Abstract
In the last decade, the humanization of medicine has contributed to an important shift in medical paradigms (from a doctor-centered to a patient-centered approach to care). This paradigm shift promoted a greater acknowledgement of patient engagement as a crucial asset for healthcare due to its benefits on both clinical outcomes and healthcare sustainability. Particularly, patient engagement should be considered a vital parameter for the healthcare system as well as it is a marker of the patients’ ability to be resilient to the illness experience and thus to be an effective manager of his/her own health after the diagnosis. For this reason, measuring and promoting patient engagement both in chronic and acute care is today a priority for healthcare systems all over the world. In this contribution, the authors propose the Patient Health Engagement (PHE) model and the PHE scale as scientific and reliable tools to orient clinical actions and organizational strategies based on the patient engagement score. Particularly, this work discusses the implication of the adoption of these scientific tools in the enhanced recovery after surgery (ERAS) experience and their potentialities for healthcare professionals working in thoracic surgery settings.
Keywords: Patient engagement, Patient Health Engagement model (PHE model), Patient Health Engagement scale (PHE-s), patient-doctor relationship, resilience
Citizens’ expectations towards the healthcare system are changing in both quantitative and qualitative terms (1,2). Life expectancy has increased, thanks to continuous technical and medical advancements. Diseases once lethal and deeply impacting on patient’s quality of life became curable or, at least, treatable. These issues translate into an increased demand for care and cure services, often over a longer period. Furthermore, thanks to the diffusion of new means of communication (with particular reference to the Internet) we assist to a more equitable access to health information sources (3,4): this contributes to enhance people knowledge about their health condition and the available options for its treatment and their willingness to be engaged in choices related to their health course. Today people know more about their health but ask to know even more: the phenomenon of expert patient is an example of this increasing desire to acquire health information in an effective way (5). Moreover, they expect to be up-dated about the continuous advances of medical research. As a consequence, patients today claim for an enhanced participation along their healthcare journey, in terms of ability not only to express their health priorities, but also to advocate for a better alignment of the healthcare system to their psychological experience and needs (6).
In the last decade, the humanization movement in medicine has contributed to an important shift in medical paradigms (7,8). From an exclusive focus on the organic components of the disease (i.e., “doctor-centered model of care”) medicine opened to a broader consideration of also the psychosocial components of the illness experience lived by the patient (i.e., “patient-centered model of care”) (9). This paradigm shift promoted a greater acknowledgement of the potential impact of the patients’ lifestyles and attitudes on their therapeutic adherence and thus on the clinical effectiveness of the medical intervention (10). The active role of the patient in his/her healthcare management became more and more a crucial focus for healthcare providers and a goal for therapeutic education (11). Therefore, we are assisting to an enhanced commitment of the healthcare system in sustaining patients and their family health literacy and in equipping them of the needed skills for effective self-management (12,13). The idea is that providing information to patients and increasing their literacy and self-management skills would improve patients’ motivation to be more active and participative in the medical encounter and in the care process.
Several studies, to date, have demonstrated how the increased participation of patients in their healthcare is an important factor affecting medical adherence (14-16) patients’ satisfaction about their healthcare experience and patients’ psychological wellbeing (17-20). Furthermore, studies demonstrated how the enhanced participation of patients in their healthcare improves the quality of medical relationship, also contributing to reduce medical errors and improve safety of medical action (6,21,22).
Along this direction, there is increased acknowledgment about the importance of including patients’ values and preferences in a shared decision-making process about treatments options. Behind this assumption there is the idea that the medical treatment will be higher effective if aligned with the patients’ subjective priorities in terms of values and of quality of life expectations. This implies a change in the dynamics and philosophy of the medical encounter, towards a more open and reciprocal relationship: this means to recognize that both practitioners and patients are experts (the first one of the technical aspects of the care process and the second one of the subjective impact that the disease has on their life and of the criteria that lead them in positively or negatively evaluating their care experience) called to share their knowledge and experience in order to make the care process really aligned with the patients priorities and expectations (23-26).
However, medical information can be unfamiliar, difficult to be decoded and emotionally overwhelming for patients, particularly when they are experiencing critical moments in their healthcare pathway (such as the diagnosis moment, the occurrence of relapse, the decision to undergo a surgery…).
Critical health conditions, such as those typically linked to thoracic surgery, deeply impact on patients’ emotional wellbeing and on their resilience ability (27,28). The diagnosis often is lived like a “bolt from the blue”, even more critical at the psychological level when it is followed by the proposal to undergo a surgery. Furthermore, often in the case of thoracic surgery, patients come to the diagnosis without a real awareness of the gravity of their health condition due to the little visibility of signs and symptoms of the disease. Time after the diagnosis goes fast from patients’ perspective. Patients describe the time after the diagnosis as an overwhelming sequence of duties and of emotionally burdening choices that they have to take in relation to their disease treatment. Patients and their families try to cope at their best with these various duties, although very often they feel not adequately equipped at the informative and emotional level. The option of a thoracic surgery is one of the most difficult and emotionally burdening among those requirements (29-31).
Given the specificities of thoracic surgery patients’ psychological experience, it is key to guarantee the full alignment of the therapeutic team (and the whole healthcare organization) to patients and family psychological needs and expectations. Patients awareness and conscious participation to the decisions on treatment procedures is fundamental, not only in order to guarantee their informed consent, but to provide a protected and scaffolding relational space where patients and healthcare professional may feel real partners of a common health endeavor. In other term, to sustain patients’ engagement in shared decision making and in the care relationship is a crucial predictor of the quality of patients’ psychological and medical experience (32-36).
The concept of engagement is established in the scope of long-term treatment of chronic patients, particularly where integrated care models are concerned. Less attention has been paid so far to the application of patient engagement measures in the hospital setting and in particular in acute care. Experience of patient’s engagement assessment and promotion in the specific setting of surgery, moreover, are just a few (15,37,38). However, given the previous premises, the setting of surgery appears particularly relevant and challenging for the promotion of patient engagement. At the organizational level, the hospital is the setting that often corresponds with the first enrollment of a patient in the healthcare pathway. This first moment is crucial in order to set the base for the effective education of the patient and his/her family and for the construction of a good partnership not only with the doctor and the healthcare professional team, but also with the whole healthcare system. In this phase, specific actions need to be planned in order to foster patients’ and family literacy about disease and treatment but also to sustain a process of psychological resilience to effectively face the post-acute care process. This is indeed a necessary condition to make patient engagement in healthcare a reality.
In other words, surgeons and their team are required to deal with the need of engaging their patients from the very beginning of their care relationship. This is the priority condition to guarantee patients’ ability to engage also after discharge and in the follow up phases of their care pathway.
To focus of early patient engagement is particularly crucial in the scenario of new organizational models of patients’ management in thoracic surgery such as enhanced recovery after surgery (ERAS) (39,40): this approach is finalized to improve the post-surgical period with a faster and more effective clinical recovery and the reduction of hospitalization.
Minimally invasive thoracic surgery is a cornerstone of ERAS: many review and different meta-analysis in the past years has demonstrate the improvement in surgical outcome in terms of duration of hospitalization, reduction of complication and pain both in the comparison of video-assisted thoracoscopic surgery (VATS) surgery vs. open surgery (41).
The Italian VATS Group has developed a project called “ERAS and Fast Track in VATS Lobectomy” that incorporates the individual aspects of this work, with the aim of obtaining an ERAS protocol for thoracic surgery that is complete, easily to apply, and fit for today’s healthcare environment. The Italian VATS Group has a fundamental enrolment tool, the VATS Registry, in which all VATS lobectomies carried out by accredited Italian centers are recorded; to date, more than 5,000 cases have been included. In addition to this and for the purpose of the aforementioned ERAS project, a dedicated and prospective ERAS Registry was created to validate specific ERAS indicators for minimally invasive thoracic surgery.
The ERAS model drives to consider patients like co-protagonist of their care journey and crucial allied of the healthcare professional team to gain effective clinical outcomes. The engagement of patients, indeed, is a key factor to sustain the effectiveness of the clinical act and to guarantee patients adherence to therapeutic and life-styles prescription in the follow-up. However, the ability of patients to become co-protagonists of their clinical course is function of dedicated initiatives to inform and educate them. Furthermore, it depends on the quality of patient-doctor relationship: to be engaged, patients need a healthcare team able to recognize their illness experience in terms of emotional burden, willingness to be active participants in the healthcare process and oriented to motivate and reassure them.
In other words, surgeons as well as all the professionals involved in the surgical team, need to be sensitized and trained to an actual cultural change in thoracic surgery approach to the patients’ care, finalized to a more aware promotion of patient engagement along the whole care pathway.
Monitoring and mirroring patient engagement: a goal of ERAS
If patient engagement in ERAS becomes a goal, it is important to equip healthcare systems and professionals with scientific measures to evaluate, monitor and promote the levels of patient’s participation in their care.
The recently concluded Consensus Conference for Patient Engagement (42) advocated for a more systematic approach in patient engagement assessment within the healthcare system. The adoption of scientific measures of patient engagement, thus, is important according to different considerations. First, in a scenario of value-based healthcare, to insure strategies for giving voice to patients’ and their caregivers about their needs and priorities is crucial (43). This may allow clinicians to best orient communicative and educational initiatives to the specific expectations of their patients (44). Systematically measure patient engagement levels, furthermore, may help clinicians become better empathetic to patients’ experiences and psychological burden related to the disease and its treatment. However, this should be achieved with the support of scientifically validates measures, and should not only relay on the clinicians’ subjective evaluation based on their professional experience. Furthermore, the adoption of validated measurement to assess patient engagement is a way to insure the best personalization of educational initiatives and relational acts. These interventions should be personalized according to the specific position of the patients along their engagement journey (8,36,45). Not all patients, and not in all stage of their healthcare experience, indeed, are able and willing to really assume a proactive position in their healthcare management. A democratic and ethical perspective about patient engagement promotion, particularly in the ERAS setting, should move from this awareness in order to be maximally respectful of patients’ values and priorities. Finally, the adoption of reliable measures for patient engagement in ERAS would allow to evaluate the effectiveness of educational initiative in promoting patients’ participation, by providing useful feedback to optimize them and to guarantee their effectiveness and sustainability in time.
The Patient Health Engagement (PHE) model: mirroring patients’ engagement and psychological recovery
The debate about patient engagement and about the importance of assess the level of patients’ participation along their healthcare journey is florid and increasing year-by-year. Several tentative exist in the scientific literature to define engagement and its process of development. Among the most established definition of engagement, Légaré and colleagues (46) describe engagement as related to the patients’ level of knowledge and literacy about their health status and their medical prescriptions. Their definition, thus, mainly consider the cognitive and informative dimensions of the engagement experience. According to these authors, the essence of engagement consists in the patients’ ability to search for health information, to decode such information and to use them. Gruman and colleagues (47), mainly focused on the behavioural components of patient engagement and on the level of patients’ ability enact effective self-care behaviours. These behavioural indicators are considered by these authors such an indicator of patients’ ability to self-determinate their health status, and thus, of them being well engaged in their care. Hibbard and colleagues (48) developed the patient activation theory (and its related measurement PAM-13) and they underlined that the level of patient engagement depends on the level of patients’ perception of self-efficacy and on their confidence on their own knowledge and ability to participate in the care process. These definitions, although substantial, do not capture and describe the emotional and psychodynamic component of the engagement experience, although scholars agree on the role of patients’ emotional and psychological resilience in hindering or sustaining patients’ participation in healthcare (8,11,27,49,50).
This appears as a potential limit when patient engagement has to be applied in the setting of critical or acute care. As mentioned above, critical health conditions, the ERAS environment and the long recovery from surgery present unique challenges for patient engagement. Patients’ participation in shared decision making and in the crucial points of treatment may be particularly burdensome for patients and their caregiver due to the acute psychological stress and the risk of death. Recently, some scholars emphasize that, at the contrary from chronic care management, in acute and in post-intensive care the physiological outcomes of the intervention may depend on the levels of patient and family engagement, such as function of patients’ psychological resilience and sense of ownership of recovery (51). They thus claim for a revision of definition of patient engagement currently adopted in chronic care management in order to highlight the role of emotions and of psychological resilience to the health condition in such a process.
The component of psychological resilience and of identity reconfiguration along the process of engagement is the key element of the PHE model developed by Graffigna and colleagues (52). This model of patient engagement, rooted in the tradition of health psychology, describes engagement as the result of a complex process of psychological adaptation to illness and to the impact of this on the patients’ self-image. The possibility for a patient to assume a proactive and participative position in healthcare, indeed, is featured by this model as the result of a complex dynamics among cognitive, emotional and behavioral components of the illness experience. The evolution along this “journey of engagement” is function of the balanced activation of such experiential components and in particular of patients’ ability to self-determinate as an “author” of his/her healthcare course and of requiring a sense of ownership on his/her disease trajectory and quality of life (20). This model has been developed on the basis of extensive qualitative and quantitative studies of illness stories across different disease conditions and age cohorts and showed applicability in a broad spectrum of acute and chronic settings.
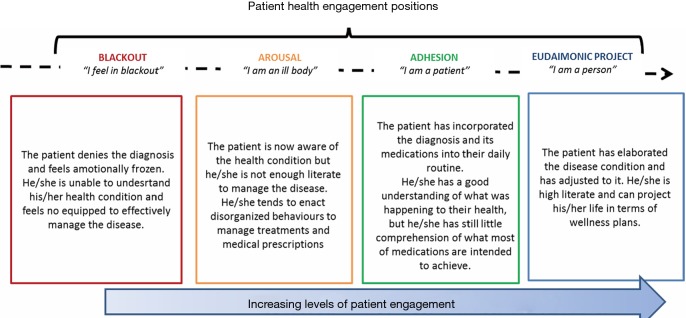
The PHE model features four positions of patient engagement, as described below (see Figure 1).
Figure 1.
The PHE model. PHE, Patient Health Engagement.
Blackout
The occurrence of a critical episode (e.g., a new diagnosis, the worsening of a disease condition, a disease relapse, etc.) leaves patients in a state of emotional, behavioral, and cognitive blindness. Patients in this position perceive a sense of lost control over the disease and their life. They feel “in suspension”, and report state of anxiety. In this position of their engagement journey, the disease onset and its management are lived as overwhelming and unacceptable. At this stage, patients do not have yet acquired effective coping strategies to manage their new health condition, and they feel confuse about the changes occurring in their health status and in their body. Furthermore, patients in this position ten to have poor literacy about their health conditions, and they cannot easily elaborate the received information about their health condition (cognitive blindness). Moreover, patients feel blocked and unable to enable self-management actions (behavioral freezing). Patients in this stage, due to the disruptive emotive burden caused by the disease, appear completely focused on their illness, by scarifying other interests or activities. These patients are passive toward their healthcare system and they not engaged.
Arousal
In the position of “arousal”, patients are hyper-attentive to every signal of their disease (emotional alert). Symptoms are lived as potential “alarms” that worries the patient and may cause acutely negative emotional reactions. Compared to the position of “blackout”, in this position patients are better informed about their health condition, but their health literacy is still superficial and fragmented (superficial knowledge). Moreover, they are not effective in enact self-management strategies (behavioral disorganization). These patients are at the very beginning of their engagement journey since there are starting to acquire a first awareness about their health and treatment requirements. However, they are not yet equipped to engage in an enhanced participation in their healthcare.
Adhesion
In a more advanced stage of their engagement journey, patients acquire a broader spectrum of health literacy (cognitive adhesion) and behavioral skills (formal adherence) to comply with medical prescriptions. They feel confident in their ability and motivation to cope with their illness. Furthermore, patients have accepted their health conditions and have elaborated the negative emotions connected with the critical health events showing a good resilience (acceptance). However, patients are still not autonomous in managing their health conditions and related treatment rules; they are not completely able to change their life style and to adhere correctly to the medication regimen, or at least they are not persistent in this. Every time life contexts change (e.g., going to holiday, travelling for work) or changes occur in their healthcare relationship (i.e. absence of the reference doctor, discontinuity of the healthcare team…) patients are challenged in their effort of being participative along their healthcare journey. Patients in this position experience an intermediate experience of engagement but they are still passively complying to the healthcare systems requirements because they have not fully understood and elaborated the rationale behind medical prescriptions (e.g., the final “whys” of rules and treatments).
Eudaimonic project
In the “eudaimonic project” position, patients have fully accepted their condition; furthermore, they have understood and elaborated that the “identity of patient” is only one possible identity. They are able to better incorporate the disease into their life projects, and they are no longer overwhelmed (such as in the blackout phase) by their health conditions; rather, they are able to integrate other spheres of their lives (elaboration). In this position of engagement, they appear more self-determined and resilient at the psychological level. To achieve this emotional elaboration, they use internal resources to project satisfactory life plans for their futures. Patients gradually become co-producers of their health, and they are capable of enacting more effective health management. In this process, patients become more active in effectively search for information about their disease conditions and management. This allows them to better master their healthcare experience at the psychological level (sense making) and to enact self-management conducts more effectively, despite eventual changes in the context (situated practices). Patients mature a positive attitude towards their illness and its treatment, being aware that “they are not their disease” and that despite the diagnosis it is still possible to maintain some form of satisfactory quality of life.
Application of the PHE model in the clinical setting: the PHE scale (PHE-s)
The model has been operationalized into a scientific measure, which allows to easily evaluate the level of patient engagement along the medical journey: the PHE-s (53).
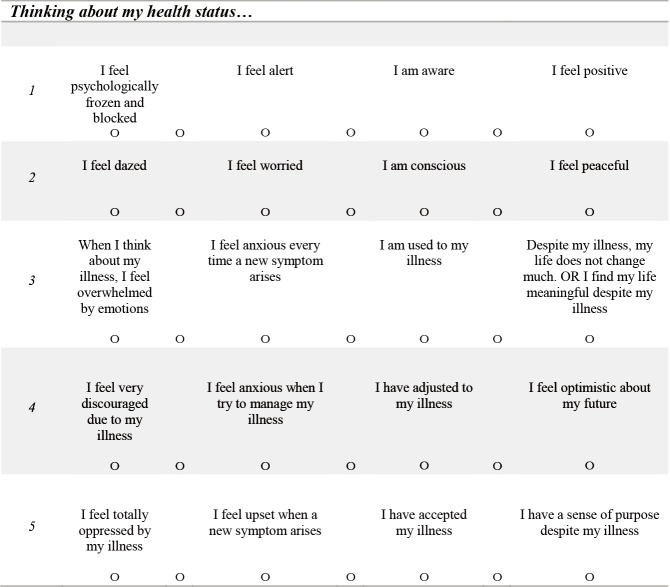
The PHE-s is a patient self-administrable short psycho-metric questionnaire developed with the aim of diagnosing the level of patient engagement in their healthcare process that is function of his/her degree of emotional elaboration of the health condition. The clinician has to explain to the patient the aim of the assessment by specifying that they should refer to how he/she is currently feels in relation to his/her health status to answer the questions. The response options featuring this instrument (i.e., ordinal scale) allow patients to easily mirroring their current emotional states within a continuum of possible emotional states and illness experience. The PHE-s, indeed, allows to easily assessing the position of engagement of the patient by asking five simple questions. The PHE-s options of answer features the different possible experience of a patient along his/her process of psychological elaboration about the mutated health condition and of their engagement needs (way of “feeling” when reflecting on health status). This instrument is today the only one specifically dedicated to assess the degree of emotional elaboration and adjustment reached by the patient concerning his/her ability to engage in health management.
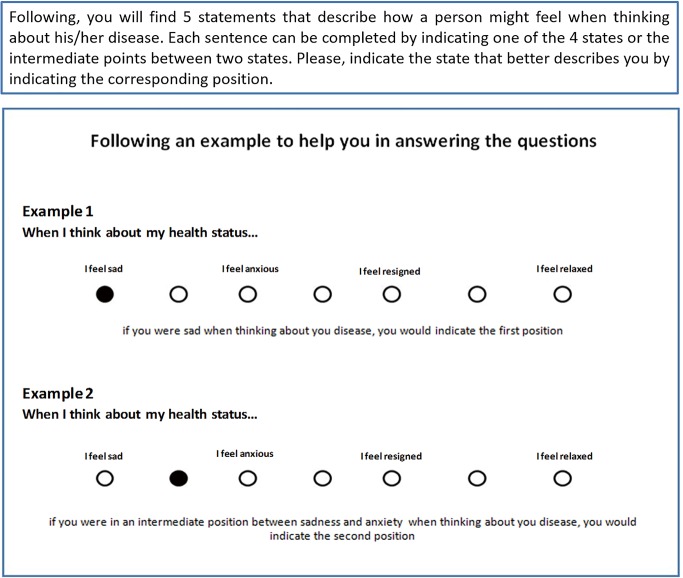
The specificity of this scale lays in the fact that it is rooted in a solid scientific framework of patient engagement. This allows not only to assess the actual patient’s attitude towards his/her engagement and self-management, but also to detect patients at risk for disengagement and thus to design preventive targeted intervention to educate and motivate him/her to be more compliant and participative. Thus, the PHE-s engagement outcome is useful to orient clinicians, caregivers, policy makers and researchers in better personalize educational and counselling programs by making them better aligned to patients’ priorities and expectations. Moreover, this tool allows clinicians to better understanding their patients’ illness experience, and, consequently, this improve their communication and relational skills. Figure 2 shows the instruction for the administration of the PHE-s. Figure 3 shows the complete PHE-s.
Figure 2.
Introductive formula to propose the PHE scale to the patient. PHE, Patient Health Engagement.
Figure 3.
The PHE scale. PHE, Patient Health Engagement.
The PHE model in practice: implication for medical practice
The PHE model and the PHE-s, as discussed in the previous paragraphs, might be concrete tools to collect a deep understanding of the patients’ emotional status and of their ability to be active agents in their disease management. Furthermore, these instruments allow practitioners to have a dynamic picture of the patient engagement journey and to identify the position of engagement featuring a patient. This is particularly crucial if we consider that patient engagement is a process along which patient’s needs, priorities and role expectations change basing on the phase occurring. As a consequence, to make a patient evolve from one phase to the subsequent one it is necessary to detect his/her priority needs and to effectively address them.
Research on the PHE model widely discussed the phase-specific levers to sustain the evolution of the patient engagement trajectory.
Particularly, to pass from the blackout position to the arousal position the patient should be emotionally sustained and supported in being resilient when facing his/her new health condition. This also means to help patients in overcoming the emotional confusion emerged after the diagnosis, by building a trusted relationship with the healthcare provider. The health practitioner is asked, particularly, to scaffold patients and offer solidarity by making an empathic response and educating patients about the nature and the characteristics of their new health condition. This informative action is expected from the referential clinician who becomes, since the time of the diagnosis, the main interlocutor for the patient along the care process. If patients fail to build a reliable and trusted relationship with the healthcare provider, their emotional responses may become dysfunctional, often leading to the patients’ dropout. In this phase, technologies that facilitate the communication with the referential clinicians and the monitoring of symptoms—such as telemonitoring or wearable devices—can make the patient feel protected and safe.
To pass from the arousal position to the adhesion position the patient need to become confident and feel effective in managing his/her health condition. Patients in this position need to be motivated and sustained in an effective behavioral change regarding their care and life style. In the arousal position, indeed, patients perceive healthcare professionals as an important point of reference who can help them managing their illnesses and treatment experiences which are a cause of stress. This requires clinicians to set realistic goals and positively reinforce patients when they succeed in managing the disease and the treatments. To foster a good relationship with healthcare providers since the time of diagnosis allows patients to improve their confidence and self-esteem. Healthcare professional, beside motivating patients to self-management behaviors, should also legitimize their active role and their willingness to become protagonist of their care. Technologies in this phase could be useful to generate in the patient a sense of mastery over their illness experience and to network with other individuals in similar conditions in order to share practices and solutions to face with the disease.
To pass from the adhesion position to the eudaimonic project position, the patient should acquire a more positive approach to their illness and their life, becoming more optimistic to their ability to improve quality of life. Their resilience in the disease journey need to be sustained and they should be motivated and educated in broadening their perception horizons, in terms of not being exclusively focused on the disease and its treatment, but also inclusive of other life sphere which may be potential source of motivation and optimism. Health coaching and positive psychological intervention may be important in order to allow the patients to adjust from the traumatic health experience and to lessen the negative impact of the disease on quality of life. To achieve this goal, it is important to sustain patients in maintaining active social roles in their communities and satisfactory interpersonal relationships. Furthermore, patients need help to make realistic plans and to set achievable goals in their quality of life management. In other words, patients need to be sustained in re-achieving some form of life projects, even if confined. Patients in the eudaimonic project position, furthermore, need to be sustained in their motivation and ability to influence other patients towards a more engaged approach to their healthcare. These patients may become privileged testimony of a positive and effective approach to illness and healthcare and they may lead the process of engagement transformation of their peers. In this direction, the role of patient association and patient advocacy is crucial and need to be sustained. Patient association may become the testing ground (and the magnifier) of good practices of patient engagement. At this stage new technologies may play an important role, not only with self-monitoring tools, but also allowing patients sharing and networks, patient advocacy and the storytelling of illness (and healing) experiences that may motivate and support at the emotional level patients still at the beginning of their engagement journey.
The PHE model in the ERAS setting: the experience of the VATS Group register
To substantially contribute to the debate about patient engagement promotion in thoracic surgery, the VATS Group dedicated to the diffusion and improvement of the ERAS approach in minimally invasive, is experimenting the collection of patient engagement data within their patients’ register.
As anticipated, the assessment of engagement levels and the monitoring of how these levels change in time is a first important goal to allow clinicians to better make patients active partners in their thoracic surgery experience. In particular, the introduction of PHE-s in the VATS register, and the collection of patient engagement data along the healthcare journey will have both scientific and pragmatic relevance.
At the scientific level, this will allow to obtain “real words” data about the variance and evolution of engagement trajectories over time. Furthermore, since the clinical and socio-demographic data collected in the register are various and numerous, this would open to the possibility to study the co-variance of engagement and other clinical characteristics of the patients. Moreover, this will guarantee the possibility to perform secondary analysis aimed at modeling how the clinical, contextual and psychological variables interlace and influences each-others in the process of engagement. This real-world modeling of the causal relationship among key variables will produce a scientific algorithm able to understand what are the key factors (or levers) on which it is opportune to work in order to improve the levels of patient engagement
Further then at the scientific and theoretical level, it is evident how this experimentation, if successful, may impact on clinical practice. The objective of the PHE-s is, indeed, to equip the healthcare professional with an easy and applicable measure to scientifically assess the levels of engagement. This, thanks to the linkage between the scale outcome and the PHE model, may provide the clinical team with concrete cues on patients’ experience and with advices and strategies to intervene at the best.
Conclusions
Although the debate about the clinical and organizational value of patients’ engagement is already well established in the scope of chronic disease management, less experience has been matured in the setting of acute care, and in particular in surgery.
However today the diffusion of new approach to surgery, such as ERAS or Fast Track put into question the need for a deep revision of traditional medical paradigms. The success of an ERAS approach in surgery, indeed, is not only dependent on the innovation of technological supports and of therapeutic acts. It is also dependent on the ability of the healthcare system and the surgery team of engaging patients in become more participative in their treatment and illness experience.
Particularly thoracic surgery is often lived by patients as a burdensome experience. The diagnosis and the consequent request of undergoing a thoracic surgery is often unexpected for patients and their families. This usually generates discomfort and negative psychological responses. In order to become able to cope with the disease and the stress of the therapeutic action, patients need to be sustained in their emotional journey of acceptance and resilience. Furthermore, the ability of patients to cope with their emotions and to assume a more positive approach to their illness and its treatment is a key to sustain patient engagement along the healthcare pathway.
Moving from these premises, in this article we have argued how the PHE model, which features the evolution of patient engagement trajectories and of its implication at the psychological level, may be a useful framework in thoracic surgery, particularly when the ERAS approach is concerned. This process-like modeling of patients’ engagement potentially leads to a real revolution of healthcare paradigms in research and intervention by posing the bases for a true and sustainable partnership between patients and health practitioners. In this perspective, while the process of patient engagement evolves, even the patient-practitioner relationship assumes different shapes (from passivity to partnership) thus implying a continuous realignment of roles and power dynamics.
The PHE model, operationalized in the PHE-s, allow clinicians to easily assessing patients’ level of engagement, and thus their needs and expectations in terms of doctor-patient communication, health literacy and therapeutic education. The introduction of the PHE-s along the patient journey, thus, would allow to track the evolution of patient engagement, to identify critical cases and even to verify the effectiveness of patients support programs in sustaining patients’ psychological resilience and participation in healthcare.
PHE-s has been inserted in the Italian VATS Group and ERAS Registry. This testifies an important turning point in the cultural approach to patients’ role in thoracic surgery. This experimentation deserves particular attention due to its scientific and clinical potential. It would allow—for the first time—to collect real world data about patient engagement trajectories in ERAS surgery and to put this in relationship with clinical and socio-demographic data of the patients.
A very ambitious project that at least it is worthy to be pursued. Future results will tell if the experimentation has been successful and fruitful.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Baron-Epel O, Dushenat M, Friedman N. Evaluation of the consumer model: relationship between patients' expectations, perceptions and satisfaction with care. Int J Qual Health Care 2001;13:317-23. 10.1093/intqhc/13.4.317 [DOI] [PubMed] [Google Scholar]
- 2.Badcott D. The expert patient: Valid recognition or false hope? Med Health Care Philos 2005;8:173-8. 10.1007/s11019-005-2275-7 [DOI] [PubMed] [Google Scholar]
- 3.Ramsey I, Corsini N, Peters MDJ, et al. Patient Education and Counseling Review article A rapid review of consumer health information needs and preferences. Patient Educ Couns 2017;100:1634-42. 10.1016/j.pec.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 4.Lober WB, Flowers JL. Consumer empowerment in health care amid the internet and social media. Semin Oncol Nurs 2011;27:169-82. 10.1016/j.soncn.2011.04.002 [DOI] [PubMed] [Google Scholar]
- 5.Ng CJ, Lee PY, Lee YK, et al. An overview of patient involvement in healthcare decision-making: a situational analysis of the Malaysian context. BMC Health Serv Res 2013;13:408. 10.1186/1472-6963-13-408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin LT, Schonlau M, Haas A, et al. Patient activation and advocacy: which literacy skills matter most? J Health Commun 2011;16 Suppl 3:177-90. 10.1080/10810730.2011.604705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaba R, Sooriakumaran P. The evolution of the doctor-patient relationship. Int J Surg 2007;5:57-65. 10.1016/j.ijsu.2006.01.005 [DOI] [PubMed] [Google Scholar]
- 8.Barello S, Graffigna G, Vegni E, et al. 'Engage me in taking care of my heart': a grounded theory study on patient-cardiologist relationship in the hospital management of heart failure. BMJ Open 2015;5:e005582. 10.1136/bmjopen-2014-005582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beisecker AE, Beisecker TD. Using Metaphors to Characterize Doctor--Patient Relationships: Paternalism Versus Consumerism. Health Commun 1993;5:41-58. 10.1207/s15327027hc0501_3 [DOI] [Google Scholar]
- 10.Taylor K. Paternalism, participation and partnership - the evolution of patient centeredness in the consultation. Patient Educ Couns 2009;74:150-5. 10.1016/j.pec.2008.08.017 [DOI] [PubMed] [Google Scholar]
- 11.Hibbard JH, Mahoney E. Toward a theory of patient and consumer activation. Patient Educ Couns 2010;78:377-81. 10.1016/j.pec.2009.12.015 [DOI] [PubMed] [Google Scholar]
- 12.Weinberger SE, Johnson BH, Ness DL. Patient- and family-centered medical education: the next revolution in medical education? Ann Intern Med 2014;161:73-5. 10.7326/M13-2993 [DOI] [PubMed] [Google Scholar]
- 13.Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood) 2013;32:223-31. 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 14.Kinney RL, Lemon SC, Person SD, et al. The association between patient activation and medication adherence, hospitalization, and emergency room utilization in patients with chronic illnesses: a systematic review. Patient Educ Couns 2015;98:545-52. 10.1016/j.pec.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 15.Skolasky RL, Mackenzie EJ, Wegener ST, et al. Patient activation and adherence to physical therapy in persons undergoing spine surgery. Spine (Phila Pa 1976) 2008;33:E784-91. 10.1097/BRS.0b013e31818027f1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall R, Beach MC, Saha S, et al. Patient activation and improved outcomes in HIV-infected patients. J Gen Intern Med 2013;28:668-74. 10.1007/s11606-012-2307-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hochhalter AK, Song J, Rush J, et al. Making the Most of Your Healthcare intervention for older adults with multiple chronic illnesses. Patient Educ Couns 2010;81:207-13. 10.1016/j.pec.2010.01.018 [DOI] [PubMed] [Google Scholar]
- 18.Hadgkiss EJ, Jelinek GA, Taylor KL, et al. Engagement in a program promoting lifestyle modification is associated with better patient-reported outcomes for people with MS. Neurol Sci 2015;36:845-52. 10.1007/s10072-015-2089-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mosen DM, Schmittdiel J, Hibbard J, et al. Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manage 2007;30:21-9. 10.1097/00004479-200701000-00005 [DOI] [PubMed] [Google Scholar]
- 20.Barello S, Graffigna G. Engaging patients to recover life projectuality: an Italian cross-disease framework. Qual Life Res 2015;24:1087-96. 10.1007/s11136-014-0846-x [DOI] [PubMed] [Google Scholar]
- 21.Mitchell SE, Gardiner PM, Sadikova E, et al. Patient Activation and 30-Day Post-Discharge Hospital Utilization. J Gen Intern Med 2014;29:349-55. 10.1007/s11606-013-2647-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexander JA, Hearld LR, Mittler JN, et al. Patient-physician role relationships and patient activation among individuals with chronic illness. Health Serv Res 2012;47:1201-23. 10.1111/j.1475-6773.2011.01354.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boivin A, Lehoux P, Lacombe R, et al. Involving patients in setting priorities for healthcare improvement: a cluster randomized trial. Implement Sci 2014;9:24. 10.1186/1748-5908-9-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee YK, Low WY, Ng CJ. Exploring patient values in medical decision making: a qualitative study. PLoS One 2013;8:e80051. 10.1371/journal.pone.0080051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez-Osorio CA, Dominguez-Cherit G. Medical decision making: paternalism versus patient-centered (autonomous) care. Curr Opin Crit Care 2008;14:708-13. 10.1097/MCC.0b013e328315a611 [DOI] [PubMed] [Google Scholar]
- 26.Elwyn G, Lloyd A, May C, et al. Collaborative deliberation: A model for patient care. Patient Educ Couns 2014;97:158-64. 10.1016/j.pec.2014.07.027 [DOI] [PubMed] [Google Scholar]
- 27.Markovitz SE, Schrooten W, Arntz A, et al. Resilience as a predictor for emotional response to the diagnosis and surgery in breast cancer patients. Psychooncology 2015;24:1639-45. 10.1002/pon.3834 [DOI] [PubMed] [Google Scholar]
- 28.Hart KE, Wilson TL, Hittner JB. A Psychosocial Resilience Model to Account for Medical Well-being in Relation to Sense of Coherence. J Health Psychol 2006;11:857-62. 10.1177/1359105306069082 [DOI] [PubMed] [Google Scholar]
- 29.Gardner G, Elliott D, Gill J, et al. Patient experiences following cardiothoracic surgery: An interview study. Eur J Cardiovasc Nurs 2005;4:242-50. 10.1016/j.ejcnurse.2005.04.006 [DOI] [PubMed] [Google Scholar]
- 30.Morganstern BA, Bochner B, Dalbagni G, et al. The psychological context of quality of life: a psychometric analysis of a novel idiographic measure of bladder cancer patients’ personal goals and concerns prior to surgery. Health Qual Life Outcomes 2011;9:10. 10.1186/1477-7525-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bäckström S, Wynn R, Sørlie T. Coronary bypass surgery patients' experiences with treatment and perioperative care - a qualitative interview-based study. J Nurs Manag 2006;14:140-7. 10.1111/j.1365-2934.2006.00608.x [DOI] [PubMed] [Google Scholar]
- 32.Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6-8. 10.1056/NEJMp1209500 [DOI] [PubMed] [Google Scholar]
- 33.Kash BA, Zhang Y, Cline KM, et al. The perioperative surgical home (PSH): a comprehensive review of US and non-US studies shows predominantly positive quality and cost outcomes. Milbank Q 2014;92:796-821. 10.1111/1468-0009.12093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moulton B, King JS. Aligning ethics with medical decision-making: the quest for informed patient choice. J Law Med Ethics 2010;38:85-97. 10.1111/j.1748-720X.2010.00469.x [DOI] [PubMed] [Google Scholar]
- 35.Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ 2010;341:c5146. 10.1136/bmj.c5146 [DOI] [PubMed] [Google Scholar]
- 36.Barello S, Graffigna G. Engagement-sensitive decision making: Training doctors to sustain patient engagement in medical consultations. In: Graffigna G, Barello S, Triberti S. editors. Patient Engagement: A Consumer-Centered Model to Innovate Healthcare. Berlin/Boston: Walter de Gruyter GmbH & Co., 2016:78- 93. [Google Scholar]
- 37.Skolasky RL, Mackenzie EJ, Riley LH, et al. Psychometric properties of the Patient Activation Measure among individuals presenting for elective lumbar spine surgery. Qual Life Res 2009;18:1357-66. 10.1007/s11136-009-9549-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cook DJ, Manning DM, Holland DE, et al. Patient engagement and reported outcomes in surgical recovery: effectiveness of an e-health platform. J Am Coll Surg 2013;217:648-55. 10.1016/j.jamcollsurg.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 39.Bianchini C, Pelucchi S, Pastore A, et al. Enhanced recovery after surgery (ERAS) strategies: possible advantages also for head and neck surgery patients? Eur Arch Otorhinolaryngol 2014;271:439-43. 10.1007/s00405-013-2502-4 [DOI] [PubMed] [Google Scholar]
- 40.Melnyk M, Casey RG, Black P, et al. Enhanced recovery after surgery (ERAS) protocols: Time to change practice? Can Urol Assoc J 2011;5:342-8. 10.5489/cuaj.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McKenna RJ, Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. 10.1016/j.athoracsur.2005.07.078 [DOI] [PubMed] [Google Scholar]
- 42.Graffigna G, Barello S, Riva G, et al. Fertilizing a Patient Engagement Ecosystem to Innovate Healthcare: Toward the First Italian Consensus Conference on Patient Engagement. Front Psychol 2017;8:812. 10.3389/fpsyg.2017.00812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coulter A. Measuring what matters to patients. BMJ 2017;356:j816. 10.1136/bmj.j816 [DOI] [PubMed] [Google Scholar]
- 44.Graffigna G, Barello S. The Value of Measuring Patient Engagement in Healthcare: New Frontiers for Healthcare Quality. In: Graffigna G. editor. Promoting Patient Engagement and Participation for Effective Healthcare Reform. Hershey, PA, USA: Medical Information Science Reference, 2016:192-214. [Google Scholar]
- 45.Menichetti J, Graffigna G. "PHE in Action": Development and Modeling of an Intervention to Improve Patient Engagement among Older Adults. Front Psychol 2016;7:1405. 10.3389/fpsyg.2016.01405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Légaré F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood) 2013;32:276-84. 10.1377/hlthaff.2012.1078 [DOI] [PubMed] [Google Scholar]
- 47.Gruman J, Rovner MH, French ME, et al. From patient education to patient engagement: implications for the field of patient education. Patient Educ Couns 2010;78:350-6. 10.1016/j.pec.2010.02.002 [DOI] [PubMed] [Google Scholar]
- 48.Hibbard JH, Stockard J, Mahoney ER, et al. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Epstein RM, Street RL Jr. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, MD: National Cancer Institute, NIH Publication, 2017. [Google Scholar]
- 50.Meglic M, Furlan M, Kuzmanic M, et al. Feasibility of an eHealth service to support collaborative depression care: results of a pilot study. J Med Internet Res 2010;12:e63. 10.2196/jmir.1510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haskell H, Lord T. Patients and Families as Coproducers of Safe and Reliable Outcomes. In: Sanchez J, Barach P, Johnson JK, et al. editors. Surgical Patient Care: Improving Safety, Quality and Value. Cham: Springer International Publishing, 2017:101-20. [Google Scholar]
- 52.Graffigna G, Barello S, Triberti S. Patient engagement: A consumer-centered model to innovate healthcare. Patient Engagement: A Consumer-Centered Model to Innovate Healthcare. Warsaw: Walter de Gruyter GmbH and Co KG, 2016. [Google Scholar]
- 53.Graffigna G, Barello S, Bonanomi A, et al. Measuring patient engagement: development and psychometric properties of the Patient Health Engagement (PHE) Scale. Front Psychol 2015;6:274. 10.3389/fpsyg.2015.00274 [DOI] [PMC free article] [PubMed] [Google Scholar]