Abstract
Background
We estimated the efficacy of the Addiction-Comprehensive Health Enhancement Support System (A-CHESS) in increasing the use of services for addiction and examined the extent to which this use of services mediated the effects of A-CHESS on risky drinking days and abstinence from drinking.
Methods
We conducted secondary data analyses of the A-CHESS randomized controlled trial. Recruitment occurred in five residential treatment programs operated by two addiction treatment organizations. Participants were 349 adults with alcohol use disorders recruited two weeks before discharge from residential treatment. We provided intervention arm participants with a smartphone, the A-CHESS application, and an 8-month service plan. Control arm participants received treatment as usual. Telephone interviews at 4, 8, and 12-month follow-ups assessed past-month risky drinking days, past-month abstinence, and post-discharge service utilization (past-month outpatient addiction treatment and past-week mutual help including Alcoholics Anonymous and Narcotics Anonymous). Using mixed effects latent variable models, we estimated the indirect effects of A-CHESS on drinking outcomes, as mediated by post-discharge service utilization.
Results
Approximately 50.5% of participants reported outpatient addiction treatment and 75.5% reported mutual help at any follow-up interview in the year following randomization. Assignment to the A-CHESS intervention was associated with an increased odds of outpatient addiction treatment across follow-ups, but not mutual help. This use of outpatient addiction treatment mediated the effect of A-CHESS on risky drinking days, but not abstinence. The effect of A-CHESS through outpatient addiction treatment appeared to reduce the expected number of risky drinking days across follow-ups by 11%.
Conclusions
The mobile health (mHealth) intervention promoted the use of outpatient addiction treatment, which appeared to contribute to its efficacy in reducing risky drinking. Future research should investigate how mHealth interventions could link patients to needed treatment services and promote the sustained use of these services.
Keywords: Treatment utilization, smartphone, mobile health, mediation, aftercare, continuing care, randomized controlled trial
1. Introduction
The Comprehensive Health Enhancement Support System (CHESS) (Gustafson et al., 2002) is an electronic health framework that has been applied to a diverse set of health problems, including pediatric asthma control (Gustafson et al., 2012) and recovery support for breast (Gustafson et al., 2005, 2008) and lung (Gustafson et al., 2013) cancer. Addiction-CHESS (A-CHESS) is a multi-component smartphone application based on the CHESS framework that was designed to provide continuing support to people in substance use recovery (Gustafson et al., 2011, 2014). With a design consistent with self-determination theory (Ryan & Deci, 2000), A-CHESS seeks to increase coping competence by enhancing skills that prevent relapse, enhance social relatedness by connecting end-users to sources of social support, and promote autonomy in managing one’s recovery from their addiction. Accordingly, this mobile health (mHealth) system allows individuals to gain knowledge and skills, to connect with others who share their struggles, and to set their own goals and to choose to use some or all of its components (see Appendix A for a list and description of A-CHESS components) (McTavish, Chih, Shah, & Gustafson, 2012).
In the A-CHESS randomized controlled trial (n = 349; the study that produced the secondary data analyzed in the current report), persons with alcohol use disorders discharged from residential treatment from one of two nonprofit organizations were assigned to A-CHESS for 8 months or a control condition that only received assessments (Gustafson et al., 2014). Individuals assigned to receive A-CHESS had significantly fewer risky drinking days and increased abstinence over twelve months than those in the control condition. These findings raise questions about mechanisms that may have helped produced treatment efficacy. The identification of effective mechanisms is particularly important in the field of mHealth research, where clinical trials have generated mixed findings regarding the efficacy of interventions (Dedert et al., 2015).
Prior analyses of mHealth interventions for addiction and other health conditions have largely focused on identifying psychological mechanisms of behavior change that are common in face-to-face interventions (Dallery et al., 2015). For instance, self-efficacy was found to be a mechanism of change in the A-CHESS trial (Gustafson et al., 2014). However, mHealth interventions may have other possible mechanisms of behavior change beyond traditional psychological mechanisms. Some have proposed that mHealth interventions may be best used to strengthen connections between patients and existing healthcare delivery systems, rather than solely relying on mHealth solutions to produce change on their own (Labrique, Vasudevan, Kochi, Fabricant, & Mehl, 2013; Mohr, Burns, Schueller, Clarke, & Klinkman, 2013). Thus, one candidate mechanism of change is that technology-based recovery support interventions such as A-CHESS may encourage people to seek additional in-person treatment. For instance, in the case of the A-CHESS trial among individuals discharging from residential addiction treatment, recovery support features in A-CHESS may have influenced individuals to seek aftercare in the form of outpatient treatment or mutual help (e.g., Alcoholics Anonymous or Narcotics Anonymous).
Aftercare, also known as “step-down” care or continuing care, refers to addiction treatment received after an initial intensive treatment phase, such as outpatient care following residential care, and may involve additional support including mutual help programs (McKay, 2005, 2009). Aftercare is a new phase of treatment that may be initiated to reduce risk of relapse and/or to maintain progress after a relapse occurs. Given that substance use disorders can manifest as chronic conditions, keeping patients engaged in treatment systems is often a desirable goal (McKay, 2005; McLellan, Lewis, O’Brien, & Kleber, 2000), and systematic reviews suggest that aftercare can improve addiction-related outcomes. The majority of trials investigate aftercare in outpatient settings, but some have investigated mutual help as a form of aftercare (Blodgett, Maisel, Fuh, Wilbourne, & Finney, 2014; McKay, 2009). Thus, if mHealth recovery support interventions such as A-CHESS could facilitate the use of outpatient addiction treatment or mutual help following residential care, this could be a potentially effective approach to improving patient outcomes. To our knowledge, no studies have examined whether mHealth interventions could potentially increase the use of services for addiction following residential care, and additionally, whether this use of additional services would in turn have an impact on substance use outcomes, helping to explain the mechanisms of behavior change in terms of reduced risky drinking and increased abstinence.
The study reported here was a secondary data analysis of the A-CHESS randomized controlled trial. We estimated the efficacy of A-CHESS in increasing the utilization of post-discharge addiction services including outpatient addiction treatment and (separately) mutual help, and examined the extent to which this use of services mediated the effect of A-CHESS on the primary study outcome, risky drinking days, as well as a secondary study outcome, abstinence. We hypothesized that 1) participants assigned to the A-CHESS study arm made more use of post-discharge addiction services in the year following discharge when compared to controls, 2) the use of post-discharge addiction services was associated with reduced drinking days and increased abstinence, and 3) the use of post-discharge addiction services mediated the association of study arm with risky drinking days and abstinence.
2. Method
2.1 Participants and procedures
The A-CHESS randomized controlled trial recruited participants from five residential addiction treatment programs in two addiction treatment organizations two weeks before their anticipated date of discharge. Inclusion criteria were: DSM-IV alcohol dependence upon entering residential treatment, age 18 or older, willing to be randomized, and able to identify two contacts to help reach the participant. Participants were excluded if information in the medical chart indicated that they had a significant developmental impairment, cognitive impairment, or vision problems that would limit the ability to use the smartphone application. A total of 349 adults with alcohol use disorders were enrolled (91.8% of those approached). A more detailed description of the participants and procedures can be found in a prior publication (Gustafson et al., 2014).
2.2 Intervention
Participants were randomized to receive the intervention (A-CHESS) for eight months or to receive treatment as usual. Intervention group participants were provided with a smartphone and eight-month service plan. The smartphone was loaded with the A-CHESS application and participants were taught how to use it before discharge under counselor guidance. After this brief training, intervention arm participants were required to demonstrate a minimal understanding of smartphone use, text messaging, and basic A-CHESS use; set up an anonymous profile; and load contact information for two persons who would receive text messages if the patient pressed the panic button. A research team member served as an “A-CHESS coach”, providing intervention group participants with regular, empathic outreach, primarily through electronic discussion board posts. Participants were followed for one year after randomization and surveys were administered by the research team in person at baseline and by telephone at four, eight, and 12 months. Intervention arm participants kept the smartphone at the end of the eight-month intervention period and could continue using the A-CHESS system if they desired, though they had to pay for their own service plan or use wireless internet. Prior reports showed that approximately 80% of participants assigned to the A-CHESS arm continued to access the system four months after randomization (McTavish et al., 2012), and 57.6% of participants used A-CHESS at least once in the last week of the 8-month intervention (Gustafson et al., 2014). Intervention design, recruitment, and follow-up procedures have been described in prior publications (Gustafson et al., 2011, 2014; McTavish et al., 2012). Appendix A contains descriptions of A-CHESS components.
2.3 Outcome Measures
Primary and secondary outcomes
The primary outcome of the A-CHESS trial was risky drinking days, using the National Institute on Alcohol Abuse and Alcoholism definition of a standard drink. One item asked patients to report the number of risky drinking days in the previous 30 days, which were defined as exceeding 4 standard drinks in a 2-hour period for men or 3 standard drinks in a 2-hour period for women. Abstinence was a secondary outcome, assessed with one item, which we coded as positive for those who reported consuming 0 drinks in the previous 30 days.
Post-discharge outpatient addiction treatment and mutual help attendance
We assessed post-discharge outpatient addiction treatment services by querying the presence of any past-month outpatient addiction treatment versus none at each follow-up (months 4, 8, and12). The follow-up survey included a study-specific measure of addiction treatment utilization asking participants, “Have you been back to treatment in the past month?” followed by the question, “are you going to outpatient treatment?” To assess mutual help attendance, we relied upon an item from the Brief Addiction Monitor (Cacciola et al., 2013; Nelson, Young, & Chapman, 2014) that assessed past-week Alcoholics Anonymous or Narcotics Anonymous group attendance at each follow-up interview. The item was phrased, “how many days did you attend self-help meetings like Alcoholics Anonymous or Narcotics Anonymous to support your recovery?” We coded mutual help attendance as any versus none in the past week at each interval, dichotomizing this item so the measurement scales of these two service utilization variables would be consistent for the mediation analysis.
2.4 Covariates
Baseline covariates assessed in patient interviews included sociodemographic characteristics (age, gender, race), any mental health problems beyond substance use disorders (yes/no), and lifetime use of addiction treatment prior to entering residential care (yes/no), given that these variables may influence both treatment utilization and study outcomes (Booth, Curran, Han, & Edlund, 2013; Glass et al., 2010; Glass, Grant, Yoon, & Bucholz, 2015; Ilgen et al., 2011). As a measure of motivation for treatment, we assessed reasons for entering residential care (treatment sought per own initiative, family/friend pressures, employer pressures, court referral, family services referral; each reason was coded as yes/no).
2.5 Statistical analysis
Descriptive statistics
We described the sample by calculating means and standard deviations for continuous variables and totals and proportions for categorical variables, using Stata 14.0 (StataCorp, 2015).
Main effects analysis
To estimate the association of study arm with risky drinking days, we used a log-linear mixed effects Poisson model for count data with time nested within persons, and we used a logistic model when estimating the dichotomous outcomes of post-discharge outpatient addiction treatment, mutual help, and abstinence. Study arm, time (with values corresponding to interview month), recruitment site, and all covariates were modeled as fixed effects, with a random intercept for subjects.
Mediation analysis
Conceptually, mediation models seek to explain the extent to which causal relationships between independent variables and their outcomes occur through intervening variables (MacKinnon, 2008). Modern statistical methods for mediation analysis include the ability to estimate an “indirect effect” that quantifies the extent to which a change in an independent variable affects a change in the dependent variable specifically through its influence on a mediating variable (MacKinnon, 2008).
We sought to identify whether and how much post-discharge services for addiction, including outpatient addiction treatment and mutual help, were each responsible for the effects of the A-CHESS intervention on two study outcomes, risky drinking days and abstinence. We used Mplus 7.4 for the mediation analyses (Muthén & Muthén, 1998) which used a log-linear model for risky drinking days, and a logistic model for abstinence. With the maximum likelihood robust estimator, we modeled these outcomes as a function of post-discharge service utilization (outpatient addiction treatment and mutual help) and study arm. We used mixed effects models with time nested within persons to accommodate the longitudinal design and adjusted for all covariates in the analyses.
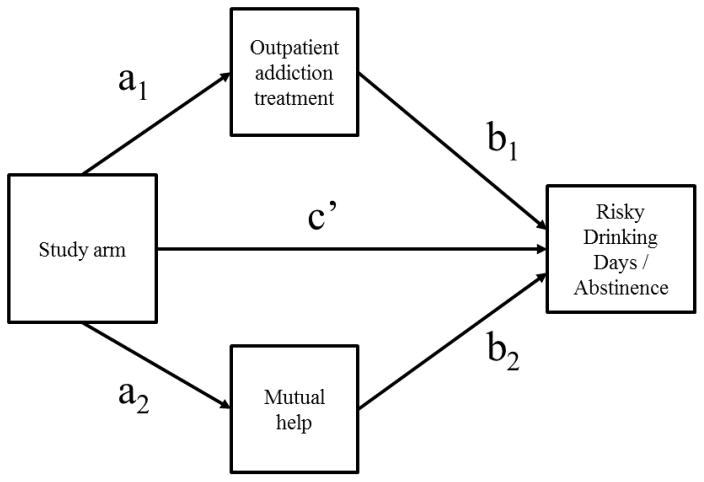
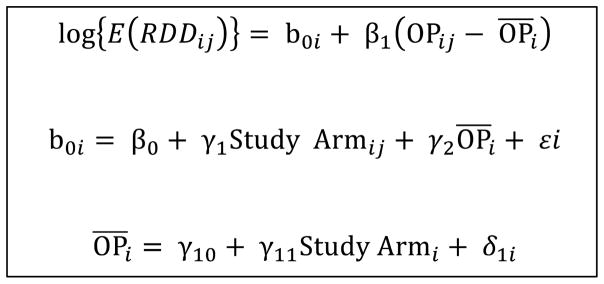
To calculate the indirect effect, we used the product of coefficients approach, which multiplies coefficients “a” (the effect of study arm on each subject’s mean service utilization across study periods) and “b” (the between-person association of each subject’s mean service utilization with drinking days or abstinence) (MacKinnon, 2008). Preacher, Zyphur, and Zhang (2010) demonstrate that between-person differences (e.g., differences in mean service utilization), rather than within-person differences (e.g., deviations from the mean), must be modeled in mediation analyses of randomized controlled trials; the independent variable (study arm) varies at the participant-level but stays constant over time, thus assignment to study arm must have an effect at the participant-level. Therefore, we estimated separate between- and within-person coefficients by modeling both the participant-level mean of service utilization and time-specific deviations from the participant-level mean (Begg & Parides, 2003). This approach in testing mediation has been deemed the “unconflated multilevel model” (Preacher et al., 2010). We estimated separate models for each outcome, because abstinence from alcohol would preclude risky drinking. Figure 1 contains a path diagram and Appendix B contains the system of equations for the mediation model (MacKinnon, 2008).
Figure 1.
Path diagram for the analyses examining the mediation of the intervention effect on alcohol outcomes through post-discharge outpatient addiction treatment and mutual help. Mediation was examined with the product of coefficients approach (e.g., a1*b1). Tables 4 and 5 contain corresponding estimates from this figure computed with Mplus. Appendix B contains the system of equations underlying this path diagram.
We compared the results of two approaches, the first using concurrent measurements of service utilization and the outcome variable (both service utilization and outcome measurements at 4, 8, and 12 months), and the second using lagged measurements (service utilization at 4 and 8 months and outcome measurements at 8 and 12 months). For a measure of effect size, we transformed the indirect effect to estimate the percent change in the expected number of risky drinking days or the percent change in the probability of abstinence, attributed to the effect of A-CHESS operating through post-discharge service utilization (Long, 1997). We also used these calculations to estimate the ratio of the mediated effect of A-CHESS (through post-discharge addiction services) to the total effect of A-CHESS (the mediated effect plus the direct effect) (Preacher & Kelley, 2011).
3. Results
3.1 Sample characteristics
Table 1 contains descriptive statistics for the analytic sample. Participants were 80.2% white, 39.3% female, and had a mean age of 38.3 years. About 50.5% of participants reported past-month outpatient addiction treatment at any follow-up (36.0% at month 4, 23.9% at month 8, and 19.9% at month 12) and 75.5% reported past-week mutual help attendance at any follow-up (60.1% at month 4, 60.1% at month 8, and 57.7% at month 12) (see Table 2). Participants who reported past-month outpatient addiction treatment at any follow-up were more likely than those who did not to be male or to enter residential care because of a court referral (not shown). Those who reported past-week mutual help at any follow-up period were more likely than those who did not to have a history of attending addiction treatment prior to entering residential care (not shown).
Table 1.
Characteristics of participants enrolled in the A-CHESS trial (n = 349)
| Overall | A-CHESS | Controls | ||
|---|---|---|---|---|
|
| ||||
| M (SD) or N (%) | F (df), p | |||
| Age | 38.3 (10.4) | 38.3 (9.5) | 38.4 (11.2) | 0.0 (1), p = 0.927 |
| Female | 137 (39.3%) | 67 (39.4%) | 70 (39.1%) | 0.0 (1), p = 0.953 |
| Race | 0.2 (2), p = 0.893 | |||
| African American | 45 (12.9%) | 21 (12.4%) | 24 (13.4%) | |
| Other | 11 (3.2%) | 6 (3.5%) | 5 (2.8%) | |
| White | 293 (84.0%) | 143 (84.1%) | 150 (83.8%) | |
| Prior addiction treatment | 267 (76.5%) | 130 (76.5%) | 137 (76.5%) | 0.0, (1), p = 0.988 |
| Began residential treatment due to: | ||||
| Family pressure | 120 (34.4%) | 56 (33.0%) | 64 (35.8%) | 0.3 (1), p = 0.580 |
| Employer pressure | 28 (8.0%) | 8 (4.7%) | 20 (11.2%) | 5 (1), p = 0.026 |
| Court referral | 72 (20.6%) | 37 (21.8%) | 35 (19.6%) | 0.3 (1), p = 0.610 |
| Children or family services referral | 27 (7.7%) | 15 (8.8%) | 12 (6.7%) | 0.5 (1), p = 0.459 |
| Own initiative | 329 (94.3%) | 161 (94.7%) | 168 (93.9%) | 0.1 (1), p = 0.732 |
| Past-month risky drinking daysa | 2.0 (5.8) | 1.3 (4.5) | 2.7 (6.7) | 8.7 (1), p = 0.003 |
| Past-month abstinenceb | 250 (89.6%) | 127 (93.4%) | 123 (86.0%) | 4.1 (1), p = 0.044 |
| Post-discharge outpatient addiction treatmentb | 141 (50.5%) | 79 (58.1%) | 62 (43.4%) | 6.1 (1), p = 0.014 |
| Post-discharge mutual helpb | 210 (75.5%) | 108 (79.4%) | 102 (71.8%) | 2.2 (1), p = 0.142 |
F statistics were calculated with a Pearson chi-square test for categorical variables and Wald tests for continuous variables.
Mean risky drinking days across follow-ups are reported.
The presence of abstinence, outpatient addiction treatment, and mutual help at any follow-up is reported.
Table 2.
Rates of post-discharge outpatient addiction treatment and mutual help at each follow-up overall and within study arms
| Outpatient addiction treatment | Mutual help | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Month 4 n = 311 |
Month 8 n = 297 |
Month 12 n = 281 |
Month 4 n = 298 |
Month 8 n = 288 |
Month 12 n = 279 |
|
| % (n) receiving treatment | ||||||
| Overall | 36.0% (112) | 23.9% (71) | 19.9% (56) | 60.1% (179) | 60.1% (173) | 57.7% (161) |
| A-CHESS arm (n = 156) | 40.4% (63) | 29.5% (43) | 25.7% (35) | 63.2% (96) | 63.6% (91) | 64.7% (88) |
| Control arm (n = 155) | 31.6% (49) | 18.5% (28) | 14.5% (21) | 56.9% (83) | 56.6% (82) | 51.1% (73) |
Proportions were among participants with complete data within each follow-up interview.
3.2 Main effects analysis
Table 3 contains results of mixed effects models estimating the association of study arm with post-discharge service utilization, risky drinking days, and abstinence. Participants in the A-CHESS arm had increased odds of obtaining outpatient addiction treatment (OR=2.14, 95% CI=1.27–3.61), but not mutual help, compared to those in the control arm when examining the intervention effect over all follow-up periods combined. Assignment to the A-CHESS intervention was associated with reduced risking drinking days and increased abstinence over time, which has been reported previously (Gustafson et al., 2014).
Table 3.
The association of study arm in the A-CHESS trial with outcomes over 12 months (n = 349)
| Dependent variable | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Post-discharge outpatient addiction treatment | Post-discharge mutual help | Risky drinking days | Abstinence | |||||
|
|
|
|
|
|||||
| Effect | Odds Ratio (95% CI) | P | Odds Ratio (95% CI) | p | Incidence rate ratio (95% CI) | p | Odds ratio (95% CI) | p |
| Overall intervention effect (all follow-up periods)1 | 2.14 (1.27–3.61) | 0.004 | 2.06 (0.96–4.37) | 0.061 | 0.47 (0.25–0.90) | 0.023 | 1.99 (1.08–3.65) | 0.025 |
| Time effect (interview month) | 0.86 (0.81–0.91) | <0.001 | 0.96 (0.90–1.02) | 0.271 | 0.98 (0.96–0.99) | 0.006 | 1.01 (0.95–1.07) | 0.083 |
| Intervention effect at each follow-up period2 | ||||||||
| Month 4 | 1.53 (0.93–2.52) | 0.091 | 1.39 (0.81–2.37) | 0.231 | 0.55 (0.47–0.65) | <0.001 | 1.45 (0.86–2.45) | 0.161 |
| Month 8 | 1.96 (1.09–3.52) | 0.024 | 1.47 (0.85–2.55) | 0.165 | 0.55 (0.46–0.65) | <0.001 | 1.76 (1.01–2.95) | 0.046 |
| Month 12 | 2.16 (1.13–4.12) | 0.019 | 2.00 (1.16–3.44) | 0.013 | 0.42 (0.34–0.51) | <0.001 | 1.87 (1.07–3.29) | 0.028 |
Bolded values are statistically significant (p < 0.05). Models controlled for treatment site, interview month, sociodemographic characteristics, any mental health problems, lifetime addiction treatment prior to entering residential care, and reasons for entering treatment.
All available data were analyzed with mixed effects regression.
Analyses within follow-up periods included participants with complete data at the time point of interest (for post-discharge outpatient addiction treatment, n = 311 at month 4, n = 297 at month 8, and n = 281 at month 12; for mutual help, n = 298 at month 4, n = 288 at month 8, and n = 279 at month 12; for risky drinking days, n = 314 at month 4, n = 297 at month 8, and n = 281 at month 12; for abstinence, n = 311 at month 4, n = 297 at month 8, and n = 281 at month 12).
Looking within follow-up periods, the odds of outpatient addiction treatment utilization were significantly higher among A-CHESS participants than controls at months eight (OR=1.96, 95% CI=1.09–3.52) and 12 (OR=2.16, 95% CI=1.13–4.12), but not month four (OR=1.53 95% CI=0.93–2.52) (Table 3). The odds of mutual help were significantly higher in the A-CHESS group than in controls at month 12 (OR=2.00, 95% CI=1.16–3.44), but not at months four (OR=1.39, 95% CI=0.81–2.37) or eight (OR=1.47, 95% CI=0.85–2.55). Rates of outpatient addiction treatment at each follow-up were approximately 9–11 percentage points higher in the A-CHESS arm than in the control arm (e.g., 40.4% vs. 31.6% at month four; Table 2). Rates of mutual help at month 12 were approximately 13.6 percentage points higher in the A-CHESS arm than in the control arm. Appendix C shows that for both study arms, and in particular, the A-CHESS arm, the majority of outpatient addiction treatment and mutual help received at months 8 and 12 was among participants who had received those services at month 4.
3.3 Mediation analysis
Risky drinking days
Table 4 contains estimates for the mediation analyses examining the outcome of risky drinking days computed in Mplus for both concurrent and lagged (services at four and eight months and risky drinking days at eight and 12 months) associations. There was a statistically significant association of study arm with both post-discharge outpatient addiction treatment and risky drinking days, but not with mutual help, which was consistent with the main effects analysis presented above. Both the lagged and concurrent associations were consistent, supporting the robustness of these results.
Table 4.
Post-discharge outpatient addiction treatment and mutual help as mediators of the association between study arm and risky drinking days in the A-CHESS trial (n = 349)
| Dependent variable | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Post-discharge outpatient addiction treatment (Mediator) | Mutual help (Mediator) | Risky drinking days (Outcome) | Indirect effect | |||||
|
|
|
|
|
|||||
| b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | |
| Independent variable | Concurrent associations - b (95% CI) | |||||||
|
| ||||||||
| A-CHESS (study arm) | 0.11 (0.04–0.17) | 0.002 | 0.07 (−0.01–0.15) | 0.101 | −0.60 (−1.04-−0.17) | 0.007 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | −1.16 (−1.85-−0.41) | 0.002 | −0.12 (−0.24-−0.01) | 0.035 |
| Post-discharge mutual help | -- | -- | -- | -- | −1.43 (−2.03-−0.83) | <0.001 | −0.01 (−0.22-−0.03) | 0.119 |
|
| ||||||||
| Lagged associations - b (95% CI) | ||||||||
|
| ||||||||
| A-CHESS (study arm) | 0.10 (0.02–0.18) | 0.018 | 0.08 (−0.05–0.17) | 0.064 | −0.63 (−1.17-−0.09) | 0.021 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | −1.34 (−2.22-−0.45) | 0.003 | −0.13 (−0.27–0.01) | 0.071 |
| Post-discharge mutual help | -- | -- | -- | -- | −1.49 (−2.19-−0.79) | <0.001 | −0.12 (−0.27–0.02) | 0.094 |
Coefficients are displayed from Mplus models computed with the maximum likelihood robust estimator. Linear regression coefficients are shown for post-discharge outpatient addiction treatment and mutual help (the dependent variable was the person-level mean of service use follow-up periods) and Poisson regression coefficients are displayed for risky drinking days. Bolded values are statistically significant (p < 0.05). Models controlled for treatment site, interview month, age, gender, race, presence of mental health problems, prior addiction treatment, reasons for entering treatment, and within-person changes in service utilization. Race was dichotomized to white vs. other (collapsing black and other categories) due to empty bivariate cells. Within-person estimates for the associations between services utilization and risky drinking days are provided in Appendix D.
Post-discharge outpatient addiction treatment mediated the association of study arm with risky drinking days, as indicated by the statistically significant indirect effect. Mutual help did not mediate an association between study arm and risky drinking days. The magnitude of the mediated effect through outpatient addiction treatment, which was based on a transformation of the indirect effect to the scale of the dependent variable (expected number of risky drinking days), is summarized as follows. A-CHESS, operating through post-discharge outpatient addiction treatment, was associated with an 11.3% (95% CI=1.33–21.3) decrease in risky drinking days. To put this value in context, we also transformed the direct effect (the c’ path, which was adjusted for treatment utilization, Figure 1). The transformed direct effect indicated that A-CHESS independently decreased the expected number of risky drinking days by 45.2% (95% CI=21.4–76.5). These estimates are on the same scale, and thus, the ratio of the mediated effect of A-CHESS through post-discharge outpatient addiction treatment (11%) to the total effect of A-CHESS (56%, including the direct and indirect effect) was approximately 19.6% (Preacher & Kelley, 2011). We note that the indirect effect was statistically significant when examining concurrent associations; however, the indirect effect for the lagged associations approached but did not achieve statistical significance (p = 0.094).
Abstinence
Table 5 contains estimates for the mediation analyses examining the outcome of abstinence computed in Mplus for both concurrent and lagged (services at four and eight months and abstinence at eight and 12 months) associations. There was a statistically significant association of study arm with both post-discharge outpatient addiction treatment and abstinence, but not mutual help, which was consistent with the main effects analysis. The concurrent and lagged associations between mutual help and abstinence were statistically significant. Outpatient addiction treatment was not significantly associated with abstinence. The indirect effects were not statistically significant, indicating that for the outcome of abstinence, mediation did not occur through outpatient addiction treatment or mutual help.
Table 5.
Post-discharge outpatient addiction treatment and mutual help as mediators of the association between study arm and past-month abstinence in the A-CHESS trial (n = 349)
| Dependent variable | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Post-discharge outpatient addiction treatment (Mediator) | Mutual help (Mediator) | Abstinence (Outcome) | Indirect effect | |||||
|
|
|
|
|
|||||
| b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | |
|
|
||||||||
| Independent variable | Concurrent associations - b (95% CI) | |||||||
|
| ||||||||
| A-CHESS (study arm) | 0.11 (0.04–0.20) | 0.002 | 0.07 (−0.01–0.15) | 0.101 | 0.64 (0.20–1.26) | 0.043 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | 0.81 (−0.18–1.80) | 0.108 | 0.09 (−0.04–0.21) | 0.168 |
| Post-discharge mutual help | -- | -- | -- | -- | 1.93 (1.02–2.85) | <0.001 | 0.13 (−0.04–0.31) | 0.135 |
|
| ||||||||
| Lagged associations - b (95% CI) | ||||||||
|
| ||||||||
| A-CHESS (study arm) | 0.10 (0.02–0.18) | 0.018 | 0.08 (−0.01–1.71) | 0.064 | 0.85 (0.09–1.60) | 0.027 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | 0.79 (−0.34-−1.92) | 0.169 | 0.06 (−0.05–1.69) | 0.287 |
| Post-discharge mutual help | -- | -- | -- | -- | 1.87 (0.83–2.92) | <0.001 | 0.16 (−0.04–0.35) | 0.120 |
Coefficients are displayed from Mplus models computed with the maximum likelihood robust estimator. Linear regression coefficients are shown for post-discharge outpatient addiction treatment and mutual help (the dependent variable was the person-level mean of service use across follow-up periods) and probit regression coefficients are displayed for abstinence. Bolded values are statistically significant (p < 0.05). Models controlled for treatment site, interview month, age, gender, race, presence of mental health problems, prior addiction treatment, reasons for entering treatment, and within-person changes in service utilization. Race was dichotomized to white vs. other (collapsing black and other categories) due to empty bivariate cells. Within-person estimates for the associations between services utilization and abstinence are provided in Appendix E.
4. Discussion
The primary purpose of this study was to investigate the use of post-discharge addiction services as a potential mechanism of behavior change in A-CHESS, an efficacious mHealth intervention for alcohol use disorder for patients leaving residential treatment. A-CHESS increased the odds of outpatient addiction treatment, and the use of these treatment services was associated with reduced risky drinking days. Mediation analyses indicated that the use of post-discharge outpatient addiction treatment mediated some of the effect that A-CHESS had on risky drinking days. A-CHESS’s effect on risky drinking specifically through outpatient addiction treatment was equivalent to an 11% decrease in the expected number of risky drinking days across follow-ups. This reduction was approximately one-fifth of the total effect of A-CHESS on risky drinking days. In contrast, mutual help did not mediate the effects of A-CHESS on risky drinking days, and the effect of A-CHESS on mutual help services was present only at month 12. While A-CHESS increased abstinence, neither outpatient treatment nor mutual help mediated the effects of the A-CHESS intervention on abstinence.
Mediation analysis is an important first step in identifying possible mechanisms through which interventions may exert their effects, in order to inform future intervention development (Kazdin, 2007). Per these analyses, A-CHESS was efficacious in reducing risky drinking independent of participants’ outpatient treatment utilization, and A-CHESS promoted the use of outpatient treatment following discharge from residential care, which may have further reduced risky drinking. This study is unique in its attempts to quantify the extent to which an mHealth intervention may produce changes in individuals’ interactions with the environment—in particular, interactions with treatment systems—which may in turn lead to improved outcomes. Most of those who received addiction treatment during the latter follow-up periods had already received treatment by month 4, and those who received the A-CHESS intervention were more likely to receive treatment in the latter follow-up periods. This could indicate that A-CHESS facilitates sustained engagement in aftercare. The A-CHESS trial had a relatively lengthy intervention period (8 months), which could have helped sustain participants’ use of additional treatment. Aftercare is an important part of the addiction treatment continuum that may lead to improved addiction-related outcomes (Blodgett et al., 2014; McKay, 2005, 2009). We note that although approximately 20% of the total effect of A-CHESS on risky drinking days appeared to be through outpatient treatment, A-CHESS was not specifically designed to facilitate the use of outpatient treatment. Thus, mHealth intervention researchers may wish to evaluate ways to facilitate ongoing care intentionally, perhaps by helping patients navigate treatment choices and overcome barriers to treatment.
There are a number of explanations for how an mHealth recovery support intervention like A-CHESS could increase the use of outpatient treatment when provided to individuals leaving residential treatment. A-CHESS components were designed to be available anytime and anywhere, increasing the chance that participants could obtain encouragement and support to enter treatment during critical moments in which they desire this type of assistance. For instance, the Discussions component allows users to post and respond to electronic messages as a way to provide and obtain social support, which could increase recovery-promoting behaviors, including participation in aftercare or entrance into a new episode of care. Pressing a Panic Button can connect users to friends, family, or other sources of support, who may advocate for more treatment, and the A-CHESS coach encouraged participants to reach out to others when in need of support. Several other components (e.g., Recovery Info, Our Stories) provide information resources related to the benefits of treatment, which could also promote interest in aftercare. In addition, the general focus on enhancing recovery in all functions of A-CHESS may motivate individuals to seek out additional support via treatment services. It is unknown whether the effect of mHealth on treatment utilization will generalize across studies of mHealth interventions or this effect is specific to some aspect of the A-CHESS design.
While it is useful to theorize about which specific aspects of A-CHESS may have led to increased use of post-discharge outpatient addiction treatment, this topic needs rigorous study in several areas before testing this association empirically. First, approaches to measuring mHealth use need further conceptualization and validation. Researchers can analyze mHealth log files to measure how much participants used specific components, but the optimal approach to operationalizing these data for regression analyses remain unknown. What constitutes meaningful use of a component? Do you measure all “hits” or uses of a component, or is there specific content within each component that matters the most? Do you measure the number of days participants used a component, the number of times participants used a component, or the number of minutes spent using a component? We are currently executing a project to explore such questions. Second, what analytic techniques are best suited to establish a causal link between mHealth component use and subsequent outcomes? A-CHESS was developed under the principle of self-determination theory, specifically competence, relatedness, and autonomy, whereby users select what information they consume, interactions they explore, and components they utilize. Thus, associations between component use and outcomes would be highly confounded by self-selection. Factorial experiments that randomize individuals to mHealth components would be better suited to answering questions about what components produce treatment efficacy (Collins, Dziak, Kugler, & Trail, 2014; McClure et al., 2014).
Several specific findings in the current study warrant further comment. While A-CHESS increased abstinence, it did not have an overall effect on mutual help across all follow-ups (only increasing mutual help at month 12), and thus mutual help attendance did not mediate the effect of A-CHESS. However, most participants used mutual help services (e.g., 60.1% in the past week at month four). Perhaps, the majority of the sample may have already realized improvements owing to mutual help participation, independent of their A-CHESS involvement. This high prevalence of mutual help as compared to outpatient treatment (30.6% used outpatient treatment in the past month at month 4) may suggest that some residential treatment programs may emphasize mutual help attendance for aftercare more than formal treatment. However, in the current study, mutual help program attendance following discharge from residential care was associated with an increased odds of abstinence. This lends additional support to the notion that mutual help attendance should be encouraged among individuals discharging from formal treatment as a means to support abstinence and long-term recovery (Kelly & Yeterian, 2011), and thus, both mutual help and outpatient treatment attendance should perhaps be encouraged when discharging from higher levels of care.
When examining mediation through outpatient addiction treatment, mediation was present when analyzing concurrent relationships between aftercare utilization and risky drinking days, but not when examining lagged relationships. In the lagged analyses, the mediation effect only approached statistical significance. Perhaps, other mechanisms of behavior change in A-CHESS may better explain the system’s sustained outcomes, such as increases in abstinence self-efficacy, which has been identified as a mechanism of change in prior research on A-CHESS (Gustafson et al., 2014). However, it is important to consider that the assessment intervals for outpatient treatment were long (4 months in between assessments), and may have been too long to detect a lagged relationship. Moreover, we did not find mediation when examining the outcome of abstinence. Rates of abstinence were high (and conversely, rates of risky drinking were low) across follow-up periods, which could suggest a possible floor effect (e.g., patients underestimating their drinking, or a sample of patients who were largely successful in reducing their drinking), which could have made it more difficult to detect a mediation effect as well as a stronger intervention effect. Finally, although outpatient addiction treatment mediated a notable proportion (20%) of A-CHESS’s total effect on risky drinking days, this also suggests that the majority of A-CHESS’s effects on risky drinking can be attributed to other factors. It remains important for mHealth interventions to continue to target established psychological mechanisms of change in mHealth interventions, such as self-efficacy (Dallery, Jarvis, Marsch, & Xie, 2015).
4.1 Limitations
We randomly assigned participants to study arms; however, the utilization of post-discharge outpatient addiction treatment and mutual help involved self-selection, which could introduce bias into the mediation analysis. Measures assessing risky drinking days, abstinence, and treatment utilization were not from comprehensive validated instruments, and we did not assess a broad range of services such as inpatient treatment. We opted to use single items to reduce participant burden, but measurement properties are unknown, which makes the findings harder to replicate. We measured the use of services, but not the amount of treatment use (e.g., number of outpatient sessions), which may be important to consider in future studies. While outpatient addiction treatment could have occurred in the past month at each follow-up period, we assessed mutual help attendance in the past-week using an item from a different measure to avoid duplicate questions. All measures relied upon self-report; the trial did not obtain objective measures of the outcomes (e.g., breathalyzers, medical records), though we note that several studies have found self-report to have good concordance with objective measures (Babor, Brown, & del Boca, 1990; Glass & Bucholz, 2011; Hesselbrock, Babor, Hesselbrock, Meyer, & Workman, 1983; Killeen, Brady, Gold, Tyson, & Simpson, 2004). While the analyses reduced threats to validity by exploiting the longitudinal design (Begg & Parides, 2003) and by controlling for reasons for initially entering residential treatment, threats to causal inference remain and interpretations should not be causal in nature. We may have also missed fluctuations in the predictors or outcomes due to the relatively long follow-up intervals, and because some follow-up interviews did not occur strictly at the four-month interview marks. While participants were randomized to study conditions, and while study procedures included asking counselors at the residential treatment agencies to provide care for all participants as they normally would, study arm could not be masked, making it possible that more attention was given to intervention arm participants. Rates of risky drinking were low, which could have resulted in zero-inflated distributions for the count outcome. Violation of assumptions for linear models can introduce bias. The analyses adjusted for differences in participants’ use of addiction treatment prior to entering residential treatment, but our surveys did not assess use of mutual help prior to entering residential treatment.
4.2. Conclusions
Advancing knowledge about mechanisms of behavior change in mHealth interventions is a critical step towards understanding how to best leverage these new technologies. Recently, there has been an increasing availability of mHealth applications, making it especially important to identify effective principles so that investigators can apply these broadly. Future clinical trials should investigate mHealth intervention components that could facilitate the linkage of participants to needed treatment services and promote the sustained use of these services.
Highlights.
A-CHESS, a mobile intervention, reduces drinking following residential treatment
In this study, A-CHESS also increased the use of outpatient addiction treatment
This use of outpatient treatment mediated the effects of A-CHESS on risky drinking
Appendix A
Table A.1.
Brief descriptions of the Addiction-Comprehensive Health Enhancement Support System (A-CHESS) components
| Component | Brief description |
|---|---|
| My Profile | A central location allowing the user to establish a recovery identity. Limited personal information can be displayed, a user can upload photos, and a sobriety counter (days of abstinence) is shown. |
| My Messages | A means to send private messages to other A-CHESS users. |
| Team Feed | A chronological list of what’s been going on with other members of the Support Team. Items in the list include new pictures that have been posted and new discussion group topics. |
| Support Team | Support Team allows users to look over the profiles of other A-CHESS users recruited from the same residential treatment organization. They can look at pictures, share information about interests, and links are provided to send private messages to each other. |
| Discussions | Users can exchange emotional support and information with other patients via online bulletin-board support groups. |
| Meetings | Provides time, place, date and directions to meetings (e.g., Alcoholics Anonymous, Narcotics Anonymous) in the area. |
| Panic Button | Provides in-the-moment support to help prevent a relapse. When pressed, alerts are issued to key self-identified people that help is needed, the user is presented with their own personal motivations for not drinking, and specific tools are presented to help the user deal with urges. |
| Ask An Expert | Users can pose questions and receive personal responses from experts in addiction. |
| Events | A source to learn about healthy substance-free events taking place nearby. |
| Recovery Info | Provides access to knowledge about addiction and recovery through resources such as recovery articles and links to external websites. |
| News | Provides brief summaries of recent news articles and research about addiction and provides a link to the actual article. |
| Our Stories | Audio, video or text accounts of individual and family members in recovery. |
| Recovery Podcasts | Provides access to podcasts including Alcoholics Anonymous speaker recordings and addiction talk shows. |
| Easing Distress | A program with a designed based on cognitive-behavioral therapy to help people cope with harmful thoughts that can lead to relapse. |
| Weekly Check-Ins | A brief survey to monitor negative affect, lifestyle balance, and substance use. Data is made available to counselors, who may be automatically notified if a score reaches a pre-set threshold. |
| My Settings | Allows for the customization of various A-CHESS components to facilitate autonomy in how users interact with the system. |
| Daily Check-Ins | A brief survey asking participants if they think they can make it through the day. |
| Tutorials | Tutorials provide online assistance on how to use A-CHESS. |
Appendix B
Figure B.1.
The system of equations underlying the mediation models. Preacher, Zyphur, and Zhang (2009) have named this approach the “unconflated multilevel model” implemented within a multilevel structural equation model framework.
Note:
RDD= risky drinking days, OP=post-discharge outpatient addiction treatment. An analogous approach was used for the outcome of abstinence and for the mediator of mutual help attendance.
γ1 in this figure corresponds to path c’ in Figure 1.
γ2 in this figure corresponds to path b1 in Figure 1.
γ11 in this figure corresponds to path a1 in Figure 1.
Appendix C
Table C.1.
Rates of post-discharge outpatient addiction treatment and mutual help within study arms. Supplemental data are provided showing rates of service receipt at months 8 and 12, stratified by the receipt of services at month 4.
| Outpatient addiction treatment | Mutual help | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Month 4 | Month 8 | Month 12 | Month 4 | Month 8 | Month 12 | |
|
| ||||||
| Sample size at each follow-up period % (n) receiving treatment | ||||||
| Among all participants | n = 311 | n = 297 | n = 281 | n = 298 | n = 288 | n = 279 |
|
| ||||||
| Overall | 36.0% (112) | 23.9% (71) | 19.9% (56) | 60.1% (179) | 60.1% (173) | 57.7% (161) |
| A-CHESS arm (n = 156) | 40.4% (63) | 29.5% (43) | 25.7% (35) | 63.2% (96) | 63.6% (91) | 64.7% (88) |
| Control arm (n = 155) | 31.6% (49) | 18.5% (28) | 14.5% (21) | 56.9% (83) | 56.6% (82) | 51.1% (73) |
|
| ||||||
| Among those receiving the service at month 4 | n = 112 | n = 109 | n = 103 | n = 179 | n = 162 | n = 160 |
|
| ||||||
| Overall | -- | 42.2% (46) | 28.2% (29) | -- | 82.7% (134) | 77.5% (124) |
| A-CHESS arm | -- | 48.3% (29) | 34.5% (20) | -- | 86.4% (76) | 82.6% (71) |
| Control arm | -- | 34.7% (17) | 20% (9) | -- | 78.4% (58) | 71.5% (53) |
|
| ||||||
| Among those not receiving the service at month 4 | n = 199 | n = 184 | n = 176 | n = 119 | n = 112 | n = 107 |
|
| ||||||
| Overall | -- | 13.0% (24) | 15.34% (27) | -- | 25.9% (29) | 26.2% (28) |
| A-CHESS arm | -- | 16.3% (14) | 19.2% (15) | -- | 21.6% (11) | 28.3% (13) |
| Control arm | -- | 10.2% (10) | 12.2% (12) | -- | 29.5% (18) | 25.6% (15) |
Proportions were calculated overall and within study arm among participants with complete data within each follow-up interview.
Appendix D
Table D.1.
Post-discharge outpatient addiction treatment and mutual help as mediators of the association between study arm and risky drinking days in the A-CHESS trial (n = 349). This supplement includes within-person estimates, which were omitted from manuscript Table 4 for brevity.
| Independent variable | Dependent variable | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Post-discharge outpatient addiction treatment (Mediator) | Post-discharge mutual help (Mediator) | Risky drinking days (Outcome) | Indirect effect | |||||
|
|
|
|
|
|||||
| b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | |
|
| ||||||||
| Concurrent associations - b (95% CI) | ||||||||
| Between-person associations | ||||||||
| A-CHESS (study arm) | 0.11 (0.04–0.17) | 0.002 | 0.07 (−0.01–0.15) | 0.101 | −0.60 (−1.04–−0.17) | 0.007 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | −1.16 (−1.85–−0.41) | 0.002 | −0.12 (−0.24–−0.01) | 0.035 |
| Post-discharge mutual help | -- | -- | -- | -- | −1.43 (−2.03–−0.83) | <0.001 | −0.01 (−0.22–−0.03) | 0.119 |
| Within-person associations | ||||||||
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | −1.16 (−1.97–−0.35) | 0.005 | -- | -- |
| Post-discharge mutual help | -- | -- | -- | -- | −1.48 (−2.19–−0.76) | <0.001 | -- | -- |
|
| ||||||||
| Lagged associations - b (95% CI) | ||||||||
|
| ||||||||
| Between-person associations | ||||||||
| A-CHESS (study arm) | 0.10 (0.02–0.18) | 0.018 | 0.08 (−0.05–0.17) | 0.064 | −0.63 (−1.17–−0.09) | 0.021 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | −1.34 (−2.22–−0.45) | 0.003 | −0.13 (−0.27–0.01) | 0.071 |
| Post-discharge mutual help | -- | -- | -- | -- | −1.49 (−2.19–−0.79) | <0.001 | −0.12 (−0.27–0.02) | 0.094 |
| Within-person associations | ||||||||
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | −1.34 (−2.23–−0.45) | 0.003 | -- | -- |
| Post-discharge mutual help | -- | -- | -- | -- | −0.70 (−1.60–−0.25) | 0.154 | -- | -- |
Coefficients are displayed from Mplus models computed with the maximum likelihood robust estimator. Linear regression coefficients are shown for post-discharge outpatient addiction treatment and mutual help (the dependent variable was the person-level mean of service use follow-up periods) and Poisson regression coefficients are displayed for risky drinking days. Bolded values are statistically significant (p < 0.05). Models controlled for treatment site, interview month, age, gender, race, presence of mental health problems, prior addiction treatment, and reasons for entering treatment. Race was dichotomized to white vs. other (collapsing black and other categories) due to empty bivariate cells. The multilevel structural equation model provided separate estimates for between-person estimates (i.e., person-level means of risky drinking days and addiction treatment or mutual help) and within-person estimates (i.e., within-person observations of risky drinking days and group-mean centered addiction treatment or mutual help). Between-person estimates were used to calculate the indirect effects. Within-person estimates are shown for completeness.
Appendix E
Table E.1.
Post-discharge outpatient addiction treatment and mutual help as mediators of the association between study arm and past-month abstinence in the A-CHESS trial (n = 349). This supplement includes within-person estimates, which were omitted from manuscript Table 5 for brevity.
| Independent variable | Dependent variable | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Post-discharge outpatient addiction treatment (Mediator) | Post-discharge mutual help (Mediator) | Abstinence (Outcome) | Indirect effect | |||||
|
|
|
|
|
|||||
| b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | b (95% CI) | p | |
|
| ||||||||
| Concurrent associations - b (95% CI) | ||||||||
| Between-person associations | ||||||||
| A-CHESS (study arm) | 0.11 (0.04–0.20) | 0.002 | 0.07 (−0.01–0.15) | 0.101 | 0.64 (0.20–1.26) | 0.043 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | 0.81 (−0.18–1.80) | 0.108 | 0.09 (−0.04–0.21) | 0.168 |
| Post-discharge mutual help | -- | -- | -- | -- | 1.93 (1.02–2.85) | <0.001 | 0.13 (−0.04–0.31) | 0.135 |
| Within-person associations | ||||||||
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | 0.97 (0.24–1.71) | 0.010 | -- | -- |
| Post-discharge mutual help | -- | -- | -- | -- | 1.52 (0.74–2.31) | <0.001 | -- | -- |
|
| ||||||||
| Lagged associations - b (95% CI) | ||||||||
|
| ||||||||
| Between-person associations | ||||||||
| A-CHESS (study arm) | 0.10 (0.02–0.18) | 0.018 | 0.08 (−0.01–1.71) | 0.064 | 0.85 (0.09–1.60) | 0.027 | -- | -- |
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | 0.79 (−0.34-−1.92) | 0.169 | 0.06 (−0.05–1.69) | 0.287 |
| Post-discharge mutual help | -- | -- | -- | -- | 1.87 (0.83–2.92) | <0.001 | 0.16 (−0.04–0.35) | 0.120 |
| Within-person associations | ||||||||
| Post-discharge outpatient addiction treatment | -- | -- | -- | -- | 0.58 (−0.38-−1.54) | 0.239 | -- | -- |
| Post-discharge mutual help | -- | -- | -- | -- | 0.95 (0.10–1.80) | 0.029 | -- | -- |
Coefficients are displayed from Mplus models computed with the maximum likelihood robust estimator. Linear regression coefficients are shown for post-discharge outpatient addiction treatment and mutual help (the dependent variable was the person-level mean of service use across follow-up periods) and probit regression coefficients are displayed for abstinence. Bolded values are statistically significant (p < 0.05). Models controlled for treatment site, interview month, age, gender, race, presence of mental health problems, prior addiction treatment, and reasons for entering treatment. Race was dichotomized to white vs. other (collapsing black and other categories) due to empty bivariate cells. The multilevel structural equation model provided separate estimates for between-person estimates (i.e., person-level means of abstinence and addiction treatment or mutual help) and within-person estimates (i.e., within-person observations of abstinence and group-mean centered addiction treatment or mutual help). Between-person estimates were used to calculate the indirect effects. Within-person estimates are shown for completeness.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Joseph E. Glass, Kaiser Permanente Washington Health Research Institute, Kaiser Foundation Health Plan of Washington, Seattle, WA
James R. McKay, Department of Psychiatry, Perelman School of Medicine, University of Pennsylvania; and Philadelphia Veterans Affairs Medical Center, Philadelphia, PA
David H. Gustafson, Center for Health Enhancement Systems Studies, College of Engineering, University of Wisconsin-Madison, Madison, WI
Rachel Kornfield, Mass Communication Research Center, School of Journalism and Mass Communication, University of Wisconsin-Madison, Madison, WI
Paul J. Rathouz, Department of Biostatistics and Medical Informatics, University of Wisconsin-Madison, Madison, WI
Fiona M. McTavish, Center for Health Enhancement Systems Studies, College of Engineering, University of Wisconsin-Madison, Madison, WI
Amy K. Atwood, Center for Health Enhancement Systems Studies, College of Engineering, University of Wisconsin-Madison, Madison, WI
Andrew Isham, Center for Health Enhancement Systems Studies, College of Engineering, University of Wisconsin-Madison, Madison, WI
Andrew Quanbeck, Center for Health Enhancement Systems Studies, College of Engineering, University of Wisconsin-Madison, Madison, WI
Dhavan Shah, Mass Communication Research Center, School of Journalism and Mass Communication, University of Wisconsin-Madison, Madison, WI
References
- Babor TF, Brown J, del Boca FK. Validity of self-reports in applied research on addictive behaviors: fact or fiction? Behavioral Assessment. 1990;12(1):5–31. [Google Scholar]
- Begg MD, Parides MK. Separation of individual-level and cluster-level covariate effects in regression analysis of correlated data. Statistics in Medicine. 2003;22(16):2591–2602. doi: 10.1002/sim.1524. https://doi.org/10.1002/sim.1524. [DOI] [PubMed] [Google Scholar]
- Blodgett JC, Maisel NC, Fuh IL, Wilbourne PL, Finney JW. How effective is continuing care for substance use disorders? A meta-analytic review. Journal of Substance Abuse Treatment. 2014;46(2):87–97. doi: 10.1016/j.jsat.2013.08.022. https://doi.org/10.1016/j.jsat.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth BM, Curran GM, Han X, Edlund MJ. Criminal justice and alcohol treatment: results from a national sample. Journal of Substance Abuse Treatment. 2013;44(3):249–255. doi: 10.1016/j.jsat.2012.07.008. https://doi.org/10.1016/j.jsat.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Dephilippis D, Drapkin ML, Valadez C, Jr, Fala NC, … McKay JR. Development and initial evaluation of the Brief Addiction Monitor (BAM) Journal of Substance Abuse Treatment. 2013;44(3):256–263. doi: 10.1016/j.jsat.2012.07.013. https://doi.org/10.1016/j.jsat.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Dziak JJ, Kugler KC, Trail JB. Factorial experiments: efficient tools for evaluation of intervention components. American Journal of Preventive Medicine. 2014;47(4):498–504. doi: 10.1016/j.amepre.2014.06.021. https://doi.org/10.1016/j.amepre.2014.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Jarvis B, Marsch L, Xie H. Mechanisms of change associated with technology-based interventions for substance use. Drug and Alcohol Dependence. 2015;150:14–23. doi: 10.1016/j.drugalcdep.2015.02.036. https://doi.org/10.1016/j.drugalcdep.2015.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedert EA, McDuffie JR, Stein R, McNiel JM, Kosinski AS, Freiermuth CE, … Williams JW. Electronic Interventions for Alcohol Misuse and Alcohol Use Disorders: A Systematic Review. Annals of Internal Medicine. 2015;163(3):205. doi: 10.7326/M15-0285. https://doi.org/10.7326/M15-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Bucholz KK. Concordance between self-reports and archival records of physician visits: a case-control study comparing individuals with and without alcohol use disorders in the community. Drug and Alcohol Dependence. 2011;116(1–3):57–63. doi: 10.1016/j.drugalcdep.2010.11.021. https://doi.org/10.1016/j.drugalcdep.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Grant JD, Yoon HY, Bucholz KK. Alcohol problem recognition and help seeking in adolescents and young adults at varying genetic and environmental risk. Drug and Alcohol Dependence. 2015;153:250–257. doi: 10.1016/j.drugalcdep.2015.05.006. https://doi.org/10.1016/j.drugalcdep.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Perron BE, Ilgen MA, Chermack ST, Ratliff S, Zivin K. Prevalence and correlates of specialty substance use disorder treatment for Department of Veterans Affairs Healthcare System patients with high alcohol consumption. Drug and Alcohol Dependence. 2010;112(1–2):150–5. doi: 10.1016/j.drugalcdep.2010.06.003. https://doi.org/10.1016/j.drugalcdep.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, DuBenske LL, Namkoong K, Hawkins R, Chih MY, Atwood AK, … Cleary JF. An eHealth system supporting palliative care for patients with non-small cell lung cancer: A randomized trial. Cancer. 2013;119(9):1744–1751. doi: 10.1002/cncr.27939. https://doi.org/10.1002/cncr.27939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, McTavish F, Pingree S, Chen WC, Volrathongchai K, … Serlin RC. Internet-Based Interactive Support for Cancer Patients: Are Integrated Systems Better? Journal of Communication. 2008;58(2):238–257. doi: 10.1111/j.1460-2466.2008.00383.x. https://doi.org/10.1111/j.1460-2466.2008.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins RP, Boberg EW, McTavish F, Owens B, Wise M, … Pingree S. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. International Journal of Medical Informatics. 2002;65(3):169–177. doi: 10.1016/s1386-5056(02)00048-5. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih MY, Atwood AK, Johnson RA, Boyle MG, … Shah D. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):566–572. doi: 10.1001/jamapsychiatry.2013.4642. https://doi.org/10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Stengle W, Ballard D, Jones E, Julesberg K, … Hawkins R. Reducing the Digital Divide for Low-income Women With Breast Cancer: A Feasibility Study of a Population-Based Intervention. Journal of Health Communication. 2005;10(sup1):173–193. doi: 10.1080/10810730500263281. https://doi.org/10.1080/10810730500263281. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, Shaw BR, Isham A, Baker T, Boyle MG, Levy M. Explicating an Evidence-Based, Theoretically Informed, Mobile Technology-Based System to Improve Outcomes for People in Recovery for Alcohol Dependence. Substance Use & Misuse. 2011;46(1):96–111. doi: 10.3109/10826084.2011.521413. https://doi.org/10.3109/10826084.2011.521413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Wise M, Bhattacharya A, Pulvermacher A, Shanovich K, Phillips B, … Kim J-S. The effects of combining Web-based eHealth with telephone nurse case management for pediatric asthma control: a randomized controlled trial. Journal of Medical Internet Research. 2012;14(4):e101. doi: 10.2196/jmir.1964. https://doi.org/10.2196/jmir.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock M, Babor TF, Hesselbrock V, Meyer RE, Workman K. “Never believe an alcoholic”? On the validity of self-report measures of alcohol dependence and related constructs. The International Journal of the Addictions. 1983;18(5):593–609. doi: 10.3109/10826088309027359. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Price AM, Burnett-Zeigler I, Perron B, Islam K, Bohnert AS, Zivin K. Longitudinal predictors of addictions treatment utilization in treatment-naïve adults with alcohol use disorders. Drug and Alcohol Dependence. 2011;113(2–3):215–221. doi: 10.1016/j.drugalcdep.2010.08.006. https://doi.org/10.1016/j.drugalcdep.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD. The role of mutual-help groups in extending the framework of treatment. Alcohol Research & Health: The Journal of the National Institute on Alcohol Abuse and Alcoholism. 2011;33(4):350–355. [PMC free article] [PubMed] [Google Scholar]
- Killeen TK, Brady KT, Gold PB, Tyson C, Simpson KN. Comparison of self-report versus agency records of service utilization in a community sample of individuals with alcohol use disorders. Drug and Alcohol Dependence. 2004;73(2):141–147. doi: 10.1016/j.drugalcdep.2003.09.006. https://doi.org/S0376871603002837 [pii] [DOI] [PubMed] [Google Scholar]
- Labrique A, Vasudevan L, Kochi E, Fabricant R, Mehl G. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Global Health: Science and Practice. 2013;1(2):160–71. doi: 10.9745/GHSP-D-13-00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks, CA: Sage Publications, Inc; 1997. [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. New York: Erlbaum Psych Press; 2008. [Google Scholar]
- McClure JB, Peterson D, Derry H, Riggs K, Saint-Johnson J, Nair V, … Shortreed SM. Exploring the “active ingredients” of an online smoking intervention: a randomized factorial trial. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2014;16(8):1129–1139. doi: 10.1093/ntr/ntu057. https://doi.org/10.1093/ntr/ntu057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100(11):1594–610. doi: 10.1111/j.1360-0443.2005.01208.x. https://doi.org/ADD1208 [pii] [DOI] [PubMed] [Google Scholar]
- McKay JR. Continuing care research: what we have learned and where we are going. Journal of Substance Abuse Treatment. 2009;36(2):131–45. doi: 10.1016/j.jsat.2008.10.004. https://doi.org/S0740-5472(08)00180-3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–95. doi: 10.1001/jama.284.13.1689. https://doi.org/jsc00024 [pii] [DOI] [PubMed] [Google Scholar]
- McTavish FM, Chih MY, Shah D, Gustafson DH. How Patients Recovering From Alcoholism Use a Smartphone Intervention. Journal of Dual Diagnosis. 2012;8(4):294–304. doi: 10.1080/15504263.2012.723312. https://doi.org/10.1080/15504263.2012.723312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D, Burns M, Schueller S, Clarke G, Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. General Hospital Psychiatry. 2013;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- Nelson KG, Young K, Chapman H. Examining the performance of the brief addiction monitor. Journal of Substance Abuse Treatment. 2014;46(4):472–481. doi: 10.1016/j.jsat.2013.07.002. https://doi.org/10.1016/j.jsat.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. https://doi.org/10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods. 2010;15(3):209–233. doi: 10.1037/a0020141. https://doi.org/10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. The American Psychologist. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp, LP; 2015. [Google Scholar]