Abstract
Enhanced recovery after surgery (ERAS) is a multimodal, polyhedral approach to surgical management for patients undergoing surgical therapy. Since ERAS is not a specific procedure, these protocols are not exclusively created for particular clinical settings but they are prone to be adapted to a large variety of healthcare programs after surgery. ERAS Society was the platform in which a new multidisciplinary methodology to promote a fast recovery, a considerable patient involvement and resource optimization has been developed. ERAS Society has also produced guidelines for different surgical specialties and has already generated some evidence regarding preoperative, intraoperative and postoperative practice. ERAS in Thoracic Surgery has had a slow-growing development but some hints suggest that introducing ERAS methodology in pulmonary resections for cancer could be feasible and effective with potential tangible benefits for patients, families, caregivers and welfare. There is no evidence yet concerning ERAS principles in Thoracic Surgery; for this reason, a new possibility for prospective data collection and analysis is created using the VATS Group Web Registry in which additional records, documents and facts have now the possibility to be registered and eventually explored to possibly adjust the ERAS protocols to major pulmonary resections.
Keywords: Lung resection, fast recovery, videothoracoscopy, registry
Introduction
Enhanced recovery after surgery (ERAS) program was first illustrated by Henrik Kehlet in 1997 with the specific interest for quality improvement of perioperative protocols (1). The ERAS principles have then become a Society with progressive interest and support in generating guidelines and programs for a fast recovery after surgery. ERAS is not specific for surgical subspecialties but applies general principles for the best patient response to physical and psychological impact of surgery (2).
During the last decade, a growing interest for ERAS practice has been observed with an increasing trend in scientific contribution and clinical practise. Most experiences of ERAS/fast track concern abdominal surgery and urology with very promising results (3-6). More recently, ERAS programme has been applied in particular patient subsets such as obesity and geriatric surgery. The available results, although they are preliminary, seem to support the ERAS directions to develop new strategies for patient management after surgery and indicate the intent to progressively adjust specific methodologies for a more and more appropriate patient-centred care (7). Some data also support ERAS/fast track for potential economic benefit coming from a systematically applied ERAS protocols (8).
ERAS Society has produced guidelines to facilitate the use of ERAS code but Thoracic Surgery subspecialties (cardiac, general thoracic, thoracic surgical oncology) and others are still spaces to be explored for possible application of ERAS. In fact, very limited experiences are available in literature with poor evidence (9).
For this reason, a prospective database of patients undergoing VATS pulmonary anatomical resections is created to possibly evaluate the applicability, the feasibility and the cost/effectiveness of ERAS standards in thoracic surgery using the VATS Group data collection and analytical methodology in order to highlight possible standardized procedure, clinical guidelines and economical aspects (10-13).
Summary of ERAS principles
ERAS/fast track includes different multidisciplinary approach to prepare, to support and to early discharge patients when they require a surgical procedure. The ERAS methodology lies on a strong connection between patients and caregivers including the surgeon with the goal to arrange and speed up the recovery process (14). Since this ideal process has already been developed, some steps of the ERAS route to recovery are already available (15).
Firstly, great importance is associated to the patient engagement. Patients must be educated and informed regarding their health condition and must be conscious of the therapeutic programme in order to be active part during the medical process and recovery. There are different tools to engage a patient for enhancing a fast recovery but evidence is limited. Likewise, the patient education is definitely a crucial aspect and it represents a momentous step in the ERAS process for a fast improvement after surgical manipulation (16). Additionally, emphasis is put on the nutritional and general condition especially regarding the comorbidities and their management in view of the surgical schedule (17). The traditional perioperative agenda is also discussed in recent literature with preliminary results supporting a shorter preoperative fasting time and early return to physical activity. For the ERAS Society, Anaesthesiology protocols should develop a more and more flexible management and, finally, the multidisciplinary approach must involve non-medical caregivers to help the progression of patients to the final discharge. Physiotherapists, nutritionists, behaviourists and other practitioners must be involved in the entire therapeutic management to create a single systematic care mission out of many specific serial inputs.
The Registry
Based on the VATS Group Registry Platform (12), a new section of the VATS Group Registry is created. A dedicated Commission with interest in implementing ERAS/fast track in Thoracic Surgery has developed the series of indicators according to ERAS Society standards. Based on the experiences of other surgical subspecialties and the available limited literature, the VATS Group dedicated Commission has developed possible ERAS protocols to be followed as instructions to manage patients undergoing VATS anatomical pulmonary resections.
The Registry allows for a prospective collection of data and possible analysis of effectiveness, feasibility and weakness of ERAS/fast track in pulmonary resection.
Admission is identified with a numerical code, which relates to the single patient and surgical Centre. There is no possibility to have the admission page and the patient identity page open at the same time according to privacy policy. The admission page also represents a page of synthesis of the enrolled patient (Figure 1).
Figure 1.
Admission page. A code is generated by the system and assigned to each patient, a summary of patient perioperative data is furnished and drop-out causes are signaled (arrows).
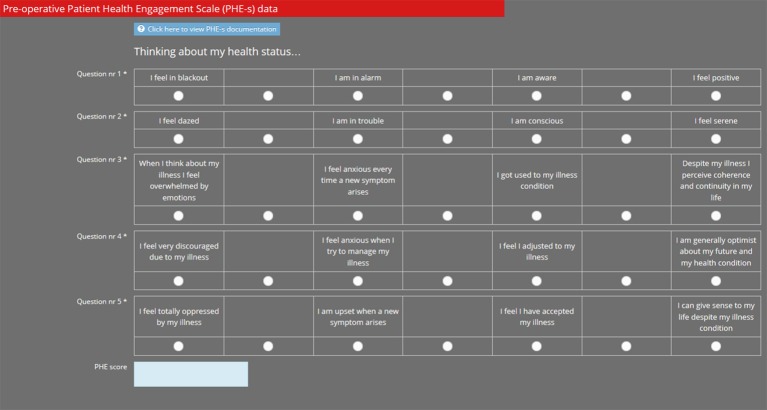
The functional page, already present in the VATS Group Registry, has been edited in the ERAS platform. The Preoperative Patient Health Engagement scale (PHE-s) was added and represents a mandatory indicator to put in the patient’s records otherwise the subject is automatically indicated as out of the protocol (Figure 2).
Figure 2.
Preoperative PHE-s is uploaded with a survey model. *, means that the field is required, to be mandatory filled. PHE-s, Patient Health Engagement scale.
Perioperative management and nutritional support data need to be reported as part of the ERAS perioperative course of actions. Anemia and malnutrition are of crucial importance. Information regarding anemia and its management must be reported as well as preoperative fasting, postoperative nutrition resume, fluid balance and post-operative mobilization. Variables are expressed as a choice between two mutually exclusive possibilities (Figure 3).
Figure 3.
Perioperative management page. Information about anemia and nutritional status are presented in this page and information regarding treatment are required. *, means that the field is required, to be mandatory filled.
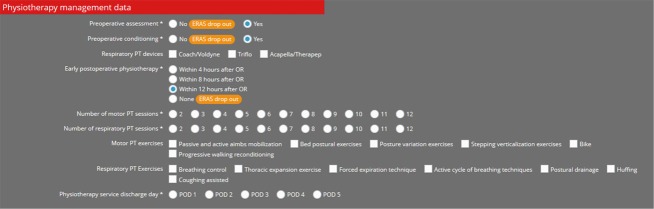
Physiotherapy represents a momentous issue in the ERAS methodology, so a dedicated page is provided with a series of mandatory data that represent possible causes of ERAS protocol failure if not submitted to patients during the perioperative period. Information regarding the preoperative physiotherapy management, preparation to surgery, type of exercise and service provided as well as number and timing of physiotherapy sessions are the requested information to be put in the registry (Figure 4).
Figure 4.
Physiotherapy page. According to ERAS Society, physiotherapy must be provided during the entire perioperative period; the Registry asks for information regarding preoperative management, number and type of exercises, timing and duration of tutored sessions. *, means that the field is required, to be mandatory filled. ERAS, enhanced recovery after surgery.
Anesthesiology protocols have been developed in many surgical specialties. Being so, to analyze different strategies for intraoperative management, especially concerning circulation, ventilation and drugs is considered promising for further critical analysis (Figure 5).
Figure 5.
Anesthesia page. A list of anesthesiology data is added, with emphasis on cardiovascular and respiratory conditions. *, means that the field is required, to be mandatory filled.
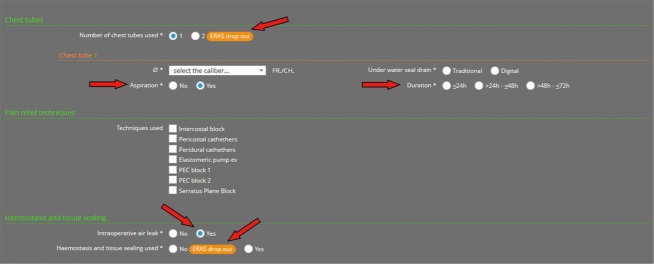
Surgery must be performed according to VATS criteria and several additional rules are proposed in the protocol. Only one chest tube with or without suction is admitted for the ERAS VATS surgery with a maximal time span of maximum 72 hours. Intraoperative air leaks must be reported and treated with sealants eventually (Figure 6).
Figure 6.
Surgical procedure page. Surgical protocol for ERAS VATS are required, despite information regarding of a possible second chest tube, ERAS protocol is considered accomplished if only one chest tube is placed for a limited duration up to 72 hours (arrows above). Moreover, information of pain relief techniques are required. Finally, intraoperative air leak must be treated with sealants and reported (arrows below). *, means that the field is required, to be mandatory filled. ERAS, enhanced recovery after surgery.
Analgesia is a crucial issue for ERAS methodology. Mandatory acknowledgements are: scheduled pain evaluation, loco-regional analgesic technique to be performed and systemic analgesic adjuvant if necessary. A series of details regarding the techniques and timing of administration of analgesics are required (Figure 7).
Figure 7.
Analgesia data page. The focus of ERAS methodology in the analgesia management is the continuous control of analgesia and the flexibility and patient-centered protocol. ERAS patients must be evaluated at scheduled time, treated with loco-regional techniques with systemic adjuvants. *, means that the field is required, to be mandatory filled. ERAS, enhanced recovery after surgery.
At discharge, patient engagement and pain are the two subjective indicators asked. All the other information concerns the chest tube management and the day of discharge. Considering the objective of ERAS to enhance a fast track, the cut off day for a supposed successful ERAS VATS lobectomy is postoperative day 4 (Figure 8).
Figure 8.
Discharge data page. Patient engagement (PHE-s) is asked again (arrow above); pain condition is remarkable for a fine ERAS process to fast recovery and thus asked again (arrow). The discharge day is hypothetically put at day 4 as the limit for an acceptable ERAS/fast track route. Moreover, information on the chest drainage are requested to highlight the association between discharge from hospital and chest tube management (arrows below). *, means that the field is required, to be mandatory filled. PHE-s, Patient Health Engagement scale; ERAS, enhanced recovery after surgery.
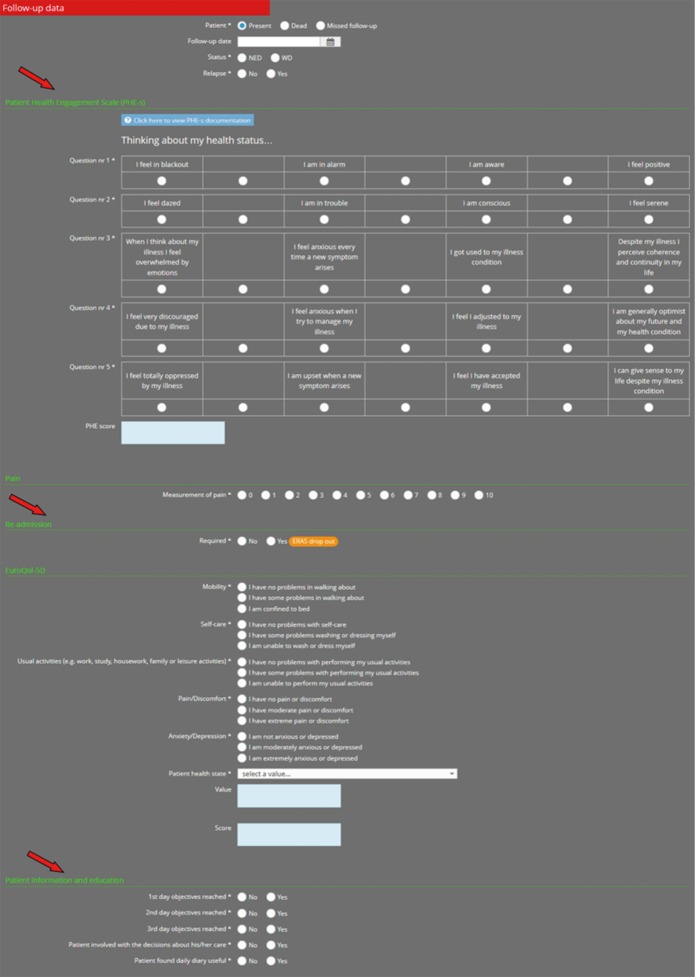
The Registry is finally closed with the follow up pages. Already present in the original VATS Group database, data regarding facts happening during the first 30 days post-operatively are required. In this page, two items are added to the original database version according to ERAS Society guidelines: patients engagement and self-assessment of the goals accomplished during the recovery period. In case of return to hospital for events that require new admission for any kind of medical procedure, the patient is automatically marked as a patient in which the ERAS route has been fallacious (Figure 9).
Figure 9.
Follow-up data page. A series of data regarding the 30 days after surgery are collected; ERAS items are: patient engagement (arrow above) with a new and final PHE-s, possible causes of readmission to hospital are here placed (arrow) and educational objectives accomplished (arrow below). All complications and events leading to enhanced recovery failure are reported here. *, means that the field is required, to be mandatory filled. PHE-s, Patient Health Engagement scale; ERAS, enhanced recovery after surgery.
Acknowledgements
None.
Ethical Statement: The manuscript is produced in accordance with the Helsinki Declaration as revised in 2013.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- 1.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. 10.1093/bja/78.5.606 [DOI] [PubMed] [Google Scholar]
- 2.Aarts MA, Rotstein OD, Pearsall EA, et al. Postoperative ERAS Interventions Have the Greatest Impact on Optimal Recovery: Experience With Implementation of ERAS Across Multiple Hospitals. Ann Surg 2018. [Epub ahead of print]. 10.1097/SLA.0000000000002632 [DOI] [PubMed] [Google Scholar]
- 3.Li Z, Wang Q, Li B, et al. Influence of enhanced recovery after surgery programs on laparoscopy-assisted gastrectomy for gastric cancer: a systematic review and meta-analysis of randomized control trials. World J Surg Oncol 2017;15:207. 10.1186/s12957-017-1271-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ding J, Sun B, Song P, et al. The application of enhanced recovery after surgery (ERAS)/fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Oncotarget 2017;8:75699-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao Y, Qin H, Wu Y, et al. Enhanced recovery after surgery program reduces length of hospital stay and complications in liver resection: A PRISMA-compliant systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2017;96:e7628. 10.1097/MD.0000000000007628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tyson MD, Chang SS. Enhanced Recovery Pathways Versus Standard Care After Cystectomy: A Meta-analysis of the Effect on Perioperative Outcomes. Eur Urol 2016;70:995-1003. 10.1016/j.eururo.2016.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Małczak P, Pisarska M, Piotr M, et al. Enhanced Recovery after Bariatric Surgery: Systematic Review and Meta-Analysis. Obes Surg 2017;27:226-35. 10.1007/s11695-016-2438-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kagedan DJ, Devitt KS, Tremblay St-Germain A, et al. The economics of recovery after pancreatic surgery: detailed cost minimization analysis of an enhanced recovery program. HPB (Oxford) 2017;19:1026-33. 10.1016/j.hpb.2017.07.013 [DOI] [PubMed] [Google Scholar]
- 9.Li S, Zhou K, Che G, et al. Enhanced recovery programs in lung cancer surgery: systematic review and meta-analysis of randomized controlled trials. Cancer Manag Res 2017;9:657-70. 10.2147/CMAR.S150500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nosotti M, Droghetti A, Luzzi L, et al. First Italian Consensus Conference on VATS lobectomy for NSCLC. Tumori 2017;103:124-35. 10.5301/tj.5000578 [DOI] [PubMed] [Google Scholar]
- 11.Bertani A, Gonfiotti A, Nosotti M, et al. Nodal management and upstaging of disease: initial results from the Italian VATS Lobectomy Registry. J Thorac Dis 2017;9:2061-70. 10.21037/jtd.2017.06.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crisci R, Droghetti A, Migliore M, et al. Video-assisted thoracic lobectomy for lung cancer in Italy: the 'VATS Group' Project. Future Oncol 2016;12:9-11. 10.2217/fon-2016-0466 [DOI] [PubMed] [Google Scholar]
- 13.Droghetti A, Marulli G, Vannucci J, et al. Cost analysis of pulmonary lobectomy procedure: comparison of stapler versus precision dissection and sealant. Clinicoecon Outcomes Res. 2017;9:201-6. 10.2147/CEOR.S115322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spanjersberg WR, Reurings J, Keus F, et al. Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev 2011;(2):CD007635. [DOI] [PubMed] [Google Scholar]
- 15.ERAS Compliance Group The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection: Results From an International Registry. Ann Surg 2015;261:1153-9. 10.1097/SLA.0000000000001029 [DOI] [PubMed] [Google Scholar]
- 16.Thorn CC, White I, Burch J, et al. Active and passive compliance in an enhanced recovery programme. Int J Colorectal Dis 2016;31:1329-39. 10.1007/s00384-016-2588-4 [DOI] [PubMed] [Google Scholar]
- 17.Byrnes A, Banks M, Mudge A, et al. Enhanced Recovery After Surgery as an auditing framework for identifying improvements to perioperative nutrition care of older surgical patients. Eur J Clin Nutr 2017. [Epub ahead of print]. 10.1038/s41430-017-0049-y [DOI] [PubMed] [Google Scholar]