Abstract
Background
Prosthetic breast reconstruction rates have risen in the U.S. while autologous techniques have stagnated. Meanwhile, single institution data demonstrate that physician payments for prosthetic reconstruction are rising, whereas payments for autologous reconstruction are unchanged. This study aims to assess payment trends and variation for tissue expander and free flap breast reconstruction.
Methods
The Blue Health Intelligence (Blue Cross/Blue Shield) database was queried from 2009–2013, identifying women with claims for breast reconstruction. Trends in the incidence of surgery and physician reimbursement were characterized by method and year using regression models.
Results
21,259 episodes of breast reconstruction occurred, with a significant rise in tissue expander cases (incidence rate ratio (IRR) 1.09, p<0.001) and unchanged incidence in free flap cases (IRR 1.02, p=0.222). Bilateral tissue expander cases reimbursed 1.32 times more than unilateral tissue expanders, whereas bilateral free flaps reimbursed 1.61 times more than unilateral variants. The total growth in adjusted tissue expander mean payments was 6.5%($2,232 to $2,378) compared to −1.8%($3,858 to $3,788) for free flaps. Linear modeling showed significant increases for tissue expander reimbursements only. Surgeon payments varied more for free flaps; 25–75th interquartile range was $2,243 for free flaps vs. $987 for tissue expanders.
Conclusion
The incidence of tissue expander cases and reimbursements rose over a period where the incidence of free flap cases and reimbursements plateaued. Patient demand for prosthetic reconstruction may be one underlying factor. Reasons for stagnation in free flap incidence are unclear; however, the opportunity cost of performing this procedure may incentivize the alternative technique. Greater payment variation in autologous reconstruction suggests opportunity for negotiation with payers.
Intro
Breast reconstruction has steadily increased in the United States over the past two decades with a notable rise in prosthetic techniques(1). Evidence suggests at least part of this trend is explained by increasing bilateral reconstructions in the setting of contralateral prophylactic mastectomy as well as decreased relative contraindications for implants in traditionally high-risk patients (1)(2)(3). In contrast, the slower growth of autologous transfer has not been adequately explained. Aside from patient related factors and preference, some have questioned whether physician reimbursement may present a barrier to autologous reconstruction(2). Increased operative labor with the advent of perforator flaps, longer surgical times, and specialized postoperative care distinguish autologous reconstruction. Considering these factors, prosthetic reconstruction reimburses considerably more per hour of surgeon time (4).
Single institution data demonstrate that physician payments have stagnated for autologous transfer while payments have risen for prosthetic reconstruction (4). This observation begs further substantiation from a multi-state claims database. The current study aims to describe variation in physician payment for both implant and autologous methods over time. We hypothesize that the payment disparity between implant and autologous techniques is increasing.
Methods
The Blue Health Intelligence (Blue Cross/Blue Shield, BHI)(5), a national commercial claim-based database, was queried for the period of 2009–2013. Included subjects consisted of all women aged 18 or older with a claim filed for breast reconstruction. Current procedural terminology (CPT) codes were used to identify the method of reconstruction using 19357 & 11970 for tissue expanders (TE) and 19364 for free-flap based reconstruction (FF). Modifier 50 was used to identify bilateral procedures. Both immediate and delayed reconstructions were included. Patients with pedicled flaps, hybrid reconstructions, and unknown claim status were excluded.
Episodes of reconstruction were sorted by method, laterality, physician payment, and year of service. The yearly incidence of breast reconstruction was trended over the five-year period using Poisson regression, reporting incidence rate ratios (IRR). In addition, the ratios of TE to FF cases were compared to assess relative growth for any given year. Physician payment trends were analyzed using linear regression. In order to compare physician reimbursements at the aggregate level of TE or FF, bilateral reimbursements were adjusted to an equivalent unilateral payment, given that bilateral cases reimbursed less than twice the unilateral amount. This multiplicative factor was determined for TE and FF cases after comparing all payments over the five-year period. To account of inflation, all reimbursements were transformed into 2013 dollars using the consumer price index (CPI) per the Bureau of Labor Statistics (6).
To illustrate payment variations between the two methods, the magnitude and shape of payment variations were displayed with whisker box plots. Coefficients of variation were determined by dividing the standard deviation of physician payments by the mean. Statistical analyses were completed with Stata 14 (Stata Corp LLC. College Station Texas, USA). All statistical tests were considered significant for p values less than 0.05. The following study was exempt from institutional review board evaluation.
Results
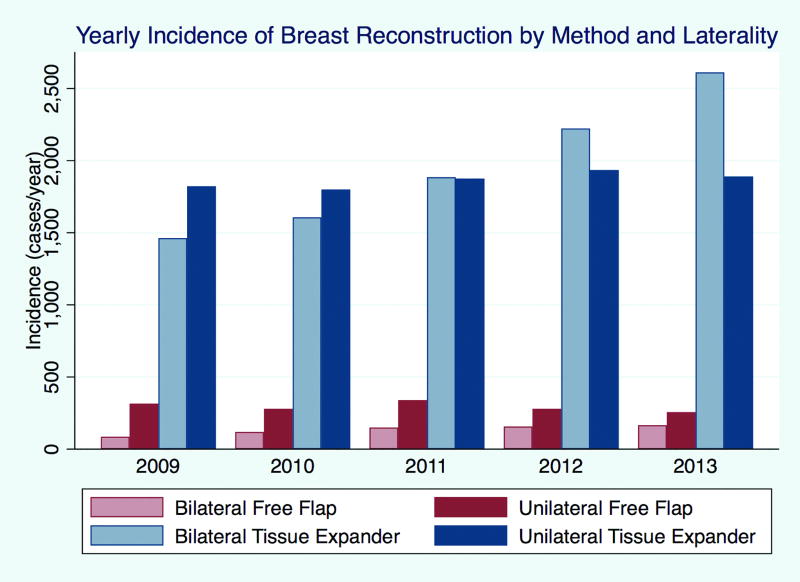
During the five-year study period, there were 21,259 episodes of breast reconstruction, growing from 3,686 cases/year in 2009 to 4,924 cases/year in 2013 (Table 1, Figure 1). TE cases saw a significant increase with an IRR of 1.09 (p<0.001) compared to no appreciable change in FF cases with an IRR of 1.02, (p=0.222). Parsing by laterality, the incidence of both unilateral and bilateral TE cases increased with an IRR of 1.01 (p=0.047) and 1.16 (p<0.001) respectively. Though the overall FF incidence did not increase, when stratifying by laterality, bilateral cases increased with an IRR of 1.16 (p<0.001). Thus, unilateral FF cases declined over the period with an IRR of 0.96 (p=0.030). Unilateral TE cases had the greatest incidence in the early study period of 2009 at 1,822 cases/year; however, by 2011, bilateral TE cases became the most frequent operation at 2,223 cases/year. For FF cases, the incidence of unilateral reconstructions was greater than bilateral for all years, although the gap narrowed each year. Comparing the growth of TE relative to FF cases, the ratio of TE/FF cases increased by 30.3% (8.19 to 10.67). This trend held true selecting for unilateral cases (27.7% gain in TE), but showed the opposite trend for bilateral cases whereby there was a relative gain in bilateral FF to bilateral TE by 7.5%.
Table 1.
Incidence of Breast Reconstruction by Method and Laterality
| Method & Laterality | Year | Total | IRR (95% CI) | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | ||||
| TE unilateral | 1,822 | 1,800 | 1,875 | 1,935 | 1,890 | 9,322 | 1.01 (1.00—1.03) | 0.047 |
| TE bilateral | 1,463 | 1,607 | 1,885 | 2,223 | 2,612 | 9,790 | 1.16 (1.15—1.18) | <0.001 |
| TE total | 3,285 | 3,407 | 3,760 | 4,158 | 4,502 | 19,112 | 1.09 (1.08—1.10) | <0.001 |
|
| ||||||||
| FF unilateral | 315 | 279 | 340 | 279 | 256 | 1,469 | 0.96 (0.93—0.99) | 0.030 |
| FF bilateral | 86 | 119 | 150 | 157 | 166 | 678 | 1.16 (1.10—1.22) | <0.001 |
| FF total | 401 | 398 | 490 | 436 | 422 | 2,147 | 1.02 (0.99—1.05) | 0.222 |
|
| ||||||||
| Ratio TE/FF | Average | 5-year growth | ||||||
|
| ||||||||
| Total | 8.19 | 8.56 | 7.67 | 9.54 | 10.67 | 8.90 | 30.3% | - |
| Unilateral | 5.78 | 6.45 | 5.51 | 6.94 | 7.38 | 6.35 | 27.7% | - |
| Bilateral | 17.01 | 13.50 | 12.57 | 14.16 | 15.73 | 14.44 | −7.5% | - |
IRR, Incidence Rate Ratio; CI, Confidence Interval; TE, tissue expander; FF free flap
Figure 1.
Yearly Incidence of Breast Reconstruction by Method and Laterality. Bar graph demonstrating yearly incidence of breast reconstruction parsed by method and laterality
Looking at physician reimbursements per case per year, unilateral and bilateral TE mean physician payments increased over the five year period (Table 2). Unilateral TE mean physician payments increased by 8.01% ($2,209/case to $2,386/case) compared to bilateral TE mean payments at 4.7% ($2,979/case to $3,120/case) over the five-year period. For bilateral FF mean physician payments, there were bidirectional changes over the interval, with a peak in 2012 at $6,398/case; the overall five-year growth was −7.5% ($6,228/case to $5,762/case). Unilateral FF mean payments experienced a 1.8% overall increase at five years ($3,859/case to $3,930/case).
Table 2.
Physician Payments of Reconstructive Method and Laterality by Year
| Method & Laterality |
Mean by Year | *p-value | Total Mean |
Total Median |
25th—75th percentile |
||||
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2013 | |||||
| TE unilateral | $2,209 | $2,334 | $2,312 | $2,410 | $2,386 | <0.001 | $2,331 | $2,137 | $1,655—2,652 |
| TE bilateral | $2,979 | $3,087 | $3,010 | $3,033 | $3,120 | 0.018 | $3,052 | $2,847 | $2,170—3,483 |
| TE total (adjusted) | $2,232 | $2,339 | $2,300 | $2,354 | $2,378 | <0.001 | $2,326 | $2,152 | $1,670—2,657 |
|
| |||||||||
| FF unilateral | $3,859 | $3,848 | $3,832 | $3,733 | $3,930 | 0.443 | $3,839 | $2,543 | $1,771—4,016 |
| FF bilateral | $6,228 | $6,133 | $6,314 | $6,398 | $5,762 | 0.761 | $6,156 | $3,060 | $2,107—5,486 |
| FF total (adjusted) | $3,858 | $3,834 | $3,856 | $3,816 | $3,788 | 0.422 | $3,831 | $2,239 | $1,569—3,812 |
|
| |||||||||
| Ratio of mean payments TE/FF | 5 year growth | ||||||||
|
| |||||||||
| Unilateral | 0.57 | 0.61 | 0.60 | 0.65 | 0.61 | 6.1% | 0.61 | 0.84 | |
| Bilateral | 0.48 | 0.50 | 0.48 | 0.47 | 0.54 | 13.2% | 0.50 | 0.93 | |
| Total (adjusted) | 0.58 | 0.61 | 0.60 | 0.62 | 0.63 | 8.5% | 0.61 | 0.96 | |
p-value for linear regression of payments per case per year over five-year period
Monetary values reflective of US 2013 dollars
IQR, interquartile range (difference between 75th and 25th percentiles)
TE, tissue expander; FF free flap
In order to compare TE and FF payments in aggregate regardless of laterality, bilateral cases were normalized to unilateral dollars based on an actuarial multiplicative factor. Bilateral TE cases reimbursed 1.32 times more than unilateral cases, while bilateral FF cases reimbursed 1.61 times more than unilateral cases. After adjustment, the total growth in TE mean physician payments was 6.5% ($2,232 to $2,378) compared with −1.8% ($3,858 to $3,788) for FF mean payments. Comparing the growth of mean physician payments for TE cases relative to FF cases, there was a 8.4% increase (0.58 to 0.63).
Linear modeling of physician payments per case per year showed significant increases for total TE reimbursements (p<0.001); this held true even when stratifying laterality (unilateral p<0.001, bilateral p=0.018). Normalized FF payments showed no significant growth, (p=0.422), which was factual even when parsing laterality (unilateral p=0.443, bilateral p=0.442) (Table 2).
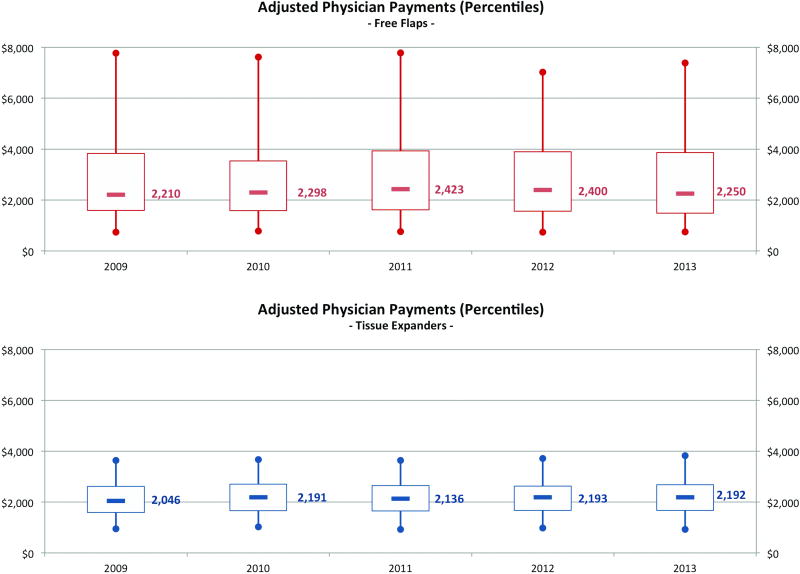
Examining differences across all physician payments by year demonstrated greater variation for FF compared to TE payments (Figure 2). The overall coefficient of variation was considerably lower for TE payments at 0.59 compared to 1.08 for FF payments. Both payment distributions were rightward skewed towards higher payments; however, FF payments showed a greater deviation. The overall interquartile range (25th to 75th) for FF payments was greater at $2,243 compared to $987 for TE payments.
Figure 2.
Adjusted Physician Payment Distributions by Method and Year. Yearly percentiles for physician payments. Bilateral payments are adjusted to unilateral for normalized comparison. Whiskers represent 5th and 95th percentiles; boxes represent 25th and 75th percentiles; and hash lines represent medians.
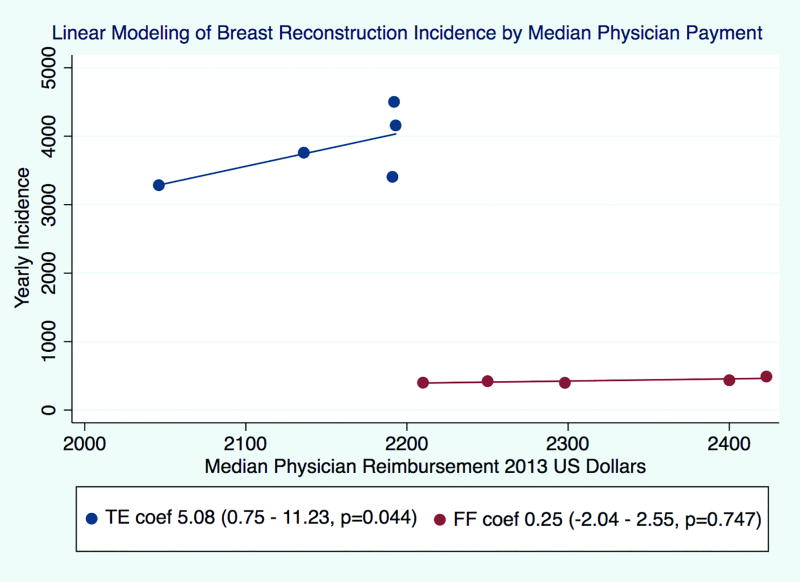
Finally, determining whether adjusted median physician payments were associated with the incidence of reconstructive method, linear models showed a significant trend for median TE payments (coefficient 5.08, 95% confidence interval 0.75 – 11.23, p=0.044) (Figure 3). There was no correlation with the incidence of FF cases and median physician payments for FF cases (coefficient 0.25, 95% confidence interval −2.04 – 2.55), p=0.747).
Figure 3.
Linear Modeling of Breast Reconstruction Incidence & Median Physican Payment. Scatter plot of breast reconstruction incidence versus median physician payment with linear model. FF, free flaps represented with red squares. TE, tissue expanders represented with blue dots. Median physician payments are adjusted for laterality such that bilateral cases are transformed into unilateral equivalent payment. P-value represents significance of linear model.
Discussion
Data from the BHI claims database mirror findings of national outcomes datasets(7)(8)showing an overall increase in the incidence of breast reconstruction with a simultaneous rise in both prosthetic and bilateral variants. For the first time, there is documentation of bilateral TE cases surpassing unilateral TE reconstructions—a finding that likely correlates with a well-documented expansion in nationwide rates of contralateral prophylactic mastectomy(9). While FF cases grew in total over the period, only the subset of bilateral FF cases increased significantly. Further, the change in case mix between TE and FF showed continual relative gains for TE cases, nearing a 11:1 ratio to autologous flaps in the late study period.
This is the first published national claims analysis looking at physician payments—not charges—for the two most common methods of immediate breast reconstruction. The results support prior single institution data showing a rise in surgeon payments for TE cases with stagnation in payments for FF cases(4). The BHI data paralleled this with both unilateral and bilateral TE mean physician payments increasing significantly over the study period, while FF payments, regardless of laterality, showed no significant changes. Payment variation per case, as expressed by the coefficient of variation and interquartile ranges, was much greater for FF cases than TEs, demonstrating wide disparities in flap reimbursements.
Associations between surgery incidence and payment (Figure 3) should be interpreted cautiously as causality may run in either direction, depending on interpretation of economic factors. Considering neoclassical economic theory(10), the rising TE incidence was found to correlate with rising payments, implying TE demand may be driving the payment increase. This is substantiated by consideration of other relevant economic factors, such as the stable supply of reconstruction surgeons(11). Thus, the supply curve is likely unchanged against rising demand. An important non-market force which impacts physician reimbursements is the Revenue Value Unit (RVU) schedules proposed by the American Medical Association’s Relative Value Scale Update Committee (RUC)(12). While this study examined a commercial payer, Medicare fee schedules often directly influence commercial rates (13). Interestingly, in this claims database, TE payments rose despite no corresponding increase to the RVU schedule. There was actually a decline in the RVUs for TE cases in 2010 from 21.07 to 18.50, suggesting that the rise in reimbursement documented herein has resulted principally from market forces(14).
The implications for FF reconstruction and associated physician payments are less clear. The absent growth in the incidence of FF cases or FF payments implies market equilibrium. Thus, a balance in supply and demand is the most parsimonious cause for price stability, with other explanations such as price ceilings unlikely (15). Similar to considerations for TE payment trends, there is no evidence to indicate fluctuations in the supply of reconstructive surgeons (11). In fact, it could be argued that the shift to perforator flaps has lead to an inadequate supply of microsurgeons as a cause for the relatively low case number, but this would only serve to raise payments. Looking at non-market influences on physician payment, there was no change in the RVU schedule for FF reconstructions over the study period. The RVU schedule showed a slight bump in 2009 from 42.40 to 42.58 with no changes thereafter (14).
The choice of reconstruction method does not occur in a vacuum, as surgeons help patients decide on the best operation in a shared decision-making process(16). The current pattern of rising prosthetic reconstruction is well supported by patient interest in prosthetic techniques. Features that favor implants include but are not limited to: greater requests for bilateral reconstructions, patient desire for shorter recovery, and decreasing relative contraindications, such as radiation (1)(2)(3). Despite these patient-driven factors, the relative increase in payments for prosthetic reconstruction could persuade surgeons to favor this operation all things being equal. Single institution data(17) showed a considerable financial disparity between prosthetic and autologous reconstruction relative to operative labor; delayed prosthetic reconstruction reimbursed over eight times more per hour of operative time than delayed autologous free tissue transfer. Although the current study did not account for office related procedures in the 90-day global period, including the physician time required to perform tissue expansion, the hourly TE reimbursement was many factors greater than autologous reconstruction. Furthermore, no consideration was given to the additional revenue obtained from exchanging tissue expanders to permanent implants. Therefore, it is plausible that at some remuneration threshold the opportunity cost of providing autologous reconstruction could sway surgeons to consider the alternative method.
Ways to ensure autologous tissue remains widely available include both policy and market considerations. Looking to policy, suggestions include adopting value-based payment models that reimburse based on quality outcomes, such as the Breast-Q, appreciating that autologous reconstruction has demonstrated greater long-term patient satisfaction (18). Simultaneously, these outcomes must be reliably communicated to patients who choose between breast reconstruction techniques. Additionally, update of the current RVU schedule for FF, could be achieved through surveys to ensure current reimbursement accurately reflects time and effort.
Non-policy considerations could leverage the wide variation in FF payments shown in this study. Reconstructive microsurgeons received payments that varied by $2,243 between the 25th and 75th percentiles. Though this analysis considered the BHI database in aggregate, in reality the BHI is comprised of over 120 unique markets, which may be sensitive to varying patient and physician preferences for FF cases. Moreover the greater variation in payments for FFs can be seen in a positive light, suggesting there is room for negotiations between payers and providers to remunerate the increased labor for FFs.
Limitations
Interpretations of this study are generated by a single commercial payer and thus represent a potential source of sample bias. Multiple commercial payers exist throughout the US and participate to varying degrees in markets. In addition, the-demographic profile of patients represented in the database may not accurately reflect the current profile of patients who comprise U.S. breast reconstruction. That said, the BHI database includes 165 million Americans (nearly half of the US), representing a significant sample of the US population(5). Regarding determinations of statistical significance, our data was modeled using Poisson and linear regression. Given the short time horizon, these trends could be altered by market fluctuations in subsequent years. For the payment data, only linear functions were assessed, which were reasonable approximations given the data distribution; however, it is also possible that the five year snap shot is part of a greater non-linear function. By definition, this study cannot analyze data outside the captured interval.
Many assumptions are required to apply market equilibrium theory to breast reconstruction volume and payment, notably a direct relationship between the consumer (patient) and supplier (surgeon) needs to be present. Third-party payers (e.g. commercial insurance) intermediate the exchange of payments, which confounds the ability of patient demand to directly influence payments. Further, health economists have written extensively(19) on the limitations of treating patients as rational consumers given significant information asymmetries and the ability of physicians to induce demand(20). Nonetheless, patient demand can still affect payments through insurers competing for physician contracts(15).
Conclusion
Use of a commercial claims database demonstrates that TE reimbursements increased over a period during which reimbursements for FF plateaued, perhaps reflective of greater demand for prosthetic techniques. Stagnation in autologous reconstruction payments could at some point perversely promote the alternative technique if the opportunity cost of performing these procedures is too great. Large payment variations documented for autologous reconstruction represent an opening for negotiation with payers that should be bolstered by objective quality data from patient-reported outcomes. Further investigations exploring economic drivers of reconstructive method are needed to ensure equitable access to all reconstructive methods.
Acknowledgments
This research was funded in part though the NIH/NCI Cancer Center Support Grant P30 CA008748
Footnotes
Financial Disclosure: None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References
- 1.Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013 Jan;131(1):15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 2.Farhangkhoee H, Matros E, Disa J. Trends and concepts in post-mastectomy breast reconstruction. J Surg Oncol. 2016 Jun;113(8):891–4. doi: 10.1002/jso.24201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albornoz CR, Cordeiro PG, Pusic AL, McCarthy CM, Mehrara BJ, Disa JJ, et al. Diminishing relative contraindications for immediate breast reconstruction: a multicenter study. J Am Coll Surg. 2014 Oct;219(4):788–95. doi: 10.1016/j.jamcollsurg.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Alderman AK, Storey AF, Nair NS, Chung KC. Financial Impact of Breast Reconstruction on an Academic Surgical Practice. Plast Reconstr Surg. 2009 May;123(5):1408–13. doi: 10.1097/PRS.0b013e3181a0722d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. [cited 2017 Apr 21];Blue Health Intelligence [Internet] Available from: https://bluehealthintelligence.com/markets/life-sciences/index.html.
- 6.Consumer Price Index (CPI). Bureau of Labor Statistics (BLS) [cited 2017 Sep 19];United States Department of Labor. [Internet] Available from: https://www.bls.gov/cpi/
- 7.Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM. Breast reconstruction after mastectomy: A ten-year analysis of trends and immediate postoperative outcomes. Breast Edinb Scotl. 2017 Apr;32:7–12. doi: 10.1016/j.breast.2016.11.023. [DOI] [PubMed] [Google Scholar]
- 8.Cemal Y, Albornoz CR, Disa JJ, McCarthy CM, Mehrara BJ, Pusic AL, et al. A paradigm shift in U.S. breast reconstruction: Part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013 Mar;131(3):320e–6e. doi: 10.1097/PRS.0b013e31827cf576. [DOI] [PubMed] [Google Scholar]
- 9.Nash R, Goodman M, Lin CC, Freedman RA, Dominici LS, Ward K, et al. State Variation in the Receipt of a Contralateral Prophylactic Mastectomy Among Women Who Received a Diagnosis of Invasive Unilateral Early-Stage Breast Cancer in the United States, 2004–2012. JAMA Surg. 2017 Mar 29; doi: 10.1001/jamasurg.2017.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marshall A. Principles of Economics: An Introductory Volume [Internet] Rochester, NY: Social Science Research Network; 1927. [cited 2017 Apr 21]. Report No.: ID 1496227. Available from: https://papers.ssrn.com/abstract=1496227. [Google Scholar]
- 11.Rohrich RJ, McGrath MH, Lawrence WT, Ahmad J American Society of Plastic Surgeons Plastic Surgery Workforce Task Force. Assessing the plastic surgery workforce: a template for the future of plastic surgery. Plast Reconstr Surg. 2010 Feb;125(2):736–46. doi: 10.1097/PRS.0b013e3181c830ec. [DOI] [PubMed] [Google Scholar]
- 12.Revenue Value Scale (RVS) Update Committee | RUC |. [cited 2017 Aug 14];American Medical Association. [Internet] Available from: https://www.ama-assn.org/rvs-update-committee-ruc.
- 13.Franzini L, Mikhail OI, Zezza M, Chan I, Shen S, Smith JD. Comparing variation in Medicare and private insurance spending in Texas. Am J Manag Care. 2011 Dec 1;17(12):e488–495. [PubMed] [Google Scholar]
- 14. [cited 2017 May 9];Overview of the Medicare Physician Fee Schedule Search [Internet] Available from: https://www.cms.gov/apps/physician-fee-schedule/
- 15.Ellis RP, McGuire TG. Supply-Side and Demand-Side Cost Sharing in Health Care. J Econ Perspect. 1993;7(4):135–51. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- 16.Lee CN-H, Deal AM, Huh R, Ubel PA, Liu Y-J, Blizard L, et al. Quality of Patient Decisions About Breast Reconstruction After Mastectomy. JAMA Surg. 2017 Aug 1;152(8):741–8. doi: 10.1001/jamasurg.2017.0977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sando IC, Chung KC, Kidwell KM, Kozlow JH, Malay S, Momoh AO. Comprehensive Breast Reconstruction in an Academic Surgical Practice: An Evaluation of the Financial Impact. Plast Reconstr Surg. 2014 Dec;134(6):1131–9. doi: 10.1097/PRS.0000000000000757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pusic AL, Matros E, Fine N, Buchel E, Gordillo GM, Hamill JB, et al. Patient-Reported Outcomes 1 Year After Immediate Breast Reconstruction: Results of the Mastectomy Reconstruction Outcomes Consortium Study. J Clin Oncol Off J Am Soc Clin Oncol. 2017 Aug 1;35(22):2499–506. doi: 10.1200/JCO.2016.69.9561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zweifel P, Breyer F, Kifmann M. Health Economics. Springer Science & Business Media; 2009. p. 539. [Google Scholar]
- 20.Fuchs VR. The supply of surgeons and the demand for operations. J Hum Resour. 1978;13(Suppl):35–56. [PubMed] [Google Scholar]