – 67.0 | 13.2§ | 9.2 – 17.3 | 6.0§ | 2.6 – 9.3 | 11.1§ | 8.7 – 13.6 | 71.3 | 63.0 – 79.6 | 74.8 | 68.5 – 81.1 | 65.3 | 59.7 – 70.9 | 37.2§ | 29.7 – 44.6 | 77.1 | 70.0 – 84.2 | 34.0§ | 23.8 – 44.1 | 60.1 | 31.6 – 88.5 | 51.5 | 42.7 – 60.3 | 40.4 | 33.3 – 47.5 | 53.9 | 28.2 – 79.6 | – | ||
|
| |||||||||||||||||||||||||||||||||||||
| Russian Federation (5 registries) | 2000–2004 | 10.9 | 8.8 – 13.0 | 22.9 | 21.7 – 24.1 | 40.4 | 38.9 – 41.9 | 38.5 | 36.4 – 40.6 | 7.4 | 5.2 – 9.5 | 7.5 | 6.0 – 9.1 | 16.8 | 15.7 – 17.8 | 64.7 | 61.4 – 68.0 | 71.6 | 69.8 – 73.4 | 59.8 | 57.3 – 62.2 | 38.1 | 35.2 – 41.1 | 58.8 | 55.4 – 62.1 | 25.2 | 21.3 – 29.0 | 61.2 | 50.4 – 72.0 | 33.1 | 28.7 – 37.5 | 40.5 | 37.4 – 43.5 | 71.3 | 62.6 – 80.0 | 67.0 | 54.9 – 79.1 |
| 2005–2009 | 8.6 | 7.0 – 10.2 | 20.2 | 19.3 – 21.1 | 42.4 | 41.2 – 43.6 | 38.9 | 37.3 – 40.5 | 5.1 | 3.6 – 6.6 | 5.4 | 4.5 – 6.4 | 13.9 | 13.2 – 14.6 | 63.3 | 60.3 – 66.3 | 67.7 | 66.4 – 69.0 | 58.0 | 56.0 – 59.9 | 33.2 | 31.3 – 35.0 | 68.6 | 66.2 – 71.0 | 21.2 | 19.2 – 23.2 | 61.2 | 50.3 – 72.0 | 35.3 | 31.7 – 39.0 | 42.4 | 39.8 – 45.0 | 74.2 | 65.3 – 83.0 | 73.5 | 62.6 – 84.4 | |
| 2010–2014 | 8.6 | 7.1 – 10.1 | 21.0 | 20.0 – 21.9 | 44.9 | 43.8 – 46.1 | 41.9 | 40.2 – 43.5 | 6.3 | 4.8 – 7.9 | 4.4 | 3.7 – 5.2 | 13.7 | 13.0 – 14.4 | 66.5 | 63.6 – 69.3 | 70.8 | 69.5 – 72.1 | 57.7 | 55.7 – 59.7 | 34.8 | 32.8 – 36.8 | 79.3 | 77.1 – 81.5 | 22.8 | 20.8 – 24.9 | 61.7 | 51.5 – 71.8 | 33.2 | 29.8 – 36.7 | 45.5 | 42.9 – 48.2 | 76.9 | 68.4 – 85.4 | 92.1 | 84.6 – 99.6 | |
|
| |||||||||||||||||||||||||||||||||||||
| Slovakia* | 2000–2004 | 5.8§ | 3.8 – 7.9 | 20.6§ | 19.1 – 22.0 | 50.4 | 49.1 – 51.7 | 43.6 | 41.7 – 45.5 | 5.6§ | 4.1 – 7.2 | 4.8§ | 3.8 – 5.8 | 9.5§ | 8.7 – 10.3 | 75.0 | 72.7 – 77.3 | 75.3 | 73.5 – 77.2 | 61.8 | 59.4 – 64.3 | 35.0 | 32.4 – 37.6 | 63.6 | 61.1 – 66.0 | 22.0§ | 20.0 – 24.0 | 67.9 | 60.5 – 75.4 | 35.1§ | 32.2 – 38.1 | 46.6 | 44.6 – 48.6 | 79.2 | 71.8 – 86.5 | 83.8 | 75.1 – 92.5 |
| 2005–2009 | 6.4 | 4.7 – 8.0 | 20.9 | 19.5 – 22.4 | 51.2 | 50.1 – 52.4 | 47.5 | 45.8 – 49.2 | 6.1§ | 4.8 – 7.5 | 5.8 | 4.8 – 6.7 | 10.5 | 9.7 – 11.2 | 79.7 | 77.7 – 81.7 | 76.6 | 75.1 – 78.2 | 58.9 | 56.5 – 61.3 | 34.5 | 31.7 – 37.3 | 74.4 | 72.7 – 76.2 | 27.2 | 25.3 – 29.0 | 70.0 | 62.5 – 77.5 | 37.1 | 34.8 – 39.4 | 49.6 | 48.0 – 51.2 | 80.7 | 73.8 – 87.7 | 94.6 | 90.1 – 99.1 | |
| 2010–2014 | 6.4 | 3.3 – 9.4 | 21.1 | 17.8 – 24.3 | 51.8 | 49.1 – 54.4 | 48.6 | 44.9 – 52.4 | 7.6§ | 4.5 – 10.7 | 6.4 | 4.4 – 8.4 | 11.2 | 9.5 – 12.8 | 78.2 | 73.9 – 82.5 | 75.5 | 72.4 – 78.5 | 60.5 | 56.2 – 64.9 | 33.4 | 28.6 – 38.2 | 74.7 | 70.9 – 78.6 | 28.5 | 24.3 – 32.8 | 80.6 | 69.4 – 91.7 | 37.5 | 32.2 – 42.8 | 51.6 | 48.0 – 55.2 | 87.0 | 77.3 – 96.7 | 88.6 | 75.4 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Slovenia* | 2000–2004 | 8.2 | 5.7 – 10.8 | 25.9 | 23.8 – 27.9 | 53.6 | 51.6 – 55.6 | 48.6 | 46.1 – 51.1 | 3.8 | 2.2 – 5.4 | 4.7 | 3.4 – 6.1 | 9.9 | 9.1 – 10.8 | 79.3 | 76.7 – 81.9 | 78.7 | 76.9 – 80.5 | 67.2 | 63.8 – 70.7 | 37.8 | 34.4 – 41.2 | 74.4 | 71.9 – 76.9 | 23.0 | 19.9 – 26.1 | 76.5 | 66.8 – 86.3 | 42.4 | 38.5 – 46.2 | 52.7 | 50.2 – 55.2 | 89.7 | 82.1 – 97.3 | 80.1 | 68.7 – 91.5 |
| 2005–2009 | 9.3 | 6.2 – 12.3 | 25.8 | 23.7 – 27.8 | 56.2 | 54.4 – 58.0 | 57.0 | 54.6 – 59.4 | 7.0 | 5.2 – 8.8 | 5.7 | 4.3 – 7.1 | 12.7 | 11.7 –13.7 | 85.0 | 83.0 – 87.0 | 82.5 | 81.0 – 84.1 | 67.1 | 63.3 – 70.9 | 35.4 | 32.3 – 38.4 | 83.2 | 81.6 – 84.8 | 24.1 | 21.2 – 27.0 | 61.2 | 49.2 – 73.1 | 39.8 | 36.6 – 42.9 | 56.7 | 54.6 – 58.9 | 79.1 | 67.1 – 91.1 | 100.0 | 86.3 – 100.0 | |
| 2010–2014 | 8.6 | 5.2 – 11.9 | 28.8 | 26.4 – 31.2 | 61.9 | 60.0 – 63.8 | 60.3 | 57.7 – 62.9 | 7.4 | 5.3 – 9.5 | 6.6 | 4.9 – 8.4 | 14.8 | 13.6 – 16.1 | 85.1 | 83.0 – 87.1 | 83.5 | 81.8 – 85.2 | 65.5 | 61.3 – 69.8 | 37.0 | 33.4 – 40.5 | 85.0 | 83.3 – 86.7 | 24.8 | 21.4 – 28.3 | 60.1 | 44.2 – 76.1 | 37.5 | 34.2 – 40.7 | 59.0 | 56.6 – 61.3 | 70.1 | 54.4 – 85.8 | 100.0 | 100.0 – 100.0 | |
|
| |||||||||||||||||||||||||||||||||||||
| Spain (10 registries) | 2000–2004 | 8.9 | 7.5 – 10.3 | 25.7 | 24.5 – 26.9 | 56.5 | 55.6 – 57.4 | 55.2 | 53.7 – 56.6 | 14.4 | 13.2 – 15.7 | 5.6 | 4.8 – 6.4 | 10.8 | 10.4 – 11.3 | 85.3 | 83.8 – 86.8 | 82.9 | 82.0 – 83.8 | 63.6 | 61.3 – 65.9 | 36.0 | 34.1 – 37.9 | 85.0 | 84.1 – 85.9 | 21.6 | 20.2 – 23.0 | 63.6 | 57.7 – 69.4 | 45.4 | 43.6 – 47.2 | 58.2 | 57.1 – 59.3 | 80.9 | 76.3 – 85.5 | 85.8 | 80.2 – 91.4 |
| 2005–2009 | 11.6 | 10.2 – 13.1 | 26.7 | 25.5 – 27.9 | 61.1 | 60.3 – 61.9 | 58.6 | 57.3 – 59.9 | 16.3 | 15.1 – 17.4 | 6.9 | 6.1 – 7.7 | 12.5 | 12.0 – 13.0 | 87.1 | 85.9 – 88.3 | 84.6 | 83.8 – 85.4 | 64.5 | 62.2 – 66.8 | 37.9 | 36.1 – 39.6 | 90.4 | 89.7 – 91.1 | 27.2 | 25.8 – 28.7 | 63.4 | 58.2 – 68.6 | 52.3 | 50.8 – 53.8 | 62.2 | 61.3 – 63.2 | 80.0 | 75.4 – 84.5 | 89.9 | 85.9 – 94.0 | |
| 2010–2014 | 13.0 | 10.6 – 15.4 | 27.6 | 25.7 – 29.5 | 63.2 | 62.0 – 64.5 | 59.5 | 57.4 – 61.5 | 17.3 | 15.4 – 19.2 | 7.7 | 6.3 – 9.2 | 13.5 | 12.7 – 14.3 | 86.8 | 84.8 – 88.7 | 85.2 | 84.0 – 86.5 | 64.5 | 60.8 – 68.1 | 39.8 | 36.9 – 42.7 | 89.7 | 88.6 – 90.7 | 27.4 | 25.2 – 29.7 | 66.2 | 58.0 – 74.4 | 50.0 | 47.7 – 52.3 | 62.0 | 60.5 – 63.6 | 84.7 | 77.6 – 91.7 | 92.9 | 87.5 – 98.3 | |
|
| |||||||||||||||||||||||||||||||||||||
| Sweden* | 2000–2004 | 11.4 | 9.6 – 13.1 | 21.2 | 19.8 – 22.6 | 60.2 | 59.2 – 61.2 | 59.9 | 58.7 – 61.1 | 7.8 | 6.4 – 9.1 | 4.9 | 4.1 – 5.8 | 13.9 | 13.2 – 14.6 | 88.9 | 88.1 – 89.8 | 85.6 | 84.9 – 86.3 | 66.9 | 64.7 – 69.1 | 43.2 | 41.6 – 44.8 | 85.9 | 85.3 – 86.5 | 26.5 | 25.1 – 28.0 | 75.9 | 70.5 – 81.3 | 30.7 | 28.9 – 32.6 | 58.5 | 57.6 – 59.5 | 86.8 | 82.6 – 90.9 | 84.7 | 75.8 – 93.6 |
| 2005–2009 | 13.1 | 11.4 –14.8 | 23.6 | 22.1 – 25.1 | 64.2 | 63.3 – 65.2 | 63.0 | 61.9 – 64.2 | 13.0 | 11.4 –14.6 | 7.9 | 6.9 – 8.9 | 16.6 | 15.9 – 17.3 | 90.3 | 89.5 – 91.0 | 87.9 | 87.2 – 88.5 | 67.7 | 65.6 – 69.9 | 42.9 | 41.2 – 44.6 | 90.1 | 89.6 – 90.6 | 29.0 | 27.5 – 30.4 | 78.4 | 73.2 – 83.6 | 54.6 | 53.1 – 56.1 | 64.2 | 63.3 – 65.1 | 87.1 | 82.6 – 91.5 | 88.6 | 81.5 – 95.8 | |
| 2010–2014 | 14.8 | 12.8 – 16.7 | 24.8 | 23.3 – 26.3 | 64.9 | 64.0 – 65.8 | 64.7 | 63.5 – 65.8 | 16.6 | 14.9 – 18.3 | 9.7 | 8.7 – 10.8 | 19.5 | 18.7 – 20.2 | 91.5 | 90.9 – 92.2 | 88.8 | 88.2 – 89.4 | 68.3 | 66.1 – 70.4 | 46.5 | 44.8 – 48.2 | 90.7 | 90.2 – 91.2 | 31.6 | 30.1 – 33.0 | 79.8 | 74.9 – 84.7 | 57.5 | 56.0 – 58.9 | 66.7 | 65.9 – 67.6 | 89.0 | 84.6 – 93.3 | 88.0 | 80.4 – 95.7 | |
|
| |||||||||||||||||||||||||||||||||||||
| Switzerland† (10 registries) | 2000–2004 | 16.1 | 13.6 – 18.6 | 29.2 | 26.9 – 31.4 | 62.8 | 61.3 – 64.3 | 59.5 | 57.2 – 61.8 | 12.2 | 10.3 – 14.0 | 5.6 | 4.4 – 6.9 | 14.7 | 13.8 – 15.6 | 90.7 | 88.4 – 92.9 | 84.4 | 83.3 – 85.5 | 63.4 | 58.4 – 68.4 | 36.9 | 34.4 – 39.5 | 86.9 | 85.8 – 87.9 | 26.4 | 23.9 – 28.8 | 73.7 | 67.7 – 79.8 | 46.5 | 43.9 – 49.1 | 61.6 | 60.1 – 63.2 | 87.3 | 82.4 – 92.2 | 94.0 | 89.5 – 98.6 |
| 2005–2009 | 20.6 | 17.9 – 23.2 | 31.4 | 29.0 – 33.7 | 65.1 | 63.7 – 66.6 | 65.6 | 63.5 – 67.7 | 13.4 | 11.6 –15.3 | 7.0 | 5.8 – 8.2 | 17.3 | 16.5 – 18.2 | 92.4 | 91.3 – 93.5 | 86.4 | 85.3 – 87.4 | 69.4 | 65.1 – 73.6 | 42.0 | 39.5 – 44.4 | 88.6 | 87.6 – 89.5 | 29.0 | 26.7 – 31.2 | 68.0 | 61.2 – 74.8 | 51.6 | 49.3 – 53.9 | 70.9 | 69.5 – 72.3 | 89.2 | 84.9 – 93.4 | 94.2 | 89.5 – 98.9 | |
| 2010–2014 | 23.9 | 21.0 – 26.9 | 32.2 | 29.9 – 34.5 | 67.3 | 65.7 – 68.9 | 67.3 | 65.0 – 69.6 | 15.4 | 13.5 – 17.4 | 9.4 | 7.9 – 10.8 | 20.4 | 19.4 – 21.4 | 93.6 | 92.4 – 94.7 | 86.2 | 85.1 – 87.3 | 71.4 | 66.6 – 76.2 | 44.1 | 41.3 – 46.8 | 89.2 | 88.2 – 90.3 | 29.7 | 27.5 – 31.9 | 71.6 | 65.1 – 78.0 | 49.7 | 47.2 – 52.2 | 72.0 | 70.4 – 73.5 | 90.3 | 86.1 – 94.5 | 93.6 | 88.1 – 99.1 | |
|
| |||||||||||||||||||||||||||||||||||||
| United Kingdom* (4 registries) | 2000–2004 | 11.5 | 11.1 –11.9 | 16.2 | 15.7 – 16.6 | 52.0 | 51.6 – 52.3 | 54.6 | 54.0 – 55.1 | 7.1 | 6.6 – 7.7 | 3.7 | 3.4 – 4.0 | 8.3 | 8.1 – 8.5 | 86.4 | 85.9 – 86.8 | 79.8 | 79.5 – 80.1 | 58.9 | 58.0 – 59.9 | 30.2 | 29.7 – 30.7 | 81.9 | 81.6 – 82.3 | 20.6 | 20.1 – 21.2 | 68.4 | 66.2 – 70.7 | 42.3 | 41.7 – 42.9 | 54.3 | 53.9 – 54.6 | 85.9 | 84.1 – 87.7 | 86.8 | 84.1 – 89.5 |
| 2005–2009 | 14.0 | 13.5 – 14.4 | 19.2 | 18.7 – 19.7 | 56.5 | 56.2 – 56.9 | 58.7 | 58.2 – 59.2 | 9.7 | 9.1 – 10.2 | 5.2 | 4.9 – 5.5 | 10.1 | 9.9 – 10.3 | 89.2 | 88.9 – 89.6 | 83.8 | 83.6 – 84.1 | 61.9 | 61.0 – 62.9 | 33.2 | 32.6 – 33.7 | 86.7 | 86.4 – 86.9 | 23.8 | 23.3 – 24.4 | 69.1 | 66.9 – 71.3 | 47.7 | 47.1 – 48.2 | 60.7 | 60.4 – 61.1 | 91.4 | 89.9 – 92.8 | 90.6 | 88.3 – 93.0 | |
| 2010–2014 | 15.7 | 15.3 – 16.1 | 20.7 | 20.1 – 21.2 | 60.0 | 59.7 – 60.4 | 62.5 | 62.0 – 63.0 | 13.0 | 12.4 – 13.6 | 6.8 | 6.5 – 7.2 | 13.3 | 13.1 – 13.5 | 90.9 | 90.6 – 91.3 | 85.6 | 85.4 – 85.9 | 63.8 | 62.8 – 64.7 | 36.2 | 35.7 – 36.8 | 88.7 | 88.5 – 89.0 | 26.3 | 25.7 – 26.8 | 71.9 | 69.8 – 74.0 | 48.7 | 48.1 – 49.2 | 64.9 | 64.6 – 65.3 | 92.2 | 90.9 – 93.6 | 91.7 | 89.7 – 93.8 | |
|
OCEANIA | |||||||||||||||||||||||||||||||||||||
| Australia* (8 registries) | |||||||||||||||||||||||||||||||||||||
| 2000–2004 | 18.0 | 16.9 – 19.2 | 27.7 | 26.7 – 28.8 | 63.7 | 63.2 – 64.3 | 64.4 | 63.5 – 65.2 | 14.2 | 13.1 – 15.3 | 7.3 | 6.7 – 8.0 | 14.8 | 14.4 – 15.2 | 92.0 | 91.7 – 92.4 | 87.0 | 86.5 – 87.4 | 67.9 | 66.1 – 69.6 | 37.3 | 36.1 – 38.6 | 87.8 | 87.4 – 88.2 | 24.5 | 23.5 – 25.4 | 62.0 | 57.7 – 66.3 | 43.3 | 42.3 – 44.3 | 61.5 | 60.9 – 62.1 | 86.5 | 83.8 – 89.1 | 91.4 | 88.0 – 94.8 | |
| 2005–2009 | 19.9 | 18.7 – 21.0 | 29.8 | 28.8 – 30.9 | 68.1 | 67.6 – 68.6 | 68.6 | 67.8 – 69.5 | 17.7 | 16.6 – 18.7 | 9.1 | 8.5 – 9.8 | 17.1 | 16.7 – 17.5 | 92.5 | 92.2 – 92.8 | 88.5 | 88.1 – 89.0 | 67.5 | 65.7 – 69.3 | 41.0 | 39.8 – 42.2 | 93.2 | 92.9 – 93.5 | 28.9 | 27.9 – 29.8 | 60.6 | 56.4 – 64.9 | 50.3 | 49.4 – 51.1 | 68.1 | 67.6 – 68.7 | 90.3 | 87.9 – 92.6 | 94.2 | 91.4 – 96.9 | |
| 2010–2014 | 23.7 | 22.4 – 25.0 | 31.8 | 30.7 – 32.9 | 70.7 | 70.1 – 71.2 | 71.0 | 70.2 – 71.9 | 19.2 | 18.1 – 20.3 | 12.0 | 11.2 –12.8 | 19.4 | 19.0 – 19.9 | 92.9 | 92.5 – 93.2 | 89.5 | 89.1 – 90.0 | 66.4 | 64.5 – 68.2 | 42.0 | 40.8 – 43.2 | 94.5 | 94.1 – 94.8 | 30.2 | 29.2 – 31.2 | 67.1 | 62.9 – 71.4 | 51.8 | 50.9 – 52.7 | 71.2 | 70.6 – 71.8 | 90.7 | 88.3 – 93.1 | 92.3 | 89.2 – 95.4 | |
|
| |||||||||||||||||||||||||||||||||||||
| New Zealand* | 2000–2004 | 11.5 | 9.4 – 13.6 | 24.6 | 22.4 – 26.8 | 61.4 | 60.2 – 62.7 | 60.1 | 58.0 – 62.1 | 12.4 | 9.9 – 15.0 | 7.0 | 5.5 – 8.5 | 11.4 | 10.5 – 12.2 | 90.0 | 89.1 – 90.8 | 82.8 | 81.6 – 84.1 | 67.4 | 63.8 – 71.1 | 38.7 | 36.0 – 41.4 | 89.1 | 88.1 – 90.0 | 19.0 | 16.8 – 21.2 | 60.2 | 50.6 – 69.8 | 40.3 | 37.8 – 42.9 | 61.0 | 59.6 – 62.5 | 85.8 | 79.9 – 91.6 | 93.6 | 88.7 – 98.4 |
| 2005–2009 | 14.5 | 12.1 – 16.8 | 24.8 | 22.5 – 27.0 | 62.8 | 61.6 – 64.0 | 63.3 | 61.4 – 65.3 | 16.8 | 14.4 – 19.1 | 7.7 | 6.3 – 9.0 | 12.4 | 11.6 –13.3 | 91.1 | 90.3 – 91.8 | 86.1 | 84.9 – 87.3 | 64.4 | 60.4 – 68.4 | 33.4 | 31.0 – 35.9 | 89.3 | 88.4 – 90.2 | 22.7 | 20.4 – 25.0 | 54.4 | 42.9 – 66.0 | 49.7 | 47.7 – 51.8 | 63.5 | 62.1 – 64.9 | 91.2 | 86.8 – 95.6 | 93.5 | 88.0 – 99.0 | |
| 2010–2014 | 15.3 | 13.0 – 17.7 | 25.7 | 23.5 – 27.9 | 64.0 | 62.8 – 65.1 | 66.0 | 64.1 – 67.9 | 19.0 | 16.7 – 21.4 | 8.1 | 6.7 – 9.6 | 15.3 | 14.3 – 16.2 | 91.8 | 91.1 – 92.5 | 87.6 | 86.4 – 88.7 | 67.4 | 63.4 – 71.5 | 36.7 | 34.1 – 39.3 | 90.3 | 89.4 – 91.1 | 23.3 | 21.0 – 25.7 | 58.2 | 46.1 – 70.4 | 44.1 | 42.1 – 46.2 | 65.6 | 64.3 – 66.9 | 91.4 | 86.7 – 96.1 | 96.6 | 92.7 – 100.0 | |
Survival estimates that are not age-standardised are italicised.
Survival estimates of 100% shown without a confidence interval are those for which the first event (either death or censoring) in that group of patients occurred more than five years after diagnosis.
Data with 100% coverage of the national population.
Data with 100% coverage of the national population for childhood malignancies only.
Korea: Republic of Korea; Russia: Russian Federation.
Survival estimate considered less reliable because 15% or more of patients were (a) lost to follow-up or censored alive within five years of diagnosis or, if diagnosed in 2010 or later, before 31 December 2014; or (b) registered only from a death certificate or at autopsy; or (c) registered with incomplete dates, i.e., unknown year of birth, unknown month and/or year of diagnosis or unknown year of last vital status.
Italics denote survival estimates that are not age-standardised
Survival was highest in Japan (36%), China (34%) and Korea* (31%), and below 30% in all other countries (Table 5, web-figure 2). Survival was in the range 20–30% in 11 countries: Mauritius*, Puerto Rico*, the US, 2 countries in western Asia (Israel*, Turkey), in 5 European countries (North: Ireland*; West: Belgium*, Germany, the Netherlands*, Switzerland) and in Australia*.
Survival trends from 2000 to 2014 increased by 4–5% in Singapore*, 3 European countries (North: Denmark*, the UK*; West: Germany) and in the US (web-figure 3). Survival increased by 6–10% in China, Israel* and Japan, in 6 European countries (North: Ireland*, Norway*; South: Portugal*; West: Belgium*, the Netherlands*, Switzerland) and in Australia*. The increase in Korea* was 13%.
Stomach
Results are available for 2,019,382 adults from 294 registries in 62 countries (Tables 2 and 4).
Age-standardised five-year net survival was generally in the range 20–40%, with very wide variation in Asia (web-figure 4). Most estimates were considered reliable (Table 5, web-table 4).
In 2010–2014, survival was very high in Korea* (69%) and Japan (60%), followed by Jordan* (56%) and Costa Rica* (46%) (Table 5, web-figure 2). Survival was in the range 30–40% in 16 countries: in Canada and the US; in Puerto Rico* and Martinique*; 5 Asian countries (South: Malaysia (Penang), Singapore*; East: China, Taiwan*; West: Israel*); 6 European countries (South: Italy, Portugal*; West: Austria*, Belgium*, Germany, Switzerland) and in Australia* (Table 5, web-figure 2).
Survival was in the range 20–29% in 25 countries (Mauritius*, Brazil, Kuwait*, Turkey, 20 European countries, New Zealand*), and below 20% in Chile, Ecuador, Thailand and Bulgaria*.
Survival trends between 1995–1999 and 2010–2014 were rather flat in most countries, but after 2000, survival increased by 5% in Canada and the US, Singapore* and in 6 European countries (North: Denmark*, Lithuania*, the UK*; East: Poland*; West: Austria*, the Netherlands*).
Over the same 20 years, 5-year survival increased by up to 10% in Israel*, Japan, Estonia* and Ireland*, and by 20% or more in China and Korea*.
Colon
Results are available for 4,198,637 adults from 296 registries in 65 countries (Tables 2 and 4).
Survival for colon cancer varied widely, especially in Central and South America, in Asia and in Europe (Figure 4A, web-figure 4). Most estimates were considered reliable (Table 5, web-table 4).
Figure 4. Global range of breast cancer* survival among 296 cancer registry populations in 64 countries: age-standardised five-year net survival (%) estimates for 6,420,288 women diagnosed during 2000–2014, by continent and calendar period of diagnosis.
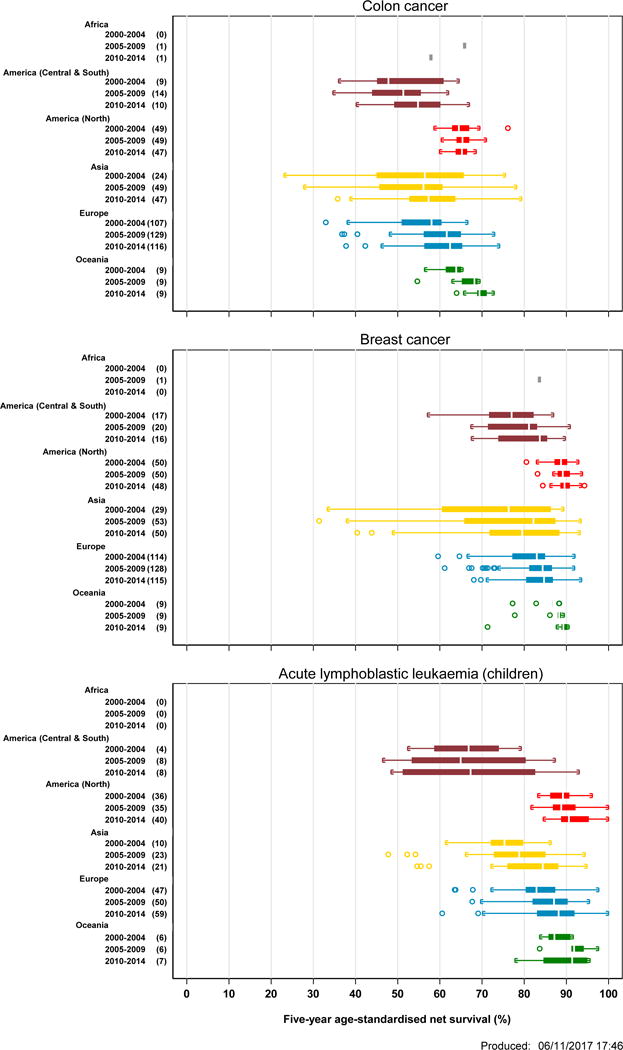
*See web-figure 4 for other cancers.
Each box-plot shows the range of survival estimates among all cancer registries for which suitable estimates could be obtained for patients diagnosed in each calendar period, in each continent. The number of registries included in each box-plot is shown in parentheses. Survival estimates considered less reliable are not included (see text). The vertical line inside each box represents the median survival estimate among all contributing registries (the central value in the range, or 50th centile). The box covers the inter-quartile range (IQR) between the lower and upper quartiles (25th and 75th centiles). Where there are only a few widely scattered estimates, the median may be close to the lower or upper quartile. The extreme limits of the box-plot are 1.5*IQR below the lower quartile and 1.5*IQR above the upper quartile. Open circles indicate „outlier‟ values, outside this range.
For patients diagnosed during 2010–2014, survival was higher than 70% in 4 countries: Israel*, Jordan*, Korea* and Australia*. Survival was in the range 50–69% in 26 countries: Mauritius*; in Costa Rica* and Puerto Rico*; in Canada and the US; in Japan, Singapore* and Taiwan*; in 17 European countries (North: Denmark*, Finland*, Iceland*, Ireland*, Norway*, Sweden*, the UK*; South: Italy, Portugal*, Slovenia*, Spain; West: Austria*, Belgium*, France, Germany, the Netherlands*, Switzerland) and in New Zealand* (Table 5, web-figure 2).
Survival ranged from 50% to 60% in 20 countries: in 4 Central and South American countries (Brazil, Martinique, Peru (Lima), Uruguay*); in 5 Asian countries (South: Malaysia (Penang) East: China, Hong Kong*; West: Kuwait*, Turkey) and in 9 European countries (North: Estonia*, Lithuania*, Latvia*; South: Croatia*, Malta*; East: Bulgaria*, Czech Republic*, Poland*, Slovakia*).
Five-year net survival was below 50% in Ecuador (48%), Thailand (47%), Russia (45%) and India (39%).
Survival trends between 1995–1999 and 2000–2014 were generally flat or increasing (web-figure 3). Five-year survival increased over this period by 5–10% in 11 countries: in Canada; in Japan and Taiwan*, and in 7 European countries (North: Estonia*, Ireland*, Lithuania*, Norway*, Sweden*; South: Italy; West: the Netherlands*) and in Australia*.
Over the same period, survival increased by more than 10% in China, Israel* and Korea*, and in 8 European countries (North: Denmark*, Iceland*, Latvia*, the UK*; South: Slovenia*, Spain; East: Bulgaria*, Czech Republic*, Poland*).
Rectum
Results are available for 1,720,488 adults from 294 registries in 64 countries (Tables 2 and 4).
As for colon, five-year net survival for rectal cancer varied widely. The range of survival estimates in Asia for 2010–2014 was even wider than for colon cancer (web-figure 4). Almost all the survival estimates were considered reliable (Table 5, web-table 4).
Survival was higher than 70% in Jordan* (73%), Korea* (71%), and Australia* (71%).
For patients diagnosed during 2010–2014, survival was in the range 60–69% in 24 countries: in Canada and the US; in 4 Asian countries (South: Singapore*; East: Japan, Taiwan*; West: Israel*), in 17 European countries: (North: Denmark*, Finland*, Iceland*, Ireland*, Norway*; Sweden*, the UK*; South: Italy, Portugal*, Slovenia*, Spain; West: Austria*; Belgium*; France, Germany, the Netherlands*, Switzerland); and in New Zealand* (Table 5, web-figure 2).
Survival was in the range 50–59% in 18 countries: in 7 countries in Central and South America (Argentina, Brazil, Costa Rica*, Martinique*, Peru (Lima), Puerto Rico*, Uruguay*); in 5 Asian countries (South: Malaysia (Penang); East: China, Hong Kong*; West: Kuwait*, Turkey) and in 6 European countries (North: Estonia*, Latvia*, Lithuania*; South: Malta*; East: Czech Republic*, Romania (Cluj)).
Five-year survival was below 50% in Slovakia* (49%), Poland* (48%), Croatia* (48%), Bulgaria* (46%), Ecuador (45%), Thailand (44%), Russia (42%) and India (30%).
Survival trends between 1995–1999 and 2000–2014 were generally increasing, especially since 2000, in Asia, Europe and Oceania (web-figure 3). Survival increased by 5–10% in Japan and Taiwan*; in Finland*, Italy and Sweden; and in New Zealand*.
Over the same period, 5-year survival increased by 10% or more in Canada; in China, Israel* and Korea*; in 13 European countries (North: Denmark*, Estonia*, Ireland*, Lithuania*, Norway*, the UK*; South: Portugal*, Spain, East: Bulgaria*, Czech Republic*, Poland*; West: the Netherlands*, Switzerland), and in Australia*. The increase was about 20% in Korea* and Slovenia*.
Liver
Results are available for 1,178,364 adults from 291 registries in 61 countries (Tables 2 and 4).
Five-year net survival was in the range 5–30% throughout 2000–2014 (web-figure 4). Estimates are often flagged as less reliable than for other solid tumours (Table 5, web-table 4), because of the exclusion of higher proportions of DCO registrations (Table 3, web-table 2).
For patients diagnosed during 2010–2014, age-standardised five-year net survival was 30% in Japan, and in the range 20–29% only in Korea*, Singapore* and Taiwan*; and in Belgium* and Italy.
Survival was in the range 10–19% in 32 countries: Canada and the US, in 4 countries in Central and South America (Argentina, Brazil, Martinique*, Puerto Rico*); in 4 Asian countries (East: China; West: Israel*, Kuwait*, Turkey); in 15 European countries (North: Iceland*, Ireland*, Latvia*, Norway*, Sweden*, the UK*; South: Portugal*, Spain; East: Poland*, Romania (Cluj); West: Austria*, France, Germany, the Netherlands*, Switzerland) and in Australia* and New Zealand*.
Five-year survival was less than 10% in Denmark*, Slovenia*, Thailand, Czech Republic*, Russia and Estonia*.
In most countries, survival has changed very little during the 20-year period 1995–1999 to 2000–2014. It increased by 5–10% in Canada and the US; in Japan; in 9 European countries (North: Denmark*, Ireland, the UK*; South: Italy, Spain; West: France, Germany, the Netherlands*, Switzerland) and Australia* and New Zealand*. Survival increased by more than 10% in China, Korea* and Taiwan*; and in Norway*, Portugal* and Sweden*.
Pancreas
Results are available for 1,229,379 adults from 290 registries in 59 countries (Tables 2 and 4).
Age-standardised five-year net survival estimates were generally in the range 5–15% throughout 2000–2014 (web-figure 4). As for liver cancer, some estimates are less reliable (Table 5, web-table 4), due to the high proportion of DCO registrations (Table 3, web-table 2).
For patients diagnosed during 2010–2014, survival was higher in Kuwait* (24%) and Malaysia (Penang, 19%) (Table 5, web-figure 2). Survival was in the range 10–15% in 16 countries: in Canada and the US; in Brazil and Martinique*; in China, Korea* and Turkey, in 8 European countries (North: Estonia*, Ireland*, Latvia*, Norway*, Sweden*; South: Portugal*; West: Belgium*, Germany), and in Australia*. Five-year net survival ranged between 5% and 10% in 19 countries. Survival was very low in Russia (4%).
Trends in 5-year survival between 2000–2004 and 2010–2014 were generally flat, but increases of 3–5% were seen in Canada and the US; in Korea* and Singapore*, in 12 European countries (North: Denmark*, Estonia*, Ireland*, Latvia*, Norway*, Sweden*, the UK*; South: Portugal*; East: Czech Republic*; West: Belgium*, the Netherlands*, Switzerland), and in Australia* (web-figure 3).
Lung
Results are available for 6,051,262 adults from 290 registries in 61 countries (Tables 2 and 4).
Age-standardised five-year net survival was in the range 10–20% in most countries (Table 5, web-figure 4). Most estimates in Central and South America were less reliable, due to the high proportion of DCO registrations excluded from analysis (Table 5, web-table 4), although the proportion of DCOs has generally decreased world-wide (Table 3, web-table 3).
For patients diagnosed during 2010–2014, the five-year survival estimate was high in Japan (33%). It was in the range 20–30% in 12 countries: Mauritius*, Canada and the US; 4 Asian countries (East: China, Korea*, Taiwan*; West: Israel*), and 5 European countries (North: Latvia*, Iceland*, Sweden*; West: Austria*, Switzerland) (Table 5, web-figure 2). In most countries, however, survival was in the range 10–19%: in Martinique* and Puerto Rico*; in 6 Asian countries (South: Malaysia (Penang), Singapore*; West: Cyprus*, Kuwait*, Qatar*, Turkey); in 21 European countries (North: Denmark*, Estonia*, Finland*, Lithuania*, Norway*; South: Croatia*, Italy, Malta*, Portugal*, Slovenia*, Spain; East: Czech Republic*, Poland*, Russia, Slovakia*; West: Belgium*, France, Germany, Ireland*, the Netherlands*, the UK*); and in Oceania (Australia* and New Zealand*).
Survival was below 10% in Thailand, Brazil, Bulgaria and India.
Lung cancer survival trends between 1995–1999 and 2000–2014 were generally flat, but survival increased by 5–10% in 21 countries: in Canada and the US; in Israel*, Singapore* and Taiwan*; and in 15 European countries (North: Denmark*, Estonia*, Iceland*, Ireland*, Latvia*, Norway*, Sweden*, the UK*; South: Portugal*, Slovenia*; West: Austria*, France, Germany, the Netherlands*, Switzerland), and in Australia*. Survival increased by more than 10% in China, Japan and Korea* (Table 5, web-figure 3).
Melanoma of the skin
Results are available for 1,553,109 adults from 281 registries in 59 countries (Tables 2 and 4).
Age-standardised 5-year net survival was in the range 60–90% in most countries (web-figure 4). Most estimates were considered reliable (Table 5, web-table 4).
For patients diagnosed during 2010–2014, five-year survival estimates exceeded 90% in 14 countries: in the US, and in 8 European countries (North: Denmark*, Sweden*, the UK*; West: Belgium*, France, Germany, the Netherlands, Switzerland); and in Australia* and New Zealand* (Table 5, web-figure 2).
Survival was in the range 80–89% in 14 countries: in Canada, in Israel* and in 12 European countries (North: Estonia*, Finland*, Iceland*, Ireland*, Norway*; South: Italy, Malta*, Portugal*, Slovenia*, Spain; East: Czech Republic*; West: Austria*).
Survival was in the range 70–79% in 10 countries: in 4 countries in Central and South America (Argentina, Brazil, Costa Rica*, Puerto Rico*); and in 6 European countries (North: Latvia*, Lithuania*; South: Croatia*; East; Poland*, Romania (Cluj), Slovakia*).
Survival was in the range 60–69% in 7 countries: in 5 Asian countries (South: India, Singapore*; East: Korea*, Japan; West: Turkey) and in Bulgaria* and Russia. Survival was below 60% in Ecuador and in 5 Asian countries (South: Thailand; East: China, Taiwan*; West: Jordan*, Kuwait*).
Trends between 2000–2004 and 2010–2014 were generally stable in North America, Oceania and Japan, and in several European countries, where five-year survival was already around 85–90% among patients diagnosed during 2000–2004. Survival increased by 5–10% in China and Korea*; 13 European countries (North: Denmark*, Estonia*, Latvia*, Lithuania*, UK*; South: Croatia*, Portugal*, Slovenia*; East: Bulgaria*, Czech Republic*, Poland*; West: Austria*, Belgium*).
Women’s cancers
Breast
Results are available for 6,422,553 women from 298 cancer registries in 66 countries (Tables 2 and 4).
The range of survival estimates is still wide in each continent, apart from North America and Oceania (Figure 4, web-figure 4). Most estimates were considered reliable (Table 5, web-table 4).
For women diagnosed during 2010–2014, age-standardised five-year net survival was 85% or above in 25 countries: in Costa Rica* and Martinique*; Canada* and the US; in Israel*, Japan and Korea*; in 16 European countries (North: Denmark*, Finland*, Iceland*, Norway*, Sweden*, the UK*; West: Austria*, Belgium*, France, Germany, the Netherlands*, Switzerland; South: Italy, Malta*, Portugal*, Spain); and in Australia* and New Zealand* (Table 5, Figure 2B, web-figure 2).
Figure 2. Global distribution of age-standardised five-year net survival (%) for adults (15–99 years) diagnosed during 2010–2014 with colon cancer or breast cancer (women) and children (0–14 years) diagnosed with acute lymphoblastic leukaemia: continent and country.
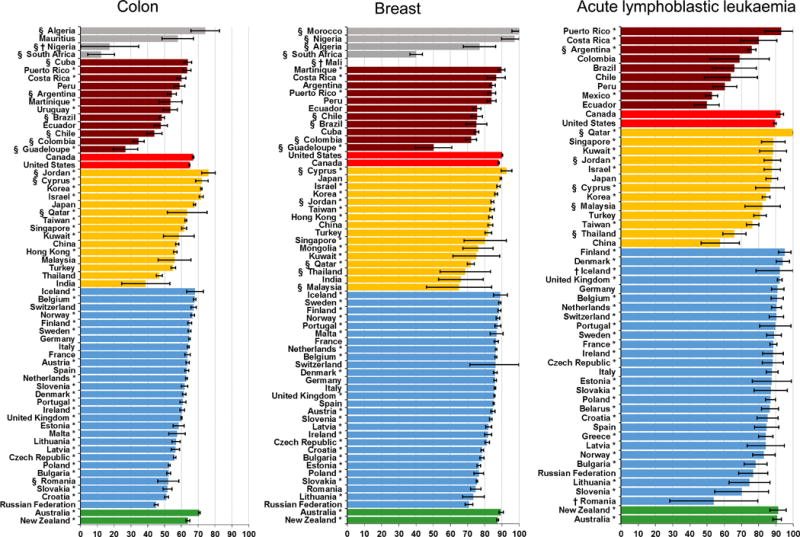
Survival estimates for each country are ranked from highest to lowest within each continent. Where data were available for more than one registry in a given country, the survival estimates are derived by pooling the data for that country, but excluding data from registries for which the estimates are considered less reliable (see text).
See web-figures 2.1–2.18 for all 18 cancers included in CONCORD-3, and for each calendar period 2000–2004, 2005–2009, 2010–2014.
*Data with 100% coverage of the national population.
†National estimate not age-standardised.
§National estimate flagged as less reliable because the only available estimates are from a registry or registries in this category (see text).
Five-year survival was in the range 80–84% in 13 countries: 4 countries in Central and South America (Argentina, Brazil, Peru (Lima), Puerto Rico*); 5 Asian countries (South: Singapore*; East: China, Hong Kong*, Taiwan*; West: Turkey) and 4 European countries (North: Ireland*; East: Czech Republic*, Latvia*; South: Slovenia*). Survival was in the range 70–79% in 12 countries: in Cuba* and Ecuador; in Kuwait* and Mongolia*; and 8 countries in Europe (North: Estonia*, Lithuania*; South: Croatia*; East: Bulgaria*, Poland*, Romania (Cluj), Russia, Slovakia*).
Survival was still low in Thailand (69%) and India (Karunagappally, 66%).
Five-year net survival continued to increase up to 2010–2014 in most countries in Central and South America, Eastern and Western Asia and in all of Europe. Even so, survival remains lower in Eastern Europe than in other parts of the continent. In North America and Oceania, five-year net survival approached 90% (Figure 3, web-figure 3).
Figure 3. 20-year trends in age-standardised five-year net survival (%) for women (15–99 years) with breast cancer,* by calendar period of diagnosis (1995–1999, 2000–2004, 2005–2009 and 2010–2014), continent (or continental region) and country.
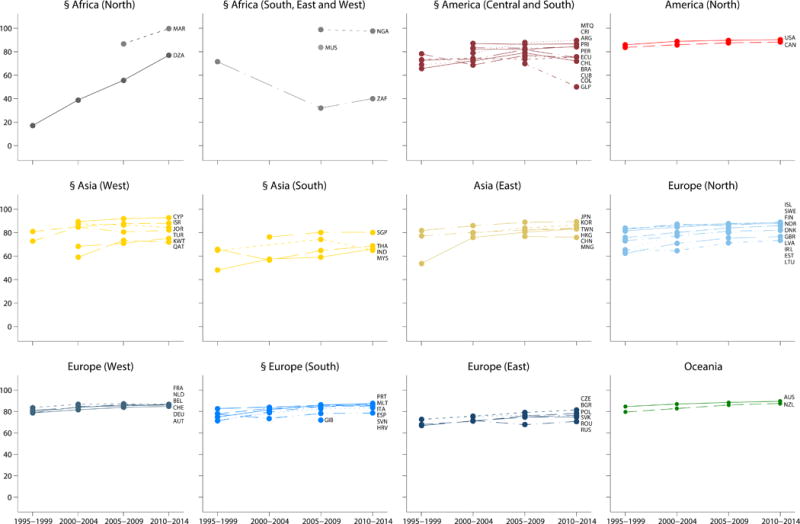
Estimates for women diagnosed during 1995–1999 are taken from the analyses for CONCORD-2.6 Where data were available for more than one registry in a given country, the survival estimates are derived by pooling the data for that country, excluding data from registries for which the survival estimates are considered less reliable (see text).
*See web-figures 3.1–3.18 for other cancers.
§Continent or continental region with one or more national estimates flagged as less reliable.
Standard ISO abbreviations for country names: Algeria - DZA; Argentina - ARG; Australia - AUS; Austria - AUT; Belgium - BEL; Brazil - BRA; Bulgaria - BGR; Canada - CAN; Chile - CHL; China - CHN; Colombia - COL; Costa Rica - CRI; Croatia - HRV; Cuba - CUB; Cyprus - CYP; Czech Republic - CZE; Denmark - DNK; Ecuador - ECU; Estonia - EST; Finland - FIN; France - FRA; Germany - DEU; Gibraltar - GIB; Guadeloupe - GLP; Hong Kong SAR - HKG; Iceland - ISL; India - IND; Ireland - IRL; Israel - ISR; Italy - ITA; Japan - JPN; Jordan - JOR; Kuwait - KWT; Latvia - LVA; Lithuania - LTU; Malaysia - MYS; Malta - MLT; Martinique - MTQ; Mauritius - MUS; Mongolia - MNG; Morocco - MAR; Netherlands - NLD; New Zealand - NZL; Nigeria - NGA; Norway - NOR; Peru - PER; Poland - POL; Portugal - PRT; Puerto Rico - PRI; Qatar - QAT; Republic of Korea - KOR; Romania - ROU; Russian Federation - RUS; Singapore - SGP; Slovakia - SVK; Slovenia - SVN; South Africa - ZAF; Spain - ESP; Sweden - SWE; Switzerland - CHE; Taiwan - TWN; Thailand - THA; Turkey - TUR; United Kingdom of Great Britain and Northern Ireland - GBR; United States of America - USA
Cervix
Results are available for 660,744 women from 295 cancer registries in 64 countries (Tables 2 and 4).
The global range in cervical cancer survival is still wide (50–70%), especially in Central and South America, Asia and Europe (Table 5, web-figure 4). Most survival estimates are reliable (web-table 4).
For women diagnosed during 2010–2014, age-standardised five-year net survival was 70% or higher in 7 countries, of which 5 with national coverage: in Japan, Korea* and Taiwan*; in Denmark*, Norway* and Switzerland, and in Cuba* (Table 5, web-figure 2).
Survival was in the range 60–69% in 29 countries: Canada and the US; Brazil and Puerto Rico*; 5 countries in Asia (East: China, Hong Kong*; South: Singapore*; West: Israel*, Turkey), 18 countries in Europe, and in Australia* and New Zealand*.
Survival was in the range 50–59% in 5 countries in Central and South America (Argentina, Ecuador, Martinique, Peru (Lima), Uruguay*); in India, Kuwait* and Thailand, and in 6 European countries (North: Latvia*, Lithuania*; East: Bulgaria*, Poland*, Russia; South: Malta*).
Over the 15 years up to 2014, five-year survival has increased by 4–6% in Japan and in 11 European countries (North: Denmark*, Estonia*, Ireland*, Lithuania*, Norway*; the UK*; South: Portugal*; East: Bulgaria*, Poland*; West: Switzerland) (web-figure 3). Survival increased by 8–10% in Cuba* and India. In China, five-year survival increased from 53% for women diagnosed during 2000–2004 to 68% in 2010–2014.
Ovary
Results are available for 865,501 women from 289 registries in 61 countries (Tables 2 and 4).
Age-standardised five-year net survival was mostly in the range 30–50%, with even wider variation in Europe and Asia (web-figure 4). Most survival estimates were reliable (Table 5, web-table 4).
For women diagnosed during 2010–2014, five-year survival was still below 50% in most countries, except Costa Rica* (62%) (Table 5, web-figures 2–4). Survival was in the range 40–49% in 25 countries: in Canada and the US, in 8 countries in Asia (South: Singapore*; East: China, Korea*, Japan, Taiwan*; West: Israel*, Turkey), in 14 European countries (North: Denmark*, Estonia*, Finland*, Iceland*, Latvia*, Norway*, Sweden*; South: Portugal*, Spain; West: Austria*, Belgium*, France, Germany, Switzerland), and in Australia*.
Survival was in the range 30–39% in 19 countries: 4 in Central and South America (Argentina, Brazil, Ecuador, Puerto Rico*); in Kuwait* and Thailand, in 12 European countries (North: Ireland*, Lithuania*, the UK* South: Croatia*, Italy, Slovenia*; East: Bulgaria*, Czech Republic*, Poland*, Russia, Slovakia*; West: the Netherlands*), and in New Zealand*.
Survival was below 30% in Malta* (28%) and India (16%).
Survival trends between 1995–1999 and 2010–2014 were rather flat in most countries. However, five-year survival rose by 5–10% in the US; in Israel*, Korea* and Taiwan*; in 11 European countries (North: Denmark*, Iceland*, Ireland*, Norway*, Sweden*; South: Portugal*, Spain; East: Bulgaria*, Poland*; West: France, Switzerland), and in Australia*. Survival increased by more than 10% in Estonia* and Latvia*, and by 20% in Japan.
Prostate
Results are available for 5,864,878 men from 290 registries in 62 countries (Tables 2 and 4).
Age-standardised five-year net survival was in the range 70–100% in most countries (web-figure 4). Most estimates were reliable (Table 5, web-table 4).
For men diagnosed during 2010–2014, five-year survival was approaching 100% in Puerto Rico*, Martinique* and the US. Survival was higher than 90% in a further 22 countries: in Brazil and Costa Rica*; in Canada; in Israel*, Japan and Korea*; in 14 European countries (North: Iceland*, Ireland*, Finland*, Latvia*, Lithuania*, Norway*, Sweden*; South: Italy, Portugal*, Spain; West: Austria*, Belgium*, France, Germany), and in Australia* and New Zealand*.
Survival was in the range 80–89% in 18 countries: in Argentina, Ecuador and Uruguay*; in 6 Asian countries (South: Malaysia (Penang), Singapore*; East: Taiwan*; West: Jordan*, Kuwait*, Turkey); and in 9 European countries (North: Denmark*, Estonia*, the UK*; South: Croatia*, Malta*, Slovenia*; East: Czech Republic*; West: the Netherlands*, Switzerland).
Survival was approaching 80% in Russia (79%), Poland* (78%) and Romania (Cluj, 77%). It was 75% in Slovakia*, and below 70% in China (69%), Mauritius* (69%), Bulgaria* (68%) and Thailand (68%). Five-year survival was 44% in India.
Over the 20-year period between 1995–1999 and 2010–2014, age-standardised five-year net survival was rising in most countries. Survival increased by 5–10% in Brazil and Ecuador; in Canada; in China and Turkey; in Austria* and Portugal*; and in New Zealand*.
Five-year survival rose by more than 10% in Israel*, Taiwan* and Thailand, and in 12 European countries (North: Finland*, Iceland*, Norway*, Sweden*; South: Croatia*, Italy, Malta*, Spain; West: France, Germany, the Netherlands*, Switzerland), and in Australia.
Survival increased by more than 20% in 13 countries: in Japan, Korea* and Malaysia (Penang), and in 10 European countries (North: Denmark*, Estonia*, Ireland*, Latvia*, Lithuania*, the UK*; South: Slovenia*; East: Bulgaria*, Czech Republic*, Poland*).
Brain
Results are available for 656,659 adults from 286 registries in 59 countries (Tables 2 and 4).
Age-standardised five-year net survival was in the range 20–40% in most countries (web-figure 4). Most estimates were considered reliable (Table 5, web-table 5).
For patients diagnosed during 2010–2014, five-year survival was higher than 40% only in Japan (46%) and Croatia* (42%).
Survival was in the range 30–40% in 22 countries: Canada, the US, Puerto Rico* and Martinique; in 8 Asian countries (South: Singapore*, East: China, India, Korea*; West: Israel*, Jordan*, Kuwait*, Turkey), in 9 European countries (North: Denmark*, Estonia*, Finland*, Ireland*, Norway*, Sweden*; West: Belgium*, Germany, Switzerland), and in Australia*.
Survival was in the range 20–29% in 20 countries: Chile and Ecuador; in Malaysia (Penang) and Taiwan*; in 15 European countries (North: Iceland*, Latvia*, the UK*; South: Italy, Malta*, Portugal*, Slovenia*, Spain; East: Czech Republic*, Poland*, Russia, Slovakia*; West: Austria*, France, The Netherlands*), and in New Zealand*. Five-year survival was 15% in Thailand.
Trends in 5-year survival between 2000–2004 and 2010–2014 were generally rather flat, but survival increased by 3–5% in 15 countries: Martinique* and Puerto Rico*; in Canada; in Israel* and Thailand; in 9 European countries (North: Iceland*, Latvia*, Lithuania*, Norway*, Sweden*; South: Croatia*, Italy; West: France, Switzerland), and in New Zealand*.
Survival increased by 6–10% in a further 13 countries: the US; in China, India (Karunagappally); Korea* and Singapore*, and in 7 European countries (North: Denmark*, Estonia*, Ireland*, the UK*; South: Malta*, Spain; West: the Netherlands*), and Australia*. A striking increase (18%) was observed in Japan.
Haematological malignancies
Myeloid malignancies
Results are available for 1,151,226 adults from 286 registries in 61 countries (Tables 2 and 4).
Age-standardised five-year net survival was in the range 30–50% in most countries, although lower in Asia (web-figure 4). Most estimates were considered reliable (Table 5, web-table 5).
For patients diagnosed during 2010–2014, survival was 55–60% in Belgium*, France, Germany and Sweden*; in the range 50–54% in Canada, Turkey and in 8 European countries (North: Ireland*, Lithuania*, Norway*; South: Portugal*, Spain; East: Romania (Cluj); West: the Netherlands*, Switzerland) and in Australia*.
Five-year survival was in the range 40–49% in 11 countries: the US, Martinique and Puerto Rico*, in Israel*, Korea* and Singapore*; in 4 European countries (North: Denmark*, Iceland*, the UK*; South: Italy), and in New Zealand*.
Survival was in the range 30–39% in 13 countries: Argentina, Brazil and Costa Rica*, in Japan, Malaysia (Penang) and Taiwan*; and in 7 European countries (North: Estonia*; South: Croatia*, Slovenia*; East: Czech Republic*, Russia, Slovakia*; West: Austria*). Survival was below 30% in Chile and Ecuador; in China, Kuwait* and Thailand; and in Latvia* and Poland*.
Over the 15 years between 2000–2004 and 2010–2014, age-standardised five-year net survival increased by 5–10% in 14 countries: in the US; in China, Japan, Singapore* and Taiwan*; in 8 European countries (North: Ireland*, the UK*; South: Portugal*, Spain; East: Poland*; West: Austria*, Belgium*, Germany) and in Australia*. Survival rose by more than 10% in Korea*; and in Denmark*, the Netherlands* and Norway*.
Survival increased dramatically in both Lithuania* and Sweden* (27%) and the Czech Republic* (17%).
Lymphoid malignancies
Results are available for 3,011,054 adults from 289 registries in 62 countries (Tables 2 and 4).
Five-year age-standardised net survival was usually in the range 40–70% in most countries, lower in Asia and in Central and South America (web-figure 4). Most estimates were considered reliable (Table 5, web-table 5).
For patients diagnosed during 2010–2014, 5-year survival was 70% or higher in 6 European countries (North: Denmark*, Iceland*, Latvia*; West: Belgium*, France, Switzerland) and Australia*. Survival was in the range 60–69% in Mauritius*; Puerto Rico*, Canada and the US; in Israel* and Kuwait*; and in 12 European countries (North: Finland*, Ireland*, Norway*, Sweden*, the UK*; South: Italy, Malta*, Portugal*, Spain; West: Austria*, Germany, the Netherlands*), and in New Zealand*.
Survival was 50–59% in 15 countries: in Costa Rica* and in 6 Asian countries (South: Malaysia (Penang), Singapore*; East: Japan, Korea*, Taiwan*; West: Turkey) and in 7 European countries (North: Estonia*, Lithuania*; South: Croatia*, Slovenia*; East: Czech Republic*, Poland*, Slovakia*).
Survival was lower than 50% in 5 countries in Central and South America (Argentina, Brazil, Chile, Ecuador, Martinique); in China, India and Thailand; and in Bulgaria*, Romania (Cluj) and Russia.
Five-year survival trends between 2000–2004 and 2010–2014 were increasing in most countries. Survival increased by 5–10% in 22 countries: Ecuador; in Canada and the US; in Japan, Taiwan* and Thailand, in 15 European countries (North: Finland*, Estonia*, Iceland*, Sweden*; South: Croatia*, Portugal*, Slovenia*; East: Bulgaria*, Czech Republic*, Russia, Slovakia*; West: Austria*, Belgium*, France, Germany) and in New Zealand*.
Survival increased by more than 10% in 15 countries: in Puerto Rico*; in Korea*, Kuwait* and Singapore*; in 10 European countries (North: Denmark*, Ireland*, Latvia*, Lithuania*, Norway*, the UK*; South: Malta*; East: Poland*; West: the Netherlands*, Switzerland), and in Australia*.
Childhood cancers
Brain
Results are available for 66,814 children (Table 4) from 260 registries in 60 countries (Tables 2 and 4).
For children diagnosed during 2010–2014, age-standardised five-year net survival was close to 80% in Denmark*, Slovakia* and Sweden*. Survival was in the range 70–79% in 17 countries: in Canada and the US; in Costa Rica* and Puerto Rico*; in Israel* and Japan; and in 11 European countries (North: Finland*, Ireland*, Norway*, the UK*; South: Croatia*, Italy, Portugal*; West: Belgium*, France*, Germany, Switzerland*).
Survival was in the range 60–69% in 15 countries: in Argentina; in Korea*, Singapore* and Turkey; in 10 European countries (North: Estonia*, Latvia*, Lithuania*; South: Greece*, Slovenia*, Spain; East: Belarus*, Poland*, Russia; West: the Netherlands*); and in Australia*.
Five-year survival was below 40% in Brazil and Mexico*.
Survival trends between 2000–2004 and 2010–2014 were generally stable or increasing. Five-year age-standardised survival increased by 5–10% in China, Korea* and Turkey; in 6 European countries (North: Ireland*; South: Croatia*, Italy, Portugal* West: Germany, the Netherlands*) and in Australia*.
Survival increased by 10% or more in Argentina, Thailand, and 4 European countries (North: Denmark*, Lithuania*; East: Czech Republic*, Slovakia*).
Acute lymphoblastic leukaemia (ALL)
Results are available for 87,351 children from 254 registries in 61 countries (Tables 2 and 4).
The global range in survival was very wide, from 50% to more than 90% (Figure 2C, web-figures 2 and 4). For children diagnosed during 2010–2014, age-standardised five-year net survival was 90% or above in Puerto Rico*, in Canada and the US; in Qatar*, in 9 European countries (North: Denmark*, Finland*, the UK*; South: Malta*, Portugal*; West: Belgium*, Germany, the Netherlands*, Switzerland*), and in Australia* and New Zealand*.
Survival was in the range 80–89% in Costa Rica*, in 9 Asian countries (South: Malaysia (Penang), Singapore*; East: Japan, Korea*; West: Cyprus*, Israel*, Jordan*, Kuwait*, Turkey), and in 14 European countries (North: Estonia*, Ireland*, Latvia*, Norway*, Sweden*; South: Croatia*, Greece*, Italy, Spain; East: Belarus*, Czech Republic*, Poland*, Slovakia*; West: France*). (Table 5, Figure 2C, web-figure 2).
Five-year net survival was still below 70%, even after adjustment for the very high background mortality in childhood: in Brazil, Chile, Colombia, Peru and Thailand. Survival was below 60% in China, Ecuador and Mexico*.
In the 20-year period between 1995–1999 and 2010–2014, five-year survival increased by 10% or more in 18 countries: in Colombia; in 8 Asian countries (South: Thailand; East: China, Japan, Korea*, Taiwan*; West: Cyprus*, Kuwait*, Turkey), and in 9 European countries (North: Finland*; Lithuania*, the UK*; South: Malta*; Portugal*, Spain; East: Belarus*, Bulgaria*; West: Belgium*) (web-figure 3).
Lymphoma
Results are available for 41,196 children from 257 registries in 62 countries (Tables 2 and 4).
Five-year age-standardised net survival was generally in the range 80–95% (Table 5, web-figure 4).
For children diagnosed during 2010–2014, five-year survival was 90% or higher in 27 countries: in Canada and the US; in Costa Rica* and Puerto Rico*; in 4 Asian countries (South: Singapore*; East: Korea*; West: Israel*, Kuwait*); in 17 European countries (North: Denmark*, Finland*, Ireland*, Lithuania*, Norway*, the UK*; South: Croatia*, Italy, Portugal*, Slovenia*, Spain; East: Poland*, Russia; West: Belgium*, France*, Germany, Switzerland*), and in Australia* and New Zealand*. Five-year survival was below 70% only in Ecuador (67%) and China (61%).
Five-year survival trends were generally rather flat over the 15 years between 2000–2004 and 2010–2014 (web-figure 3), but survival increased by 5–10% in the US; in Korea*, Singapore* and Taiwan*; and in 4 European countries (North: the UK*; South: Portugal*, Spain; West: Germany).
Five-year survival increased by more than 10% in Brazil; in Bulgaria*, Croatia* and Poland*, and by 20% or more in Slovenia* and Russia.
Discussion
CONCORD-3 updates the world-wide surveillance of cancer survival to 2014. It is the largest and most up-to-date study of international cancer survival trends. It includes individual data for over 37.5 million patients diagnosed with cancer during the 15-year period 2000–2014. Data were provided by over 320 population-based cancer registries in 71 countries and territories, in 47 of which the data covered 100% of the population. The participating countries were home to 67% of the world’s population in 2014 (7.3 billion).27 The registries record all cancers diagnosed in a combined population of almost one billion people, or 14% of the world population.
Internationally comparable survival trends are now available for 18 cancers that collectively represent 75% of all cancers diagnosed world-wide every year.
We used a similar design and statistical methods to those used in CONCORD-26, to enable evaluation of survival trends for 10 cancers over the 20-year period 1995–2014. World-wide survival trends are also available for the first time for melanoma of the skin and cancers of the oesophagus and pancreas in adults, and for brain tumours and lymphomas in both adults and children.
Five-year survival has been recognised by clinicians as an index of the effectiveness of the treatment of cancer for more than 60 years. When applied to hospital case series, it has often been labelled as the “five-year cure rate”, because “with so mortal a disease as cancer, those who survive for this length of time can be considered cured.”44 Five-year survival has increased for many cancers since the 1950s, but it remains a widely used benchmark, even though it cannot be directly interpreted as the proportion of patients who are cured.45
Population-based cancer survival is increasingly recognised as a key indicator of the overall effectiveness of the health systems in managing care and treatment for all cancer patients.46,47 Other outcome measures with applications in cancer control include the number of avoidable premature deaths,48–53 person-years of life lost,54,55 disability-adjusted life-years lost,56 and levels of population “cure”.57–61 Cancer survival has applications to cancer control and health policy at the state, national and global levels, in both high-income and low-income countries.62
In some countries, population-based cancer survival estimates may be considered as too high, potentially discouraging ministerial action to improve survival. Estimates showing ethnic or regional variation in cancer survival may be politically sensitive. Survival estimates may also be considered too low, if they are seen as a reflection of clinical competence.63
Low levels of survival in a country or region should not be interpreted as an indicator of the competence of the health professionals who work there. Population-based survival reflects the overall effectiveness of the health service, which depends on much wider issues than the competence of any individual doctor or team.64–66
The Organisation for Economic Co-operation and Development (OECD) recently concluded from the wide international variation in cancer survival that many countries could do better in cancer control.64 It recommended a national cancer plan, adequate funding, and initiatives for early detection and rapid access to high-quality treatment.64 OECD also recommended improving the quality of cancer data to support monitoring improvements in survival.
From 2017, OECD will include age-standardised five-year net survival estimates from the CONCORD programme for colorectal and breast cancers in adults and acute lymphoblastic leukaemia in children among the indicators of healthcare quality in its biennial and online publications Health at a Glance.67 This is formal recognition of the global coverage, methodological rigour and international comparability of the CONCORD survival estimates, which will now contribute to the comparative evaluation of health systems performance in 48 countries, including all OECD Member countries. The findings will also help monitor progress toward the overarching goal of the 2013 World Cancer Declaration, to achieve major improvements in cancer survival by 2020.68
We carried out extensive checks on data quality, and liaised with the cancer registries to resolve problems. Many registries told us that the CONCORD data quality reports helped them improve their data. Some centres in Nigeria and India have modified hospital admission forms or pathology request forms to capture telephone numbers of patients and their next of kin, to facilitate follow-up of their patients. We extended the data quality control programs and the reports. Rectifying errors or inconsistencies in the data often led to extensive discussion with registry staff, and re-submission of data with higher quality.
The quality and completeness of cancer registration data and follow-up vary between countries, and this can affect the comparability of survival estimates. We have provided extensive documentation of data quality with standard indicators69 for each cancer and each cancer registry (web-table 2). Survival figures and trends should be interpreted alongside those indicators. The overall proportion of tumour records excluded because of incomplete dates (0.5%), or for other reasons such as missing vital status (1.2%), has remained very low. The overall proportion of cancers registered solely from a death certificate (DCO), or detected at autopsy, dropped to 2.9%, but it remains high in some countries where cancer registration processes are slow, especially for the more rapidly lethal cancers of the oesophagus, pancreas and liver. These are well-known issues in population-based cancer registration. DCOs can be included in cancer incidence statistics under certain assumptions, but they reflect some under-estimation of incidence.69 By contrast, DCO cases must be excluded from survival analyses, because the patient’s survival time is unknown. This tends to inflate survival estimates.70
In some countries, survival estimates have fluctuated or declined in successive calendar periods; this is likely to reflect improvements in the completeness of cancer registration data and in the completeness of follow-up for vital status. In Jordan, for example, linkage with the national death index has been insufficient because only about 70% of deaths are certified. Survival estimates were very high for stomach and colorectal cancers and they are flagged as less reliable. One recent hospital-based survival study from Jordan71 suggests that colon cancer survival in Jordan is much lower than the estimates we have obtained. Other countries with incomplete death registration, such as India, follow up their patients actively to determine their vital status.
Despite the problems, we believe these findings represent the best that can be achieved with the available coverage and quality of cancer registration systems and vital statistics systems world-wide. The quality of diagnostic evidence is generally high. Data quality has improved in many countries, with increasing proportions of cases for which the diagnosis was confirmed by pathology, imaging or biomarkers, and reduction in the proportion of patients lost to follow-up. Pathological confirmation of a primary, invasive malignancy was available for more than 94% of all patients. The proportion varies widely between countries and for different cancers, but the evidence supporting a cancer diagnosis in routine cancer registry data is far more precise and definitive than for the cause(s) of death recorded on death certificates, from which mortality statistics are obtained.72–75
In some cases, especially in South America, the improvement in data quality is reflected in survival estimates that are actually lower than those previously published,6 with fewer death-certificate-only registrations and more complete follow-up. In Brazil, for example, improvement in the quality and completeness of the national death registry (Sistema de Informações sobre Mortalidade, or SIM) during 2000–201576 has enabled more complete linkage of death records with the cancer registries. In several countries, survival estimates that were flagged as less reliable in CONCORD-2 are now more reliable, even if the survival estimates are lower.
To estimate the global burden of cancer incidence, assumptions are required where there are no cancer registries, usually by modelling incidence and mortality data from other countries in the same world region.2,77 By contrast, we have made no attempt to model cancer survival in countries or regions where population-based cancer registration data were not available. Cancer survival cannot be estimated or modelled by assuming that the health system is as effective as in some other country where population-based survival estimates are available. On the contrary, cancer survival estimates are required to assess the overall effectiveness of a country’s health system in the first place. For that, cancer registries are essential.
The survival estimates reported here are derived directly from the records of individual patients diagnosed with cancer, and from long-term follow-up to ascertain their vital status, followed by standardised quality control and central analysis. This is not a compilation of published reports or a meta-analysis.
Survival for most cancers remains among the highest in the world in the US, Canada, Australia and New Zealand, and in Finland, Iceland, Norway and Sweden. Publications that showed surprisingly low survival in Denmark78,79 prompted national cancer plans in 2000, 2005 and 2011, focused on early diagnosis and treatment to improve survival.80 From 2007, cancer was regarded as an acute life-threatening disease, leading to accelerated cancer-specific pathways for diagnosis, with public monitoring of hospitals‟ compliance with waiting times. For most cancers, survival has increased more in Denmark, and survival has nearly caught up with the other Nordic countries.81,82 Norway and Sweden have now established similar cancer patient pathways.
Cancer survival trends are generally increasing, even for some of the more lethal cancers. In some countries, survival increased up to 5% for liver, pancreas and lung cancers. For example, survival trends for liver cancer were generally stable during 1995 to 2014, but survival increased by more than 10% in Korea, Singapore and Norway.
However, where five-year survival remains extremely low in all countries (e.g. pancreatic cancer, range 5–15%), international efforts will be required to understand risk factors and improve prevention, but also to promote earlier diagnosis and better treatment, to improve outcomes. International comparisons of survival for pancreatic cancer include both ductal adenocarcinomas and the less common neuroendocrine tumours, for which survival is generally higher. The impact of variation in these proportions will require detailed analysis.
Age-standardised five-year net survival for stomach cancer was below 30% in most countries, but high in Korea (69%) and Japan (60%), where it increased by up to 10% between 2000–2004 and 2010–2014. This pattern is likely to be associated with longstanding population-based endoscopic screening programmes for early detection of gastric and oesophageal cancers, which are very common. Population awareness is high. Gastric cancer screening in Korea started in 1999 as part of the National Cancer Screening Programme, with biennial contrast radiology or endoscopy for adults aged 40 years or over.83 This doubles the chances of early diagnosis compared with unscreened patients.84 Endoscopic resection with clear margins may be curative in stage I oesophageal and gastric cancers (up to 2cm diameter), if invasion is limited to the superficial submucosa, and there is no lymphovascular invasion.85 By contrast, where gastric cancer is a less serious public health issue, and in the absence of screening, it is often diagnosed at an advanced stage. In Russia in 2015, for example, stomach cancer was most often diagnosed in stage IV (40%), and open laparotomy, chemotherapy and radiation were required for 22% and 25% of cases in stages II and III, respectively. Screening for oesophageal and gastric cancers should be considered as part of national cancer control plans where these tumours are common, or in high-risk populations.86
Survival trends for colorectal cancer were generally flat, or increasing, over the 20 years 1995–2014. Survival for rectal cancer was very similar among the Nordic countries (64–65%) and among most southern European countries (61%).
Survival from melanoma of the skin is generally lower in Asian populations than the rest of the world. One explanation may be lower public awareness, because melanoma is less common, but it may also be that Asian patients typically present with more advanced disease, and with acral lentiginous melanoma. This is one of the more lethal sub-types, and it is more common than in western populations.87 In the CONCORD data (not shown), acral lentiginous melanoma represents 1.2% of all skin melanomas, and 1% in Europe and North America, but 6% in Asia.
The increasing trend in five-year net survival from breast cancer during the 15 years 1995–2009 has continued in most countries up to 2014, but it remains lower in India, Thailand and several of the eastern European countries.
Five-year survival from cervical cancer has increased in several European and Asian countries. However, survival may even decline following an increase in diagnostic activity. In North America and Oceania, survival is lower than in other countries, due to more intensive screening programmes that detect precancerous cells and in situ tumours. These can be cured with a range of simple techniques, reducing cancer incidence by removal of the more indolent malignancies, while the more aggressive tumours are less likely to be detected by screening.
Some of the global range in survival may be attributable to differences in the intensity of diagnostic activity, and to over-diagnosis from the detection of very small or less aggressive tumours, that would not have been expected to lead to symptomatic diagnosis or death in the patient’s expected lifetime.88,89 As in CONCORD-2,6 we were unable to use the proportion of in situ cancers to compare the intensity of diagnostic activity for solid tumours. Some registries still do not record in situ tumours, while other registries did not submit data for in situ tumours.
Since screening programmes are only available in wealthier countries, mainly in selected age ranges for cancers of the breast, cervix and colon, the extent of over-diagnosis seems unlikely to have a large impact on the global range of cancer survival. Measures of over-diagnosis are only available at the population level, so their application in the interpretation of cancer survival patterns would be limited to ecological comparisons, as for GDP or total national expenditure on health. By contrast, data on stage at diagnosis are available for individuals. Analyses of the distribution of stage at diagnosis and stage-specific survival will be expected to provide further insight into international variation in cancer survival.90,91
Survival from the adult leukaemias up to 2009 in Asian populations was much lower than in Europe, North America and Oceania.6 One possible explanation was the relative rarity in Asian populations of chronic lymphocytic leukaemia (CLL), which has a relatively good prognosis in western populations. However, survival from CLL is also much lower in Taiwan than in the US,92 and the findings reported here also show that survival is generally lower in south-east Asia than in other countries in adults, for both myeloid and lymphoid malignancies. The difference between the median of the survival estimates for Asian populations and for other populations narrowed between 2000–2004 and 2010–2014, for both myeloid and lymphoid malignancies. In most south-east Asian countries, survival for myeloid malignancies has risen by 5–14%, and by 10% or more for lymphoid malignancies.
Survival from brain tumours in children is generally higher than for adults, but the global range is much more pronounced. Some of the international variation in survival from brain tumours may be due to variation in the proportion that are benign. Where benign tumours are registered, the proportion typically ranges up to 10–15% in both adults and children (data not shown). However, some registries do not record benign brain tumours, and this varies both between and within countries. For example, benign brain tumours are not registrable in New South Wales or Western Australia (45% of the national population), whereas they comprise up to 5% of brain tumours in Queensland and Victoria, with a similar combined population. The impact of morphology, behaviour and grade on international patterns of brain tumour survival needs further research.
International variation in survival for childhood lymphoma was less marked than for childhood ALL. The marked increase in five-year survival among children diagnosed with lymphoma in Brazil (from 69% in 2000–2004 to 88% in 2010–2014) may reflect a real improvement in diagnosis and treatment.
Cancer kills more than 100,000 children every year, mainly in low- and middle-income countries,93 where access to health services is often poor, and abandonment of treatment is a major problem.94,95 Reliable data on the cost and the effectiveness of health services in managing childhood cancer are scarce, yet such data would offer important evidence for countries to compare the impact of their strategies for managing children with cancer.96 Survival estimates published here for children diagnosed with a brain tumour, lymphoma or leukaemia will be deployed in a Lancet Oncology Commission on childhood cancer, designed to establish the evidence for investing in effective interventions to reduce the burden of childhood cancer.
Survival trends could not be systematically assessed in Africa. In some registries, the proportion of records with incomplete dates ranged up to 40%. Survival estimates for acute lymphoblastic leukaemia in Algeria were less reliable because follow-up was less than 5 years for more than 50% of children. For Nigeria (Ibadan) and South Africa (Eastern Cape), data were only available for 12 and 7 children, respectively, and survival was not estimated. Where survival could be estimated with some confidence, it was often very low, although survival in Mauritius was generally higher. In Nigeria, for example, there are no trained medical oncologists. Some haematologists and paediatric oncologists administer chemotherapy, but the availability of chemotherapy is limited in both the public and private sectors, and most patients pay out of their own pocket. The cost is prohibitive. These factors frequently disrupt treatment and may lead to poor outcomes.
To control for background mortality by age and sex, we updated the library of life tables for 1995–201097 by country, registry, race (selected countries) and calendar year to 2014, with a statistical summary for each set of life tables. It will shortly be available from the Cancer Survival Group web-site. In some countries, it has become more difficult to obtain the death and population counts required to construct life tables.
Survival estimates from CONCORD-2 for cancers of the breast and cervix were used in a recent Lancet Series on Women‟s Cancers,98,99 to help describe trends in the global burden of these cancers. Survival for the 2 million women diagnosed with one of these cancers every year remains highly dependent on the country in which they live. The Series highlighted the urgent need for more cost-effective cancer control strategies in low- and middle-income countries.
The global economic cost of treating the 12.9 million new cancer patients diagnosed worldwide in 2009 was estimated at US$286 billion.100 The costs of cancer treatment and care in the US alone were projected to rise by 23% between 2010 and 2020, from US$128 to US$158 billion, solely on the basis of demographic change, and with fixed incidence rates, survival probabilities and treatment costs.101 If treatment costs rise by 2% a year, the overall cost of treatment and care – in the US alone – could reach US$173 billion, a 39% increase. If incidence rates continue to rise, the prevalence of cancer survivors will increase further, triggering still further increase in the costs of care.
On the basis of these figures, it seems plausible that the global cost of cancer treatment and care in 2017 must already be substantially higher than US$300 billion a year. Spiralling costs102 threaten the viability of health systems and national economies. Where universal health coverage has not been achieved, the out-of-pocket costs can lead to financial catastrophe for individuals and families.3
The indirect economic costs associated with premature death and lost productivity from the growing cancer burden have been estimated at US$1.16 trillion a year,3 or approaching 2% of global GDP.103 It has been argued that the increasing cost and complexity of cancer treatment requires a radical shift in cancer policy, in which inequitable access to affordable cancer treatment ceases to be politically acceptable.104 Population-based data on cancer survival trends that are comparable within and between countries are part of the evidence base needed to drive such a policy shift.
With this background, cancer registries can be seen as efficient public health instruments, producing a continuous stream of valuable information for cancer control at low cost.105 In Europe in 2013, the average cost per patient registered, including the registry’s costs for personnel, IT and infrastructure, was €51 (range €6–213; US$59, range US$7–252). This is less than the typical cost of a chest X-ray. For the population as a whole, the cost was less than €1 (US$1.18) per person per year.
In 2015, the UN introduced 17 Sustainable Development Goals (SDG), aiming to end poverty, protect the planet, and ensure prosperity for all.106 Goal 3 is “to ensure healthy lives and promote well-being for all at all ages”. For this goal, target 3.4 is to reduce “premature” mortality (among persons aged 30–70 years) from non-communicable diseases, including cancer, by one-third, by 2030, through prevention and treatment.107 The challenge will be to secure overall improvements in health outcomes that do not lead to wider inequalities.108
Achieving the SDG target of a one-third reduction in premature mortality by 2030 clearly requires more effective prevention, to reduce cancer incidence. However, the 15-year time-frame is short, and achieving the target will also require investment in more effective health systems, to improve survival.46
WHO recently called for the development of population-based cancer registries, so that effective policies for cancer control can be founded on accurate data.3 It also called for stronger civil registration and vital statistics systems. These systems support the basic functions of government and enable measurement of progress towards development goals,109 yet population coverage is poor in low- and middle-income countries, and closely related to gross national income.110
Most cancer registries establish the vital status of all patients registered with cancer by linkage with vital statistics data (regional or national death indexes). This is known as passive follow-up, although many registries also contact patients’ doctors or families directly (active follow-up). For passive follow-up to work, efficient civil registration systems that capture information on all deaths are required. This underpins the estimation of population-based cancer survival, even though active follow-up can be effective in some populations. Yet cancer registries report increasing difficulty in linking their databases to regional or national death indexes. Legal and administrative obstacles and technical difficulties have all been reported. Some national authorities holding death indexes clearly give very low priority to such linkages.
These problems undermine the public health purpose of cancer registration. Of the 400 operational registries we contacted, more than 20 were unable to follow up all registered patients to ascertain their vital status. This problem arose in 16 countries, including some high-income countries. Some registries were unable to provide survival data at all. In Canada, for example, national coverage of cancer survival statistics was achieved for the first time in CONCORD-2,6 with data from all 13 provinces and territories for 1995–2009, but several jurisdictions were unable to participate in CONCORD-3 because of legal or administrative difficulties in linking their cancer registry with death records. For 8 countries that expressed interest or even submitted data, these difficulties meant that no survival estimates could be produced at all: Bénin, Bosnia-Herzegovina, Indonesia, Panama, the Philippines, Saudi Arabia, Serbia and Tunisia.
It is crucial for national and regional governments to recognise that population-based cancer registries are key policy tools, both to monitor the impact of cancer prevention strategies, and to evaluate the effectiveness of the health system for all patients diagnosed with cancer. All registries, especially those in low- and middle-income countries, need to be given adequate resources to register all patients with cancer in timely fashion, the right to access up-to-date national and regional death records to establish their vital status, and the legislative stability to operate efficiently over the long term.111
Supplementary Material
Panel: Research in context.
Evidence before this study
In 2015, the second cycle of the CONCORD programme established global surveillance of cancer survival, as one of the key metrics of the effectiveness of health systems and to inform global policy on cancer control. This was done by analysis of individual records for 25.7 million patients diagnosed with one of 10 common cancers during 1995–2009 and followed up to 31 December 2009. The data were provided by 279 population-based cancer registries in 67 countries.
CONCORD-2 revealed wide differences in cancer survival trends that were attributed to differences in access to early diagnosis and optimal treatment.
Added value of this study
CONCORD-3 covers almost one billion people world-wide. It includes 15 common cancers in adults and 3 common cancers in children. Data quality has improved. The results are timely: published within 3 years of the end of follow-up.
CONCORD-3 updates the world-wide surveillance of cancer survival to 2014. It includes data for over 37.5 million patients diagnosed with cancer during the 15-year period 2000–2014. Data were provided by over 320 population-based cancer registries in 71 countries and territories, including 26 countries of low or middle income; 47 countries provided data with 100% population coverage. The study now includes 18 cancers or groups of cancers: oesophagus, stomach, colon, rectum, liver, pancreas, lung, breast (women), cervix, ovary, prostate and melanoma of the skin in adults, together with brain tumours, leukaemias and lymphomas in both adults and children. These cancers represent 75% of all cancers diagnosed world-wide every year, in both low- and high-income countries.
The use of a similar study design and the same statistical methods enables the evaluation of survival trends for 10 cancers over the 20-year period 1995–2014. For the first time, worldwide trends in survival are also available for cancers of the oesophagus, pancreas, brain, and lymphomas and leukaemias.
Implications of all the available evidence
The CONCORD programme enables comparative evaluation of the effectiveness of health systems in providing cancer care. It also contributes to the evidence base for global policy on cancer control.
CONCORD monitors progress towards the overarching goal of the 2013 World Cancer Declaration, to achieve “major reductions in premature deaths from cancer, and improvements in quality of life and cancer survival” by 2020. It provides evidence to support WHO policy following the Cancer Resolution passed by the World Health Assembly in 2017.
The International Atomic Energy Agency’s Programme for Action on Cancer Therapy (PACT) used CONCORD-2 results in 2015 to launch its world-wide campaign to highlight the global divide in cancer survival, and to raise awareness of persistent inequalities in access to life-saving cancer services. The results were used in a Lancet Series on women’s cancers in 2016. The US Centers for Disease Control and Prevention has used the results in a 2017 supplement to the journal Cancer to inform cancer control policy designed to reduce racial differences in cancer survival.
CONCORD-3 can be expected to impact cancer control policy world-wide, especially in countries with low survival. The Organisation for Economic Co-operation and Development published CONCORD-3 results in 2017 as the official benchmark of cancer survival, among their indicators of the quality of health care in 48 countries world-wide. The survival estimates will also form part of The Lancet Oncology Commission on childhood cancer in 2018.
Future research will include examination of the impact of stage at diagnosis, compliance with treatment guidelines and the quality of healthcare on international differences in cancer survival.
Acknowledgments
This work was funded by Centers for Disease Control and Prevention (Atlanta GA, USA); Swiss Re (London, UK); Swiss Cancer Research foundation (Bern, Switzerland); Swiss Cancer League (Bern, Switzerland); Institut National du Cancer (Paris, France); La Ligue Contre le Cancer (Paris, France); Rossy Family Foundation (Montréal QC, Canada); National Cancer Institute (Bethesda MD, USA); American Cancer Society® (Atlanta GA, USA); Susan G Komen Foundation® (Dallas TX, USA).
We gratefully acknowledge the cancer registry personnel who have recorded the diagnosis and outcome for every cancer patient in their jurisdictions over many years: without their efforts, we would know very little about trends in the global cancer burden or the effectiveness of health systems in addressing it.
The protocol was translated into Arabic by Mufid El Mistiri (Qatar Cancer Registry) and Eiman Alawadhi (LSHTM); into Chinese by Ning Wang, Shuo Liu (Beijing Cancer Registry, China), Yannan Yuan (Beijing University Cancer Hospital, China) and Chun-Ju Chiang (Taiwan Cancer Registry); into French by Audrey Bonaventure and Michel Coleman (LSHTM); into Italian by Veronica Di Carlo, Cristina Renzi and Claudia Allemani (LSHTM); into Japanese by Tomohiro Matsuda (National Cancer Centre, Japan), Mari Kajiwara and Kayo Nakata (LSHTM); into Portuguese by Gulnar Azevedo e Silva (Rio de Janeiro, Brazil); into Russian by Daria Dubovichenko and Mikhail Valkov (Arkhangelsk Cancer Registry, Russian Federation), and into Spanish by Gustavo Hernandez Suarez (National Cancer Institute, Colombia), Natalia Sanz (LSHTM) and Enrique Barrios (Cancer Registry of Uruguay).
We are grateful for expert advice and ideas from many colleagues, including Marc Maynadié (Hémopathies Malignes de Côte d’Or, France) for advice on the classification of haematological malignancies; Amy Kahn (New York State Cancer Registry, USA), Ron Dewar (Cancer Care Nova Scotia, Canada) and Jennifer Stevens (National Cancer Institute, USA) for the program to convert NAACCR data structures to meet the CONCORD protocol; Angela Mariotto (National Cancer Institute, USA) for US mortality data, Reda Wilson (Centers for Disease Control and Prevention, USA) for assistance with the National Program of Cancer Registries, and Giovanni Luca Lo Magno (Caltanissetta, Italy) for the program to convert Stata output into Word® files. We also thank Gabriela Abriata (Instituto Nacional del Cáncer, Argentina); Cristian Herrera (Ministerio de Salud, Chile); Daniel Salas Peraza (Ministerio de Salud, Costa Rica); Noorlia Yahaya (Penang State Health Department, Malaysia); Niek Klazinga and Rie Fujisawa (OECD, France), and Steve Scoppa (Information Management Services, Inc., USA). We thank our LSHTM colleagues Natalia Sanz (CONCORD Programme Manager to March 2017), Lisa Montel (CONCORD Programme Manager from April 2017), Yuki Alencar (Cancer Survival Group Coordinator), Adrian Turculeţ for maps and database management, and Hakim Miah for the CONCORD file transmission utility.
We gratefully acknowledge endorsement of CONCORD by the following agencies: American Cancer Society® (Atlanta GA, USA); Asociación Española contra el Cáncer (aecc) (Madrid, Spain); Association of European Cancer Leagues (ECL) (Brussels, Belgium); Canadian Association of Provincial Cancer Agencies (CAPCA) (Toronto, Canada); Canadian Council of Cancer Registries (Toronto, Canada); Childhood Cancer International (CCI) (Nieuwegein, the Netherlands); Children with Cancer UK (London, UK); Danish Cancer Society (Copenhagen, Denmark); European CanCer Organisation (ECCO) (Brussels, Belgium); European Cancer Patient Coalition (ECPC) (Brussels, Belgium); European Institute for Women’s Health (Dublin, Ireland); European Society for Medical Oncology (ESMO) (Lugano, Switzerland); Fondation de France (Paris, France); International Agency for Research on Cancer (IARC) (Lyon, France); International Atomic Energy Agency (IAEA) (Vienna, Austria); International Network for Cancer Treatment and Research (INCTR) (Brussels, Belgium); International SOS (Papua, Indonesia); Israel Centre for Disease Control (Tel-Hashomer, Israel); Jolanta Kwaśniewska’s Foundation (Warsaw, Poland); Liga Argentina de Lucha contra el Cancer (LALCEC) (Buenos Aires, Argentina); Members of the European Parliament Against Cancer (MAC) (Brussels, Belgium); National Cancer Institute (NCI) Center for Global Health (Bethesda MD, USA); National Cancer Research Institute (NCRI) Consumer Liaison Group (Leeds, UK); National Institute for Cancer Epidemiology and Registration (NICER) (Zürich, Switzerland); NCD Asia Pacific Alliance (NCDAPA) (Tokyo, Japan); North American Association of Central Cancer Registries (NAACCR) (Springfield IL, USA); Organisation for Economic Co-operation and Development (OECD) (Paris, France); Société Internationale d’Oncologie Pédiatrique (SIOP) (Geneva, Switzerland); Union for International Cancer Control (UICC) (Geneva, Switzerland); WHO Regional Office for Europe (WHO-EURO) (Copenhagen, Denmark); World Bank (Washington DC, USA).
The interpretation of the findings in this report, and the opinions, conclusions and recommendations are those of the authors, and do not necessarily reflect the views or official position of the British Columbia Cancer Agency or Cancer Care Ontario (Canada); the Centers for Disease Control and Prevention, the National Cancer Institute, Maryland Cancer Registry, New Hampshire Department of Health and Human Services, New York City Department of Health and Mental Hygiene, Ohio Department of Health, Pennsylvania Department of Health, West Virginia Cancer Registry, or the Susan G Komen® Foundation (USA); the Health Directorate of the Australian Capital Territory, or the Institut National du Cancer (France).
Funding: American Cancer Society® (Atlanta GA, USA); Centers for Disease Control and Prevention (Atlanta GA, USA); Swiss Re (London, UK); Swiss Cancer Research foundation (Bern, Switzerland); Swiss Cancer League (Bern, Switzerland); Institut National du Cancer (Paris, France); La Ligue Contre le Cancer (Paris, France); Rossy Family Foundation (Montréal QC, Canada); National Cancer Institute (Bethesda MD, USA); Susan G Komen Foundation® (Dallas TX, USA).
Abbreviations
- ALL
acute lymphoblastic leukaemia
- CDC
US Centers for Disease Control and Prevention
- DCO
Death Certificate Only registration
- IACR
International Association of Cancer Registries
- IARC
International Agency for Research on Cancer
- ICD-O
International Classification of Diseases for Oncology
- NAACCR
North American Association of Central Cancer Registries
- NPCR
National Program of Cancer Registries
- SDG
Sustainable Development Goals
- SEER
Surveillance, Epidemiology and End Results programme
- TNM
Tumour Nodes Metastasis
- UN
United Nations
- WHO
World Health Organisation
CONCORD Working Group
Africa—Algeria: S Bouzbid (Registre du Cancer d’Annaba); M Hamdi-Chérif*, Z Zaidi (Registre du Cancer de Sétif); K Meguenni, D Regagba (Registre du Cancer Tlemcen); Mali: S Bayo, T Cheick Bougadari (Kankou Moussa University); Mauritius: SS Manraj (Mauritius National Cancer Registry); Morocco: K Bendahhou (Registre du Cancer du Grand Casablanca); Nigeria: A Fabowale, OJ Ogunbiyi* (Ibadan Cancer Registry); South Africa: D Bradshaw, NIM Somdyala (Eastern Cape Province Cancer Registry)
America (Central and South)—Argentina: I Kumcher, F Moreno (National Childhood Cancer Registry); GH Calabrano, SB Espinola (Chubut Cancer Registry); B Carballo Quintero, R Fita (Registro Provincial de Tumores de Córdoba); MC Diumenjo, WD Laspada (Registro Provincial de Tumores de Mendoza); SG Ibañez (Population Registry of Cancer of the Province Tierra del Fuego); Brazil: CA Lima (Registro de Câncer de Base Populacional de Aracaju); PCF De Souza (Registro de Câncer de Base Populacional de Cuiabá); K Del Pino, C Laporte (Registro de Curitiba); MP Curado, JC de Oliveira (Registro de Goiânia); CLA Veneziano, DB Veneziano (Registro de Câncer de Base Populacional de Jaú); MRDO Latorre, LF Tanaka (Registro de Câncer de São Paulo); MS Rebelo, MO Santos (Instituto Nacional de Câncer, Rio de Janeiro); G Azevedo e Silva* (University of Rio de Janeiro); Chile: JC Galaz (Registro Poblacional de Cáncer Region de Antofagasta); M Aparicio Aravena, J Sanhueza Monsalve (Registro Poblacional de Cáncer de la Provincia de Biobio; Registro Poblacional de Cáncer Provincia de Concepción); DA Herrmann, S Vargas (Registro Poblacional Region de Los Rios); Colombia: VM Herrera, CJ Uribe (Registro Poblacional de Cáncer Area Metropolitana de Bucaramanga); LE Bravo, LS Garcia (Cali Cancer Registry); NE Arias-Ortiz, D Morantes (Registro Poblacional de Cáncer de Manizales); DM Jurado, MC Yépez Chamorro (Registro Poblacional de Cáncer del Municipio de Pasto); Costa Rica: S Delgado, M Ramirez (National Registry of Tumors, Costa Rica); Cuba: YH Galán Alvarez, P Torres (Registro Nacional de Cáncer de Cuba); Ecuador: F Martínez-Reyes (Cuenca Tumor Registry); L Jaramillo, R Quinto (Guayaquil Cancer Registry); J Castillo (Loja Cancer Registry); M Mendoza (Manabí Cancer Registry); P Cueva, JG Yépez (Quito Cancer Registry); France: B Bhakkan, J Deloumeaux (Registre des cancers de la Guadeloupe); C Joachim, J Macni (General Cancer Registry of Martinique); Mexico: R Carrillo, J Shalkow Klincovstein (Centro Nacional para la Salud de la Infancia y la Adolescencia); R Rivera Gomez (Registro Poblacional de Cancer Region Fronteriza Norte de Mexico Zona Tijuana); Peru: E Poquioma (Lima Metropolitan Cancer Registry); Puerto Rico: G Tortolero-Luna, D Zavala (Puerto Rico Central Cancer Registry); Uruguay: R Alonso, E Barrios (Registro Nacional de Cáncer)
America (North)—Canada: A Eckstrand, C Nikiforuk (Alberta Cancer Registry); RR Woods (British Columbia Cancer Registry); G Noonan, D Turner* (Manitoba Cancer Registry); E Kumar, B Zhang (New Brunswick Provincial Cancer Registry); FR McCrate, S Ryan (Newfoundland & Labrador Cancer Registry); M MacIntyre, N Saint-Jacques (Nova Scotia Cancer Registry); DE Nishri* (Ontario Cancer Registry); CA McClure, KA Vriends (Prince Edward Island Cancer Registry); S Kozie, H Stuart-Panko (Saskatchewan Cancer Agency); USA: T Freeman, JT George (Alabama Statewide Cancer Registry); JT Brockhouse, DK O’Brien (Alaska Cancer Registry); A Holt (Arkansas Central Cancer Registry); L Almon (Metropolitan Atlanta Registry); S Kwong, C Morris (California State Cancer Registry); R Rycroft (Colorado Central Cancer Registry); L Mueller, CE Phillips (Connecticut Tumor Registry); H Brown, B Cromartie (Delaware Cancer Registry); AG Schwartz, F Vigneau (Metropolitan Detroit Cancer Surveillance System); GM Levin, B Wohler (Florida Cancer Data System); R Bayakly (Georgia Cancer Registry); KC Ward (Georgia Cancer Registry; Metropolitan Atlanta Registry); SL Gomez, M McKinley (Greater Bay Area Cancer Registry); R Cress (Cancer Registry of Greater California); MD Green, K Miyagi (Hawaii Tumor Registry); CJ Johnson (Cancer Data Registry of Idaho); LP Ruppert (Indiana State Cancer Registry); CF Lynch (State Health Registry of Iowa); B Huang, TC Tucker* (Kentucky Cancer Registry); D Deapen, L Liu (Los Angeles Cancer Surveillance Program); MC Hsieh, XC Wu (Louisiana Tumor Registry); M Schwenn (Maine Cancer Registry); ST Gershman, RC Knowlton (Massachusetts Cancer Registry); G Alverson, GE Copeland (Michigan State Cancer Surveillance Program); S Bushhouse (Minnesota Cancer Surveillance System); DB Rogers (Mississippi Cancer Registry); J Jackson-Thompson (Missouri Cancer Registry and Research Center); D Lemons, HJ Zimmerman (Montana Central Tumor Registry); M Hood, J Roberts-Johnson (Nebraska Cancer Registry); JR Rees, B Riddle (New Hampshire State Cancer Registry); KS Pawlish, A Stroup (New Jersey State Cancer Registry); C Key, C Wiggins (New Mexico Tumor Registry); AR Kahn, MJ Schymura (New York State Cancer Registry); S Radhakrishnan, C Rao (North Carolina Central Cancer Registry); LK Giljahn, RM Slocumb (Ohio Cancer Incidence Surveillance System); RE Espinoza, F Khan (Oklahoma Central Cancer Registry); KG Aird, T Beran (Oregon State Cancer Registry); JJ Rubertone, SJ Slack (Pennsylvania Cancer Registry); L Garcia, DL Rousseau (Rhode Island Cancer Registry); TA Janes, SM Schwartz (Seattle Cancer Surveillance System); SW Bolick, DM Hurley (South Carolina Central Cancer Registry); MA Whiteside (Tennessee Cancer Registry); P Miller-Gianturco, MA Williams (Texas Cancer Registry); K Herget, C Sweeney (Utah Cancer Registry); AT Johnson (Vermont Cancer Registry); MB Keitheri Cheteri, P Migliore Santiago (Washington State Cancer Registry); SE Blankenship, S Farley (West Virginia Cancer Registry); R Borchers, R Malicki (Wisconsin Department of Health Services); JR Espinoza, J Grandpre (Wyoming Cancer Surveillance Program); HK Weir*, R Wilson (Centers for Disease Control and Prevention); BK Edwards*, A Mariotto (National Cancer Institute)
Asia—China: Y Lei, N Wang (Beijing Cancer Registry); JS Chen, Y Zhou (Changle City Cancer Registry); YT He, GH Song (Cixian Cancer Registry); XP Gu (Dafeng County Center for Disease Control and Prevention); D Mei, HJ Mu (Dalian Centers for Disease Prevention and Control); HM Ge, TH Wu (Donghai County Center for Disease Prevention and Control); YY Li, DL Zhao (Feicheng County Cancer Registry); F Jin, JH Zhang (Ganyu Center for Disease Prevention and Control); FD Zhu (Guanyun Cancer Registry); Q Junhua, YL Yang (Haimen Cancer Registry); CX Jiang (Haining City Cancer Registry); W Biao, J Wang (Jianhu Cancer Registry); QL Li (Jiashan County Cancer Registry); H Yi, X Zhou (Jintan Cancer Registry); J Dong, W Li (Lianyungang Center for Disease Prevention and Control); FX Fu, SZ Liu (Linzhou Cancer Registry); JG Chen, J Zhu (Qidong County Cancer Registry); YH Li, YQ Lu (Sihui Cancer Registry); M Fan, SQ Huang (Taixing Cancer Registry); GP Guo, H Zhaolai (Cancer Institute of Yangzhong City); K Wei (Zhongshan City Cancer Registry); WQ Chen*, H Zeng (The National Cancer Center); Cyprus: AV Demetriou (Cyprus Cancer Registry); Hong Kong: WK Mang, KC Ngan (Hong Kong Cancer Registry); India: AC Kataki, M Krishnatreya (Guwahati Cancer Registry); PA Jayalekshmi, P Sebastian (Karunagappally Cancer Registry); A Nandakumar* (National Centre for Disease Informatics and Research); Iran: R Malekzadeh, G Roshandel (Golestan Population-based Cancer Registry); Israel: L Keinan-Boker, BG Silverman (Israel National Cancer Registry); Japan: H Ito, H Nakagawa (Aichi Cancer Registry); M Sato, F Tobori (Akita Prefectural Cancer Registry); I Nakata, N Teramoto (Ehime Prefectural Cancer Registry); M Hattori, Y Kaizaki (Fukui Cancer Registry); F Moki (Gunma Prefectural Cancer Registry); H Sugiyama, M Utada (Hiroshima Prefecture Cancer Registry); M Nishimura, K Yoshida (Hyogo Prefectural Cancer Registry); K Kurosawa, Y Nemoto (Ibaraki Prefectural Cancer Registry); H Narimatsu, M Sakaguchi (Kanagawa Cancer Registry); S Kanemura (Miyagi Prefectural Cancer Registry); M Naito, R Narisawa (Niigata Prefecture Cancer Registry); I Miyashiro, K Nakata (Osaka Cancer Registry); S Sato, M Yoshii (Saga Prefectural Cancer Registry); I Oki (Tochigi Prefectural Cancer Registry); N Fukushima, A Shibata (Yamagata Prefectural Cancer Registry); K Iwasa, C Ono (Yamanashi Cancer Registry); T Matsuda* (National Cancer Center); Jordan: O Nimri (Jordan National Cancer Registry); Korea: KW Jung, YJ Won (Korea Central Cancer Registry); Kuwait: E Alawadhi, A Elbasmi (Kuwait Cancer Registry); Malaysia: A Ab Manan (Malaysia National Cancer Registry); F Adam (Penang Cancer Registry); Mongolia: E Sanjaajmats, U Tudev (Cancer Registry of Mongolia); C Ochir (Mongolian National University of Medical Sciences); Qatar: AM Al Khater, MM El Mistiri (Qatar Cancer Registry); Singapore: GH Lim, YY Teo (Singapore Cancer Registry); Taiwan: CJ Chiang, WC Lee (Taiwan Cancer Registry); Thailand: R Buasom, S Sangrajrang (Bangkok Cancer Registry); S Kamsa-ard, S Wiangnon (Khon Kaen Provincial Cancer Registry); K Daoprasert, D Pongnikorn (Lampang Cancer Registry; Lamphun Cancer Registry); A Leklob, S Sangkitipaiboon (Lopburi Cancer Registry); SL Geater, H Sriplung (Songkhla Cancer Registry); Turkey: O Ceylan, I Kög (Ankara Cancer Registry); O Dirican (Antalya Cancer Registry); T Köse (Bursa Cancer Registry); T Gurbuz (Edirne Cancer Registry); FE Karaşahin, D Turhan (Erzurum Cancer Registry Center); U Aktaş, Y Halat (Eskişehir Cancer Registry); S Eser, CI Yakut (Izmir Cancer Registry); M Altinisik, Y Cavusoglu (Samsun Cancer Registry); A Türkköylü, N Üçüncü (Trabzon Cancer Registry) Europe—Austria: M Hackl (Austrian National Cancer Registry); Belarus: AA Zborovskaya (Belarus Childhood Cancer Subregistry); OV Aleinikova (Belarusian Research Center for Pediatric Oncology, Hematology and Immunology); Belgium: K Henau, L Van Eycken (Belgian Cancer Registry); Bulgaria: Z Valerianova, MR Yordanova (Bulgarian National Cancer Registry); Croatia: M Šekerija (Croatian National Cancer Registry); Czech Republic: L Dušek, M Zvolský (Czech National Cancer Registry); Denmark: G Engholm, H Storm* (Danish Cancer Society); Estonia: K Innos, M Mägi (Estonian Cancer Registry); Finland: N Malila, K Seppä (Cancer Society of Finland); France: J Jégu, M Velten (Bas-Rhin General Cancer Registry); E Cornet, X Troussard (Registre Régional des Hémopathies Malignes de Basse Normandie); AM Bouvier (Registre Bourguignon des Cancers Digestifs); AV Guizard (Registre Général des Tumeurs du Calvados); V Bouvier, G Launoy (Registre des Tumeurs Digestives du Calvados); P Arveux (Breast cancers registry of Côte-d’Or France); M Maynadié, M Mounier (Hémopathies Malignes de Côte d’Or); AS Woronoff (Doubs and Belfort Territory General Cancer Registry); M Daoulas, M Robaszkiewicz (Finistère Cancer Registry); J Clavel, S Goujon (French National Registry of Childhood Hematopoietic Malignancies); B Lacour (National Registry of Childhood Solid Tumors); I Baldi, C Pouchieu (Gironde Registry of Primary Central Nervous System Tumors); B Amadeo, G Coureau (General Cancer Registry of Gironde Department); A Monnereau (Registre des Hémopathies Malignes de la Gironde; French Network of Cancer Registries (FRANCIM)); S Orazio (Registre des Hémopathies Malignes de la Gironde); PM Preux, F Rharbaoui (Registre Général des Cancers de Haute-Vienne); E Marrer (Haut-Rhin Cancer Registry); B Trétarre (Registre des Tumeurs de l’Hérault); M Colonna, P Delafosse (Registre du Cancer du Département de l’Isère); K Ligier, S Plouvier (Registre Général des Cancers de Lille et de sa Region); A Cowppli-Bony, F Molinié (Loire-Atlantique-Vendée Cancer Registry); S Bara (Manche Cancer Registry); O Ganry, B Lapôtre-Ledoux (Registre du Cancer de la Somme); P Grosclaude (Tarn Cancer Registry); N Bossard, Z Uhry (Hospices Civils de Lyon); F Bray*, M Piñeros* (International Agency for Research on Cancer); J Estève (Université Claude Bernard, Lyon); Germany: R Stabenow, H Wilsdorf-Köhler (Common Cancer Registry of the Federal States); A Eberle, S Luttmann (Bremen Cancer Registry); I Löhden, AL Nennecke (Hamburg Cancer Registry); J Kieschke, E Sirri (Epidemiological Cancer Registry of Lower Saxony); K Emrich, SR Zeissig (Rhineland Palatinate Cancer Registry); B Holleczek (Saarland Cancer Registry); N Eisemann, A Katalinic (Schleswig-Holstein Cancer Registry); Gibraltar: RA Asquez, V Kumar (Gibraltar Cancer Registry); Greece: E Petridou (Nationwide Registry for Childhood Haematological Malignancies and Solid Tumors); Iceland: EJ Ólafsdóttir, L Tryggvadóttir (Icelandic Cancer Registry, Icelandic Cancer Society); Ireland: K Clough-Gorr, PM Walsh (National Cancer Registry Ireland); H Sundseth* (European Institute of Women‟s Health); Italy: G Mazzoleni, F Vittadello (Registro Tumori Alto Adige); E Coviello, F Cuccaro (Registro Tumori Puglia – Sezione ASL BT); R Galasso (Registro Tumori di Basilicata); G Sampietro (Registro Tumori di Bergamo); A Giacomin† (Piedmont Cancer Registry Provinces of Biella and Vercelli); M Magoni (Registro Tumori Dell’ASL Di Brescia); A Ardizzone (Registro Tumori Brindisi); A D’Argenzio (Caserta Cancer Registry); M Castaing, G Grosso (Integrated Cancer Registry of Catania-Messina-Siracusa-Enna); AM Lavecchia, A Sutera Sardo (Registro Tumori Catanzaro); G Gola (Registro Tumori della Provincia di Como); L Gatti, P Ricci (Registro Tumori Cremona; Registro Tumori Mantova); S Ferretti (Registro Tumori della Provincia di Ferrara); D Serraino, A Zucchetto (Registro Tumori del Friuli Venezia Giulia); MV Celesia, RA Filiberti (Registro Tumori Regione Liguria); F Pannozzo (Registro Tumori della Provincia di Latina); A Melcarne, F Quarta (Registro Tumori Della Provincia Di Lecce Sezione RTP); AG Russo (Registro Tumori Milano); G Carrozzi, C Cirilli (Registro Tumori della Provincia di Modena); L Cavalieri d’Oro, M Rognoni (Registro Tumori di Monza e Brianza); M Fusco, MF Vitale (Registro Tumori della ASL Napoli 3 Sud); M Usala (Nuoro Cancer Registry); R Cusimano, W Mazzucco (Registro Tumori di Palermo e Provincia); M Michiara, P Sgargi (Registro Tumori della Provincia di Parma); L Boschetti (Cancer Registry of the province of Pavia); E Borciani, P Seghini (Registro Tumori Piacenza); MM Maule, F Merletti (Piedmont Childhood Cancer Registry); R Tumino (Registro Tumori della Provincia di Ragusa); P Mancuso, M Vicentini (Registro Tumori Reggio Emilia); T Cassetti, R Sassatelli (Reggio Emilia Cancer Registry (Pancreas)); F Falcini, S Giorgetti (Registro Tumori della Romagna); AL Caiazzo, R Cavallo (Registro Tumori Salerno); R Cesaraccio, DR Pirino (Registro Tumori della Provincia di Sassari); ML Contrino, F Tisano (Registro Tumori Siracusa); AC Fanetti, S Maspero (Registro Tumori della Provincia di Sondrio); S Carone, A Mincuzzi (Registro Tumori Taranto); G Candela, T Scuderi (Registro Tumori Trapani); MA Gentilini, S Piffer (Registro Tumori Trento); S Rosso (Piedmont Cancer Registry); A Barchielli, A Caldarella (Registro Tumori della Regione Toscana); F Bianconi, F Stracci (Registro Tumori Umbro di Popolazione); P Contiero, G Tagliabue (Registro Tumori Lombardia, Provincia di Varese); M Rugge, M Zorzi (Registro Tumori Veneto); S Beggiato, A Brustolin (Registro Tumori Della Provincia Di Viterbo); F Berrino*, G Gatta, M Sant* (Fondazione IRCCS Istituto Nazionale dei Tumori); C Buzzoni, L Mangone (Italian Association of Cancer Registries (AIRTUM)); R Capocaccia*, R De Angelis (National Centre for Epidemiology); R Zanetti* (International Association of Cancer Registries; Piedmont Cancer Registry); Latvia: A Maurina, S Pildava (Latvian Cancer Registry); Lithuania: N Lipunova, I Vincerževskienė (Lithuanian Cancer Registry); Malta: D Agius, N Calleja (Malta National Cancer Registry); Netherlands: S Siesling, O Visser (Netherlands Cancer Registry, IKNL); Norway: S Larønningen, B Møller (The Cancer Registry of Norway); Poland: A Dyzmann-Sroka, M Trojanowski (Greater Poland Cancer Registry); S Góźdź, R Mężyk (Holy Cross Cancer Registry); T Mierzwa (Kuiavian-Pomeranian Cancer Registry); L Molong, J Rachtan (Lesser Poland Cancer Registry); S Szewczyk (Łódź Cancer Registry); J Błaszczyk, K Kępska (Lower Silesian Cancer Registry); B Kościańska (Lublin Cancer Registry); K Tarocińska (Lubush Cancer Registry); M Zwierko (Mazovian Cancer Registry); K Drosik (Opole Cancer Registry); KM Maksimowicz, E Purwin-Porowska (Podlahian Cancer Registry); E Reca, J Wójcik-Tomaszewska (Pomeranian Cancer Registry); A Tukiendorf (Silesian Cancer Registry); M Grądalska-Lampart, AU Radziszewska (Subcarpathian Cancer Registry); A Gos (Varmian-Mazurian Cancer Registry); M Talerczyk, M Wyborska (West-Pomeranian Cancer Registry); JA Didkowska, U Wojciechowska (National Cancer Registry); M Bielska-Lasota (National Institute of Public Health, NIH); Portugal: G Forjaz de Lacerda, RA Rego (Registo Oncológico Regional dos Açores); J Bastos, MA Silva (Registo Oncológico Regional do Centro); L Antunes, J Laranja Pontes (Registo Oncológico Regional do Norte); A Mayer-da-Silva, A Miranda (Registo Oncólogico Regional do Sul); Romania: LM Blaga, D Coza (Cancer Institute I. Chiricuta); Russia: MY Valkov (Arkhangelsk Regional Cancer Registry); L Gusenkova, O Lazarevich (Population Cancer Registry of the Republic of Karelia); O Prudnikova, DM Vjushkov (Omsk Regional Cancer Registry); AG Egorova, AE Orlov (Samara Cancer Regional Registry); LA Kudyakov, LV Pikalova (Tomsk Regional Cancer Registry); Slovakia: J Adamcik, C Safaei Diba (National Cancer Registry of Slovakia); Slovenia: M Primic- Žakelj, V Zadnik (Cancer Registry of Republic of Slovenia); Spain: N Larrañaga, A Lopez de Munain (Basque Country Cancer Registry); AA Herrera, R Redondas (Registro Poblacional de Cáncer de la Comunidad Autónoma de Canarias); R Marcos-Gragera, ML Vilardell Gil (Epidemiology Unit and Girona Cancer Registry); E Molina, MJ Sánchez Perez (Granada Cancer Registry); P Franch Sureda, M Ramos Montserrat (Mallorca Cancer Registry); MD Chirlaque, C Navarro (Murcia Cancer Registry); EE Ardanaz, MM Guevara (Registro de Cáncer de Navarra); R Fernández-Delgado, R Peris-Bonet (Registro Español de Tumores Infantiles); M Carulla, J Galceran (Tarragona Cancer Registry); C Alberich, M Vicente-Raneda (Comunitat Valenciana Childhood Cancer Registry); Sweden: S Khan, D Pettersson (Swedish Cancer Registry); P Dickman* (Karolinska Institutet, Stockholm); Switzerland: I Avelina, K Staehelin (Basel Cancer Registry); B Camey (Registre Fribourgeois des Tumeurs); C Bouchardy, R Schaffar (Geneva Cancer Registry); H Frick, C Herrmann (Cancer Registry Grisons and Glarus; Cancer Registry of St Gallen-Appenzell); JL Bulliard, M Maspoli-Conconi (Registre Neuchâtelois et Jurassien des Tumeurs); CE Kuehni, SM Redmond (Swiss Childhood Cancer Registry); A Bordoni, L Ortelli (Registro Tumori Canton Ticino); A Chiolero, I Konzelmann (Registre Valaisan des Tumeurs); KL Matthes, S Rohrmann (Cancer Registry Zürich and Zug); United Kingdom: J Broggio, J Rashbass (National Cancer Registration and Analysis Service England); D Fitzpatrick, A Gavin (Northern Ireland Cancer Registry); DI Clark, AJ Deas (Scottish Cancer Registry); DW Huws, C White (Welsh Cancer Intelligence & Surveillance Unit); C Allemani*, A Bonaventure, MP Coleman*, V Di Carlo, R Harewood, M Matz, L Montel, M Nikńić, B Rachet*, AD Turculeț (London School of Hygiene & Tropical Medicine); R Stephens* (National Cancer Research Institute, London); C Stiller* (Public Health England)
Oceania—Australia: E Chalker, H Phung (Australian Capital Territory Cancer Registry); R Walton, H You (NSW Central Cancer Registry); S Guthridge, F Johnson (Northern Territory of Australia Cancer Registry); J Aitken, P Gordon (Queensland Cancer Registry); K D’Onise, K Priest (South Australian Cancer Registry); BC Stokes, A Venn (Tasmanian Cancer Registry); H Farrugia, V Thursfield (Victorian Cancer Registry); J Dowling (Western Australian Cancer Registry); D Currow* (Cancer Institute NSW); New Zealand: J Hendrix, C Lewis (New Zealand Cancer Registry)
* CONCORD Steering Committee
† Dr A Giacomin passed away on 23 March 2017.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
CA, AB, CS and MPC drafted the protocol; CA and MPC obtained statutory and ethical approvals; GAS, WQC, GE, SE, CJJ, GHL, AM, TM, OJO, MV and HKW contributed to data acquisition; CA, VDC and MPC prepared the life tables; CA, VDC, RH, MM, MN, AB and MPC had access to all the raw data; CA, VDC, RH, MM, MN, AB, CJJ and MPC did the data preparation, quality control and analyses, and CA, VDC, RH, MM, MN, AB, JA, GE, JE, SE, OV, RW and MPC checked the results; CA and MPC drafted the report. All authors contributed to writing the final report and approved the version to be published. All members of the CONCORD Working Group had access to the results of all steps of data preparation, quality control and analyses, and contributed to interpretation of the findings.
Conflicts of interest
We declare no conflicts of interest.
References
- 1.Schottenfeld D, Fraumeni JF, editors. Cancer epidemiology and prevention. 3rd. Oxford: Oxford University Press; 2006. [Google Scholar]
- 2.International Agency for Research on Cancer. GLOBOCAN 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012. Lyon: IARC; http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx?cancer=stomach (accessed 25 September 2017). [Google Scholar]
- 3.World Health Organisation. Cancer prevention and control in the context of an integrated approach: report by the Secretariat. Geneva: WHO; 2016. http://apps.who.int/gb/ebwha/pdf_files/EB140/B140_31-en.pdf (accessed 25 September 2017) [Google Scholar]
- 4.World Health Organisation. Cancer prevention and control [WHA 58.22] Geneva: WHO; 2017. (accessed 25 September 2017) [Google Scholar]
- 5.Vázquez TR, Ghebreyesus TA. Beating NCDs can help deliver universal health coverage. Lancet. 2017;390:1473–4. doi: 10.1016/S0140-6736(17)32470-4. [DOI] [PubMed] [Google Scholar]
- 6.Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang X-S, Bannon F, Ahn JV, Johnson CJ, Bonaventure A, Marcos-Gragera R, Stiller C, Azevedo e Silva G, Chen W-Q, Ogunbiyi OJ, Rachet B, Soeberg MJ, You H, Matsuda T, Bielska-Lasota M, Storm H, Tucker TC, Coleman MP, CONCORD Working Group Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet. 2015;385:977–1010. doi: 10.1016/S0140-6736(14)62038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harlan LC, Warren JL. Global survival patterns: potential for cancer control. Lancet. 2015;385:926–8. doi: 10.1016/S0140-6736(14)62251-0. [DOI] [PubMed] [Google Scholar]
- 8.Walters S, Benitez-Majano S, Muller P, Coleman MP, Allemani C, Butler J, Peake M, Guren MG, Glimelius B, Bergström S, Påhlman L, Rachet B. Is England closing the international gap in cancer survival? Br J Cancer. 2015;113:848–60. doi: 10.1038/bjc.2015.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Independent Cancer Taskforce. Achieving world-class cancer outcomes: a strategy for England 2015–2020. London: NHS England; 2015. (accessed 23 March 2016) [Google Scholar]
- 10.International Atomic Energy Agency. PACT’s new campaign raises awareness of the persistent inequalities in access to lifesaving cancer services: PACT highlights the growing global divide in cancer survival rates. Vienna: IAEA; 2015. [Google Scholar]
- 11.Weir HK, Stewart S, Allemani C, White M, Thomas C, White A, Coleman MP. Population-based cancer survival 2001-2009 in the United States: findings from the CONCORD-2 study. Cancer. 2017:xx–yy. doi: 10.1002/cncr.31028. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allemani C, Coleman MP. Public health surveillance of cancer survival in the US and world-wide: the contribution of the CONCORD programme. Cancer. 2017 doi: 10.1002/cncr.30854. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 14.Fritz AG, Percy C, Jack A, Shanmugaratnam K, Sobin LH, Parkin DM, Whelan SL, editors. International Classification of Diseases for Oncology (ICD-O) 3rd. Geneva: World Health Organization; 2000. [Google Scholar]
- 15.Fritz AG, Percy C, Jack A, Shanmugaratnam K, Sobin LH, Parkin DM, Whelan SL. International Classification of Diseases for Oncology (ICD-O) Geneva: World Health Organisation; 2013. First revision of 3rd edn. [Google Scholar]
- 16.Matz M, Coleman MP, Sant M, Chirlaque López MD, Visser O, Gore M, Allemani C, the CONCORD Working Group The histology of ovarian cancer: world-wide distribution and implications for international survival comparisons (CONCORD-2) Gynecol Oncol. 2017;144:405–13. doi: 10.1016/j.ygyno.2016.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sant M, Karjalainen-Lindsberg ML, Maynadié M, Raphael M, Ferretti S, Giacomin A, Tereanu C, Giraldo P, Marcos-Gragera R, Martos C, Lutz JM, Visser O, HAEMACARE Working Group Manual for coding and reporting haematological malignancies. Tumori. 2010;96:i–A32. [PubMed] [Google Scholar]
- 18.Morton LM, Turner JJ, Cerhan JR, Linet MS, Treseler PA, Clarke CA, Jack A, Cozen W, Maynadie M, Spinelli JJ, Costantini AS, Rudiger T, Scarpa A, Zheng T, Weisenburger DD. Proposed classification of lymphoid neoplasms for epidemiologic research from the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph) Blood. 2007;110:695–708. doi: 10.1182/blood-2006-11-051672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turner JJ, Morton LM, Linet MS, Clarke CA, Kadin ME, Vajdic CM, Monnereau A, Maynadie M, Chiu BC, Marcos-Gragera R, Costantini AS, Cerhan JR, Weisenburger DD. InterLymph hierarchical classification of lymphoid neoplasms for epidemiologic research based on the WHO classification (2008): update and future directions. Blood. 2010;116:e90–8. doi: 10.1182/blood-2010-06-289561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P. International Classification of Childhood Cancer, third edition. Cancer. 2005;103:1457–67. doi: 10.1002/cncr.20910. [DOI] [PubMed] [Google Scholar]
- 21.Woods LM, Rachet B, Ellis L, Coleman MP. Full dates (day, month, year) should be used in population-based cancer survival studies. Int J Cancer. 2012;131:E1120–E4. doi: 10.1002/ijc.27545. [DOI] [PubMed] [Google Scholar]
- 22.Surveillance Epidemiology and End Results program Multiple Primary and Histology Coding Rules Manual. Bethesda MD: National Cancer Institute; 2013. http://seer.cancer.gov/tools/mphrules/download.html (accessed 24 September 2017) [Google Scholar]
- 23.IARC Working Group. International Rules for Multiple Primary Cancers (ICD-O Third Edition) Eur J Cancer Prev. 2005;14:307–8. doi: 10.1097/00008469-200508000-00002. [DOI] [PubMed] [Google Scholar]
- 24.UN Statistical Division. Standard country or area codes for statistical use (M49) New York NY, USA: 2015. https://unstats.un.org/unsd/methodology/m49/ (accessed 1 Sep 2017) [Google Scholar]
- 25.Environmental Systems Research Institute. ArcGIS Desktop: Release 10.3. Redlands CA, USA: ESRI; 2015. http://desktop.arcgis.com/en/arcmap/10.3/main/get-started/whats-new-in-arcgis.htm (accessed 1 June 2017) [Google Scholar]
- 26.Hijmans R. Database of Global Administrative Areas (version 2.8) Davis CA, USA: University of California; 2015. http://www.gadm.org/ (accessed 20 September 2017) [Google Scholar]
- 27.United Nations. World Population Prospects: The 2015 Revision. Department of Economic and Social Affairs, Population Division; 2015. http://esa.un.org/unpd/wpp/ (accessed 10 January 2017) [Google Scholar]
- 28.Allemani C, Harewood R, Johnson C, Carreira H, Spika D, Bonaventure A, Ward K, Weir HK, Coleman MP. Population-based cancer survival in the US: data, quality control and statistical methods. Cancer. 2017:xx–yy. doi: 10.1002/cncr.31025. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Estève J, Benhamou E, Raymond L. Statistical methods in cancer research, volume IV Descriptive epidemiology. Lyon: International Agency for Research on Cancer; 1994. (IARC Scientific Publications No. 128). [PubMed] [Google Scholar]
- 30.Cutler SJ, Ederer F. Maximum utilisation of the life table method in analyzing survival. J Chronic Dis. 1958;8:699–712. doi: 10.1016/0021-9681(58)90126-7. [DOI] [PubMed] [Google Scholar]
- 31.Brenner H, Gefeller O. An alternative approach to monitoring cancer patient survival. Cancer. 1996;78(9):2004–10. [PubMed] [Google Scholar]
- 32.Brenner H, Spix C. Combining cohort and period methods for retrospective time trend analyses of long-term cancer patient survival rates. Br J Cancer. 2003;89:1260–5. doi: 10.1038/sj.bjc.6601295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pohar Perme M, Stare J, Estève J. On estimation in relative survival. Biometrics. 2012;68:113–20. doi: 10.1111/j.1541-0420.2011.01640.x. [DOI] [PubMed] [Google Scholar]
- 34.Clerc-Urmès I, Grzebyk M, Hédelin G. Net survival estimation with stns. Stata J. 2014;14:87–102. [Google Scholar]
- 35.StataCorp. STATA statistical software. 14. College Station, TX: Stata Corporation; 2015. [Google Scholar]
- 36.Rachet B, Maringe C, Woods LM, Ellis L, Spika D, Allemani C. Multivariable flexible modelling for estimating complete, smoothed life tables for sub-national populations. BMC Public Health. 2015;15:1240. doi: 10.1186/s12889-015-2534-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Micheli A, Baili P, Mugno E, Quinn M, Capocaccia R, Grosclaude PC, EUROCARE Working Group Life expectancy and cancer survival in the EUROCARE-3 cancer registry areas. Ann Oncol. 2003;14(Suppl. 5):28–40. doi: 10.1093/annonc/mdg752. [DOI] [PubMed] [Google Scholar]
- 38.Ewbank DC, Gómez de León JC, Stoto MA. A reducible four-parameter system of model life tables. Pop Studies. 1983;37:105–29. doi: 10.1080/00324728.1983.10405927. [DOI] [PubMed] [Google Scholar]
- 39.Brass W. On the scale of mortality. In: Brass W, editor. Biological aspects of demography. London: Taylor and Francis; 1971. pp. 69–110. [Google Scholar]
- 40.Elandt-Johnson RC, Johnson NL. Survival models and data analysis. Indianapolis: John Wiley & Sons, Inc.; 1980. (Wiley Series in Probability and Mathematical Statistics). [Google Scholar]
- 41.Corazziari I, Quinn MJ, Capocaccia R. Standard cancer patient population for age standardising survival ratios. Eur J Cancer. 2004;40:2307–16. doi: 10.1016/j.ejca.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Stiller CA, Bunch KJ. Trends in survival for childhood cancer in Britain diagnosed 1971-85. Br J Cancer. 1990;62:806–15. doi: 10.1038/bjc.1990.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenwood M. The natural duration of cancer. London: HMSO; 1926. (Report on Public Health and Medical Subjects No. 33). [Google Scholar]
- 44.Berkson J, Gage RP. Survival curve for cancer patients following treatment. J Am Stat Assoc. 1952;47:501–15. [Google Scholar]
- 45.Dickman PW, Adami HO. Interpreting trends in cancer patient survival. J Intern Med. 2006;260:103–17. doi: 10.1111/j.1365-2796.2006.01677.x. [DOI] [PubMed] [Google Scholar]
- 46.Coleman MP. Cancer survival: global surveillance will stimulate health policy and improve equity. Lancet. 2014;383:564–73. doi: 10.1016/S0140-6736(13)62225-4. [DOI] [PubMed] [Google Scholar]
- 47.Allemani C. The importance of global surveillance of cancer survival for cancer control: the CONCORD programme. Cancer Control. 2017:xx–yy. [in press] [Google Scholar]
- 48.Abdel-Rahman MA, Stockton DL, Rachet B, Hakulinen T, Coleman MP. What if cancer survival in Britain were the same as in Europe: how many deaths are avoidable? Br J Cancer. 2009;101(Suppl. 2):115–24. doi: 10.1038/sj.bjc.6605401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ellis L, Coleman MP, Rachet B. How many deaths would be avoidable if socioeconomic inequalities in cancer survival in England were eliminated? A national population-based study, 1996-2006. Eur J Cancer. 2012;48:270–8. doi: 10.1016/j.ejca.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 50.Ho GF, Taib NA, Pritam Singh RK, Yip CH, Abdullah MM, Lim TO. What if all patients with breast cancer in Malaysia have access to the best available care: how many deaths are avoidable? Global Journal of Health Science. 2017;9 [Google Scholar]
- 51.Pokhrel A, Martikainen P, Pukkala E, Rautalahti M, Seppä K, Hakulinen T. Education, survival and avoidable deaths in cancer patients in Finland. Br J Cancer. 2010;103:1009–114. doi: 10.1038/sj.bjc.6605861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sandiford P, Abdel-Rahman ME, Allemani C, Coleman MP, Gala G. How many cancer deaths could New Zealand avoid if five-year relative survival ratios were the same as in Australia? Aust N Z J Public Health. 2015;39:157–61. doi: 10.1111/1753-6405.12344. [DOI] [PubMed] [Google Scholar]
- 53.Seppä K, Hakulinen T, Läärä E. Avoidable deaths and random variation in patients’ survival. Br J Cancer. 2012 doi: 10.1038/bjc.2012.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mirzaei M, Mirzadeh M, Mirzaei M. Expected years of life lost due to adult cancer mortality in Yazd (2004-2010) Asian Pac J Cancer Prev. 2016;17:101–5. doi: 10.7314/apjcp.2016.17.s3.101. [DOI] [PubMed] [Google Scholar]
- 55.Brustugun OT, Møller B, Helland Å. Years of life lost as a measure of cancer burden on a national level. Br J Cancer. 2014;111:1014–20. doi: 10.1038/bjc.2014.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soerjomataram I, Lortet-Tieulent J, Parkin DM, Ferlay J, Mathers C, Forman D, Bray F. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012;380(9856):1840–50. doi: 10.1016/S0140-6736(12)60919-2. [DOI] [PubMed] [Google Scholar]
- 57.Woods LM, Morris M, Rachet B. No ‘cure’ within 12 years of diagnosis among breast cancer patients who are diagnosed via mammographic screening: women diagnosed in the West Midlands region of England 1989-2011. Ann Oncol. 2016;27 doi: 10.1093/annonc/mdw408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Andersson TML, Eriksson H, Hansson J, Månsson-Brahme E, Dickman PW, Eloranta S, Lambe M, Lambert PC. Estimating the cure proportion of malignant melanoma, an alternative approach to assess long term survival: A population-based study. Cancer Epidemiol. 2014;38(1):93–9. doi: 10.1016/j.canep.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 59.Gatta G, Rossi S, Foschi R, Trama A, Marcos-Gragera R, Pastore G, Peris-Bonet R, Stiller C, Capocaccia R. Survival and cure trends for European children, adolescents and young adults diagnosed with acute lymphoblastic leukemia from 1982 to 2002. Haematologica. 2013;98(5):744–52. doi: 10.3324/haematol.2012.071597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ito Y, Nakayama T, Tsukuma H, Miyashiro I, Ioka A, Sugimoto T, Rachet B. Role of age and tumour stage in the temporal pattern of ‘cure’ from stomach cancer: A population-based study in Osaka, Japan. Cancer Epidemiol. 2012;36:128–32. doi: 10.1016/j.canep.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 61.Shack LG, Shah A, Lambert P, Rachet B. “Cure” by age and stage at diagnosis for colorectal cancer patients: a population-based study. Cancer Epidemiol. 2012;36:548–53. doi: 10.1016/j.canep.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 62.Coleman MP. Why we need global surveillance of cancer survival: the CONCORD programme. In: McGrath I, editor. Cancer care in emerging health systems. Oxford: International Network for Cancer Treatment and Research; 2013. pp. 60–5. [Google Scholar]
- 63.Cookson JB. Cancer survival. Lancet. 2000;356:1611. doi: 10.1016/s0140-6736(05)74461-5. [DOI] [PubMed] [Google Scholar]
- 64.Organisation for Economic Co-operation and Development. Cancer care: assuring quality to improve survival. Paris: OECD; 2013. http://dx.doi.org/10.1787/9789264181052-en (accessed 25 September 2017) [Google Scholar]
- 65.Atun R, Jaffray DA, Barton MB, Bray F, Baumann M, Vikram B, Hanna TP, Knaul FM, Lievens Y, Lui TY, Milosevic M, O’Sullivan B, Rodin DL, Rosenblatt E, Van Dyk J, Yap ML, Zubizarreta E, Gospodarowicz M. Expanding global access to radiotherapy. Lancet Oncol. 2015;16(10):1153–86. doi: 10.1016/S1470-2045(15)00222-3. [DOI] [PubMed] [Google Scholar]
- 66.Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J, Mérisier ED, El-Halabi S, Farmer PE, Gawande A, Gillies R, Greenberg SLM, Grimes CE, Gruen RL, Ismail EA, Kamara TB, Lavy C, Lundeg G, Mkandawire NC, Raykar NP, Riesel JN, Rodas E, Rose J, Roy N, Shrime MG, Sullivan R, Verguet S, Watters D, Weiser TG, Wilson IH, Yamey G, Yip W. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 67.Organisation for Economic Co-operation and Development. Health at a Glance 2017: OECD indicators. Paris, France: OECD Publishing; 2017. [Google Scholar]
- 68.Union for International Cancer Control. World Cancer Declaration 2013. Geneva: UICC; 2013. http://www.uicc.org/world-cancer-declaration (accessed 25 September 2017) [Google Scholar]
- 69.Jensen OM, Parkin DM, MacLennan R, Muir CS, Skeet RG, editors. Cancer registration: principles and methods. Lyon: International Agency for Research on Cancer; 1991. (IARC Scientific Publications No. 95). [Google Scholar]
- 70.Berrino F, Estève J, Coleman MP. Basic issues in the estimation and comparison of cancer patient survival. In: Berrino F, Sant M, Verdecchia A, Capocaccia R, Hakulinen T, Estève J, editors. Survival of cancer patients in Europe: the EUROCARE study. Lyon: International Agency for Research on Cancer (WHO); 1995. pp. 1–14. (IARC Scientific Publications No 132). [Google Scholar]
- 71.Abdel-Razeq H, Attiga F, Mansour A. Cancer care in Jordan. Hematol Oncol Stem Cell Ther. 2015;8:64–70. doi: 10.1016/j.hemonc.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 72.Laurenti R, Coleman MP, Aylin P. Accuracy of statements of the cause of death on death certificates and the international comparability of mortality statistics. In: Coleman MP, Aylin P, editors. Death certification and mortality statistics: an international perspective. London: Office for National Statistics; 2000. pp. 1–9. [Google Scholar]
- 73.Ovcharov VK, Tishuk EA. The improvement of statistical records of the causes of death in Russia. In: Coleman MP, Aylin P, editors. Death certification and mortality statistics: an international perspective. London: Office for National Statistics; 2000. pp. 28–30. [Google Scholar]
- 74.Filippatos G, Andriopoulos P, Panoutsopoulos G, Zyga S, Souliotis K, Gennimata V, Tsironi M. The quality of death certification practice in Greece. Hippokratia. 2016;20(1):19–25. [PMC free article] [PubMed] [Google Scholar]
- 75.Haghighi MH, Dehghani M, Teshizi SH, Mahmoodi H. Impact of documentation errors on accuracy of cause of death coding in an educational hospital in Southern Iran. The HIM journal. 2014;43(2):35–42. [PubMed] [Google Scholar]
- 76.Cândida da Cunha C, Teixeira R, França E. Assessment of the investigation of ill-defined causes of death in Brazil in 2010. Epidemiologia e Serviços de Saúde. 2017;26:1–12. doi: 10.5123/S1679-49742017000100003. [DOI] [PubMed] [Google Scholar]
- 77.Antoni S, Soerjomataram I, Møller B, Bray F, Ferlay J. An assessment of GLOBOCAN methods for deriving national estimates of cancer incidence. Bulletin of the World Health Organization. 2016;94:174–84. doi: 10.2471/BLT.15.164384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Engeland A, Haldorsen T, Dickman PW, Hakulinen T, Möller TR, Storm HH, Tulinius H. Relative survival of cancer patients: a comparison between Denmark and other Nordic countries. Acta Oncol. 1998;37:49–59. doi: 10.1080/028418698423177. [DOI] [PubMed] [Google Scholar]
- 79.Berrino F, Capocaccia R, Estève J, Gatta G, Hakulinen T, Micheli A, Sant M, Verdecchia A, editors. Survival of cancer patients in Europe: the EUROCARE-2 study. Lyon: International Agency for Research on Cancer; 1999. (IARC Scientific Publications No. 151). [Google Scholar]
- 80.Storm HH, Gislum M, Engholm G. Cancer survival before and after initiating the Danish Cancer Control plan. Ugeskr Læger [Danish Medical Journal] 2008;170(39):3065–9. [In Danish, English abstract] [PubMed] [Google Scholar]
- 81.Engholm G, Ferlay J, Christensen N, Kejs AMT, Hertzum-Larsen R, Johannesen TB, Khan S, Leinonen MK, Ólafsdóttir E, Petersen T, Schmidt LKH, Trykker H, Storm H. NORDCAN: Cancer incidence, mortality, prevalence and survival in the Nordic Countries, Version 7.3. Association of the Nordic Cancer Registries, Danish Cancer Society; 2016. 08.07.2016. http://www.ancr.nu (accessed 3 November 2017) [Google Scholar]
- 82.Storm HH, Engholm G, Hakulinen T, Tryggvadóttir L, Klint A, Gislum M, Kejs AM, Bray F. Survival of patients diagnosed with cancer in the Nordic countries up to 1999-2003 followed to the end of 2006. A critical overview of the results. Acta Oncol. 2010;49:532–44. doi: 10.3109/02841861003801148. [DOI] [PubMed] [Google Scholar]
- 83.Yoo KY. Cancer control activities in the Republic of Korea. Jpn J Clin Oncol. 2008;38(5):327–33. doi: 10.1093/jjco/hyn026. [DOI] [PubMed] [Google Scholar]
- 84.Choi KS, Jun JK, Suh M, Park B, Noh DK, Song SH, Jung KW, Lee HY, Choi IJ, Park EC. Effect of endoscopy screening on stage at gastric cancer diagnosis: results of the National Cancer Screening Programme in Korea. Br J Cancer. 2015;112:608–12. doi: 10.1038/bjc.2014.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pech O, May A, Manner H, Behrens A, Pohl J, Weferling M, Hartmann U, Manner N, Huijsmans J, Gossner L, Rabenstein T, Vieth M, Stolte M, Ell C. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology. 2014;146:652–60. doi: 10.1053/j.gastro.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 86.Suh YS, Yang HK. Screening and early detection of gastric cancer: East versus West. Surg Clin North Am. 2015;95:1053–66. doi: 10.1016/j.suc.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 87.Chang JW-C, Guo J, Hung C-Y, Lu S, Shin SJ, Quek R, Ying A, Ho GF, Nguyen HS, Dhabhar B, Sriuranpong V, Tiambeng ML, Prayogo N, Yamazaki N. Sunrise in melanoma management: time to focus on melanoma burden in Asia. Asia Pac J Clin Oncol. 2017:1–5. doi: 10.1111/ajco.12670. [DOI] [PubMed] [Google Scholar]
- 88.Brawley OW. Accepting the existence of breast cancer overdiagnosis. Ann Intern Med. 2017;166:364–5. doi: 10.7326/M16-2850. [DOI] [PubMed] [Google Scholar]
- 89.Marcus PM, Prorok PC, Miller AB, DeVoto EJ, Kramer BS. Conceptualizing overdiagnosis in cancer screening. J Natl Cancer Inst. 2015;107:1–4. doi: 10.1093/jnci/djv014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Allemani C, Rachet B, Weir HK, Richardson LC, Lepage C, Faivre J, Gatta G, Capocaccia R, Sant M, Baili P, Lombardo C, Aareleid T, Ardanaz E, Bielska-Lasota M, Bolick S, Cress R, Elferink M, Fulton JP, Galceran J, Góźdź S, Hakulinen T, Primic- Žakelj M, Rachtan J, Diba CS, Sánchez MJ, Schymura MJ, Shen T, Tagliabue G, Tumino R, Vercelli M, Wolf HJ, Wu XC, Coleman MP. Colorectal cancer survival in the USA and Europe: a CONCORD high-resolution study. BMJ Open. 2013;3:e003055. doi: 10.1136/bmjopen-2013-003055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Maringe C, Walters S, Rachet B, Butler J, Fields T, Finan PJ, Maxwell R, Nedrebø B, Påhlman L, Sjövall A, Spigelman A, Engholm G, Gavin A, Gjerstorff ML, Hatcher J, Johannesen TB, Morris EJ, McGahan CE, Tracey E, Turner D, Richards MA, Coleman MP, ICBP Module 1 Working Group Stage at diagnosis and colorectal cancer survival in six high-income countries: a population-based study of patients diagnosed during 2000-7. Acta Oncol. 2013;52:919–32. doi: 10.3109/0284186X.2013.764008. [DOI] [PubMed] [Google Scholar]
- 92.Wu SJ, Chiang CJ, Lin CT, Tien HF, Lai MS. Improving but inferior survival in patients with chronic lymphocytic leukemia in Taiwan: a population-based study, 1990-2004. PLoS One. 2013;8:e62930. doi: 10.1371/journal.pone.0062930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sullivan R, Kowalczyk JR, Agarwal B, Ladenstein R, Fitzgerald E, Barr R, Steliarova-Foucher E, Magrath I, Howard SC, Kruger M, Valsecchi MG, Biondi A, Grundy P, Smith MA, Adamson P, Vassal G, Pritchard-Jones K. New policies to address the global burden of childhood cancers. Lancet Oncol. 2013;14:e125–e35. doi: 10.1016/S1470-2045(13)70007-X. [DOI] [PubMed] [Google Scholar]
- 94.Magrath I, Steliarova-Foucher E, Epelman S, Ribeiro RC, Harif M, Li C-K, Kebudi R, Macfarlane SD, Howard SC. Paediatric cancer in low-income and middle-income countries. Lancet Oncol. 2013;14:e104–e16. doi: 10.1016/S1470-2045(13)70008-1. [DOI] [PubMed] [Google Scholar]
- 95.Mostert S, Arora RS, Arreola M, Bagai P, Friedrich P, Gupta S, Kaur G, Koodiyedath B, Kulkarni K, Lam CG, Luna-Fineman S, Pizer B, Rivas S, Rossell N, Sitaresmi MN, Tsimicalis A, Weaver M, Ribeiro RC. Abandonment of treatment for childhood cancer: position statement of a SIOP PODC Working Group. Lancet Oncol. 2011;12:719–20. doi: 10.1016/S1470-2045(11)70128-0. [DOI] [PubMed] [Google Scholar]
- 96.Pritchard-Jones K, Stiller CA. What can we learn from geographical comparisons of childhood cancer survival? Br J Cancer. 2007;96:1493–7. doi: 10.1038/sj.bjc.6603749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Spika D, Rachet B, Bannon F, Woods LM, Maringe C, Bonaventure A, Coleman MP, Allemani C. Life tables for the CONCORD-2 study. London: CONCORD Central Analytic Team; 2015. http://csg.lshtm.ac.uk/tools-analysis/ (accessed 24 September 2016) [Google Scholar]
- 98.Ginsburg O, Bray F, Coleman MP, Vanderpuye V, Alexandru E, Rani Kotha S, Sarker M, Huong T, Allemani C, Dvaladze A, Gralow J, Yeates K, Taylor C, Oomman N, Krishnan S, Sullivan R, Kombe D, Blas M, Parham G, Kassami N, Conteh L. The global burden of women’s cancers: a grand challenge in global health. Lancet. 2017;389:847–60. doi: 10.1016/S0140-6736(16)31392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ginsburg O, Badwe R, Boyle P, Derricks G, Dare A, Evans T, Eniu A, Jiménez J, Kutluk T, Lopes G, Mohammed SI, Qiao YL, Rashid SF, Summers D, Sarfati D, Temmerman M, Trimble EL, Padela AI, Aggarwal A, Sullivan R. Changing global policy to deliver safe, equitable and affordable care for women’s cancers. Lancet. 2017;389:871–80. doi: 10.1016/S0140-6736(16)31393-9. [DOI] [PubMed] [Google Scholar]
- 100.Economist Intelligence Unit. Breakaway: the global burden of cancer - challenges and opportunities: The Economist. 2009 [Google Scholar]
- 101.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103:117–28. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fojo T, Grady C. How much is life worth: cetuximab, non-small cell lung cancer, and the $440 billion question. J Natl Cancer Inst. 2009;101:1044–8. doi: 10.1093/jnci/djp177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Knaul FM, Gralow J, Atun R, Bhadelia A. Closing the cancer divide: an equity imperative. Boston, MA: Harvard University Press; 2011. [Google Scholar]
- 104.Sullivan R, Peppercorn J, Sikora K, Zalcberg J, Meropol NJ, Amir E, Khayat D, Boyle P, Autier P, Tannock IF, Fojo T, Siderov J, Williamson S, Camporesi S, McVie JG, Purushotham AD, Naredi P, Eggermont A, Brennan MF, Steinberg ML, De Ridder M, McCloskey SA, Verellen D, Roberts T, Storme G, Hicks RJ, Ell PJ, Hirsch BR, Carbone DP, Schulman KA, Catchpole P, Taylor D, Geissler J, Brinker NG, Meltzer D, Kerr D, Aapro M. Delivering affordable cancer care in high-income countries. Lancet Oncol. 2011;12:933–80. doi: 10.1016/S1470-2045(11)70141-3. [DOI] [PubMed] [Google Scholar]
- 105.Tangka FKL, Subramanian S, Beebe MC, Weir HK, Trebino D, Babcock F, Ewing J. Cost of operating central cancer registries and factors that affect cost: findings from an economic evaluation of Centers for Disease Control and Prevention National Program of Cancer Registries. J Public Health Manag Pract. 2016;22:452–60. doi: 10.1097/PHH.0000000000000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.United Nations. Sustainable Development Goals. New York NY: UN; 2015. http://www.un.org/sustainabledevelopment/sustainable-development-goals/ (accessed 25 September 2017) [Google Scholar]
- 107.United Nations. Sustainable Development Goal 3. New York NY: UN; 2015. https://sustainabledevelopment.un.org/sdg3 (accessed 25 September 2017) [Google Scholar]
- 108.Schmidt H, Gostin LO, Emanuel EJ. Public health, universal health coverage, and sustainable development goals: can they coexist? Lancet. 2015;386:928–30. doi: 10.1016/S0140-6736(15)60244-6. [DOI] [PubMed] [Google Scholar]
- 109.López A, Thomason J. Civil registration and vital statistics – everybody’s business but nobody’s business. Lancet. 2013;381:1275–6. doi: 10.1016/S0140-6736(13)60838-7. [DOI] [PubMed] [Google Scholar]
- 110.Setel PW, Macfarlane SB, Szreter S, Mikkelsen L, Jha P, Stout S, AbouZahr C. Who counts? 1: A scandal of invisibility: making everyone count by counting everyone. Lancet. 2007;370:1569–77. doi: 10.1016/S0140-6736(07)61307-5. [DOI] [PubMed] [Google Scholar]
- 111.World Health Organisation. Cancer prevention and control in the context of an integrated approach [A70/A/CONF./9] Geneva: WHO; 2017. (accessed 25 September 2017) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


