We present a unique case of a patient with anti–dipeptidyl peptidase-like protein 6 (DPPX) encephalitis in which severe pruritus was the cardinal symptom. Anti-DPPX encephalitis is caused by cell surface autoantigens to DPPX, a subunit of the Kv4.2 potassium channel.1 Most patients had a combination of limbic encephalitis, brainstem dysfunction, diarrhea, and weight loss.1–3 We describe a patient with severe pruritus and provide long-term follow-up, offering recommendations for treatment.
Case presentation
A 57-year-old patient presented with a variety of complaints, developing over months. These started with gastrointestinal symptoms (diarrhea and abdominal pain). Blastocystis hominis infection was cultured in stool, but without improvement to treatment. Five months later, he developed cognitive decline and severe pruritus with allodynia centered on his trunk. There was severe self-neglect. Our patient was admitted on and off neuropsychiatric wards for 3 years. During progression, he also developed myoclonic jerks, autonomic failure, rigidity, and ataxia.
On neurologic examination, his consciousness was clear. The muscle tone was slightly rigid. There was severe rigidity of the trunk muscles, slight rigidity of the extremities, and antecollis. He had action myoclonus and hyperekplexia. His gait was remarkably “marionette-like,” and broad-based, tandem gate was impossible. Deep tendon reflexes of the legs were diminished. He had scratching marks from pruritus centered on his trunk and could not bear clothing.
Neurocognitive testing revealed psychomotor slowing on all tasks. Brain MRI showed bilateral temporal lobe atrophy and an aspecific white matter lesion. EEG showed slight background slowing. Routine blood examination was normal. CSF analysis showed mild lymphocytosis (12 cells/μL), a slightly elevated protein level (0.52 g/L), and matched oligoclonal bands. Extensive ancillary examinations (among others, CT-thorax/abdomen, bone marrow biopsy, and serologic tests on lues, borrelia, and HIV) were all normal. A diagnosis of progressive encephalomyelitis with rigidity and myoclonus (PERM) was established. Subsequent testing for DPPX antibodies was positive in both serum and CSF cell-based assays and confirmed by neuropil staining on immunohistochemistry. Other autoimmune antibodies were negative. A skin biopsy from the symptomatic lumbar region showed a normal intraepidermal nerve fiber density for this region.
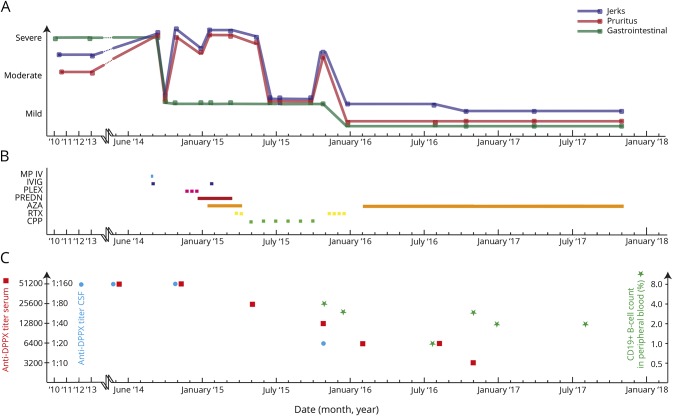
After the start of immunosuppressive therapy, our patient improved, but several relapses followed. Multiple immunosuppressive agents were tried, and only after adequate treatment with cyclophosphamide and rituximab, aiming for complete B-cell depletion, our patient improved markedly without any further relapses to the present (figure). Two and a half years after the diagnosis of PERM, our patient developed B-cell non-Hodgkin lymphoma (NHL).
Figure. Forty-two months of follow-up of clinical symptoms in parallel with therapeutic interventions and antibody titers/B-cell count.
(A) Symptom severity. (B) Medication overview. (C) Antibody titers/B-cell counts. AZA = azathioprine; CPP = cyclophosphamide; DPPX = dipeptidyl peptidase-like protein 6; IVIG = IV immunoglobulin; MP IV = IV methylprednisolone; PLEX = plasma exchange; PREDN = prednisone; RTX = rituximab.
Discussion
PERM is a syndrome that is believed to result from brainstem and spinal cord dysfunction. Patients with PERM often have glycine receptor antibodies or in a minority anti-GAD65 antibodies.4 Only recently, the association with anti-DPPX antibodies and PERM has been described.5 These cases were characterized mainly by CNS symptoms and autonomic dysfunction, while pruritus was a minor symptom.2 By contrast, in our patient pruritus, that was refractory to dermatological treatments (reviewed elsewhere) was the cardinal symptom.6
Anatomically, two pruritus-sensitive afferent pathways exist (histamine- and cowhage-stimulated pathways). From the level of the dorsal horn, the pathway travels in the contralateral spinothalamic tract and synapse onto neurons in the thalamus. The role of Kv4.2 in neurogenic pruritus is not exactly known. Genetic elimination of Kv4.2 in mice increased excitability of dorsal horn neurons resulting in enhanced sensitivity to tactile and thermal stimuli and might explain its role in neurogenic itch.7
In our patient, the normal intraepidermal nerve fiber density and the absence of an effect from dermatological treatments suggest pruritus was of central origin located at the dorsal horn induced by anti-DPPX antibodies.
In line with other forms of autoimmune encephalitis (AIE), such as anti-Caspr2 encephalitis, anti-DPPX encephalitis is less subacute, resembling a neurodegenerative disease. Fulminant and rapidly progressive (autonomic or sensory) symptoms have been attributed to paraneoplastic neuropathy associated with Hu or amphiphysin antibodies. In contrast to other AIEs, such as anti-NMDA receptor encephalitis, patients with anti-DPPX encephalitis tend to need prolonged immunosuppressive therapy. As illustrated by our case, every attempt to taper immunosuppressive therapy resulted in a very rapid decline. This necessitates the use of chronic immunosuppressive therapy, and complete B-cell depletion seems necessary.
B-cell NHL is associated with chronic immunosuppressive therapy. B-cell neoplasms developed in 3/39 patients with anti-DPPX encephalitis, remitting after rituximab.2,3 In our case, the delayed diagnosis of B-cell NHL could have been masked by treatment (steroids and rituximab). Therefore, it is important to perform diagnostic tests in advance of immunosuppressive therapy and during follow-up, especially during relapses.
Author contributions
J. Wijntjes: concept and design. M. Bechakra, M.W.J. Schreurs, J.L.M. Jongen, and A. Koppenaal: critical revision of the manuscript for important intellectual content. M.J. Titulaer: concept and design/supervision.
Study funding
No targeted funding reported.
Disclosure
J. Wijntjes reports no disclosures. M. Bechakra is supported by an Erasmus MC grant 2011. M.W.J. Schreurs received travel funding from Thermo Scientific Innova; served on the editorial board of Nederlands tijdschrift voor Allergie & Astma; and received research support from Combined Ophthalmic Research, Stichting De Merel, MDen Haag, and Stichting Blindenbelangen. J.L.M. Jongen received speaker compensation from Amgen Inc. and received research funding from Erasmus MC and Stichting Erasmus Fonds Pijnbestrijding. A. Koppenaal reports no disclosures. M.J. Titulaer received research funds for serving on the scientific advisory board of MedImmune LLC and for consultation at Guidepoint Global LLC and an unrestricted research grant from Euroimmun AG; serves on the editorial board of Neurology® Neuroimmunology & Neuroinflammation; has filed a patent for Methods for typing neurological disorders and cancer, and devices for use therein; was supported by an Erasmus MC fellowship; and has received funding from the Netherlands Organization for Scientific Research (NWO, Veni incentive), Dutch Epilepsy Foundation (NEF, project 14-19), and ZonMw (Memorabel program). Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/NN.
References
- 1.Boronat A, Gelfand JM, Gresa-Arribas N, et al. Encephalitis and antibodies to dipeptidyl-peptidase-like protein-6, a subunit of Kv4.2 potassium channels. Ann Neurol 2012;73:120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hara M, Ariño H, Petit-Pedrol M, et al. DPPX antibody–associated encephalitis. Neurology 2017;88:1340–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tobin WO, Lennon VA, Komorowski L, et al. DPPX potassium channel antibody: frequency, clinical accompaniments, and outcomes in 20 patients. Neurology 2014;83:1797–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martinez-Hernandez E, Ariño H, McKeon A, et al. Clinical and immunologic investigations in patients with stiff-person spectrum disorder. JAMA Neurol 2016;73:714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balint B, Jarius S, Nagel S, et al. Progressive encephalomyelitis with rigidity and myoclonus: a new variant with DPPX antibodies. Neurology 2014;82:1521–1528. [DOI] [PubMed] [Google Scholar]
- 6.Yosipovitch G. Chronic pruritus: a paraneoplastic sign. Dermatol Ther 2010;23:590–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu H-J, Carrasquillo Y, Karim F, et al. The Kv4.2 potassium channel subunit is required for pain plasticity. Neuron 2006;50:89–100. [DOI] [PubMed] [Google Scholar]