Abstract
The Korean Breast Cancer Society (KBCS) has established a nationwide breast cancer database using an online registration program in 1996. The present study aimed to analyze the basic findings and trends of breast cancer in Korea in 2015 using the data provided by the Korea Central Cancer Registry and the KBCS. In 2015, a total of 22,550 patients were newly diagnosed with breast cancer, of which 3,331 were carcinoma in situ cases and 19,219 were invasive cancer cases. The incidence rate of breast cancer in Korea has steadily increased since the nationwide database was established, and the crude rate and age-standardized rate including that of carcinoma in situ, were 88.1 and 66.0 cases per 100,000 women, respectively. In terms of age, the incidence of breast cancer was the highest in the 40–49-year-old age group (7,889 patients, 35.0%). With regard to surgical procedure, breast-conserving surgery was frequently performed (62.3%). However, the rate of mastectomy has been gradually increasing since 2012, that is, from 32.3% in 2014 to 36.1% in 2015. The rate of early breast cancer has continued to increase, and that of stages III and IV breast cancer was only 9.1% at the time of diagnosis. However, the 5-year survival rate of patients with carcinoma in situ from 2011 to 2015 was 92.3%, which was 14.4% higher than that from 1993 to 1995 (77.9%). Analysis of data from the nationwide registry of breast cancer will not only help to understand the characteristics of breast cancer in individuals in Korea, but will also significantly contribute to the treatment and research of breast cancer. Therefore, a high quality database for breast cancer in Korea must be established by further initiating registration project and establishing an objective legal basis.
Keywords: Breast neoplasms, Epidemiology, Registries
INTRODUCTION
Cancer is the leading cause of death worldwide. In 2012, about 14 million individuals were diagnosed with cancer and 8.2 million cancer-related deaths were reported [1]. Breast cancer is the leading cause of death in women, and 520,000 individuals died from breast cancer in 2012 [1]. According to the statistics of the Korea Central Cancer Registry (KCCR), breast cancer was the second most common cancer in women after thyroid cancer, with 22,550 new cases and 2,353 deaths reported in 2015 [2].
Population aging and lifestyle westernization have led to a higher incidence of cancer and a steady increase in the incidence of breast cancer [2]. As a result, individual and social costs and burdens associated with treating cancer have been steadily increasing steadily [3]. Therefore, the current status and trends of cancer must be investigated via the establishment of a national cancer-related database to treat patients with cancer and prevent cancers.
The Korean Breast Cancer Society (KBCS) has been investigating the status of breast cancer in Korea using data from the nationwide, hospital-based breast cancer registry that was established in 1996. Unlike the national cancer registry program, it contains various clinicopathological and treatment data, including the breast cancer site, histologic type, biological markers, stage of the disease, and surgical procedure. In addition it, it provides useful information for the treatment and research of breast cancer.
The present study aimed to investigate the basic findings regarding breast cancer in Korea in 2015. Moreover the trends on the characteristics and management of breast cancer in Korea over 15 years were analyzed.
DATA COLLECTION
Data sources
Data from this study were collected from patients who were newly diagnosed with breast cancer in Korea from January 1, 2015 to December 31, 2015. The number of patients who were diagnosed with breast cancer (including those with invasive cancer and carcinoma in situ) was investigated by referring to the KCCR data. Since it was established in 1980, the KCCR has been collecting cancer-related data through the papulation-based cancer registry program since 1999, and it publishes the national cancer incidence rate, survival rate, and prevalence rate annually [4].
The patient characteristics (age, menopausal status, and surgical treatment) and disease characteristics (stage, histol-ogic type, and biological markers) were analyzed using the KBCS online breast cancer registry system (https://registry.kbcs.or.kr/ecrf/).
Statistical analysis
The incidence rate is usually presented as the crude rate (CR) and age-standardized rate (ASR), and it is generally expressed as the number of patients per 100,000 people. The CR is defined as the number of patients who were newly diagnosed with cancer in a specific population group during the study period. The ASR is a weighted average incidence rate calculated by using the rate of the standard population of each age group as weight for an equation that is used for comparison with other groups. The standard population consisted of 2,000 Koreans. Generally, the CR is mainly used to evaluate the cancer incidence of the population in terms of absolute values, and the ASR, which has been adjusted for age structure differences, is used to compare the cancer incidence rates according to region or period of time.
The annual percent change (APC) is often used to measure trends in diseases and a common estimator of this parameter uses a linear model on the log of the age-standardized rates. This is interpreted as an average annual percent change in the cancer incidence [5]. Unlike APC, the average annual percent change (AAPC) is mainly used to identify the overall change over a fixed period of time, and it is used to examine the overall trend without considering annual changes [6]. We used the Joinpoint model 4.3.1 (National Cancer Institute, Bethesda, USA) to analyze the APC and AAPC.
A linear regression analysis was carried out to evaluate the trends in each characteristic over time. Statistical analysis was performed using SPSS version 20.0 (IBM Corp., Armonk, USA), and a p-value <0.05 was considered statistically significant.
BASIC FINDINGS REGARDING BREAST CANCER IN KOREA IN 2015
Total number of patients who were newly diagnosed with breast cancer
A total of 22,550 patients were newly diagnosed with breast cancer in 2015. Among them, 19,219 (85.2%) were diagnosed with invasive cancer and 3,331 (14.8%) were diagnosed with carcinoma in situ. There were 82 male patients with breast cancer, including those with carcinoma in situ (five patients), accounting for 0.4% of the total patients with breast cancer. In addition, the overall CR of breast cancer, including carcinoma in situ, was 88.1 per 100,000 people, which ranked first among all types of cancer excluding thyroid cancer. After age standardization in terms of the population in Korea, the ASR was 66.0 per 100,000 people.
Age distribution
The KBCS and KCCR data were analyzed, and results showed that the age distribution of patients who were newly diagnosed in 2015 was similar to that of previous pattern. According to the KBCS data, the median age at the time of diagnosis was 50.0 years. Individuals as young as 15 years and those as old as 92 years presented with breast cancer. In terms of age distribution, the incidence of breast cancer was highest in the 40–49-year-old age group (3,067 cases, 34.7%), followed by the 50–59-year-old age group (2,742 cases, 31.0%). The KCCR data also showed that the incidence rate of breast cancer was highest in the 40–49-year-old age group (7,889 cases, 35.0%), and particularly, individuals aged, 45–49 years had the highest incidence rate (4,395 cases, 19.5%), followed by those aged 50–54 years (3,908 cases, 17.3%) (Table 1).
Table 1. Age distribution of newly diagnosed breast cancer patients in Korea in 2015.
| Age (yr) | KBCS registry data, no. (%) | KCCR data, no. (%) |
|---|---|---|
| < 20 | 4 ( < 0.1) | 5 ( < 0.1) |
| 20–29 | 67 (0.7) | 212 (0.9) |
| 30–39 | 798 (9.0) | 2,143 (9.5) |
| 40–49 | 3,067 (34.7) | 7,889 (35.0) |
| 50–59 | 2,742 (31.0) | 6,842 (30.3) |
| 60–69 | 1,351 (15.3) | 3,464 (15.4) |
| 70–79 | 589 (6.7) | 1,583 (7.0) |
| ≥ 80 | 94 (1.1) | 412 (1.8) |
| Unknown | 121 (1.4) | 0 |
| Total | 8,833 (100) | 22,550 (100) |
KBCS=Korean Breast Cancer Society; KCCR=Korea Central Cancer Registry.
Surgery and staging
Surgical procedure and staging at the time of diagnosis were analyzed based on the KBCS online registry data. Among the 8,833 patients who were enrolled, 5,502 (62.3%) and 3,191 (36.1%) underwent breast-conserving surgery and mastectomy, respectively (Supplementary Table 1, available online). Stage I was the most common phase (3,821 patients, 43.3%), followed by stage II (2,593 patients, 29.3%), stage 0 (1,311 patients, 14.8%), and stage III (706 patients, 8.0%). Thus, around 87.4% (7,725) of the patients were diagnosed with early breast cancer (stages 0–II) (Table 2).
Table 2. Stage distribution of newly diagnosed breast cancer patients in 2015 (KBCS registry data).
| Stage | No. of patients (%) |
|---|---|
| 0 | 1,311 (14.8) |
| I | 3,821 (43.3) |
| II | 2,593 (29.3) |
| III | 706 (8.0) |
| IV | 95 (1.1) |
| Unknown | 307 (3.5) |
| Total | 8,833 (100) |
KBCS=Korean Breast Cancer Society.
Pathology and biological markers
The histologic type of breast cancer in 7,851 patients who were enrolled was identified and invasive ductal carcinoma was the most common type (6,088 patients, 68.9%). Except for invasive ductal carcinoma, ductal carcinoma in situ and invasive lobular carcinoma were the most common types (Table 3). In the analysis of biological markers, estrogen receptor (ER) and progesterone receptor (PR) expressions were identified in 6,116 patients (73.7%) and 5,203 patients (62.7%), respectively. In the analysis that used immunohistochemical staining, the c-erbB-2 expression was examined by classifying it into negative, 1+, 2+, and 3+. It was identified in only 7,323 out of 8,833 patients, and 1,272 (17.4%) patients presented with 1+ c-erbB-2 expression, 1,751 (23.9%) with 2+ c-erbB-2 expression, and 1,344 (18.3%) with 3+ c-erbB-2 expression (Supplementary Table 2, available online).
Table 3. Histologic type of newly diagnosed breast cancer patients in 2015 (KBCS data).
| Histologic type | No. of patients (%) |
|---|---|
| Ductal carcinoma in situ | 1,164 (13.2) |
| Invasive ductal carcinoma | 6,088 (68.9) |
| Lobular carcinoma in situ | 76 (0.8) |
| Invasive lobular carcinoma | 333 (3.8) |
| Paget's disease (pure form) | 8 (< 0.1) |
| Malignant phyllodes tumor | 35 (0.4) |
| Lymphoma | 4 (< 0.1) |
| Sarcoma | 6 (< 0.1) |
| Others | 137 (1.5) |
| Unknown | 982 (11.1) |
| Total | 8,833 (100) |
KBCS=Korean Breast Cancer Society.
VARYING PATTERNS OF BREAST CANCER IN KOREA
Incidence
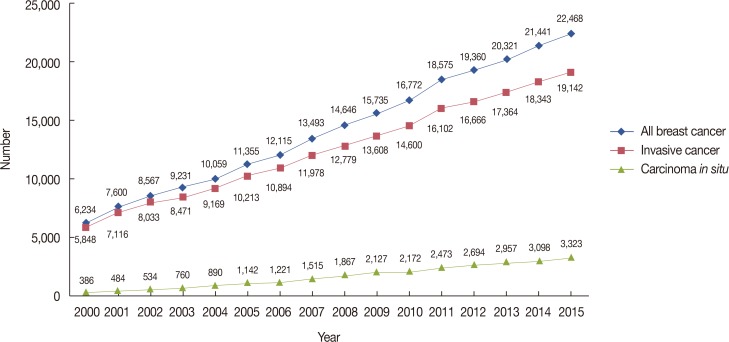
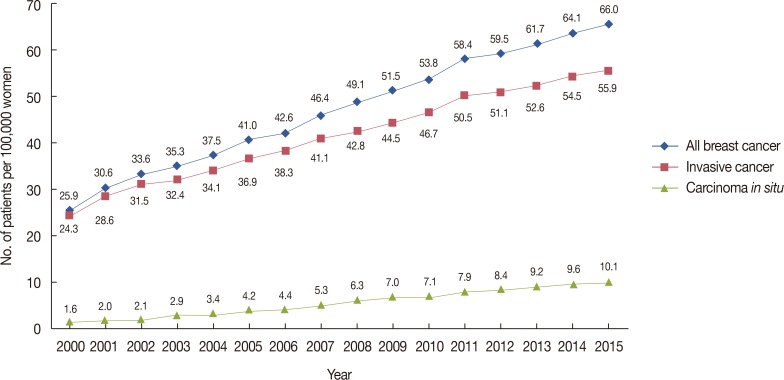
The number of newly diagnosed patients with breast cancer has been increasing annually, showing a steady increase within the last 10 years. The number of female patients who newly diagnosed with breast cancer increased from 6,234 in 2002 to 22,468 in 2015, which corresponds to a 3.6-fold increase (260.2% increase; R2=0.997, p<0.001) (Figure 1). In 2015, the CR of female patients with breast cancer, including those with carcinoma in situ was 88.1 per 100,000 people. For patients with invasive cancer, 19,142 were newly diagnosed in 2015, with a CR of 75.1/100,000 people, which is a 3.1-fold increase from 24.3/100,000 in 2000 (210.1% increase; R2=0.998, p<0.001). The CR of carcinoma in situ was 13.0/100,000 people, which is 8.1 times higher than 1.6/100,000 in 2000 (710.2% increase; R2=0.991, p<0.001). This is significantly higher than that of invasive cancer. The ASR has also increased by 2.3 times, that is, from 24.3 in 2000 to 55.9 in 2015 (130.0% increase; R2=0.945, p<0.001) (Figure 2) [7,8,9].
Figure 1. Number of newly diagnosed Korean female breast cancer patients.
Figure 2. Trends in age-standardized incidence rates of Korean female breast cancer from 2000 to 2015.
Between 1999 and 2015, the AAPC of the ASR of total breast cancer increased by 6.2%, with 5.6% and 13.3% increase in invasive cancer and carcinoma in situ cases, respectively (Table 4).
Table 4. Trends in age-standardized incidence rates for breast cancer according to joinpoint analysis (1999–2015).
| AAPC 1999–2015 | Trend 1 | Trend 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | APC | 95% CI | Period | APC | 95% CI | ||||
| Lower | Higher | Lower | Higher | ||||||
| All breast cancer | +6.2* | 1999–2007 | +7.9* | 6.9 | 8.9 | 2007–2015 | +4.5* | 3.5 | 5.5 |
| Invasive breast cancer | +5.6* | 1999–2005 | +7.7* | 6.0 | 9.4 | 2005–2015 | +4.4* | 3.6 | 5.1 |
| Carcinoma in situ | +13.3* | 1999–2008 | +18.6* | 17.0 | 20.2 | 2008–2015 | +6.9* | 4.8 | 9.0 |
9.0AAPC=average annual percentage change (%); APC=annual percent change (%); CI=confidence interval.
*The APC or AAPC is a significantly different from zero (p<0.05).
Median age and menopausal state upon diagnosis
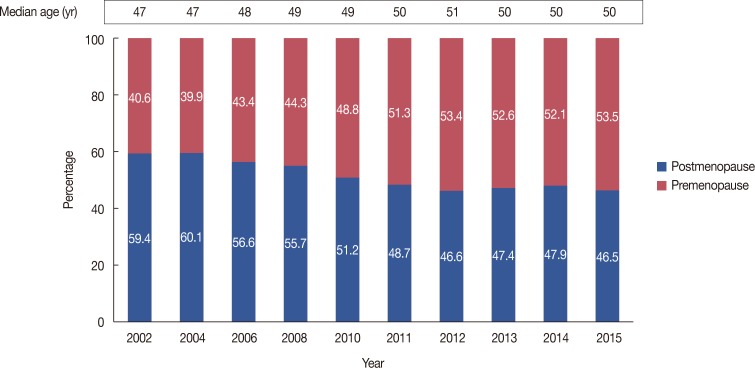
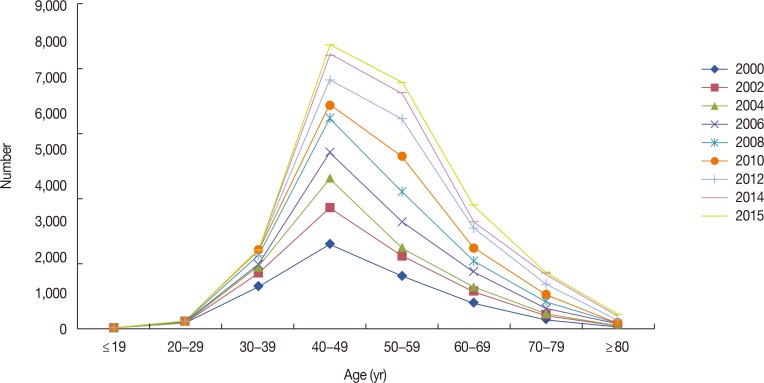
Based on the KBCS registry data, we analyzed the ages of patients with breast cancer who were newly diagnosed between 2000 and 2015. The median age of the patients who were diagnosed with breast cancer in 2015 is 50 years, showing a steady increase from the median age of 47 years in 2002. The proportion of postmenopausal women was 40.6% in 2002. However, it continued to increase, reaching approximately 53.5% in 2015, which is the highest proportion in history (36.4% increase; R2=0.924, p<0.001) (Figure 3). In contrast to the increase in the median age of patients with breast cancer and that of the proportion of postmenopausal women, the age distribution pattern was similar to that of previous studies (Figure 4).
Figure 3. Trends in the median age at breast cancer diagnosis in Korea and the ratio of postmenopausal to premenopausal women at diagnosis.
Figure 4. Trends in age distribution pattern of Korean female breast cancer from 2000 to 2015.
Biologic markers and stage distribution
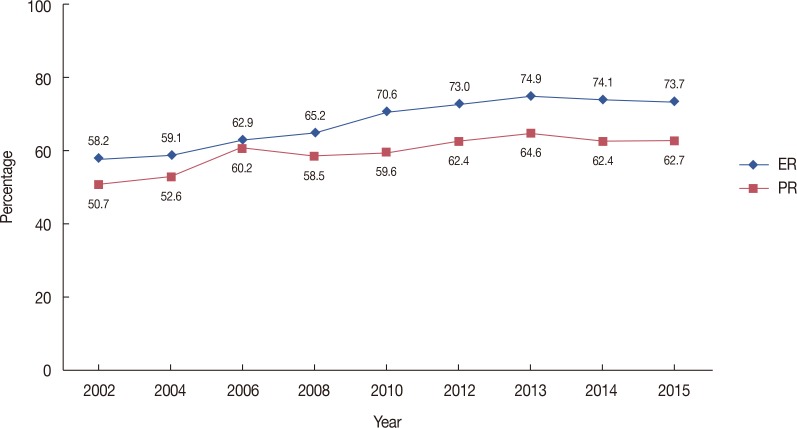
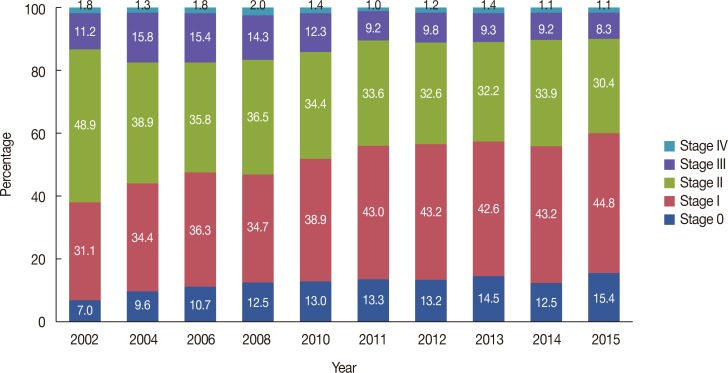
Hormone receptor positive (ER or PR positive) breast cancer has been steadily increasing since 2002, and this trend is observed in patients with both ER- and PR-positive breast cancer. The proportion of ER-positive breast cancers increased from 58.2% in 2002 to 73.7% in 2015 (26.6% increase; R2=0.995, p<0.001), and the incidence rate of PR-positive breast cancer increased from 50.7% in 2002 to 62.7% in 2015 (23.7% increase; R2=0.824, p<0.001) (Figure 5). The analysis of breast cancer stage from 2002 onwards showed that the proportions of stages 0 and I cancer were continuously increasing; specifically, the rates of stages 0 and I cancer increased from 7.0% to 31.1% in 2002 and from 14.8% (111.4% increase; R2=0.847, p<0.001) to 43.3% (25.8% increase; R2=0.894, p<0.001) in 2015, respectively. During the same period, the rate of stage II–IV cancer significantly decreased from 61.9% to 38.4% (38.0% decrease; R2=0.948, p<0.001) (Figure 6).
Figure 5. Changes in the hormone receptor-positive breast cancer.
ER=estrogen receptor; PR=progesterone receptor.
Figure 6. Changes in the stage distribution of Korean breast cancer.
Surgical patterns
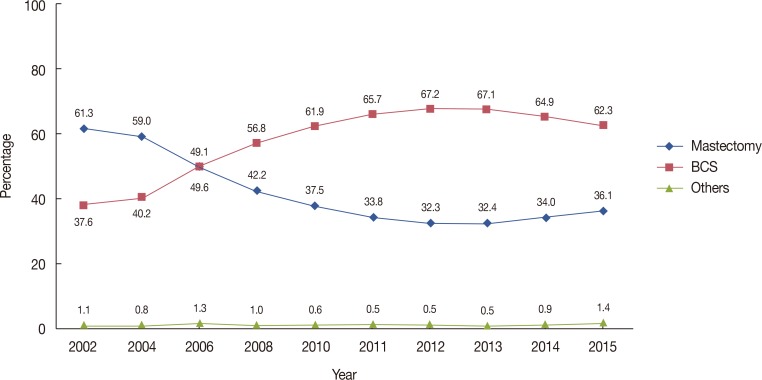
In 2002, mastectomy was the most common surgical method performed in 61.3% of the patients. However, the rate gradually decreased to 32.3% in 2012 (47.3% decrease; R2=0.984, p<0.001). Then, it slightly increased, and in 2015, mastectomy was performed in 36.1% of the patients (11.8% increase; R2=0.893, p=0.006). The rate of breast-conserving surgery was 37.6% in 2002. It gradually increased to 67.2% in 2012 (78.2% increase; R2=0.893, p<0.001) but, slightly decreased to 62.3% in 2015 (7.6% decrease; R2=0.858, p=0.005) (Figure 7).
Figure 7. Changes in the surgical management of breast cancer.
BCS=breast-conserving surgery.
Five-year and 10-year relative survival rates
Based on the KCCR data, the 5-year survival rate of patients who were diagnosed with breast cancer between 1993 and 1995 was 77.9%, and the survival rate continued to increase to 92.3% in patients with breast cancer who were diagnosed from 2011 to 2015, which is 14.4% higher than that of patients with breast cancer who were diagnosed between 1993 and 1995 [2]. The survival rate of patients with breast cancer who were diagnosed from 2006 to 2010 was 86.6%, which was 14.9% higher than that of patients (71.7%) with breast cancer who were diagnosed from 1993 to 1995.
DISCUSSION
According to the KCCR data in 2015, the ASR of all types of cancer increased by 3.6% on average from 1999 (when cancer statistics were first compiled) to 2012. Meanwhile, the incidence rate of cancer has been decreasing annually by 6.1% on average since 2012. Particularly, the incidence rates of the major types of cancer, such as gastric cancer, colorectal cancer, and lung cancer, have significantly decreasing trend since 2012 [2]. However, the rate of breast cancer had been increasing by 7.9% annually from 1999 to 2007 and by 4.5% annually from 2007 to 2015. The ASR of breast cancer (invasive cancer) in Korea in 2015 is 55.9/100,000 people, which is a sharp increase from 24.3/100,000 people in 2000, and Korea is one of the countries with a rapidly increasing rate worldwide [10].
As shown in Figure 1, the number of patients diagnosed with breast cancer in Korea has been steadily increasing since 2000. Based on previous studies, this may be a result of lifestyle westernization [11]. In fact, the incidence of breast cancer has been increasing in several Asian countries, particularly in countries with fast-growing economies [11]. However, in western countries, the incidence of breast cancer continues to increase as well, which is a result of longer life expectancy and changes in the reproductive pattern such as delayed childbearing and women having fewer children [12]. In addition, the widespread use of screening tests is associated with an increase in the incidence, and the increase in the incidence rate of breast cancer in Korea may have been caused by a combination of these factors. In particular, the CR of carcinoma in situ increased by 8.1 times, that is, from 1.6/100,000 people in 2000 to 13.0/100,000 people in 2015, which is a significant increase compared with approximately 3-fold increase in the rate of invasive cancer. This rapid increase is may be due to the widespread use of screening mammography [13].
The median age of patients with breast cancer who were diagnosed in 2015 was 50 years, was higher than that in patients (47 years) diagnosed in 2002, but significantly lower than that in patients (62 years) diagnosed in 2014 in the United States [14]. Meanwhile, the proportion of individuals aged 40–49 years who were diagnosed with breast cancer was the highest. In Korea, the incidence rate of breast cancer is highest in the 40–49-year-old age group, which has not changed since 2000. The age range of individuals with the highest incident rate in Korea differs by more than 10 years from that of individuals in the United States, where the incidence rate of breast cancer is highest in individuals aged 55–64 years [14]. In Japan, majority of breast cancer cases involved individuals in the 50–59-year-old age group [15], and in China, most breast cancer cases included patients in the 55-59-year-old age group. Meanwhile, patients with breast cancer in Korea were diagnosed at younger ages [16]. The reason for these differences has not yet fully elucidated. However, an analysis that includes a cohort with an internationally standardized age range must be conducted to minimize bias. In 2002, the proportion of postmenopausal women was only 40.6%. Then, the rate continued to increase, accounting for 53.5% of breast cancer patients diagnosed in 2015. However, among patients with breast cancer, the rate of postmenopausal women is still significantly lower in Korea than in Western countries. Therefore, in Korea, health care services in terms of childbearing, such as those for pregnancy and childbirth, as well as screening tests and treatments of breast cancer need different approaches from those used in Western countries.
Since 2002, the rate of hormone receptor-positive breast cancer has been increasing. This phenomenon is also observed in Western countries. However, hormone receptor-positive breast cancer has a good prognosis, which may have an impact on the increase in the survival rate of patients with breast cancer [12]. The cause of the increased proportion of hormone receptor-positive breast cancer is not yet known. In some studies, this phenomenon is attributed to the fact that the cutoff value for immunohistochemical staining has been lowered from 10% to 1% based on the previous criteria for ER and PR positivity [17,18]. However, in countries where the cutoff value has been constant, the rate of hormone receptor positive breast cancer is still increasing, making the analysis not likely valid [19]. Recent studies have suggested that an increase in the obese population and changes in the reproductive pattern are associated with the increase in the incidence of hormone receptor-positive breast cancer [20,21].
The trend of surgical procedures has been steadily changing. In 2002, the rate of breast-conserving surgery was only 37.6%. However, it has steadily increased since then, reaching 67.2% in 2012. This is due to the fact that screening tests are widely used and neoadjuvant therapy has been expanded. Interestingly, after 2012, the rate of breast-conserving surgery did not steadily increase but slightly decreased, reaching 62.3% in 2015 [9]. In contrast, the rate of mastectomy steadily decreased from 61.3% in 2002 to 32.3% in 2012, and then slightly increased to 36.1% in 2015 [9]. Although there are differences depending on the time of the survey, this phenomenon is commonly observed in several countries such as the United States and Japan. This is a result of the widespread use of preoperative magnetic resonance imaging and genetic tests in patients with breast cancer and the active reflection of patient opinion (the fear of recurrence and expectation of improvement in the survival rate) regarding the decision on the surgical procedure. In addition, it may also be the result of an increase in contralateral prophylactic mastectomy due to changes in the perception of plastic surgery [22,23,24,25,26]. According to Mahmood et al. [27], the proportion of mastectomy in the United States is highest in the 20–39-year-old age group (49.5%) and lowest in the 60–69-year-old age group (34.4%). On the other hand, in Korea, the rate of mastectomy is 38.0% in the 20–39-year-old age group and highest in the 70–79-year-old age group (52.0%). This contrast indicates that the important factors in determining the appropriate surgical procedure include not only the aspects of the disease but also the difference in perception and culture [27].
With an increasing interest in breast cancer and the development of diagnostic techniques, the proportion of early breast cancer has steadily increased, with stage 0, I, and II accounting for 14.8%, 43.3%, and 29.3%, of the cases in 2015, respectively. In terms of the rates of stage 0, I, and II breast cancer (7%, 31.1%, and 48.9%, respectively) in 2002, the proportions of stage 0 and I have been continuously increasing. Considering that the screening rate with recommendation increased from 33.2% in 2004 to 59.7% in 2013, the increase in breast cancer screening is thought to have contributed to the increase in early breast cancer [28].
Based in the KCCR data, it was confirmed that the survival rate of breast cancer has been continuously improving in Korea. The 5-year survival rate of invasive cancer increased from 77.9% from 1993 to 1995 to 92.3% from 2011 to 2015 [2]. According to the U.S. Surveillance, Epidemiology, and End Results data, the survival rate of patients with breast cancer gradually increased from 85.2% between 1990 and 1992 to 91.3% between 2007 and 2013 [29]. In addition to the development of treatment methods such as target therapy, the increase in the proportion of early breast cancer due to the widespread practice of health screening is considered as the primary reason for such an increase in the survival rate. This analysis is based on the fact that the survival rate in the United States is higher in the states where breast screening is well performed than in those where it is not well performed [30].
Since the number of cancer survivors is increasing due to a continuous increase in the cancer survival rate, studies on cancer survivors are becoming increasingly important in terms of socioeconomic costs and the improvement of the quality of life. According to KCCR data on January 1, 2016, 1.61 million patients with cancer survived, and thyroid cancer was the most common in both men and women (355,057 patients, 22.0%). The survivors of stomach cancer were most likely men (17,194 patients, 24.1%), and those of breast cancer were most likely women (179,081 patients, 19.7%) [2]. Since there is a growing social interest in the increasing number of the survivors of cancer, proper management is important. To initiate a systemic nationwide cancer research at a period when management and research for patients with cancer is important, it is necessary to continuously strengthen the cancer management infrastructure by establishing legal policies as well as developing a geographic information system for patients with cancer and national cancer databases in the future.
CONCLUSION
The incidence rate of breast cancer has been gradually increasing, whereas the incidence rates of other major types of cancer in Korea have been declining in recent years. The rates of early breast cancer and hormone receptor-positive breast cancer are increasing along with the incidence rate, and the rate of mastectomy also gradually increases. Since the survival rate of patients with cancer continues to increase, the number of cancer survivors, including breast cancer survivors, is increasing, and thus, the efficient management of cancer survivors is essential. An analysis that uses data from nationwide registry for breast cancer will not only contribute to the understanding of the characteristics of breast cancer in Korea, but will also be extremely useful for future treatment for and studies on breast cancer.
ACKNOWLEDGMENTS
We thank all members of the KBCS who participated in KBCS online registry.
Footnotes
CONFLICT OF INTEREST: The authors declare that they have no competing interests.
SUPPLEMENTARY MATERIALS
Surgical management of newly diagnosed breast cancer patients in 2015 (KBCS registry data)
Biologic markers of newly diagnosed breast cancer patients in 2015 (KBCS data)
References
- 1.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC CancerBase No. 11. International Agency for Research on Cancer; [Accessed February 13th, 2018]. http://globocan.iarc.fr. [Google Scholar]
- 2.National Cancer Information Center; Ministry of Health and Welfare. Cancer statistics. [Accessed February 13th, 2018]. https://www.cancer.go.kr/
- 3.Lee KS, Chang HS, Lee SM, Park EC. Economic burden of cancer in Korea during 2000-2010. Cancer Res Treat. 2015;47:387–398. doi: 10.4143/crt.2014.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999~2001: first result using the national cancer incidence database. Cancer Res Treat. 2005;37:325–331. doi: 10.4143/crt.2005.37.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fay MP, Tiwari RC, Feuer EJ, Zou Z. Estimating average annual percent change for disease rates without assuming constant change. Biometrics. 2006;62:847–854. doi: 10.1111/j.1541-0420.2006.00528.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim HJ, Luo J, Chen HS, Green D, Buckman D, Byrne J, et al. Improved confidence interval for average annual percent change in trend analysis. Stat Med. 2017;36:3059–3074. doi: 10.1002/sim.7344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim Z, Min SY, Yoon CS, Jung KW, Ko BS, Kang E, et al. The basic facts of Korean breast cancer in 2012: results from a nationwide survey and breast cancer registry database. J Breast Cancer. 2015;18:103–111. doi: 10.4048/jbc.2015.18.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2016;19:1–7. doi: 10.4048/jbc.2016.19.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park EH, Min SY, Kim Z, Yoon CS, Jung KW, Nam SJ, et al. Basic facts of breast cancer in Korea in 2014: the 10-year overall survival progress. J Breast Cancer. 2017;20:1–11. doi: 10.4048/jbc.2017.20.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. 2013. Lyon: International Agency for Research on Cancer; 2014. [Google Scholar]
- 11.Bhatia H. Breast cancer in Asia. Gen Re; [Accessed February 4th, 2018]. http://www.genre.com/knowledge/publications/ri16-4-en.html. [Google Scholar]
- 12.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64:52–62. doi: 10.3322/caac.21203. [DOI] [PubMed] [Google Scholar]
- 13.Ernster VL, Ballard-Barbash R, Barlow WE, Zheng Y, Weaver DL, Cutter G, et al. Detection of ductal carcinoma in situ in women undergoing screening mammography. J Natl Cancer Inst. 2002;94:1546–1554. doi: 10.1093/jnci/94.20.1546. [DOI] [PubMed] [Google Scholar]
- 14.National Cancer Institute. Cancer stat facts: female breast cancer. [Accessed February 4th, 2018]. https://seer.cancer.gov/statfacts/html/breast.html.
- 15.Saika K, Sobue T. Epidemiology of breast cancer in Japan and the US. Japan Med Assoc J. 2009;52:39–44. [Google Scholar]
- 16.Zeng H, Zheng R, Zhang S, Zou X, Chen W. Female breast cancer statistics of 2010 in China: estimates based on data from 145 population-based cancer registries. J Thorac Dis. 2014;6:466–470. doi: 10.3978/j.issn.2072-1439.2014.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeSantis C, Howlader N, Cronin KA, Jemal A. Breast cancer incidence rates in U.S. women are no longer declining. Cancer Epidemiol Biomarkers Prev. 2011;20:733–739. doi: 10.1158/1055-9965.EPI-11-0061. [DOI] [PubMed] [Google Scholar]
- 18.Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version) Arch Pathol Lab Med. 2010;134:e48–e72. doi: 10.5858/134.7.e48. [DOI] [PubMed] [Google Scholar]
- 19.Anderson WF, Rosenberg PS, Petito L, Katki HA, Ejlertsen B, Ewertz M, et al. Divergent estrogen receptor-positive and -negative breast cancer trends and etiologic heterogeneity in Denmark. Int J Cancer. 2013;133:2201–2206. doi: 10.1002/ijc.28222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL, et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst. 2011;103:250–263. doi: 10.1093/jnci/djq526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colditz GA, Rosner BA, Chen WY, Holmes MD, Hankinson SE. Risk factors for breast cancer according to estrogen and progesterone receptor status. J Natl Cancer Inst. 2004;96:218–228. doi: 10.1093/jnci/djh025. [DOI] [PubMed] [Google Scholar]
- 22.Fancellu A. Considerations arising from requests from patients for a bilateral mastectomy who are eligible for breast-conserving surgery: factors weighing for and against performing the operation. Oncol Lett. 2016;12:764–766. doi: 10.3892/ol.2016.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xia C, Schroeder MC, Weigel RJ, Sugg SL, Thomas A. Rate of contralateral prophylactic mastectomy is influenced by preoperative MRI recommendations. Ann Surg Oncol. 2014;21:4133–4138. doi: 10.1245/s10434-014-3852-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heil J, Rauch G, Szabo AZ, Garcia-Etienne CA, Golatta M, Domschke C, et al. Breast cancer mastectomy trends between 2006 and 2010: association with magnetic resonance imaging, immediate breast reconstruction, and hospital volume. Ann Surg Oncol. 2013;20:3839–3846. doi: 10.1245/s10434-013-3097-0. [DOI] [PubMed] [Google Scholar]
- 25.Miller BT, Abbott AM, Tuttle TM. The influence of preoperative MRI on breast cancer treatment. Ann Surg Oncol. 2012;19:536–540. doi: 10.1245/s10434-011-1932-8. [DOI] [PubMed] [Google Scholar]
- 26.Fisher CS, Martin-Dunlap T, Ruppel MB, Gao F, Atkins J, Margenthaler JA. Fear of recurrence and perceived survival benefit are primary motivators for choosing mastectomy over breast-conservation therapy regardless of age. Ann Surg Oncol. 2012;19:3246–3250. doi: 10.1245/s10434-012-2525-x. [DOI] [PubMed] [Google Scholar]
- 27.Mahmood U, Hanlon AL, Koshy M, Buras R, Chumsri S, Tkaczuk KH, et al. Increasing national mastectomy rates for the treatment of early stage breast cancer. Ann Surg Oncol. 2013;20:1436–1443. doi: 10.1245/s10434-012-2732-5. [DOI] [PubMed] [Google Scholar]
- 28.Lee EA, Shin J, Hwang EJ, Lee JW. Breast and cervical cancer screening behavior in female cancer survivors: the Korea National Health and Nutrition Examination Survey, 2007-2012. Korean J Fam Med. 2017;38:116–121. doi: 10.4082/kjfm.2017.38.3.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Cancer Institute. Surveillance, Epidemiology, and End Results Program. [Accessed February 2nd, 2018]. https://surveillance.cancer.gov/joinpoint/help.html.
- 30.DeSantis CE, Ma J, Goding Sauer, A, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017;67:439–448. doi: 10.3322/caac.21412. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical management of newly diagnosed breast cancer patients in 2015 (KBCS registry data)
Biologic markers of newly diagnosed breast cancer patients in 2015 (KBCS data)