Abstract
Background
Scarce reports exist of permanent deployment of Solitaire FR™ devices for arterial steno-occlusive disease as it is primarily indicated for temporary deployment for thrombectomy in large-vessel, anterior-circulation ischemic strokes. Even more scarce are reports describing permanent deployment of the Solitaire device for posterior circulation strokes.
Summary
We present 2 cases where the Solitaire device was electrolytically detached to re-establish flow in an occluded or stenotic basilar artery in acutely symptomatic patients. In both cases, a 4 × 15 mm Solitaire device was positioned across the stenotic or occluded portion of the basilar artery and electrolytically detached to maintain vessel patency. Both cases had good clinical outcomes with a National Institutes of Health Stroke Scale (NIHSS) score of 1 (from 24) on 90-day follow-up and an NIHSS score of 2 (from 7) on 30-day follow-up.
Key Messages
Permanent deployment of the Solitaire device may potentially be a safe and effective means of maintaining vessel patency in an occluded or stenotic basilar artery.
Keywords: Acute stroke, Solitaire, Thrombectomy
Introduction
Mechanical thrombectomy with stent retrievers for anterior circulation strokes has been shown to be effective in the recanalization of proximal large-vessel occlusions which have been shown to translate to good clinical outcomes [1, 2, 3, 4, 5]. Studies reporting on the use of stent retrievers for posterior circulation strokes have been limited, however [6, 7, 8, 9, 10].
Given the devastating consequences of an acute basilar occlusion, carrying a poor prognosis with 90% mortality and a severe residual benefit in 65% of survivors [11], treatment strategies aimed at recanalization of the basilar artery may be of benefit [6] as has been demonstrated for anterior circulation strokes.
The recanalization rates with stentrievers for acute basilar occlusion (alone or in combination with other therapies) have been reported at 74% [6], 100% [9, 12], 81% [13], 96% [7], and 94.4% [10]. In instances of treatment failure, strategies such as stenting [9, 10] or thrombus aspiration [9] have been employed. We present 2 cases wherein the Solitaire FR™ stentriever device was permanently deployed in the basilar artery in an acute stroke setting.
Case Report
Case 1
A 47-year-old female initially presented with a 3-day history of confusion and nonfluent speech, had a National Institutes of Health Stroke Scale (NIHSS) score of 4, and was found to have a subacute right occipital stroke. Intravenous tissue plasminogen activator (tPA) was not given at that time, as she was out of the treatment window. Computed tomography (CT) angiography of the head then showed complete occlusion of the left vertebral artery to the mid-basilar artery. Conventional angiogram was done with intent to treat and showed good collateral filling past the occlusion, mostly through the left posterior communicating artery (PCOM) and posterior inferior cerebellar artery to anterior inferior cerebellar artery collaterals. There was no intervention at this time, given the fairly mild exam with good collateral flow.
Ten days into admission, she had acute worsening of symptoms, i.e., obtundation with quadriparesis and NIHSS score of 24. International normalized ratio at that time was 4.6, as she had been placed on anticoagulation for antiphospholipid antibody syndrome. CT showed interval development of an acute infarct on the left brachium pontis and left paramedian pons on top of subacute infarctions within the left cerebellar hemisphere and right occipital lobe. The decision was made to treat, given the acute worsening of symptoms. Groin puncture occurred 90 min after symptom onset.
Conventional angiogram showed diminished reconstitution of the basilar artery from the previously demonstrated left PCOM collateral (Fig. 1). The decision was thus made to treat, given the acute worsening of the symptoms as well as diminished hemodynamic reconstitution of the basilar artery.
Fig. 1.
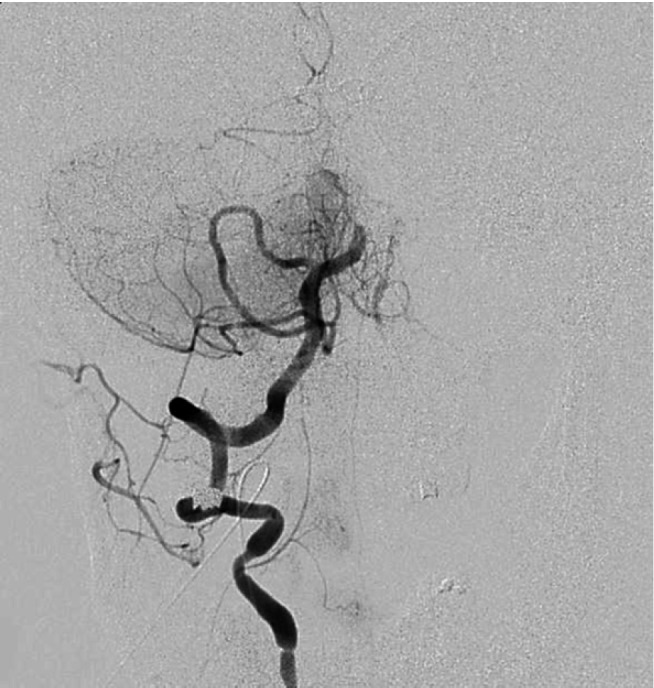
Digital subtraction angiography showing proximal basilar occlusion. 49 × 52 mm (300 × 300 DPI).
A 6-Fr NeuronMax sheath was advanced and positioned within the right subclavian artery. Under roadmap guidance, a coaxial 0.058-inch Navien catheter was then introduced over a 150-cm Marksman microcatheter/0.014-inch Transcend wire into the C1 segment of the right vertebral artery. This construct was then used to traverse the occluded segment, and the wire tip was positioned in the P2 segment of the right posterior cerebral artery (PCA). The microcatheter was then exchanged for a 2 × 9 mm Maverick balloon microcatheter that was used for angioplasty of the segment with maximal pressure at 10 atm (Fig. 2).
Fig. 2.
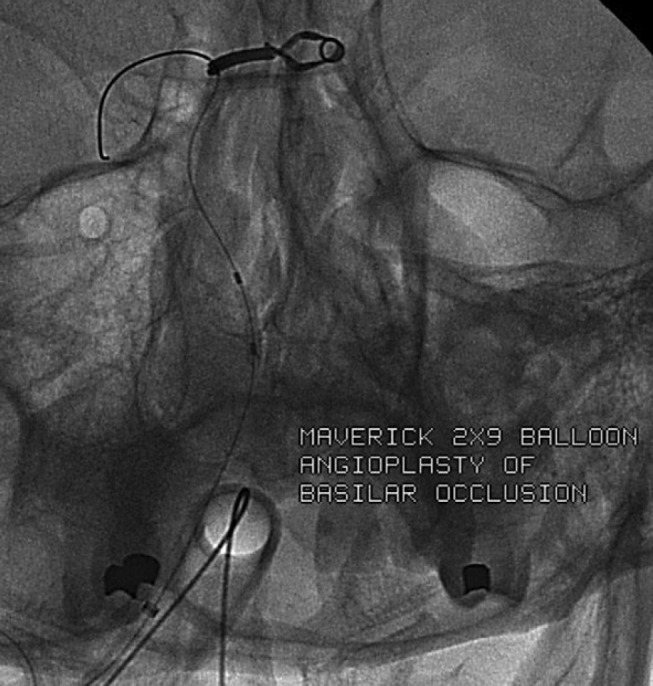
2 × 9 mm Maverick balloon microcatheter in the occluded segment. 114 × 76 mm. 45 × 48 mm (300 × 300 DPI).
The balloon was removed while maintaining wire access across the now open but still irregularly stenosed segment. A Marksman catheter was advanced, through which a 4 × 15 mm Solitaire device was positioned across the diseased segment and was electrolytically detached (Fig. 3). The mid-segment of the construct was balloon angioplastied after that.
Fig. 3.

4 × 15 mm Solitaire FR device positioned and electrolytically detached across the diseased segment. 51 × 51 mm (300 × 300 DPI).
Good antegrade flow was restored in the basilar artery (TICI 3; Fig. 4). Groin puncture to recanalization time was 204 min. The postprocedure clinical course was complicated by an asymptomatic, 4 × 3 cm vermian/right medial cerebellar hemorrhage on postoperative day (POD) 4, which was stable on subsequent imaging. She was discharged on POD 14 with an NIHSS score of 4. She had follow-up 90 days after recanalization and had a left facial droop (NIHSS = 1) with reported gait instability.
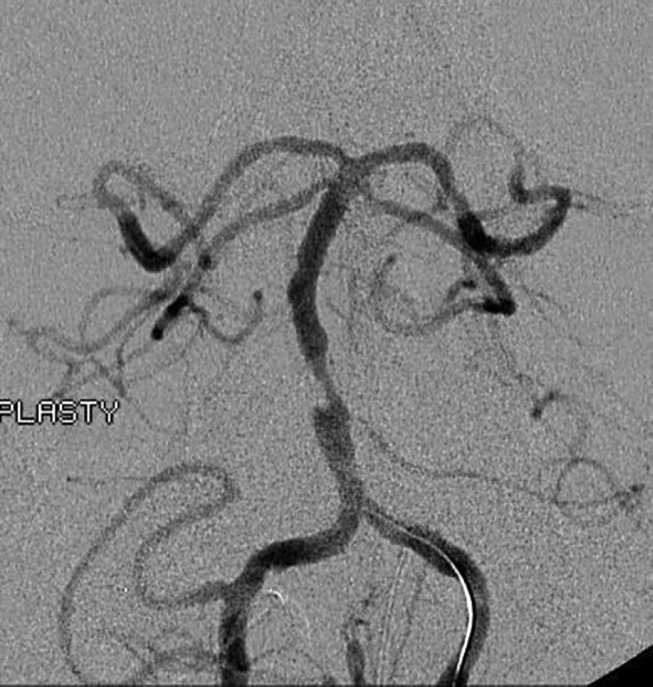
Fig. 4.
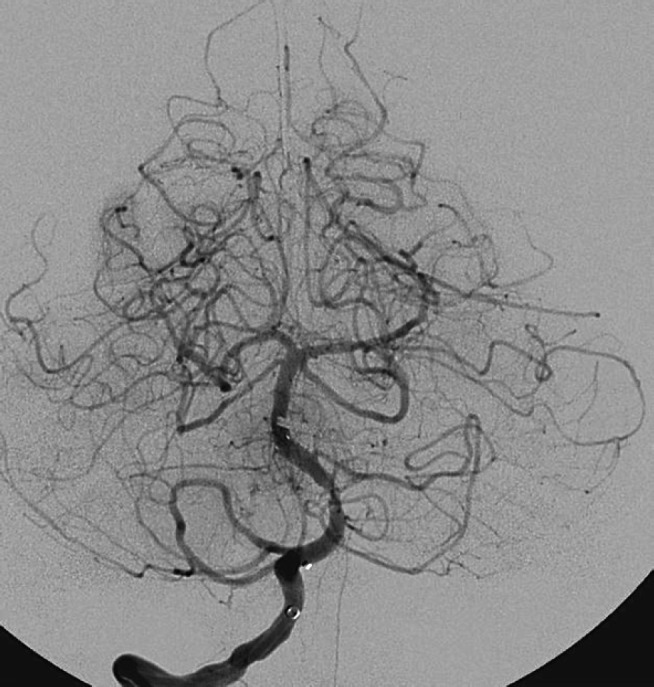
TICI 3 recanalization after 204 min from groin puncture. 53 × 56 mm (300 × 300 DPI).
Case 2
A 53-year-old male with hyperlipidemia presented with dizziness, dysarthria, and right hemiparesis (NIHSS = 7). There was no clear onset, but it had at least been 12 h since symptom recognition. No intravenous tPA was given as he presented out of the treatment window. Initial CT at presentation and a repeat CT 14 h after symptom recognition did not show an acute infarct. CT angiography showed a 4-mm area of severe narrowing of the mid third of the basilar artery. Groin puncture was done at 30 h after symptom recognition. Conventional angiogram showed 90% stenosis of the mid-basilar artery with persistent antegrade flow (Fig. 5), though with poor collaterals from the PCOMs: a small right PCOM and no left PCOM, with the former not showing filling of the PCA branches. The decision to treat was based on the degree of stenosis vis-à-vis the poor collaterals coming from the aforementioned PCOMs.
Fig. 5.
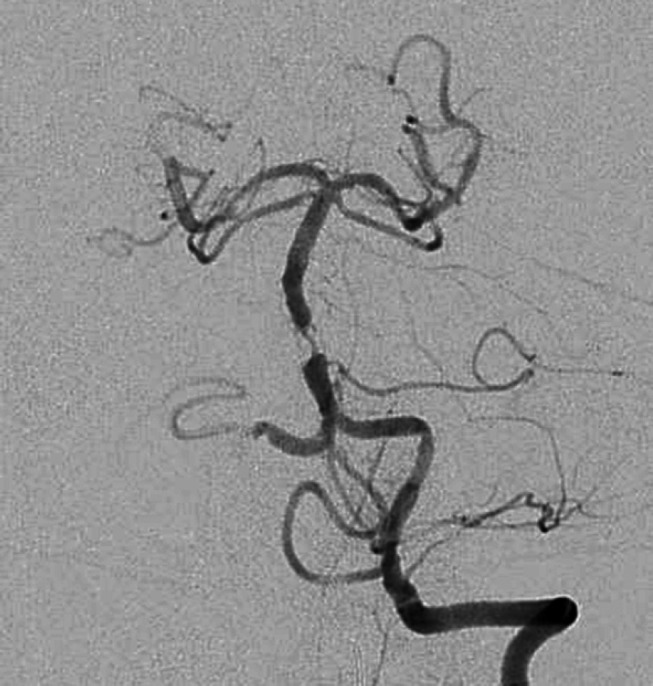
Digital subtraction angiography showing 90% of stenosis of the proximal to mid-portion of the basilar artery. 35 × 38 mm (300 × 300 DPI).
A 6-Fr NeuronMax sheath was advanced and positioned within the left subclavian artery. Under roadmap guidance, a 5-Fr Navien catheter was advanced, through which an SL-10 microcatheter over an exchange-length 0.014-inch Transcend wire was advanced to the basilar artery through the critically stenosed segment with the distal wire tip within the P2 segment of the right PCA (Fig. 6).
Fig. 6.
0.014-inch Transcend wire advanced through the stenosed segment with the distal wire tip in the right P2 segment. 38 × 59 mm (300 × 300 DPI).
Multiple strategies were employed for the stenosed basilar artery before stenting: 6 mg of intra-arterial tPA was given followed by balloon angioplasty, wherein the microcatheter was exchanged for a 2 mm × 9 mm noncompliant balloon microcatheter and was positioned within the stenosed segment. A total of 3 balloon inflations to 10 atm were carried out under fluoroscopic guidance. Angiography after angioplasty showed 70% stenosis (Fig. 7). Given that no sufficient dilatation could be achieved, the decision was made to deploy a stent.
Fig. 7.
Post-balloon angioplasty to 10 atm 3 times with no sufficient dilatation achieved. 37 × 41 mm (300 × 300 DPI).
A Prowler Select microcatheter was advanced over the indwelling wire into the basilar artery, and a 4 × 15 mm Solitaire device was electrolytically deployed with its distal end just proximal to the superior cerebellar artery (Fig. 8). There was a decrease in the degree of stenosis from 90% to 50% after stenting. Groin puncture to recanalization time was 303 min. He was discharged on POD 4 with an NIHSS score of 2. The patient had a follow-up on POD 30 with mild right hand weakness but had otherwise regained full strength throughout, though with residual dizziness.
Fig. 8.

4 × 15 mm Solitaire FR device electrolytically detached resulting in decrease in stenosis from 90% to 50%. 32 × 48 mm (300 × 300 DPI).
Discussion
The above reported cases illustrate that the Solitaire device can be electrolytically detached to effectively recanalize an occluded or stenotic basilar artery. Though the device is Food and Drug Administration (FDA) approved for use in thrombus retrieval, the FDA does not mention its use as an intracranial stent [14]. In both instances, the Solitaire device had to be detached, effectively working as an intracranial stent in the basilar artery after angiographic evidence of insufficient recanalization/dilatation after balloon angioplasty. Admittedly, Solitaire FR was the device used in both cases, as it was the only device available during that emergent period.
It is worth mentioning that the use of the Solitaire device as a stentriever came rather serendipitously. Perez et al. [15] reported its first use as a stentriever as other devices being used during that period were not available in their facility. The same group of authors also mentioned that it can be detached in the same manner as reported to restore flow in a target vessel. Duan et al. [16], in a series of 44 patients, recently demonstrated the safe and effective use of the Solitaire AB device as an intracranial stent in complex intracranial artery stenosis.
The authors are aware that intracranial stenting has been shown to have fairly high periprocedural complication rates at 15% [17, 18]. Notable of late is the strategy of submaximal angioplasty as a viable interventional treatment option for symptomatic intracranial artery disease. In a phase I study involving 24 patients [18], it has been shown to have a recurrent stroke rate of 0 and 5.55% at 30 days and 1 year, respectively, though the mean postangioplasty stenosis was 54.62% from a preangioplasty stenosis of 80.16%. Angioplasty was attempted in both cases in our small series, but vessel dilatation was not deemed to be sufficient at that time.
The authors are also aware that stenting would require a dual antiplatelet regimen at least temporarily with its attendant risks of hemorrhagic conversion of an acute stroke. It should be noted, however, that even patients who had angioplasty alone have been given dual antiplatelet agents for at least 3 months in 1 clinical trial for angioplasty with no patients having hemorrhage at 30-day follow-up [18]. In relation to our reported cases, the first case did have hemorrhage, though it must be mentioned that the patient had a supratherapeutic international normalized ratio at the time of the intervention and had recent strokes at that time as well.
The authors are cognizant of the results of the SAMMPRIS trial reporting that aggressive medical therapy is superior to stenting in preventing stroke and death [17]. Anterior circulation strokes, however, comprise 65% of the subjects in SAMMPRIS; hence, the superiority of the medical arm may not translate to those with vertebrobasilar stenosis. Treatment decisions based on stenosis location may thus be of benefit [19].
Ischemic strokes and transient ischemic attacks involving the posterior circulation comprise one fifth of all cerebrovascular ischemic events [20]. As compared to anterior circulation strokes, posterior circulation strokes may have a more aggressive natural history, manifesting as greater stroke recurrence. The Warfarin-Aspirin Symptomatic Intracranial Disease [19, 21] study group reported a 23% risk of stroke recurrence for posterior circulation strokes versus a 8% risk for anterior circulation strokes in patients on aspirin, while it was 10% versus 2% for posterior and anterior circulation stroke recurrence, respectively, in the warfarin group [19, 21].
As posterior circulation strokes tend to recur more, with potentially devastating clinical outcomes, aggressive treatment in the form of intracranial stenting for symptomatic intracranial artery disease may be warranted. The natural history of the Solitaire device used as an intracranial stent is unknown, and the appropriate clinical and angiographic scenario may be warranted before adopting this strategy.
Conclusion
The Solitaire FR device can be effectively detached and permanently deployed in the setting of acute basilar occlusion. The long-term effectiveness of this approach is unknown, however. It must also be noted that the Solitaire FR device is no longer available in many centers and that the current technology is not compatible with the technique described in this paper.
Statement of Ethics
Since this paper is a retrospective case series, it would not be possible to obtain consent at this point in time. The patients (or their representative) whose clinical courses are described in this series did give their consent for treatment at the time of presentation.
Disclosure Statement
The authors have no financial disclosures in reference to this paper.
References
- 1.Berkhemer OA, Puck SS, Fransen MD, Beumer D, van den Berg LA, Lingsma HF, et al. MR CLEAN Investigators A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornon J, et al. ESCAPE Trial Investigators Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 3.Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churiloy L, Yassi N, et al. EXTEND-IA Investigators Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–1018. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 4.Saver JL, Goyal M, Diener HC, Levy EI, Pereira VM, et al. SWIFT PRIME Investigators Stent-retriever thrombectomy after intravenous t-PA versus t-PA alone in stroke. N Engl J Med. 2015;372:2285–2295. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 5.Jovin TG, Chamorro A, Cobo E, de Miquel M, Molina CA, Rovira A, et al. REVASCAT Trial Investigators Thrombectomy within 8 h after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 6.Mourand I, Machi P, Milhaud D, Picot MC, Lobotesis K, Arquizan C, Costalat V, Héroum C, Sablot D, Bouly S, Lalu T, Bonafé A. Mechanical thrombectomy with the Solitaire device in acute basilar artery occlusion. J Neurointerv Surg. 2014;6:200–204. doi: 10.1136/neurintsurg-2012-010629. [DOI] [PubMed] [Google Scholar]
- 7.Andersson T, Kuntze Söderqvist Å, Söderman M, Holmin S, Wahlgren N, Kaijser M. Mechanical thrombectomy as the primary treatment for acute basilar artery occlusion: experience from 5 years of practice. J Neurointerv Surg. 2013;5:221–225. doi: 10.1136/neurintsurg-2011-010096. [DOI] [PubMed] [Google Scholar]
- 8.Roth C, Mielke A, Siekmann R, Ferbert A. First experiences with a new device for mechanical thrombectomy in acute basilar artery occlusion. Cerebrovasc Dis. 2011;32:28–34. doi: 10.1159/000324948. [DOI] [PubMed] [Google Scholar]
- 9.Mordasini P, Brekenfeld C, Byrne JV, Fischer U, Arnold M, Heldner MR, Lüdi R, Mattle HP, Schroth G, Gralla J. Technical feasibility and application of mechanical thrombectomy with the Solitaire FR revascularization device in acute basilar artery occlusion. AJNR Am J Neuroradiol. 2013;34:159–163. doi: 10.3174/ajnr.A3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espinosa de Rueda M, Parilla G, Zamarro J, García-Villalba B, Hernández F, Moreno A. Treatment of acute vertebrobasilar occlusion using thrombectomy with stent retrievers: initial experience with 18 patients. AJNR Am J Neuroradiol. 2013;34:1044–1048. doi: 10.3174/ajnr.A3329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005;76:1238–1241. doi: 10.1136/jnnp.2004.049924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miteff F, Faulder KC, Goh AC, Steinfort BS, Sue C, Harrington TJ. Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB): experience in 26 patients with acute cerebral artery occlusion. AJNR Am J Neuroradiol. 2011;32:1078–1081. doi: 10.3174/ajnr.A2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Costalat V, Machi P, Lobotesis K, Maldonado I, Vendrell JF, Riquelme C, Mourand I, Milhaud D, Héroum C, Perrigault PF, Arquizan C, Bonafé A. Rescue, combined, and standalone thrombectomy in the management of large vessel occlusion stroke using the Solitaire device: a prospective 50-patient single center study - timing, safety and efficacy. Stroke. 2011;42:1929–35. doi: 10.1161/STROKEAHA.110.608976. [DOI] [PubMed] [Google Scholar]
- 14.Department of Health and Human Services, Food and Drug Administration http://www.accessdata.fda.gov/cdrh_docs/pdf14/K141491.pdf.
- 15.Perez MA, Miloskavski E, Fischer S, Bäzner H, Henkes H. Intracranial thrombectomy using the Solitaire stent: a historical vignette. J Neurointervent Surg. 2012;4:e32. doi: 10.1136/neurintsurg-2011-010149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duan G, Feng Z, Zhang L, Zhang P, Chen L, Hong B, Xu Y, Zhao W, Liu J, Huang Q. Solitaire stents for the treatment of complex symptomatic intracranial stenosis after antithrombotic failure: safety and efficacy evaluation. J Neurointervent Surg. 2016;8:680–684. doi: 10.1136/neurintsurg-2015-011734. [DOI] [PubMed] [Google Scholar]
- 17.Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, Janis LS, Lutsep HL, Barnwell SL, Waters MF, Hoh BL, Hourihane JM, Levy EI, Alexandrov AV, Harrigan MR, Chiu D, Klucznik RP, Clark JM, McDougall CG, Johnson MD, Pride GL, Jr, Torbey MT, Zaidat OO, Rumboldt Z, Cloft HJ, SAMMPRIS Trial Investigators Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993–1003. doi: 10.1056/NEJMoa1105335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dumont TM, Sonig A, Mokin M, Eller JL, Sorkin GC, Snyder KV, Nelson Hopkins L, Levy EI, Siddiqui AH. Submaximal angioplasty for symptomatic intracranial atherosclerosis: a prospective phase I study. J Neurosurg. 2016;125:964–997. doi: 10.3171/2015.8.JNS15791. [DOI] [PubMed] [Google Scholar]
- 19.Kasner SE, Lynn MJ, Chimowitz MI, Frankel MR, Howlett-Smith H, Hertzberg VS, Chaturvedi S, Levine SR, Stern BJ, Benesch CG, Jovin TG, Sila CA, Romano JG. Warfarin vs aspirin for symptomatic intracranial stenosis: subgroup analyses from WASID. Neurology. 2006;67:1275–1278. doi: 10.1212/01.wnl.0000238506.76873.2f. [DOI] [PubMed] [Google Scholar]
- 20.Gulli G, Khan S, Markus HS. Vertebrobasilar stenosis predicts high early recurrent stroke risk in posterior circulation stroke and TIA. Stroke. 2009;40:2732–2737. doi: 10.1161/STROKEAHA.109.553859. [DOI] [PubMed] [Google Scholar]
- 21.Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S, Pessin MS, Weichel E, Sila CA, Furlan AJ. The warfarin-aspirin symptomatic intracranial disease study. Neurology. 1995;45:1488–1493. doi: 10.1212/wnl.45.8.1488. [DOI] [PubMed] [Google Scholar]


