Abstract
The purpose of this review was to better understand how to market the Chronic Disease Self-Management Program to new audiences. Eight databases were searched for peer-reviewed studies of the CDSMP. 39 articles were analyzed to describe the theoretical basis of recruitment strategies and their effectiveness while engaging diverse populations. Findings included that female, Caucasian, and elderly groups are overrepresented in CDSMP literature and recruitment efforts have not been explicitly grounded in theory. This review provides insight into trends in CDSMP recruitment and identifies the need for further research regarding the application of marketing theory to future enrollment efforts.
Keywords: self-management, chronic disease, adult
Over the past decade, morbidity and mortality from chronic disease has increased dramatically in adults under the age of 65. Chronic disease-related morbidity – such as the associated symptom burden and limitations of daily functioning – contribute to higher health care costs, work productivity losses, and decreases in quality of life (National Center for Chronic Disease Prevention and Health Promotion, 2015). In terms of mortality, approximately 38 million people die from chronic disease each year, 16 million (42%) of whom are under 70 years old (World Health Organization, 2015). Given the vast majority of chronic disease morbidity and mortality is preventable with effective self-management, these burdens can be mitigated by extending effective, evidence-based education programs to all adults with chronic disease.
In 1996, the Chronic Disease Self-Management Program (CDSMP) was developed, which has been shown to be a cost-effective solution for helping people successfully manage their chronic conditions (Stanford School of Medicine, 2015). A recent meta-analysis revealed that CDSMP participants experienced significant improvements in self-efficacy, health distress, social limitations, and cognitive symptoms (Brady et al, 2011). Health officials are now working harder than ever to disseminate this evidence-based intervention to populations that have traditionally had less participation in the CDSMP, such as working adults of diverse socioeconomic backgrounds under age 65 (Brady et al, 2011; Franek, 2013). As researchers attempt to extend the CDSMP to a broader audience, understanding the marketing-related factors that have influenced CDSMP participation is critical. While studies routinely describe the recruitment efforts used to engage populations in CDSMP efficacy and effectiveness studies, no review has been conducted to synthesize this information or examine the role marketing plays in eliciting program participation.
Therefore, the purpose of this review is to describe the CDSMP recruitment efforts since the program was developed in 1996. This article describes what recruitment strategies have been: (1) rooted in theoretical principles, (2) most effective within and across geographic and cultural contexts, and (3) successful in reaching lower-SES populations. We also examine what barriers and facilitators have been reported in relation to prior recruitment attempts. The results can help guide researchers trying to market the program to wider populations with high chronic disease morbidity burden.
Methods
We implemented a scoping methodology to conduct this review, which is gaining recognition for synthesizing research evidence (Pham et al., 2014). Where the goal of a systematic review is often to reach a conclusion about the level, or strength of evidence available on a particular topic (Pham et al., 2014), scoping reviews are broader in purpose, and are undertaken to “examine the extent, range, and nature of research activity in a topic area” (p.371). Given the goal here is to broadly determine the populations that CDSMP marketing efforts have targeted, whether these efforts have been informed by theory, and whether they have been successful, a scoping review approach is logically consistent with these aims.
Pub-Med, CINAHL, Web of Science, Cochrane Library, PsychInfo, Embase, ABI/Inform, and Science Direct databases were searched for peer-reviewed reports of CDSMP research published between January 1996 and February 2015. The following search string was used (“Chronic Disease Self-Management Program” OR “CDSMP”) AND (recruit* OR market*). Studies met inclusion criteria if they involved the recruitment of participants to the CDSMP or a program derivative of the CDSMP. Program derivatives included CDSMP courses that were redesigned for a specific disease group, such as stroke or pain self-management courses, or those which were adapted for implementation in another country, such as the Expert Patients Program (EPP) (Goldfinger et al, 2012; Kennedy et al, 2007). Studies were excluded if they were literature reviews or were presented in a language other than English. When multiple articles reported findings from the same study, the article with more descriptive recruitment processes was included.
Three hundred and thirty seven articles were identified in the initial search. An independent reviewer screened the titles and abstracts according to the inclusion and exclusion criteria (see Figure 1), and those articles meeting criteria were retained for full text review. A table was developed to extract data from each article regarding recruitment methods, barriers to recruitment, sample size, representativeness of the sample, enrollment rates, and marketing-related theory. Data were then reviewed to provide an overview of the most common and effective recruitment strategies used to enroll participants in CDSMP studies, the most frequently represented demographics in the research, and the theoretical basis of recruitment efforts.
Figure 1.
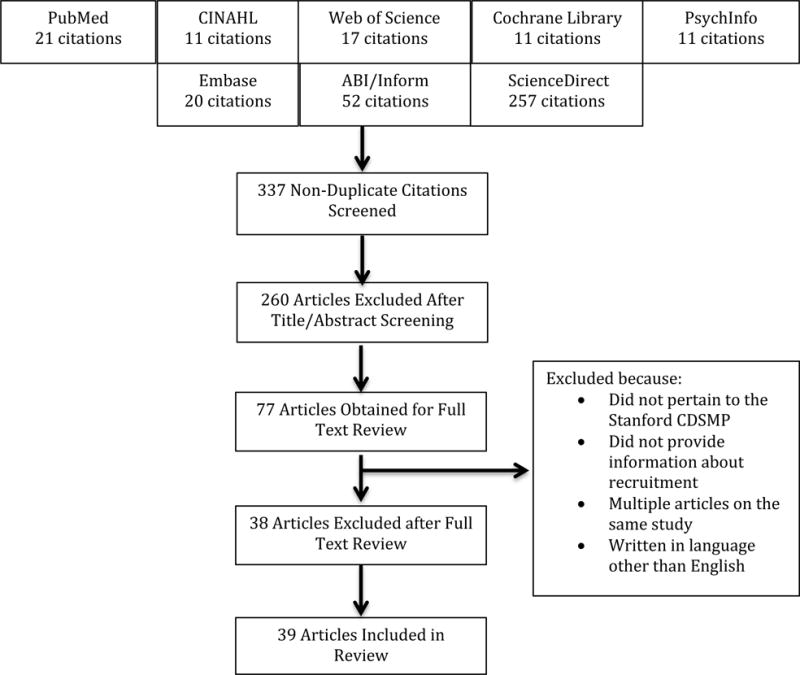
PRISMA Diagram
Findings
Theories Reported to Support Recruitment Efforts
A primary finding is that, of the 39 articles included, none presented information about the use of theory to guide recruitment efforts. While several authors discussed implementing recruitment approaches that may be supported by theory, none were specifically cited. For example, authors commonly reported establishing community partners who related well to their target populations, which is a practice supported by the Diffusion of Innovations Theory (DIT); however, DIT was not explicitly identified in guiding their recruitment efforts. According to DIT, people evaluate a new idea or program based on the descriptions of their peers (Rogers, 2003). There are also other aspects of the theory that may further inform recruitment efforts. These include how the individuals being recruited may be weighing key attributes of the CDSMP, such as relative advantage, complexity, compatibility, trialability, and observability, as outlined in the persuasion phase of the DIT (Rogers, 2003). Thus, finding spokespersons that can relate to the population of interest is a theory-driven practice, yet no author reported it as such. Moreover, recruitment efforts that are not theory-driven can overlook potentially relevant details in the design and/or distribution of recruitment materials that could be used to persuade the target population. Due to this gap in the literature, it is currently unknown whether the use of one theoretical perspective over another could facilitate participation in studies of the CDSMP or in CDSMP programs being offered in local communities.
Study Sample Characteristics
Of the 39 articles included, studies were conducted in countries across the globe, targeting various ethnic minority groups within each country. While only two studies reported struggling to recruit participants from minority populations, 13 of the 39 articles, all from the US, Canada or England, reported a sample composed of over 50% non-Hispanic white participants. Researchers discussed the over-representation of women in their study in only six articles, yet 26 of the 35 studies that reported gender had a sample of over 60% females. While one study in Hong Kong included a sample with nearly 50% of participants under the age of 45, the average age represented in each study ranged from 48 – 77.2 years (Chan, Siu, Poon & Chan, 2005). No additional information regarding whether the generally younger group studied in Hong Kong was recruited by tailoring the recruitment materials and/or the dissemination of study information to this population. A full overview of sample characteristics of each study is listed in Table 1.
Table 1.
Study Demographics
| Study | Setting | Majority Ethnic Group | Majority Gender | Design | |
|---|---|---|---|---|---|
| 1 | Barlow et al., (2009) | NS | Caucasian | Female | RCT |
| 2 | Bazargani et al., (2011) | Iraq | NS | Male | RCT |
| 3 | Cadilhac et al., (2011) | Australia | NS | Female | RCT |
| 4 | Cameron-Tucker et al. (2014) | Australia | NS | Male | RCT |
| 5 | Catalano et al. (2003) | Australia | NS | Male | RCT |
| 6 | Chan et al. (2005) | Hong Kong | NS | Female | Quasi-experimental |
| 7 | Chan et al., (2010) | Hong Kong | NS | Female | Quasi-experimental |
| 8 | Chang et al. (2008) | Australia | NS | NS | RCT |
| 9 | Chouinard et al. (2013) | Canada | NS | NS | Multiple Case Study RCT |
| 10 | Detaille et al., (2013) | Netherlands | NS | Female | RCT |
| 11 | Druss et al., (2010) | USA | African-American | Female | RCT |
| 12 | Elzen et al., (2007) | Netherlands | NS | Female | RCT |
| 13 | Farrell et al., (2004) | USA | Caucasian | Female | Quasi-experimental |
| 14 | Franks et al., (2009) | USA | Caucasian | Female | RCT |
| 15 | Fu Dongbo et al., (2003) | China | Han | Female | RCT |
| 16 | Gitlin et al., (2008) | USA | African-American | Female | RCT |
| 17 | Goldfinger et al., (2012) | USA | African-American | Female | RCT |
| 18 | Goto, (2013) | USA | Caucasian | Female | Quasi-experimental |
| 19 | Griffiths et al., (2005) | England | Bangladeshi | Female | RCT |
| 20 | Groupp et al., (2005) | USA | Caucasian | Female | RCT |
| 21 | Horowitz et al., (2009) | USA | Latino | Female | Comparative |
| 22 | Jerant et al., (2009) | USA | Caucasian | Female | RCT |
| 23 | Kennedy et al., (2007) | England | Caucasian | Female | RCT |
| 24 | Lorig et al., (2005) | USA | Caucasian | Female | RCT |
| 25 | Lorig et al., (2006). | USA | Caucasian | Female | RCT |
| 26 | Lorig et al., (2001). | USA | Caucasian | Female | RCT |
| 27 | Lorig, et al., (1999). | USA | Caucasian | Female | RCT |
| 28 | Lorig et al., (2014) | USA | Caucasian | Female | Translational |
| 29 | McGillion et al., (2008) | Canada | Caucasian | Male | RCT |
| 30 | Murphy et al., (2003) | Australia | NS | NS | NS |
| 31 | Siu et al., (2007) | Hong Kong | NS | Female | Quasi-experimental |
| 32 | Smeulders et al., (2009) | Netherlands | NS | Male | RCT |
| 33 | Smeulders et al., (2007) | Netherlands | NS | Male | One group pre-test/post-test |
| 34 | Swerissen et al., (2006) | Australia | Greek, Italian, Vietnamese, Chinese | Female | RCT |
| 35 | Tomioka et al., (2012) | USA | Native Hawaiian, Filipino, Caucasian, Japanese, Pacific Islander | Female | One group pre-test/post-test |
| 36 | Tomioka et al., (2014) | USA | Filipino | Female | One group pre-test/post-test |
| 37 | Walker et al., (2005) | Australia | Greek, Italian, Vietnamese, Chinese | Gender balanced | Focus Groups |
| 38 | Wang et al., (2014) | USA | Chinese | NS | Practical-Participatory Evaluation |
| 39 | Yip et al., (2007) | Hong Kong | Chinese | Female | Experimental |
Recruitment Strategies
Table 2 displays the frequency with which each recruitment strategy was utilized both around the world and specifically within the US, and Table 3 lists the strategies used in each study reviewed. Eleven of 39 studies were conducted in the US, while 8 were set in Australia, 4 in the Netherlands, 4 in Hong Kong, 2 in Canada, 2 in England, 1 in China and 1 in Iraq. Strategies within the US are presented in Table 2 to highlight differences in recruitment practices between this country, where many faced limited access to healthcare during the years under review, and other countries, where access to care may have been more available. Nearly all recruitment strategies were utilized with greater frequency in the US, yet the US also had a higher percentage of studies that did not meet recruitment goals (27%) compared to other countries. Particularly notable is the frequency with which researchers in the US used local media, posted materials in public spaces, and partnered with community professionals, compared to those in other countries where a health care provider recommendation was implemented most often. While the US did not recruit in the clinical setting any less frequently than other countries, US researchers supplemented clinical recruitment techniques with community-based approaches more frequently than researchers in other countries.
Table 2.
Recruitment Strategy Frequency
| Recruitment Strategy | Global Frequency | U.S. Frequency |
|---|---|---|
| Clinical Setting | ||
| Provider recommendation | 41% | 55% |
| Flyers/brochures in clinic setting | 27% | 55% |
| Direct contact with potential participants (letters, phone calls, etc.) | 18% | 36% |
| Medical records used to identify participants | 10% | 18% |
| Community Setting | ||
| Local media | 36% | 55% |
| Partnered with trusted professionals in the community | 26% | 55% |
| Flyers/posters/brochures in community setting | 25% | 55% |
| Advertised in patient organizations (listserv, database, magazine, etc.) | 21% | 27% |
| Newsletters | 18% | 36% |
| Promotion booths | 18% | 27% |
| Word-of-mouth | 13% | 27% |
| Presentations | 10% | 27% |
| Direct phone calls | 5% | 0% |
| Recruitment events | 5% | 18% |
| Internet advertisement | 3% | 1% |
Table 3.
Study Recruitment Data
| Study | *Strategy | Goal | % Goal Reached | Potential Participants | % Invited that Enrolled | Sample Size |
|---|---|---|---|---|---|---|
| 1 | 5, 8, 13, 15 | NS | NS | NS | NS | 216 |
| 2 | 2 | NS | NS | NS | NS | 300 |
| 3 | 5, 9, 13 | 150 | 95% | 2112 | 7% | 143 |
| 4 | 1 | 78 | 108% | 316 | 27% | 84 |
| 5 | 3 | NS | NS | 37 | 100% | 37 |
| 6 | 2 | NS | NS | NS | NS | 23 |
| 7 | 1, 6 7, 9, 10 | NS | NS | 772 | 100% | 772 |
| 8 | 5, 13 | 318 | NS | NS | NS | NS |
| 9 | 1, 4 | 400 | NS | NS | NS | NS |
| 10 | 1, 5, 6 | 84 | 94% | 109 | 72% | 79 |
| 11 | 2 | NS | NS | 137 | 58% | 80 |
| 12 | 2, 5, 8 | 200 | 72% | 411 | 35% | 144 |
| 13 | 1 | 100 | 48% | 100 | 48% | 48 |
| 14 | 1, 2, 3, 4 | NS | NS | 782 | 53% | 415 |
| 15 | 2, 5, 7, 11 | 962 | 99% | 954 | 100% | 954 |
| 16 | 5, 9, 11, 12 | NS | NS | 569 | 73% | 414 |
| 17 | 1, 3, 6, 7 | 600 | 97% | NS | NS | 582 |
| 18 | 1, 6 | 80 | 105% | 298 | 28% | 84 |
| 19 | 3, 4, 5, 11 | 216 | 220% | 1363 | 35% | 476 |
| 20 | 2, 5, 6, 7, 8, 9, 10, 12 | 100 White 100 African-American | 55% | NS | NS | 109 |
| 21 | 1, 5, 7, 8, 14 | NS | NS | 555 | 18% | 99 |
| 22 | 2, 3 | 360 | 115% | 782 | 53% | 415 |
| 23 | 1, 5, 13, 15 | 600 | 105% | 1260 | 50% | 629 |
| 24 | 5, 8, 12 | NS | NS | 437 | 81% | 355 |
| 25 | 15 | NS | NS | 1952 | 49% | 958 |
| 26 | 1, 2, 3, 4 | NS | NS | 703 | 70% | 489 |
| 27 | 2, 5, 6, 7, 9 | NS | NS | 1140 | 84% | 952 |
| 28 | 6 | NS | NS | 199 | 70% | 139 |
| 29 | 1, 2, 5, 9 | 104 | 113% | 277 | 42% | 117 |
| 30 | 1, 2, 5, 6, 8 10, 13, 15 | NS | NS | NS | NS | 52 |
| 31 | 1 | 160 | 93% | NS | NS | 148 |
| 32 | 3 | 360 | 88% | 717 | 44% | 317 |
| 33 | 3 | NS | NS | 63 | 16% | 10 |
| 34 | 1, 2, 5, 9, 10, 12 | NS | NS | 728 | 65% | 474 |
| 35 | 5, 6, 9, 10, 11 | NS | NS | NS | NS | 492 |
| 36 | 7, 10, 11 | NS | NS | NS | NS | 96 |
| 37 | 1, 6 | NS | NS | NS | NS | NS |
| 38 | 7, 14 | NS | NS | NS | NS | 18 |
| 39 | 2 | NS | NS | NS | NS | 120 |
Strategies
1 = Provider recommendation; 2 = Flyers/brochures in clinic setting; 3 = Direct contact with potential participants (letters, phone calls, etc.); 4 = Medical records used to identify participants; 5 = Local media; 6 = Partnered with trusted professionals in the community; 7 = Flyers/posters/brochures in community setting; 8 = Advertised in patient organizations (listserv, database, magazine, etc.); 9 = Newsletters; 10 = Promotion booths; 11 = Word-of-mouth; 12 = Presentations; 13 = Direct phone calls; 14 = Recruitment events; 15 = Internet advertisement
As noted in Table 2, the most commonly implemented method of recruitment globally was provider recommendation, with 16 (41%) of the studies enlisting the help of care providers. Fifteen of these studies asked healthcare providers to approach patients directly, while one study had providers send letters to patients recommending study participation. Researchers used clinical sites in other ways as well, with four identifying potential participants through medical records and 10 leaving fliers and promotional materials in clinic waiting rooms. Though clinically based recruitment efforts may be effective when targeting elderly patients who likely have greater access to care, it may be ineffective when trying to reach working adults of lower-SES status who may not have time or money available for primary care services. While noting differences in recruitment practices between countries sheds some light on recruitment efforts and successes through the health care system, the remainder of the findings generally focus on those used in the US, where there is significant interest in extending the CDSMP to a broader population in an attempt to ameliorate the high rate of chronic disease morbidity.
Thirteen of the 39 (33%) studies recruited participants within the clinical setting, while 10 enrolled only volunteer participants from the community, and 16 recruited participants in both settings. While recruiting within the community, nine studies left flyers and brochures with study information in a community center, seven set-up promotional booths at community events, and six reported using ‘interpersonal persuasion’ or ‘word-of-mouth’ to entice participants to join the study. Just as recruiters turned to care providers for support during clinical recruitment efforts, ten studies turned to trusted non-healthcare professionals within the community to guide recruitment and communicate the value of CDSMP and study participation.
Recruitment Effectiveness
Twenty-five studies reported either the number of participants approached during recruitment or the number of volunteers who expressed interest, but only ten of these studies successfully enrolled over 60% of potential participants. With this said, recruitment effectiveness frequently was not quantified, and only 17 of the articles stated goals for study enrollment. Of these, only four failed to meet enrollment goals, and only two enrolled fewer than 70% of their target. Reasons for failing to meet recruitment goals included difficulty recruiting in rural areas, time constraints, and cultural barriers. Cultural barriers included a mistrust of unfamiliar research encountered amongst both African American and Chinese communities within the US (Wang et al., 2014; Groupp, Haas, Fairwether, Ganger & Attwood, 2005). Recruitment methods in these studies did not vary from the methods used in successful enrollment efforts, however, special attempts made to reach both the Chinese and African American populations were unsuccessful. Such attempts included holding orientations and introductory sessions to the CDSMP within the Chinese community and seeking the support of community members that were particularly relevant within the African American population, such as an African-American chiropractor, clergy members, and the National Association for the Advancement of Colored People (Wang et al., 2014; Groupp, Haas, Fairwether, Ganger & Attwood, 2005).
Data were extracted from five of the studies regarding the efficacy of recruitment methods within specific populations. One U.S. study targeted a Chinese population, first with impersonal recruitment such as flier distribution, and then through personal interactions, such as introduction sessions. No recruitment goal was set in this study, and no results were given regarding the percent of the available population enrolled, but the researchers recruited only 18 participants over an 8-month period (Wang et al., 2014). Researchers in another U.S. study successfully recruited Filipino participants. Again, no recruitment goals were set and no results were provided regarding the reach of the program, but 91.7% of the 96- person sample was Filipino (Tomioka, Braun, Ah Cook, Compton & Wertin, 2014). Though only 15 studies offered information regarding the representativeness of the sample and the generalizability of results, females and the elderly were frequently cited as being overrepresented in the study sample.
Barriers to Participation
To explain the variation between key demographics in the target populations and study samples, researchers outlined a variety of pragmatic, or resource-driven barriers that inhibited study enrollment. With this said, it was not clear from the information provided in the articles whether those who were not interested were averted more to participating in a research study or to the CDSMP. Barriers broadly included transportation (n=5 studies), particularly in rural counties, and the time commitment required and/or scheduling difficulties to complete the CDSMP (n=six). One of these studies reported that information about the availability of the program was communicated through pamphlets. The other studies, however, did not indicate how the locations and times were communicated in study-related materials or communication.
Cultural barriers to recruitment were also noted in three studies. In one study, Chinese participants wanted to know the researchers running the study prior to enrollment. In another, Bangladeshi participants failed to see the value of the CDSMP due to cultural beliefs around predetermination. In yet another study, authors discussed the historically embedded mistrust of researchers they encountered while trying to recruit African-American participants. Four authors also explained that physical complications kept many prospective participants from enrolling in their study. Finally, researchers in five studies noted prospective participants that simply were not interested in joining the study. Two of these studies recorded the number of uninterested recruits at 10-20% of possible participants; yet, there was no explanation of why people were not interested, and whether there were marketing strategies that promoted or deterred participation.
Review Limitations
There are limitations of this review. First, as is inherent in most reviews, publication bias could skew results. None of the studies included were generalizable to the population at-large, as all either utilized a volunteer sample or reported issues with generalizability. Because only one researcher coded the information, there is also chance for rater drift to skew results. Nine databases were searched and systematic coding procedures were followed in an effort to address and reduce these methodological limitations that can occur when conducting a literature review.
Discussion
In this scoping review, none of the 39 articles analyzed reported applying an explicit theoretical perspective to guide their recruitment efforts. While this may indicate that researchers are truly implementing atheoretical approaches during recruitment, it simply may not be current practice to report such theories within peer-reviewed publications. If the former is true, future research should be conducted to test whether the application of marketing theory – which incorporates both cognitive and behavioral dimensions – may be implemented to enhance recruitment (French, Blair-Stevens, McVey & Merritt, 2010). For example, researchers might apply the Diffusion of Innovations Theory (DIT) to target early recruitment efforts towards leaders within the community, who may, in turn, influence others to join the study (French et al., 2010).
Utilizing a DIT approach builds on the concepts of innovators and early adopters, who are the first to adopt an innovation and who influence members of their social circle to do the same (French et al., 2010). Innovators and early adopters are most influential when they reflect the target population, meaning they share similar background characteristics (Rogers, 1995). Applying these principles to establish partnerships with influential community members may help reach audiences who are skeptical of research, such as the Chinese and African-American samples mentioned in this review (Wang et al., 2014; Groupp et al., 2005). Many of the issues experienced while trying to reach such populations are rooted in a history of mistrust in researchers and the research process itself; thus, it is unclear whether professionals would experience similar difficulties while trying to enroll participants in a non-study related CDSMP course. The answer to this inquiry could have important effects on the promotion of the CDSMP in both research and non-research contexts, and should be further investigated.
Researchers and others responsible for marketing the CDSMP may build upon other constructs embedded throughout communication theories as well, such as perceived vulnerability, severity, response efficacy and self-efficacy (French et al., 2010). Implementing these concepts during recruitment would involve disseminating materials that maximize people’s perceived vulnerability and severity of their illness, perceived efficacy of the program to improve disease symptoms, and perceived self-efficacy to complete the program. Such efforts may be utilized to reach members of cultural groups who believe in predetermination, such as the Bangladeshi participants featured in one article (Griffiths et al., 2005). Building on additional theories, researchers could manipulate the color, graphics, and messages of advertisements to enhance recruitment. For example, specific forms of message framing can be applied to encourage health promotion activity (Gallagher & Updergraff, 2012).
The concept of “framing” advertisement content refers to whether you present the benefits of partaking in health promotion (a gain-framed message), the dangers of not partaking in the health behavior (a loss-framed message), or both (mixed-frame) (Gallagher & Updergraff, 2012; Gainforth, Cao, Latimer-Cheung, 2012). According to Gallagher & Updergraff (2012), gain-framed messaging is the most effective technique when trying to encourage health promotion behaviors. Implementing this concept may help recruit participants who previously allowed barriers such as busy schedules, transportation and disease acuity prevent them from enrolling in the CDSMP. The 4 P’s of marketing; product, price, place and promotion, may also be implemented to enhance the recruitment of isolated populations (Lee & Kotler, 2011). Under these principles, advertisements must make the product (the CDSMP) appear effective, the price affordable (generally CDSMP courses have no monetary cost, but require an investment of time and energy), the place accessible (holding the CDSMP near bus routes), and the promotion effective (using newspaper advertisements to reach the homebound). Though these are a few examples of applicable marketing principles, there are a number of theories that can be applied to improve recruitment efforts of future investigators. Future research should test each theory for effectiveness when applied to recruitment, particularly when targeting underserved populations.
Despite the sweeping efforts of researchers to increase enrollment, several populations were underrepresented in the samples reviewed for this study. As noted above, rural, male, and African-American populations were grossly underrepresented in most samples. Furthermore, Hispanic Latinos made up over 50% of the sample in only one study (Horowitz et al., 2009). The average age of recruited participants was also below 55 in only seven of the study samples. Thus, further research should be conducted to discover recruitment methods that can be used to attract these underrepresented groups. One strategy currently untapped in the CDSMP literature is social media recruitment, which may be an area in need of further research while trying to engage diverse, difficult-to-reach populations. Continued efforts should be made to understand what media, information sources, and messages attract participants of various backgrounds to the CDSMP. These studies should occur not only to enhance study enrollment rates, but also to recruit people to CDSMP programs that are not affiliated with a research team. As chronic illnesses continue to spread to the most vulnerable populations of society, public health officials must continue to adapt to reach and serve those most burdened by chronic disease morbidity.
References
- Barlow J, Turner A, Edwards R, Gilchrist M. A randomised controlled trial of lay-led self-management for people with multiple sclerosis. Patient Education and Counseling. 2009;77(1):81–89. doi: 10.1016/j.pec.2009.02.009. http://dx.doi.org/10.1016/j.pec.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Bazargani RH, Besharat MA, Hadi, Ehsan B, Nejatian M, Hosseini K. The efficacy of chronic disease self-management program and tele- health on adherence by increasing self efficacy in patients with CABG. Procedia - Social and Behavioral Sciences. 2011;30(0):817–821. http://dx.doi.org/10.1016/j.sbspro.2011.10.158. [Google Scholar]
- Brady TJ, Murphy L, Beauchesne D, Bhalakia A, Chervin D, Daniels B, O’Colmain B. Sorting through the evidence for the arthritis self-management program and the chronic disease self-management program: Executive summary of ASMP/CDSMP meta-analyses. Centers for Disease Control and Prevention; 2011. Retrieved from http://www.cdc.gov/arthritis/docs/ASMP-executive-summary.pdf. [Google Scholar]
- Cadilhac DA, Hoffmann S, Kilkenny M, Lindley R, Lalor E, Osborne RH, Batterbsy M. A phase II multicentered, single-blind, randomized, controlled trial of the stroke self-management program. Stroke; a Journal of Cerebral Circulation. 2011;42(6):1673–1679. doi: 10.1161/STROKEAHA.110.601997. [DOI] [PubMed] [Google Scholar]
- Cameron-Tucker HL, Wood-Baker R, Owen C, Joseph L, Walters EH. Chronic disease self-management and exercise in COPD as pulmonary rehabilitation: A randomized controlled trial. International Journal of Chronic Obstructive Pulmonary Disease. 2014;9:513–523. doi: 10.2147/COPD.S58478. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano T, Dickson P, Kendall E, Kuipers P, Posner TN. The perceived benefits of the chronic disease self-management program among participants with stroke: A qualitative study. Australian Journal of Primary Health. 2003;9(2–3):80–89. Retrieved from https://www.researchgate.net/publication/29457468. [Google Scholar]
- Chan SC, Siu AM, Poon PK, Chan CC. Chronic disease self-management program for Chinese patients: A preliminary multi-baseline study. International Journal of Rehabilitation Research Internationale Zeitschrift Fur Rehabilitationsforschung Revue Internationale De Recherches De Readaptation. 2005;28(4):351–354. doi: 10.1097/00004356-200512000-00008. doi:00004356-200512000-00008 [pii] [DOI] [PubMed] [Google Scholar]
- Chan WL, Hui E, Chan C, Cheung D, Wong S, Wong R, Woo J. Evaluation of chronic disease self-management programme (CDSMP) for older adults in Hong Kong. The journal of nutrition, health & aging. 2011;15(3):209–214. doi: 10.1007/s12603-010-0257-9. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21369669. [DOI] [PubMed] [Google Scholar]
- Chang AT, Haines T, Jackson C, Yang I, Nitz J, Low Choy N, Vicenzino B. Rationale and design of the PRSM study: Pulmonary rehabilitation or self management for chronic obstructive pulmonary disease (COPD), what is the best approach? Contemporary Clinical Trials. 2008;29(5):796–800. doi: 10.1016/j.cct.2008.04.004. http://dx.doi.org/10.1016/j.cct.2008.04.004. [DOI] [PubMed] [Google Scholar]
- Chouinard M, Hudon C, Dubois M, Roberge P, Loignon C, Tchouaket E, Sasseville M. Case management and self-management support for frequent users with chronic disease in primary care: A pragmatic randomized controlled trial. Bmc Health Services Research. 2013;13:49. doi: 10.1186/1472-6963-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detaille SI, Heerkens YF, Engels JA, van der Gulden JWJ, van Dijk FJH. Effect evaluation of a self-management program for Dutch workers with a chronic somatic disease: A randomized controlled trial. Journal of Occupational Rehabilitation. 2013;23(2):189–99. doi: 10.1007/s10926-013-9450-0. http://dx.doi.org/10.1007/s10926-013-9450-0. [DOI] [PubMed] [Google Scholar]
- Druss BG, Zhao L, von Esenwein SA, Bona JR, Fricks L, Jenkins-Tucker S, Lorig K. The health and recovery peer (HARP) program: A peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophrenia Research. 2010;118(1–3):264–270. doi: 10.1016/j.schres.2010.01.026. http://dx.doi.org/10.1016/j.schres.2010.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elzen H, Slaets JPJ, Snijders TAB, Steverink N. Evaluation of the chronic disease self-management program (CDSMP) among chronically ill older people in the Netherlands. Social Science & Medicine. 2007;64(9):1832–1841. doi: 10.1016/j.socscimed.2007.02.008. http://dx.doi.org/10.1016/j.socscimed.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Farrell K, Wicks MN, Martin JC. Chronic disease self-management improved with enhanced self-efficacy. Clinical Nursing Research. 2004;13(4):289–308. doi: 10.1177/1054773804267878. [doi] [DOI] [PubMed] [Google Scholar]
- Franek J. Self-management support interventions for persons with chronic disease: An evidence-based analysis. Ontario Health Technology Assessment Series. 2013;13(9):1–60. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24194800. [PMC free article] [PubMed] [Google Scholar]
- Franks P, Chapman B, Duberstein P, Jerant A. Five factor model personality factors moderated the effects of an intervention to enhance chronic disease management self-efficacy. British Journal of Health Psychology. 2009;14:473–487. doi: 10.1348/135910708X360700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French J, Blair-Stevens C, McVey D, Merritt R. Social marketing and public health: Theory and practice. Oxford: Oxford University Press; 2010. [DOI] [Google Scholar]
- Dongbo Fu, Fu H, McGowan P, Yi-e S, et al. Implementation and quantitative evaluation of chronic disease self-management programme in shanghai, china: Randomized controlled trial. World Health Organization. Bulletin of the World Health Organization. 2003;81(3):174–82. Retrieved from http://search.proquest.com/docview/229548253?accountid=14244. [PMC free article] [PubMed] [Google Scholar]
- Gainforth HL, Cao W, Latimer-Cheung AE. Message framing and parents’ intentions to have their children vaccinated against HPV. Public Health Nursing (Boston, Mass) 2012;29(6):542–552. doi: 10.1111/j.1525-1446.2012.01038.x. [doi] [DOI] [PubMed] [Google Scholar]
- Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: A meta-analytic review. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2012;43(1):101–116. doi: 10.1007/s12160-011-9308-7. [doi] [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Chernett NL, Harris LF, Palmer D, Hopkins P, Dennis MP. Harvest health: Translation of the chronic disease self-management program for older African Americans in a senior setting. The Gerontologist. 2008;48(5):698–705. doi: 10.1093/geront/48.5.698. doi:48/5/698 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfinger JZ, Kronish IM, Fei K, Graciani A, Rosenfeld P, Lorig K, Horowitz CR. Peer education for secondary stroke prevention in inner-city minorities: Design and methods of the prevent recurrence of all inner-city strokes through education randomized controlled trial. Contemporary Clinical Trials. 2012;33(5):1065–1073. doi: 10.1016/j.cct.2012.06.003. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto LS. A quasi-experimental study examining the impact of physician support on sustaining patient self-management. 2013 (2013-99060-352). Retrieved from http://gradworks.umi.com/35/10/3510602.html.
- Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, Barlow J. Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. The British Journal of General Practice: The Journal of the Royal College of General Practitioners. 2005;55(520):831–837. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1570787/ [PMC free article] [PubMed] [Google Scholar]
- Groupp, E. Haas M, Fairweather A, Ganger B, Attwood M. Recruiting seniors with chronic low back pain for a randomized controlled trial of a self-management program. Journal of Manipulative and Physiological Therapeutics. 2005;28(2):97–102. doi: 10.1016/j.jmpt.2005.01.004. doi:S0161475405000059 [pii] [DOI] [PubMed] [Google Scholar]
- Horowitz CR, Brenner BL, Lachapelle S, Amara DA, Arniella G. Effective recruitment of minority populations through community-led strategies. American Journal of Preventive Medicine. 2009;37(6, Supplement 1):S195–S200. doi: 10.1016/j.amepre.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant A, Moore-Hill M, Franks P. Home-based, peer-led chronic illness self-management training: Findings from a 1-year randomized controlled trial. Annals of Family Medicine. 2009;7(4):319–327. doi: 10.1370/afm.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy A, Reeves D, Bower P, Lee V, Middleton E, Richardson G, Rogers A. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: A pragmatic randomised controlled trial. Journal of Epidemiology and Community Health. 2007;61(3):254–261. doi: 10.1136/jech.2006.053538. 61/3/254 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee NR, Kotler PA. Social Marketing: Influencing Behaviors for Good. Fourth. Thousand Oaks, CA: SAGE Publications; 2011. [Google Scholar]
- Lorig K, Ritter PL, Plant K. A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthritis and Rheumatism. 2005;53(6):950–957. doi: 10.1002/art.21604. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, Laurent DD, Plant K. Internet-based chronic disease self-management: A randomized trial. Medical Care. 2006;44(11):964–971. doi: 10.1097/01.mlr.0000233678.80203.c1. Retrieved from https://auth.lib.unc.edu/ezproxy_auth.php?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2009337132&site=ehost-live&scope=site. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice : ECP. 2001;4(6):256–262. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11769298. [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BJ, Bandura A, Ritter P, Holman HR. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10413387. [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Pifer C, Werner P. Effectiveness of the chronic disease self-management program for persons with a serious mental illness: A translation study. Community Mental Health Journal. 2014;50(1):96–103. doi: 10.1007/s10597-013-9615-5. http://dx.doi.org/10.1007/s10597-013-9615-5. [DOI] [PubMed] [Google Scholar]
- McGillion MH, Watt-Watson J, Stevens B, LeFort SM, Coyte P, Graham A. Randomized controlled trial of a psychoeducation program for the self-management of chronic cardiac pain. Journal of Pain and Symptom Management. 2008;36(2):126–140. doi: 10.1016/j.jpainsymman.2007.09.015. http://dx.doi.org/10.1016/j.jpainsymman.2007.09.015. [DOI] [PubMed] [Google Scholar]
- Murphy M, Saunders JE, Campbell M, Jackson B, Berlowitz D. The process of implementing the Stanford model chronic disease self-management program: The northern hospital experience. Australian Journal of Primary Health. 2003;9(2–3):127–131. Retrieved from https://www.researchgate.net/publication/246382499. [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion. Chronic disease overview. 2015 Retrieved from http://www.cdc.gov/chronicdisease/overview/index.htm.
- Pham MT, Rajic A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Research Synthesis Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. Fourth. New York: Free Press; 1995. Retrieved from https://books.google.com/books?hl=en&lr=&id=v1ii4QsB7jIC. [Google Scholar]
- Rogers EM. Diffusion of Innovations. 5th. New York: Free Press; 2003. 2003. [Google Scholar]
- Siu AM, Chan CC, Poon PK, Chui DY, Chan SC. Evaluation of the chronic disease self-management program in a Chinese population. Patient Education and Counseling. 2007;65(1):42–50. doi: 10.1016/j.pec.2006.04.013. doi: S0738-3991(06)00155-8 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeulders ES, Haastregt JC, Ambergen T, Janssen-Boyne JJ, Eijk JT, Kempen GI. The impact of a self-management group programme on health behaviour and healthcare utilization among congestive heart failure patients. European Journal of Heart Failure. 2009;11(6):609–616. doi: 10.1093/eurjhf/hfp047. [DOI] [PubMed] [Google Scholar]
- Smeulders ESTF, Van Haastregt JCM, Dijkman-Domanska BK, Van Hoef EFM, Van Eijk JTM, Kempen GIJM. Nurse- and peer-led self-management programme for patients with an implantable cardioverter defibrillator; a feasibility study. BMC Nursing. 2007;6 doi: 10.1186/1472-6955-6-6. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2096621/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford School of Medicine. Chronic disease self-management program (better choices, better health® workshop) 2015 Retrieved from http://patienteducation.stanford.edu/programs/cdsmp.html.
- Swerissen H, Belfrage J, Weeks A, Jordan L, Walker C, Furler J, Peterson C. A randomised control trial of a self-management program for people with a chronic illness from Vietnamese, Chinese, Italian and Greek backgrounds. Patient Education and Counseling. 2006;64(1–3):360–368. doi: 10.1016/j.pec.2006.04.003. doi: S0738-3991(06)00118-2 [pii] [DOI] [PubMed] [Google Scholar]
- Tomioka M, Braun KL, Compton M, Tanoue L. Adapting Stanford’s chronic disease self-management program to Hawaii’s multicultural population. The Gerontologist. 2012;52(1):121–132. doi: 10.1093/geront/gnr054. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomioka M, Braun KL, Ah Cook V, Compton M, Wertin K. Improving behavioral and clinical indicators in Asians and pacific islanders with diabetes: Findings from a community clinic-based program. Diabetes Research and Clinical Practice. 2014;104(2):220–225. doi: 10.1016/j.diabres.2013.12.035. http://dx.doi.org/10.1016/j.diabres.2013.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker C, Weeks A, McAvoy B, Demetriou E. Exploring the role of self-management programmes in caring for people from culturally and linguistically diverse backgrounds in Melbourne, Australia. Health Expectations. 2005;8(4):315–323. doi: 10.1111/j.1369-7625.2005.00343.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16266419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Hardin HK, Zhou L, Fang L, Shi P, Robinson KM. Implementation and evaluation of the chronic-disease self-management program among Chinese immigrant older adults in the US. Geriatric Nursing. 2014;35(6):448–450. doi: 10.1016/j.gerinurse.2014.07.002. http://dx.doi.org/10.1016/j.gerinurse.2014.07.002. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Noncommunicable diseases. 2015 Retrieved from http://www.who.int/mediacentre/factsheets/fs355/en/
- Yip YB, Sit JW, Fung KKY, Wong DYS, Chong SYC, Chung LH, Ng TP. Impact of an arthritis self-management programme with an added exercise component for osteoarthritic knee sufferers on improving pain, functional outcomes, and use of health care services: An experimental study. Patient Education and Counseling. 2007;65(1):113–121. doi: 10.1016/j.pec.2006.06.019. http://dx.doi.org/10.1016/j.pec.2006.06.019. [DOI] [PubMed] [Google Scholar]


