Abstract
Background:
The World Health Organization guidelines provide suggestions on early recognition and treatment of severe dengue (SD); however, mortality in this group can be high and is related both to disease severity and the treatment complications.
Subjects and Methods:
In this prospective observational study, we report our results where standard therapy (ST) was enhanced by Intensive Care Unit (ICU) supportive measures that have proven beneficial in other conditions that share similar pathophysiology of capillary leak and fluid overload. These include early albumin for crystalloid-refractory shock, proactive monitoring for symptomatic abdominal compartment syndrome (ACS), application of a high-risk intubation management protocol, and other therapies. We compared outcomes in a matched retrospective cohort who received ST.
Results:
We found improved outcomes using these interventions in patients with the most devastating forms of dengue (ST+ group). We could demonstrate decreased positive fluid balance on days 1–3 and less symptomatic ACS that necessitated invasive percutaneous drainage (7.7% in ST+ group vs. 30% in ST group, P = 0.025). Other benefits in ST+ group included lower intubation and positive pressure ventilation requirements (18.4% in ST+ vs. 53.3% in ST, P = 0.003), lower incidence of major hemorrhage and acute kidney injury, and reduced pediatric ICU stays and mortality (2.6% in ST+ group vs. 26% in ST group, P = 0.004).
Conclusion:
Children with SD with refractory shock are at extremely high mortality risk. We describe the proactive application of several targeted ICU supportive interventions in addition to ST and could show that these interventions resulted in decreased resuscitation morbidity and improved outcomes in SD.
Keywords: Albumin, colloids, fluid overload, intra-abdominal hypertension, plasma leak, resuscitation morbidity, severe dengue, shock
INTRODUCTION
Outcomes of dengue infections are usually excellent;[1,2,3] however, mortality in severe dengue (SD) shock can be as high as 44%–72%,[4,5,6,7] with fluid overload (FO) and malignant edema due to capillary leak being major contributors.[1,2,3,4,5,6,7]
While FO has been alluded to both in the World Health Organization (WHO) guideline and our dengue publications,[3,6,7] therapeutic interventions to manage malignant edema and prevent treatment morbidity have not been fully described. Cognizant of this shortcoming, we focused on several pathophysiology-based Intensive Care Unit (ICU) and emergency department (ED) interventions which may be useful in severe and refractory dengue shock.
In this prospective observational study, we aimed to determine the effect of these proactively applied interventions on mortality, positive fluid balance (PFB), ventilator requirements, Pediatric ICU (PICU) days, and mortality as compared to a matched retrospective cohort with SD who received standard therapy (ST) as per the WHO guidelines.
SUBJECTS AND METHODS
Setting and patient selection
Consecutive patients aged 2 months to 16 years with SD admitted to a 10-bed PICU between September 2009 and November 2015 were included. All patients received ST as per the WHO guidelines.[1] However, patients admitted from October 2011 to November 2015 also received one or more targeted interventions in addition to standard therapy (ST+) in an anticipatory manner. Thus, patients fell into two groups: the prospective cohort (ST+ group: October 2011–November 2015) and the matched retrospective cohort (ST group: September 2009–September 2011).
Inclusions and exclusions
Of all PICU admissions with dengue, only patients with severe forms of dengue in the critical phase whose diagnosis was laboratory confirmed were included. Non-SD, those in the recovery phase of dengue, bacterial co-infections, and moribund patients who died within 3 h of admission were excluded from the study.
Demographic data
At baseline, demographic and clinical data, hemodynamic status, number with hypotensive shock, complete blood count, and Pediatric Risk of Mortality scores were entered in a standard datasheet and samples were drawn to confirm dengue diagnosis and perform blood gas and lactate measurements.
Protocol for management of severe dengue (for all patients)
Management of SD began in the ED, where there was extensive training focusing on early recognition of shock and hemorrhage, serial cardiorespiratory monitoring, and carefully titrated fluids to correct hypovolemia while minimizing FO.[1,3]
Standard therapy group
Management included fluid resuscitation, blood components for major hemorrhage, intubation and ventilation for refractory shock or respiratory failure, and peritoneal dialysis (PD) or continuous renal replacement therapy (CRRT) for established acute kidney injury (AKI) or FO.[1,3]
Targeted intervention group
In addition to ST, one or more targeted ICU interventions [Table 1] were also implemented in a proactive manner.
Table 1.
Targeted interventions for patients with severe dengue and high mortality risk

Ethics
No new interventions were used in the ST+ group, rather the choice of preferred colloid differed in both groups, and standard WHO recommendations were complemented by well-described ICU supportive therapies in a proactive anticipatory manner. The ST group also received ICU supportive interventions in addition to the standard WHO recommendations; however, these were applied in a reactive manner in most cases. Since no new interventions were used, and both colloids have been recommended in dengue,[1,2,3,8] the Institutional Ethics Committee approved the study and waived the need for informed consent.
Statistical analysis
The results are expressed as mean ± standard deviation or median and interquartile range, as appropriate. Comparisons between the ST and ST+ groups were carried out using Student's t-test or Chi-square or Fisher's exact test, or the Wilcoxon test, as appropriate. P = 0.05 was considered statistically significant.
Intervention #1: Restrictive resuscitation and “albumin rescue”
In both groups, and as suggested by the WHO guidelines, controlled fluid replenishment aiming for the lower limit of euvolemia was implemented. Further, in patients who remained in shock despite 30 ml/kg crystalloid over 3 h (crystalloid refractory shock), colloid was used for volume replacement, provided hemorrhage had been ruled out.
In the ST group, the majority received 4% gelatin (gelofusine) at volumes not >30 m/kg/day.
In the ST+ group, albumin was the preferred colloid (“Albumin Rescue”), this was administered at a dose of 1 g/kg as an infusion over 6 h in addition to crystalloids, the total volumes of which were titrated to maintain perfusion targets.
Intervention #2: Large volume ascites and intra-abdominal hypertension
Approach in standard therapy group
In this group, intra-abdominal pressure (IAP) monitoring through bladder pressure measurement was performed in patients who developed tense ascitic collections. If the IAP was elevated, medical treatment followed by percutaneous drainage was initiated [Table 1].
Approach in targeted intervention group
In this group, rather than waiting for clinically obvious abdominal distension, the IAP was proactively monitored 2 hourly in all patients who received >30 ml/kg fluid in 3–4 h, and elevated values were treated similarly.
Intervention #3: Peri-intubation decompensation and the high-risk intubation management protocol
Noninvasive positive pressure ventilation (NIPPV) was the initial choice in both groups among patients requiring respiratory support. Intubation and PPV were initiated for failed NIPPV and for patients who presented in extremis.
Approach in standard therapy group
Peri-intubation strategies for intubation included lower doses of benzodiazepines and opioids, and in patients who developed peri-intubation hypotension, fluid resuscitation and inopressors were initiated.
Approach in targeted intervention group
A high-risk intubation management protocol comprising of preemptive strategies to prevent peri-intubation cardiorespiratory decompensation was used, including preference for low-dose ketamine, preintubation continuous positive airway pressure (CPAP), and inopressor infusions in all cases prior to induction [Table 1].
Intervention #4: Prevention and management of major hemorrhage
Approach in both groups
Central lines and arterial catheters were considered only in fluid refractory shock, and both groups had invasive lines inserted under ultrasound guidance with a preference for compressible sites. Nasal tubes (tracheal/enteral) were avoided, thereby minimizing hemorrhagic complications.
Approach in standard therapy group
In the event of major hemorrhage, circulatory support and targeted blood components (platelets, fresh frozen plasma, cryoprecipitate, and packed red blood cells) were infused repeatedly aiming to normalize deranged coagulation.
Approach in the targeted intervention group
Hemorrhage and bleeding were controlled by a multipronged approach, including hemostatic measures in the first instance wherever possible. Other interventions included proactive efforts directed at minimizing components of the lethal triad and preference for fresh whole blood (FWB) rather than individual blood components and tranexamic acid (TXA) infusion.
Intervention #5: Fluid removal and renal replacement therapy
Fluid removal using diuretics was instituted in patients who developed features of FO after shock/plasma leak was under control. RRT was considered in diuretic-resistant patients who developed FO and/or AKI.
p>Approach in standard therapy group
In the ST group, PD and CRRT were used for diuretic-resistant FO/AKI.
Approach in targeted intervention group
Sustained low-efficiency dialysis (SLED) was preferentially used for patients with diuretic-resistant FO/AKI.
RESULTS
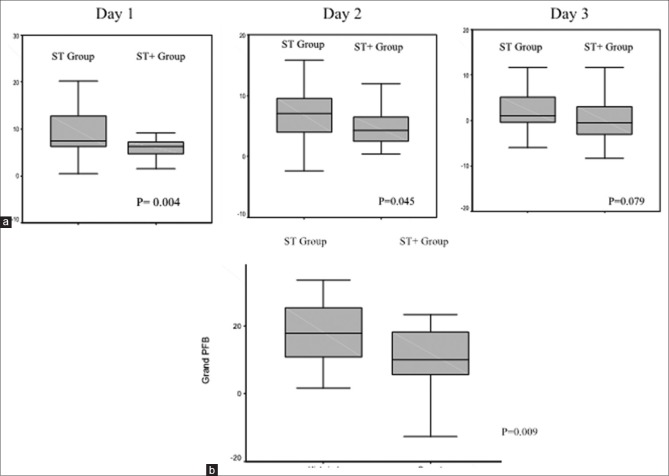
During the ST-only period, thirty of forty PICU admissions with SD satisfied inclusion criteria, while during the ST+ period, of 43 patients with SD who required PICU admission, 38 qualified for inclusion and constituted the ST+ group [Figure 1a].
Figure 1.
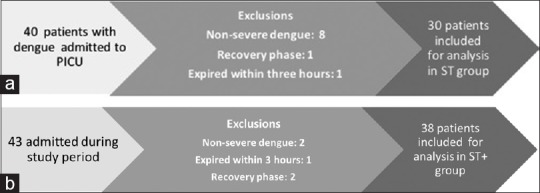
(a)Flow of patients in standard therapy group. (b) Flow pattern of patients in ST+ group
Table 2 describes the baseline demography. There were no differences in age, weight, and severity grades, including the number admitted with hypotensive shock between the groups. However, the admission hematocrit was lower in the ST group compared to the ST+ group.
Table 2.
Demography and patient details
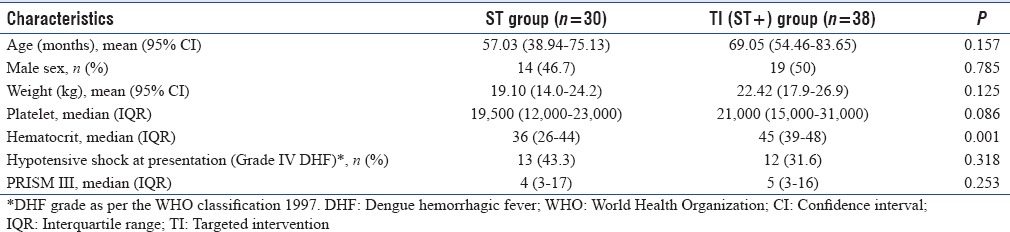
Table 3 describes the ICU supportive therapies and complications of SD patients in both groups.
Table 3.
Intensive care supportive therapies and complications in severe dengue

With respect to the choice of colloid in patients who remained in shock despite 30 ml/kg crystalloid, 4% gelatin was the preferred colloid in the ST group and one patient also received albumin. In the ST+ group, albumin was used as the preferred colloid in 42% of patients (albumin rescue).
The ST+ group had a significant reduction in FO and less PFB on days 1–3 [Table 3 and Figures 1, 2]. A significantly fewer number required intubation and IPPV compared to the ST group (18.4% ST+ vs. 53.3% in ST, P = 0.003). Furthermore, fewer patients in the ST+ group developed symptomatic abdominal compartment syndrome (ACS) that necessitated invasive percutaneous drainage compared to the ST group (7.7% vs. 30%, P = 0.025) [Table 3].
Figure 2.
(a) Box plots showing positive fluid balance on days 1, 2, and 3, with P value 0.004 ( Day-1), 0.045 ( Day 2), 0.079 ( Day 3). (b) Box plots showing grand positive fluid balance on the first 72 h of pediatric Intensive Care Unit. ST: Standard therapy group; ST+: Targeted intervention group
With regard to peri-intubation events, hypotension occurred soon after induction in 3 of 16 intubated patients in the ST group, all of whom were stabilized with fluid and inopressors [Table 3].
Among the ST+ group, all the seven patients who needed emergent intubation received preemptive strategies to prevent peri-intubation cardiorespiratory decompensation [Table 1], and these were successful in maintaining peri-intubation cardiopulmonary stability in all the seven patients.
With respect to hemorrhage, better control of shock led to a lower incidence of major hemorrhage in the ST+ group (23.6% in ST+ vs. 53% in ST group) [Table 3], and among those with major hemorrhage, the total volume of infused blood products was lower compared in the ST group (44.4 ± 18.7 ml/kg vs. 79.9 ± 66.4 ml/kg, P = 0.228). Hemostatic measures were successful in controlling local hemorrhage in 5 patients, thereby avoiding the requirement for blood products: two patients had torrential nasopharyngeal hemorrhage which was successfully controlled by cuff tamponade of a Foley catheter inserted nasally, and in three patients, local hemostatic sutures successfully controlled large-volume femoral arterial line hemorrhage.
The incidence of AKI was lower in the ST+ group (5.3% vs. 33%, P = 0.04). Among patients requiring RRT, two patients in the ST group received PD and three underwent CRRT; all the three who underwent CRRT developed hypothermia despite the use of an in-line CRRT fluid-warming device and insulation of tubing. During the ST+ period, two patients developed AKI and were dialyzed using SLED, the latter modality was tolerated well in terms of circulatory and temperature stability.
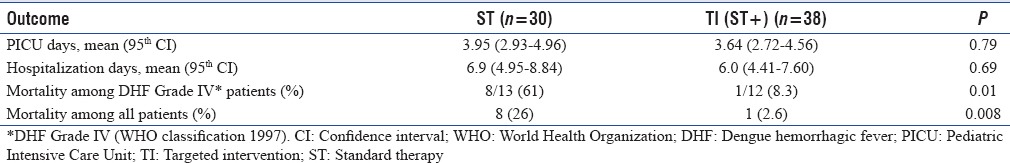
Overall, the PICU days and mortality were significantly reduced in ST+ group versus ST group [mortality 2.6% vs. 26%, P = 0.004, Table 4].
Table 4.
Outcomes of patients with severe dengue requiring intensive care
-
Of The 5 interventions were utilized in the ST+ group as follows [Figure 3 and Table 3], the following findings were noted [Figure 3]:
- “Albumin rescue” was used most frequently in 16 (42%) patients with unresolved shock despite 30 ml/kg crystalloid and was the sole intervention in 11 patients
- Only one patient required tracheal intubation.
-
Three patients required two interventions as follows:
- Two required high-risk intubation management and major hemorrhage management
- One required albumin and major hemorrhage management.
-
Five patients required three interventions each as follows:
- Two required albumin, intubation, and major hemorrhage management
- One required intubation, peritoneal drains, and major hemorrhage management
- One patient required albumin, major hemorrhage management, and peritoneal drain for ACS
- One required intubation, major hemorrhage management, and SLED.
Two patients required four interventions each: Albumin, peritoneal drain, intubation, and major hemorrhage management
One patient required all the five interventions.
Figure 3.
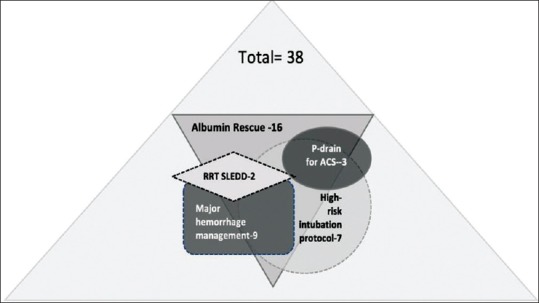
Pictogram depicting targeted interventions among 38 patients in the ST+ group. P-drain: Peritoneal drain; ACS: Abdominal compartment syndrome; RRT-SLED: Renal replacement therapy with slow extended daily dialysis; ST+: Targeted intervention group
DISCUSSION
In this report, we describe several ICU- and ED-targeted interventions that were applied in an anticipatory manner in addition to the standard WHO recommendations in the sickest patients with dengue. These were associated with decreased fluid accumulation and lower incidence of ACS, intubation, and ventilator requirement, less AKI, PICU days, and lower mortality in children with SD as compared to ST. These findings are important because dengue fever occurs mostly in low-/middle-income countries with limited resources and hence an approach that limits treatment morbidity and mortality and conserves intensive care resources is important. While the gold standard for proving benefit is the randomized clinical trial, a pragmatic approach based on improving outcomes may be more practical.[17]
The WHO guidelines emphasize the crucial importance of restrictive fluid resuscitation in order to minimize FO;[1,2] however, FO is common in hypotensive dengue patients who require large volumes for shock reversal.[3] Colloid rescue is suggested by the WHO and Centers for Disease Control and Prevention (CDC) in refractory shock despite crystalloids where hemorrhage has been excluded.[1,3,17] During the ST period, we used gelatin in children with unresolved shock despite initial resuscitation with crystalloid, since dextran was one of the two colloids used in an RCT in dengue shock that compared colloids versus crystalloids and reported improved shock resolution with colloids.[18]
Albumin was preferred in the ST+ group and is suggested by the CDC in SD.[17] A strategy using “Albumin Rescue” has been shown to show decreased “fluid creep” and mortality in severe burn shock, another condition which shares similar pathophysiology of extensive capillary leak and tendency for compartment syndromes as SD.[19,20] In septic shock, reported benefits of albumin include support of the disrupted glycocalyx,[21] better safety profile, and less complications compared to the other synthetic colloids.[22]
Albumin use was associated with shock resolution with lesser PFB in the ST+ group and the decreased FO may have contributed to the lower incidence of malignant edema and ACS [Table 3].
Plasma leak leading to tense ascitic fluid collections and raised IAP resulting in ACS can develop rapidly during large-volume fluid therapy. ACS can further exacerbate shock and oliguria leading to even more fluid infusion and further IAP increase.[9] While extensively reported in trauma and burns, dengue-associated ACS has been infrequently reported and is quite likely to be underrecognized.[3,7,23] Proactive monitoring of IAP in SD receiving > 30 ml/kg in the first 2–3 h can prompt earlier recognition and control of IAP.
With respect to respiratory issues, SD patients may develop hypoxemic respiratory failure due to various reasons; however, PPV can worsen shock by decreasing venous return to the heart.[1,3] Evidence supports efforts to preserve the patient's spontaneous respiratory drive by the use of either NIPPV or CPAP in dengue,[2,3,10] and it was the initial choice of respiratory support in both the ST and ST+ groups.
Patients who fail NIV, or present in extremis, may need intubation, but this can be fraught with complications. Intubation of the hypoxemic, shocked, acidotic dengue patient, who may also be bleeding, may be associated with worsening hypoxemia, hypotension, aspiration, and cardiac arrest,[2,11] and these complications were seen more frequently in the ST group. A high-risk intubation management protocol which comprises preemptive measures to avoid peri-intubation deterioration have been well described and include minimal sedatives, peri-intubation PPV, and inopressors[11,12] and was successful in preventing peri-intubation complications in the ST+ group.
Moreover, sedatives used for induction and after intubation can worsen hypoperfusion by vasodilation and myocardial depression (benzodiazepines) and by blunting adrenergic-mediated stress response (opioids).[11,12] Ketamine was used preferentially in the ST+ group since it can augment blood pressure and is preferred for emergency induction of patients with acute circulatory instability.[12]
The WHO guidelines stress that control of shock is the most important method to prevent hemorrhagic complications and organ failure in dengue patients,[1] and this was borne out in the ST+ group, where better control of shock may have been responsible for a lower incidence of major hemorrhage and renal failure.
Major hemorrhage can compound plasma leak and lead to much worse shock in dengue, and management dictates a delicate balance between correction of shock and coagulopathy and avoiding FO/massive transfusions; these patients have a high mortality risk.[1,3]
In the ST group, a standard approach was followed in the event of major hemorrhage, and large volumes of blood components were transfused in an attempt to correct deranged hemostasis and reverse shock.
Among the ST+ group, among the nine children with intractable hemorrhage, bleeding was controlled with significantly lower volumes of blood products using a multipronged approach, including hemostatic measures where applicable, preferential use of FWB rather than individual blood components, minimizing components of the lethal triad, and TXA infusion.
Modern transfusion medicine advocates fractionation of whole blood into its components to better accommodate specific blood deficiencies, logistics, and financial reasons.[24]
However, the WHO and CDC advocate FWB as the product of choice in SD with hemorrhagic shock, as FWB can correct hemostatic deficiencies and improve circulation and oxygen delivery with minimal FO[1,2,17] although this may be difficult to procure from modern blood banks.
There is a resurgence of interest in FWB, and trauma and cardiac-surgical literatures report that FWB transfusions are associated with a decreased incidence of hypothermia, acidosis, infections, FO, and organ failure.[13] FWB can reverse dilution coagulopathy, and one single warm unit has hemostatic effect similar to 10 units of platelet concentrates, thus conferring major benefits in terms of avoiding FO.[13]
In addition to coagulopathy, bleeding in SD patients may occur due to activated fibrinolysis.[25] TXA, an antifibrinolytic agent, has been reported in the setting of dengue with bleeding[26] and is also useful in trauma patients to overcome fibrinolysis and improve hemostasis.[14]
The concept of the “lethal triad” consisting of coagulopathy, hypothermia, and acidosis is familiar in major trauma[15] which can also occur in bleeding dengue patients where preexisting coagulopathy is compounded by hypothermia and acidosis, but may be underrecognized.[27]
Hypothermia is a potent anticoagulant and has been reported to further worsen bleeding risk by causing qualitative platelet dysfunction.[28]
With respect to renal replacement, modalities such as PD, CRRT, or hemodialysis may be required in diuretic-resistant FO and AKI.[2,3,6] While CRRT was long considered most suited for hemodynamically unstable ICU patients, there are emerging reports that SLED, a hybrid form of RRT, may be an effective and cheaper option in the critical care setting.[16]
All the three patients in the ST group who received CRRT became hypothermic despite measures to circumvent temperature drop in the extracorporeal circuit. Of note, SLED may be ideally suited to coagulopathic dengue patients with precarious hemodynamics, since SLED, like CRRT, has excellent hemodynamic stability, but in addition has decreased need for anticoagulation and lesser hypothermic risk.[16]
LIMITATIONS
Limitations of our findings include the small numbers, a single-center experience, and the possibility that care process improved over time accounting for the improved results. While we cannot attribute outcomes to any particular therapy, the evidence seems possible that approaches targeted to the underlying pathophysiology may be beneficial and justify their inclusion in future large-scale research endeavors in critically ill dengue patients.
CONCLUSION
The use of the proactive targeted interventions was associated with improved outcomes [Tables 3 and 4] in a sick cohort of SD patients at the highest risk of complications and death.
While both groups received standard ICU supportive therapies in conjunction with standard WHO therapy, the ST+ group received specific interventions that were proactively targeted to the underlying pathophysiology of capillary leak, FO, shock and bleeding, and these may have contributed to improved outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.3rd ed. Geneva: World Health Organization, Special Programme for Research and Training in Tropical Diseases; 2009. World Health Organization, Special Programme for Research and Training in Tropical Diseases. Dengue Hemorrhagic Fever: Diagnosis, Treatment, Prevention and Control. [Google Scholar]
- 2.Geneva: World Health Organization, Special Programme for Research and Training in Tropical Diseases; 2012. [Last accessed on 2016 Oct 30]. World Health Organization, Special Programme for Research and Training in Tropical Diseases. Handbook for Clinical Management of Dengue. Available from: http://www.wpro.who.int/mvp/documents/handbook_for_clinical_management_of_dengue.pdf . [Google Scholar]
- 3.Ranjit S, Kissoon N. Dengue hemorrhagic fever and shock syndromes. Pediatr Crit Care Med. 2011;12:90–100. doi: 10.1097/PCC.0b013e3181e911a7. [DOI] [PubMed] [Google Scholar]
- 4.Anders KL, Nguyet NM, Chau NV, Hung NT, Thuy TT, Lien le B, et al. Epidemiological factors associated with dengue shock syndrome and mortality in hospitalized dengue patients in ho Chi Minh city, Vietnam. Am J Trop Med Hyg. 2011;84:127–34. doi: 10.4269/ajtmh.2011.10-0476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang CC, Liu SF, Liao SC, Lee IK, Liu JW, Lin AS, et al. Acute respiratory failure in adult patients with dengue virus infection. Am J Trop Med Hyg. 2007;77:151–8. [PubMed] [Google Scholar]
- 6.Ranjit S, Kissoon N, Jayakumar I. Aggressive management of dengue shock syndrome may decrease mortality rate: A suggested protocol. Pediatr Crit Care Med. 2005;6:412–9. doi: 10.1097/01.PCC.0000163676.75693.BF. [DOI] [PubMed] [Google Scholar]
- 7.Kamath SR, Ranjit S. Clinical features, complications and atypical manifestations of children with severe forms of dengue hemorrhagic fever in South India. Indian J Pediatr. 2006;73:889–95. doi: 10.1007/BF02859281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centre for Disease Control and Prevention. CDC Dengue Clinical & Laboratory Guidance. [Last accessed on 2016 Oct 30]. Available from: https://www.cdc.gov/dengue/resources/dengue-clinician-guide_508.pdf .
- 9.Ejike JC, Bahjri K, Mathur M. What is the normal intra-abdominal pressure in critically ill children and how should we measure it? Crit Care Med. 2008;36:2157–62. doi: 10.1097/CCM.0b013e31817b8c88. [DOI] [PubMed] [Google Scholar]
- 10.Cam BV, Tuan DT, Fonsmark L, Poulsen A, Tien NM, Tuan HM, et al. Randomized comparison of oxygen mask treatment vs. nasal continuous positive airway pressure in dengue shock syndrome with acute respiratory failure. J Trop Pediatr. 2002;48:335–9. doi: 10.1093/tropej/48.6.335. [DOI] [PubMed] [Google Scholar]
- 11.Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC, et al. The physiologically difficult airway. West J Emerg Med. 2015;16:1109–17. doi: 10.5811/westjem.2015.8.27467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaber S, Jung B, Corne P, Sebbane M, Muller L, Chanques G, et al. An intervention to decrease complications related to endotracheal intubation in the Intensive Care Unit: A prospective, multiple-center study. Intensive Care Med. 2010;36:248–55. doi: 10.1007/s00134-009-1717-8. [DOI] [PubMed] [Google Scholar]
- 13.Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66:S69–76. doi: 10.1097/TA.0b013e31819d85fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunt BJ. The current place of tranexamic acid in the management of bleeding. Anaesthesia. 2015;70(Suppl 1):50–3. doi: 10.1111/anae.12910. e18. [DOI] [PubMed] [Google Scholar]
- 15.De Robertis E, Kozek-Langenecker SA, Tufano R, Romano GM, Piazza O, Zito Marinosci G, et al. Coagulopathy induced by acidosis, hypothermia and hypocalcaemia in severe bleeding. Minerva Anestesiol. 2015;81:65–75. [PubMed] [Google Scholar]
- 16.Schwenger V, Weigand MA, Hoffmann O, Dikow R, Kihm LP, Seckinger J, et al. Sustained low efficiency dialysis using a single-pass batch system in acute kidney injury – A randomized interventional trial: The REnal replacement therapy study in Intensive Care Unit PatiEnts. Crit Care. 2012;16:R140. doi: 10.1186/cc11445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riviello ED, Sugira V, Twagirumugabe T. Sepsis research and the poorest of the poor. Lancet Infect Dis. 2015;15:501–3. doi: 10.1016/S1473-3099(15)70148-9. [DOI] [PubMed] [Google Scholar]
- 18.Dung NM, Day NP, Tam DT, Loan HT, Chau HT, Minh LN, et al. Fluid replacement in dengue shock syndrome: A randomized, double-blind comparison of four intravenous-fluid regimens. Clin Infect Dis. 1999;29:787–94. doi: 10.1086/520435. [DOI] [PubMed] [Google Scholar]
- 19.Saffle JI. The phenomenon of “fluid creep” in acute burn resuscitation. J Burn Care Res. 2007;28:382–95. doi: 10.1097/BCR.0B013E318053D3A1. [DOI] [PubMed] [Google Scholar]
- 20.Lawrence A, Faraklas I, Watkins H, Allen A, Cochran A, Morris S, et al. Colloid administration normalizes resuscitation ratio and ameliorates “fluid creep”. J Burn Care Res. 2010;31:40–7. doi: 10.1097/BCR.0b013e3181cb8c72. [DOI] [PubMed] [Google Scholar]
- 21.Becker BF, Chappell D, Bruegger D, Annecke T, Jacob M. Therapeutic strategies targeting the endothelial glycocalyx: Acute deficits, but great potential. Cardiovasc Res. 2010;87:300–10. doi: 10.1093/cvr/cvq137. [DOI] [PubMed] [Google Scholar]
- 22.Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, et al. Acomparison of albumin and saline for fluid resuscitation in the Intensive Care Unit. N Engl J Med. 2004;350:2247–56. doi: 10.1056/NEJMoa040232. [DOI] [PubMed] [Google Scholar]
- 23.Gala HC, Avasthi BS, Lokeshwar MR. Dengue shock syndrome with two atypical complications. Indian J Pediatr. 2012;79:386–8. doi: 10.1007/s12098-011-0551-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murdock AD, Berséus O, Hervig T, Strandenes G, Lunde TH. Whole blood: The future of traumatic hemorrhagic shock resuscitation. Shock. 2014;41(Suppl 1):62–9. doi: 10.1097/SHK.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 25.Huang YH, Liu CC, Wang ST, Lei HY, Liu HL, Lin YS, et al. Activation of coagulation and fibrinolysis during dengue virus infection. J Med Virol. 2001;63:247–51. doi: 10.1002/1096-9071(200103)63:3<247::aid-jmv1008>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 26.Gan VC. Dengue: Moving from current standard of care to state-of-the-art treatment. Curr Treat Options Infect Dis. 2014;6:208–26. doi: 10.1007/s40506-014-0025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chuansumrit A, Chaiyaratana W. Hemostatic derangement in dengue hemorrhagic fever. Thromb Res. 2014;133:10–6. doi: 10.1016/j.thromres.2013.09.028. [DOI] [PubMed] [Google Scholar]
- 28.Lee IK, Liu JW, Yang KD. Fatal dengue hemorrhagic fever in adults: Emphasizing the evolutionary pre-fatal clinical and laboratory manifestations. PLoS Negl Trop Dis. 2012;6:e1532. doi: 10.1371/journal.pntd.0001532. [DOI] [PMC free article] [PubMed] [Google Scholar]