Abstract
Background
The effects of psychiatrist staffing are unclear. The aim of this study was to assess the association of high psychiatrist staffing with prolonged hospitalization, follow-up visits, and readmission in acute psychiatric units.
Methods
A retrospective cohort study was conducted using the National Database of Health Insurance Claim Information and Specified Medical Checkups. Patients newly admitted to acute psychiatric units between October 2014 and September 2015 were followed up until September 2016. The primary exposure was a patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units). Outcomes were prolonged hospitalization of >90 days, number of follow-up psychiatric visits within 90 days after discharge, and psychiatric readmission within 90 days after discharge. Incidence rate ratios (IRRs) and their 95% confidence intervals (CIs) were estimated by using generalized estimating equations, adjusting for potential covariates.
Results
Among the 24,678 newly admitted patients at 190 hospitals, 13,138 patients (53.2%) were admitted to high-staffing units in 92 hospitals. After adjustment, high-staffing units were associated with a lower risk of prolonged hospitalization (incidence rate, 16.9 vs 21.3%; IRR, 0.79 [95% CI, 0.70, 0.89]), higher number of follow-up visits (incidence rate of ≥7 visits, 16.9 vs 13.4%; IRR, 1.06 [95% CI, 1.01, 1.12]), and lower risk of readmission (incidence rate, 13.0 vs 14.4%; IRR, 0.90 [95% CI, 0.82, 0.99]).
Conclusion
High-staffing units are associated with a reduced risk of prolonged hospitalization and readmission and an increased number of follow-up visits. Further research is needed to improve the generalizability of these findings and establish the optimal level of staffing.
Keywords: readmission rate, length of stay, quality of care, physician ratio, workforce, psychiatrist staffing
Background
A high patient-to-provider ratio is a major impediment to the provision of high quality of care and patient safety.1,2 To date, several studies have investigated the effect of patient-to-nurse ratio on mortality in acute care settings.3,4 A better understanding of the association between patient-to-nurse ratio and outcomes is important for clinical practice, unit organization, and health policy.4 Such evidence provides insights for determining the optimal level of patient-to-provider ratio. However, little attention has been paid to the effects of patient-to-physician ratio.5
To the best of our knowledge, there are only two studies on this issue in the field of psychiatric inpatient care.6,7 A cross-sectional study of 673 patients in 25 hospitals across 11 countries found that lower patient-to-psychiatrist ratio (high staffing) was associated with higher treatment satisfaction (percentage of patients with low satisfaction: 18% in high-staffing hospitals and 40% in low-staffing hospitals).6 Additionally, a cohort study of 35,884 patients in 53 hospitals in South Korea revealed that lower inpatient volume per psychiatrist (high staffing) – the total length of stay for mental disorders divided by the number of psychiatrists in a hospital – was associated with a lower 30-day readmission rate (odds for readmission in high-staffing vs low-staffing hospitals: 0.38).7 To confirm these findings, further studies should investigate the effect of psychiatrist staffing on outcomes in psychiatric inpatient care.
In Japan’s acute psychiatric care units, the patient-to-psychiatrist ratio is standardized into two types by the health insurance system. The units with high staffing are required to allocate at least one psychiatrist per 16 patients, while the units with low staffing are only required to allocate at least one psychiatrist per 48 patients.8 In this study, we aimed to assess the association of high psychiatrist staffing with prolonged hospitalization, follow-up visits, and readmission in acute psychiatric units.
Methods
Design
A retrospective cohort study was conducted using the National Database of Health Insurance Claim Information and Specified Medical Checkups (NDB). A detailed description on the NDB has been provided elsewhere.9 Briefly, the Ministry of Health, Labour and Welfare in Japan has recorded almost all claims since April 2009.10 The NDB includes information on the hospital, patient, and procedural characteristics such as hospital codes, patient identification number, sex, age group, medical practice codes, administration date of medical practice, and diagnostic codes. The NDB has been used in several studies.11–14
Setting
In Japan, there are three per diem payment plans for acute psychiatric inpatient care: 1) psychiatric emergency units, 2) psychiatric emergency and physical complication units, and 3) psychiatric acute care units. Psychiatric emergency units provide emergency and acute psychiatric care mainly in nongeneral hospitals and have one of the highest certification criteria for staffing including that at least one full-time physician per 16 patients, at least one nurse per 10 patients per day, and at least two full-time psychiatric social workers should be allocated to the unit. Psychiatric emergency and physical complication units provide emergency and acute psychiatric care for individuals with physical complications in general hospitals that provide tertiary emergency medical service. Psychiatric acute care units provide acute psychiatric care mainly in nongeneral hospitals and have lower certification criteria for staffing than psychiatric emergency units.
In this study, we focused on “psychiatric acute care unit I”, because the patient-to-psychiatrist ratio is standardized into two types in the units reimbursed by this plan. These units include 15,000 beds in >300 hospitals, accounting for 5% of all types of psychiatric beds.15 The major certification criteria for these units include that 1) the hospital should participate in the emergency psychiatric medical system coordinated by local governments; 2) at least one full-time certified psychiatrist should be allocated to the unit; 3) at least one nurse per 13 patients per day should be allocated to the unit; 4) at least one isolation room should be equipped in the unit; and 5) at least 40% of patients admitted to the unit should be discharged to the community within 3 months after admission.16 Here, discharge to the community is defined as patients discharged to home or institutions and not readmitted to psychiatric units at least 3 months after discharge. The hospital fee for the unit is 19,840 yen per patient per day during 1–30 days after admission.17
Although the standard psychiatrist staffing was defined by the health insurance system as at least one psychiatrist per 48 patients in nongeneral hospitals,8 units with high staffing (ie, at least one psychiatrist per 16 patients) can be reimbursed with an additional fee of 5,000 yen per patient per day in acute psychiatric units.17 The certification criteria for the additional reimbursement include that 1) at least one full-time psychiatrist per 16 patients should be allocated to the unit and 2) 60% of patients admitted to the unit should be discharged to the community within 3 months after admission.
Patient selection
We identified nongeneral hospitals with acute psychiatric units reimbursed through the payment plan psychiatric acute care unit I between October 2014 and September 2015. We excluded general hospitals that had ≥100 beds within the following five specialties: internal medicine, surgery, obstetrics and gynecology, otolaryngology, and ophthalmology. This is because they are required to keep a patient-to-psychiatrist ratio of 16:1 irrespective of the additional reimbursement.8 To avoid contamination, we focused only on hospitals with or without claims of additional reimbursement for all patients admitted to acute psychiatric units throughout the study period. Namely, we excluded hospitals certified as having additional reimbursement in the middle of the study period. We identified all new admissions to acute psychiatric units between October 2014 and September 2015. A single episode of psychiatric admission was defined as the period from the date of admission to an acute psychiatric unit from a community setting (ie, home or institution) or general ward to the date of hospital discharge to community settings. To increase traceability, we used the new algorithm for patient identification (ID0).18 Initial admissions to an acute psychiatric unit during the study period were included in the present study. Planned admissions for electroconvulsive therapy with a hospital stay of ≤3 days were excluded. To focus on patients at risk of readmission, patients discharged to a general ward or deceased were excluded. To ensure a follow-up period of at least 180 days after discharge, patients who continued to be hospitalized after April 1, 2016, were excluded. To control the history of psychiatric admissions as much as possible, patients who were admitted to any psychiatric unit within 180 days before the index admission were excluded and patients who had at least one claim in the database prior to the 180-day period from the index admission were included. All patients were followed up until September 30, 2016.
Outcomes
The outcomes of interest in this study were as follows: 1) prolonged hospitalization >90 days, 2) number of follow-up psychiatric visits within 90 days after discharge, and 3) psychiatric readmission within 90 days after discharge. Planned readmissions for electroconvulsive therapy were excluded from the definition of psychiatric readmission.
Exposure
The exposure of interest was a patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units). We obtained this information from claims for additional reimbursement.
Covariates
As potential covariates, we extracted information on hospital characteristics (hospital code and number of new psychiatric admissions), patient demographic characteristics (sex and age), preindex admission characteristics (Charlson index, history of psychiatric visits, and history of intensive care unit [ICU] admissions), and index admission characteristics (type of admission and principal diagnosis). These covariates were selected on the basis of evidence from previous studies and clinical experience.19–22 The number of new psychiatric admissions during the study period was calculated for each hospital based on all types of psychiatric units rather than just acute psychiatric units. Subsequently, hospitals were categorized into four classes based on the number of new psychiatric admissions (the first quartile [lowest volume] to the fourth quartile [highest volume]). The Sundararajan version of the Charlson comorbidity index score (0, 1, 2, and ≥3) was calculated using claims within 90 days prior to index admissions.23 History of psychiatric visits and ICU admissions within 90 days prior to the index admission was also identified. Type of admission was categorized into voluntary and involuntary admissions. A principal diagnosis (schizophrenia, bipolar affective disorders, unipolar depressive disorders, dementia, or others) was selected based on the algorithm defined by the Ministry of Health, Labour and Welfare.24
Statistical analyses
First, we assessed the covariate balance between high- and low-staffing units using a standardized difference, in which an absolute value of >10% indicates an important imbalance in the prevalence of a covariate between the groups.25 Second, we used generalized estimating equations with a Poisson distribution and a log-link function to account for the correlated data structure (patients clustered within hospitals) and compared the incidence rates of each outcome between high- and low-staffing units.26 All potential covariates were simultaneously entered into the models. Incidence rate ratios (IRRs) and their 95% confidence intervals (CIs) were derived from the models. Additionally, we conducted a sensitivity analysis to assess the potential effect of the NDB traceability issue. The NDB cannot identify whether patients continued to be enrolled in the database; therefore, we focused on patients who had at least one claim after 90 days from the discharge date in the sensitivity analysis. We conducted a subgroup analysis to examine whether the association between patient-to-psychiatrist ratio and outcomes varied across the levels of all covariates. We assessed the statistical significance of interaction terms with a significance level of 0.05. Statistical analyses were performed using R Version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria) with the geepack package.27
Ethics approval and informed consent
Our study protocol was approved by the Institutional Review Board at the Institute of Health Economics and Policy (no H28-002). Consent to participate was not applicable because our study was based on data from an anonymous database.
Results
Study population
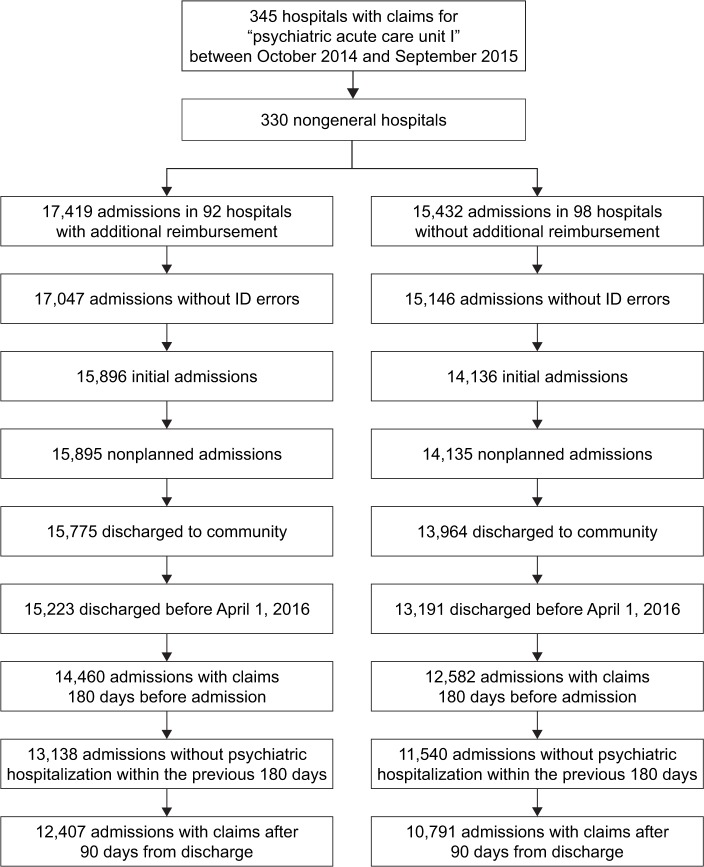
There were 345 hospitals that reimbursed claims through the payment plan psychiatric acute care unit I between October 2014 and September 2015. For main analyses, a total of 24,678 patients at 190 hospitals met the eligibility criteria (Figure 1), of whom 13,138 (53.2%) patients were admitted to high-staffing units at 92 hospitals. A comparison of sample characteristics between high- and low-staffing units showed major imbalances in hospital volume (Table 1). For sensitivity analysis, a total of 23,198 patients met the additional eligibility criterion (Figure 1).
Figure 1.
Flow diagram.
Table 1.
Sample characteristics
| Characteristics | High-staffing units (N=13,138)
|
Low-staffing units (N=11,540)
|
Standardized difference (%) | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Quartile of number of new psychiatric admissions (range) | |||||
| First quartile (103–217) | 1,874 | 14.3 | 4,197 | 36.4 | −52.5 |
| Second quartile (218–307) | 2,480 | 18.9 | 3,689 | 32.0 | −30.4 |
| Third quartile (308–417) | 4,355 | 33.1 | 1,893 | 16.4 | 39.4 |
| Fourth quartile (418–1,082) | 4,429 | 33.7 | 1,761 | 15.3 | 43.8 |
| Age (years) | |||||
| 0–19 | 297 | 2.3 | 329 | 2.9 | −3.8 |
| 20–39 | 3,425 | 26.1 | 2,528 | 21.9 | 9.8 |
| 40–64 | 5,411 | 41.2 | 4,320 | 37.4 | 7.8 |
| 65–74 | 1,862 | 14.2 | 1,739 | 15.1 | −2.5 |
| ≥75 | 2,143 | 16.3 | 2,624 | 22.7 | −16.2 |
| Sex, women | 7,345 | 55.9 | 6,459 | 56.0 | −0.2 |
| Charlson index | |||||
| 0 | 7,320 | 55.7 | 5,934 | 51.4 | 8.6 |
| 1 | 2,864 | 21.8 | 2,579 | 22.3 | −1.2 |
| 2 | 1,373 | 10.5 | 1,334 | 11.6 | −3.5 |
| ≥3 | 1,581 | 12.0 | 1,693 | 14.7 | −7.9 |
| History of psychiatric visit within 90 days | 10,312 | 78.5 | 8,722 | 75.6 | 6.9 |
| History of admission to ICU within 90 days | 297 | 2.3 | 214 | 1.9 | 2.8 |
| Voluntary admission | 7,993 | 60.8 | 7,289 | 63.2 | −4.9 |
| Principal diagnosis (ICD-10 codes) | |||||
| Schizophrenia (F2) | 4,570 | 34.8 | 4,108 | 35.6 | −1.7 |
| Bipolar affective disorders (F30–F31) | 1,415 | 10.8 | 1,068 | 9.3 | 5.0 |
| Unipolar depressive disorders (F32–F33, F341) | 2,743 | 20.9 | 2,045 | 17.7 | 8.1 |
| Dementia (F00–F03, G30–G31) | 974 | 7.4 | 1,364 | 11.8 | −15.0 |
| Other | 3,436 | 26.2 | 2,955 | 25.6 | 1.4 |
Note: Patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units).
Abbreviations: ICD, International Classification of Diseases; ICU, intensive care unit.
Main analyses
Compared to the low-staffing units, high-staffing units were associated with a lower risk of prolonged hospitalization (incidence rate, 16.9 vs 21.3%; IRR, 0.79 [95% CI, 0.70, 0.89]), a higher number of psychiatric follow-up visits after discharge (incidence rate ≥7 visits, 16.9 vs 13.4%; IRR, 1.06 [95% CI, 1.01, 1.12]), and a lower risk of psychiatric readmissions within 90 days (incidence rate, 13.0 vs 14.4%; IRR, 0.90 [95% CI, 0.82, 0.99]) (Tables 2 and S1). A sensitivity analysis focusing on patients with at least one claim after 90 days from the discharge date did not change these associations.
Table 2.
Association of psychiatrist staffing and outcomes
| Outcome | Psychiatrist staffing
|
|
|---|---|---|
| High | Low | |
| Prolonged hospitalization | ||
| Incident case, n | 2,313 | 2,692 |
| Adjusted incidence rate, % (95% CI)a | 16.9 (14.7, 19.3) | 21.3 (18.5, 24.6) |
| Incidence rate ratio (95% CI) | ||
| Crude | 0.75 (0.68, 0.84)* | Reference |
| Adjusteda | 0.79 (0.70, 0.89)* | Reference |
| Follow-up visit within 90 days | ||
| Number of visits (%) | ||
| 0 | 17.5 | 22.2 |
| 1–2 | 15.0 | 16.4 |
| 3–4 | 30.0 | 30.4 |
| 5–6 | 20.6 | 17.5 |
| ≥7 | 16.9 | 13.4 |
| Incidence rate ratio (95% CI) | ||
| Crude | 1.13 (1.05, 1.22)* | Reference |
| Adjusteda | 1.06 (1.01, 1.12)* | Reference |
| Readmission within 90 days | ||
| Incident case, n | 1,606 | 1,631 |
| Adjusted incidence rate, % (95% CI)a | 13.0 (11.4, 14.9) | 14.4 (12.6, 16.5) |
| Incidence rate ratio (95% CI) | ||
| Crude | 0.86 (0.79, 0.94)* | Reference |
| Adjusteda | 0.90 (0.82, 0.99)* | Reference |
Notes:
P<0.05.
Adjusted for hospital, number of new psychiatric admissions, sex, age, Charlson index, history of psychiatric visits, history of intensive care unit admissions, type of admission, and principal diagnosis. Patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units).
Abbreviation: CI, confidence interval.
Subgroup analyses
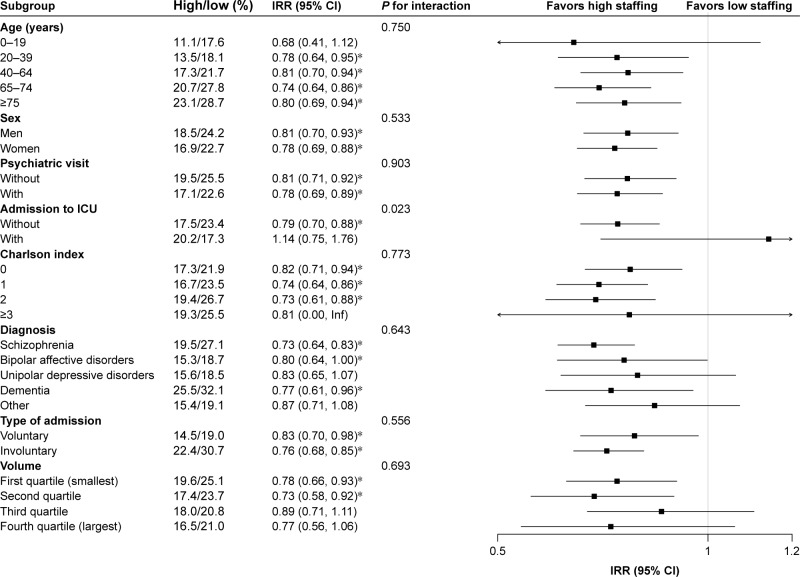
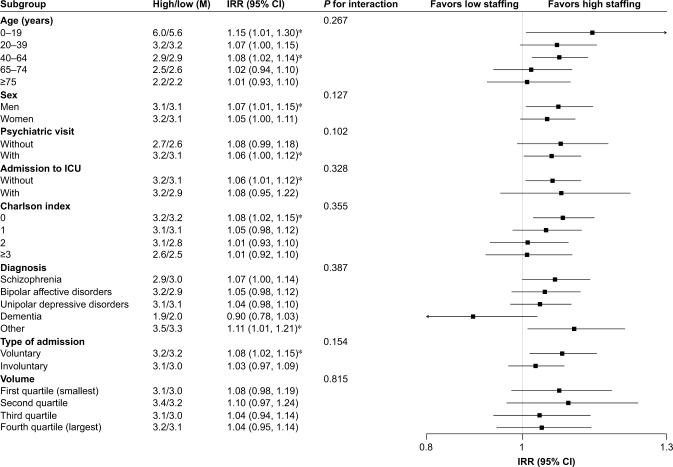
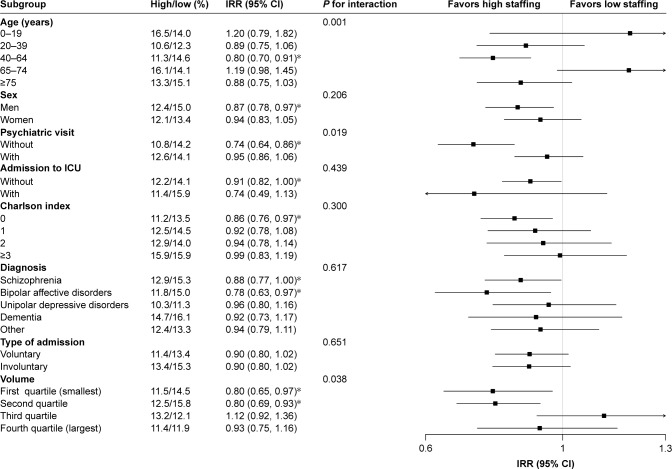
Subgroup analyses suggested that the association between psychiatrist staffing and prolonged hospital stay differed by the history of admission to ICU (P for interaction =0.023) (Figure 2). The associations between psychiatrist staffing and psychiatric follow-up visits were consistent across the subgroups (Figure 3). The association between psychiatrist staffing and psychiatric readmission differed by age (P for interaction =0.001), history of psychiatric visits (P for interaction =0.019), and hospital volume (P for interaction =0.038) (Figure 4).
Figure 2.
Subgroup analysis of the effect of psychiatrist staffing on prolonged hospital stay.
Notes: Patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units). *P<0.05.
Abbreviations: CI, confidence interval; ICU, intensive care unit; IRR, incidence rate ratio.
Figure 3.
Subgroup analysis of the effect of psychiatrist staffing on psychiatric follow-up visits.
Notes: Patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units). *P<0.05.
Abbreviations: CI, confidence interval; ICU, intensive care unit; IRR, incidence rate ratio.
Figure 4.
Subgroup analysis of the effect of psychiatrist staffing on readmission.
Notes: Patient-to-psychiatrist ratio of 16:1 (high-staffing units) vs 48:1 (low-staffing units). *P<0.05.
Abbreviations: CI, confidence interval; ICU, intensive care unit; IRR, incidence rate ratio.
Discussion
To the best of our knowledge, this is the second largest study to assess the association of high psychiatrist staffing with outcomes in acute psychiatric units. The findings of this study support the effectiveness of high-staffing units in decreasing prolonged hospitalization, increasing follow-up psychiatric visits, and reducing psychiatric readmissions. Our findings are consistent with that of a previous study that found lower readmission rates among high-staffing hospitals compared to low-staffing hospitals.7 Our results extend previous work by showing the effectiveness of psychiatrist staffing to not only reduce readmission and prolonged hospitalization rates but also increase follow-up psychiatric visits.
A potential mechanism for these effects is that psychiatrists in high-staffing units are more likely to devote more time to their patients, which may lead to perform more comprehensive psychiatric assessments, select more effective treatments, and increase patient’s satisfaction during admissions.6 Patients’ positive views on psychiatric treatments during admissions might contribute to increased follow-up psychiatric visits. In turn, continuous outpatient treatment would contribute a reduction in the risk of readmission.28
The associations between psychiatrist staffing and outcomes were generally consistent across several subgroups. We observed that admission to the ICU was a potential effect modifier between psychiatrist staffing and prolonged hospitalization. In addition, the possible effect modifiers between psychiatrist staffing and readmission included age, history of psychiatric visits, and hospital volume. Given the number of comparisons in the subgroup analyses, these findings may be due to chance. Further studies are needed to confirm these explanatory findings regarding effect modifiers.
Our findings have important implications for policymakers, as high psychiatrist staffing has a substantial impact on the risk of prolonged hospitalization and readmissions. This suggests that a financial incentive for high staffing might be a potential solution to not only increase the quality of care but also reduce the length of psychiatric hospitalization in the population. However, it remains unclear whether the associations between high staffing and outcomes vary by unit type (eg, nonacute care unit), graduation of patient-to-psychiatrist ratio, and type of health professional (eg, nurse and psychiatric social worker). Therefore, more studies are needed to improve the generalizability of our findings and establish the optimal level of staffing.
Our study has several limitations. First, we could not identify the exact patient-to-psychiatrist ratio for each hospital. Namely, a low-staffing unit has the possibility of allocating more psychiatrists than the standard 48:1. Second, we could not measure the important potential covariates such as history of psychiatric hospitalizations and history of suicide attempts,21 although we focused on patients without psychiatric admissions at least 180 days before index admissions. Third, our follow-up period was limited to a short-term interval (ie, 90 days after discharge). Long-term follow-up studies are needed to compare the cost-effectiveness of high psychiatrist staffing. Fourth, our findings were not free from selection bias. Namely, high-staffing units could select patients who are more likely to be discharged to the community within a short-term period in order to comply with the requirements for the additional reimbursement, although this would be rare in acute care settings. To confirm our findings, future research should assess clinical characteristics and compare them between high- and low-staffing units.
Conclusion
High-staffing units are associated with a reduced risk of prolonged hospitalization, an increased number of follow-up visits, and a reduced risk of readmission. These findings suggest that a financial incentive for high staffing might be a potential solution to reduce the length of psychiatric hospitalization in the population. Further research is needed to improve the generalizability of our findings and establish the optimal level of staffing.
Data availability
The Ministry of Health, Labour and Welfare has made considerable restrictions on data accessibility. This restriction made us unable to share our dataset.
Supplementary material
Table S1.
Full estimates from multivariable models for psychiatrist staffing and outcomes
| Variable | Incidence rate ratio (95% CI)a
|
||
|---|---|---|---|
| Prolonged hospitalization | Follow-up visits | Psychiatric readmissions | |
| High-staffing units (reference = low-staffing units) | 0.79 (0.70, 0.89)* | 1.06 (1.01, 1.12)* | 0.90 (0.82, 0.99)* |
| Age (years) (reference =0–19) | |||
| 20–39 | 1.09 (0.77, 1.53) | 0.64 (0.60, 0.68)* | 0.74 (0.60, 0.92)* |
| 40–64 | 1.39 (0.96, 2.01) | 0.55 (0.52, 0.59)* | 0.83 (0.67, 1.04) |
| 65–74 | 1.76 (1.21, 2.54)* | 0.45 (0.42, 0.48)* | 0.97 (0.77, 1.22) |
| ≥75 | 1.79 (1.23, 2.60)* | 0.34 (0.32, 0.37)* | 0.86 (0.67, 1.10) |
| Sex, women (reference = men) | 0.90 (0.86, 0.95)* | 1.11 (1.09, 1.13)* | 0.94 (0.88, 1.00)* |
| Charlson index (reference =0) | |||
| 1 | 0.94 (0.87, 1.00) | 0.99 (0.96, 1.01) | 1.08 (0.99, 1.19) |
| 2 | 0.96 (0.88, 1.04) | 0.97 (0.93, 1.00) | 1.05 (0.94, 1.18) |
| ≥3 | 0.87 (0.79, 0.95)* | 0.88 (0.85, 0.92)* | 1.24 (1.11, 1.38)* |
| History of psychiatric visit within 90 days | 1.02 (0.96, 1.07) | 1.58 (1.52, 1.64)* | 1.16 (1.07, 1.25)* |
| History of admission to ICU within 90 days | 1.04 (0.86, 1.26) | 1.01 (0.94, 1.07) | 1.03 (0.82, 1.29) |
| Principal diagnosis (reference = dementia) | |||
| Schizophrenia | 1.05 (0.93, 1.19) | 1.48 (1.36, 1.61)* | 1.04 (0.90, 1.21) |
| Bipolar affective disorders | 0.78 (0.68, 0.90)* | 1.72 (1.58, 1.88)* | 0.96 (0.80, 1.15) |
| Unipolar depressive disorders | 0.82 (0.72, 0.94)* | 1.68 (1.55, 1.83)* | 0.79 (0.67, 0.93)* |
| Other | 0.84 (0.73, 0.96)* | 1.39 (1.27, 1.52)* | 0.94 (0.81, 1.09) |
| Involuntary admission (reference = voluntary admission) | 1.45 (1.34, 1.56)* | 0.97 (0.95, 1.00) | 1.10 (1.03, 1.18)* |
| Quartile of number of new psychiatric admissions (reference =First quartile) | |||
| Second quartile | 0.93 (0.80, 1.06) | 1.04 (0.96, 1.13) | 1.09 (0.97, 1.21) |
| Third quartile | 0.92 (0.80, 1.06) | 1.01 (0.95, 1.08) | 1.02 (0.90, 1.16) |
| Fourth quartile (largest) | 0.90 (0.76, 1.07) | 1.06 (0.99, 1.13) | 0.91 (0.80, 1.04) |
Notes:
P<0.05.
Adjusted for hospital, number of new psychiatric admissions, sex, age, Charlson index, history of psychiatric visits, history of ICU admissions, type of admission, and principal diagnosis.
Abbreviations: CI, confidence interval; ICU, intensive care unit.
Acknowledgments
We would like to thank Editage for English language editing. This work was funded by a Research on Policy Planning and Evaluation grant from the Ministry of Health, Labour and Welfare of Japan.
Footnotes
Disclosure
During the past 3 years, YO received personal fees from Merck & Co., Inc., Janssen Pharmaceuticals, Inc., Medical Technology Association, Cando Inc., and Japan Medical Data Center. He has also received research grants from the Japan Agency for Medical Research and Development, the Ministry of Health, Labour and Welfare, the Japan Society for the Promotion of Science, the Institute for Health Economics and Policy, and the Mental Health and Morita Therapy. NaS reports grants from the Ministry of Health, Labour and Welfare, personal fees and nonfinancial support from Otsuka Pharmaceutical, Janssen Pharmaceutical KK, Eli Lilly Japan KK, Pfizer Inc., Meiji Seika Pharma Co., Ltd., MSD KK, and Daiichi-Sankyo Company, Ltd., outside the submitted work. NoS reports personal fees from Daiichi Sankyo Co., Ltd, outside the submitted work. The authors report no other conflicts of interest in this work.
Author contributions
YO, NaS, and TN contributed to the conception and design of the study. YO contributed to the acquisition of data, analyzed the data, and wrote the article. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
References
- 1.Goddard AF, Hodgson H, Newbery N. Impact of EWTD on patient:doctor ratios and working practices for junior doctors in England and Wales 2009. Clin Med (Lond) 2010;10(4):330–335. doi: 10.7861/clinmedicine.10-4-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 3.Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–1045. doi: 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- 4.Sherenian M, Profit J, Schmidt B, et al. Nurse-to-patient ratios and neonatal outcomes: a brief systematic review. Neonatology. 2013;104(3):179–183. doi: 10.1159/000353458. [DOI] [PubMed] [Google Scholar]
- 5.Ward NS, Howell MD. Intensivist-to-patient ratios in ICUs: is there a number? Curr Opin Anaesthesiol. 2015;28(2):172–179. doi: 10.1097/ACO.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 6.Krupchanka D, Khalifeh H, Abdulmalik J, et al. Satisfaction with psychiatric in-patient care as rated by patients at discharge from hospitals in 11 countries. Soc Psychiatry Psychiatr Epidemiol. 2017;52(8):989–1003. doi: 10.1007/s00127-017-1366-0. [DOI] [PubMed] [Google Scholar]
- 7.Han KT, Lee SY, Kim SJ, et al. Readmission rates of South Korean psychiatric inpatients by inpatient volumes per psychiatrist. BMC Psychiatry. 2016;16:96. doi: 10.1186/s12888-016-0804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of Health, Labour and Welfare Case-mix and quality improvement in psychiatric care. [Accessed December 4, 2012]. Available from: http://www.mhlw.go.jp/stf/shingi/2r9852000002e9b4-att/2r9852000002e9eq.pdf.
- 9.Ministry of Health, Labour and Welfare On the use of the National Database of Health Insurance Claim Information and Specified Medical Checkups. [Accessed December 4, 2017]. Available from: http://www.mhlw.go.jp/stf/shingi/2r9852000002ss9z-att/2r9852000002ssfg.pdf.
- 10.Ministry of Health, Labour and Welfare Population Census in 2015. [Accessed December 4, 2017]. Available from: http://www.e-stat.go.jp/SG1/estat/GL08020103.do?_csvDownload_&fileId=000007809775&releaseCount=3.
- 11.Okumura Y, Nishi D. Risk of recurrent overdose associated with prescribing patterns of psychotropic medications after nonfatal overdose. Neuropsychiatr Dis Treat. 2017;13:653–665. doi: 10.2147/NDT.S128278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okumura Y, Sakata N, Takahashi K, Nishi D, Tachimori H. Epidemiology of overdose episodes from the period prior to hospitalization for drug poisoning until discharge in Japan: An exploratory descriptive study using a nationwide claims database. J Epidemiol. 2017;27(8):373–380. doi: 10.1016/j.je.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kubota K, Kamijima Y, Sato T, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015;5(1):e006450. doi: 10.1136/bmjopen-2014-006450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toyokawa S, Maeda E, Kobayashi Y. Estimation of the number of children with cerebral palsy using nationwide health insurance claims data in Japan. Dev Med Child Neurol. 2017;59(3):317–321. doi: 10.1111/dmcn.13278. [DOI] [PubMed] [Google Scholar]
- 15.Ministry of Health, Labour and Welfare Inpatient care. [Accessed December 4, 2017]. Available from: http://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000165657.pdf.
- 16.Ministry of Health, Labour and Welfare Certification criteria of revision of medical fee in 2014. [Accessed December 4, 2017]. Available from: http://www.mhlw.go.jp/file/06-Seisakujouhou-12400000-Hokenkyoku/0000041257.pdf.
- 17.Ministry of Health, Labour and Welfare Hospital fee in revision of medical fee in 2014. [Accessed December 4, 2017]. Available from: http://www.mhlw.go.jp/file/06-Seisakujouhou-12400000-Hokenkyoku/0000041342.pdf.
- 18.Noda T, Kubo S, Myojin M, et al. A new algorithm for patient matching in the National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB) (in Japanese) J Health Welfare Stat. 2017;64:3–15. [Google Scholar]
- 19.Rylander M, Colon-Sanchez D, Keniston A, Hamalian G, Lozano A, Nussbaum AM. Risk factors for readmission on an adult inpatient psychiatric unit. Qual Manag Health Care. 2016;25(1):22–31. doi: 10.1097/QMH.0000000000000077. [DOI] [PubMed] [Google Scholar]
- 20.Filipcic I, Simunovic Filipcic I, Ivezic E, et al. Chronic physical illnesses in patients with schizophrenia spectrum disorders are independently associated with higher rates of psychiatric rehospitalization; a cross-sectional study in Croatia. Eur Psychiatry. 2017;43:73–80. doi: 10.1016/j.eurpsy.2017.02.484. [DOI] [PubMed] [Google Scholar]
- 21.Donisi V, Tedeschi F, Wahlbeck K, Haaramo P, Amaddeo F. Pre-discharge factors predicting readmissions of psychiatric patients: a systematic review of the literature. BMC Psychiatry. 2016;16(1):449. doi: 10.1186/s12888-016-1114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee HC, Lin HC. Is the volume-outcome relationship sustained in psychiatric care? Soc Psychiatry Psychiatr Epidemiol. 2007;42(8):669–672. doi: 10.1007/s00127-007-0214-z. [DOI] [PubMed] [Google Scholar]
- 23.Sundararajan V, Quan H, Halfon P, et al. Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med Care. 2007;45(12):1210–1215. doi: 10.1097/MLR.0b013e3181484347. [DOI] [PubMed] [Google Scholar]
- 24.Ministry of Health, Labour and Welfare [webpage on the Internet] Methods for identifying one principle diagnose. [Accessed December 4, 2017]. Available from: http://www.mhlw.go.jp/file/06-Seisakujouhou-12400000-Hokenkyoku/0000090763.xls.
- 25.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 27.Højsgaard S. Package “geepack”. [Accessed December 4, 2017]. Available from: https://cran.r-project.org/web/packages/geepack/geepack.pdf.
- 28.Lee SY, Kim KH, Kim T, et al. Outpatient follow-up visit after hospital discharge lowers risk of rehospitalization in patients with schizophrenia: a nationwide population-based study. Psychiatry Investig. 2015;12(4):425–433. doi: 10.4306/pi.2015.12.4.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Full estimates from multivariable models for psychiatrist staffing and outcomes
| Variable | Incidence rate ratio (95% CI)a
|
||
|---|---|---|---|
| Prolonged hospitalization | Follow-up visits | Psychiatric readmissions | |
| High-staffing units (reference = low-staffing units) | 0.79 (0.70, 0.89)* | 1.06 (1.01, 1.12)* | 0.90 (0.82, 0.99)* |
| Age (years) (reference =0–19) | |||
| 20–39 | 1.09 (0.77, 1.53) | 0.64 (0.60, 0.68)* | 0.74 (0.60, 0.92)* |
| 40–64 | 1.39 (0.96, 2.01) | 0.55 (0.52, 0.59)* | 0.83 (0.67, 1.04) |
| 65–74 | 1.76 (1.21, 2.54)* | 0.45 (0.42, 0.48)* | 0.97 (0.77, 1.22) |
| ≥75 | 1.79 (1.23, 2.60)* | 0.34 (0.32, 0.37)* | 0.86 (0.67, 1.10) |
| Sex, women (reference = men) | 0.90 (0.86, 0.95)* | 1.11 (1.09, 1.13)* | 0.94 (0.88, 1.00)* |
| Charlson index (reference =0) | |||
| 1 | 0.94 (0.87, 1.00) | 0.99 (0.96, 1.01) | 1.08 (0.99, 1.19) |
| 2 | 0.96 (0.88, 1.04) | 0.97 (0.93, 1.00) | 1.05 (0.94, 1.18) |
| ≥3 | 0.87 (0.79, 0.95)* | 0.88 (0.85, 0.92)* | 1.24 (1.11, 1.38)* |
| History of psychiatric visit within 90 days | 1.02 (0.96, 1.07) | 1.58 (1.52, 1.64)* | 1.16 (1.07, 1.25)* |
| History of admission to ICU within 90 days | 1.04 (0.86, 1.26) | 1.01 (0.94, 1.07) | 1.03 (0.82, 1.29) |
| Principal diagnosis (reference = dementia) | |||
| Schizophrenia | 1.05 (0.93, 1.19) | 1.48 (1.36, 1.61)* | 1.04 (0.90, 1.21) |
| Bipolar affective disorders | 0.78 (0.68, 0.90)* | 1.72 (1.58, 1.88)* | 0.96 (0.80, 1.15) |
| Unipolar depressive disorders | 0.82 (0.72, 0.94)* | 1.68 (1.55, 1.83)* | 0.79 (0.67, 0.93)* |
| Other | 0.84 (0.73, 0.96)* | 1.39 (1.27, 1.52)* | 0.94 (0.81, 1.09) |
| Involuntary admission (reference = voluntary admission) | 1.45 (1.34, 1.56)* | 0.97 (0.95, 1.00) | 1.10 (1.03, 1.18)* |
| Quartile of number of new psychiatric admissions (reference =First quartile) | |||
| Second quartile | 0.93 (0.80, 1.06) | 1.04 (0.96, 1.13) | 1.09 (0.97, 1.21) |
| Third quartile | 0.92 (0.80, 1.06) | 1.01 (0.95, 1.08) | 1.02 (0.90, 1.16) |
| Fourth quartile (largest) | 0.90 (0.76, 1.07) | 1.06 (0.99, 1.13) | 0.91 (0.80, 1.04) |
Notes:
P<0.05.
Adjusted for hospital, number of new psychiatric admissions, sex, age, Charlson index, history of psychiatric visits, history of ICU admissions, type of admission, and principal diagnosis.
Abbreviations: CI, confidence interval; ICU, intensive care unit.
Data Availability Statement
The Ministry of Health, Labour and Welfare has made considerable restrictions on data accessibility. This restriction made us unable to share our dataset.