Abstract
Introduction
Integration of psychological services into pediatric primary care is increasingly common, but models of integration vary with regards to their level of coordination, co-location, and integration. High-integration models may provide some distinct advantages, such as preventative care and brief consultation for sub-clinical behavior concerns; however, psychologists face barriers to seeking reimbursement for these services. Alternatives to traditional psychotherapy and psychological testing codes, specifically Health & Behavior (H&B) codes, have been proposed as one method for supporting integrated care. The aim of this study was to investigate the relationships between psychologists’ reported billing practices, reimbursement rates, and model of integration in pediatric primary care.
Method
As part of a larger survey study, 55 psychologists working in pediatric primary care reported on characteristics of their practice’s model of integration, billing practices, and frequency of reimbursement for consultative services.
Results
Compared to those who categorized their integrated care model as Co-located, psychologists who endorsed working in Integrated models reported a significantly higher usage of H&B codes and more frequent reimbursement for consultations. Overall, use of H&B codes was associated with higher reported levels of coordination and integration.
Discussion
Survey results showed a clear pattern of higher integration being associated with greater utilization of H&B codes and better reimbursement for consultation activities. These results underscore the importance of establishing and maintaining billing and reimbursement systems that adequately support integrated care.
Keywords: Integrated care, primary care, pediatrics, billing practices, reimbursement
Behavioral health professionals are increasingly being integrated into pediatric primary care (PPC; Asarnow, Kolko, Miranda, & Kazak, 2017). Models of primary care integration vary on dimensions of coordination (i.e., the degree of shared treatment planning by behavioral and medical providers), co-location (i.e., the relative physical proximity of medical and behavioral services), and integration (i.e., the degree to which behavioral services are part of routine medical care for all patients; Blount, 2003). While models differ on these dimensions, the terms are used nominally to denote categories of care (Herein, capitalization indicates categorical use of those terms.): Coordinated (i.e., high coordination, low co-location, low integration), Co-located (i.e., low or high coordination, high co-location, low integration), and Integrated (i.e., high coordination, high co-location, high integration).
High-integration models of care may feature a host of nontraditional services, including screening, prevention, and consultation for sub-clinical and prodromal behavioral problems (Asarnow et al, 2017). While potentially beneficial, obtaining reimbursement for the full suite of high-integration activities may prove challenging (Mauch, Kautz, & Smith, 2008). For example, most PPC psychologists report providing screening and consultation services, but a minority bill for these services (Hoffses et al., 2017).
Talmi and Fazio (2012) proposed utilization of Health and Behavior (H&B) codes to bill for behavioral services provided during routine care in PPC. Unlike Current Procedural Technology (CPT) psychotherapy and psychological testing codes, H&B codes do not require a mental health diagnosis to be reimbursed; potentially allowing provision of behavioral services to individuals who would benefit from care, but do not exhibit psychopathology. Despite this potential, some reports cast doubt on the viability H&B codes in PPC settings (Cederna-Meko, Ellens, Burrell, Perry, & Rafiq, 2016) and reimbursement for H&B codes is currently unavailable in some states (Substance Abuse and Mental Health Services Administration [SAMHSA], 2014). So, while H&B codes may support a higher level of integration in PPC, the current impact of H&B codes is unclear.
If high-integration models are to proliferate in PPC, it will be important to identify sustainable methods of payment that adequately support that work. To better understand payment in PPC, this study explored associations between PPC psychologists’ reported billing practices, reimbursement, and integration models. This information was collected as part of a larger study assessing PPC psychologists’ professional practices, training, and funding (Hoffses et al., 2017). A positive correlation between level of integration, utilization of H&B codes, and more frequent reimbursement for consultation services was hypothesized.
Method
Survey instrument
Procedures were approved by the authors’ institutional review boards. Briefly, a survey was created by a group of PPC psychologists through an iterative piloting and refinement process to characterize current PPC practice parameters (see Hoffses et al. [2017], for a full description of survey development). The survey items reported on herein are available as an online supplement.
Model of integration
Participants were asked to identify their PPC practice as Coordinated, Co-located, or Integrated, and rate their practice on the dimensions of coordination, co-location, and integration on a 4-point scale from not at all to fully. Definitions and rating scale anchors derived from Blount (2003) were provided for each category and dimension.
Billing practices
Participants rated their frequency of billing CPT codes (e.g., psychotherapy and psychological testing codes), H&B codes, consultation codes, and “other” codes on a 4-point scale from never to often. The consultation code category was included as a catch-all for any billing of consultation outside of the other options.
Consultation reimbursement
Participants provided a free response estimate of the percentage of their consultation activities that are reimbursed by providing a percentage between 0–100.
Recruitment and Data Collection
The survey was distributed through relevant professional listservs and a registry of PPC training programs. Eligible participants were licensed psychologists who reported working in PPC. Data were collected electronically using Research Electronic Data Capture (REDCap) electronic data capture tools (Harris et al., 2009).
Analyses
Spearman’s Rho was calculated to test for associations between variables. Kruskal-Wallis tests and one-way ANOVAs were performed to test for differences between categorical models of integration for ordinal and continuous variables, respectively. If an overall significant effect was detected, post-hoc comparisons were made using the Mann-Whitney U or Tukey HSD tests corrected for multiple comparisons.
Results
A total of 55 psychologists completed survey items assessing integration model, billing practices, and consultation reimbursement. Table 1 displays information for dimensional ratings of coordination, colocation, integration, as well as billing frequency and percent of consultations reimbursed. Ratings of coordination, co-location, and integration ratings were all significantly correlated. Use of H&B codes was positively associated with levels of reported coordination and integration, as well as consultation code usage and reimbursement for consultation. Consultation code utilization was positively correlated with estimated percentage of consultations reimbursed.
Table 1.
Means, standard deviations, and correlations of integration dimension ratings, billing practices, and reimbursement for consultation.
| Response Item | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Coordination rating | 3.27 | .68 | - | |||||||
| 2. Colocation rating | 3.67 | .64 | .56*** | - | ||||||
| 3. Integration rating | 2.95 | .87 | .72*** | .52*** | - | |||||
| 4. H&B codes | 2.23 | 1.13 | .46*** | .26 | .45*** | - | ||||
| 5. CPT codes | 3.54 | 1.00 | .01 | −.10 | −.10 | .08 | - | |||
| 6. Consultation codes | 1.56 | .85 | −.08 | −.03 | .27 | .34** | .21 | - | ||
| 7. Other codes | 1.35 | .93 | .08 | .12 | .08 | .28 | −.00 | .00 | - | |
| 8. % of consultations reimbursed | 26.00 | 33.60 | .09 | .18 | .18 | .31 | .10 | .39** | .17 | - |
Note. Ratings were made on a 4-point Likert scale except for #8, which allowed for free entry of an integer between 0–100; H&B= Health and Behavior; CPT = Current Procedural Terminology;
p ≤ .05;
p ≤ .01;
p ≤ .001.
Three respondents identified their PPC model as Coordinated, contrasted with 17 Co-located and 35 Integrated. Analyses were conducted with and without the small Coordinated group. No differences were found, so they were retained in the results. The Integrated group reported higher ratings of coordination (M=3.57, SD=.55), co-location, (M=3.85, SD=.44) and integration (M=3.34, SD=.73) than Co-located (coordination: M=2.82, SD=.53; co-location: M=3.53, SD=.51; integration: M=2.24, SD=.56) and Coordinated (coordination: M=2.33, SD=.58; co-location: M=2.33, SD=.1.5; integration: M=2.33, SD=1.16).
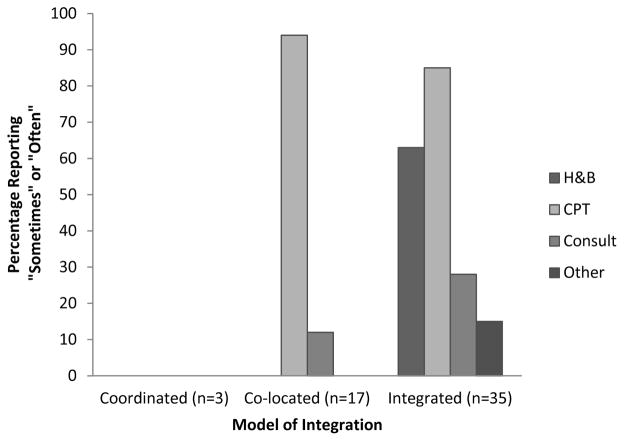
Figure 1 displays the percentage of respondents who endorsed using each billing code type “sometimes” or “often” across integration models. There was a significant interaction between the reported model of integration and utilization frequency for both H&B (H[2]=19.2, p<.001) and CPT codes (H[2]=7.3, p=.03). Pairwise comparisons indicated H&B code utilization was significantly higher for Integrated than Co-located models (U=84.5, p<.001, r=.58) and CPT code utilization was significantly higher for Co-located than Coordinated models (U=10.0, p<.01, r=.26). Other pairwise comparisons were non-significant after correction for multiple comparisons.
Figure 1.
The percentage of pediatric primary care psychologists who reported using different billing codes “sometimes” or “often.” H&B = Health and Behavior; CPT = Current Procedural Terminology; Consult = consultation codes.
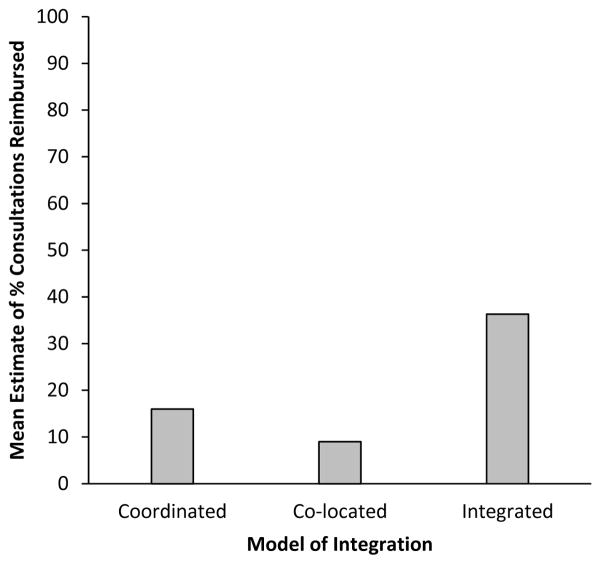
A significant effect of integration model on estimated percentage of consultations reimbursed emerged, (F[2,47]=4.10, p=.02). Post-hoc comparisons indicated the estimated percentage of consultations reimbursed was higher for Integrated (M=37%, SD=36.7) than Co-located (M=9%, SD=20.1), p=.02. Other pairwise comparisons were non-significant.
Discussion
Survey responses from PPC psychologists evidenced a pattern of higher integration being associated with greater utilization of H&B codes and more frequent reimbursement for consultation activities. While the exact nature of this association remains unclear, these results have implications for practitioners and policymakers. Pediatric practices pursuing full integration should take advantage of available compensation strategies, including but not limited to H&B codes. For policymakers and payers who wish to encourage high-integration models of PPC, the findings suggest the establishment of payment systems that support a wide range of valued activities is essential. The findings further buttress the movement to explore alternatives to traditional payment, such as bundled payment and capitation, to support integrated care (see Miller et al. [2017] for a recent review).
While this study suggests some benefits of H&B code utilization, the impact of H&B codes in PPC remains unclear. For psychologists working in Integrated models, only 37% of consultations were estimated to be reimbursed. Certain high-integration activities, such as consultations for patients with diagnosed psychopathology, ostensibly are not reimbursable under H&B codes. Further, this study attempted to assess whether consultations are reimbursed, but did not evaluate how well those services are reimbursed. Remittance for H&B codes is typically below that for CPT codes, and may not adequately support psychologists’ efforts. Alternatively, because H&B codes represent less intensive care, they may allow for higher volume of patient care that results in revenues commensurate to CPT codes. It is also important to consider that high-integration may offer some financial value beyond direct billing. For example, the presence of a behavioral health consultant may allow physicians to see more patients, thereby generating higher revenues (Gouge, Polaha, Rogers, & Harden, 2016).
This study has a number of limitations and any conclusions should be considered tentative. The sample size was relatively small and its representativeness is unclear. Only psychologists were surveyed, and the findings may not pertain to other professionals, such as clinical social workers, who make up a considerable portion of the integrated PPC workforce. Integration characteristics and billing practices were based on psychologists’ subjective impressions rather than validated measures, and may be inaccurate. Survey items related to billing and reimbursement assessed overall practices, but not exact procedures for specific activities (e.g., brief consultation for subclinical behavioral concerns) or actual dollar amounts reimbursed, precluding a more fine-grained analysis. Further, the survey assessed perceived level of integration, reported use of H&B codes, and proportion of consultations reimbursed, but did not specifically assess the availability of reimbursement for H&B codes, which varies state-to-state (SAMSHA, 2014), or how often practices seek reimbursement of consultation. Whether the availability of H&B codes causally impacts the level of integration, or if highly-integrated practices are just more likely to seek out this form of reimbursement is unclear.
Despite limitations, the results provide an interesting perspective on the state of payment for psychologists in PPC and points to the viability of a highly integrated approach when appropriate compensation is available. As integrated care evolves, policy makers, researchers, and clinicians should collaborate to develop and sustain family-centered models of care that are evidence-based, pragmatic, and financially viable.
Supplementary Material
Figure 2.
Mean values of estimated of percentage of consultation activities reimbursed by integration model type. Post-hoc comparisons indicated percentage of reimbursement for consultation was significantly higher for Integrated (M=37%, SD=36.7) than Co-located (M=9%, SD=20.1), p=.02.
Contributor Information
Andrew R. Riley, Institute on Development & Disability, Department of Pediatrics, Oregon Health & Science University, Portland, Oregon
Allison Grennan, Munroe-Meyer Institute, University of Nebraska Medical Center, Omaha, Nebraska.
Kathryn Menousek, Munroe-Meyer Institute, University of Nebraska Medical Center, Omaha, Nebraska.
Kathryn W. Hoffses, Division of Behavioral Health, Nemours/A.I. duPont Hospital for Children, Wilmington, Vermont
References
- Asarnow JR, Kolko DJ, Miranda J, Kazak AE. The Pediatric Patient-Centered Medical Home: Innovative models for improving behavioral health. American Psychologist. 2017;72(1):13. doi: 10.1037/a0040411. [DOI] [PubMed] [Google Scholar]
- Blount A. Integrated Primary Care: Organizing the Evidence. Families, Systems, & Health. 2003;21(2):121. [Google Scholar]
- Cederna-Meko CL, Ellens RE, Burrell KM, Perry DS, Rafiq F. An exploration of behavioral health productivity and billing practices within pediatric primary care. Journal of Pediatric Psychology. 2016;41(10):1133–1143. doi: 10.1093/jpepsy/jsw063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouge N, Polaha J, Rogers R, Harden A. Integrating behavioral health into pediatric primary care: Implications for provider time and cost. Southern Medical Journal. 2016;109(12):774. doi: 10.14423/SMJ.0000000000000564. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffses KW, Riley AR, Menousek K, Schellinger K, Grennan A, Cammarata C, Steadman JL. Professional practices, training, and funding mechanisms: A survey of pediatric primary care psychologists. Clinical Practice in Pediatric Psychology. 2017;5(1):39–49. [Google Scholar]
- Mauch D, Kautz MA, Smith S. Reimbursement of mental health services in primary care settings. 2008 (HHS Pub. No. SMA-08-4324). Retrieved from Rockville, MD: http://www.integration.samhsa.gov/Reimbursement_of_Mental_Health_Services_in_Primary_Care_Settings.pdf.
- Miller BF, Ross KM, Davis MM, Melek SP, Kathol R, Gordon P. Payment reform in the patient-centered medical home: Enabling and sustaining integrated behavioral health care. American Psychologist. 2017;72(1):55–68. doi: 10.1037/a0040448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Paying for primary care and behavioral health services provided in integrated care settings. 2014 Retrieved from http://www.integration.samhsa.gov/financing/billing-tools.
- Talmi A, Fazio E. Commentary: Promoting health and well-being in pediatric primary care settings: Using health and behavior codes at routine well-child visits. Journal of Pediatric Psychology. 2012;37(5):496–502. doi: 10.1093/jpepsy/jss047. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.