Abstract
Background
Alcohol and other drug (AOD) treatment and recovery research typically has focused narrowly on changes in alcohol/drug use (e.g., “percent days abstinent”) with little attention on changes in functioning or well-being. Furthermore, little is known about if and when such changes may occur, and for whom, as people progress in recovery. Greater knowledge would improve understanding of recovery milestones and points of vulnerability and growth.
Method
National, probability-based, cross-sectional sample of US adults who screened positive to the question, “Did you used to have a problem with alcohol or drugs but no longer do?” (Response=63.4% from 39,809; final weighted sample n=2,002). Linear, spline, and quadratic regressions tested relationships between time in recovery and five measures of well-being: quality of life, happiness, self-esteem, recovery capital, and psychological distress, over two temporal horizons: the first 40 years, and the first 5 years, after resolving an AOD problem and tested moderators (sex, race, primary substance) of effects. LOWESS regression was used to explore turning points.
Results
In general, in the 40-year horizon there were initially steep increases in indices of well-being (and steep drops in distress), during the first 6 years, followed by shallower increases. In the 5-year horizon, significant drops in self-esteem and happiness were observed initially during the first year followed by increases. Moderator analyses examining primary substance found that compared to alcohol and cannabis, those with opioid or other drugs (e.g., stimulants) had substantially lower recovery capital in the early years; mixed race/native Americans tended to exhibit poorer well-being compared to Whites; and women consistently reported lower indices of well-being over time than men.
Conclusions
Recovery from AOD problems is associated with dynamic monotonic improvements in indices of well-being with the exception of the first year where self-esteem and happiness initially decrease, before improving. In early recovery, women, certain racial-ethnic groups, and those suffering with opioid and stimulant-related problems appear to face ongoing challenges that suggest a need for greater assistance.
Keywords: recovery, remission, alcohol use disorder, quality of life, national, epidemiology
1. Introduction
During the past 50 years we have learned a great deal about the causes, consequences, onset, clinical course, and treatment, of alcohol and other drug (AOD) problems and related disorders (Sher, 2016; McCrady and Epstein, 2013). In the treatment realm specifically, dozens of randomized clinical trials (RCTs), meta-analyses, and systematic reviews have revealed small to medium standardized effect-size differences between active treatments and inert control conditions (e.g., placebo) or less well-articulated interventions, whether they be behavioral or pharmacological in nature (Maisel et al, 2013; Prendergast et al, 2002; Wells et al, 2010). While there are exceptions that have examined additional quality of life-related outcomes (e.g., Griffin, Bennett, Fitzmaurice et al, 2015; Humphreys, Moos, Cohen, 1997; Zemore and Pagano, 2008), typically, these outcome studies have focused on the short-term (e.g., the first 12 weeks, or 6 months, following intervention) and been based almost entirely on one or two measures of substance use alone (e.g., the percentage of days on which patients are abstinent in the past 90 days; drinks per drinking day). While early stabilization and abstinence are important indicators of clinical response and are convenient and reliable to collect, such outcomes have come under scrutiny and criticism as being too narrowly focused failing to consider patients’ broader functioning and well-being (Laudet, 2011; Office of the Surgeon General, 2016; Betty Ford Institute Consensus Panel, 2007; Groshkova, Best & White, 2013; Vilsaint et al, 2017).
The degree to which individuals may be functioning better physically, socially, and psychologically, how happy they may be, and what they think of themselves (e.g., self-esteem) may all be important to assess as people progress over time in recovery from significant AOD problems (Laudet, 2011; Donovan et al, 2005). Conceptually, the initial goal of resolving an AOD problem to stave off negative consequences, including reducing one’s likelihood of death and disability, may shift toward the achievement of personal growth and contributing positively to society and one’s community (Betty Ford Institute Consensus Panel, 2007; Laudet, Becker & White, 2009). Also, given the reciprocal associations among abstinence, remission, and the availability, accessibility, and attainment of recovery resources (i.e., social support, health insurance, employment, financial resources; “recovery capital”; Cloud and Granfield, 2008; Kaskutas et al, 2014; Kelly and Hoeppner, 2014; Laudet, 2011), it may be important also to assess the degree to which individuals accrue recovery capital following AOD problem resolution. Furthermore, greater understanding of not just whether, but when and to what degree, people experience significant changes in these variables is critical. Laudet, Morgen and White (2008) for example, in a cross-sectional study found that quality of life improves and stress decreases, more steeply in the first year, changing more slowly thereafter over a 3-year period. Also, Dennis, Foss, and Scott (2007) in a prospective study of recovery pathways found general improvements with time but an exacerbation of psychological distress around three years into recovery. More knowledge about the course of recovery following AOD problem resolution, including the nature, degree, and timing of changes in different indices reflecting functioning and well-being, could help the field identify potential recovery milestones or turning points that can highlight periods of vulnerability, resilience, or growth in adaptive change; these, in turn, could inform the types of services that may be needed, for which individuals, and at what junctures, in order to support long-term recovery.
While knowledge of the nature of the relationship between time in recovery and indices of functioning and well-being is very welcome in general regardless of how long ago it has been since individuals have resolved a significant AOD problem, of particular interest is the first five years following problem resolution (DuPont, Compton, McLellan, 2015). This is particularly significant because it is a clinically important horizon, and findings from both prospective clinical studies (Dennis, Foss & Scott, 2007) and epidemiological data (Grant et al, 2015; Dawson et al, 2015), indicate 4–5 years is the time frame after which the risk of meeting criteria for AOD disorder in the following year drops below 15% - the approximate annual risk in the general population (White, 2012). Understanding what happens to indices of well-being and recovery capital during this critical change period and whether the magnitude and rate of change differs at different time points for different subgroups of individuals (e.g., men and women; different racial/ethnic groups; those with different primary substances) would help the field identify potential recovery milestones or turning points that can highlight periods of vulnerability or progress in adaptive change among such subgroups.
To this end, using a nationally representative sample of US adults who have successfully resolved a significant AOD problem (Kelly et al, 2017), this study describes and tests for significant changes in the relationship between time since problem resolution and a number of functioning and well-being indices (e.g., quality of life, happiness, self-esteem, psychological distress) and other recovery outcomes (recovery capital) with a focus on the long-term (i.e., during the first 40 years of problem resolution) and more specifically, in the first 5 years following AOD problem resolution. In addition, interactions between time since problem resolution and these indices of well-being is explored in relation to sex, race-ethnicity, and primary substance, in order to determine whether any observed progress during the first five years, differs in magnitude or rate across these different subgroups.
2. Materials and Method
Procedure
As detailed in the National Recovery Survey (NRS) target population was the US noninstitutionalized civilian population 18 years or older that had resolved an AOD problem, indicated by affirmative response to the screener question: “Did you used to have a problem with drugs or alcohol, but no longer do?” (Kelly et al, 2017), Data were collected by the survey company GfK, using a probability sampling approach to select respondents at random. GfK screened everyone in their “KnowledgePanel” (GfK, 2013), which consists of approximately 55,000 adult individuals (18 and older). The KnowledgePanel uses address-based sampling (ABS) to randomly select individuals from 97% of all U.S. households based on the U.S. Postal Service’s Delivery Sequence File. If necessary, GfK provides individuals with a web-enabled computer and free Internet service. Using this ABS approach, Gfk is able to include households that a) have unlisted telephone numbers, b) do not have landline telephones, c) are cell phone only, d) do not have current internet access, and e) do not have devices to access the internet. This type of broad scale sampling helps redress socioeconomic differences in landline telephone use and internet access. For the current study, a representative subset of 39,809 individuals from the Gfk KnowledgePanel received the screening question. In order to draw this subsample, Gfk uses a probability proportional to size (PPS) sampling approach, a patented strategy (U.S. Patent No. 7,269,570) unique to Gfk. PPS assures that subsamples from a finite panel membership remains a reliable approximation of the entire U.S. Population. See http://www.knowledgenetworks.com/knpanel/docs/knowledgepanel(R)-design-summary-description.pdf for more information on GfK’s probability-based sampling methodology.
The survey was first piloted on 20 individuals over 3 days in July 2016 then formally administered over 19 days in July-August 2016. Median time to completion was 24 minutes (IQR = 18–36 minutes). Of those in the initial sampling frame (N=39,809), 25,229 individuals responded to the screening question (63.4%). This response rate is comparable to most other current nationally representative surveys, including the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III; 60.1%; Grant et al., 2015) the 2015 National Survey on Drug Use and Health (NSDUH; 58.3%; Center for Behavioral Health Statistics and Quality, 2016) and the 2013–2014 National Health and Nutrition Examination Survey (NHANES; 68.5%; CDC NCHS, 2013). Data were weighted to accurately represent the civilian population using the method of “iterative proportional fitting” (Battaglia et al., 2009).
In order to produce unbiased estimates of population parameters from these respondents, GfK first computed base weights then made post-stratification adjustments according to benchmarks from the Current Population Survey (CPS), conducted March 2015 by the U.S. Bureau of the Census, along eight dimensions: 1) gender; 2) age; 3) race/Hispanic ethnicity; 4) education; 5) geographical region; 6) household income; 7) home ownership status; and 8) metropolitan area. A thorough systematic investigation of response patterns (Thomas, 2014) was conducted to examine sub-optimal or fraudulent responding (e.g., responding “yes” to the screening question in order to receive the monetary compensation) as well as likely misunderstandings/misreading of questions. Detailed independent review by two team members led to removal of 45 cases. Of these 45, seven were eliminated because they were determined to have misunderstood or misread the screening question (three did not have an AOD problem, two had a problem with tobacco only, one was prescribed steroids by a doctor for a health problem, and one had a persisting rather than resolved AOD problem). Among the remaining 38 eliminated cases, 73.7% (n = 28) denied all substances they used 10 or more times were a problem, 76.3% (n = 29) reported “0” for serious problem resolution attempts or skipped the item, 71.1% (n = 27) reported “0” for time since problem resolution or skipped the item, 60.5% (n = 23) had nonsensical or blank qualitative responses, and 36.8% (n = 14) had a survey time of 9 minutes or less. This resulted in a final sample of 2,002 individuals. Because excluded cases constituted only 2.2% of the original sample, derived weights remained valid (Thomas, 2014). Non-Hispanic Black individuals were significantly more likely to be excluded than Whites and males were significantly more likely to be excluded than females (p < .05). GfK’s population-based probability sampling approach has been vetted and validated in dozens of published studies in the medical and behavioral health fields (https://www.gfk.com/fileadmin/user_upload/dyna_content/US/documents/GfK_Bibliography.pdf). KnowledgePanel-derived estimates are comparable to those derived from national surveys that used non-internet methodologies to recruit and collect data (Bethell et al., 2004; Chang and Krosnick, 2009; Heeren et al., 2008; Novak et al., 2007; Yeager et al., 2011). Heeren et al. (2008) for example, showed that estimates of current drinking obtained through a GfK KnowledgePanel-derived sample were similar to those obtained by NESARC.
IRB Statement
All study procedures were approved by the Partners HealthCare Institutional Review Board.
Measures
Demographic characteristics
Demographic data were derived both from GfK’s existing KnowledgePanel data (collected prior to the survey) as well as from survey data. Regarding previously collected demographic data, participants reported the following: a) age; b) level of education (less than high school; high school; some college; bachelor’s degree or higher), race/ethnicity (White/Non-Hispanic, Black/Non-Hispanic, Other/Non-Hispanic, 2+ Races/Non-Hispanic, Hispanic), gender (Male, Female), household income (nineteen categories ranging from less than $5,000 to $175,000 or more) and current employment.
Substance use and problem resolution history
From a list of 15 substances that participants had used 10+ times in their life (Dennis, Titus, White, Unsicker, & Hodgkins, 2002), participants reported their primary substance (“drug of choice”). We then categorized these into one of four primary substance groups: alcohol, cannabis, opioid, or other drug. They also reported time in years and months since they resolved their problem, which we converted into one continuous variable.
Quality of life
The EUROHIS-QOL (Schmidt et al., 2006) is a widely used eight-item measure of quality of life, adapted from the World Health Organization Quality of Life – Brief Version (WHOQOL-BREF). Item responses are Likert-scaled: 1 to 5 (e.g., “How satisfied are you with your personal relationships?; 1 = very dissatisfied to 5 = very satisfied). The measure has strong psychometrics, including good-excellent predictive and convergent validity with other measures of health and wellness (rs = .4–.6), and internal consistency (α = .83); current sample α = .90.
Happiness and self-esteem
Participants rated their happiness on a scale from 1 = completely unhappy to 5 = completely happy (Meyers and Smith, 1995). They also rated extent to which “I have high self-esteem” was true on a scale from 1 = not very true to 5 = very true (Robins et al., 2001).
Recovery capital
The 10-item Brief Assessment of Recovery Capital (Vilsaint et al., 2017) is an abridged version of the Addiction Recovery Capital Scale (Groshkova et al., 2013). Participants reported level of agreement (1 = strongly disagree to 6 = strongly agree) with statements on their recovery, environmental support, and well-being (e.g., “I regard my life as challenging and fulfilling without the need for using drugs or alcohol”). This measure has demonstrated excellent concurrent validity with the longer recovery capital measure (r = .92) as well as excellent internal consistency (α = .95); current sample α = .93.
Psychological Distress
The Kessler-6 (Kessler et al., 2003) is a 6-item measure of psychological distress that asks participants to rate from 0 = none of the time to 4 = all of the time, they felt each of 6 symptoms occurred (e.g., nervousness and depression) during the past 30 days (sample α = .93).
Participants
On average, participants (N = 2002) used 3.4 different substances 10 or more times (SD = 2.6; min = 1; max = 15), identified 1.5 substances as problems (SD = 1.4; min = 0; max = 15; mode = 1), and were 17.7 years old (SD = 6.0) when they first began using one or more substances regularly (i.e., weekly). Slightly less than half (48.6%) reported current use of at least one substance (i.e., they were not abstinent from AODs).
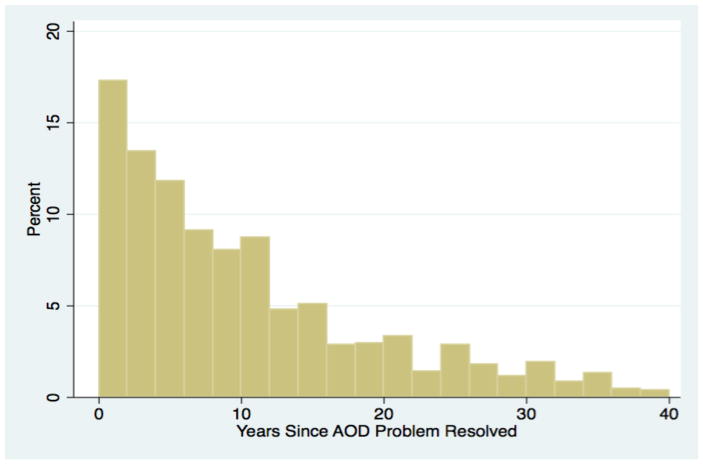
Regarding AOD problem resolution and recovery history, participants resolved their AOD problem an average of 11.9 years ago (SD = 10.6) including 6.5% with less than 1 year, 28.7% with 1–5 years (i.e., through 5 years 11 months), 21.9% with 6–10 years, 13.8% with 11–15 years, 9.5% with 16–20 years, and 19.6% with 21 or more years. Among just those who reported a non-zero number, average time since problem resolution was 12.2 years (SD = 10.6; Figure 1). Almost half (45.2%) identified as being “in recovery” currently (see Kelly et al, 2017 for more details).
Figure 1.
Distribution of time since resolving a significant alcohol or drug problem in a National Probability Based Sample of the US Population
Analytic Plan
Prior to beginning analyses we subset the full sample (n=2002) into two groups: 1) participants that reported resolving their alcohol or drug problem within the last 40 years (n=1879), and 2) participants that reported resolving their alcohol or drug problem within the last 5 years (n=488). The full sample represented 1980 persons once survey sampling weights were applied. The 40- and 5-year subsamples represented 1876 and 637 persons, respectively. We then described these two groups in terms of age, gender, race/ethnicity, household income primary substance, employment, education, years since problem resolution, and mean scores of the primary outcomes (i.e., quality of life, psychological distress, happiness, self-esteem, recovery capital) using survey-weighted estimation methods (see Kelly et al, 2017 for more details).
To evaluate quality of life, psychological distress, happiness, self-esteem, and recovery capital, we graphed the relationship between self-reported time since problem resolution (in years) and each of primary outcome, which were z-standardized to improve comparability by placing all on the same scale. All graphs applied a LOWESS (Locally-Weighted Scatterplot Smoothing) function with a smoothing bandwidth of 0.8. For the 40-year and 5-year samples respectively, we modeled the five primary outcomes (unstandardized) using linear regression as a function of years since problem resolution and controlling for age. Years since problem resolution was modeled flexibly as a linear, spline, or quadratic term. The final models were selected based on fit to the data, as observed through graphical representations of the different parameterizations, as well as using R-squared estimates as an empirical indicator of goodness of fit, given that applying survey weights precludes calculation of model fit statistics relying on the traditional likelihood function (Skinner et al., 1989). Models incorporating spline terms allow the slope of the time since problem resolution parameter to change at a specified value. Thus, these coefficients are interpreted as the change in slope as compared to prior time periods, with the first time interval serving as the reference category. Once final models were selected for each outcome, we investigated the role of sex, race/ethnicity, and primary substance as moderators during the first five years since AOD resolution by including interactions between factors and years since resolution. All models incorporated sampling weights and were conducted in Stata Version 14 (StataCorp, 2015).
3. Results
Recovery indices during the first 40 years after problem resolution
In our survey-weighted sample, there were 1,876 participants that reported resolving an AOD problem within the last 40 years. These participants were 46.7 years of age on average (SD=15.0). The majority were male (59.7%), non-Hispanic White (61.0%), reported a household income less than $50,000USD (51.8%), employed (54.5%), and had received a college education (52.2%). The majority reported alcohol as their primary AOD problem (58.6%) followed by drugs other than opioids and cannabis (23.0%), cannabis (12.8%) and opioids (5.7%). On average, these participants reported resolving their AOD problem 11.4 years prior to their participation in the survey (SD=9.8; Table 1). As shown in figure 1, however, the distribution of time since problem resolution was positively skewed.
Table 1.
Characteristics of the 40- and 5-year samples
| Variable | 40-year
sample (n=1879) |
5-year sample (n=488) |
|---|---|---|
| Age, M(SD) | 46.65(14.99) | 37.79(13.90) |
| Male Gender, % | 59.67 | 57.10 |
| Race Ethnicity, % | ||
| White, Non-Hispanic | 61.00 | 57.49 |
| Black, Non-Hispanic | 13.66 | 12.08 |
| Hispanic | 17.79 | 22.95 |
| Other, Non-Hispanic | 7.54 | 7.48 |
| Household Income less than 50,000 USD, % | 51.75 | 50.80 |
| Primary Substance, % | ||
| Alcohol | 58.55 | 61.30 |
| Cannabis | 12.80 | 15.20 |
| Opioids | 5.67 | 9.90 |
| Other Drug | 22.98 | 13.60 |
| Employed, % | 54.52 | 57.80 |
| College Education, % | 52.22 | 53.13 |
| Years Since AOD Problem Resolved, M(SD) | 11.42(9.81) | 2.17(1.61) |
| Quality of Life, M(SD) | 3.65(0.83) | 3.42(0.89) |
| Psychological Distress, M(SD) | 4.86(5.42) | 6.87(5.84) |
| Happiness, M(SD) | 3.76(.94) | 3.5(.98) |
| Self-Esteem, M(SD) | 3.5(1.15) | 3.23(1.19) |
| Recovery Capital, M(SD) | 46.81(9.77) | 43.67(10.48) |
Note: sample size estimates in the header are unweighted; proportions, means and standard deviations reported in the table incorporate sampling weights
Overall, participant reports of primary outcomes revealed moderate to high levels of quality of life (M=3.7, SD=0.8, Range=1–5), happiness (M=3.8, SD=0.9, Range=1–5), self-esteem (M=3.5, SD=1.2, Range=1–5), and recovery capital (M=46.8, SD=9.8, Range=10–60). Also, average psychological distress was quite low (M=4.9, SD=5.4, Range=0–24). Quality of life, happiness, self-esteem and recovery capital all suggest rapid increases in these constructs during the earlier years after problem resolution followed by a continued, albeit attenuated increase (Table 2). Quality of life, happiness and self-esteem displayed highest rates of improvement during the first 6–11 years after problem resolution followed by an attenuation in the slope for the remaining period, as indicated by the negative coefficient for the spline term describing the second time interval (Table 2). Of note, given that some norms (were available for our quality of life measure based on general population samples from the US (Da Rocha et al, 2012) and similar developed countries (i.e., UK, Germany, France; Schmidt, Muhlen, Power, 2006;) we were able to estimate at what point similar levels of QOL may be achieved among recovering individuals in our sample; results suggested it takes approximately 15 yrs of recovery, on average, to reach the same QOL as the general population in a healthy Western European sample (M=4.02). In a US sample based on depressed patients in primary care, after 1 year of problem resolution, our sample was significantly higher (M=3.40) than the primary care depressed sample (M=2.66). Overall, QOL mean scores in our sample also was higher with increasing recovery milestones: 5 years = 3.63; 10 yrs.= 3.87; 15 yrs. 4.02; 20 yrs.=4.25; 30 yrs.=4.73; 40 yrs.=5.20.
Table 2.
Relationship between recovery indices and years since problem resolution in the 40-year sample
| Model | β | SE | t | p |
|---|---|---|---|---|
| DV: Quality of life | ||||
| Age (in years) | 0.05 | 0.02 | 2.92 | 0.004 |
| Time since problem resolution (spline terms) | ||||
| Years (0–8) | 0.46 | 0.11 | 4.07 | 0.000 |
| Years (8–15) | −0.23 | 0.11 | −2.07 | 0.039 |
| Years (15–37) | 0.14 | 0.04 | 3.61 | 0.000 |
| Intercept | 24.50 | 0.99 | 24.78 | 0.000 |
| DV: Happiness | ||||
| Age (in years) | 0.01 | 0.00 | 3.39 | 0.001 |
| Time since problem resolution (spline terms) | ||||
| Years (0–11) | 0.04 | 0.01 | 3.57 | 0.000 |
| Years (11–18) | −0.03 | 0.01 | −1.90 | 0.058 |
| Years (18+) | 0.02 | 0.01 | 3.10 | 0.002 |
| Intercept | 3.13 | 0.13 | 24.58 | 0.000 |
| DV: Self esteem | ||||
| Age (in years) | 0.01 | 0.00 | 4.93 | 0.000 |
| Time since problem resolution (spline terms) | ||||
| Years (0–6) | 0.08 | 0.03 | 2.91 | 0.004 |
| Years (6–15) | −0.03 | 0.02 | −2.17 | 0.030 |
| Years (15–32) | 0.04 | 0.01 | 4.22 | 0.000 |
| Years (32+) | −0.04 | 0.02 | −2.01 | 0.044 |
| Intercept | 2.51 | 0.17 | 14.86 | 0.000 |
| DV: Recovery capital | ||||
| Age (in years) | 0.08 | 0.02 | 3.17 | 0.002 |
| Time since problem resolution | ||||
| Years (linear) | 0.39 | 0.11 | 3.63 | 0.000 |
| Years (Quadratic) | −0.01 | 0.00 | −2.45 | 0.014 |
| Intercept | 40.29 | 1.34 | 30.08 | 0.000 |
| DV: Psychological distress | ||||
| Age (in years) | −0.09 | 0.01 | −7.27 | 0.000 |
| Time since problem resolution | ||||
| Years (linear) | −0.21 | 0.05 | −3.80 | 0.000 |
| Years (Quadratic) | 0.00 | 0.00 | 2.90 | 0.004 |
| Intercept | 10.62 | 0.68 | 15.71 | 0.000 |
Note: DV: dependent variable
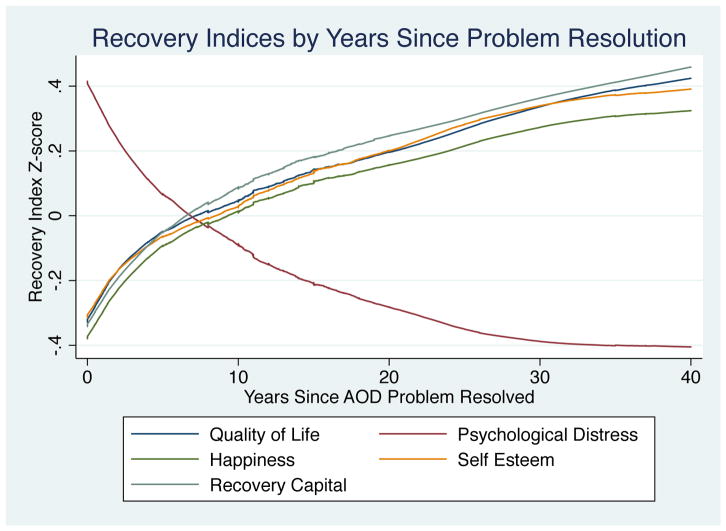
The relationship between recovery capital and time since problem resolution was best characterized by a quadratic term, which similarly suggests rapid accrual of recovery capital during the early years after problem resolution followed by a continued, but attenuated accrual. The pattern for psychological distress mirrored the aforementioned patterns such that psychological distress was associated with a more rapid decline during the early period after problem resolution, which similarly was best explained by a quadratic term. These patterns can also be seen in the graphs of the standardized outcomes as a function of years since problem resolution (Figure 2). In these graphs, it appears that the most extreme values indicating poor outcomes are observed immediately after problem resolution and outcomes continue to improve over time. The mean difference in these recovery indices between less than one year and 40 years after problem resolution resulted in large effect size difference of approximately 0.8 standard deviation units (Figure 2).
Figure 2.
Locally Weighted Scatterplot and Smoothing (LOWESS) analysis representing recovery indices (standardized) during the first forty years after problem resolution
Recovery indices during first 5 years after problem resolution
Participants in our 5-year sub-sample represent 637 persons who have resolved an AOD problem within the past 5 years. These participants were 37.8 years of age on average (SD=13.9). The majority were male (57.1%), non-Hispanic White (57.5%), reported a household income less than $50,000USD (50.8%), were employed (57.8%), and had received a college education (53.1%). The majority had resolved a problem with alcohol (61.3%) followed by cannabis (15.2%), drugs other than opioids and cannabis (13.6%) and opioids (9.9%). On average, these participants reported resolving their problem with alcohol and other drugs 2.2 years prior to their participation in the survey (SD=1.6; Table 1).
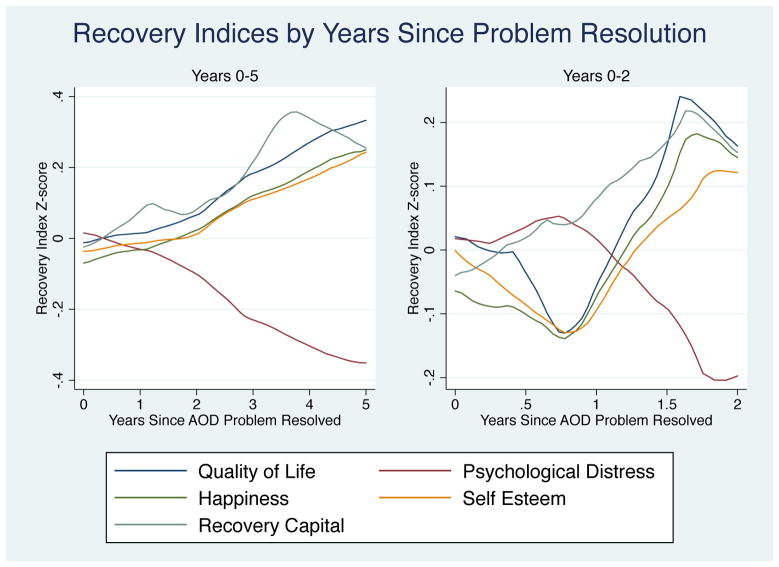
Participant reports on primary outcomes revealed moderate to high levels of quality of life (M=3.4, SD=0.9, Range=1–5), happiness (M=3.5, SD=1.0, Range=1–5), self-esteem (M=3.2, SD=1.2, Range=1–5), and recovery capital (M=43.7, SD=10.5, Range=10–60); average psychological distress was quite low (M=6.9, SD=5.8, Range=0–24). In general, these recovery indices indicated slightly less gain in these indices of well-being for the 5-year sample relative to the 40-year sample, which is consistent with observations suggesting gradual improvements in these outcomes over the course of 40 years post-problem resolution. Nevertheless, the outcomes for quality of life and recovery capital suggest linear increases in these indices over the first five years after problem resolution (Table 3) with psychological distress declining linearly during these initial five years. Happiness and self-esteem, on the other hand displayed a delay in their improvements during this initial period. Initially after problem resolution, happiness was lower in the early months into recovery then remained stationary followed by higher happiness after 4.8 months (p=0.062). Self-esteem appears to decrease during the first 4.8 months (sample size contributing to this estimate n = 121) followed by a stabilization and gradual increase after about 12 months, for the remainder of the 5-year period. Graphs displaying the standardized recovery indices as a function of years since problem resolution also suggest improvements directed towards extreme values of their 5-year distributions over time. For each of these recovery indices the mean difference between less than one year and 5 years after problem resolution is approximately 0.3–0.4 standard deviation units (Figure 3).
Table 3.
Relationship between recovery indices and years since problem resolution in the 5-year sample
| Main Effects Models
|
Interaction Tests (β)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | t | p | Male (v. Female) | Black (v. White) | Hispanic (v. White) | Other Race (v. White) | Alcohol (v. Cannabis) | Opioid (v. Cannabis) | Other Drug (v. Cannabis) | ||
| Model 1: Quality of life | ||||||||||||
| Age (in years) | 0.06 | 0.03 | 2.15 | 0.032 | ||||||||
| Time since problem resolution | Main Effect (Moderator) | 2.18* | 0.40 | −0.02 | −4.87 | −0.45 | −0.10 | −2.84 | ||||
| Years (Linear) | 0.60 | 0.29 | 2.11 | 0.036 | Interaction Terms | 0.76 | 0.29 | −0.13 | −3.02* | 2.45* | 1.74 | 1.25 |
| Intercept | 23.75 | 1.45 | 16.33 | <.001 | ||||||||
| Model 2: Happiness | ||||||||||||
| Age (in years) | 0.01 | 0.00 | 1.55 | 0.122 | ||||||||
| Time since problem resolution | Main Effect (Moderator) | 0.05 | 0.33 | 0.12 | −0.66* | −0.17 | −0.22 | −0.43 | ||||
| Years (0–0.4) | −0.36 | 0.54 | −0.67 | 0.501 | Interaction Terms | −0.16 | −3.07* | 0.12 | −0.73 | 0.33 | 4.60 | 2.26 |
| Years (0.4–5) | 0.09 | 0.05 | 1.87 | 0.062 | −0.04 | 0.22* | −0.10 | −0.07 | −0.01 | −0.13 | −0.29 | |
| Intercept | 3.23 | 0.24 | 13.41 | <.001 | ||||||||
| Model 3: Self esteem | ||||||||||||
| Age (in years) | 0.01 | 0.00 | 2.31 | 0.022 | ||||||||
| Time since problem resolution | Main Effect (Moderator) | 0.29* | 0.64* | 0.20 | −0.17 | 0.04 | −0.48 | −0.24 | ||||
| Years (0–0.4) | −2.29 | 0.77 | −2.97 | 0.003 | Interaction Terms | 1.21 | 0.52 | −0.10 | −2.51 | 1.44 | −0.61 | 2.00 |
| Years (0.4–1.2) | 0.76 | 0.38 | 2.00 | 0.046 | −0.24 | −0.53 | −0.17 | 0.16 | −1.58 | −1.99 | −1.58 | |
| Years (1.2–5) | 0.07 | 0.08 | 0.91 | 0.365 | 0.10 | 0.26 | −0.01 | −0.01 | 0.44 | 0.12 | 0.20 | |
| Intercept | 3.11 | 0.27 | 11.65 | <.001 | ||||||||
| Model 4: Recovery capital | ||||||||||||
| Age (in years) | 0.12 | 0.04 | 2.99 | 0.003 | ||||||||
| Time since problem resolution | Main Effect (Moderator) | 0.77 | 3.48 | −0.68 | −6.25* | −3.53 | −5.04 | −5.83* | ||||
| Years (linear) | 0.77 | 0.41 | 1.89 | 0.059 | Interaction Terms | 0.41 | −0.33 | −0.19 | −1.79 | 1.89 | 3.68* | 2.32 |
| Intercept | 37.40 | 2.20 | 17.03 | <.001 | ||||||||
| Model 5. Psychological distress | ||||||||||||
| Age (in years) | −0.10 | 0.02 | −4.59 | <.001 | ||||||||
| Time since problem resolution | Main Effect (Moderator) | −1.24 | −0.84 | 0.02 | 3.67* | 0.75 | 1.37 | 2.97 | ||||
| Years (linear) | −0.40 | 0.23 | −1.69 | 0.091 | Interaction Terms | −0.10 | −0.19 | 0.61 | 1.31 | −1.30 | −1.77 | −0.30 |
| Intercept | 11.58 | 1.09 | 10.64 | <.001 | ||||||||
Notes:
denotes statistical significance (p<0.05) of interaction or main effect term
Figure 3.
Locally Weighted Scatterplot and Smoothing (LOWESS) analysis of recovery indices (standardized) during the first five years (left) and two years (right) after problem resolution
Moderators of the relationship between time since problem resolution and recovery indices
Evaluation of gender, race/ethnicity and primary substance as moderators of the relationship between time since problem resolution and the five recovery indices revealed some notable differences by subgroup. Gender did not display an interaction with time for any of the primary outcomes; however, there was a consistent main effect of gender for quality of life and self-esteem such that males had higher average quality of life and self-esteem scores relative to females. A similar pattern whereby males had lower psychological distress, on average, was also observed; however this main effect was marginally statistically significant (p=0.068).
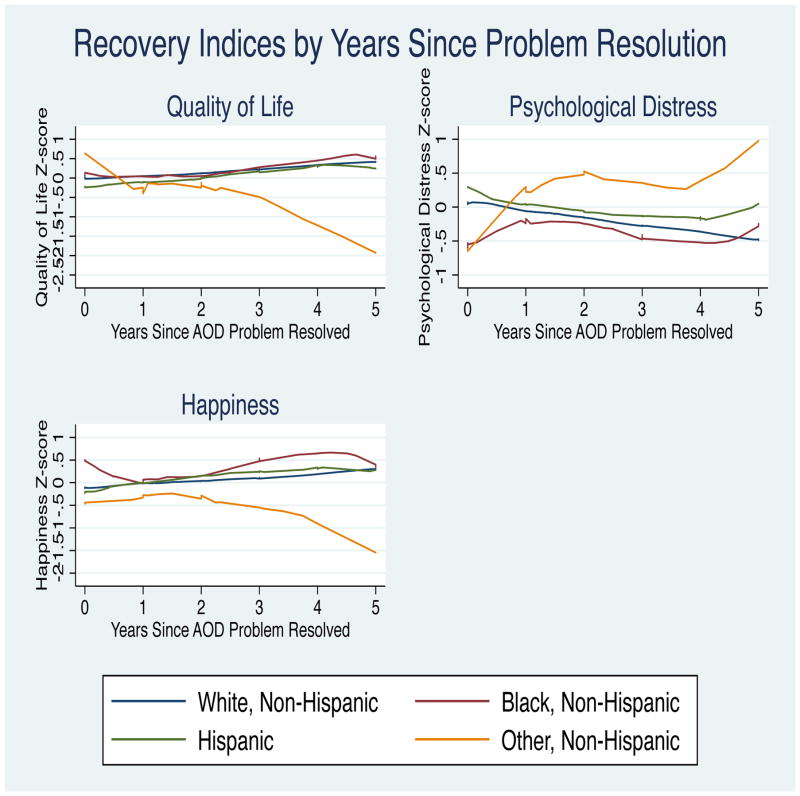
With regards to race/ethnicity, Whites had significantly greater happiness, recovery capital and lower psychological distress relative to participants reporting a race/ethnicity other than White, Hispanic, or Black. The other race group (not Hispanic, White, or Black) also displayed marginally poorer quality of life relative to Whites (p=0.057). In contrast, Blacks had significantly greater self-esteem and marginally greater happiness (p=0.064) relative to Whites. There were no significant differences observed in recovery indices between Hispanics and Whites. Race/ethnicity was also found to moderate psychological distress, quality of life and happiness. Specifically, quality of life appears to decline and psychological distress to increase at a faster rate over years since problem resolution among other race (non-Hispanic, non-Black) participants relative to Whites (Figure 4). Moreover, happiness appears to decrease at a significantly greater rate during the first 4.8 months among Blacks relative to Whites, but this was followed by a significantly greater increase in happiness after this period in Blacks relative to Whites.
Figure 4.
Locally Weighted Scatterplot and Smoothing (LOWESS) analysis of recovery indices by years since problem resolution stratified by race/ethnicity during the first 5 years
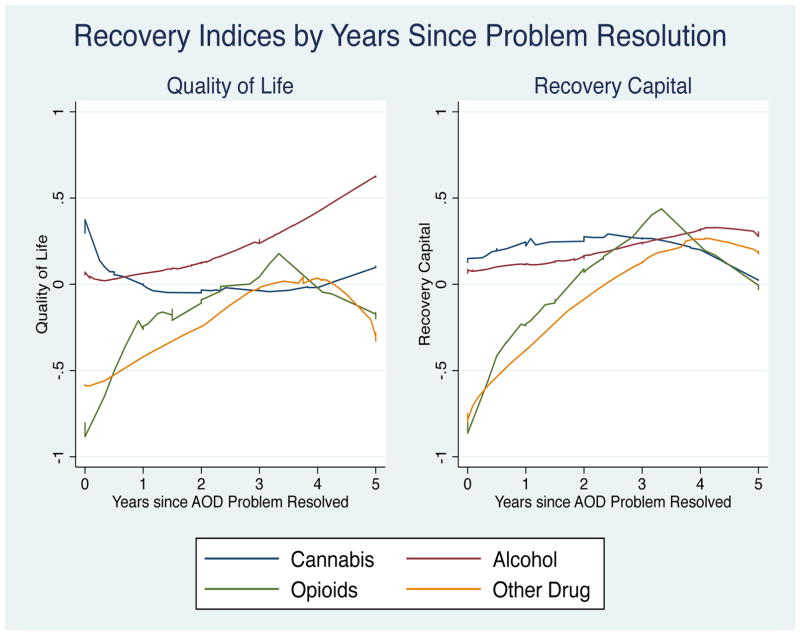
With regards to differences by primary substance, the other illicit drug group (i.e., not alcohol, opioid, or cannabis as primary substance) had lower recovery capital on average relative to the cannabis group during the first five years post-problem resolution (p=0.05). Moderation by primary substance over time was observed for quality of life, and recovery capital. The alcohol group appears to have a significantly greater increase in quality of life over years since problem resolution relative to the cannabis group. Additionally, the opioid and other drug group had significantly lower recovery capital compared to the cannabis and alcohol groups immediately following problem resolution; however, both groups achieved comparable recovery capital levels around 3 years. The opioid group’s recovery capital appears to accrue at a significantly greater rate over years since problem resolution relative to the cannabis group (Figure 5).
Figure 5.
Locally Weighted Scatterplot and Smoothing (LOWESS) analysis of recovery indices by years since problem resolution stratified by primary substance
4. Discussion
The vast majority of research studies on addictive behavior change has examined substance use-specific outcomes only; typically, the proportion of days a person may be abstinent following a cessation attempt or intervention, and has focused mostly on short-term impacts during the first three to six months thereafter. Results from this study augment these findings by offering new insights regarding the extent and nature of potential changes in indices of functioning and psychological well-being beyond abstinence during this early period, but also over the longer-term following successful AOD problem resolution in a nationally-representative sample of US adults.
It should be remembered that these are cross-sectional data and therefore caution should be taken when extrpolating these findings to signify longitudinal trends in the same people across time. The results in this study are suggestive only of such longitudinal trends. Prospective studies are needed to confirm these initial findings. With that in mind, in general, the pattern of results suggests that individuals resolving significant AOD problems show more substantial and rapid attainment of recovery capital and improvements in indices of quality of life and well-being during the early years of recovery, followed by more gradual, ableit still increasing, gains in the years thereafter up through 40 years. These findings are similar to those of Kaskutas et al’s (2014) recovery study which examined recovery definitions among those self-identifying as “in recovery” and found that those with longer duration of recovery were more likely to endorse recovery as being grateful, giving back, and having an increased sense of belonging.
A closer examination of the first few years following problem resolution, however, reveal things may get worse before they get better – notably, happiness and self-esteem appear to drop during the first few months followed by a gradual increase beginning 6 to 12 months into recovery. Noteworthy, too, during the first five years of recovery was that the same patterns of improvements were not observed for all individuals, with men showing consistently higher quality of life and lower psychological distress compared to women; mixed racial or racial groups other than Black, White, or Hispanic, showing persistent challenges following AOD problem resolution; and, compared to those with alcohol and cannabis problems, those with opioid or other drug use problems (e.g., stimulants) begin their recovery journey at a substantial disadvantage in terms of recovery capital.
If one imagines a serious substance use problem as like a burning building, most would agree that, as a field, clinical success has been achieved in terms of initially extinguishing the fire—at helping stop substance use. Far less success has been achieved, however, in preventing the fire from restarting—from preventing relapse. This may be due, in part, to the fact that compared to detoxification and stabilization, a relatively poor job has been done at providing the architectural planning for reconstructing that person’s life once the fire is out, and providing access to the building materials (recovery capital) necessary to reconstruct their lives. From a legal and policy standpoint also, a poor job has been done at granting the “rebuilding permits” needed to allow the recovery process to begin. If someone has a criminal record, for example—often directly related to their substance use—they often cannot get a job, housing, or a loan for college or job training (Kelly, 2017). The more rapid attainment of recovery capital observed during the early years of recovery suggest a more immediate need for people to gain access to the “building materials” needed to reconstruct their lives early in the recovery phase. Good news suggested from these findings is that among those who continue to stay in recovery, these useful resources appear to increase monotonically over time up through 40 years of recovery. Given the cross-sectional and correlational nature of our data, however, it remains to be tested, in future studies, whether actually providing people who have an active, or recently resolved, AOD problem, more recovery-supportive resources and rebuilding materials (recovery capital) and quickly granting “rebuilding permits” can increase AOD problem resolution prevalence.
An intriguing finding was that during the first few years of recovery, things may get worse before they get better – notably, happiness and self-esteem appears to drop during the first few months followed by a gradual increase beginning 6 to 12 months into recovery. It may be that as individuals’ brains clear from the residual effects of substance use, the increased ability to more accurately appraise an objectively impoverished and diminished life situation may be difficult emotionally for people to cope with. Also, the increased opportunity and ability to reflect psychologically on the past and the future may be responsible, at least in part, for the observed decrease in happiness as well as lowered self-esteem. These observations fit well with the phenomonelogy and clinical observations of individuals in early recovery who often experience intense remorse, regret, guilt, and a sense of hopelessness that things will not improve going forward. This can often result in a return to substance use during this early phase (Hunt et al, 1971; Witkiewitz et al, 2008). Even for treatments with the best available evidence of short-term efficacy, there is substantial room for improvement [Project MATCH Research Group, 1999; Lee et al, 2017; Prendergast et al, 2002). The message suggested by these data is that if people can find a way to navigate through this difficult early phase in the first year of recovery the picture looks brigher in terms of gains in happiness and self-esteem. It also behooves those clinically involved in recovery management to help those early in recovery to shift their inter-temporal horizon toward the 6 and 12-month milestones as times of potentially significant positive cognitive and affective change.
During the first five years of recovery we observed that the same patterns of improvements were not evident for all individuals, with men, for instance, showing consistently higher quality of life and self-esteem and lower psychological distress compared to women. This is consistent with other recent findings (Giffin, Bennett, Fitzmaurice et al, 2015) and suggests a potentially more persistent challenge facing women in recovery than men, as they appear to struggle more with psychological stress and are less satisfied with physical, psychological, and social aspects of their life in recovery. Some of these may reflect ongoing different biological (e.g., increased cortisol; Fox et al, 2009) and psychosocial challenges (e.g., negative affect; Kelly and Hoeppner, 2013), or socio-cultural challenges (e.g., gender bias/discrimination) compared to men. Similarly, individuals reporting mixed race or a racial group other than Black, White, or Hispanic (e.g., Native American) showed persistent challenges following AOD problem resolution in these indices of quality of life and psychological well-being. This group includes native/indigenous Americans and other mixed ethnicities who appear to be assiduously disadvantaged and show worsening, rather than improvements, in quality of life and psychological distress over time. More needs to be learned about the scope and nature of the recovery needs of this subgroup, in particular, to help them achieve the same benefits of recovery as those in other racial-ethnic groups.
Finally, those with opioid or other drug use problems (e.g., stimulants) appear to begin their recovery journey at a substantial disadvantage in terms recovery capital relative to those resolving alcohol or cannabis problems, taking several years to achieve similar rates to other primary drug use groups. Individuals with these primary substance-related problems, in particular, may be among the most marginalized and stigmatized (i.e., those with heroin, methamphetamine, or crack cocaine as their primary substance). As such, they appear to be at a distinct disadvantage early in the recovery process in terms of access to recovery resources. Attention may need to be paid to these individuals’ needs, in particular. Those with opioid or stimulant use disorders may require more resources and more immediate granting of “rebuilding permits” compared to other primary drug groups as they may be more likely to have drug-related criminal records (Bureau of Justice Statistics, 2006) that can prevent access to jobs, loans, education and training opportunities, and housing.
Limitations
The study’s findings should be considered in light of important limitations. It should be kept in mind that the term “resolution of an AOD problem” we use in this paper may certainly overlap with but not necessarily signify diagnostic remission. The findings here apply to people in the US general population who acknowledge and report that they themselves believe they once had a problem with alcohol/drugs but no longer do. We believe this group of individuals to be important because, while national concerns are typically focused around the prevalence and impact of clinically-defined disorders, from a broad public health and safety perspective it is important also to recognize that many people who misuse substances actually do not meet diagnostic criteria for an AOD disorder (e.g., based on the diagnostic and statistical manual of mental disorders; [DSM]) but can still suffer from significant problems. For example, more than 66 million Americans report past-month hazardous/harmful alcohol consumption (i.e., consuming 5+ standard drinks within two hours), increasing risk of motor vehicle crashes, accidents, and alcohol-poisonings. While only a minority of these individuals meet the diagnostic threshold for alcohol use disorder, this type of harmful alcohol consumption accounts for three-quarters of the yearly economic burden attributable to alcohol (Center for Behavioral Health Statistics and Quality, 2016). Also, in 2015, 12.5 million individuals reported past-year misuse of a pain reliever—increasing risk for a variety of consequences including overdose—but only 2.9 million met diagnostic criteria for a DSM prescription medication disorder (Office of the Surgeon General, 2016). Given the public health and safety burden conferred by this broad population of individuals engaging in various degrees of problem use, understanding more about them and how they resolve such problems is important, regardless of whether or not they meet criteria for an AOD disorder, per se.
Importantly, as noted above, our study is cross-sectional and correlational, therefore, appropriate caution should be taken when making inferences about dynamic changes in the same individuals, as well as any causal connections among variables. Future research should attempt to capture dynamic shifts longitudinally in the same individuals over time to shed more light on these preliminary findings. Also, although state of the art methodology was employed to ensure national representativeness of the sample, we cannot be absolutely certain of this degree of national representativeness. Current findings, therefore, should be considered as useful population benchmarks pending replication in further samples.
Conclusion
It has long been recognized that recovery from serious AOD problems is not just a matter of abstinence or symptom reductions but improvements in functioning, psychological well-being, and quality of life. The US Substance Abuse and Mental Health Services Administration (SAMHSA) defines recovery as a “process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential” (SAMHSA, 2014). With the cross-sectional design of the current study duly noted, results here suggest that individuals resolving significant AOD problems do indeed experience functional improvements and increasing satisfaction in physical, psychological, and social areas of life, and that these positive shifts generally are more rapid in the early recovery years but continue to improve over ensuing decades. Notably, however, during early recovery, women, certain racial-ethnic minority groups, and those who have suffered with opioid and stimulant-related problems appear to face ongoing challenges that point to a need for greater assistance to help them sustain the recovery process.
Supplementary Material
Acknowledgments
Funding: MCG is supported by the National Institute on Drug Abuse (T32DA002792). JFK is supported by the NIAAA K24AA22136
The authors declare no financial or other conflicts of interest that could affect the integrity or veracity of this work.
References
- Battaglia MP, Hoaglin DC, Frankel MR. Practical considerations in raking survey data. Survey Practice. 2009;2(5):1–10. [Google Scholar]
- Bethell C, Fiorillo J, Lansky D, Hendryx M, Knickman J. Online Consumer Surveys as a Methodology for Assessing the Quality of the United States Health Care System. J Med Internet Res. 2004;6(1):e2. doi: 10.2196/jmir.6.1.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat. 2007;33(3):221–228. doi: 10.1016/j.jsat.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Bureau of Justice Statistics. Drug Use and Dependence, State and Federal Prisoners, 2004. Washington, DC: Office of Justice Programs, Bureau of Justice Statistics. Department of Justice publication NCJ 213530; 2006. [Accessed November 30, 2017]. Available at: https://www.bjs.Gov/Content/Pub/Pdf/Dudsfp04.pdf. Revised January 19, 2007. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health (NSDUH): Methodological Summary and Definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) Unweighted Response Rates for The National Health and Nutrition Examination Survey (NHANES) 2011–2012. CDC National Center for Health Statistics; Hyattsville, MD: 2013. [Accessed November 30, 2017]. Available at: https://www.cdc.gov/nchs/nhanes/response_rates_cps.htm. [Google Scholar]
- Chang L, Krosnick JA. National Surveys Via RDD Telephone Interviewing Versus the Internet: Comparing Sample Representativeness and Response Quality. Public Opin Q. 2009;73(4):641–678. [Google Scholar]
- Cloud W, Granfield R. Conceptualizing recovery capital: expansion of a theoretical construct. Subst Use Misuse. 2008;43(12–13):1971–1986. doi: 10.1080/10826080802289762. [DOI] [PubMed] [Google Scholar]
- Da Rocha NS, Power MJ, Bushnell DM, Fleck MP. The EUROHIS-QOL 8-item index: comparative psychometric properties to its parent WHOQOL-BREF. Value Health. 2012 May;15(3):449–57. doi: 10.1016/j.jval.2011.11.035. Epub 2012 Feb 9. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Saha TD, Grant BF. Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug Alcohol Depend. 2015:56–61. doi: 10.1016/j.drugalcdep.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Titus J, White M, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): Administration Guide for The GAIN and Related Measures. Chestnut Health Systems; Bloomington, IL: 2002. [Accessed November 30, 2017]. Available at: https://chestnut.app.box.com/v/GAIN-I-Materials/file/63671257181. [Google Scholar]
- Dennis ML, Foss MA, Scott CK. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 2007;31(6):585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Donovan D, Mattson ME, Cisler RA, Longabaugh R, Zweben A. Quality of life as an outcome measure in alcoholism treatment research. J Stud Alcohol Suppl. 2005;15:119–139. doi: 10.15288/jsas.2005.s15.119. [DOI] [PubMed] [Google Scholar]
- DuPont RL, Compton WM, McLellan AT. Five-Year Recovery: A New Standard for Assessing Effectiveness of Substance Use Disorder Treatment. J Subst Abuse Treat. 2015;57:1–5. doi: 10.1016/j.jsat.2015.06.024. [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KL, Siedlarz KM, Bergguist K, Angerson G, Kreek MJ, Sinha R. Sex-specific dissociations in autonomic and HPA responses to stress and cues in alcohol-dependent patients with cocaine abuse. Alcohol Alcohol. 2009;44(6):575–585. doi: 10.1093/alcalc/agp060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gfk. [Accessed November 30, 2017];Knowledgepanel Design Summary. 2013 Available at: http://www.Knowledgenetworks.Com/Knpanel/Docs/Knowledgepanel(R)-Design-Summary-Description.pdf.
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS. Epidemiology of DSM-5 Alcohol Use Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin ML, Bennett HE, Fitzmaurice GM, Hill KP, Provost SE, Weiss RD. Health-related quality of life among prescription opioid-dependent patients: Results from a multi-site study. Am J Addict. 2015 Jun;24(4):308–14. doi: 10.1111/ajad.12188. Epub 2015 Mar 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groshkova T, Best D, White W. The Assessment of Recovery Capital: Properties and psychometrics of a measure of addiction recovery strengths. Drug Alcohol Rev. 2013;32(2):187–194. doi: 10.1111/j.1465-3362.2012.00489.x. [DOI] [PubMed] [Google Scholar]
- Heeren T, Edwards EM, Dennis JM, Rodkin S, Hingson RW, Rosenbloom DL. A comparison of results from an alcohol survey of a prerecruited Internet panel and the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2008;32(2):222–229. doi: 10.1111/j.1530-0277.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Moos RH, Cohen C. Social and community resources and long-term recovery from treated and untreated alcoholism. J Stud Alcohol. 1997 May;58(3):231–8. doi: 10.15288/jsa.1997.58.231. [DOI] [PubMed] [Google Scholar]
- Hunt WA, Barnett LW, Branch LG. Relapse rates in addiction programs. J Clin Psychol. 1971;27(4):455–456. doi: 10.1002/1097-4679(197110)27:4<455::aid-jclp2270270412>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Borkman TJ, Laudet A, Ritter LA, Witbrodt J, Subbaraman MS, Stunz A, Bond J. Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs. 2014;75(6):999–1010. doi: 10.15288/jsad.2014.75.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF. How Can Jobs, Housing, & Friends Aid Remission? The nuances of neuroscience, addiction, social resources, and recovery. Psychology Today, Blog. 2017 Posted Sep 12, 2017. [Google Scholar]
- Kelly JF, Bergman BG, Hoeppner BB, Vilsaint CL, White WL. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug Alcohol Depend. 2017;181:162–169. doi: 10.1016/j.drugalcdep.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Hoeppner BB. Does Alcoholics Anonymous work differently for men and women? A moderated multiple-mediation analysis in a large clinical sample. Drug Alcohol Depend. 2013;130(1–3):186–193. doi: 10.1016/j.drugalcdep.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Hoeppner BB. A biaxial formulation of the recovery construct. Addict Res Theory. 2014;23(1):5–9. [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Laudet AB. The case for considering quality of life in addiction research and clinical practice. Addict Sci Clin Pract. 2011;6(1):44–55. [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Becker JB, White WL. Don’t wanna go through that madness no more: Quality of life satisfaction as predictor of sustained remission from illicit drug misuse. Subst Use Misuse. 2009;44(2):227–252. doi: 10.1080/10826080802714462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, Morgen K, White WL. The Role of Social Supports, Spirituality, Religiousness, Life Meaning and Affiliation with 12-Step Fellowships in Quality of Life Satisfaction Among Individuals in Recovery from Alcohol and Drug Problems. Alcohol Treat Q. 2006;24(1–2):33–73. doi: 10.1300/J020v24n01_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: When are these medications most helpful? Addiction. 2013;108(2):275–293. doi: 10.1111/j.1360-0443.2012.04054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE. Addictions: A comprehensive guidebook. 2. Oxford University Press; New York: 2013. [Google Scholar]
- Meyers RJ, Smith JE. Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach. Guilford Press; New York: 1995. [Google Scholar]
- Novak SC, Kroutil LA, Williams RL, Van Brunt DL. The nonmedical use of prescription ADHD medications: Results from a national Internet panel. Subst Abuse Treat Prev Policy. 2007;2:32. doi: 10.1186/1747-597X-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, And Health. United States Department of Health and Human Services; Washington, DC: 2016. [PubMed] [Google Scholar]
- Prendergast ML, Podus D, Chang E, Urada D. The effectiveness of drug abuse treatment: A meta-analysis of comparison group studies. Drug Alcohol Depend. 2002;67(1):53–72. doi: 10.1016/s0376-8716(02)00014-5. [DOI] [PubMed] [Google Scholar]
- Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: Construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Pers Soc Psychol Bull. 2001;27(2):151–161. [Google Scholar]
- Schmidt S, Muhlan H, Power M. The EUROHIS-QOL 8-Item Index: Psychometric results of a cross-cultural field study. Eur J Public Health. 2006;16(4):420–428. doi: 10.1093/eurpub/cki155. [DOI] [PubMed] [Google Scholar]
- Sher KJ. The Oxford handbook of substance use and substance use disorders. 1. Oxford University Press; New York: 2016. [Google Scholar]
- Skinner CJ, Holt D, Smith TMF. Analysis of Complex Surveys. Wiley; Hoboken, NJ: 1989. [Google Scholar]
- StataCorp [computer program] Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Definition of Recovery. US Department of Health and Human Services; 2014. [Google Scholar]
- Thomas RK. Fast and Furious…Or Much Ado About Nothing? Sub-Optimal Respondent Behavior and Data Quality. J Advert Res. 2014;54(1):17–31. [Google Scholar]
- Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, White W. Development and validation of a Brief Assessment of Recovery Capital (BARC-10) for alcohol and drug use disorder. Drug and Alc Dep. 2017;177(1):71–76. doi: 10.1016/j.drugalcdep.2017.03.022. [DOI] [PubMed] [Google Scholar]
- Wells EA, Saxon AJ, Calsyn DA, Jackson TR, Donovan DM. Study results from the Clinical Trials Network’s first 10 years: Where do they lead? J Subst Abuse Treat. 2010;38(Suppl 1):S14–S30. doi: 10.1016/j.jsat.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL. Recovery/Remission from Substance Use Disorders: An Analysis of Reported Outcomes in 415 Scientific Reports, 1868–2011. Philadelphia Department of Behavioral Health and Intellectual Disability Services; Philadelphia, PA: 2012. [Google Scholar]
- Witkiewitz K, Masyn KE. Drinking Trajectories Following an Initial Lapse. Psychol Addict Behav. 2008;22(2):157–167. doi: 10.1037/0893-164X.22.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, Krosnick JA, Chang L, Javitz HS, Levendusky MS, Simpser A, Wang R. Comparing the accuracy of RDD telephone surveys and internet surveys conducted with probability and non-probability samples. Public Opin Q. 2001;75(4):709–747. [Google Scholar]
- Zemore SE, Pagano ME. Kickbacks from helping others: health and recovery. Recent Dev Alcohol. 2008;18:141–66. doi: 10.1007/978-0-387-77725-2_9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.