Abstract
Obesity remains a persistent public health and health disparity concern in the United States. Eliminating health disparities, particularly among racial/ethnic minority groups, is a major health priority in the US. The primary aim of this review was to evaluate representation of racial/ethnic sub-group members in behavioral weight loss interventions conducted among adults in the United States. The secondary aims were to assess recruitment and study design approaches to include racial/ethnic groups and the extent of racial/ethnic sub-group analyses conducted in these studies. PubMed, PsycInfo, Medline, and CINAHL were searched for behavioral weight loss intervention trials conducted in 2009–2015 using keywords: weight, loss, overweight, obese, intervention and trial. Most of the 94 studies included a majority of White participants compared to any other racial/ethnic group. Across the included studies, 58.9% of participants were White, 18.2% were African American, 8.7% were Hispanic/Latino, 5.0% were Asian and 1.0% were Native Americans. An additional 8.2% were categorized as “Other”. Nine of the 94 studies exclusively included minority samples. Lack of adequate representation of racial and ethnic minority populations in behavioral trials limits the generalizability and potential public health impact of these interventions to groups that might most benefit from weight loss. Given racial/ethnic disparities in obesity rates and the burden of obesity and obesity-related diseases among minority groups in the United States, greater inclusion in weight loss intervention studies is warranted.
Keywords: Weight loss, Intervention, Review, Minority health, Race/ethnicity
Highlights
-
•
Describes racial/ethnic minority inclusion in behavioral weight loss studies
-
•
Majority of studies continue to include a majority white sample.
-
•
Modest increases in the representation of some racial/ethnic minority groups.
-
•
Lack of adequate representation of minority groups limits generalizability.
-
•
Greater racial/ethnic inclusion in weight loss intervention studies is warranted.
1. Introduction
Eliminating health disparities in chronic conditions such as obesity, particularly among racial/ethnic minority groups, is a major health priority in the United States (U.S.) (Koh et al., 2011; U.S. Department of Health and Human Services, 2013). Health disparities is defined as differences ins health outcomes related to social, economic, or environmental disadvantage that negatively affect groups of people (National Partnership for Action, n.d.). Over one third (38%) of American adults are obese, with disproportionately higher rates of obesity among Latinos (42.7%), African Americans (48.5%) and Alaskan Natives/Native Americans (43.7%) (Flegal et al., 2016; Ogden et al., 2015; Centers for Disease Control, 2015). These estimates exceed those of non-Latino Whites (37.1%) and Asian Americans (12.7%) (Ogden et al., 2015). Racial/ethnic minority groups in the U.S. also face a higher burden of obesity-related diseases including cardiovascular disease, diabetes, and certain cancers (Frieden, 2013).
Achieving and sustaining healthy weight loss can reduce health problems and co-morbidities associated with obesity among burdened racial/ethnic groups (Guh et al., 2009; Cossrow and Falkner, 2004). Research suggests that a weight loss of 5% among obese adults can prevent or delay health problems caused by obesity (Pasanisi et al., 2001; Norman et al., 2003; Knowler et al., 2002), and even very modest weight loss may contribute to important health improvements (Ockene et al., 2012). Several key meta-analyses have shown that obesity treatment through behavioral interventions focused on diet and physical activity can produce significant and clinically meaningful short-term (i.e., six months) (Franz et al., 2007) and long-term (i.e., three years) (Ockene et al., 2012) weight loss in the general population. However, the literature on behavioral weight loss interventions for racial/ethnic minorities is less conclusive.
There have been several systematic reviews examining the effectiveness of behavioral weight loss interventions among racial and ethnic subgroups (4 among African Americans, 2 among Latinos, 1 among Asians, and 2 among all racial/ethnic minorities) (Kong et al., 2014; Newton et al., 2014; Tussing-Humphreys et al., 2013; Fitzgibbon et al., 2012; Bender et al., 2014; Perez et al., 2013; Corona et al., 2015; Seo and Jaesin, 2008; Osei-Assibey et al., 2010). Overall, these studies have observed a range of weight losses among racial/ethnic groups, and not all weight changes were significant. This existing body of literature also has several methodological weaknesses, including small sample sizes (Newton et al., 2014; Tussing-Humphreys et al., 2013; Bender et al., 2014) and high attrition rates (Corona et al., 2015; Osei-Assibey et al., 2010). An additional review published in 2012 found that males, especially ethnic minority males, are underrepresented in behavioral weight loss trials, with those representing only 1.8% of participants in the studied samples and no studies specifically targeting ethnic minority males (Pagoto et al., 2012). Recent examinations of racial/ethnic representation in behavioral weight loss trials are lacking. This review aims to fill that gap.
In 1993, the NIH Revitalization Act and Federal Law was enacted and required that racial/ethnic minority groups, as well as women, be included in federally funded human subject research studies as appropriate for the proposed goals and aims of the study (NIH Policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research, n.d.). Despite this, underrepresentation of minorities in research has been documented in numerous health related clinical trials (Kanakamedala and Haga, 2012; Geller et al., 2011). Barriers for participation of minorities may include mistrust, fear, and stigma of participation, and competing demands (George et al., 2014). A proven strategy to improve recruitment, participation and retention entails involving the community in study design, sampling, recruitment, data collection, and intervention delivery (Bonevski et al., 2014).
The primary goal of this systematic review is to evaluate racial/ethnic inclusion in behavioral weight loss trials published from 2009 to 2015, extending previous reviews that examined racial/ethnic representation in behavioral weight loss interventions until 2009. This review is a secondary analysis of data abstracted for a systematic review assessing methodological quality of behavioral weight loss studies published in this time period (Lemon et al., 2016). The secondary aims were to assess recruitment and study design approaches used to include racially and ethnically diverse samples and to determine the extent to which additional analyses of weight loss outcomes by racial/ethnic sub-groups were conducted in these studies.
2. Methods
2.1. Data sources and search strategy
A literature search was conducted using four online databases (i.e. PubMed, PsycInfo, Medline, and CINAHL) for behavioral weight loss intervention trials conducted among adults in the U.S. and published between January 1, 2009 and December 31, 2015. Key words used in these searches included “weight”, “loss”, “overweight”, “obese”, “intervention”, and “trial”. The reference sections of eligible articles for full text review were also reviewed for additional relevant articles.
2.2. Inclusion and exclusion criteria
Inclusion criteria for the efficacy and effectiveness studies selected for this review were: (1) measured weight loss as an outcome, (2) implementation and evaluation of behavioral intervention for developing healthy eating and/or physical activity skills for weight loss, (3) study samples comprised of adult participants (≥18 years) who were non-hospitalized and non-institutionalized, (4) studies had a follow-up of 6 months or longer, (5) publication in peer-reviewed journal between January 1, 2009 and December 31, 2015 (6), studies were conducted in the U.S., (7) studies were randomized controlled trials and (8) studies were published in English language.
Studies were excluded if they met any of the following criteria: (1) evaluation of pharmacological, surgical, environmental or policy interventions only (2) basic science studies, (3) study focused on program evaluation, (4) studies focused on survey development, (5) studies of weight maintenance or weight gain prevention, and (6) studies of secondary/mediation analysis of a trial. For interventions that yielded multiple publications meeting inclusion criteria, only the article with the final assessment point was reviewed.
2.3. Article selection and coding criteria
Titles of articles generated in the initial search were screened for inclusion. Abstracts of articles deemed relevant for inclusion were reviewed for eligibility. Two authors (CH, SL) reviewed each abstract separately (90.1% agreement) and discussed discrepancies in eligibility until a consensus of inclusion or exclusion was determined. Articles that met inclusion criteria based on the abstract review were selected for a full text review using a standardized data abstraction form. The reference sections of articles eligible for full text review were searched for additional articles that met inclusion criteria. Articles that remained eligible after the full text review process were included in the systematic review.
Initial coding criteria for data abstraction form was developed and tested on a set of five randomly selected articles that met eligibility for full text review. Each item on the form was reviewed and discussed for meaning and clarity. This process was repeated with another set of five randomly selected articles that met eligibility for full text review until complete consensus on all coding items was achieved. A document describing agreed upon coding procedures was used by each author during full text article review. Two authors reviewed each article and met to discuss results until consensus on abstracted data points and article eligibility was reached. Inter-rater agreement (IRA) between coders was calculated for each abstracted variable and reported by each item below.
3. Race/ethnicity categories
The approach of assessing race/ethnicity in the study was coded as self-report, medical records, or both. The racial/ethnic categories were coded as White, African American, Latino/Hispanic, Asian, Native American, or “Other”. The category “Other” was used when racial/ethnic categories were not reported, were unable to be determined, or was a category used by study investigators to describe the sample. Study participants also were included in the “Other” category when the entire sample's racial/ethnic distribution was not presented (e.g. only presented the percent of the sample that was white), and when investigators used “two or more races” as a category to describe the sample but did not specify the races included. (IRA = 100%). The number of participants in each racial/ethnic category was determined. When race/ethnicity was presented as a percent of the study sample, calculations were conducted to estimate the number of participants in each category. When race and ethnicity were listed as two separate variables, both were reported.
3.1. Study design and recruitment strategies to enhance racial and ethnic minority group participation
Articles were searched to determine if the investigators described recruitment strategies, particularly focusing on methods that enhanced the recruitment of racial and ethnic minorities. Coders described recruitment strategies used in the study. Articles were coded as to whether or not they intended to recruit a diverse racial/ethnic sample and/or failed to include descriptions of approaches to recruit a diverse racial/ethnic sample. Articles that included a description of their approach to recruit a diverse sample were further coded as either: having a target percentage of the sample to be from minority groups, recruitment at locations that serve racial/ethnically diverse populations, or intention to recruit a sample that was representative of the study's geographic location. (IRA = 89.4%).
3.2. Race/ethnicity sub-group analysis
Studies were searched for information on whether additional sub-analysis by race/ethnicity was conducted. Coders cited article text to describe analysis, which were categorized as one of the following: no sub-analysis by race/ethnicity, study participation analysis by race/ethnicity, and weight loss outcomes by race/ethnicity. (IRA = 96.8%).
3.3. Study characteristics
Behavioral Target(s): Studies were coded for whether the intervention targeted diet, physical activity, or both (IRA = 96.8%). Intervention Setting: The type of setting where the study was conducted was determined as a health care institute or facility, community organization, worksite location, church, college, neighborhood, or academic facility (IRA = 86.2%). Study Location. Coders recorded the state in which the study was conducted (IRA = 98.9%). Intervention Format: The format in which the intervention was delivered was coded into one of the following categories: group, individual, in-person, phone, web, other technology (IRA = 93.6%).
3.4. Analysis
Distributions across studies were examined. Assessment methods of race/ethnicity and the number of racial/ethnic categories reported in each study were described. To assess racial/ethnic representation in the included studies, we summed the total number and associated percentages of individuals within racial/ethnic categories across relevant studies. The percent of the sample for each racial/ethnic group was determined within each study, and descriptive statistics, including medians and ranges and means and standard deviations, were calculated to describe the distribution of racial/ethnic groups. Recruitment approaches to include a diverse sample were assessed and described narratively. The extent to which the studies included additional analyses by race/ethnicity was determined; methods used were described narratively. Statistical analyses were conducted using Stata version 13.1 (College Park, Texas).
4. Results
4.1. Study selection
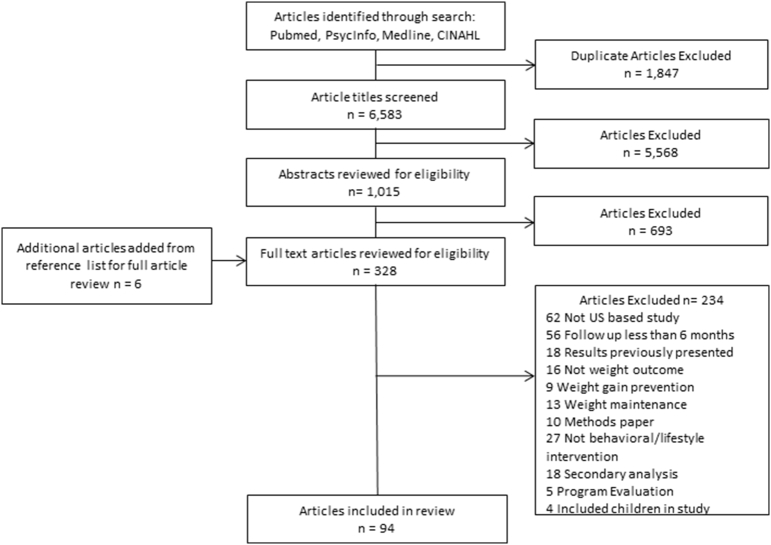
The literature search yielded a total of 6583 non-duplicate articles (Fig. 1). Of those, 5568 articles were excluded based on title review. Abstracts of the remaining 1015 articles were reviewed for eligibility; of those, 693 were subsequently excluded, resulting in 322 articles. An additional 6 articles were identified from those articles' references, yielding 328 articles that were examined in the full text review. A total of 94 articles met eligibility criteria and were included in this review.
Fig. 1.
Flow diagram of article inclusion and exclusion.
4.2. Study characteristics
The vast majority of studies (95.7%) included both diet and physical activity behavioral targets compared to diet only (3.2%) or physical activity only (1.1%). Most of the studies included both individual and group intervention components (71.3%). Interventions were most often delivered through health care (35.1%) and academic research centers (46.8%). Other delivery locations included community organizations (9.6%), worksites (5.3%), commercial (2.1%), and clinical settings (1.1%). Over half (63.8%) of study participants were recruited through convenience sampling (flyers, advertisements, mailings, etc.). The study sample sizes across the 94 articles ranged from 34 to 5145 participants.
4.3. Measurement and categorization of race/ethnicity
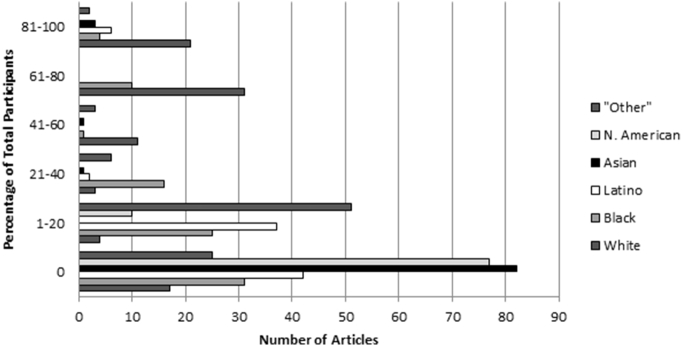
All but one of the 94 (98.9%) studies reported race/ethnicity in the description of participant characteristics (Fig. 2). A total of 66 articles reported the method used to assess racial/ethnic data, while the remaining 28 studies did not describe how race/ethnicity was collected or assessed. Of those that reported a method, the majority (96.9%) utilized participant self-report. The remaining studies (3.1%) reported collecting race/ethnicity data through a combination of both self-report and abstraction from medical records. Seven articles (10.6%) stated the specific categories provided on their measurement tool for participants to select from.
Fig. 2.
Number of articles that reported specific racial/ethnic categories and the percent of the total sample of each category represented in behavioral weight loss intervention studies in the United States between 2009 and 2015 (n = 94).
In 16 of the 94 articles (17.0%), race and ethnicity were assessed separately. Those 16 articles reported race on all study participants and also reported the number of participants that were of Hispanic/Latino ethnicity. No study reported which race was selected among participants that reported Hispanic/Latino ethnicity.
The racial/ethnic categories (White, African American, Asian, Latino/Hispanic, Native American, or “Other”) used to describe the sample varied. The number of categories ranged from a single racial/ethnic group to six different groups. At both ends of this continuum, nine studies (9.6%) reported one racial/ethnic group and eight studies (8.5%) reported six racial/ethnic groups. The “Other” racial/ethnic category was used in a total of 66 of the 94 (70.2%) studies and only 6 studies (6.4%) defined what racial/ethnic groups were included in the “Other” category.
4.4. Representation of racial/ethnic groups
Of the 29,320 trial participants included in the 94 studies in this review, 58.9% were identified as White, 18.2% as Black or African American, 8.7% as Hispanic or Latino, 5.0% as Asian or Pacific Islander and 1.0% as Native American. An additional 8.2% were categorized as “Other” (Table 1). Across the 94 studies, the median percentage of the sample size for each racial/ethnic category was 67.1% for White participants, 13.2% for African American participants and 0.5% for Hispanics/Latinos; with medians of 0% for both Asian/Pacific Islanders and Native Americans (Fig. 3). The majority of studies had samples that represented White participants (76 out of 94; 80.9%). African American participants were represented in 63 of the 94 studies (67.0%), and Latinos were represented in 51 (54.2%). Asian and Native American participants were represented in 29 and 11 studies (30.8% and 11.7%), respectively. There were nine studies that exclusively included one racial/ethnic group in their trials. Of those nine studies, 5 studies exclusively included Hispanic/Latinos, 3 Asians, and 1 African Americans.
Table 1.
Number and percentage of participants by racial/ethnic category in behavioral weight loss interventions in the United States 2009–2015 across the 94 included studies and the US Census data.
| Study n | Study n% | Census % | |
|---|---|---|---|
| White | 17,276 | 58.9% | 63.7% |
| African American | 5340 | 18.2% | 12.2% |
| Latino/Hispanic | 2538 | 8.7% | 16.3% |
| Asian | 1468 | 5.0% | 4.7% |
| Native American | 299 | 1.0% | 0.7% |
| “Other” | 2399 | 8.2% | 3.4% |
Fig. 3.
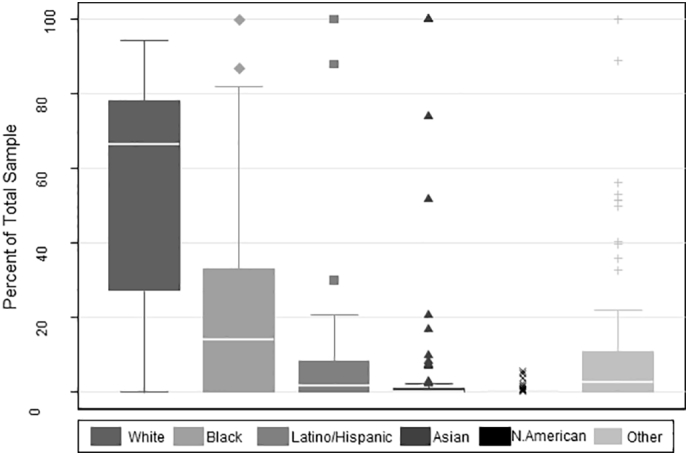
Boxplots of distributions of the sample size percenatge of racial/ethnic categories among behavioral weight loss interventions in the United States 2009–2015 (n = 94).
4.5. Study design and recruitment strategies to enhance racial and ethnic minority group participation
More than half (61.7%) of the included studies did not report an intention, approach or specific site/location targeted to recruit a sample that was racially or ethnically diverse. Of those studies that did not report an intention to recruit a diverse sample, 84.6% of the studies had a majority white sample. Two of the studies (1.7%) that did not have a majority white sample, reported in their discussion that they recruited a diverse sample, but did not state specific recruitment approaches or intention for recruiting diverse participants in the methods of their study.
Thirty-six of the 94 studies (38.3%) reported an intention, approach or specific site/location targeted to recruit a sample that was racially or ethnically diverse. Ten of these 36 studies (27.8%) intentionally recruited a sample consisting of only one racial/ethnic minority group: five of them were comprised of Hispanics/Latinos, two were comprised of African Americans, and three were comprised of Asians. Twenty-six of these 36 studies reported using specific recruitment approaches to obtain a diverse or representative sample including: pre-specified a recruitment goal for minority participants (4 out of 26; 15.4%), sought to obtain a diverse sample by targeting centers or location sites that served racially or socioeconomically diverse populations (16 out of 26; 61.5%), and stated that they intended to recruit a sample that was representative of the community or location in which the study took place (6 out of 26, 23.1%). Among the 16 studies that targeted centers or location sites that served diverse populations, specific methods for recruitment varied, including mass mailings, social media, electronic medical records, word of mouth, and partnerships with local organizations. Among the 6 studies that recruited a sample that was representative of the community or location in which the study took place, two took place in an area with a low percentage of minority populations (Pittsburgh, PA). The other four stated that their sample reflected the higher percentage of minority populations within the community.
4.6. Racial/ethnic sub-group analysis
Of the 60 studies that included more than one racial/ethnic group, eight included sub-group analyses of weight loss outcomes by race/ethnicity and two included sub-group analyses of predictors of intervention attendance by race/ethnicity.
5. Discussion
This review described racial/ethnic inclusion in behavioral lifestyle weight loss interventions among adults in the U.S. Across the 94 studies included in this review, 58.9% of participants were White, 18.2% were African American, 8.7% were Hispanic/Latino, 5.0% were Asian and 1.0% were Native American. An additional 8.2% were categorized as “Other”, a category that included individuals whose race/ethnicity was unknown or not reported. Compared to the current U.S. Census, representation of African Americans (18%) slightly exceeded the population proportion (~12%); representation of Latinos/Hispanics was below the population proportion (~16%) (United Stated Census Bureau, 2015); and representation of Native Americans was similar to the population proportion (1%). These results also demonstrate improvements in the representation of African American and Latino/Hispanic participants in behavioral weight loss studies compared to the findings from a 1999–2009 review where 14% and 5% of participants were African American and Latino/Hispanic, respectively (Pagoto et al., 2012). Compared to the 2009 review, this review found that African Americans were well represented in trials specifically targeting this group, as well as studies with mixed racial/ethnic composition, while the increase in Latino participants appears to be due to an increased number of studies specifically targeting this group. Representation of Asian Americans/Pacific Islanders and Native Americans in behavioral weight loss trials was similarly low across the two time periods, with no studies specifically targeting Native Americans. Finally, this study also found that the majority of the articles included in this review did not report strategies or approaches to recruit diverse samples. Only a small number of studies looked at weight loss results by race/ethnicity. This is of particular concern given the widespread obesity disparities experienced particularly by African Americans, Latinos and Native Americans (Ogden et al., 2015; Centers for Disease Control, 2015; Frieden, 2013). Greater inclusion in weight loss intervention studies and increases in the number of intervention trials specifically targeting these populations are warranted.
There are several possible reasons why racial and ethnic minorities remain under-represented in behavioral weight loss intervention studies. Geography may be a critical consideration, with studies conducted in predominantly White areas having less likelihood of achieving diverse participation. Further, most studies did not report specific efforts to recruit a diverse sample or efforts to retain these participants once they were in the study. However, other factors must be considered. We observed that most studies did not report specific efforts to recruit a diverse sample or efforts to retain these participants once they are in the study. It is possible that specific efforts were not described in the studies due to limited space and lack of reporting guidelines requiring this information.
A growing body of literature has identified barriers to research participation among racial and ethnic minority populations that can be addressed when developing recruitment and retention protocols. An important barrier to consider is the perceptions of research in general among potential participants. Mistrust in both healthcare and health-related research exists, particularly among African Americans (George et al., 2014). Additional barriers that are important to consider include language and cultural influences specific to weight, weight loss and weight-related behaviors.
There are numerous strategies that can be used to potentially address these barriers and enhance racial/ethnic diversity of study samples [Table 2]. Community engagement (Wang and Beydoun, 2007; Schwartz, 2001; Cho, 2006; Foster and Sharp, 2002; George et al., 2014), community based participatory research (CBPR) (Las Nueces et al., 2012) and research partnerships, as well as effective workforce strategies (Warner et al., 2013; Carroll et al., 2011; Pagoto et al., 2015; Coday et al., 2005) and peer to peer sampling may be effective in increasing participation of racial/ethnic diverse populations. Further, the use of technology to both recruit and deliver behavioral weight loss interventions shows promise for increasing inclusion of diverse samples. A recent review found that weight loss trials that incorporated smartphone use had greater enrollment of racial/ethnic minority participants than trials that did not incorporate smartphones (Rosenbaum et al., 2017). Emerging studies are revealing that interventions delivered via online programs (Sepah et al., 2015) and online social networks are effective at producing weight loss in the absence of clinic visits (Pagoto et al., 2015; Turner-McGrievy and Tate, 2011). Such interventions should specifically target minority populations, many of whom have been shown to be heavy users of online social networks (Perrin and Duggan, 2015).
Table 2.
Approaches to recruit and retain diverse racial/ethnic populations in behavioral lifestyle weight loss intervention trials.
| Strategy | Description |
|---|---|
| Community engagement |
|
| Community based participatory research (CBPR) |
|
| Research partnerships |
|
| Effective workforce strategies for recruitment and retention |
|
| Peer to peer sampling strategies (respondent-driven and snowballing) |
|
| Technology to recruit and deliver |
|
Factors that influence obesity may vary widely across racial/ethnic groups. Lack of adequate representation of racial/ethnic minority populations in behavioral weight loss trials limits the generalizability and potential public health impact of these interventions to groups that might benefit the most from weight loss. Cultural and environmental factors that may influence weight loss include the social and family context, immigration status, socioeconomic mobility, and cultural beliefs and behaviors (Elfhag and Rössner, 2005; Davis et al., 2005; Wang and Beydoun, 2007). Thus, some researchers have argued for the exclusion of racial and ethnic classifications from biomedical research given the acknowledgment of these categories as socio-cultural constructs rather than biologic in nature (Schwartz, 2001; Cho, 2006; Foster and Sharp, 2002). However, the use of racial/ethnic categories in weight loss studies is important for reducing obesity disparities and for advancing our understanding of ways in which cultural and environmental factors may impact weight loss outcomes. This understanding is critical to the development of interventions that effectively promote weight loss among individuals from racial/ethnic groups that bear the greatest burden of obesity and obesity-related diseases.
Study findings should be considered given the following limitations. Studies were restricted to those with a minimum six-month follow-up, which could exclude pilot studies with more racially or ethnically diverse samples (Kanakamedala and Haga, 2012). We were only able to evaluate the racial/ethnic categorizations the authors created and/or reported in their studies which may inhibit knowing all the racial/ethnic groups represented or included in the studies. Surgical and medication trials were excluded to focus on behavioral studies. Studies that focused solely on weight gain prevention were excluded. Thus, results may not be generalizable to study samples captured in weight gain prevention studies. The two authors that reviewed articles for inclusion were aware of the topic of investigation and were not blinded; this could be a potential source of bias in selection of articles. Strengths of these findings include the comprehensive review of racial/ethnic groups in the behavioral weight loss literature and the potential to highlight the need to include racial/ethnic groups in the future.
Results from this systematic review of behavioral weight loss interventions indicated that despite modest increases in the representation of some racial/ethnic minority groups in recent years, most studies continue to include a majority White sample. Given persistent racial/ethnic disparities in obesity, the high morbidity, mortality, and economic costs associated with obesity-related conditions, and national initiatives to eliminate health disparities in obesity, findings from this review emphasize the need to maximize representation of underrepresented racial/ethnic groups in behavioral lifestyle weight loss trials. Greater inclusion of Latino/Hispanic populations in behavioral lifestyle weight loss trials is a priority area for future research, given their underrepresentation in these studies compared and almost half of Latino/Hispanic adults being obese.
Conflicts of interest
None. The authors declare no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2018.01.012.
Appendix A. Articles included in review
Supplementary material
References
- Bender M.S., Choi J., Won G.Y., Fukuoka Y. Randomized controlled trial lifestyle interventions for Asian Americans: a systematic review. Prev. Med. 2014;67:171–181. doi: 10.1016/j.ypmed.2014.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonevski B., Randell M., Paul C. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med. Res. Methodol. 2014;14 doi: 10.1186/1471-2288-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll J.K., Yancey A.K., Spring B. What are successful recruitment and retention strategies for underserved populations? Examining physical activity interventions in primary care and community settings. Trans. Behav. Med. 2011;1:234–251. doi: 10.1007/s13142-011-0034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control Summary Health Statistics for U.S. Adults: 2015. 2015. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_A-15.pdf Table A-15A. Available from:
- Cho M.K. Racial and ethnic categories in biomedical research: there is no baby in the bathwater. J. Law Med. Ethics. 2006;34:497. doi: 10.1111/j.1748-720x.2006.00061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coday M., Boutin-Foster C., Sher T.G. Strategies for retaining study participants in behavioral intervention trials: retention experiences of the NIH Behavior Change Consortium. Ann. Behav. Med. 2005;29(2):55–65. doi: 10.1207/s15324796abm2902s_9. [DOI] [PubMed] [Google Scholar]
- Corona E., Flores Y.N., Arab L. Trends in evidence-based lifestyle interventions directed at obese and overweight adult Latinos in the US: a systematic review of the literature. J. Community Health. 2015;41:1–7. doi: 10.1007/s10900-015-0119-9. [DOI] [PubMed] [Google Scholar]
- Cossrow N., Falkner B. Race/ethnic issues in obesity and obesity-related comorbidities. J. Clin. Endocrinol. Metab. 2004;89(6):2590–2594. doi: 10.1210/jc.2004-0339. [DOI] [PubMed] [Google Scholar]
- Davis E.M., Clark J.M., Carrese J.A., Gary T.L., Cooper L.A. Racial and socioeconomic differences in the weight-loss experiences of obese women. Am. J. Public Health. 2005;95:1539–1543. doi: 10.2105/AJPH.2004.047050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfhag K., Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes. Rev. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon M.L., Tussing-Humphreys L.M., Porter J.S., Martin I.K., Odoms-Young A., Sharp L.K. Weight loss and African–American women: a systematic review of the behavioural weight loss intervention literature. Obes. Rev. 2012;13:193–213. doi: 10.1111/j.1467-789X.2011.00945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. J. Am. Med. Assoc. 2016;315:2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster M.W., Sharp R.R. Race, ethnicity, and genomics: social classifications as proxies of biological heterogeneity. Genome Res. 2002;12:844–850. doi: 10.1101/gr.99202. [DOI] [PubMed] [Google Scholar]
- Franz M.J., VanWormer J.J., Crain A.L. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J. Am. Diet. Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Frieden T.R. CDC health disparities and inequalities report-United States, 2013. Foreword. Morb. Mortal. Wkly Rep. Suppl. 2013;62(3):1–2. [PubMed] [Google Scholar]
- Geller S.E., Koch A., Pellettieri B., Carnes M. Inclusion, analysis, and reporting of sex and race/ethnicity in clinical trials: have we made progress? J. Women's Health. 2011;20(3):315–320. doi: 10.1089/jwh.2010.2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George S., Duran N., Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific islanders. Am. J. Public Health. 2014;104(2):e16–e31. doi: 10.2105/AJPH.2013.301706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guh D.P., Zhang W., Bansback N., Amarsi Z., Birmingham C.L., Anis A.H. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanakamedala P., Haga S.B. Characterization of clinical study populations by race and ethnicity in biomedical literature. Ethn. Dis. 2012;22(1):96–101. [PMC free article] [PubMed] [Google Scholar]
- Knowler W.C., Barrett-Connor E., Fowler S.E. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh H.K., Graham G., Glied S.A. Reducing racial and ethnic disparities: the action plan from the department of health and human services. Health Aff. 2011;30:1822–1829. doi: 10.1377/hlthaff.2011.0673. [DOI] [PubMed] [Google Scholar]
- Kong A., Tussing-Humphreys L.M., Odoms-Young A.M., Stolley M.R., Fitzgibbon M.L. Systematic review of behavioural interventions with culturally adapted strategies to improve diet and weight outcomes in African American women. Obes. Rev. 2014;15:62–92. doi: 10.1111/obr.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Las Nueces D., Hacker K., DiGirolamo A., Hicks L.S. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Serv. Res. 2012;47:1363–1386. doi: 10.1111/j.1475-6773.2012.01386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemon S.C., Wang M.L., Haughton C.F., Estabrook D.P., Frisard C.F., Pagoto S.L. Methodological quality of behavioural weight loss studies: a systematic review. Obes. Rev. 2016;17(7):636–644. doi: 10.1111/obr.12412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Partnership for Action. National Stakeholder Strategy for Achieving Health Equity. Rockville (MD): Department of Health and Human Services; [cited 2011 Aug 19]. Available from: http://www.minorityhealth.hhs.gov/npa/templates/content.aspx?lvl (Internet).
- Newton R.L., Griffith D.M., Kearney W.B., Bennett G.G. A systematic review of weight loss, physical activity and dietary interventions involving African American men. Obes. Rev. 2014;15:93–106. doi: 10.1111/obr.12209. [DOI] [PubMed] [Google Scholar]
- NIH Policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research. Bethesda, MD: National Institutes of Health.
- Norman J.E., Bild D., Lewis C.E., Liu K., West D.S. The impact of weight change on cardiovascular disease risk factors in young black and white adults: the CARDIA study. Int. J. Obes. Relat. Metab. Disord. 2003;27:369–376. doi: 10.1038/sj.ijo.0802243. [DOI] [PubMed] [Google Scholar]
- Ockene I.S., Tellez T.L., Rosal M.C. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino diabetes prevention project. Am. J. Public Health. 2012;102:336–342. doi: 10.2105/AJPH.2011.300357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C.L., Carroll M.D., Fryar C.D., Flegal K.M. Vol. 219. 2015. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014; pp. 1–8. NCHS Data Brief. [PubMed] [Google Scholar]
- Osei-Assibey G., Kyrou I., Adi Y., Kumar S., Matyka K. Dietary and lifestyle interventions for weight management in adults from minority ethnic/non-White groups: a systematic review. Obes. Rev. 2010;11:769–776. doi: 10.1111/j.1467-789X.2009.00695.x. [DOI] [PubMed] [Google Scholar]
- Otado J., Kwagyan J., Edwards D., Ukaegbu A., Rockcliffe F., Osafo N. Culturally competent strategies for recruitment and retention of African American populations into clinical trials. Clin. Transl. Sci. 2015;8:460–466. doi: 10.1111/cts.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagoto S.L., Schneider K.L., Oleski J.L., Luciani J.M., Bodenlos J.S., Whited M.C. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2012;20:1234–1239. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- Pagoto S.L., Waring M.E., Schneider K.L. Twitter-delivered behavioral weight-loss interventions: a pilot series. J. Med. Internet Res. Protoc. 2015;4 doi: 10.2196/resprot.4864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasanisi F., Contaldo F., De Simone G., Mancini M. Benefits of sustained moderate weight loss in obesity. Nutr. Metab. Cardiovasc. Dis. 2001;11:401–406. [PubMed] [Google Scholar]
- Perez L.G., Arredondo E.M., Elder J.P., Barquera S., Nagle B., Holub C.K. Evidence-based obesity treatment interventions for Latino adults in the US: a systematic review. Am. J. Prev. Med. 2013;44:550–560. doi: 10.1016/j.amepre.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin A., Duggan M. Vol. 26. Pew Research Center; 2015. Americans Internet Access: 2000–2015. [Google Scholar]
- Rosenbaum D.L., Piers A.D., Schumacher L.M., Kase C.A., Butryn M.L. Racial and ethnic minority enrollment in randomized clinical trials of behavioural weight loss utilizing technology: a systematic review. Obes. Rev. 2017;18(7):808–817. doi: 10.1111/obr.12545. [DOI] [PubMed] [Google Scholar]
- Schwartz R.S. Racial profiling in medical research. N. Engl. J. Med. 2001;344:1392–1393. doi: 10.1056/NEJM200105033441810. [DOI] [PubMed] [Google Scholar]
- Seo D.C., Jaesin S.A. A meta-analysis of psycho-behavioral obesity interventions among US multiethnic and minority adults. Prev. Med. 2008;47:573–582. doi: 10.1016/j.ypmed.2007.12.010. [DOI] [PubMed] [Google Scholar]
- Sepah S.C., Jiang L., Peters A.L. Long-term outcomes of a Web-based diabetes prevention program: 2-year results of a single-arm longitudinal study. J. Med. Internet Res. 2015;17 doi: 10.2196/jmir.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-McGrievy G., Tate D. Tweets, apps, and pods: results of the 6-month mobile pounds off digitally (mobile POD) randomized weight-loss intervention among adults. J. Med. Internet Res. 2011;13 doi: 10.2196/jmir.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tussing-Humphreys L.M., Fitzgibbon M.L., Kong A., Odoms-Young A. Weight loss maintenance in African American women: a systematic review of the behavioral lifestyle intervention literature. J. Obes. 2013;2013:1–31. doi: 10.1155/2013/437369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services Healthy People 2020: Improving the Health of Americans Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report—United States, 2013. 2013. http://www.cdc.gov/mmwr/pdf/other/su6203.pdf Available from:
- United Stated Census Bureau Population Estimates. National Population by Characteristics Tables: 2010–2015. Annual Estimates of the Resident Population by Sex, Race Alone or in Combination, and Hispanic Origin for the United States, States, and Counties: April 1, 2010 to July 1, 2015. 2015. https://www.census.gov/data/tables/2015/demo/popest/nation-detail.html Available from:
- Wang Y., Beydoun M.A. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol. Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Warner E.T., Glasgow R.E., Emmons K.M. Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: results and lessons learned. BMC Public Health. 2013;13:192. doi: 10.1186/1471-2458-13-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material