Abstract
Background
With the burden of chronic illness increasing globally, self-management is a crucial strategy in reducing healthcare costs and increasing patient quality of life. Low income and low health literacy are both associated with poorer health outcomes and higher rates of chronic disease. Thus, self-management represents an important healthcare strategy for these populations. The purpose of this study is to review self-management interventions in populations with low income or low health literacy and synthesize the efficacy of these interventions.
Methods
A systematic review of trials evaluating the efficacy of self-management interventions in populations with low income or low health literacy diagnosed with a chronic illness was conducted. Electronic databases were primarily searched to identify eligible studies. Data were extracted and efficacy summarized by self-management skills, outcomes, and content tailoring.
Results
23 studies were reviewed, with ten reporting an overall positive effect on at least one primary outcome. Effective interventions most often included problem-solving as well as taking action and/or resource utilization. A wide range of health-related outcomes were considered, were efficacious empowerment and disease-specific quality of life were found to be significant. The efficacy of interventions did not seem to vary by duration, format, or mode of delivery or whether these included individuals with low health literacy and/or low income. Tailoring did not seem to impact on efficacy.
Discussion
Findings suggest that self-management interventions in populations with low income or low health literacy are most effective when three to four self-management skills are utilized, particularly when problem-solving is targeted. Healthcare providers and researchers can use these findings to develop education strategies and tools for populations with low income or low health literacy to improve chronic illness self-management.
Electronic supplementary material
The online version of this article (10.1007/s11606-017-4265-x) contains supplementary material, which is available to authorized users.
KEY WORDS: self-management, chronic disease, disease management, vulnerable populations, health literacy
BACKGROUND
Currently, 50% of Americans1 and 60% of Canadians2 are diagnosed with a chronic condition, with an increasing number of patients suffering from multi-morbidities.3 The prevalence of chronic disease and the long-term follow-up required in chronic disease management are resulting in a substantial economic burden on the healthcare system.4 To assess and improve chronic disease care and control healthcare costs, the Chronic Care Model (CCM) was developed, emphasizing six essential elements in the management of chronic illnesses: healthcare organization, linkages to community resources, delivery system design, clinical decision support, clinical information systems, and self-management support.5 Several reviews have found that implementation practices in accordance with the CCM improve the quality of care and health outcomes for patients6,7 as well as reduce healthcare-associated costs.7,8 Of the six CCM elements, self-management support is the most commonly implemented and has received the most attention.7
Self-management refers to the tasks that an individual must undertake to live well with a chronic condition.9 It includes five core skills: (1) decision-making, (2) problem-solving, (3) utilizing resources, (4) forming a client-healthcare provider partnership, and (5) taking action.10 Systematic reviews have shown that self-management interventions have mixed efficacy across chronic illnesses,11–15 with positive outcomes particularly noted for symptom management, pain control, and role functioning.10,16 This research suggests that both the type of chronic illness and the nature of the self-management skills utilized mediate the efficacy of the interventions.17,18 Although most studies have been conducted with populations of females with higher socioeconomic status (SES) and education, 19,20 in the past 2 decades, there has been increased attention given to particular vulnerable subgroups, including those of low income or low health literacy.
Education and income are key factors in determining health.21 The United States Census Bureau reports that 46.7 million Americans are affected by poverty.22 This is significant because chronic illnesses and lower life expectancies are more prevalent in low-income populations regardless of age, gender, race, and geographical location.23 Lifestyle factors including limited access to affordable housing, healthy foods, and recreational facilities, as well as increased stress levels, may contribute to these unfavorable health outcomes.24 Further, low-income populations may struggle with limited access to healthcare.24
Additionally, low levels of education are associated with poorer health, more stress, and lower self-efficacy.25 Individuals with low education tend to have limited socioeconomic mobility, lower incomes, insecure employment, and poorer working conditions, all of which contribute to adverse health outcomes.26 Importantly, low education tends to decrease overall literacy and health literacy levels, which in turn adversely impact on the development self-management skills.26 It is estimated that 36% of adults in the US and 60% in Canada have limited health literacy.27,28 This has been associated with decreased medication adherence and use of preventative services, higher rates of hospitalizations and mortality, and overall poorer health outcomes.4
Thus, interventions for improving self-management skills among a population of low-income or low health literate patients may have profound effects on health outcomes. To our knowledge, the present review is the first one to describe the current use of self-management interventions in patients with low income and/or low health literacy and synthesize the efficacy of these interventions by self-management skills, health-related outcomes, and extent of content tailoring.
METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was used29 to conduct this descriptive systematic review of the literature (checklist included in the Electronic Supplementary Material S1).
Criteria for Considering Studies
Types of Studies and Participants
Eligible studies were published peer-reviewed experimental or quasi-experimental trials in which: (1) a group of adults with a chronic physical illness (with or without a comorbid mental illness) of low income and/or low health literacy received a self-management intervention and were compared with a group who did not receive the intervention; and (2) outcomes were measured pre- and post-intervention. Low income and low health literacy were defined as per study authors. Only English and French full texts were included, and studies dating more than 15 years ago were excluded.
Types of Interventions
Studies included were those that evaluated an intervention aimed at enhancing one or more of the five aforementioned core self-management skills.9 Restrictions were not applied to the mode of delivery or to the type of care setting. However, solely pharmacological interventions were excluded. Interventions targeting minority groups were also excluded to decrease potential confounding factors.
Types of Outcomes
The outcomes of interest included physiological, behavioral, and/or psychosocial outcomes. Other outcomes of interest included illness knowledge, financial, and healthcare service utilization. Therefore, studies were included if quantitative data were obtained for at least one relevant outcome and if statistical methods were used to evaluate the differences between control and intervention groups.
Search Methods
Eligible studies were identified through an electronic search of MEDLINE, PsycINFO, CINAHL, and Embase. The search strategy used a combination of keywords and medical subject heading (MeSH) terms related to low income, low health literacy, self-management, and the study design (see Electronic Supplementary Material S2). All titles were downloaded to EndNote. Hand searches were performed on the reference lists of all included manuscripts to identify other eligible studies. At least two authors independently assessed the initial eligibility of the retrieved titles and abstracts. The full-texts of all eligible citations were independently examined by at least three authors to confirm eligibility. Any disagreements were discussed at regular team meetings until a consensus was reached.
Data Collection
A standardized form based on the Cochrane Handbook for Systematic Reviews of Interventions was used to extract data30 from each manuscript (e.g., citation details, study design, inclusion criteria, sample size, population characteristics, self-management skills targeted). Two authors independently extracted the data, and disagreements were discussed and resolved with a third author.
The methodological quality of included studies was assessed by five authors using the following criteria30,31: control group, n > 25 per group, sufficient power to detect moderate effect, inclusion criteria specified, assessment of reliability and validity of measures, adequate sequence generation, allocation concealed, blind assessment, intention to treat used, > 80% of the sample in the final analysis, and reasons for attrition stated. Each criterion was scored as either a 1 = yes or 0 = no. A high methodological quality was defined as a score of at least 9 moderate methodological quality between 6 and 8, and low quality as scores of ≤5.
Data Synthesis
As there was substantial heterogeneity across studies in study design, demographics, type of interventions, and outcomes, a descriptive synthesis was conducted as opposed to a meta-analysis.32 Date extracted were summarized by one author and verified by at least one other author. Efficacy of the interventions was summarized based on self-management skills, outcomes, and integration of individualized assessment (tailoring).33 For each outcome, efficacy was based on statistical significance (p < 0.05) and a Cohen’s effect size (ES) of at least d = 0.2 or odds ratio (OR) > 1.44.34 For studies lacking sufficient data to calculate an ES, only statistical significance was considered. For the analysis by self-management skills and tailoring, an intervention was said to be effective, if the results were significant for at least one primary outcome. For the analysis by outcome, if at least 50% of the analyses were positive, the conclusion was that the interventions were effective for that outcome.
RESULTS
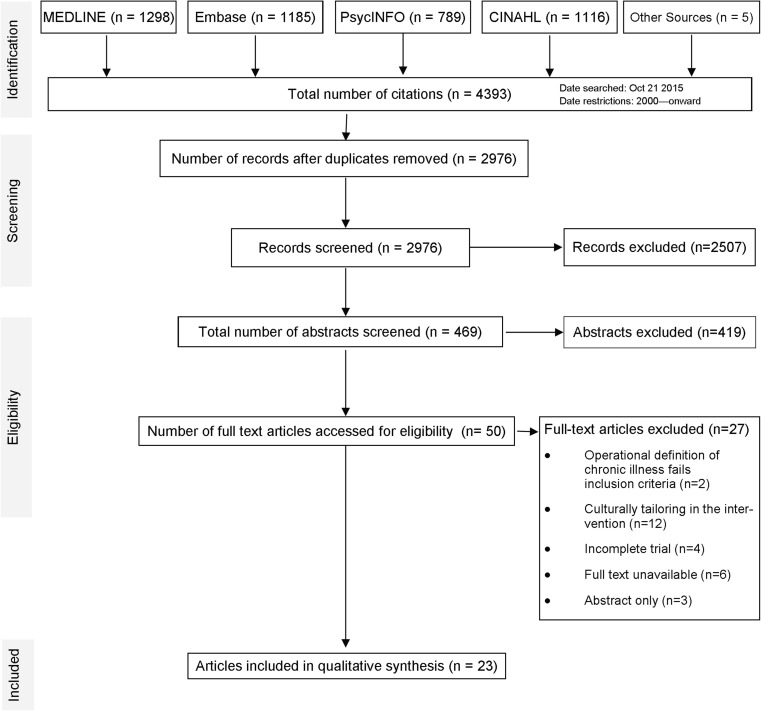
The electronic search identified 2976 titles, whereby 50 manuscripts underwent full-text review. Of these, 27 were subsequently excluded, resulting in 23 studied included in the present review. Figure 1 outlines the systematic review process.
Fig. 1.
PRISMA flow diagram. This figure illustrates the methodological flow of our study selection
Overview of Studies
Types of Studies and Participants
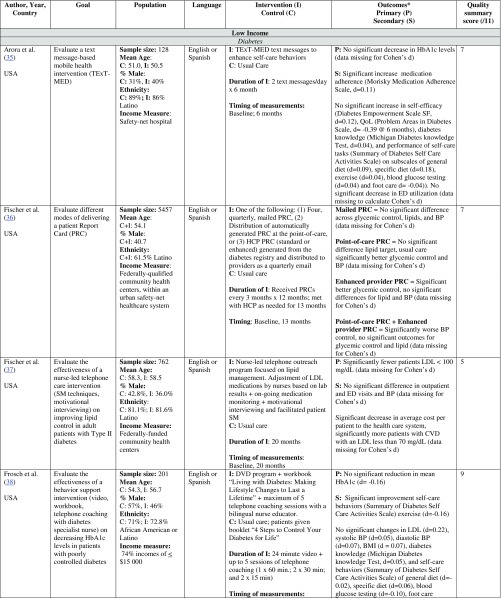
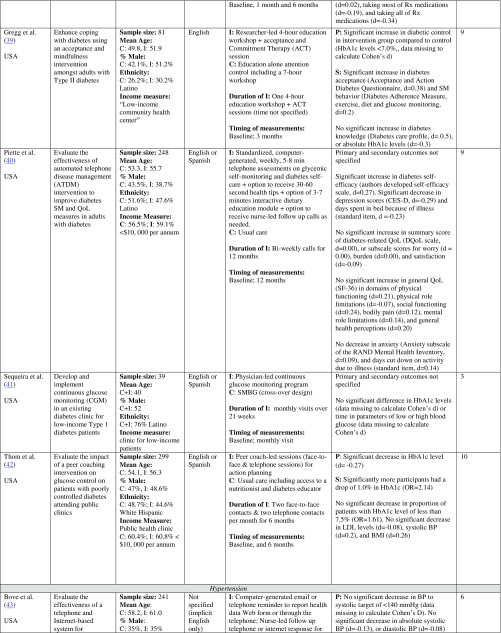
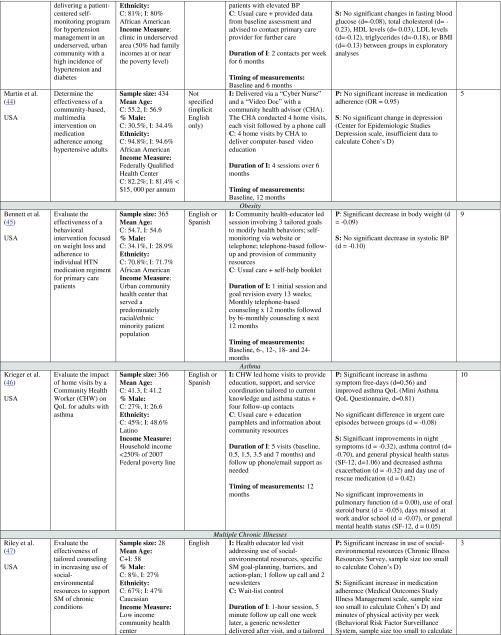
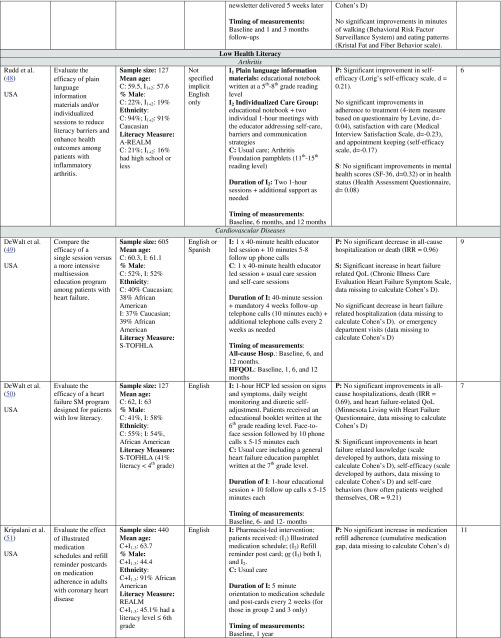
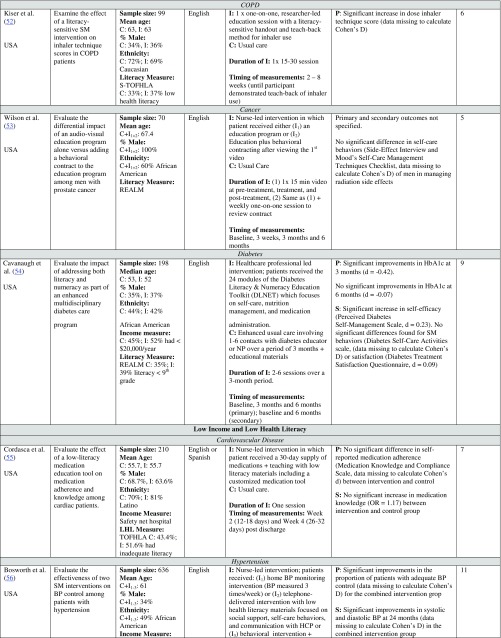
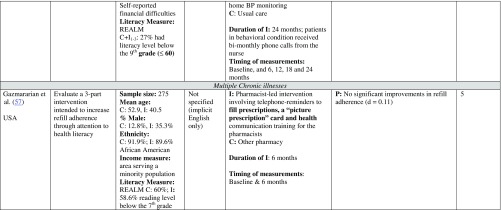
Table 1 summarizes the characteristics of the 23 studies included. Most studies compared two groups,35,37–40,42–47,49,50,52,54,55,57 and all studies were conducted in the US, with sample sizes ranging from 2847 to 5457.36 Participants were predominately female aged 40–68 diagnosed with diabetes (n = 9) or hypertension (n = 3). The majority of the studies examined the efficacy of self-management interventions in a population of low-income participants exclusively (n = 13). Seven studies examined the efficacy in participants with low health literacy. Three studies included participants with both low health literacy and low income.
Table 1.
Characteristics of Included Studies (N = 23)
ED emergency department, HbA1c hemoglobin A1c, HCP healthcare provider, QoL quality of life, SM self-management, SMBG self-monitoring blood glucose. *Effect size was calculated as the mean difference (using the last time point, unless a primary endpoint was specified) of the two study groups divided by the pooled standard deviation of the difference
Low income defined. Most studies operationalized low income by stating that participants were recruited from healthcare facilities that were “federally qualified heath centers” (n = 4),36,37,41,44 “safety-net” clinics (n = 3),35,38,55 or “low-income” or “urban” community or public health centers.39,42,45,47 Three studies identified the target communities as “underserved”43 or low income.40,57 Seven studies reported the level of participant income in dollar amounts, with the majority of annual family incomes being under $10,000 USD.38,40,42,44,45,47,57
Low literacy defined. Five studies measured literacy using the Rapid Estimate of Adult Literacy in Medicine (REALM) scale,51,53,54,56,57 with three of these studies defining low health literacy as a score between 44 and 60 (6th to 9th grade reading level51,54,56). Three studies utilized the Short Test of Functional Health Literacy in Adults (S-TOFHLA),49,50,52 with cutoff scores of less than 2249,52 or less than 16.50 The remaining study used the Test of Functional Health Literacy in Adults (TOFHLA), whereby a score of 0 to 59 constitutes inadequate literacy.55
Types of Self-Management Interventions
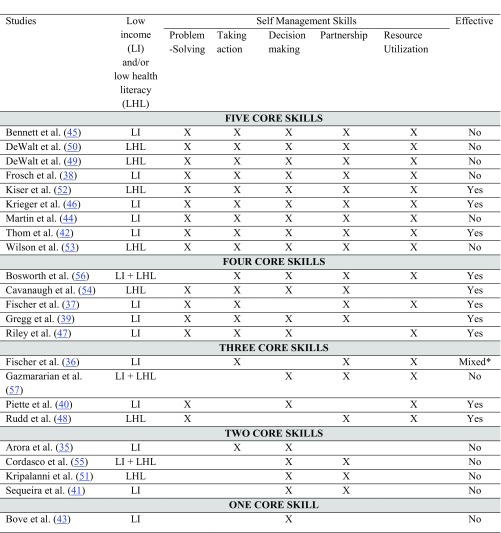
Intervention duration was variable lasting from a single session to 24 months. Most interventions were delivered face to face by a healthcare professional (n = 17).39,41,42,44–57 As detailed in Table 2, interventions were also found to vary in terms of which of the five self-management skills was targeted. Most interventions focused on four to five skills. The most common self-management skill addressed was decision-making (n = 20) and partnership with a healthcare provider (n = 19). These skills were followed by resource utilization (n = 16) and taking action (n = 16). Although problem-solving was the least addressed skill, it was still included in 15 studies.
Table 2.
Self-Management Skills Utilized
Note: Definitions of core skills: (a) Problem solving: the ability to define the problem, generate and implement solutions, and evaluate outcomes; (b) taking action: involves the creation of action plans and the development of self-efficacy; (c) decision-making: includes self-monitoring and responding to changing disease condition; (d) partnership: involves forming an ongoing client-healthcare provider partnership; (e) resource utilization: the ability to seek out and use multiple health-promoting resources. *Four interventions were tested in this study, and significant outcomes were noted for the enhanced provider PRC treatment group
Methodological Quality
Table 1 provides the methodological quality score of each study (detailed quality assessment in Electronic Supplementary Material S3). Ten studies were assessed to be of high methodological quality,38–40,42,45,46,49,51,54,56 seven of moderate methodological quality,35,36,43,48,50,52,55 and the remaining six studies were assessed to be of low methodological quality.37,41,44,47,53,57
Efficacy of Self-Management Interventions
Efficacy Assessment Based on Self-Management Skills
Of the 23 interventions, 10 were found to be effective (Table 2). Nine of these used problem-solving and eight used taking action and/or resource utilization.
Five Skills
Of the nine interventions that included all five skills, only three were effective on the primary outcomes (Table 2), representing a mix of low income and low health literacy studies. Two of these were of high methodological quality and one of moderate quality. Improved primary outcomes included hemoglobin A1C levels,42 dose inhaler technique,52 asthma symptom-free days, and disease-specific quality of life.46
Four Skills
All five interventions utilizing four self-management skills were effective on the primary and secondary outcomes measured, most of which were of moderate-high methodological quality, but including both low income and low health literacy studies. All five effective interventions included taking action, with most of them also including problem-solving or partnership (Table 2). Primary outcomes targeted were blood pressure,56 hemoglobin A1C,39,54 lipids,37 and socio-environmental resources.47 Secondary outcomes were self-efficacy,54 cost to the healthcare system,37 acceptance,39 self-management behavior,39 medication adherence,47 and minutes of physical activity.47
Three Skills
Two of the four studies targeting three self-management skills were effective40,48; these were the only interventions that included problem-solving and resource utilization. No pattern was noted across the low income versus low health literacy studies. Primary outcomes favorably affected by the interventions were self-efficacy,40 depression,40 days spent in bed because of illness,40 and self-efficacy.48 The only intervention that was not effective according to Gazmararian et al.57 was the only one to omit problem-solving or taking action.
Two or One Skill(s)
None of the interventions utilizing one or two self-management skills were effective. No pattern was noted across the low income versus low health literacy studies.
Efficacy Assessment by Outcomes
There was no consistency across studies regarding the outcomes favored, with many outcomes only measured in 1–2 studies. Those measured in at least four analyses are summarized; the remaining analyses are presented in Table 1. Of note, as no efficacy patterns were noted across the low income and low health literacy studies, these are presented together. The most frequently measured outcome was blood pressure; however, only 436,56 of the 16 analyses were significant. A1C was the next most frequent outcome, with 536,39,42,54 of the 13 analyses found to be significant. Lipids were included in 12 analyses, whereby 237 were significant. Of the nine analyses focusing on medication adherence, only one47 was significant. For health behaviors, one47 out of eight analyses was significant. None of the six analyses reporting healthcare utilization were significant.37,46,49,50 One50 out of five analyses was significant for knowledge. For self-care and self-management, two39,52 out of the seven analyses were significant. A more positive result was found for empowerment, with four40,48,50,54 of the five analyses reporting significant effects. Similarly, two46,49 of the four studies for disease-specific quality of life were significant. Based on this review, only two outcomes met the criterion of being effective in at least 50% of the analyses: empowerment or self-efficacy and disease-specific quality of life.
Efficacy Based on Tailoring
Ten interventions36,38,40,44–47,50,53,57 tailored their content, and only three (all with individuals of low income) were effective.40,46,47 No pattern in terms of skills targeted was noted.
DISCUSSION
This review sought to critically appraise the empirical evidence on the efficacy of self-management interventions in a population of low-income and/or low health literate adults diagnosed with a chronic physical illness. A thorough understanding of the components of effective self-management interventions is essential given the increased number of underserved patients living with a chronic illness.26
According to the 2015 United States federal poverty guidelines, low income is defined as a family income of $24,250 USD annually or less for four people living in the same residence.58 Fifteen of the 16 studies that examined low-income populations failed to report the participant household income relative to federal poverty guidelines. Instead, the authors reported the use of self-management interventions in “federally qualified health centers,” “safety net clinics,” or low-income clinics or neighborhoods. This assumes homogeneity of the population regarding socioeconomic status. According to Darnell,59 safety net clinics may service both low income and uninsured populations. As such, based on the studies reviewed, drawing meaningful conclusions about the efficacy of self-management interventions within a low-income population presented some challenges. This is in contrast to all studies (n = 10) examining a population of low health literate adults using a validated measure of health literacy.
Reviews of self-management interventions have further found that face-to-face contact between participants and intervention leaders is associated with better outcomes.18,60 The present review did not note any patterns potentially linking the mode of delivery or the person implementing the intervention to efficacy. Similarly, although Battersby et al.60 found that numerous intervention sessions yielded better outcomes, this pattern was not noted and both single and multi-session interventions yielded positive outcomes in the present review. Other reviews have also found that chronic illness typology may moderate the efficacy of self-management interventions.18,60,61 The present review found no discernable pattern across illness type, which may be due to the limited research on self-management in chronically ill populations with low income and/or low health literacy.
The current review found that proportionally interventions using three or four self-management skills were more effective than those presenting less than three or five skills. This likely relates to the multifaceted nature of these interventions through the use of social, behavioral, and cognitive approaches to improve disease management.10 However, participants in interventions with five skills might have felt overwhelmed and/or might not have been given enough time to develop all skills. While the use of four skills appears promising, economic constraints and/or a lack of resources may hinder the development and implementation of multifaceted self-management interventions. If only one self-management skill can be targeted, findings of the current review would suggest problem-solving, as more than half of the 15 interventions with problem-solving were effective on primary outcomes and two additional studies found significant changes in secondary outcome measures.49,50 According to Savery,62 problem-solving skills help in the development of higher-order thinking. Studies examining the use of problem-based learning have shown that such an approach enables learners to identify and understand the important elements of the situation, develop an understanding of the relationship between elements, and facilitates improved decision-making, communication, and collaboration.62–64 This is likely mediated through improvements in the client’s engagement, knowledge, confidence, skills, and commitment to making optimal health adjustments.65 Arguably, the development of problem-solving skills is implicitly linked to improvements in the other four self-management skills. As such, it has the most potential for influencing behavioral, cognitive, and social health changes. In support of this, many studies have found that problem-solving is a key component of effective self-management across various chronic conditions.66,67 In addition to problem-solving, two other self-management skills were found to be effective in half of the interventions that used them: taking action and resource utilization.
In terms of efficacy of the interventions reviewed on health-related outcomes, this review highlighted that self-management interventions among individuals with a chronic illness with low health literacy and/or low income may benefit in terms of enhanced empowerment (or self-efficacy) and disease-specific quality of life. Although a central aim of self-management interventions is to increase participants’ self-efficacy to carry out a behavior,10 only five interventions measured this outcome. For many outcomes considered, less than 50% of the analyses were not significant. Partially, this finding might be explained by the reliance on mostly ‘distal’ outcomes (e.g., lipids, blood pressure), which depend on a number of factors that are not directly influenced by the interventions.68 Reliance on proximal outcomes or outcomes that can be directly affected by the interventions’ content and goals might have been more appropriate.68
Tailoring was another feature considered in the present review, as it is hypothesized to increase the relevance, interest, and use of interventions.69,70 In general, the process of tailoring prunes out the superfluous or irrelevant information and highlights only what individuals would find most pertinent.69,70 Tailored print-71,72 and web-based73 interventions have been found to be more effective than non-tailored approaches. Contrary to these results, less than 50% of interventions with tailored content were found to be overall effective.
Strengths and Limitations
Methods are described in great detail to enhance reproducibility. However, one limitation is that several studies did not explicitly explain the core components of their self-management intervention. However, to reduce bias, five reviewers independently assessed each intervention to identify its self-management skills. Another limitation is the low methodological quality of some studies. Also, for many outcomes and some illnesses the number of analyses was small, and findings should be interpreted with caution. Furthermore, mental health comorbidities were typically not documented across studies, which precludes any subgroup analyses.
Implications for Future Research
Further inquiry is warranted regarding the use of problem-solving, taking action and resource utilization in self-management interventions, and determining which combination of these three skills result in the highest efficacy. In addition, measuring both proximal and distal outcomes in future studies might assist in further determining those interventions that are most effective for what type of outcome. Future studies would also benefit from some consensus on the type of outcomes that should be measured. Replication studies outside the US are also needed.
CONCLUSION
Low income and low health literacy are both associated with poorer health outcomes and higher rates of chronic disease. Thus, self-management represents an important healthcare strategy for these populations. This systematic review described the current use of self-management interventions in populations with low income or low health literacy and synthesized their efficacy. Overall, the current review found that effective interventions tended to focus on problem-solving and to a certain extent taking action and resource utilization. A wide range of health-related outcomes were considered, but only empowerment (or self-efficacy) and disease-specific quality of life were found to be positively affected by the interventions. Tailoring did not seem to impact on efficacy. Future high-quality trials further evaluating problem-solving in combination with taking action and resource utilization among individuals with low health literacy and/or income and replication studies outside the US are needed.
Electronic supplementary material
(DOCX 19 kb)
(DOCX 13 kb)
(DOCX 22 kb)
Acknowledgements
We wish to acknowledge Drs. Lisa Merry and Argerie Tsimicalis of McGill University for their guidance and support in the preparation of this systematic review. Preliminary results were presented in the form of an e-poster in a Graduate level class on research methods in Nursing at McGill University, and an abstract was presented (poster presentation) at the Health Literacy Annual Research Conference (HARC) in October 2016 (title: The effectiveness of tailoring self-management interventions for individuals with low health literacy or low income: A systematic review). There has been no significant financial support for this work that could have influenced its outcome. Sylvie Lambert was supported by a Canada Research Chair (Tier 2).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Contributor Information
Jamie Schaffler, Email: jamie.schaffler@mail.mcgill.ca.
Katerina Leung, Email: katerina.leung@mail.mcgill.ca.
Sarah Tremblay, Email: sarah.tremblay2@mail.mcgill.ca.
Laura Merdsoy, Email: laura.merdsoy@mail.mcgill.ca.
Eric Belzile, Email: eric.belzile@ssss.gouv.qc.ca.
Angella Lambrou, Email: Angella.lambrou@mcgill.ca.
Sylvie D. Lambert, Phone: 514-797-3762, Email: sylvie.lambert@mcgill.ca.
References
- 1.Wu S-Y, Green A. Projection of chronic illness prevalence and cost inflation. Santa Monica: RAND Health; 2000. p. 18. [Google Scholar]
- 2.Walker D, Adebajo A, Heslop P, et al. Patient education in rheumatoid arthritis: the effectiveness of the ARC booklet and the mind map. Rheumatology (Oxford) 2007;46:1593–1596. doi: 10.1093/rheumatology/kem171. [DOI] [PubMed] [Google Scholar]
- 3.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22:391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 5.Davy C, Bleasel J, Liu H, et al. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015;15:194. doi: 10.1186/s12913-015-0854-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health affairs (Milwood) 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davy C, Bleasel J, Liu H, et al. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015;15:194. doi: 10.1186/s12913-015-0854-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 9.Adams K, Greiner AC, Corrigan JM. 1st Annual Crossing the Quality Chasm Summit: A focus on communities. Washington DC: National Academies Press, 2004. [PubMed]
- 10.Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 11.Beatty L, Lambert S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev. 2013;33:609–622. doi: 10.1016/j.cpr.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Boger EJ, Demain S, Latter S. Self-management a systematic review of outcome measures adopted in self-management interventions for stroke. Disabil Rehabil. 2013;35:1415–1428. doi: 10.3109/09638288.2012.737080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dorn SD. Systematic review: self-management support interventions for irritable bowel syndrome. Aliment Pharmacol Ther. 2010;32:513–521. doi: 10.1111/j.1365-2036.2010.04374.x. [DOI] [PubMed] [Google Scholar]
- 14.Du S, Yuan C, Xiao X, et al. Self-management programs for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Patient Educ Couns. 2011;85:e299–e310. doi: 10.1016/j.pec.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 15.Plow MA, Finlayson M, Rezac M. A scoping review of self-management interventions for adults with multiple sclerosis. PM&R. 2011;3:251–262. doi: 10.1016/j.pmrj.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48:177–187. doi: 10.1016/S0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 17.Eichner J, Blumenthal D. Medicare in the 21st Century: Building a Better Chronic Care System. National Academy of Social Insurance; 2003. 10.2139/ssrn.555632.
- 18.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164:9–23. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 19.Meraviglia M, Stuifbergen A, Parsons D, Morgan S. Health promotion for cancer survivors: adaptation and implementation of an intervention. Holist Nurs Pract. 2013;27:140–147. doi: 10.1097/HNP.0b013e31828a0988. [DOI] [PubMed] [Google Scholar]
- 20.Walker D, Adebajo A, Heslop P, et al. Patient education in rheumatoid arthritis: the effectiveness of the ARC booklet and the mind map. Rheumatology. 2007;46:1593–1596. doi: 10.1093/rheumatology/kem171. [DOI] [PubMed] [Google Scholar]
- 21.Canadian Public Health Association. Ottawa Charter for Health Promotion. Can J Public Health. 1986; 77:425–430. [PubMed]
- 22.DeNavas-Walt C, Proctor BD, Smith JC. US Census Bureau, Current population reports, P60–245, income, poverty, and health insurance coverage in the United States: 2012. Washington, DC: US Government Printing Office; 2013. [Google Scholar]
- 23.Betancourt MT, Roberts KC, Bennett TL, et al. Monitoring chronic diseases in Canada: the Chronic Disease Indicator Framework. Chronic Dis Inj Can. 2014;34:1–30. [PubMed] [Google Scholar]
- 24.Dubay LC, Lebrun LA. Health, behavior, and health care disparities: disentangling the effects of income and race in the United States. Int J Health Serv. 2012;42:607–625. doi: 10.2190/HS.42.4.c. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Noncommunicable diseases. Retrieved October 2, 2015 from http://www.who.int/mediacentre/factsheets/fs355/en/
- 26.Mikkonen J, Raphael D. Social determinants of health: The Canadian facts. Toronto: York University School of Health Policy and Management. 2010. Available at http://thecanadianfacts.org/The_Canadian_Facts.pdf.
- 27.Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483). U.S. Department ofEducation. Washington, DC: National Center for Education Statistics. 2006.
- 28.Rootman I, Gordon-El-Bihbety D. A vision for a health literate Canada report of the Expert Panel on Health Literacy. Ottawa: Canadian Public Health Association; 2008. [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG. Group TP Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 30.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions version 5.0.0 [updated February 2008]. The Cochrane Collaboration. 2008. Available: http://www.cochrane-handbook.org/. Accessed 15 February 2016.
- 31.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol. 1998;66:7–18. doi: 10.1037/0022-006X.66.1.7. [DOI] [PubMed] [Google Scholar]
- 32.Blundell M. Understanding and synthesizing my numerical data. In: Boland A, Cherry MG, Dickson R, editors. Doing a systematic review—A student’s guide. Los Angeles: Sage; 2014. [Google Scholar]
- 33.Bos-Touwen I, Jonkman N, Westland H, et al. Tailoring of self-management interventions in patients with heart failure. Current Heart Failure Reports, 2015, 12(3):223-235. 10.1007/s11897-015-0259-3. [DOI] [PMC free article] [PubMed]
- 34.Cohen JH. Statistical power analysis for the behavioral sciences. 2. Hillsdale: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 35.Arora S, Peters AL, Burner E, Lam CN, Menchine M. Trial to examine text message-based mhealth in emergency department patients with diabetes (TExT-MED): A randomized controlled trial. Ann Emerg Med. 2014;63:745–754.e746. doi: 10.1016/j.annemergmed.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 36.Fischer HH, Eisert SL, Durfee MJ, et al. The impact of tailored diabetes registry report cards on measures of disease control: a nested randomized trial. BMC Med Inform Decis Mak. 2011;11:12. doi: 10.1186/1472-6947-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fischer HH, Moore SL, Ginosar D, et al. Care by cell phone: text messaging for chronic disease management. Am J Manag Care. 2012;18:e42–47. [PubMed] [Google Scholar]
- 38.Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med. 2011;171:2011–2017. doi: 10.1001/archinternmed.2011.497. [DOI] [PubMed] [Google Scholar]
- 39.Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75:336–343. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- 40.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: a randomized, controlled trial. Med Care. 2000;38:218–230. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 41.Sequeira PA, Montoya L, Ruelas V, et al. Continuous glucose monitoring pilot in low-income type 1 diabetes patients. Diabetes Technol Ther. 2013;15:855–858. doi: 10.1089/dia.2013.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thom DH, Ghorob A, Hessler D, et al. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013;11:137–144. doi: 10.1370/afm.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bove AA, Homko C, Santamore W, et al. Managing hypertension in urban underserved subjects using telemedicine: A clinical trial. J Am Coll Cardiol. 2013;1:E1401. doi: 10.1016/S0735-1097(13)61401-1. [DOI] [PubMed] [Google Scholar]
- 44.Martin MY, Kim Y, Kratt P, et al. Medication adherence among rural, low-income hypertensive adults: A randomized trial of a multimedia community-based intervention. Am J Health Promot. 2011;25:372–378. doi: 10.4278/ajhp.090123-QUAN-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bennett GG, Warner ET, Glasgow RE, et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;172:565–574. doi: 10.1001/archinternmed.2011.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krieger J, Song L, Philby M. Community health worker home visits for adults with uncontrolled asthma—the HomeBase trial randomized clinical trial. JAMA Intern Med. 2015;175:109–117. doi: 10.1001/jamainternmed.2014.6353. [DOI] [PubMed] [Google Scholar]
- 47.Riley KM, Glasgow RE, Eakin EG. Resources for health: A social-ecological intervention for supporting self-management of chronic conditions. J Health Psychol. 2001;6:693–705. doi: 10.1177/135910530100600607. [DOI] [PubMed] [Google Scholar]
- 48.Rudd RE, Blanch DC, Gall V, et al. A randomized controlled trial of an intervention to reduce low literacy barriers in inflammatory arthritis management. Patient Educ Couns. 2009;75:334–339. doi: 10.1016/j.pec.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dewalt DA, Schillinger D, Ruo B, et al. Multisite randomized trial of a single-session versus multisession literacy-sensitive self-care intervention for patients with heart failure. Circulation. 2012;125:2854–2862. doi: 10.1161/CIRCULATIONAHA.111.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.DeWalt DA, Malone RM, Bryant ME, et al. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kripalani S, Schmotzer B, Jacobson TA. Improving Medication Adherence through Graphically Enhanced Interventions in Coronary Heart Disease (IMAGE-CHD): a randomized controlled trial. J Gen Intern Med. 2012;27:1609–1617. doi: 10.1007/s11606-012-2136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kiser K, Jonas D, Warner Z, et al. A randomized controlled trial of a literacy-sensitive self-management intervention for chronic obstructive pulmonary disease patients. J Gen Intern Med. 2012;27:190–195. doi: 10.1007/s11606-011-1867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wilson FL, Mood D, Nordstrom CK, Risk J. The effect of low literacy on the self-care behaviors of men receiving radiation therapy. Nurs Sci Q. 2010;23:326–333. doi: 10.1177/0894318410380254. [DOI] [PubMed] [Google Scholar]
- 54.Cavanaugh K, Wallston KA, Gebretsadik T, et al. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009;32:2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cordasco KM, Asch SM, Bell DS, et al. A low-literacy medication education tool for safety-net hospital patients. Am J Prev Med. 2009;37:S209–S216. doi: 10.1016/j.amepre.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 56.Bosworth HB, Olsen MK, Grubber JM, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med. 2009;151:687–695. doi: 10.7326/0000605-200911170-00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gazmararian J, Jacobson KL, Pan Y, Schmotzer B, Kripalani S. Effect of a pharmacy-based health literacy intervention and patient characteristics on medication refill adherence in an urban health system. Ann Pharmacother. 2010;44:80–87. doi: 10.1345/aph.1M328. [DOI] [PubMed] [Google Scholar]
- 58.US Department of Health and Human Services . The Poverty Guidelines Updated Periodically in the Federal Register. Washington, DC: US Department of Health and Human Services; 2015. p. 42. [Google Scholar]
- 59.Darnell JS. Free clinics in the United States: a nationwide survey. Arch Intern Med. 2010;170:946–953. doi: 10.1001/archinternmed.2010.107. [DOI] [PubMed] [Google Scholar]
- 60.Battersby M, Von Korff M, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf. 2010;36:561–570. doi: 10.1016/S1553-7250(10)36084-3. [DOI] [PubMed] [Google Scholar]
- 61.Nolte S, Osborne RH. A systematic review of outcomes of chronic disease self-management interventions. Qual Life Res. 2013;22:1805–1816. doi: 10.1007/s11136-012-0302-8. [DOI] [PubMed] [Google Scholar]
- 62.Savery JR. Overview of problem-based learning: Definitions and distinctions. Interdisc J Probl-Based Learn. 2006;1:9–20. [Google Scholar]
- 63.King DK, Glasgow RE, Toobert DJ, et al. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care. 2010;33:751–753. doi: 10.2337/dc09-1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Primožič S, Avbelj M, Dernovšek MZ, Oblak MR. Specific cognitive abilities are associated with diabetes self-management behavior among patients with type 2 diabetes. Diabetes Res Clin Pract. 2012;95:48–54. doi: 10.1016/j.diabres.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 65.Auerbach JA, Krimgold BK. Income, socioeconomic status, and health: exploring the relationships. Washington DC: National Policy Association, 2001.
- 66.Glasgow RE, Fisher L, Skaff M, Mullan J, Toobert DJ. Problem solving and diabetes self-management investigation in a large, multiracial sample. Diabetes Care. 2007;30:33–37. doi: 10.2337/dc06-1390. [DOI] [PubMed] [Google Scholar]
- 67.Hill-Briggs F, Yeh H-C, Gary TL, et al. Diabetes problem-solving scale development in an adult, African American sample. Diab Educ. 2007;33:291–299. doi: 10.1177/0145721707299267. [DOI] [PubMed] [Google Scholar]
- 68.Osborne R, Elsworth G, Whitfield K. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns. 2007;66:192–201. doi: 10.1016/j.pec.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 69.Campbell MK, Quintiliani LM. Tailored interventions in public health. Where does tailoring fit in interventions to reduce health disparities? Am Behav Sci. 2006;49:1–19. [Google Scholar]
- 70.Kreuter M, Strecher V, Glassman B. One size does not fit all: The case for tailoring print materials. Ann Behav Med. 1999;21:276–283. doi: 10.1007/BF02895958. [DOI] [PubMed] [Google Scholar]
- 71.Short CE, James EL, Plotnikoff RC, Girgis A. Efficacy of tailored-print interventions to promote physical activity: a systematic review of randomised trials. Int J Behav Nutr Phys Act. 2011;8:113. doi: 10.1186/1479-5868-8-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 73.Lin ZC, Effken JA. Effects of a tailored web-based educational intervention on women’s perceptions of and intentions to obtain mammography. J Clin Nurs. 2010;19:1261–1269. doi: 10.1111/j.1365-2702.2009.03180.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19 kb)
(DOCX 13 kb)
(DOCX 22 kb)