Abstract
Background
Emerging adulthood is a period of heightened vulnerability for problematic alcohol use. Considerable research has been devoted to reducing alcohol risks in college student populations, though far less effort has focused on their noncollege-attending peers. Research targeting nonstudent emerging adults is critical as this group is at risk for experiencing alcohol-related harms. Consequently, the main objective of the present randomized study was to examine the preliminary efficacy of a brief personalized feedback intervention (PFI) tailored for nonstudent at-risk drinkers. We also examined the influence of gender on intervention outcomes. Finally, we explored participant acceptability of the intervention.
Methods
Participants were 164 (65.9% men) emerging adults (M age = 21.98, SD = 2.02) recruited from the community. They were randomly assigned to either a 50-minute, in-person PFI or an assessment-only control group and were assessed over 9 months post-intervention.
Results
Results showed that for short-term change (1-month), the PFI condition reduced drinking significantly more than controls. For longer-term change (1-month to 9-month), both conditions continued to show gradual decline in consumption. The groups did not differ in alcohol-related problems and the intervention was equally effective for both women and men. Regarding acceptability, participants were extremely satisfied with the intervention, perceived the information to be personally relevant, and thought it provided them a new way of looking at their own drinking.
Conclusions
Overall, the present research advanced knowledge regarding an understudied and at-risk group of drinkers. This is among one of the first randomized study to evaluate a brief intervention tailored to the needs of nonstudent emerging adults based on prior formative research with this group. Our data supports PFI as a promising intervention approach for nonstudent drinkers in the community. Ultimately, this line of research aims to reduce alcohol-related health disparities associated with inequities in education.
Keywords: nonstudents, emerging adults, alcohol, alcohol-related problems, brief alcohol intervention, personalized feedback
Introduction
Emerging adulthood is a period of heightened vulnerability for problematic alcohol use. Emerging adults have the highest past-year rates of alcohol abuse and dependence (Grant et al., 2004; Substance Abuse and Mental Health Services Administration, 2014). Rates of binge drinking (at least one occasion of ≥ 5 drinks in the past month) peak between the ages 21 to 25 years (SAMHSA, 2014). The extent of negative consequences associated with heavy alcohol use in this age group is well documented (White & Hingson, 2013). Although significant research has been devoted to reducing alcohol risks in college students, far less effort has focused on their noncollege-attending peers. This is despite of all 18 to 24 year-olds in the U.S., 59% are not currently enrolled in college (U.S. Department of Education, 2014) and 46% are without any postsecondary educational attainment (U.S. Census Bureau, 2014). The majority of existing alcohol research with emerging adults is focused on college student samples, and thus, misses a sizable portion of the age group.
Recognizing the disparity, the National Institute on Alcohol Abuse and Alcoholism’s Strategic Plan for Research (2017) encourages efforts to develop and evaluate interventions targeting nonstudents. The call for research on this underserved population is especially urgent as epidemiological data suggest that drinking rates are comparably high between nonstudents and college students. For instance, Monitoring the Future (MTF) data indicated prevalence rates for lifetime, annual, daily use, and heavy drinking for students and nonstudents are 81.3% vs. 80.3%, 78.9% vs. 75.2%, 4.3% vs. 3.8%, and 32.4% vs. 28.7%, respectively (Schulenberg et al., 2017). Further, students and nonstudents have similar rates of past-year alcohol abuse (Dawson et al., 2004; 2005) and dependence (Slutske, 2005). Nonstudents, however, have been found to experience more alcohol-related problems than students (Quinn & Fromme, 2011; White et al., 2005). An analysis of drinking trends from 2002 to 2012 found that noncollege emerging adults, and noncollege women in particular, exhibit significant increases in binge prevalence while rates among full-time college students remain relatively steady (White et al., 2015). These findings are consistent with a recent report showing rates of binge drinking among 18 to 24 year olds is significantly higher among noncollege-attenders than college counterparts in 2014 (40% vs. 37.4%; Hingson et al., 2017).
The elevated prevalence rates and risks experienced by college and noncollege drinkers suggest a need to broaden the scope of research on risky drinking to include both sub-groups. College-attenders have been shown to exhibit declines or “mature out” of heavy drinking in their 20s and 30s (Chen & Jacobson, 2013; Muthén & Muthén, 2000; White et al., 2005) and to exhibit a decreasing trend in drinking quantity during college and following graduation, while drinking frequency is maintained at pre-graduation levels after graduation (Arria et al., 2016). Further, even though college status is associated with increased odds of excessive alcohol use during their early 20s, nonstudents are more likely to engage in the behavior during the latter half of the decade, suggesting that nonstudents may experience prolonged drinking-related harms (Evans-Polce et al., 2017). In addition, historical analysis of MTF data (which included college and noncollege respondents) found that more recent cohorts decelerate binge drinking more slowly during their mid-20s than past cohorts (Jager et al., 2015), indicating a potential historical shift in the course and duration of binge drinking for young adults as a whole. These findings on the transition of drinking patterns during and after young adulthood suggest that risks experienced by students and nonstudents may be similarly high and that research targeting both segments of this group is equally urgent.
A need to focus on nonstudent drinking is further bolstered by a growing body of research supporting the drinking-related vulnerabilities experienced by nonstudents. In particular, findings show that nonstudents are at higher risk than college students for alcohol-related harms during emerging adulthood (Barnett et al., 2003) and later in their 20s and 30s (Muthén & Muthén, 2000; White et al., 2005). They also are at increased risk for maintaining or increasing problematic drinking throughout emerging adulthood and adulthood (Lanza & Collins, 2006; Muthén & Muthén, 2000; White et al., 2005). Relative to those with higher education, those without postsecondary education are at higher long-term risk of developing alcohol dependence (Harford et al., 2006). Further, noncollege young adults may benefit less from existing alcohol treatments than college-attenders (Davis et al., 2017), thus raising questions about the generalizability of the large college drinking literature to nonstudents. Overall, research suggests that many nonstudent drinkers experience a pattern of risk. It is essential for researchers to develop effective interventions for nonstudents as they may be most in need but are markedly understudied.
There is strong evidence supporting personalized feedback interventions (PFIs) as an effective secondary prevention approach to reduce alcohol use and alcohol-related problems among college student populations (Miller et al., 2013; Walters & Neighbors, 2005). PFIs involve providing individuals with objective information regarding aspects of their self-reported alcohol use, problems, risk factors, and normative drinking comparisons. PFIs may be delivered as a stand-alone strategy without therapeutic guidance, within the context of a brief motivational interview (BMI), or via computer (see Walters & Neighbors, 2005; Miller et al., 2013). It has been proposed that feedback-based interventions operate by influencing the self regulation process, whereby discrepancy is developed between current behavior and relevant standards, consequently triggering behavior changes (Miller et al., 2000). In PFIs, individuals receive feedback on their alcohol use and risks, and self-evaluation follows. If sufficient discrepancy develops, then motivation for change may occur.
Evaluation of PFIs among emerging adults has been largely focused on college samples. Although limited research has tested the efficacy of PFIs in community-based samples (Hester, Squires, & Delaney, 2005), the majority of these studies have been based in medical settings (e.g., Monti et al., 2007), which could be limited in reaching emerging adults. While one prior investigation examined a brief MI intervention with nonstudents, the study focused specifically on underage drinkers between 17–20 years and short-term drinking changes (Magill et al., 2017). Considering the risk for problematic drinking by nonstudents across the spectrum of young adulthood (i.e., after age 20; Hingson et al., 2017), as well as the evidence supporting PFIs, there is sufficient basis to support investigations to evaluate short and long term impact of a PFI tailored for nonstudents.
The main objective of the present study was to examine the preliminary efficacy of a brief, single-session PFI tailored for nonstudent emerging adult at-risk drinkers. Using a randomized controlled design, we sought to examine the impact of a PFI on reducing drinking and associated negative consequences in a community-based sample of nonstudents relative to a control group through 9 months of follow-up. It was hypothesized that participants receiving the PFI would show greater reductions in alcohol consumption and problems over the follow-up compared to participants in the assessment-only control condition. As a secondary objective, we explored participant acceptability of the intervention as measured by post-intervention process measures of intervention acceptability. Finally, as an exploratory goal, we examined the influence of gender on intervention outcomes. Prior implementations of in-person alcohol interventions or feedback-based interventions do not support differential impact based on gender (e.g., Carey et al., 2012; Walters & Neighbors, 2005) but given the limited prior work of testing PFIs with this at-risk group, gender was examined as a moderator of intervention effects.
Materials and Methods
Participants
Participants were 164 (65.9% men) individuals recruited from the community of a mid-size, urban southeastern city in the U.S. Participants were compensated up to $160-$180 for completing the entire study. All participants provided informed consent. The study was approved by the university’s Institutional Review Board and followed the American Psychological Association (2010) guidelines.
Mean age of the sample was 21.98 (SD = 2.02) years. Participants were largely single/never married (71.3%) and non-parents (66.7%). Employment status was 45.75% unemployed, 25.6% part-time, and 28.0% full-time. Ethnicity was 48.2% African-American, 40.9% Caucasian, 6.7% Hispanic, 1.2% Native-American/Indian, and 3.0% “other”. Median individual income was under $10,000/year. About 85% of the sample reported past month substance use in addition to alcohol. Around 40% of the total sample reported use of one additional substance, with tobacco (29.9%) and marijuana (9.8%) as most prevalent. An additional 32.9% reported use of two additional substances, and of these individuals, concurrent tobacco and marijuana use was most prevalent (29.3%). Finally, 12.1% used three or more additional substances.
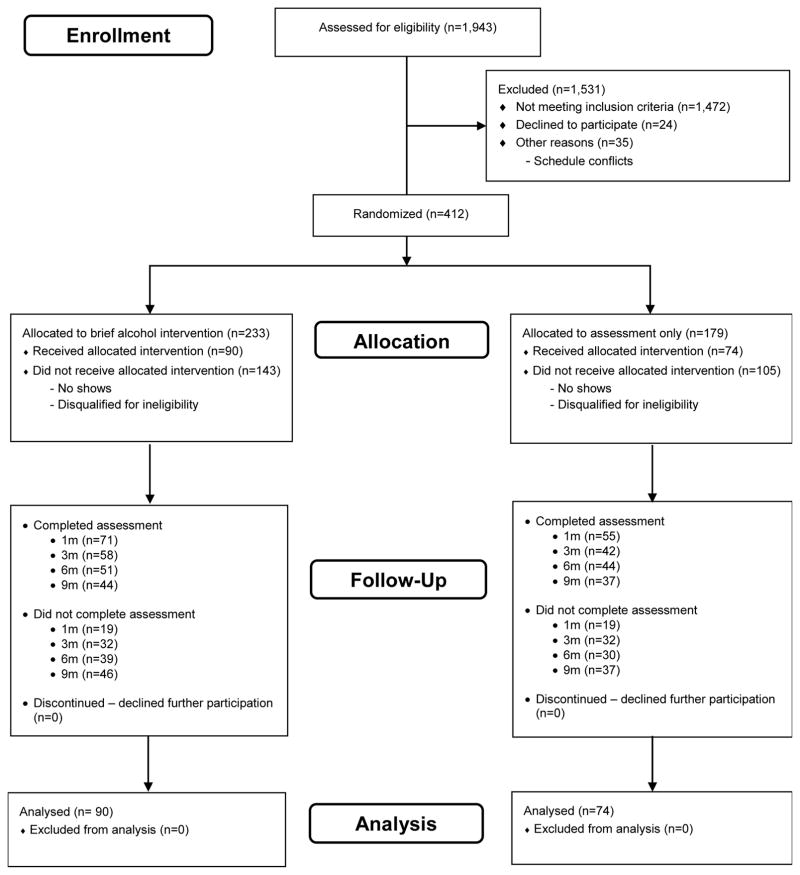
Study eligibility included being 18 to 25 years old, having no prior or current college attendance (e.g., technical/vocational programs, associate’s degree programs, or four year college programs), and not being currently enrolled in high school. High school completion was not a required eligibility criterion. They also had to report engaging in a minimum of two heavy drinking episodes (i.e., 4/5+ standard drinks for women/men on one occasion) in the past month. Exclusion criteria included consumption above 40 drinks weekly and/or a history of substance use treatment. Of those screened, 164 met eligibility criteria and attended the in-person meeting (see Figure 1).
Figure 1.
CONSORT Flow Diagram.
Study Design
The current study used a randomized controlled trial design to compare a tailored personalized feedback intervention (PFI) versus an assessment-only (AO) control group. Participants were randomly assigned to either the single-session personalized feedback intervention (PFI) condition or the assessment-only (AO) control condition1. Follow-up assessments were administered via an online survey at 1-, 3-, 6-, and 9-months. The study was completed once the minimum enrollment target was reached. Study enrollment occurred from July 2013 to February 2015, with the final follow-up assessment completed in December 2015.
Procedure
Recruitment and screening
Participants were recruited through newspaper advertisements, flyers, and internet postings (e.g., Craigslist.com, Facebook). Print advertisements were placed in local newspapers and free entertainment newspapers targeting a young adult audience. A brief initial telephone screening was conducted with interested participants to assess study eligibility. Individuals were provided with a brief description of the study (i.e., a study to understand ways to help emerging adults who drink). Participants meeting criteria were scheduled for an in-person meeting for baseline assessment, followed by the intervention session for those assigned to the PFI condition. The setting was a university-based research laboratory.
Conditions
Personalized feedback condition
The personalized feedback intervention was modeled after previous implementations of PFI with college students (Ray et al., 2014) and the Brief Alcohol Screening and Intervention for College Students (BASICS; Dimeff, 1999) manual. BASICS is a brief motivational intervention developed specifically for high-risk college drinkers that combines assessment, feedback on alcohol use and related risk factors, and provision of skills to reduce risks. The current intervention included personalized feedback regarding their alcohol consumption, alcohol-related consequences, gender-specific normative drinking comparisons, personal risk factors (e.g., dependence symptoms, family history of alcoholism), and alcohol expectancies. The intervention also included didactic material related to alcohol (e.g., effects at different BAC levels, tolerance) and drinking moderation strategies. The feedback was presented graphically in a feedback report with the individual’s information.
Our formative work with nonstudent heavy drinkers revealed important areas of focus in intervening with this group in particular (Lau-Barraco et al., 2017) and the intervention was tailored using this information to meet the needs of nonstudent drinkers in several ways. First, a robust theme to emerge from our qualitative work related to drinking for stress reduction and coping with negative emotions stemming from the various and multiple responsibilities of their daily lives. This guided the inclusion of intervention content that encouraged more adaptive ways of coping and managing stress. The information included defining stress, identifying symptoms of stress from a cognitive-behavior perspective, discussing the maladaptive negative cycle of using substances to cope, and offering strategies to reduce stress. Second, formative work suggested a high rate of co-morbid substance use among nonstudents which is associated with negative functioning (Stamates et al., 2015). Thus, participants received feedback regarding their self-reported other substance use and didactic information regarding the synergistic impact of abusing multiple substances. Third, pilot data showed that normative perceptions based on nonstudents are related to drinking but perceived norms based on college students are not (Stamates et al., 2016). Thus, the intervention was designed to correct drinking misperceptions by providing normative data specific to nonstudents rather than a general set of norms or the norms of students. Finally, heavy drinking has been linked negatively to future educational attainment (Staff et al., 2008). Achievement strivings (e.g., goal attainment) has been linked to less problematic substance use (Simons & Carey, 2003; Simons et al., 2004). Goal attainment may be facilitated by the provision of career-relevant resources and by promoting career exploration (Zikic & Saks, 2009). Accordingly, participants discussed vocational and educational options with the interventionist and received a detailed resource guide on these topics.
Feedback was delivered within the context of a brief motivational interview (BMI). Based on the guidelines delineated by Walters and Baer (2006), the 50–60 minute session was broken down to the following segments: introduction, “good/not-so-good things” motivational exercise, feedback phase, elicit readiness and interest, planning/closing, and resources review. The session was conducted following the general principles of MI (Miller & Rollnick, 2002): express empathy, develop discrepancy, roll with the resistance, and support self-efficacy. The full intervention protocol is available upon request from the study authors.
Assessment only condition
Identical to the PFI condition, AO participants were consented and completed the baseline assessment in-person with an interventionist. At the conclusion of the meeting, they were provided with a list of community resources related to drinking and were given instructions for study follow-up assessments.
Intervention fidelity
Intervention integrity and adherence was ensured through several methods. First, interventionists received ongoing supervision from the primary author, a clinical psychologist with training and experience in MI techniques. Second, sessions were taped and reviewed by the supervisor with feedback given to the interventionist on the use of MI. Third, interventionists used a checklist to rate whether the core intervention components (e.g., feedback on alcohol consumption and consequences, normative drinking comparisons, personal risk factors, moderation strategies) were covered after each session (Walters et al., 2009a). Sessions were audio recorded, and a randomly selected subset of sessions (20%) was reviewed for protocol adherence by the supervisor.
Consistent with prior research (Monti et al., 2007; Marlatt et al., 1998), PFI participants provided a measure of their perceptions of the interventionist’s MI-consistent skills. Participants rated the following on a scale from 1 (strongly disagree) to 7 (strongly agree): the counselor seemed warm and understanding (M = 6.93, SD = .3), I felt comfortable talking with my counselor (M = 6.95, SD = .26), the counselor genuinely cared about me as a person (M = 6.78, SD = .63), the counselor listened to what I had to say (M = 6.97, SD = .18), the counselor helped me believe that I can change my drinking if I want to (M = 6.84, SD = .55), the counselor made me feel that it is up to me to make decisions about my drinking and what I do when I drink (M = 6.91, SD = .39), the counselor tried to convince me to quit drinking or using substances (M = 2.49, SD = 2.10), and the counselor was judgmental of me and my attitudes towards my use of alcohol and substances (M = 1.64, SD = 1.84).
Interventionist training
Interventionists completed a 2-day workshop on motivational interviewing. They also completed readings on motivational-based brief alcohol interventions and motivational interviewing. Each interventionist submitted at least three taped practice sessions and was given feedback by the supervising clinical psychologist prior to seeing participants.
Follow-up procedures
Follow-up assessments were administered via an online survey at 1-, 3-, 6-, and 9-months. To facilitate participant retention, the research coordinator made telephone calls, sent text messages, and sent email reminders. At baseline, participants completed a locator form indicating contact information for close family and friends whom were contacted when participants could not be reached.
Participant evaluations
Following the PFI session, participants rated their experience with the intervention. They were asked: (1) I would recommend this intervention to a friend, (2) the intervention was thorough and complete, (3) I found the information provided as personally relevant, (4) the intervention gave me a new way of looking at my alcohol and substance use, (5) I am likely to use the information provided to make decisions about my drinking, and (6) overall, how satisfied were you with the intervention session. Questions were rated from 1 (strongly disagree/dissatisfied) to 7 (strongly agree/satisfied).
Measures
Alcohol use
Alcohol consumption was assessed using the Daily Drinking Questionnaire (DDQ; Collins et al., 1985). Participants reported the number of standard drinks (e.g., 12-ounce beer, 5-ounce wine, or 1.5 ounce liquor) consumed and duration each day during a typical week in the past 3 months. Indices of weekly drinking derived from the DDQ were: total quantity, frequency of drinking days, number of heavy drinking days (days where 4/5+ drinks for women/men were consumed), proportion of heavy drinking days out of total drinking days, maximum number of drinks on the heaviest drinking day, and typical blood alcohol concentration (BAC; see Matthews & Miller, 1979).
Alcohol problems
Alcohol-related problems were measured by the Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ; Kahler et al., 2005). The B-YAACQ is a 24-item, yes-no format questionnaire assessing negative drinking-related consequences experienced during the past month. Items were summed to create an overall score (ranging from 0 to 24), with higher scores indicating greater severity. For the present study, internal consistency ranged from .88 to .93 across the assessment timepoints.
Demographics
Self-reported demographic information (e.g., age, gender, ethnicity, employment, income, parent status, relationship status, and drug use history) were collected.
Analysis Approach
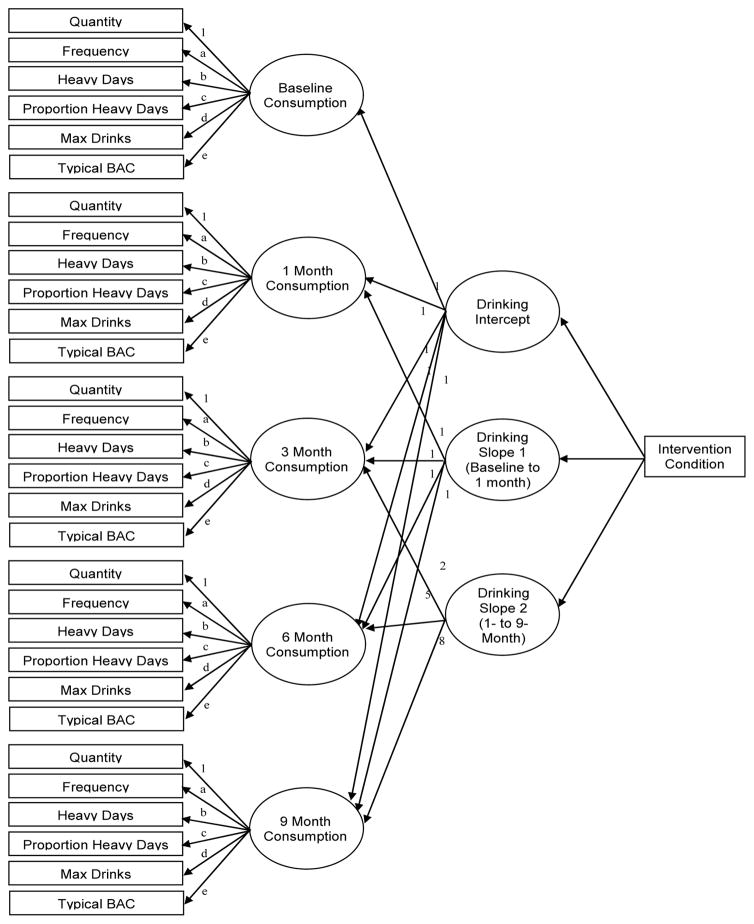
To examine the effect of the intervention on overall alcohol consumption, a curve-of-factors model was used (see Figure 2). Drinking quantity, drinking frequency, number of heavy drinking days, proportion of heavy drinking days, maximum number of drinks, and typical BAC were included as indicators for an overall consumption latent variable at each timepoint. Drinking quantity was used to scale the factor; thus, consumption is referred to as “drinks” throughout, even though the consumption latent variable represents drinks (i.e., drinking quantity, maximum number of drinks), days (i.e., drinking frequency, number of heavy drinking days), and proportions/concentrations (i.e., proportions of heavy drinking days, typical BAC). Loadings for consumption were constrained to equality across timepoints (as shown via corresponding letters in Figure 2). Constructs were correlated with adjacent timepoints (e.g., baseline quantity with 1 month quantity, 1 month quantity with 3 month quantity). A latent growth model was fitted to the consumption latent variables with an intercept factor (representing baseline consumption), a slope 1 factor (representing initial change, or growth from baseline to 1 month), and a slope 2 factor (representing maintenance, or growth from 1 month to 9 months). Loadings for the intercept factor were 1 for all timepoints; loadings for slope 1 were 0 for baseline, and 1 for all follow-up timepoints, representing growth since baseline to month 1; loadings for slope 2 were 0 for baseline and 1 month consumption, 2 for month 3, 5 for month 6, and 8 for month 9, representing growth since month 1. Condition was included as a dummy-coded predictor (0 = AO control condition, 1 = PFI condition) of the latent growth factors.
Figure 2.
Piecewise latent growth models testing the feedback effect for overall consumption (a curve-of-factors model) and alcohol-related problems. Intervention condition was coded as 0 = Assessment Only, 1 = Personalized Feedback Intervention. Factor loadings with matching letters (i.e., matching outcome indicators) were constrained to equality.
To examine the effect of the intervention on alcohol-related problems, the same latent growth approach was used. The factors for intercept, slope 1, and slope 2 had the same loadings as described above, but loaded onto the alcohol-related problems indicator. To make the distribution of problems more approximately normal, a log transformation of problems plus a constant of 1 was used. The consumption model controlled for gender at baseline; the alcohol-related problems model did not due to a lack of association. For all analyses, Mplus (version 7.11) was used. Due do the non-normal distribution for most drinking data, bootstrapping used for both models with 5,000 draws using EM estimation, and 95% bias-corrected confidence intervals were used to determine significance at the p < .05 level. Parameters were estimated using all available data, assuming data were missing-at-random (MAR).
Finally, the latent growth model for overall consumption was followed up by a series of between-subjects t tests to examine between-group differences for each alcohol indicator at 1-month and 9-months after baseline using multiple imputation to address missing follow-ups. This allowed a more detailed examination into differences for specific alcohol indictors at specific points in time. In addition, means were examined for participant evaluations of the PFI.
Results
Preliminary Analyses
Baseline comparison
The two conditions did not significantly differ at baseline on age, gender, ethnicity, living situation, relationship status, employment, or having children (see Table 1 for baseline demographic characteristics by condition). Further, the two conditions did not differ on either overall alcohol consumption or alcohol-related problems (see column labeled “Influence of Condition” on Table 2). Further, t-test and chi-square analyses confirmed that the two conditions did not differ in age, gender, ethnicity, living situation, relationship status, employment, or having children.
Table 1.
Baseline Demographic Differences between Conditions
| Variable | AO (n=74) | PFI (n=90) | df | t | p |
|---|---|---|---|---|---|
|
|
|
||||
| M (SD) | M (SD) | ||||
| Age | 21.97 (1.94) | 21.99 (2.10) | 153 | −0.55 | .957 |
|
| |||||
| n (%) | n (%) | df | c2 | p | |
|
| |||||
| Gender | 1 | 1.17 | .279 | ||
| Men | 52 (70.3) | 56 (62.2) | |||
| Women | 22 (29.7) | 34 (37.8) | |||
| Ethnicity | 3 | 4.71 | .194 | ||
| Caucasian/White | 27 (36.5) | 40 (47.1) | |||
| Native American/Indian | 2 (2.7) | 0 (0.0) | |||
| African American/Black | 41 (55.4) | 38 (44.7) | |||
| Hispanic/Latino | 4 (5.4) | 7 (8.2) | |||
| Missing | 0 | 5 (5.6) | |||
| Living Situation | 1 | 3.19 | .074 | ||
| A house, apartment, or room (not affiliated with a college) | 34 (47.9) | 54 (62.1) | |||
| A parent’s or relative’s home | 37 (52.1) | 33 (37.9) | |||
| Missing | 3 (4.1) | 3 (3.3) | |||
| Relationship Status | 3 | 3.03 | .387 | ||
| Single/Never married | 57 (77.0) | 60 (66.7) | |||
| Living with partner | 11 (14.9) | 15 (16.7) | |||
| Married | 3 (4.1) | 8 (8.9) | |||
| Divorced | 3 (4.1) | 7 (7.8) | |||
| Employment | 3 | 7.34 | .062 | ||
| Yes, part-time only | 17 (23.0) | 25 (28.1) | |||
| Yes, full and part-time | 6 (8.1) | 9 (10.1) | |||
| Yes, full-time only | 9 (12.2) | 22 (24.7) | |||
| Unemployed | 42 (56.8) | 22 (37.1) | |||
| Missing | 0 | 12 (13.3) | |||
| Children | 1 | .000 | 1.000 | ||
| Yes | 23 (33.3) | 29 (33.3) | |||
| No | 46 (66.7) | 58 (66.7) | |||
| Missing | 5 (6.8) | 3 (3.3) | |||
Note. PFI = personalized feedback intervention group, AO = assessment only group. Missing values are provided for descriptive information and were not used as categories in chi-square analyses.
Table 2.
The Influence of Intervention Condition on Consumption and Problems
| Outcome | Intercept
|
Influence of Condition
|
||||
|---|---|---|---|---|---|---|
| b | β | 95% CI | b | β | 95% CI | |
| Baseline Factor | ||||||
| Overall Consumption | 23.22* | 1.197 | [18.69, 27.85] | −1.08 | −0.034 | [−6.26, 4.34] |
| Alcohol-Related Problems | 1.98* | 2.693 | [1.80, 2.16] | −0.02 | −0.016 | [−0.26, 0.21] |
| Slope 1: Growth from Baseline to 1 Month | ||||||
| Overall Consumption | −4.09* | −0.365 | [−7.06, −1.07] | −3.93* | −0.174 | [−8.20, −0.29] |
| Alcohol-Related Problems | −0.25* | −0.470 | [−0.51, −0.03] | −0.22 | −0.205 | [−0.50, 0.10] |
| Slope 2: Growth from 1 Month to 9 Months | ||||||
| Overall Consumption | −1.01* | −0.727 | [−1.60, −0.55] | 0.40 | −0.143 | [−0.18, 1.10] |
| Alcohol-Related Problems | −0.05* | −0.582 | [−0.09, −0.01] | 0.05 | 0.293 | [−0.01, 0.11] |
Note. 95% CI = 95% bias-corrected bootstrapped confidence intervals with n = 5,000.
p < .05.
Retention
Follow-up rates were 76.8% at 1-month, 61.0% at 3-month, 57.9% at 6-month, and 49.4% at 9-month follow-up. As determined via t test, chi-square, and ANOVA analyses, attrition was unrelated to condition assignment as well as demographic characteristics (i.e., gender, ethnicity, age, living situation, relationship status, employment, having children). Of the baseline drinking variables, only frequency of drinking was associated with attrition (p < .05), such that higher drink frequency was related to higher attrition.
Outliers
There were no outliers detected for alcohol-related problems, drinking frequency, number of heavy drinking days, and proportion of heavy drinking. Four outliers were reduced for alcohol quantity at baseline, eight at 1-month, four at 3-month, two at 6-month, and one at the 9-month assessment. Four outliers were reduced for peak number of drinks at the 1-month follow-up, four at 3-month, and one at 9-month. None were detected for highest number of drinks at baseline or the 6-month follow-up.
Latent Growth Model
Consumption
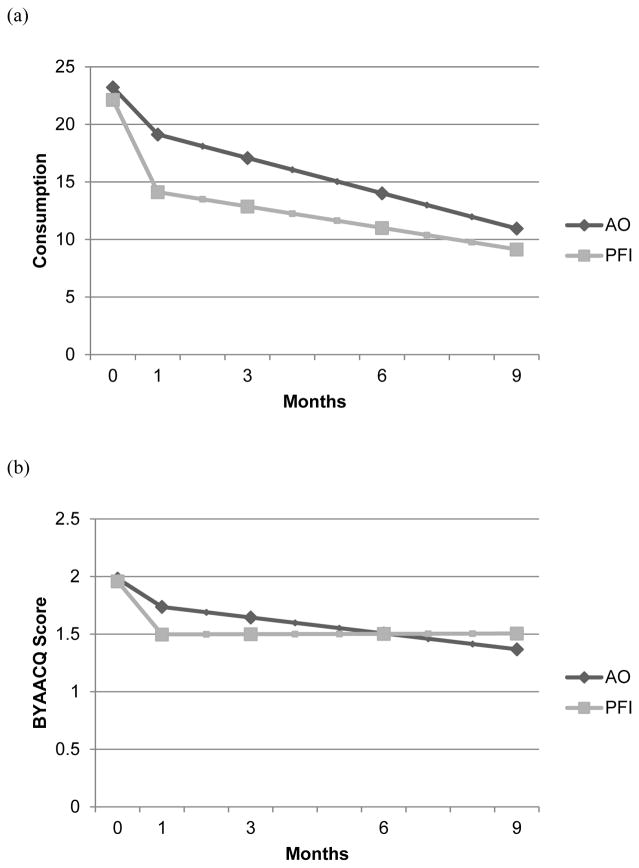
As seen in Table 2, the intercept for the slope 1 growth factor indicates that the AO control condition significantly decreased their alcohol consumption from baseline to 1-month after the intervention. However, the PFI condition reduced their drinking significantly more (by approximately 4 “drinks” in the scale of the consumption factor). The intercept for the slope 2 growth factor (i.e., “maintenance”) indicates that the AO control condition continued to significantly reduce their drinking from 1-month to 9-months post-intervention (by approximately one “drink” per month in the scale of the consumption factor). The PFI condition was not significantly different in their trajectory. The trajectories of both groups can be seen in panel (a) of Figure 3. The AO control group experiences an immediate drop in drinking post-intervention, and a continued gradual decline through month 9. The PFI group experiences a significantly stronger drop in drinking post-intervention, and also continues to gradually decline through month 9.
Figure 3.
Modeled trajectories for overall consumption (panel a) and alcohol-related problems (panel b) by condition. AO = assessment-only control group, PFI = personalized feedback intervention group, BYAACQ = Brief Young Adult Alcohol Consequences Questionnaire. Note that a natural log-transformation was used for BYAACQ score.
Problems
As seen in Table 2, the intercept for the slope 1 problems growth factor indicates that alcohol-related problems significantly decreased for the AO control condition from baseline to 1-month after the intervention. In addition, the PFI condition experiences a slightly stronger decline, but not significantly so. The intercept for the slope 2 growth factor indicates that the AO control condition continues to experience significant declines in problems from month 1 to month 9. The intercept for the slope 2 growth factor indicates that the AO control condition continues to experience significant declines in problems from month 1 to month 9. The PFI condition is not significantly different from this trajectory, but as seen in Figure 3, their trajectory appears to be very slight.
Between-group Differences
Table 3 presents the results of between-subjects t tests and effect sizes comparing the two conditions at 1-month (immediately post-intervention), and at 9-month (longer-term maintenance) follow-up. Participants in the PFI condition consumed significantly fewer drinks than participants in the AO condition at month 1, indicating a significant intervention effect, and experienced significantly fewer heavy drinking days at month 9. However, no other individual alcohol indicators demonstrated significant differences. This may be because participants in the AO condition also experienced significant reductions in alcohol outcomes.
Table 3.
Means and Differences between Conditions on Drinking Variables across Time
| PFI Mean (SD) |
AO Mean (SD) |
PFI vs. AO Independent samples t-test for 1m and 9m |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Base- line |
1m | 3m | 6m | 9m | Base- line |
1m | 3m | 6m | 9m | 1m Mean Diff |
t (d) | 9m Mean Diff |
t (d) |
| Quantity | 23.06 (20.17) | 14.34 (13.34) | 10.84 (12.36) | 10.28 (12.21) | 8.38 (12.88) | 25.50 (23.07) | 18.89 (15.18) | 17.21 (16.67) | 14.01 (13.56) | 14.40 (14.54) | 4.56 | 2.01* (2.93) | 6.22 | 1.50 (3.38) |
| Frequency | 4.07 (1.74) | 3.48 (2.39) | 2.99 (2.94) | 2.43 (2.94) | 2.01 (2.93) | 4.77 (2.02) | 4.35 (2.40) | 4.19 (3.11) | 3.56 (2.82) | 3.46 (3.19) | 0.87 | 1.83 (1.33) | 1.45 | 1.36 (1.59) |
| HD days | 2.12 (1.9) | 1.31 (1.84) | 1.16 (1.56) | 1.07 (1.82) | 0.58 (1.66) | 2.31 (2.24) | 1.92 (2.17) | 1.31 (1.70) | 1.14 (1.83) | 1.40 (1.77) | 0.61 | 1.87 (0.98) | 0.83 | 2.22* (1.27) |
| Prop HD days | 0.51 (.37) | 0.35 (.41) | 0.35 (.38) | 0.26 (.41) | 0.21 (.40) | 0.45 (.38) | 0.39 (.39) | 0.24 (.34) | 0.24 (.40) | 0.30 (.42) | 0.05 | 0.67 (0.25) | 0.09 | 1.22 (0.38) |
| Peak drinks | 8.06 (7.02) | 4.94 (3.83) | 4.15 (3.69) | 3.63 (4.08) | 3.79 (4.62) | 8.03 (7.90) | 6.09 (4.39) | 5.43 (4.62) | 4.25 (4.58) | 4.52 (5.110 | 1.06 | 1.04 (0.27) | 0.54 | 0.40 (0.58) |
| Typical BAC | 0.07 (.07) | 0.05 (.05) | 0.04 (.05) | 0.03 (.06) | 0.05 (.07) | 0.17 (.07) | 0.05 (.06) | 0.05 (.07) | 0.05 (.07) | 0.03 (.07) | 0.01 | 0.67 (0.07) | −0.02 | −0.70 (−0.13) |
| Problems | 7.66 (5.02) | 6.24 (6.05) | 5.30 (6.34) | 6.74 (7.87) | 6.13 (8.59) | 8.34 (5.70) | 7.74 (6.49) | 6.78 (7.67) | 6.04 (7.31) | 5.86 (8.75) | 1.50 | 1.30 (1.40) | −.270 | −0.12 (−0.18) |
Note. PFI = personalized feedback intervention group, AO = assessment only group, Diff = difference, Quantity = total number of drinks, Frequency = total number of drinking days, HD days = number of heavy drinking days, Prop HD days = proportion of heavy drinking days, Peak drinks = maximum number of drinks, Typical BAC = typical blood alcohol concentration, Problems = number of alcohol-related problems experienced, 1m = 1-month, 3m = 3-month, 6m = 6-month, 9m = 9-month, d = Cohen’s d. Also note that results reported for peak drinking at 1 month reflect sex-adjusted means. Other means were not adjusted because sex was not a significant predictor.
To further explore how the intervention impacted the PFI group as compared to the natural reductions observed in the AO group, effect sizes were calculated for each reduction type. Cohen’s d values represent the strength of the decline for each outcome from baseline to 1 month, and from baseline to 9 months. As seen in Table 4, effect sizes at 1-month were all considered “small” for the AO group, with some outcomes (i.e., proportion of heavy days, typical BAC, and problems) not even reaching the cutoff to be considered “small”. By comparison, the majority of reductions by the PFI group would be considered “medium” (i.e., quantity, number of heavy days, proportion of heavy days, peak drinks). Reductions for both groups increase in size for the 9-month follow-up, but all outcomes (except quantity) are considered “small” for the AO group, whereas all outcomes (excepting BAC and problems) were considered “medium” for the PFI group.
Table 4.
Within-subject Effect Sizes (Cohen’s d)
| Measure | PFI
|
AO
|
||
|---|---|---|---|---|
| 1-month | 9-month | 1-month | 9-month | |
| Quantity | .57 | .70 | .47 | .51 |
| Frequency | .28 | .74 | .23 | .41 |
| HD days | .52 | .75 | .22 | .38 |
| Prop HD days | .54 | .66 | .19 | .31 |
| Peak drinks | .50 | .57 | .30 | .44 |
| Typical BAC | .46 | .23 | .17 | .40 |
| Problems | .28 | .16 | .10 | .26 |
Note. PFI = personalized feedback intervention group, AO = assessment only group, Quantity = total number of drinks, Frequency = total number of drinking days, HD days = number of heavy drinking days, Prop HD days = proportion of heavy drinking days, Peak drinks = maximum number of drinks, Typical BAC = typical blood alcohol concentration, Problems = number of alcohol-related problems experienced.
Gender Effects
Gender was examined as a moderator of intervention and maintenance effects detected for alcohol consumption in the latent growth model. Gender and condition were both included as dummy coded predictors. An interaction term was created by multiplying the two dummy coded predictors, representing if the condition effect varied by gender. The same overall consumption model was conducted, excepting that all three predictors (gender, condition, and interaction term) were included for all three latent growth factors (baseline, slope 1, and slope 2). Neither gender nor its interaction was a significant predictor of any of the growth factors (ps > .05)
Duration of Effects
To determine the duration of the intervention effect, we explored when alcohol consumption would return to baseline levels. This approach allowed for more precise estimates of duration by revealing the exact time point at when the experimental condition could no longer be distinguished from the control condition. By knowing exactly when the intervention effects start to wane, this could inform future efforts to time potential booster sessions to extend the impact of the intervention.
Based on the assumption that the AO condition represented the untreated population, we examined when the predicted score from the modeled trajectories would return to equivalent levels using confidence intervals (CIs). Bias-corrected bootstrap CIs at the 95% level were created around baseline levels of consumption for the AO condition. Model parameters were used to calculate estimated consumption across time for the PFI condition. Once values fell within the constructed baseline CIs, the intervention effect would be considered extinguished. For overall consumption, trajectories never approached baseline levels within the period observed (through 9 months), because they continued to decline. This approach was not used for alcohol-related problems, as there was not an initial intervention effect to explore.
The approach described above established that consumption for the PFI condition did not return to baseline levels equivalent to non-intervention. However, the AO condition also experienced a significant decline in drinking post-intervention, as well as a continued gradual decline through month 9. Although the initial decline was significantly stronger for the PFI condition, their maintenance trajectory was not as strong. Therefore, we also examined when estimated drinking for the PFI condition was no longer concurrently distinguishable from the AO control condition. Therefore, we conducted a series of models identical to the original model testing the intervention effect on overall consumption, but re-centered time loadings so that the intercept represented overall consumption for the control group at month 1 (model 1), month 3 (model 2), month 6 (model 3), and month 9 (model 4). This created 95% bias-corrected bootstrap CIs around each point estimate of consumption by the AO control condition, and allowed us to compare these intervals to the point estimate of consumption by the PFI condition. At month 1, consumption by the PFI group did not fall within the 95% CI for the AO control group, indicating that their consumption was still significantly lower than control group. We found that by month 3, consumption by the PFI group did fall within the 95% CI for the AO control group, indicating equivalence, or that the effect was no longer maintained.
Participant Evaluation of Intervention
Participants rated the intervention highly. They would recommend the intervention to a friend (M = 6.76, SD = .63), found the intervention information to be accurate (M = 6.16, SD = 1.18), found the information provided to be personally relevant (M = 6.24, SD = 1.21), believed the intervention provided them a new way of looking at their alcohol and substance use (M = 6.54, SD = .97), are likely to use the information provided to make decisions about their drinking (M = 6.28, SD = 1.07), and were extremely satisfied with the intervention (M = 6.79, SD = .46).
Discussion
The present study evaluated the initial efficacy of a tailored PFI for nonstudent emerging adults in reducing consumption and associated problems. Participants recruited from the community were randomly assigned to a 50-minute in-person PFI or AO control group and were assessed over 9 months post-intervention. This study represents one of the first trials to date that tested a tailored PFI targeted for noncollege-attending emerging adult hazardous drinkers. We also sought to explore participant acceptability of the tailored intervention.
For immediate changes in drinking from baseline to 1-month post-intervention, as hypothesized, the PFI condition was associated with greater drinking reductions than the AO control group. While both conditions did decrease their consumption by 1 month, the PFI condition showed greater declines than the controls. Intervention participants reduced their consumption significantly more than control participants at approximately 4 “drinks” (in the scale of the consumption factor) at 1-month follow-up. When examining between-group differences of individual drinking indices at 1 month, control participants drank significantly more at an average of about 19 drinks weekly versus 14 drinks for PFI participants.
For maintenance of drinking changes from 1 month to 9 months following the intervention, both conditions continued to gradually decline in consumption through 9 months. Between-group differences of individual drinking outcomes at 9 months indicated that PFI participants reported an average of 0.6 days of heavy drinking per week while control participants reported 1.4 days. One reason that the control group decreased drinking in the absence of an active intervention could be related to simply completing the study assessments. Reactivity to alcohol assessment has been demonstrated to reduce risky drinking (Walters et al., 2009b), such that responding to alcohol use and consequences questions may affect drinking behaviors. This reactivity could mask stronger intervention effects and also explain the reductions observed in the assessment-only control group. Pertaining to gender, we did not find that gender moderated any of the intervention effects suggesting that the intervention worked equally well for women and men.
With regard to alcohol-related problems, we did not find the groups to exhibit significantly different trajectories. PFI participants experienced slightly, although not significantly, stronger declines from baseline to 1 month and both groups decreased alcohol-related problems over the 9 months. The lack of a commensurate impact on problems in light of observed immediate decreases in drinking may seem a bit surprising; however, this is in line with other studies of brief alcohol interventions showing null results on problems (e.g., Leeman et al., 2016) or differential impact on problems versus use (e.g., Borsari et al., 2012). It is also consistent with research showing brief alcohol intervention’s impact on problems to be relatively weaker in magnitude than consumption (Tanner-Smith et al., 2015). The absence of reductions in problems could also be related to the sensitivity of the B-YAACQ to measure changes in alcohol-related problems in our sample. The B-YAACQ was developed to assess consequences experienced by college students, and thus, may not have been ideal for use with a nonstudent population.
To further explore the intervention’s impact on drinking as compared to the natural reductions observed in the control group, effect sizes were examined to determine the magnitude of decline for each drinking outcome from baseline to 1 month and baseline to 9 months for both groups. For the AO control group at 1 month, Cohen’s d values largely fell within the “small” range, with several drinking indices falling below the cut-off (e.g., typical BAC, proportion of heavy drinking days). For the PFI group, however, effect sizes for the majority of drinking indices were in the “medium” range. As such, the reductions for both groups increase in size for the 9-month follow-up, but all outcomes (except quantity) were considered “small” for the AO group, whereas the majority of outcomes were considered “medium” or “medium-to-large” for the intervention group. In sum, while participants in both conditions exhibited reductions in consumption over time, the PFI participants exhibited stronger initial reductions at 1-month post-intervention and they also exhibited generally a stronger magnitude of change from baseline to 9 months relative to controls.
In determining the duration of the intervention effect, we found that the impact of the brief intervention lasted between 1 to 3 months. This suggests that additional efforts are needed to maintain the influence of the intervention beyond the initial months. This finding has clear implications for intervention refinement. It highlights the potential benefit of implementing maintenance strategies to prolong intervention effects and promote the long-term maintenance of drinking reduction. One such strategy may be the administration of booster follow-up sessions. The implementation and evaluation of the incremental benefit of booster sessions over the initial intervention remains relatively unexplored in brief alcohol interventions with the exception of only a small handful of studies to date with mixed results (e.g., Braitman & Henson, 2016; Caudill et al., 2007; Longabaugh et al., 2001). Many questions remain to assess the application of boosters to enhance initial intervention effects including when it is best to administer the booster, what the ideal dosing is (number and length of sessions), and what is the best modality of the booster (e.g., in-person, phone check-ups, text messaging). Research on the maintenance of initial risk reduction and strategies to maximize intervention efforts warrant more attention.
Another objective of the present investigation was to assess participant acceptability of the tailored intervention. Overall, participants rated the intervention highly. They were extremely satisfied with the intervention and would recommend the intervention to a friend. Participants perceived the intervention information to be personally relevant. This may be particularly important given that personally relevant interventions could lead to increased central processing by individuals and consequently leading to stronger drinking changes (Doumas, 2014; Petty et al., 2009). Participants endorsed strongly that the intervention provided them a new way of looking at their alcohol use and they were likely to use the information provided to make decisions about their drinking. This overwhelmingly positive reaction to the intervention supports the continued development of feedback-based brief interventions or other motivationally-based interventions for nonstudent hazardous drinkers.
Building on the current promising results, future work is warranted to test this tailored intervention in a rigorous full efficacy trial, with an extended follow-up period. Further, as noted previously, efforts to develop methods and strategies for maintaining and enhancing initial intervention effects deserves more attention. Since the intervention was successful in producing immediate reductions in drinking, efforts to capitalized on or maximize this initial effect may be a fruitful future research direction. Another valuable next step would be to adapt the intervention to a web-based format delivered without therapeutic guidance. While a face-to-face interventions may be ideal, they may not be best suited for many nonstudents due to access barriers (e.g., less reliable transportation, less job or schedule flexibility). In the present study, a sizable portion of the randomized sample did not attend the in-person study session following telephone screening. This suggests that efforts are needed to offer alternative modes of intervention delivery for nonstudent drinkers. An efficacious web-based tailored PFI could maximize reach to those who might otherwise not receive services and provide a less costly and a more flexible alternative to address heavy drinking in this population.
Finally, future intervention trials should focus on maximizing study retention in this population. While we implemented a systematic plan for issuing follow-up reminders (e.g., reminder emails, calls, text messaging, locator contacts), it is now clear that this plan was not optimal and that additional strategies were needed. One of the primary barriers we experienced was this population was unreliable telephone service. It was likely that being unable to reach them via text or phone to serve as a reminder to complete the follow-up contributed to their attrition in the study. In fact, we documented contact issues (e.g., out of service phones, full voicemail box, incorrect contact information) with 43% (n=40) of the participants during at least one time point over the 9-month follow-up period. Among these individuals, 80% (32 of 40) could not be reached for an additional subsequent follow-up at least once. Thus, if we experienced difficulties reaching the participant via phone or email for a follow-up assessment, then it was unlikely for us to reach that participant for future follow-up assessments. Efforts to develop a multifaceted approach to retention are warranted in future research, given that higher retention is associated with more strategies used (Robinson et al., 2007). Examples of strategies include fostering study identification (e.g., branded study name), dedicated retention staff teams, implementing rigorous monitoring methods, tailoring methods to the characteristics of the individual participants (e.g., paying for bus fare), providing inexpensive tokens of appreciation (thank you/birthday/holiday cards), providing benefits to participants (e.g., educational groups for participants), and using social media to locate participants (Abshire et al., 2017; Coday et al., 2005; Smith et al., 2017).
The present study had several strengths. One strength is the target population of interest. As already noted, nonstudents emerging adult drinkers are a vulnerable group in critical need of research attention. To date, there is a surprising lack of research specifically targeting nonstudent harmful drinkers and the specific intervention needs of this group. Another strength rests in our operational definition of who is considered a “nonstudent”. The operational definition of “nonstudent” in extant literature varies greatly (see Carter, Brandon, & Goldman, 2010), ranging from those not currently enrolled (e.g., Slutske, 2005), to not enrolled full-time (e.g., Barnes et al., 1992), to those with less than 4 years of postsecondary education (e.g., Bingham et al., 2005). Our conceptualization of noncollege status is someone who never attended higher education, thus resulting in a sample that was unlikely to have received any secondary prevention efforts and likely to be most in need. Another strength is that minorities were well represented in the present study, with about 50% of the sample identifying as African American. Racial minorities in the United States experience a disproportionate burden of disease across a number of health behaviors (Centers for Disease Control and Prevention, 2013), including greater vulnerability to the negative consequences associated with substance use (see Zapolski et al., 2014 for review) and less access to substance abuse services (Lê Cook & Alegria, 2011). In an effort to achieve health equity, research efforts are needed to reach this underserved population. Further, adequate representation of minorities in intervention research is an important step towards reducing disparities in health-related risk behaviors.
The current findings should be considered within the context of several study limitations. Our follow-up retention rate decreased over the duration of the study, going from 77% at 1 month to 50% at 9 months. High attrition at follow-up assessments could introduce bias in outcome analyses but several strategies were utilized to help minimize this bias, including using expectation maximization method to handle missing data, assessing differential dropout rates in relation to condition assignment, and confirming equivalence between those who did and did not drop out. Further, a limitation of our design was that we did not include an active comparison group; thus, we are unable to rule out nonspecific factors associated with the 50-minute meeting with the interventionist for the PFI group. Future research should aim to equate actual contact time between comparison groups. Another limitation is that our follow-up window was restricted to 9-months post-intervention. A longer timeframe would address the extended impact of the intervention and allow us to explore if and when participants return to baseline drinking levels. Another limitation was that assessments were based on self-report data; however, research supports the validity of self-report measures of alcohol consumption verified by use of transdermal alcohol assessments (Simons et al., 2015) and collateral reports (Borsari & Muellerleile, 2009). Finally, sessions for participants in the PFI group were not subject to formal coding (e.g., MITI or MISC) to assess interventionist competence in MI, although PFI participants strongly endorsed that the interventionists exhibited MI-consistent skills in session.
Overall, the present research advanced knowledge regarding an understudied and at-risk group of drinkers. This randomized study was one of a few to target nonstudents by evaluating a brief intervention tailored to the needs of nonstudents based on prior formative research with this group. The highly-rated intervention successfully reduced immediate drinking reductions and this drinking continued to decline over the follow-up period. As such, PFI holds considerable promise as a helpful intervention approach for nonstudent drinkers in the community. Ultimately, this line of research aims to reduce alcohol-related health disparities associated with inequities in education.
Acknowledgments
Cathy Lau-Barraco was supported by a Career Development Award (K01-AA018383) from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
Participants were randomly assigned following study screening to either the PFI or AO condition by flipping a coin by a trained research team member. However, due to a higher no show rate for the baseline/in-person session for the PFI condition, and in an effort to increase statistical power to detect effects in the PFI condition, participants were solely randomized to the PFI condition for four months (20% of the enrollment phase for the study). The over sampling of participants for the PFI group did not result in baseline differences between conditions. See Tables 1 and 2.
References
- American Psychological Association. Ethical principles of psychologists and code of conduct. 2010 Retrieved from http://www.apa.org/ethics/code/principles.pdf.
- Abshire M, Dinglas VD, Cajita MIA, Eakin MN, Needham DM, Himmelfarb CD. Participant retention practices in longitudinal clinical research studies with high retention rates. BMC Medical Research Methodology. 2017;17:1–10. doi: 10.1186/s12874-017-0310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, Allen HK, Vincent KB, Bugbee BA, O’Grady KE. Drinking like an adult? Trajectories of alcohol use patterns before and after college graduation. Alcohol Clin Exp Res. 2016;40:583–590. doi: 10.1111/acer.12973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes GM, Welte JW, Dintcheff B. Alcohol misuse among college students and other young adults: findings from a general population study in New York State. Int J Addict. 1992;27:917–934. doi: 10.3109/10826089209065584. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Monti PM, Spirito A, Colby SM, Rohsenow DJ, Ruffolo L, Woolard R. Alcohol use and related harm among older adolescents treated in an emergency department: the importance of alcohol status and college status. J Stud Alcohol. 2003;64:342–349. doi: 10.15288/jsa.2003.64.342. [DOI] [PubMed] [Google Scholar]
- Bingham CR, Shope JT, Tang X. Drinking behavior from high school to young adulthood: differences by college education. Alcohol Clin Exp Res. 2005;29:2170–2180. doi: 10.1097/01.alc.0000191763.56873.c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Muellerleile P. Collateral reports in the college setting: A meta-analytic integration. Alcohol Clin Exp Res. 2009;33:826–838. doi: 10.1111/j.1530-0277.2009.00902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Hustand JTP, Mastroleo NR, Tevyaw TO, Barnett NP, Kahler CW, Short EE, Monti PM. Alcohol use and problems in mandated college students: A randomize clinical trial using stepped care. J Consult Clin Psychol. 2012;80:1062–1074. doi: 10.1037/a0029902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman A, Henson J. Personalized boosters for a computerized intervention targeting college drinking: the influence of protective behavioral strategies. J Am Coll Health. 2016;64:509–519. doi: 10.1080/07448481.2016.1185725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caudill BD, Crosse SB, Campbell B, Howard J, Luckey B, Blane HT. High-risk drinking among college fraternity members: a national perspective. J Am Coll Health. 2006;55:141–155. doi: 10.3200/JACH.55.3.141-155. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LRA, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998–2010. Clin Psych Review. 2012;32:690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AC, Brandon KO, Goldman MS. The college and noncollege experience: a review of the factors that influence drinking behavior in young adulthood. J Stud Alcohol Drugs. 2010;71:742–750. doi: 10.15288/jsad.2010.71.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed September 7, 2016];CDC Health Disparities and Inequalities Report – United States, 2013, Supplement. 2013 :62. Available at http://www.cdc.gov/mmwr/pdf/other/su6203.pdf.
- Coday M, Boutin-Foster C, Sher TG, Tennant J, Greaney ML, Saunders SD, Somes GW. Strategies for retaining study participants in behavioral intervention trials: Retention experiences of the NIH behavior change consortium. Annals of Behavioral Medicine. 2005;90:55–65. doi: 10.1207/s15324796abm2902s_9. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psychol. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Evans-Polce RJ, Maggs JL, Staff J, Lanza ST. The age-varying association of student status with excessive alcohol use: ages 18 to 30 years. Alcohol Clin Exp Res. 2017;41:407–413. doi: 10.1111/acer.13294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P, Jacobson KC. Longitudinal relationships between college education and patterns of heavy drinking: A comparison between Caucasians and African Americans. J Adolesc Health. 2013;53:356–362. doi: 10.1016/j.jadohealth.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê Cook B, Alegría M. Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. Psychiatr Serv. 2015;62:1273–1281. doi: 10.1176/appi.ps.62.11.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Smith DC, Briley DA. Substance use prevention and treatment outcomes for emerging adults in non-college settings: A meta-analysis. Psychol Addict Beh. 2017;31:242–254. doi: 10.1037/adb0000267. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. J Stud Alcohol. 2004;65:477–488. doi: 10.15288/jsa.2004.65.477. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug Alcohol Depend. 2005;77:139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Dimeff LA. Brief Alcohol Screening and Intervention for College Students (BASICS): A Harm Reduction Approach. Guilford Press; 1999. [Google Scholar]
- Doumas DM. Web-based personalized feedback: is this an appropriate approach for reducing drinking among high school students? J Subst Abuse Treat. 2014;50:76–80. doi: 10.1016/j.jsat.2014.09.005. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Harford TC, Yi HY, Hilton ME. Alcohol abuse and dependence in college and noncollege samples: a ten-year prospective follow-up in a national survey. J Stud Alcohol. 2006;67:803–809. doi: 10.15288/jsa.2006.67.803. [DOI] [PubMed] [Google Scholar]
- Hester RK, Squires DD, Delaney HD. The drinker’s check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. J Subst Abuse Treat. 2005;28:159–169. doi: 10.1016/j.jsat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Hingson R, Zha W, Smyth D. Magnitude and trends in heavy episodic drinking, alcohol-impaired driving, and alcohol-related mortality and overdose hospitalizations among emerging adults of college ages 18–24 in the United States, 1998–2014. J Stud Alcohol Drugs. 2017;78:540–548. doi: 10.15288/jsad.2017.78.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager J, Keyes KM, Schulenberg JE. Historical variation in young adult binge drinking trajectories and its link to historical variation in social roles and minimum legal drinking age. Dev Psychol. 2015;51:962–974. doi: 10.1037/dev0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the Brief Young Adult Alcohol Consequences Questionnaire. Alcohol Clin Exp Res. 2005;29:1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Collins LM. A mixture model of discontinuous development in heavy drinking from ages 18 to 30: the role of college enrollment. J Stud Alcohol. 2006;67:552–561. doi: 10.15288/jsa.2006.67.552. [DOI] [PubMed] [Google Scholar]
- Lau-Barraco C, Linden-Carmichael AN, Hequembourg A, Pribesh S. Motivations and consequences of alcohol use among heavy drinking nonstudent emerging adults. J Adolescent Res. 2017;32:667–695. doi: 10.1177/0743558416630812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, DeMartini KS, Gueorguieva R, Nogueira C, Corbin WR, Neighbors C, O’Malley SS. Randomized controlled trial of a very brief, multicomponent web-based alcohol intervention for undergraduates with a focus on protective behavioral strategies. J Consult and Clin Psychol. 2016;84:1008–1015. doi: 10.1037/ccp0000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Woodlard RF, Nirenberg TD, Minugh AP, Becker B, Clifford PR, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Magill M, Colby SM, Orchowski L, Murphy JG, Hoadly A, Brazil LA, Barnett NP. How does brief motivational intervention change heavy drinking and harm among underage young adult drinkers? J Consult Clin Psychol. 2017;85:447–458. doi: 10.1037/ccp0000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, Somers JM, Williams E. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. J Consult Clin Psychol. 1998;65:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- Matthews DB, Miller WR. Estimating blood alcohol concentration: two computer programs and their applications in therapy and research. Addict Behav. 1979;4:55–60. doi: 10.1016/0306-4603(79)90021-2. [DOI] [PubMed] [Google Scholar]
- Miller MB, Leffingwell T, Claborn K, Meier E, Walters S, Neighbors C. Personalized feedback interventions for college alcohol misuse: an update of Walters & Neighbors (2005) Psychol Addict Behav. 2013;27:909–920. doi: 10.1037/a0031174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. Guilford Press; New York: 2002. [Google Scholar]
- Miller WR, Toscova RT, Miller JH, Sanchez V. A theory-based motivational approach for reducing alcohol/drug problems in college. Health Educ Behav. 2000;27:744–759. doi: 10.1177/109019810002700609. [DOI] [PubMed] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102:1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. The development of heavy drinking and alcohol-related problems from ages 18 to 37 in a U.S. national sample. J Stud Alcohol. 2000;61:290–300. doi: 10.15288/jsa.2000.61.290. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. NIAAA strategic plan 2017–2021. 2017 Available at https://www.niaaa.nih.gov/sites/default/files/StrategicPlan_NIAAA_optimized_2017-2020.pdf.
- Petty RE, Barden J, Wheeler SC. The elaboration likelihood model of persuasion: health promotions for sustained behavioral change. In: DiClemente RJ, Crosby RA, Kegler M, editors. Emerging theories in Health Promotion Practice and Research. 2. Jossey-Bass; San Francisco: 2009. [Google Scholar]
- Quinn PD, Fromme D. Alcohol use and related problems among college students and their noncollege peers: The competing roles of personality and peer influence. J Stud Alcohol Drugs. 2011;72:622–632. doi: 10.15288/jsad.2011.72.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray AE, Kim SY, White HR, Larimer ME, Mun EY, Clarke N, et al. When less is more and more is less in brief motivational interventions: characteristics of intervention content and their associations with drinking outcomes. Psychol Addict Behav. 2014;28:1026–1040. doi: 10.1037/a0036593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson KA, Dennison ANP, Wayman DM, Pronovost MD, Needham DM. Systematic review identifies number of strategies important for retaining study participants. J Clin Epidemiol. 2007;60:757–765. doi: 10.1016/j.jclinepi.2006.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME. Monitoring the Future national survey results on drug use, 1975–2016: volume II, College students and adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2017. [Google Scholar]
- Simons JS, Carey KB. Personal strivings and marijuana use initiation, frequency, and problems. Addict Behav. 2003;28:1311–1322. doi: 10.1016/s0306-4603(02)00247-2. [DOI] [PubMed] [Google Scholar]
- Simons JS, Christopher MS, McLaury AE. Personal strivings, binge drinking, and alcohol-related problems. Addict Behav. 2004;29:773–779. doi: 10.1016/j.addbeh.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: self-report, transdermal assessment, and prediction of dependence symptoms. Addict Behav. 2015;50:205–212. doi: 10.1016/j.addbeh.2015.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS. Alcohol use disorders among US college students and their non-college-attending peers. Arch Gen Psychiatry. 2005;62:321–327. doi: 10.1001/archpsyc.62.3.321. [DOI] [PubMed] [Google Scholar]
- Smith LJ, McNamara PJ, King AC. Optimizing follow-up and study retention in the 21st century: Advances from the front line in alcohol and tobacco research. Drug and Alcohol Dependence. 2017;175:171–178. doi: 10.1016/j.drugalcdep.2017.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staff J, Patrick ME, Loken E, Maggs JL. Teenage alcohol use and educational attainment. J Stud Alcohol Drugs. 2008;69:848–858. doi: 10.15288/jsad.2008.69.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamates AL, Amory KA, Preonas P, Ricketts N, Lau-Barraco C. The influence of normative perceptions of close friends’ drinking on alcohol-related outcomes: is gender a moderator?. Poster presented at the annual Southeastern Psychological Association; New Orleans, LA. 2016. [Google Scholar]
- Stamates AL, Lau-Barraco C, Benton T. Concurrent substance use patterns and psychological functioning among nonstudent emerging adults. Poster presented at the biannual meeting of the Virginia Psychological Association; Virginia Beach, VA. 2015. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2013 National Survey on Drug Use and Health: National Findings (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06–4194) 2014. [Google Scholar]
- Tanner-Smith EE, Lipsey MK. Brief alcohol intervention for adolescents and young adults: A systematic review and meta-analysis. J Subst Abuse Treat. 2015;51:1–18. doi: 10.1016/j.jsat.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. Current Population Survey 2014 Annual Social and Economic Supplement. Available at http://www.census.gov/hhes/socdemo/education/data/cps/2014/tables.html.
- US Department of Education. Institute of Education Sciences, National Center for Education Statistics. Table 302.60 in Digest of Education Statistics. 2014 Available at from http://nces.ed.gov/programs/digest/d13/tables/dt13_302.60.asp.
- Walters ST, Baer JS. Talking with college students about alcohol: motivational strategies for reducing abuse. Guilford Press; 2006. [Google Scholar]
- Walters ST, Neighbors C. Feedback interventions for college alcohol misuse: what, why, and for whom? Addict Behav. 2005;30:1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. J Consult Clin Psychol. 2009a;77:64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Reactivity to alcohol assessment measures: an experimental test. Addict. 2009b;104:1305–1310. doi: 10.1111/j.1360-0443.2009.02632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, Castle IJP, Chen CM, Shirley M, Roach D, Hingson R. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcohol Clin Exp Res. 2015;39:1712–1726. doi: 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- White A, Hingson R. The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res. 2013;35:201–218. [PMC free article] [PubMed] [Google Scholar]
- White HR, Labouvie EW, Papadaratsakis V. Changes in substance use during the transition to adulthood: a comparison of college students and their noncollege age peers. J Drug Issues. 2005;35:281–206. [Google Scholar]
- Zapolski TC, Pedersen SL, McCarthy DM, Smith GT. Less drinking, yet more problems: understanding African American drinking and related problems. Psychol Bullet. 2014;140:188–223. doi: 10.1037/a0032113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zikic J, Saks AM. Job search and social cognitive theory: the role of career-relevant activities. J Vocat Behav. 2009;74:117–127. [Google Scholar]