Abstract
Background:
Dysfunctional uterine bleeding (DUB) is one of the most common gynecological disorders encountered in women during the reproductive age. Yoga therapy has shown promising benefits in several gynecological disorders.
Methods:
Thirty women between the ages of 20 and 40 years with primary DUB were randomly assigned to a yoga (n = 15) and a waitlist control group (n = 15). Participants in the yoga group received a 3-month yoga module and were assessed for hemoglobin values, endometrial thickness (ET), pictorial blood loss assessment chart (PBAC), State-Trait Anxiety Inventory, perceived stress scale, and Pittsburgh Sleep Quality Index (PSQI) before and after a 3-month follow-up period.
Results:
At the end of 3 months of intervention, the yoga group, unlike the control group, reported a significant reduction in the anxiety scores (P < 0.05) and perceived stress (P < 0.05). The PSQI scores indicated a reduction in sleep disturbances (P < 0.001) and the need for sleep medications (P < 0.01) and higher global scores (P < 0.001). However, there were no changes in PBAC and ET in both the groups.
Conclusion:
The results indicate that yoga therapy positively impacts the outcome of DUB by reducing the perceived stress and state anxiety and improving the quality of sleep. This warrants larger clinical trials to validate the findings of this pilot study.
KEYWORDS: Dysfunctional uterine bleeding, menstrual disorders, yoga, yoga therapy
INTRODUCTION
Menstrual cycle is a complex entity involving many interactions of the central nervous, endocrine, and reproductive systems, i.e., hypothalamus, pituitary gland, and ovaries. It has been observed that many pathophysiological states associated with menstrual dysfunction have an increased incidence in the recent past. Over the years, it has been established that stress and drugs could have a potential to affect the menstrual cycle in various ways.[1]
Dysfunctional uterine bleeding (DUB) is defined as a state of abnormal uterine bleeding without any clinically detectable organic, systemic, or iatrogenic cause.[2] Data from the WHO's multicenter survey report the prevalence of excessive menstrual bleeding ranging from 8% to 27%.[3,4] DUB is most common in extremes of the reproductive age. Among women aged 30–49 years, one in twenty consults the general practitioner each year with menorrhagia, making DUB one of the most commonly encountered gynecological problems. About 30% of all women report having had menorrhagia, and it accounts for two-thirds of all hysterectomies.[5] The prevalence of the occurrence of DUB is found to be ovular (10%) and anovular or oligo-ovular (90%), the latter being the most common cause of abnormal uterine bleeding.[5]
Among psychological factors, stress is the most imperative factor affecting the menstrual cycle. Stress influences all the body systems through other neurohormonal connections, the hypothalamo–pituitary–adrenal (H-P-A axis) as well as hypothalamo–pituitary–ovarian axis (H-P-O axis). Studies demonstrate that the glucocorticoids released due to the stress put forth an inhibitory action on the gonadotropin-releasing hormone (GnRH), thereby distressing the ovarian function. Elevated levels of corticotrophin-releasing hormone (CRH) and cortisol also suppress the GnRH secretion and consequently decline ovulation. Thus, stress could significantly diminish reproductive functions in an effort to maintain homeostasis.[6] Previous studies have found that the stress influences the incarcerated women leading to high rates of amenorrhea and menstrual irregularity.[7] Evidence also suggests an association of sleep disturbances and disturbed circadian rhythm with menstrual disorders.[8,9] Abnormal uterine bleeding is also associated with loss of health-related quality of life when compared to healthy women with the same age. DUB leads to significant direct and indirect costs as well as loss of productivity.[10]
The most common conventional management of DUB involves progestin therapy in varied doses based on the age. Low-dose combination hormonal contraceptive therapy (20–35 μg ethinylestradiol) is the mainstay of treatment for adolescents up to the age of 18 years. For women aged 40 years or older, before menopause, the treatment consists of cyclic progestin therapy, low-dose oral contraceptive pills, levonorgestrel intrauterine device, or cyclic hormone therapy. Although these treatments are found to be effective, they do have adverse effects on the overall health of the women. The drawback to medical therapy, in addition to side effects, is that the benefit lasts only while the patient takes the medication. Surgical options have concentrated mainly on endometrial ablation and hysterectomy, and it is unclear whether one is superior to the other in terms of long-term outcome and patient satisfaction.[11]
With the advent of adversities with conventional management, patients have started exploring complementary and alternative medicine (CAM) therapies for managing DUB.[12] According to a survey, CAM therapies are commonly used by women for menstrual disorders to reduce pain and discomfort and yoga is among the top 5. The CAM therapies are found to be safe and known to enhance the quality of life in women.[13]
It has been demonstrated that regular practice of yoga has beneficial effects on both phases of the menstrual cycle by bringing physical and psychological well-being and by balancing neuro-endocrinal axis.[14,15] In India, yoga therapy is commonly recommended for treating various noncommunicable diseases and for overall well-being.[16,17,18] Yogic therapy helps in improving hormonal and biochemical changes related to H-P-O and H-P-A axes in polycystic ovarian syndrome (PCOS).[19] Yoga Nidra is reported to be beneficial in managing the psychological impact of menstrual disorders.[20,21] Overall, yoga is known to be beneficial in the general well-being of individuals in health and disease.
To the best of our knowledge, there are no studies reporting the effects of yoga practices on the health status of patients suffering from DUB. Given the vital role of yoga in the management of several disorders relating to women, the current study was executed to ascertain the role of an integrated yoga module in the management of DUB.
METHODS
Design
The present study was a parallel-arm controlled pilot trial to compare the outcome of participants assigned to experimental (yoga and conventional care) group with that of a wait-listed control (conventional care alone) group. Participants were randomly assigned to either yoga or control groups using a computer-generated program (www.randomizer.org) with a 1:1 allocation ratio.
Ethical considerations
The ethics committee of the university approved the study. The variables to be recorded and the study design were described to the participants and a signed informed consent to participate in the study was obtained.
Participants
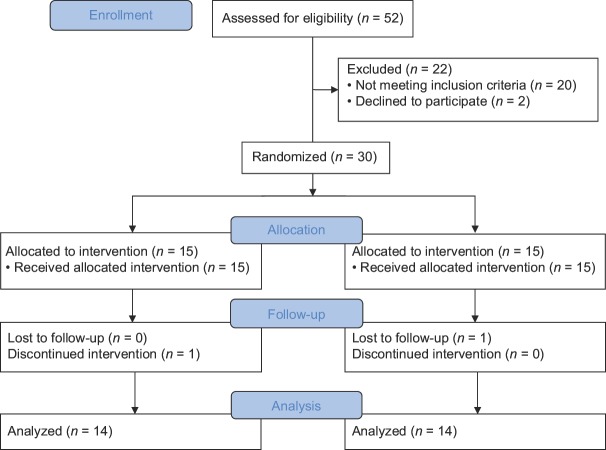
Thirty participants out of 52 were found eligible for the trial. They were randomly allocated into two groups, namely yoga (n = 15, group mean age ± standard deviation (SD), 29.85 ± 4.45 years) and a wait-listed control group (n = 15, group mean age ± SD, 30.85 ± 4.42 years). One participant from each group dropped up during the follow-up period and therefore finally 14 participants in each group were assessed and interpreted. Participants were recruited from the gynecology departments of three leading hospitals in Central India. Participants satisfying the age range of 20–50 years and diagnosed for primary DUB with no underlying systemic pathology were included in the study. Females with benign and malignant pelvic lesions, coagulation disorders, hypothyroidism, liver diseases, and pregnancy were excluded from the study. Figure 1 represents the schematic of the Trial Profile.
Figure 1.
The flow of participants through the trial (trial profile)
Intervention
Yoga group
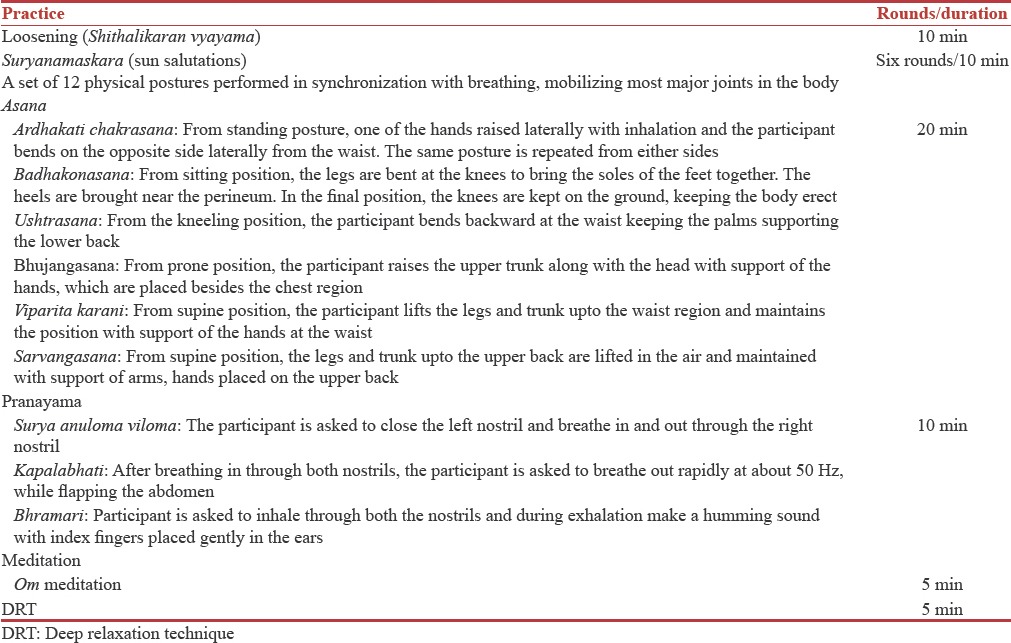
The yoga group was trained in an Integrated Approach of Yoga Therapy (IAYT) specially designed for menstrual disorders [Table 1]. Yoga group practiced this protocol for 3 consecutive months for 60 min a day for 3 days a week. This IAYT protocol included special yoga physical postures (asanas), breathing techniques (pranayama), and meditation (dhyana) for menstrual disorders aiming reduction in bleeding and pain, reduction in stress levels that women undergo during that period, and overall well-being.
Table 1.
Integrated Approach of Yoga Therapy module for dysfunctional uterine bleeding
The wait-listed control group received standard care under the supervision of the consulting gynecologist for the same duration of 3 months. They were offered general counseling and were asked to avoid any yoga-based practices during the experimental duration. After the intervention period, they were offered training in yoga for the same duration as the experimental group.
Assessments
Variables were obtained at baseline and at the end of interventional period. The variables included assessments for blood loss–comprising hemoglobin, pictorial blood loss assessment chart (PBAC), endometrial thickness (ET), and psychological assessments including Spielberger's State-Trait Anxiety Inventory (STAI), Perceived Stress Scale (PSS), and Pittsburgh Sleep Quality Index (PSQI). The assessments were as follows
For the assessment of blood loss
Hemoglobin: Hemoglobin was assessed as a fundamental indicator of blood loss as well as the general health as it signifies the nutritional support for all the systems in the body. Increased amount of blood loss is debilitating and may lead to anemia. Hence, to assess the severity of blood loss, hemoglobin was measured by taking a blood sample. The hemoglobin concentration was measured using the Coulter method
PBAC: The PBAC was used as an alternative for measuring blood loss. A pictorial chart score of 100 or more, when used as a diagnostic test for menorrhagia, was found to have a specificity and sensitivity of >80%[22]
ET: ET was assessed using routine gynecological ultrasound. In the current study, ET was measured at the 11th or 12th day of menstrual cycle.[23]
For the psychological assessment
Spielberger's STAI: Spielberger's STAI was used as a self-report measure with a subset of items for state and trait anxiety. Participants were asked to answer twenty questions in each subtest on a Likert scale from 1 (not at all) to 4 (very much so)[24]
PSS: The Perceived Stress Scale (PSS) is a classic stress assessment instrument. The tool, while originally developed in 1983, remains a popular choice for helping us understand how different situations affect our feelings and our perceived stress. The questions in this scale asked about the subjects feelings and thoughts during the previous month. In each case, subjects were asked to indicate how often they felt or thought a certain way.[25]
PSQI: PSQI is a self-rated questionnaire that assesses sleep quality and disturbances over a 1-month time interval and probes clinically important and patient-relevant symptoms in the areas of sleep quality and quantity. PSQI is a 19-item self-rated questionnaire to assess the quality of sleep. It also includes a 5-bed partner or roommate questions, which are not included in the scoring.[26]
Data analysis
Statistical analysis was performed using IBM SPSS 21.0 (IBM Corp, Armonk, NY). Data were tested for normality and appropriate statistical tests were applied for respective variables.
Paired sample t-test was applied to ascertain the within-group (pre-post) differences for both yoga and control groups. Independent samples t-test was applied to understand the between-group changes in the postscores of hemoglobin, PBAC, ET, STAI, and PSS.
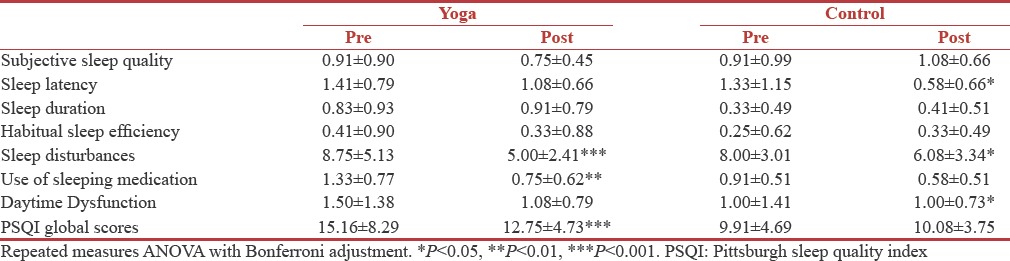
PSQI data were analyzed using repeated measures (RM) ANOVA. There were eight “within-subjects” factors, i.e., subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, daytime dysfunction, and global PSQI score. Post hoc analyses with a least significant difference were performed using Bonferroni correction and all comparisons were made with the respective “pre” states.
For all the analyses, 95% confidence intervals are presented and P < 0.05 was considered statistically significant.
RESULTS
Paired sample t-test and independent samples t-test were run within and between participants, respectively. There were no significant changes between the groups in hemoglobin levels, PBAC, and ET. However, the control group showed significant improvement (paired sample t-test, t = 2.381, P < 0.05) in the pre-post comparison of the hemoglobin levels. Yoga group demonstrated a significant reduction in the perceived stress (paired sample t-test, t = 2.622, P < 0.05) and STAI scores (paired sample t-test, t = 2.159, P < 0.05), whereas the control group had no significant changes. Yoga group also showed significant improvement in the PSQI global scores following the intervention duration (RM ANOVA, mean difference = 5.250, −5.250, P < 0.001) See Tables 2 and 3.
Table 2.
Outcome variables following 12 weeks of Integrated Approach of Yoga Therapy and control

Table 3.
The changes in Pittsburgh Sleep Quality Index following 12 weeks' Integrated Approach of Yoga Therapy and control
DISCUSSION
The present study demonstrated significant reductions in perceived stress and anxiety among women suffering from DUB following the yoga intervention for 12 weeks in comparison to the baseline data. There were no significant changes observed between groups in the hemoglobin, ET, or the PBAC. Although there was a significant increase in hemoglobin in the control group when compared to baseline, the mean postvalue of hemoglobin in the control group remained lower than that of the yoga group. In addition, a mean change of 0.4 g% may not be considered clinically significant. There was no deterioration of hemoglobin levels in the yoga group when compared to baseline. The global scores of PSQI were significantly improved following the practice of yoga and were primarily associated with reduced sleep disturbances and the need for sleep medications.
The role of yoga in reducing stress is well documented,[27,28] and our study concurs with the findings of earlier studies on yoga practices in menstrual disorders. An earlier study comparing the autonomic functions and psychological well-being of females suffering from premenstrual syndrome demonstrated enhanced autonomic functions and psychological well-being following the practice of yoga.[14] There was evidence of significant reduction of the anxiety score in women suffering from PCOS.[15] Nidhi et al. also demonstrated enhanced hormonal profile in women suffering from PCOS following a 12-week integrated yoga intervention.[19] Another study compared the practice of Yoga Nidra, a relaxation technique in yoga, practiced for 6 months by the patients suffering from menstrual irregularities with nonpractitioners. The results of this study reported a significant improvement in psychological well-being and general health following the practice of Yoga Nidra.[21] The current study indicated beneficial effects of yoga practice on sleep in patients with DUB. Earlier studies on yoga show improved sleep quality in different populations.[29] Improvement in the sleep quality may also play a potential role in the regulation of menstruation, by restoring the overall hormonal balance.[30]
The role of perceived stress and anxiety in modulating the hormonal status is well documented.[31] We postulate that yoga may influence the CRH and corticosteroid levels through reduction of perceived stress and anxiety. These hormones are known to inhibit the GnRH secretion and thereby responsible for the ovarian dysfunction in patients suffering from DUB.[5] Therefore, IAYT might be useful in reducing the stress and anxiety and thereby balancing the H-P-O and H-P-A axes. The endocrinal profile could be used as a variable in future studies to understand the underlying mechanisms of beneficial effects of yoga in DUB.
The observations from the current study suggest that there could be an improvement in the hormonal status of the individuals with menstrual disorders due to reduced anxiety, stress, and an improved sleep quality following the practice of yoga.
We speculate that the trend of improvement observed in the variables of the current study could reach statistical significance with a larger sample size. These results therefore warrant further large-scale trials to establish the efficacy of yoga as a treatment modality for patients with DUB. Yoga, being a cost-effective and easy-to-adapt lifestyle intervention, could be a beneficial tool to complement the conventional therapies involved in managing DUB.
CONCLUSION
Although the current study failed to substantiate the benefits of yoga in the objective variables in patients with DUB, the changes in subjective measures were significant to ascertain the beneficial changes. Overall, the results of this pilot study demonstrate that yoga practices can diminish perceived stress and anxiety and improve sleep quality in patients suffering from DUB and thereby improve their quality of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Neinstein LS. Menstrual dysfunction in pathophysiologic states. West J Med. 1985;143:476–84. [PMC free article] [PubMed] [Google Scholar]
- 2.Dutta D. In: Dysfuctional Uterine Bleeding (DUB) 6th ed. Hiralal K, editor. Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2013. [Google Scholar]
- 3.Omran A, Standley C. Family Formation Patterns and Health: An International Collaborative Study in India, Iran, Lebanon, Philippines and Turkey. Geneva: World Health Organization; 1976. [Google Scholar]
- 4.Omran A, Standley C. Family Formation Patterns and Health, Further Studies: An International Collaborative Study in Columbia, Egypt, Pakistan, and the Syrian Arab Republic. Geneva: World Health Organization; 1981. [Google Scholar]
- 5.Farrell E. Dysfunctional uterine bleeding. Aust Fam Physician. 2004;33:906–8. [PubMed] [Google Scholar]
- 6.Berga SL. The brain and the menstrual cycle. Gynecol Endocrinol. 2008;24:537. doi: 10.1080/09513590802296187. [DOI] [PubMed] [Google Scholar]
- 7.Allsworth JE, Clarke J, Peipert JF, Hebert MR, Cooper A, Boardman LA, et al. The influence of stress on the menstrual cycle among newly incarcerated women. Womens Health Issues. 2007;17:202–9. doi: 10.1016/j.whi.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker FC, Lamarche LJ, Iacovides S, Colrain IM. Sleep and menstrual-related disorders. Sleep Med Clin. 2008;3:25–35. [Google Scholar]
- 9.Baker FC, Driver HS. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 2007;8:613–22. doi: 10.1016/j.sleep.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value Health. 2007;10:183–94. doi: 10.1111/j.1524-4733.2007.00168.x. [DOI] [PubMed] [Google Scholar]
- 11.Committee on Practice Bulletins – Gynecology. Practice bulletin no 136: Management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstet Gynecol. 2013;122:176–85. doi: 10.1097/01.AOG.0000431815.52679.bb. [DOI] [PubMed] [Google Scholar]
- 12.Cochrane S, Smith CA, Possamai-Inesedy A, Bensoussan A. Acupuncture and women's health: An overview of the role of acupuncture and its clinical management in women's reproductive health. Int J Womens Health. 2014;6:313–25. doi: 10.2147/IJWH.S38969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fisher C, Adams J, Hickman L, Sibbritt D. The use of complementary and alternative medicine by 7427 Australian women with cyclic perimenstrual pain and discomfort: A cross-sectional study. BMC Complement Altern Med. 2016;16:129. doi: 10.1186/s12906-016-1119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qu Y, Jia Z. Preface JCDR 2013 issue 2. J Cardiovasc Dis Res. 2013;4:77–8. doi: 10.1016/j.jcdr.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effect of holistic yoga program on anxiety symptoms in adolescent girls with polycystic ovarian syndrome: A randomized control trial. Int J Yoga. 2012;5:112–7. doi: 10.4103/0973-6131.98223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vinchurkar SA, Arankalle DV. Integrating yoga therapy in the management of urinary incontinence: A case report. J Evid Based Complementary Altern Med. 2015;20:154–6. doi: 10.1177/2156587214563311. [DOI] [PubMed] [Google Scholar]
- 17.Raghavendra P, Shetty P, Shetty S, Manjunath NK, Saoji AA. Effect of high-frequency yoga breathing on pulmonary functions in patients with asthma: A randomized clinical trial. Ann Allergy Asthma Immunol. 2016;117:550–1. doi: 10.1016/j.anai.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Gowda S, Mohanty S, Saoji A, Nagarathna R. Integrated yoga and naturopathy module in management of metabolic syndrome: A case report. J Ayurveda Integr Med. 2017;8:45–8. doi: 10.1016/j.jaim.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effects of a holistic yoga program on endocrine parameters in adolescents with polycystic ovarian syndrome: A randomized controlled trial. J Altern Complement Med. 2013;19:153–60. doi: 10.1089/acm.2011.0868. [DOI] [PubMed] [Google Scholar]
- 20.Rani K, Tiwari S, Singh U, Singh I, Srivastava N. Yoga Nidra as a complementary treatment of anxiety and depressive symptoms in patients with menstrual disorder. Int J Yoga. 2012;5:52–6. doi: 10.4103/0973-6131.91715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rani K, Tiwari S, Singh U, Agrawal G, Ghildiyal A, Srivastava N, et al. Impact of Yoga Nidra on psychological general wellbeing in patients with menstrual irregularities: A randomized controlled trial. Int J Yoga. 2011;4:20–5. doi: 10.4103/0973-6131.78176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higham JM, O'Brien PM, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. Br J Obstet Gynaecol. 1990;97:734–9. doi: 10.1111/j.1471-0528.1990.tb16249.x. [DOI] [PubMed] [Google Scholar]
- 23.Nalaboff KM, Pellerito JS, Ben-Levi E. Imaging the endometrium: Disease and normal variants. Radiographics. 2001;21:1409–24. doi: 10.1148/radiographics.21.6.g01nv211409. [DOI] [PubMed] [Google Scholar]
- 24.Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (Form Y)(self-Evaluation Questionnaire) 1983 [Google Scholar]
- 25.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 26.Smyth C. The Pittsburgh Sleep Quality Index (PSQI) J Gerontol Nurs. 1999;25:10–1. doi: 10.3928/0098-9134-19991201-10. [DOI] [PubMed] [Google Scholar]
- 27.Parshad O. Role of yoga in stress management. West Indian Med J. 2004;53:191–4. [PubMed] [Google Scholar]
- 28.Saoji AA. Yoga: A Strategy to cope up stress and enhance wellbeing among medical students. N Am J Med Sci. 2016;8:200–2. doi: 10.4103/1947-2714.179962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang F, Eun-Kyoung Lee O, Feng F, Vitiello MV, Wang W, Benson H, et al. The effect of meditative movement on sleep quality: A systematic review. Sleep Med Rev. 2016;30:43–52. doi: 10.1016/j.smrv.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Nowakowski S, Meers J, Heimbach E. Sleep and women's health. Sleep Med Res. 2013;4:1–22. doi: 10.17241/smr.2013.4.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Eck M, Berkhof H, Nicolson N, Sulon J. The effects of perceived stress, traits, mood states, and stressful daily events on salivary cortisol. Psychosom Med. 1996;58:447–58. doi: 10.1097/00006842-199609000-00007. [DOI] [PubMed] [Google Scholar]