Abstract
Background
Recent retrospective data suggest that neoadjuvant androgen deprivation therapy can improve the prognosis of high-risk prostate cancer (PCa) patients. Novel androgen receptor pathway inhibitors are nowadays available for treatment of metastatic PCa and these compounds are promising for early stage disease. Apalutamide is a pure androgen antagonist with a very high affinity with the androgen receptor. The combination of apalutamide with degarelix, an LHRH antagonist, could increase the efficacy compared to degarelix alone.
Objective
The primary objective is to assess the difference in proportions of minimal residual disease at prostatectomy specimen between apalutamide + degarelix vs placebo + degarelix. Various secondary endpoints are assessed: variations of different biomarkers at the tumour level (tissue microarrays to evaluate DNA-PKs, PARP, AR and splice variants, PSMA, etc.), whole transcriptome sequencing, exome sequencing and clinical (PSA and testosterone kinetics, early biochemical recurrence free survival, quality of life, safety, etc.) and radiological endpoints.
Methods
ARNEO is a single centre, phase II, randomized, double blind, placebo-controlled trial. The plan is to include at least 42 patients per each of the two study arms. Patients with intermediate/high-risk PCa and who are amenable for radical prostatectomy with pelvic lymph node dissection can be included. After signing an informed consent, every patient will undergo a pelvic 68Ga -PSMA-11 PSMA PET/MR and receive degarelix at standard dosage and start assuming apalutamide/placebo (60 mg 4 tablets/day) for 12 weeks. Within thirty days from the last study medication intake the same imaging will be repeated. Every patient will undergo PSA and testosterone testing the day of randomization, before the first drug intake, and after the last dose. Formalin fixed paraffin embedded tumour samples will be collected and used for transcriptome analysis, exome sequencing and immunohistochemistry.
Discussion
ARNEO will allow us to answer, first, whether the combined treatment can result in an increased proportion of patients with minimal residual disease. Secondly, It will enable the study of the molecular consequences at the level of the tumour. Thirdly, what the consequences are of new generation androgen receptor pathway inhibitors on 68Ga -PSMA-11 PET/MR. Finally, various clinical, safety and quality of life data will be collected.
Trial Registration
EUDRaCT number: 2016–002854-19 (authorization date 3rd August 2017).
clinicalTrial.gov: NCT03080116.
Background
The incidence of prostate cancer (PCa) in the European Union has increased during recent decades since the opportunistic implementation of PSA screening in the clinical practice [1]. Localized PCa is classified in risk groups: low (cT1-T2a, PSA < 10 ng/ml, biopsy Gleason score 6), intermediate (cT2b, PSA10–20 ng/ml, biopsy Gleason score 7), high-risk localized (cT2c, PSA > 20 ng/ml, biopsy Gleason score 8–10) or high-risk locally advanced (cT3–4, cN1) PCa [2]. Fifteen-year cancer-related mortality rate is 20% in intermediate and 36% in high-risk non-metastatic PCa patients treated without curative intent [3]. Conversely, 10-year cancer specific survival for low-risk patients who underwent active monitoring or active treatment is 99% without differences between treatment subgroups [4]. These findings support the notion that lethal disease is rare in the low-risk subgroup. During the last years, the rates of curative treatment for high-risk disease have increased progressively. Conversely, active surveillance has been more and more dedicated to low-risk PCa [5]. However, in the high-risk group, a large part of patients requires other treatments next to radical prostatectomy (adjuvant or salvage radiotherapy, adjuvant systemic treatment) [6]. Considering the increasing application of surgery for high-risk patients, there is an urgent need for studies that assess new treatment combinations in order to maximize cure rates. Treatment of patients with intermediate and high-risk PCa presents two challenges: the need for local control and treatment of possible micro-metastases. Unfortunately, there is still no validated test to detect micro-metastatic disease [7]. Radical prostatectomy with extended pelvic lymph node dissection (ePLND) represents an important therapeutic option within a multimodal approach (adjuvant or salvage radiotherapy, adjuvant systemic treatment) [2, 8].
Neoadjuvant therapy is routinely utilized for the treatment of muscle invasive bladder, esophageal and rectal cancer with the scope of down-staging the primary tumour and control of possible micro-metastatic clones. In this context, neoadjuvant therapy before radical prostatectomy is an interesting possibility in particular for intermediate and high-risk disease. PCa has the peculiarity to be largely dependent on androgen regulation, a mechanism that is routinely targeted in advanced cases. Neoadjuvant hormonal therapy using luteinizing hormone releasing hormone (LHRH) agonists and/or anti-androgens has already demonstrated to downstage primary PCa [9], however, there is a lack of survival data especially for patients with high-risk disease, considering that the previous controlled trials generally assessed low-intermediate risk patients with various ADT regimens and relatively short follow ups [9, 10]. Recently it was suggested that neoadjuvant ADT could decrease cancer related death in high-risk patients, especially when adjuvant EBRT is associated [11]. Considering the increasing availability of new generation androgen receptor pathway inhibitors, there is a new wave of studies that are assessing the anti-tumour effect of these compounds on the primary tumour using pathologic characteristics (pathologic complete response, minimal residual disease) as proxy of an anti-tumour effect [12]. Degarelix is a well-known LHRH antagonist that is commonly used in advanced prostate cancer, with the advantage that it avoids tumour flare-up with a faster depression of testosterone levels compared to LHRH agonists [13]. It was shown that degarelix is not inferior to goserelin + bicalutamide in decreasing the prostate volume in PCa patients [14], thus it was suggested to be a valuable alternative in the neoadjuvant setting. Degarelix was recently studied before prostatectomy but the results were controversial, showing higher intra-tumour levels of dihydrotestosteron compared to LHRH agonist + bicalutamide or degarelix + bicalutamide, generating the hypothesis of unknown mechanisms of action that should be better analyzed in other trials [15]. Interestingly, pathological complete response was obtained for degarelix when it was associated with bicalutamide, generating the hypothesis that a stronger androgen blockade can result in a stronger anti-tumour effect. Degarelix was compared to leuprolide in the pivot trial CS21 in hormone sensitive patients showing a sustained testosterone suppression with improved PSA progression-free survival for degarelix compared to LHRH analogue [16]. In the extension phase, those patients who crossed-over from leuprolide to degarelix, experienced an improved PSA response and progression-free survival supporting the better effect of the LHRH antagonist [17]. Neoadjuvant studies, in the surgical setting, are also a unique opportunity to complete our knowledge on mechanisms of action and molecular response to such new generation of compounds [18]. Apalutamide (alias ARN-509) is a second-generation antiandrogen with a pure antagonist mechanism with 7–10 fold higher affinity with the androgen receptor compared to bicalutamide [19]. It is currently studied in phase III trials for treatment of castration naïve (NCT02489318, NCT02531516) or castration resistant PCa (NCT02257736, NCT02106507, NCT01946204). The possibility to study the anti-tumour effect of the complete androgen blockade based on apalutamide + degarelix is of interest, considering the safety profile of these compounds [16, 20] and potential benefit for the patients.
The therapeutic effect of EBRT is mediated by DNA damage and hence the DNA repair mechanisms are the leading mechanisms in radio-resistance. In preclinical studies, even in the absence of radiation, antiandrogens induce an increased DNA damage and decreased DNA repair in PCa cell lines [21]. Thus, DNA repair is androgen dependent in cell lines, but a better insight in these mechanisms in localized tumour tissue and the assessment of possible novel therapies to decrease the activity of DNA repair mechanisms could help understanding and optimizing treatment modalities. We hypothesize that ARN-509 in combination with degarelix can inhibit DNA repair mechanism more intensively then classic hormonal treatment.
As described above for DNA repair, most studies on androgen-regulated phenomena in prostate cancer are based on preclinical models [22]. We will analyze transcriptomes of pre-treatment biopsies and compare them with the tumor at the moment of radical prostatectomy (after degarelix or degarelix + apalutamide). Transcriptomes will be further complemented with genomic analyses because of known and unknown links between mutations and treatment responses [23].
Second generation androgen receptor pathway inhibitors can induce resistance through different mechanisms [24, 25]. One of these mechanisms is the expression of androgen receptor splice variants. More specifically, the ARV7 variant was found to be a marker for second-generation antiandrogen resistance in mCRPC [26–28]. There is a lack of data about ARV7 expression in primary PCa. Recently it was demonstrated that ARV7 can be expressed in patients treated with degarelix + bicalutamide + abiraterone + prednisolone before prostatectomy but this was not related to the therapy response [29].
PSA is commonly used as a tumour biomarker after RP in order to identify possible recurrences [30]. Early (< 3 year) biochemical failure was identified as a significant predictor of metastatic progression and cancer related death [31], thus representing a useful marker in the clinical practice. We expect an improvement of early biochemical failure in the study arm compared to the control arm. The prognostic value of PSA nadir to predict PCa survival after 3 months of hormonal treatment and before EBRT was tested [32]. PSA levels < 0.5 ng/ml can predict patient survival [32] and this observation was also confirmed recently for PSA levels ≤0.3 ng/ml [33]. PSA nadir before EBRT is, thus, an important biomarker of hormonal response and also a predictor of survival in this setting.
Novel imaging techniques are expected to overcome the problem of invasive sample collection in the near future by allowing accurate diagnosis, tumour staging and assessment of treatment response. Positron emission tomography (PET) is a recognized tool to detect tumour lesions by targeting their metabolic activity or their specific antigen expression. PSMA (prostate specific membrane antigen) is a type II trans-membrane protein that is specifically expressed on the surface of PCa cells and could be used as a tracer to investigate anti-androgen response [34]. PSMA can be targeted by a PSMA-ligand associated to 68Gallium. This tracer has been implemented in PET-computed tomography (PET-CT) for the detection of PCa in the metastatic setting [35]. There is also evidence of PSMA regulation by androgens [36]. Immunohistochemical examination of FFPE (formalin fixed paraffin embedded) PCa tissues of patients treated by different anti-androgen therapies showed an over-expression of PSMA after therapy in 55% of primary tumour samples and 100% of metastatic lesions compared to the baseline [37]. Thus, a better insight on PSMA expression in castration naïve patients following new generation ADT is of interest. Recently, PET/MR hybrid imaging has been introduced next to PET/CT in order to allow the combination of specific properties of different imaging techniques.68Ga-PSMA PET demonstrated high potential to detect minimal PCa lesions. In preliminary studies, hybrid 68Ga-PSMA PET/MR technology has demonstrated to be promising in the diagnosis and follow up of PCa [38]. The same imaging technology might also represent an important improvement for treatment follow-up. The neoadjuvant setting offers an ideal platform to study this hypothesis.
Methods
Aim
The primary objective is to assess the residual tumour after surgery. To assess this objective, we aim to evaluate the difference in proportions of patients with minimal residual disease (MRD: tumour volume ≤ 0.25 cm3 at final pathology) between the two arms as primary endpoint. MRD and residual cancer burden (RCB) will permit to correct cancer volume by tumour cellularity [39]. The secondary objectives are: a) pathology and immunohistochemistry assessment of the prostatectomy specimen b) whole transcriptome analysis c) exome sequencing d) clinical assessment e) radiological assessment by 68Ga -PSMA-11 PET/MR.
Design and setting
ARNEO is a Phase II, single centre, randomized, double-blind, placebo controlled trial sponsored by UZ Leuven (Fig. 1, Table 1).
Fig. 1.
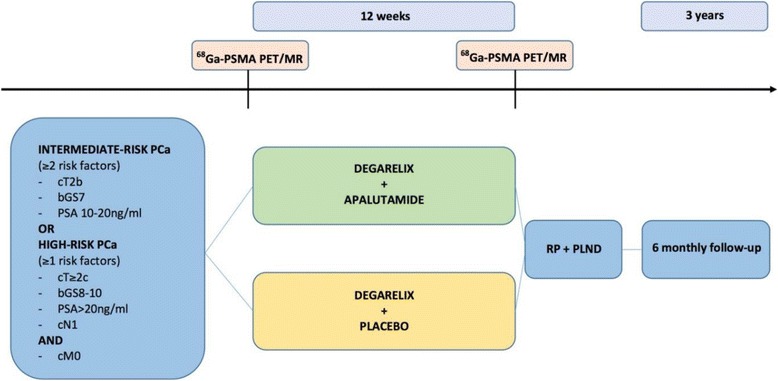
Flow diagram of ARNEO. Ga: Gallium. bGS: biopsy Gleason score. MR: magnetic resonance. PCa: prostate cancer. PET: Positron Emission Tomography. PLND: pelvic lymph node dissection. PSMA: prostate specific membrane antigen. RP: radical prostatectomy
Table 1.
Summary of the main trail activities
| Activities | Visits | Perioperative period | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening | V1 | V2 | V3 | V4 | T | PO | ||||||||||||
| Cycles (weeks) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||||||
| Randomization | X | |||||||||||||||||
| Drugs dispensation | X | X | X | |||||||||||||||
| Informed consent | X | |||||||||||||||||
| Inclusion/exclusion criteria | X | X | ||||||||||||||||
| Questionnaires IIEF5, ICIQ EORTC, QLQ-C30 | X | X | X | |||||||||||||||
| PSA | X | X | X | X | X | |||||||||||||
| Testosterone | X | X | X | X | ||||||||||||||
| SHBG | X | X | ||||||||||||||||
| Blood and urine sampling for research purposes | X | X | ||||||||||||||||
| Anestesiological visit | X | |||||||||||||||||
| RP + PLND | X | |||||||||||||||||
| Charlson comorbidity index | X | |||||||||||||||||
| Clavien-Dindo | X | |||||||||||||||||
| PSMA PET/MR | X | X | ||||||||||||||||
V: visit. T: treatment. PO: postoperative. SHBG: sex hormone binding globulin
The protocol follows the SPIRIT recommendations for interventional trials [40, 41]. Patients are recruited solely in UZ Leuven from radical prostatectomy candidates who meet the inclusion/exclusion criteria. Patients will be randomized to one of the two arms according to a 1:1 allocation. The ARNEO trial was approved by the Medical Ethics Committee UZ KU Leuven / Research (internal identifier S58827). All participants will provide written informed consent before performing any study-related procedure according to the protocol.
Participants
Patients with histologically confirmed adenocarcinoma of the prostate without neuroendocrine differentiation or small cell features with 2 intermediate risk factors (cT2b, biopsy GS 7, PSA 10–20 ng/ml) or high-risk (clinical stage≥T2c and/or biopsy GS ≥ 8 and/or PSA > 20 ng/ml and/or cN1) disease can be included. Patients with or without clinical lymph node invasion are both includable but absence of metastatic disease is mandatory. The natural history of non-treated intermediate and high-risk patients suggest that they represent most of the lethal disease [3]. There is increasing evidence that intermediate risk patients, treated with radical prostatectomy, with at least 2 clinical risk factors have poor outcome [42–44]. Thus, these subjects represent an enriched group at higher-risk of cancer specific mortality with similar characteristics as high-risk prostate cancer [42–44].
Patients must have a good performance status (ECOG 0–1), good haematological, renal and hepatic parameters and be amenable for radical prostatectomy + pelvic lymph node dissection by open or robotic approach. Patients are excluded in case of previous surgical/endoscopic treatments of prostatic disease and if assuming food supplements or herbal products that may decrease PSA levels. Exclusion is foreseen in case of other malignancies diagnosed within 5 years before randomization, severe/instable cardiovascular diseases, gastrointestinal disorder affecting absorption and history of seizure or conditions that may pre-dispose to seizure. Patients have to be able to undergo PET/MR imaging.
Randomization/Stratification/Blinding
The randomization will be centralized and managed by the Leuven Coordinating Centre (LCC). The random sequence is created by a list of random assignments generated by a computer. Allocation of patients to the treatment arms follow a stratified block randomization scheme (with block size of 6). Thus, before the randomization process patients will be stratified according to one of the 2 risk classes: intermediate risk (PSA 10–20 ng/ml, cT2b, bGS7) or high-risk PCa (PSA > 20 ng/ml and/or cT ≥ 2c and/or bGS 8–10 and/or cN1). The randomization will follow an interactive voice response system (IVRS), using a software package to stratify, randomize and allocate patients. The allocation will be managed centrally by LCC that will inform automatically, by institutional email, the pharmacy about the drug assignment. Labelling is done according to the legal requirements to guarantee blinding of participants and personnel. The blinding code can be broken in emergency situations at the discretion of the principal investigator or delegated personnel when knowledge of the study medication has safety implications. Under normal circumstances, the blinding should not be broken until the primary endpoint is reached. Randomization codes will be fully disclosed when the data relative to the primary endpoint are completely collected.
Interventions
Patients included in the study will be randomly allocated to one of the interventional arms. Before starting the treatment, every patient will undergo a 68Ga -PSMA-11 PET/MR of the pelvis (Signa PET/MR system; GE Healthcare, Waukesha, USA using 68Ga -PSMA-11 PET/MR). In both arms patients will receive open label degarelix at a dosage of 2 × 120 mg subcutaneously (SC) at first injection, followed by monthly 80 mg SC injections. Subjects will be randomized to receive 240 mg/day of apalutamide (ARN-509; 60 mg 4 tablets/day) or placebo. Within one month from the last oral study medication intake and before the surgical procedure, patients will undergo the second pelvic 68Ga -PSMA-11 PET/MR. Treatment period will cover 12 weeks before radical prostatectomy + pelvic lymph node dissection (open or robotic surgery). Patients will undergo the surgical treatment as soon as possible after the last study medication intake, with a maximum delay of 1 month to guarantee the execution of the imaging procedures. Different clinical trials assessed pathologic response to neoadjuvant hormonal therapy comparing treatment length. From the Meta-Analysis of these studies, the longer was the treatment period, the better were the surgical margin and organ confined disease rates [10]. Preclinical data about the effect of apalutamide in animal prostates showed that atrophy, probably driven by apoptosis, was already complete and stable at 28 days of treatment, suggesting an early effect on prostatic tissue [19]. More interestingly, in 28 days, the tumour volume decreased of at least 50% in 75% (6/8) of xenograft mouse models from LNCaP/AR cells and to 100% in 50% of models [19]. However, we considered 3 months as a correct period because this was the most studied and the minimal amount of time in previous comparative neoadjuvant trials with a demonstrated effect.
The lymph node dissection template was previously described [45]: the minimal required template will be an extended (e)PLND. This template includes the external iliac region (boundaries: bifurcation of the common iliac artery proximally, circumflex iliac vein distally, psoas muscle and genitofemoral nerve laterally and medial border of the external iliac vein medially), obturator fossa region (bifurcation of the common iliac artery proximally, pelvic floor distally, obturator muscle laterally, obturator nerve posteriorly, and medial border of the external iliac vein anteriorly) and internal iliac region (bifurcation of the common iliac artery proximally, pelvic floor distally, bladder wall medially, obturator muscle laterally, sciatic nerve posteriorly and obturator nerve anteriorly). The common iliac (boundaries: aortic bifurcation proximally, bifurcation of the common iliac arteries distally, psoas muscle and genitofemoral nerve laterally, and medial border of the common iliac artery medially) and presacral regions (triangle between medial borders of common iliac arteries proximally, line connecting the bifurcations of the common iliac arteries distally, promontory and proximal sacrum (S1–S2) dorsally) are not mandatory but can be included at discretion of the treating surgeon. Postoperatively, patients follow periodic medical examination to ensure safety, collecting clinical data and liquid biopsies (urine, plasma and serum) for future research purposes.
Measurements
The data collection will be implemented through an electronic case report form (eCRF) that is specifically designed for the study purposes.
The primary endpoint is to assess the difference in proportions in MRD between the two arms, correcting for RCB [39]. All pathology evaluations will be done by a dedicated uro-pathologist.
- Secondary endpoints assessed in this study:
-
Pathological endpointsProtein expression in prostatic tumour TMA’s (tissue microarrays) by immunohistochemistry (between treatment arms after radical prostatectomy). Qualitative and semiquantitative evaluation of immunohistochemistry staining will be carried out by a single experienced pathologist. Immunoreactivity will be also quantified using digital image analysis based on two parameters: intensity of immunoreactivity and percentage of immunoreactive cells [46].Different biomarkers are assessed: DNA-PKcs and PARP1 (proteins implicated in the DNA repair mechanism), PSA (marker of androgen receptor activity), androgen receptor (tumoural and stromal tissue), Ki67 (marker of proliferative activity), ARV7 (AR splice variant 7 implicated in 2° generation anti-androgen resistance), yH2AX (marker of double strand breaks), PSMA (prostate specific membrane antigen), etc.
- Difference in proportions of pathological downstaging (any decrease in T stage from clinical to pathological stage)
- Complete pathological response rates (no evidence of tumour in the postoperative specimen, pT0)
- Difference in proportions of patients with pN1 disease.
- Translational endpoints
- Whole transcriptome analysis will follow amplification with optimized reagent chemistry for FFPE extracted RNA and hybridization to 1.4 million feature gene expression microarrays.
- To assess differences at the transcriptome level in pre- vs post-treatment tissues from the same patient
- To evaluate the relationship between transcriptome alterations and clinical outcomes of patients in both arms
- To assess the full exome (exome sequencing)
-
To assess copy number aberration profiles between armsAll transcriptome analysis will be performed by Genome-DX (San Diego, CA, USA).Genomic analysis will be performed by the Laboratory of Molecular Endocrinology (KU Leuven).
- Clinical endpoints
- Differences in:
- ◦ PSA kinetics during and after treatment
- ◦ Difference in proportions of patients with PSA ≤ 0.3 ng/ml after neoadjuvant treatment and before primary treatment.
- ◦ Three-year biochemical recurrence-free survival (biochemical recurrence: PSA > 0.2 ng/ml confirmed by a second PSA evaluation taken at least one week apart).
- ◦ Testosterone changes during the study period
- ◦ Peri-operative parameters (operative time, blood loss, grade of surgical difficulty, etc.)
- ◦ Patient-Reported Sexual, continence and quality of life outcomes based on validated questionnaires (IEEF5, ICIQ EORTC, QLQ-C30)
- ◦ Safety and tolerability will be assessed during the treatment period by collecting adverse events and severe adverse events. Perioperative complications will be assessed by the Clavien-Dindo classification of surgical complications [47].
-
Radiological endpointsAll radiology evaluations will be done by a dedicated uro-radiologists and specialists in nuclear medicine.
- Maximum and mean Standardized Uptake Value (SUV) in the volume of interest (VOI) defined as index lesion on MR: 1) SUV change (delta) per arm comparing SUV values before and after treatment 2) SUV delta between the two arms.
- Correlation between SUV values and the tumour volume (TV) in the correspondent VOI at definitive pathology.
- Correlation between SUV values and PSMA expression at IHC on the prostate specimen
- Change of MR TV: 1) TV change (delta) per arm comparing TV values before and after treatment 2) TV deltas between the two arms.
- Correlation between MRI TV and TV of the correspondent ROI at definitive pathology.
- Proportion of PI-RADS scores between the arms
- Correlation between PI-RADS score (latest version available) and pathologic Gleason score
- Clinical down-staging and assessment of LNI (proportions of patients with pN1 disease)
-
Data analysis
Sample size calculation
Sample size calculation was performed to detect 30% difference in proportions of patients in MRD between the two arms with a power of 80% and an α level of 0.05. We consider a difference of at least 30% in proportions of MRD significant because we expect MRD < 20% in the control arm and at least 45% in the treatment arm. This assumption is based on recent data; 20% MRD was observed in patients treated by goserelin + dutasteride [48] probably similar to our control arm. 74% of patients treated with enzalutamide + dutasteride + LHRH analogue [49] had MRD and this group would represent a similar setting as in our study. However, previous data showed 45% MRD in patient treated by abiraterone acetate + LHRH analogue before radical prostatectomy for high-risk PCa [39]. Thus, we set the expected MRD proportion at 45% instead of 74% to be able to detect smaller differences. Calculations are based on a 2-sided Fisher exact test, using SAS PROC POWER software. A sample size of 42 patients per arm is required to verify the main hypothesis. Considering a drop-out of 20%, a total sample size of 102 patients is required. Applying a 1:1 allocation ratio, 51 patients per arm should be included.
Statistical analysis
The primary endpoint will be analyzed by using an intention to treat (ITT) approach. Per protocol (PP) analysis will be also performed, especially for translational endpoints. For the descriptive statistics, Chi-square test or Fisher exact test will be used to compare proportions and paired t-test (or non-parametric alternatives) to compare pre-post treatment variations. Kaplan-Meier analysis with log-rank test will be used for survival analyses.
The assessment of the transcriptome in tumour tissue pre vs post-treatment and in the two groups will be performed using the mean fold-difference and statistical tests for significance. Unsupervised and supervised clustering analysis will be performed using all the genes or treatment relevant gene networks and pathways. For genome analysis, unsupervised and supervised analysis of expression (e.g. hierarchical clustering, heat maps, box plots etc.) will be performed.
Discussion
ARNEO aims to assess the anti-tumour effect of a complete androgen blockade based on apalutamide + degarelix versus degarelix alone. The rapid decrease of testosterone demonstrated by degarelix obviates the need to add an antiandrogen in the placebo arm which could have masked the effect of the apalutamide, at least at the start of the treatment. The risk for selection bias due to the difference in preoperative tumour volume is compensated by the randomization process and the blinding of participants and personnel to 68Ga -PSMA-11 PET/MR. In this study there is the unique possibility to evaluate the molecular response to two ADT regimens at once. From a translational point of view, the possibility to analyze the surgical PCa specimen after neoadjuvant therapy and compare this material to the prostate biopsy, represents a unique opportunity. Preoperative treatment provides a platform to evaluate pharmacodynamics endpoints of novel agents and enable the identification of signals of biologic activity. In addition, it may allow for the identification of molecular and biologic prognostic and predictive factors. In this respect, some promising but mainly preclinical data have been reported on the relationship between androgen receptor signalling and DNA damage response pathways [21, 50–56]. We wish to explore this field through IHC, transcriptome analyses and genome analysis. We chose DNA-PKcs and PARP1 as target proteins for IHC because androgens can activate their transcription [21]. DNA-PKcs is implicated in double strand break (DSB) repair [55]. PARP1 is a nuclear enzyme implicated in DNA repair, tumour proliferation and mediation of androgen receptor-DNA interaction. It can activate the DNA repair process [56, 57]. The therapeutic potential of PARP1 inhibitors has been tested in an explant system of primary human tumours, showing that inhibiting PARP1 enzyme leads to a decrease in tumour proliferation [54]. TOPARP-A (The Trial of PARP Inhibition in Prostate Cancer) phase 2 trial studied the PARP inhibitor olaparib in mCRPC patients showing good response rates particularly for BRCA1/2 or ATM gene-mutated tumours that justified the breakthrough therapy designation by FDA (Food and Drug Administration) [23]. Changes in gene expression after hormonal treatment for PCa have been studied, and have consistently shown a relationship between androgen receptor signalling and DNA repair [50–52]. This link might explain the beneficial effects of androgen deprivation therapy in combination with EBRT, as it is well known that targeting DNA repair mechanisms results in enhanced radio-sensitivity [53]. Although LHRH analogues are commonly used together with EBRT, it is well known that other androgen sources remain active during treatment. Therefore, a certain level of androgen receptor activity remains in PCa cells even under hormonal treatment. This mechanism could sustain the DNA repair mechanisms, potentially causing tumour resistance to ionizing irradiation. The effect of three, 6 and 9 months of neoadjuvant ADT on gene expression in radical prostatectomy samples has been assessed in earlier studies [58]. Medical castration reduced tissue androgens by 75% but also the expression of several androgen-regulated genes including NDRG1, FKBP5, and TMPRSS2; however, androgen receptor and PSA gene expression were not completely suppressed. These data suggest that suboptimal suppression of the androgen receptor axis may be the cause of resistance not only at the primary tumour site but probably also at the level of micro-metastases with important implications in the neoadjuvant treatment of PCa. The use of new generation compounds with more effective androgen receptor pathway inhibition could counteract this remnant androgen activity. The recent LATITUDE phase 3 trial demonstrated that the relative risk of death decreased of 38% in the abiraterone + prednisone + ADT arm vs placebo’s + ADT in metastatic castration sensitive PCa patients [59]. These data suggest that a more effective inhibition of the AR pathway had a therapeutic effect compared to first generation ADT. From this perspective, ATLAS phase 3 trial is randomizing patients to LHRH analogue or LHRH analogue + apalutamide together with EBRT to assess metastasis free survival (NCT02531516).
Acknowledgments
The initial draft of ARNEO trial was accepted for participation (LT) at “Methods in Clinical Cancer Research Workshop” (MCCR) organized by ECCO (European CanCer Organisation)-AACR (American Association for Cancer Research)-EORTC (European Organisation for Research and Treatment of Cancer)-ESMO (European Society for Medical Oncology).
Funding
This study received research grants from Janssen and Ferring which also provide the investigational medical products (apalutamide and degarelix respectively). Leuven Cancer Institute supports part of the statistical analyses. The ULB contribution is supported by the Fonds Yvonne Boël (Brussels, Belgium) and the European Regional Development Fund and the Walloon Region (Belgium). SJ is a Senior Clinical Investigator of the Research Foundation – Flanders (FWO). De Wever Fonds supported the publication costs.
Availability of data and materials
Not applicable.
Authors’ contributions
LT and SJ authored the ARNEO protocol with specific contributions from the other coauthors. All authors were involved in drafting the manuscript or revising it critically for important intellectual content and gave final approval of the version to be published. All authors take public responsibility for appropriate portions of the content; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
Medical Ethics Committee UZ KU Leuven / Research.
Consent for publication
LT an SJ consent for publication of this article considering that similar content was available in the PhD thesis of LT (ISBN-NUMBER: 9789082757606 for the printed version and 9,789,082,757,613 for the e-version).
Competing interests
LT: research grants from Bayer, Ipsen, Ferring, Janssen; Consulting or Advisory Role for Ipsen. Travel, Accomodation, Expenses from Astellas, Bayer and Pierre-Fabre. WE: Consulting fees: Bayer, Janssen; Travel, Accomodation, Expenses from Astellas. SJ: Research grants from Bayer, Ipsen, Ferring, Janssen; Honoraria from Bayer, Ferring, Astellas, Ipsen, Janssen. Travel, Accomodation, Expenses from Bayer, Ferring, Astellas, Ipsen, Janssen. ED: employee and stockholder of GenomeDx makers of Decipher. CB: employee and stockholder of GenomeDx makers of Decipher.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 2.Mottet N, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol. 2016; 10.1016/j.eururo.2016.08.003. [DOI] [PubMed]
- 3.Rider JR, Sandin F, Andrén O, et al. Long-term outcomes among non-curatively treated men according to prostate cancer risk category in a nationwide, population-based study. Eur Urol. 2013;63(1):88–96. doi: 10.1016/j.eururo.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Hamdy FC, Donovan JL, Lane JA, et al. 10-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Localized Prostate Cancer. N Engl J Med. 2016;375(15):1415–1424. doi: 10.1056/NEJMoa1606220. [DOI] [PubMed] [Google Scholar]
- 5.Cooperberg MR, Carroll PR. Trends in Management for Patients With Localized Prostate Cancer, 1990-2013. JAMA. 2015;314(1):80–82. doi: 10.1001/jama.2015.6036. [DOI] [PubMed] [Google Scholar]
- 6.Ward JF, Slezak JM, Blute ML, Bergstralh EJ, Zincke H. Radical prostatectomy for clinically advanced (cT3) prostate cancer since the advent of prostate-specific antigen testing: 15-year outcome. BJU Int. 2005;95(6):751–756. doi: 10.1111/j.1464-410X.2005.05394.x. [DOI] [PubMed] [Google Scholar]
- 7.Kuske A, Gorges TM, Tennstedt P, et al. Improved detection of circulating tumour cells in non-metastatic high-risk prostate cancer patients. Sci Rep. 2016;6 10.1038/srep39736. [DOI] [PMC free article] [PubMed]
- 8.Mohler JL, Armstrong AJ, Bahnson RR, et al. Prostate cancer, Version 3.2012: featured updates to the NCCN guidelines. J Natl Compr Cancer Netw. 2012;10:1081–7. [DOI] [PubMed]
- 9.Shelley MD, Kumar S, Wilt T, et al. A systematic review and meta-analysis of randomised trials of neo-adjuvant hormone therapy for localised and locally advanced prostate carcinoma. Cancer Treat Rev. 2009;35(1):9–17. doi: 10.1016/j.ctrv.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Kumar S, Shelley M, Harrison C, Coles B, Wilt TJ, Mason MD. Neo-adjuvant and adjuvant hormone therapy for localised and locally advanced prostate cancer. Cochrane Database Syst Rev. 2006;18(4):CD006019. doi: 10.1002/14651858.CD006019.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tosco L, Laenen A, Briganti A, et al. The survival impact of neoadjuvant hormonal therapy before radical prostatectomy for treatment of high-risk prostate cancer. Prostate Cancer Prostatic Dis. 2017; 10.1038/pcan.2017.29. [DOI] [PubMed]
- 12.McKay RR, Choueiri TK, Taplin ME. Rationale for and review of neoadjuvant therapy prior to radical prostatectomy for patients with high-risk prostate cancer. Drugs. 2013;73(13):1417–1430. doi: 10.1007/s40265-013-0107-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sciarra A, Fasulo A, Ciardi A, et al. A meta-analysis and systematic review of randomized controlled trials with degarelix versus gonadotropin-releasing hormone agonists for advanced prostate cancer. Medicine (Baltimore) 2016;95(27):e3845. doi: 10.1097/MD.0000000000003845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Axcrona K, Aaltomaa S, da Silva CM, et al. Androgen deprivation therapy for volume reduction, lower urinary tract symptom relief and quality of life improvement in patients with prostate cancer: degarelix vs goserelin plus bicalutamide. BJU Int. 2012;110(11):1721–1728. doi: 10.1111/j.1464-410X.2012.11107.x. [DOI] [PubMed] [Google Scholar]
- 15.Sayyid RK, Evans A, Hersey K, et al. A Phase II, Randomized, Open-Label Study of Neoadjuvant Degarelix versus LHRH Agonist in Prostate Cancer Patients Prior to Radical Prostatectomy. Clin Cancer Res. 2017;23(8):1974–1980. doi: 10.1158/1078-0432.CCR-16-1790. [DOI] [PubMed] [Google Scholar]
- 16.Klotz L, Boccon-Gibod L, Shore ND, et al. The efficacy and safety of degarelix: a 12-month, comparative, randomized, open-label, parallel-group phase III study in patients with prostate cancer. BJU Int. 2008;102(11):1531–1538. doi: 10.1111/j.1464-410X.2008.08183.x. [DOI] [PubMed] [Google Scholar]
- 17.Crawford ED, Shore ND, Moul JW, Tombal B, et al. Long-term tolerability and efficacy of degarelix: 5-year results from a phase III extension trial with a 1-arm crossover from leuprolide to degarelix. Urology. 2014;83(5):1122–1128. doi: 10.1016/j.urology.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Touijer KA, Chen Y, Carver BS, et al. Establishing a neoadjuvant platform for developing targeted agents: Degarelix prior to prostatectomy for patients with intermediate- and high-risk prostate cancer. J Clin Oncol. 2014;32(suppl 15):TPS5105-TPS5105.
- 19.Clegg NJ, Wongvipat J, Joseph JD, et al. ARN-509: a novel antiandrogen for prostate cancer treatment. Cancer Res. 2012;72(6):1494–1503. doi: 10.1158/0008-5472.CAN-11-3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith MR, Antonarakis ES, Ryan CJ, et al. Phase 2 Study of the Safety and Antitumour Activity of Apalutamide (ARN-509), a Potent Androgen Receptor Antagonist, in the High-risk Nonmetastatic Castration-resistant Prostate Cancer Cohort. Eur Urol. 2016;70(6):963–970. doi: 10.1016/j.eururo.2016.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polkinghorn WR, Parker JS, Lee MX, et al. Androgen receptor signaling regulates DNA repair in prostate cancers. Cancer Discov. 2013;3(11):1245–1253. doi: 10.1158/2159-8290.CD-13-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mills IG. Maintaining and reprogramming genomic androgen receptor activity in prostate cancer. Nat Rev Cancer. 2014;14(3):187–198. doi: 10.1038/nrc3678. [DOI] [PubMed] [Google Scholar]
- 23.Mateo J, Carreira S, Sandhu S, et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N Engl J Med. 2015;373(18):1697–1708. doi: 10.1056/NEJMoa1506859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Claessens F, Helsen C, Prekovic S, et al. Emerging mechanisms of enzalutamide resistance in prostate cancer. Nat Rev Urol. 2014;11(12):712–716. doi: 10.1038/nrurol.2014.243. [DOI] [PubMed] [Google Scholar]
- 25.Karantanos T, Evans CP, Tombal B, et al. Understanding the mechanisms of androgen deprivation resistance in prostate cancer at the molecular level. Eur Urol. 2015;67(3):470–479. doi: 10.1016/j.eururo.2014.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li Y, Chan SC, Brand LJ, et al. Androgen receptor splice variants mediate enzalutamide resistance in castration-resistant prostate cancer cell lines. Cancer Res. 2013;73(2):483–489. doi: 10.1158/0008-5472.CAN-12-3630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu Z, Chen S, Sowalsky AG, et al. Rapid induction of androgen receptor splice variants by androgen deprivation in prostate cancer. Clin Cancer Res. 2014;20(6):1590–1600. doi: 10.1158/1078-0432.CCR-13-1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Efstathiou E, Titus M, Wen S, et al. Molecular characterization of enzalutamide-treated bone metastatic castration-resistant prostate cancer. Eur Urol. 2015;67(1):53–60. doi: 10.1016/j.eururo.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Corcoran N, HOvens C, Howard N, et al. The predictive value of ARv7 expression in localized prostate cancer treated with abiraterone, degarelix, and bicalutamide. J Clin Oncol. 2015;33(suppl 7):71–7.
- 30.Kane CJ, Presti JC, Jr, Amling CL, Aronson WJ, Terris MK, Freedland SJ, et al. J Urol. 2007;177:113–117. doi: 10.1016/j.juro.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 31.Briganti A, Karnes RJ, Gandaglia G, et al. Natural history of surgically treated high-risk prostate cancer. Urol Oncol. 2015;33(4):163–e7-13. doi: 10.1016/j.urolonc.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 32.McGuire SE, Lee AK, Cerne JZ, et al. PSA response to neoadjuvant androgen deprivation therapy is a strong independent predictor of survival in high-risk prostate cancer in the dose-escalated radiation therapy era. Int J Radiat Oncol Biol Phys. 2013;85(1):e39–e46. doi: 10.1016/j.ijrobp.2012.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zelefsky MJ, Gomez DR, Polkinghorn WR, et al. Biochemical response to androgen deprivation therapy before external beam radiation therapy predicts long-term prostate cancer survival outcomes. Int J Radiat Oncol Biol Phys. 2013;86(3):529–533. doi: 10.1016/j.ijrobp.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 34.Eder M, Schäfer M, Bauder-Wüst U, et al. 68Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug Chem. 2012;23(4):688–697. doi: 10.1021/bc200279b. [DOI] [PubMed] [Google Scholar]
- 35.Afshar-Oromieh A, Zechmann CM, Malcher A, et al. Comparison of PET imaging with a 68Ga-labelled PSMA ligand and 18F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41(1):11–20. doi: 10.1007/s00259-013-2525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yin L, Rao P, Elson P, et al. Role of TMPRSS2-ERG Gene Fusion in Negative Regulation of PSMA Expression. PLoS One. 2011;6(6):e21319. doi: 10.1371/journal.pone.0021319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wright GL, Jr, Grob BM, Haley C, et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology. 1996;48(2):326–334. doi: 10.1016/s0090-4295(96)00184-7. [DOI] [PubMed] [Google Scholar]
- 38.Maurer T, Beer AJ, Wester HJ, et al. Positron emission tomography/magnetic resonance imaging with 68 Gallium-labeled ligand of prostate-specific membrane antigen: Promising novel option in prostate cancer imaging? Int J Urol. 2014;21 10.1111/iju.12577. [DOI] [PubMed]
- 39.Taplin ME, Montgomery B, Logothetis CJ, et al. Intense androgen-deprivation therapy with abiraterone acetate plus leuprolide acetate in patients with localized high-risk prostate cancer: results of a randomized phase II neoadjuvant study. J Clin Oncol. 2014;32(33):3705–3715. doi: 10.1200/JCO.2013.53.4578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan A-W, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 Statement: Defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–207. doi: 10.7326/0003-4819-158-3-201302050-00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 Explanation and Elaboration: Guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kurbegovic S, Berg KD, Thomsen FB, et al. The risk of biochemical recurrence for intermediate-risk prostate cancer after radical prostatectomy. Scand J Urol. 2017;51(6):450–6. 10.1080/21681805.2017.1356369. [DOI] [PubMed]
- 43.Beauval JB, Ploussard G, Cabarrou B, et al. Improved decision making in intermediate-risk prostate cancer: a multicenter study on pathologic and oncologic outcomes after radical prostatectomy. World J Urol. 2017;35(8):1191–7. [DOI] [PubMed]
- 44.Zumsteg ZS, Chen Z, Howard LE, et al. Number of Unfavorable Intermediate-Risk Factors Predicts Pathologic Upstaging and Prostate Cancer-Specific Mortality Following Radical Prostatectomy: Results From the SEARCH Database. Prostate. 2017;77(2):154–163. doi: 10.1002/pros.23255. [DOI] [PubMed] [Google Scholar]
- 45.Joniau S, Van den Bergh L, Lerut E, et al. Mapping of pelvic lymph node metastases in prostate cancer. Eur Urol. 2013;63(3):450–458. doi: 10.1016/j.eururo.2012.06.057. [DOI] [PubMed] [Google Scholar]
- 46.Decaestecker C, Lopez XM, D'Haene N, et al. Requirements for the valid quantification of immunostains on tissue microarray materials using image analysis. Proteomics. 2009;9(19):4478–4494. doi: 10.1002/pmic.200800936. [DOI] [PubMed] [Google Scholar]
- 47.Clavien PA, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 48.Mostaghel EA, Nelson PS, Lange P, et al. Targeted androgen pathway suppression in localized prostate cancer: a pilot study. J Clin Oncol. 2014;32(3):229–237. doi: 10.1200/JCO.2012.48.6431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Montgomery B, Tretiakova MS, Joshua AM, et al. Neoadjuvant Enzalutamide Prior to Prostatectomy. Clin Cancer Res. 2016; 10.1158/1078-0432.CCR-16-1357. [DOI] [PMC free article] [PubMed]
- 50.Holzbeierlein J, Lal P, LaTulippe E, et al. Gene expression analysis of human prostate carcinoma during hormonal therapy identifies androgen-responsive genes and mechanisms of therapy resistance. Am J Pathol. 2004;164(1):217–227. doi: 10.1016/S0002-9440(10)63112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lehmusvaara S, Erkkilä T, Urbanucci A, et al. Chemical castration and anti-androgens induce differential gene expression in prostate cancer. J Pathol. 2012;227(3):336–345. doi: 10.1002/path.4027. [DOI] [PubMed] [Google Scholar]
- 52.Rajan P, Sudbery IM, Villasevil ME, et al. Next-generation sequencing of advanced prostate cancer treated with androgen-deprivation therapy. Eur Urol. 2014;66(1):32–39. doi: 10.1016/j.eururo.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jorgensen TJ. Enhancing radiosensitivity: targeting the DNA repair pathways. Cancer Biol Ther. 2009;8(8):665–670. doi: 10.4161/cbt.8.8.8304. [DOI] [PubMed] [Google Scholar]
- 54.Ramakrishnan Geethakumari P, Schiewer MJ, Knudsen KE, Kelly WK. PARP Inhibitors in Prostate Cancer. Curr Treat Options in Oncol. 2017;18(6):37. doi: 10.1007/s11864-017-0480-2. [DOI] [PubMed] [Google Scholar]
- 55.Goodwin JF, Schiewer MJ, Dean JL, et al. A hormone-DNA repair circuit governs the response to genotoxic insult. Cancer Discov. 2013;3(11):1254–1271. doi: 10.1158/2159-8290.CD-13-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bartek J, Mistrik M, Bartkova J. Androgen receptor signaling fuels DNA repair and radioresistance in prostate cancer. Cancer Discov. 2013;3(11):1222–1224. doi: 10.1158/2159-8290.CD-13-0679. [DOI] [PubMed] [Google Scholar]
- 57.Schiewer MJ, Goodwin JF, Han S, et al. Dual roles of PARP-1 promote cancer growth and progression. Cancer Discov. 2012;2(12):1134–1149. doi: 10.1158/2159-8290.CD-12-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mostaghel EA, Page ST, Lin DW, Fazli L, Coleman IM, True LD, et al. Intraprostatic androgens and androgen-regulated gene expression persist after testosterone suppression: therapeutic implications for castration-resistant prostate cancer. Cancer Res. 2007;67:5033–5041. doi: 10.1158/0008-5472.CAN-06-3332. [DOI] [PubMed] [Google Scholar]
- 59.Fizazi K, Tran N, Fein L, et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N Engl J Med. 2017;377(4):352–360. doi: 10.1056/NEJMoa1704174. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


