Abstract
Introduction
This study investigated the degree and direction (kHR) of the heart rate to performance curve (HRPC) during cardio-pulmonary exercise (CPX) testing and explored the relationship with diabetes markers, anthropometry and exercise physiological markers in type 1 diabetes (T1DM).
Material and methods
Sixty-four people with T1DM (13 females; age: 34 ± 8 years; HbA1c: 7.8 ± 1% (62 ± 13 mmol.mol-1) performed a CPX test until maximum exhaustion. kHR was calculated by a second-degree polynomial representation between post-warm up and maximum power output. Adjusted stepwise linear regression analysis was performed to investigate kHR and its associations. Receiver operating characteristic (ROC) curve was performed based on kHR for groups kHR < 0.20 vs. > 0.20 in relation to HbA1c.
Results
We found significant relationships between kHR and HbA1c (β = -0.70, P < 0.0001), age (β = -0.23, P = 0.03) and duration of diabetes (β = 0.20, P = 0.04). Stepwise linear regression resulted in an overall adjusted R2 of 0.57 (R = 0.79, P < 0.0001). Our data revealed also significant associations between kHR and percentage of heart rate at heart rate turn point from maximum heart rate (β = 0.43, P < 0.0001) and maximum power output relativized to bodyweight (β = 0.44, P = 0.001) (overall adjusted R2 of 0.44 (R = 0.53, P < 0.0001)). ROC curve analysis based on kHR resulted in a HbA1c threshold of 7.9% (62 mmol.mol-1).
Conclusion
Our data demonstrate atypical HRPC during CPX testing that were mainly related to glycemic control in people with T1DM.
Introduction
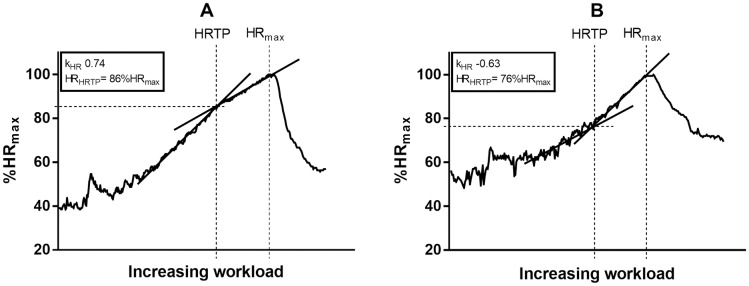
Cardio-pulmonary exercise (CPX) testing provides detailed diagnostic information about cardio-pulmonary, vascular and musculoskeletal adaptations to physical stressors [1]. Aerobic performance markers, like thresholds (e.g. ventilatory thresholds or the heart rate turn point (HRTP)) are recommended to accurately prescribe individualized exercise intensity [2]. These thresholds relativized to maximum oxygen consumption (VO2max) serve as sensitive markers to analyze effects of exercise training in both healthy individuals and patients [3]. As an example the HRTP, which is based on findings from Conconi and colleagues, was significantly associated with the second lactate threshold [4–7]. This heart rate (HR) derived threshold is defined as the intersection of two regression lines of the HR to performance curve (HRPC) between early stages of CPX testing (peri-first lactate turn point (LTP1)) and maximum power output (Pmax), determined from a second-degree polynomial representation satisfying the condition of least error squares (Fig 1) [8].
Fig 1. Schematic of the heart rate to performance curve (HRPC) and detection of the heart rate turn point (HRTP) during CPX testing, illustrating a regular HRPC (A) and an inverted HRPC (B).
The difference in HRPC translates to a lower heart rate at HRTP (HRHRTP) when given as percentage of the maximum heart rate (%HRmax) (difference 10%). kHR = degree and direction of the heart rate to performance curve. HRmax = maximum heart rate.
From a physiological point of view the main cause for the HRTP can be seen in the β1-receptor sensitivity to the catecholamine response [9]. Hofmann et al. investigated the response to a single dose of the β1-selective antagonist bisoprolol in healthy individuals [10]. This study revealed a significant association between the response to the antagonist and different patterns of the HRPC. A regular HRPC translated to inverted HRPC when using the β1-antagonist. However, an inverted HRPC under placebo did not change its pattern under a β1-antagonist application. This shows that the inverted HRPC in placebo conditions is caused by a reduced β1-receptor sensitivity.
Inter-individual differences in HRPC were observed in healthy individuals and in different groups of patients [8]. In the general population, approximately 86% of people show regular deflections of HRPC across a sub-maximal (HRTP) to maximal (Pmax) continuum; however, 8% reveal inverted deflections and 6% display linear increases in HRPC.
Chronotropic incompetence (CI) is the inability of the HR to increase in proportion to raised metabolic demand, and is found mainly in people with coronary artery disease. CI is a strong and independent predictor of overall mortality [11]. Interestingly, this non-physiological cardiac response was also reported in people with type 2 diabetes, where its origin is not fully understood. Diabetes per se and/or disease-related comorbidities as well as physiological anomalies seem to play a role for CI [12].
Poor glycemic control in people with T1DM may be associated with blunted functional capacity compared to healthy individuals, which is mainly assessed by means of VO2max [13–15]. Some studies suggested that poor glycemic control may alter cardio-respiratory and metabolic responses to exercise, which translates to a general lower functional capacity in people with T1DM [13,15]. Furthermore, it has been shown that people with T1DM have a reduced maximum HR (HRmax) in comparison to their healthy counterparts [13]. Intriguingly, the blunted effect of HRmax was shown to be dependent on glycemic control [16].
It is currently not known if the degree and the direction (kHR) of the HRPC during CPX testing is related to glycemic control in people with T1DM. Therefore, the aim of this study was to investigate kHR during CPX testing and explore relationships to diabetes markers, anthropometry and exercise physiological markers in a large group of people with T1DM.
Material and methods
Participant characteristics
For this study sixty-four people with T1DM were recruited from October 2012 until March 2013 by advertisement in local newspapers (Table 1, Fig 2):
Table 1. Participant characteristics given as mean ± SD and percentage (%).
| Characteristic | Total (n = 64) |
|---|---|
| Age (years) | 34 ± 8 |
| Female (n; %) | 13 (20) |
| Male (n; %) | 51 (80) |
| Body mass index (kg/m2) | 24 ± 2 |
| Duration of diabetes (years) | 17 ± 9 |
| HbA1c (% (mmol.mol-1)) | 7.8 ± 1 (62 ± 13) |
| Total daily dose of insulin (U) | 51 ± 15 |
| Multiple daily injections (n; %) | 47 (78) |
| Insulin pump therapy (n; %) | 17 (22) |
| Arterial hypertension | 6 |
| Hypothyroidism | 5 |
| Hypercholesterolemia | 2 |
| Hashimoto thyroiditis | 1 |
| ACE inhibitor | 6 |
| Levothyroxine | 6 |
| Statin | 2 |
| Diuretic medication | 1 |
| Calcium channel blocker | 1 |
| Physical activity (MET min.wk 1)) | 3086 ± 2736 |
| Maximum oxygen uptake (ml.kg-1.min-1) | 37 ± 5 |
Fig 2. Consort flow diagram.
Consent procedure
Participants gave their written informed consent before any trial related activities. The trial was performed accordingly to the Declaration of Helsinki (DoH) and Good Clinical Practice (GCP) Guidelines. The primary study protocol was approved by the local ethics committee and health authority board. The study protocol was registered with the universal clinical trial registry, number NCT01704417 [17].
Study procedures
Participants filled in the International Physical Activity Questionnaire (IPAQ) to assess physical activity (MET min/week). Medical history, medications and patients’ characteristics were documented on the day of the CPX testing. Immediately afterwards, HbA1c was measured from a venous blood sample (Automated Glycohemoglobin Analyzer HLC-723G8, Tosoh Europe N.V, Belgium). Venous blood was collected immediately before and after CPX testing to evaluate blood glucose concentration (Super GL Glucose Analyzer, Dr. Müller Gerätebau GmbH, Germany). Participants performed a CPX test until maximum volitional exhaustion on a cycle ergometer (Ergospirometer PowerCube®-Ergo, Ganshorn Medizin Electronic, GER) under medical supervision. Participants sat for 3 min (0 watt (W)) on the cycle ergometer before they started the warm-up period of 3 min cycling at an exercise intensity of 30 W for females and 40 W for males. After the warm-up period, the intensity was increased by 30 W for females and 40 W for males every 3 minutes until maximum volitional exhaustion. Finally, an active recovery period was conducted for 1 min.
Measurements
Pulmonary gas exchange variables were measured continuously. Data were then averaged over 10 seconds to control for artefacts. Blood pressure and HR were measured continuously via an automatic sphygmomanometer and a 12-lead electrocardiogram (Ergospirometer PowerCube®-Ergo, Ganshorn Medizin Electronic, GER). The non-invasive anaerobic threshold was defined by the HRTP. HRTP was demarcated as the intersection of two regression lines of HRPC between post-warm-up and Pmax, determined from a second-degree polynomial representation satisfying the condition of least error squares [8]. All measurements were conducted at Profil, Neuss, Germany.
Statistical analyses
Data were tested for normal distribution via Shapiro-Wilk test. Descriptive statistics included mean and standard deviation for participant’s characteristics. kHR was calculated by a second-degree polynomial representation between post-warm up and Pmax. Stepwise linear regression was used to explore relationships between kHR and diabetes markers (glycemic control (HbA1c), total daily dose of insulin (both basal- and bolus insulin), duration of diabetes), anthropometry (height, weight, body mass index (BMI)) and physical activity (IPAQ). Stepwise linear regression was also used between kHR and exercise physiological markers (CPX derived cardio-respiratory markers at HRTP and at Pmax). Stepwise linear regressions were adjusted for gender, BMI, physical activity, total daily dose of insulin, duration of diabetes and blood glucose concentration at the start of CPX testing if not included in the regression model. Logarithmic transformation was performed if data were non-normally distributed. Receiver operating characteristic (ROC) curves based on kHR for groups kHR < 0.20 vs. > 0.20 in relation to HbA1c. All statistical analyses were carried out using SPSS V.22.0 statistical software (SPSS, Chicago, Illinois, USA). A sample size of 64 individuals with T1DM resulted in a power (1 –β error probability) of 1.0 for the main outcome analyzed via stepwise linear regression, respectively.
Results
Relationships between kHR and HbA1c, total daily dose of insulin, duration of diabetes, anthropometry and physical activity
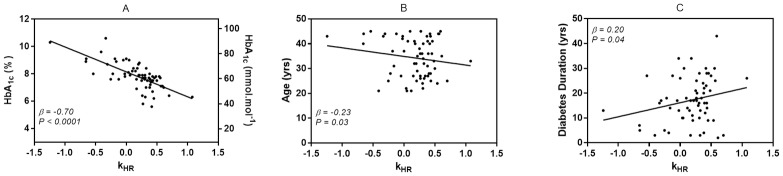
We found significant relationships between kHR and HbA1c (β = -0.70, P < 0.0001), age (β = -0.23, P = 0.03) and duration of diabetes (β = 0.20, P = 0.04) (Fig 3). Stepwise linear regression resulted in an overall adjusted R2 of 0.57 (R = 0.79, P < 0.0001).
Fig 3. Single plots of the association of kHR and HbA1c (A), age (B) and diabetes duration (C).
kHR = degree and direction of the heart rate to performance curve.
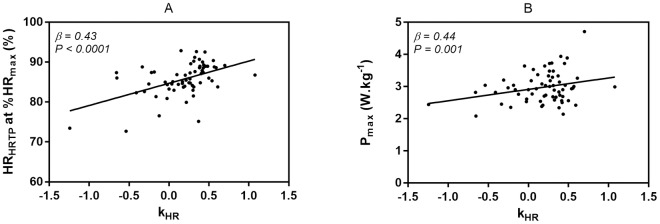
Relationships between kHR exercise physiological markers
Our data revealed significant associations between kHR and percentage of HR at HRTP from HRmax (β = 0.43, P < 0.0001) and Pmax relativized to bodyweight (β = 0.44, P = 0.001). Stepwise linear regression resulted in an overall adjusted R2 of 0.44 (R = 0.53, P < 0.0001) (Fig 4).
Fig 4. Single plots of the association of kHR and HRHRTP at %HRmax (A) and Pmax (B).
kHR = degree and direction of the heart rate to performance curve, HRHRTP at %HRmax = heart rate at the heart rate turn point given as percentages of the maximum heart rate, Pmax = maximum power output relativized to bodyweight.
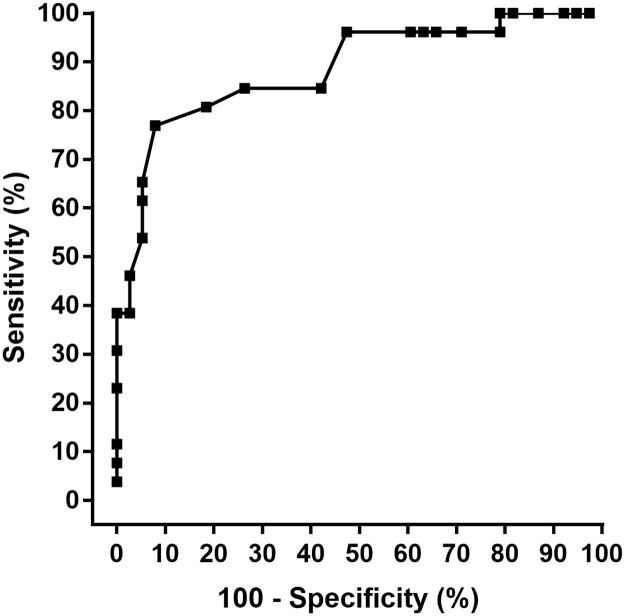
ROC curve analysis based on kHR
ROC curve analysis based on kHR for groups kHR < 0.20 vs. > 0.20 resulted in a HbA1c threshold of 7.9% (63 mmol.mol-1) (81% sensitivity and 82% specificity) (Fig 5).
Fig 5. Receiver operating characteristic (ROC) curve analysis of HbA1c.
The sensitivity is plotted against 100–specificity to indicate accuracy. The optimal value for sensitivity was 81%, which corresponded to a specificity of 82%. This represents a cut off level for HbA1c of 7.9% (63 mmol.mol-1).
Discussion
This study demonstrated the clear association between poor glycemic control and HR dynamics during CPX testing. Intriguingly, higher HbA1c and its translation to atypical kHR resulted in lower HR responses at the HRTP and lower bodyweight-relativized maximum power output. Several physiological mechanisms might explain these novel findings:
Diabetes specific co-morbidities (e.g. structural myocardial alterations, ventricular and/or arterial stiffness, impaired baroreflex sensitivity and cardiovascular autonomic neuropathy) might minimally contribute to these alterations in kHR, as the cohort in our trial underwent detailed physical examination [12,18].
Potentially the findings from our study are associated with impairments in ß1-adrenoreceptors. Poor glycaemic control is associated with chronically elevated catecholamine levels [19] and can induce ß1-adrenoreceptor insensitivity. Impairment in ß1-adrenoreceptor sensitivity is known to alter the ability of HR to respond adequately to increasing metabolic demands [20]. ß1-adrenoreceptors produces positive inotropy, chronotropy and lusitropy with further positive dromotropic effect and pacemaker activity from the sinoatrial node [21]. We hypothesize if ß1-adrenoreceptor insensitivity is present, a lower rise in free intracellular Ca2+ concentration dysregulates cardiac muscle contraction [22,23] resulting in CI during CPX testing. Taking this into account for our study cohort, we postulate that elevated HbA1c may modify the typical HR response to stress via ß1-adrenoreceptor hyposensitivity.
Similar to the findings from our study, previous studies observed reduced cardiac output during sub-maximal exercise intensities in individuals with T1DM [24][13]. Intriguingly, for our data this was not only supported by the decreased ratio of HR at HRTP as percentage of HRmax, we also found for the non-adjusted stepwise linear regression (data not shown) a significant increased O2-Pulse (surrogate parameter for stroke volume) at the HRTP in individuals with poor glycaemic control. We postulate that the decreased ratio of HR at HRTP as percentage of HRmax is compensated via increased stroke volume at the HRTP to maintain adequate cardiac output in relation to metabolic demands.
Several studies found a decreased exercise performance in comparison of individuals with T1DM and their healthy counterparts [25][26]. However, little research exists on its relation to glycaemic control [13], and to the best of our knowledge, no trials investigated the influence of CI on exercise performance. As found in our study, CI analyzed via kHR was associated with lowered Pmax (W.kg-1).
ROC curve clearly showed that HbA1c above 7.9% (63 mmol.mol-1) was associated with kHR towards CI in the transition of HRTP to Pmax. A low HbA1c accompanied with low risk of hypoglycemic episodes are important aspects of the management of T1DM. However, the percentage of people with T1DM achieving HbA1c within 7.0% (53 mmol.mol-1) and 7.5% (58 mmol.mol-1) is only from 8% to 28% [27–30] and it is unclear if such glycemic control targets are attainable for most patients. It might be that more applicable HbA1c targets (potentially supported by our threshold of 7.9% (63 mmol.mol-1)) accompanied with regular physical activity and exercise could be more beneficial in reduction of risk of all-cause mortality and cardiovascular disease [31] and eventually play a role in restoration of counter-regulatory responses to hypoglycemia [32].
From a clinical point of view the findings from this study could be of immense interest for an exact prescription of exercise intensity. The American Diabetes Association recommends at least 150 min per week of moderate intensity aerobic physical activity, defined as percentages of HRmax [33]. In consideration of the results from our study regarding HR at HRTP given as percentages of HRmax, we might dissuade from using percentages of HRmax. Fixed percentages of HRmax would lead to an overestimation of exercise intensity in individuals with poor glycaemic control as in these patients the anaerobic threshold (HRTP) was found in a lower percentage to HRmax.
This study is somewhat limited by possible differences in c-peptide status, which was not measured for the purpose of this study. Further studies are needed to investigate kHR and ß1-adrenoreceptor sensitivity in people with T1DM.
Conclusions
This is the first study, which found associations between kHR and HbA1c, age and duration of diabetes in people with T1DM. Individuals with poor glycaemic control showed slower increases in HR during early stages of CPX testing, which translated to (i) a decreased ratio of HR at HRTP as percentage of HRmax and (ii) a lowered body weight-relativized Pmax. Age and diabetes duration were also found to play a role for these findings. However, both factors contributed minimally to the results (age: β = -0.23; diabetes duration: β = 0.20).
Supporting information
(PDF)
(PDF)
Acknowledgments
O. Moser has received lecture fees from Medtronic, a travel grant from Novo Nordisk A/S and research grants from Sêr Cymru II COFUND fellowship/European Union and Novo Nordisk A/S. M. L. Eckstein has received a KESS2/European Social Fund scholarship. S. C. Bain reports having received honoraria, teaching and research grants from the Abbott, Astra Zeneca, Boehringer Ingelheim, BMS, Diartis, Eli Lily and Company, GlaxoSmithKline, Johnson & Johnson, Merck Sharp & Dohme, Novartis, Novo Nordisk, Pfizer, Roche, Sanofi-Aventis, Schering-Plough, Servier and Takeda. T. Heise reports having received research funds from Adocia, Astra Zeneca, BD, Biocon, Boehringer Ingelheim, Dance Pharmaceuticals, Grünenthal, Eli Lily and Company, Medtronic, Novo Nordisk, Novartis, Sanofi and Senseonics and having received speaker honoraria and travel grants from Eli Lily and Company, Mylan and Novo Nordisk. R. M. Bracken reports having received honoraria, travel and educational grant support from, Boehringer-Ingelheim, Eli Lily and Company, Novo Nordisk, Sanofi-Aventis. E. Zijlstra, R. Deere and O. McCarthy have no disclosures to report. H. L. Haahr is employee and shareholder in Novo Nordisk A/S. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
This study was funded by Novo Nordisk A/S. Data were extracted from a clinical trial (NCT01704417). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
The authors cannot share the data underlying this study because the data belongs to Profil Institut für Stoffwechselforschung GmbH. Qualified researchers may request data access by contacting Profil Institut für Stoffwechselforschung GmbH (marketing@profil.com). The authors did not have any special access privileges that others would not have. Profil Institut für Stoffwechselforschung GmbH, Hellersbergstraße 9, 41460 - Neuss, Germany, Telephone +49-2131-4018-345, marketing@profil.com, https://www.profil.com.
Funding Statement
This study was supported by Novo Nordisk A/S (NN1250-3999 to Tim Heise).
References
- 1.Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s Guide to Cardiopulmonary Exercise Testing in Adults: A Scientific Statement From the American Heart Association. Circulation. 2010;122: 191–225. doi: 10.1161/CIR.0b013e3181e52e69 [DOI] [PubMed] [Google Scholar]
- 2.Hofmann P, Tschakert G. Special Needs to Prescribe Exercise Intensity for Scientific Studies. Cardiol Res Pract. 2011;2011: 1–10. doi: 10.4061/2011/209302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moser O, Tschakert G, Mueller A, Groeschl W, Hofmann P, Pieber T, et al. Short-acting insulin reduction strategies for continuous cycle ergometer exercises in patients with type 1 diabetes mellitus. Asian J Sports Med. 2017;8 doi: 10.5812/asjsm.42160 [Google Scholar]
- 4.Conconi F, Ferrari M, Ziglio PG, Droghetti P, Codeca L. Determination of the anaerobic threshold by a noninvasive field test in runners. J Appl Physiol. 1982;52: 869–73. doi: 10.1152/jappl.1982.52.4.869 [DOI] [PubMed] [Google Scholar]
- 5.Ribeiro JP, Fielding RA, Hughes V, Black A, Bochese MA, Knuttgen HG. Heart rate break point may coincide with the anaerobic and not the aerobic threshold. Int J Sports Med. 1985;6: 220–4. doi: 10.1055/s-2008-1025844 [DOI] [PubMed] [Google Scholar]
- 6.Hofmann P, Bunc V, Leitner H, Pokan R, Gaisl G. Heart rate threshold related to lactate turn point and steady-state exercise on a cycle ergometer. Eur J Appl Physiol Occup Physiol. 1994;69: 132–9. [DOI] [PubMed] [Google Scholar]
- 7.Bunc V, Hofmann P, Leitner H, Gaisl G. Verification of the heart rate threshold. Eur J Appl Physiol Occup Physiol. 1995;70: 263–9. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann P, Pokan R, Duvillard S, Seibert F, Zweiker R, Schmid P. Heart rate performance curve during incremental cycle ergometer exercise in healthy young male subjects. Medicine & Science in Sports & Exercise. 1997. pp. 762–768. [DOI] [PubMed] [Google Scholar]
- 9.Hofmann P, Pokan R. Value of the application of the heart rate performance curve in sports. Int J Sports Physiol Perform. 2010;5: 437–447. [DOI] [PubMed] [Google Scholar]
- 10.Hofmann P, Wonisch M, Pokan R, Schwaberger G, Smekal G, Von Duvillard SP. β1-adrenoceptor mediated origin of the heart rate performance curve deflection. Med Sci Sports Exerc. 2005;37: 1704–1709. doi: 10.1249/01.mss.0000176308.70316.cc [DOI] [PubMed] [Google Scholar]
- 11.Dresing TJ, Blackstone EH, Pashkow FJ, Snader CE, Marwick TH, Lauer MS. Usefulness of impaired chronotropic response to exercise as a predictor of mortality, independent of the severity of coronary artery disease. Am J Cardiol. 2000;86: 602–609. doi: 10.1016/S0002-9149(00)01036-5 [DOI] [PubMed] [Google Scholar]
- 12.Keytsman C, Dendale P, Hansen D. Chronotropic incompetence during exercise in type 2 diabetes: aetiology, assessment methodology, prognostic impact and therapy. Sport Med. 2015;45: 985–995. doi: 10.1007/s40279-015-0328-5 [DOI] [PubMed] [Google Scholar]
- 13.Baldi JC, Cassuto NA, Foxx-Lupo WT, Wheatley CM, Snyder EM. Glycemic status affects cardiopulmonary exercise response in athletes with type I diabetes. Med Sci Sports Exerc. 2010;42: 1454–1459. doi: 10.1249/MSS.0b013e3181d1fdb3 [DOI] [PubMed] [Google Scholar]
- 14.Nadeau KJ, Regensteiner JG, Bauer TA, Brown MS, Dorosz JL, Hull A, et al. Insulin resistance in adolescents with type 1 diabetes and its relationship to cardiovascular function. J Clin Endocrinol Metab. 2010;95: 513–21. doi: 10.1210/jc.2009-1756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldi JC, Hofman PL. Does careful glycemic control improve aerobic capacity in subjects with type 1 diabetes? Exerc Sport Sci Rev. 2010;38: 161–7. doi: 10.1097/JES.0b013e3181f4501e [DOI] [PubMed] [Google Scholar]
- 16.Niranjan V, McBrayer DG, Ramirez LC, Raskin P, Hsia CC. Glycemic control and cardiopulmonary function in patients with insulin-dependent diabetes mellitus. Am J Med. 1997;103: 504–13. [DOI] [PubMed] [Google Scholar]
- 17.Heise T, Bain SC, Bracken RM, Zijlstra E, Nosek L, Stender-Petersen K, et al. Similar risk of exercise-related hypoglycaemia for insulin degludec to that for insulin glargine in patients with type 1 diabetes: a randomized cross-over trial. Diabetes Obes Metab. 2016;18: 196–199. doi: 10.1111/dom.12588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brahma MK, Pepin ME, Wende AR. My sweetheart is broken: role of glucose in diabetic cardiomyopathy. Diabetes Metab J. 2017;41: 1–9. doi: 10.4093/dmj.2017.41.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heyman E, Delamarche P, Berthon P, Meeusen R, Briard D, Vincent S, et al. Alteration in sympathoadrenergic activity at rest and during intense exercise despite normal aerobic fitness in late pubertal adolescent girls with type 1 diabetes. Diabetes Metab. 2007;33: 422–429. doi: 10.1016/j.diabet.2007.10.003 [DOI] [PubMed] [Google Scholar]
- 20.Wonisch M, Hofmann P, Fruhwald FM, Kraxner W, Hodl R, Pokan R, et al. Influence of beta-blocker use on percentage of target heart rate exercise prescription. Eur J Cardiovasc Prev Rehabil. 2003;10: 296–301. doi: 10.1097/01.hjr.0000085249.65733.e2 [DOI] [PubMed] [Google Scholar]
- 21.Colucci WS, Wright RF, Braunwald E. New positive inotropic agents in the treatment of congestive heart failure. N Engl J Med. 1986;314: 349–358. doi: 10.1056/NEJM198602063140605 [DOI] [PubMed] [Google Scholar]
- 22.Bers DM. Calcium cycling and signaling in cardiac myocytes. Annu Rev Physiol. 2008;70: 23–49. doi: 10.1146/annurev.physiol.70.113006.100455 [DOI] [PubMed] [Google Scholar]
- 23.Lymperopoulos A, Rengo G, Koch WJ. The adrenergic nervous system in heart failure: pathophysiology and therapy. Circ Res. 2008;6: 2166–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gusso S, Hofman P, Lalande S, Cutfield W, Robinson E, Baldi JC. Impaired stroke volume and aerobic capacity in female adolescents with type 1 and type 2 diabetes mellitus. Diabetologia. 2008;51: 1317–1320. doi: 10.1007/s00125-008-1012-1 [DOI] [PubMed] [Google Scholar]
- 25.Wilson LC, Peebles KC, Hoye NA, Manning P, Sheat C, Williams MJA, et al. Resting heart rate variability and exercise capacity in Type 1 diabetes. Physiol Rep. 2017;5: e13248 doi: 10.14814/phy2.13248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peltonen JE, Koponen AS, Pullinen K, Hägglund H, Aho JM, Kyröläinen H, et al. Alveolar gas exchange and tissue deoxygenation during exercise in type 1 diabetes patients and healthy controls. Respir Physiol Neurobiol. Elsevier B.V.; 2012;181: 267–276. doi: 10.1016/j.resp.2012.04.002 [DOI] [PubMed] [Google Scholar]
- 27.Wallymahmed M, Pinkney J, Saunders S, MacFarlane I. Vascular risk factors in patients with type 1 diabetes. Pract Diabetes Int. 2005;22: 81–85. doi: 10.1002/pdi.761 [Google Scholar]
- 28.Sastre J, Pinés PJ, Moreno J, Aguirre M, Blanco B, Calderón D, et al. Metabolic control and treatment patterns in patients with type 1 diabetes in Castilla-La Mancha: the DIAbetes tipo 1 in Castilla La Mancha study. Endocrinol y Nutr. 2012;59: 539–46. doi: 10.1016/j.endonu.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 29.Livingstone SJ, Looker HC, Hothersall EJ, Wild SH, Lindsay RS, Chalmers J, et al. Risk of Cardiovascular Disease and Total Mortality in Adults with Type 1 Diabetes: Scottish Registry Linkage Study. PLoS Med. 2012;9: e1001321 doi: 10.1371/journal.pmed.1001321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McKnight JA, Wild SH, Lamb MJE, Cooper MN, Jones TW, Davis EA, et al. Glycaemic control of type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabet Med. 2015;32: 1036–1050. doi: 10.1111/dme.12676 [DOI] [PubMed] [Google Scholar]
- 31.Kodama S, Tanaka S, Heianza Y, Fujihara K, Horikawa C, Shimano H, et al. Association between physical activity and risk of all-cause mortality and cardiovascular disease in patients with diabetes: A meta-analysis. Diabetes Care. 2013;36: 471–479. doi: 10.2337/dc12-0783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McNeilly AD, Gallagher JR, Huang JT-J, Ashford MLJ, McCrimmon RJ. High-intensity exercise as a dishabituating stimulus restores counterregulatory responses in recurrently hypoglycemic rodents. Diabetes. 2017;66: 1696–1702. doi: 10.2337/db16-1533 [DOI] [PubMed] [Google Scholar]
- 33.Chiang JL, Kirkman MS, Laffel LMB, Peters AL. Type 1 diabetes through the life span: A position statement of the American Diabetes Association. Diabetes Care. 2014;37: 2034–2054. doi: 10.2337/dc14-1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
The authors cannot share the data underlying this study because the data belongs to Profil Institut für Stoffwechselforschung GmbH. Qualified researchers may request data access by contacting Profil Institut für Stoffwechselforschung GmbH (marketing@profil.com). The authors did not have any special access privileges that others would not have. Profil Institut für Stoffwechselforschung GmbH, Hellersbergstraße 9, 41460 - Neuss, Germany, Telephone +49-2131-4018-345, marketing@profil.com, https://www.profil.com.