Abstract
Background:
The process of becoming a mother is considered as an enjoyable and evolutionary event of women's life. However, due to physical and mental changes, it can be associated with some degree of stress and anxiety that may lead to mental health problems. This study aimed to compare the effects of mental health training during pregnancy on stress, anxiety, and depression between two groups of couples and pregnant women.
Materials and Methods:
This randomized clinical trial was conducted on 120 pregnant women referring to health centers in Isfahan, Iran, from September to February 2016. The participants were randomly divided into three groups: couples (with the partner present), pregnant women (without the partner present), and control group (routine care). After completing the pretest, the intervention groups received four sessions of pregnancy mental health training. Data were collected using the Depression, Anxiety, and Stress Scales (DASS-42) and a demographic characteristics form. The collected data were analyzed using Statistical Package for the Social Sciences software.
Results:
Before the intervention, no statistical difference was observed among the three groups in the mean scores of stress, anxiety, and depression. The mean score of depression, anxiety, and stress decreased significantly in the intervention groups 2 weeks after the intervention respectively (F=5.84, p=0.004), (F=14.76, p < 0.001) and (F=11.98, p < 0.001). No significant difference was observed between the couples and pregnant women groups in terms of depression (p = 0.140).
Conclusions:
The results of this study showed that mental health training for pregnant women, especially with the presence of the partner, is a useful intervention in preventing stress, anxiety, and depression.
Keywords: Anxiety, depression, Iran, mental health, pregnancy, stress, training
Introduction
The promotion of health and well-being in each period of a woman's life leads to a better life for her and has many benefits for the society. One of these life periods is pregnancy, which is a sensitive time for a woman.[1] Significant associations have been found between anxiety and depression and physical health during pregnancy.[2] The most common psychological disorders are related to anxiety and depression. Different researches have shown anxiety and depression in the form of a U-shaped relationship; and that anxiety and depression are increased in the first trimester and third trimester.[3] Numerous studies have reported undesirable mental health among women during pregnancy. Giardinelli et al. showed that the most important risk factor for depression and anxiety during pregnancy is conflict with the family and spouse.[4] In a study on 1447 pregnant women in Brazil, it was found that 28.8 and 16.6% of them suffered from depression and anxiety, respectively.[5] A systematic review of studies related to prenatal depression in Iran in 1997–2011 showed that 27.62% of pregnant women suffer from depression.[6] In fact, the intrauterine environment is continuously affected by the emotions and mental state of the mother.[7] The adverse effects include miscarriage, low birth weight,[8] nausea, vomiting, preeclampsia,[9,10] lower cognitive performance and increased fearfulness,[11] increased episiotomy infections and infection of newborns,[12] hyperactive children, irritability and difficulty in eating and sleeping,[13,14] increased fetal heart rate,[15] decreased mental development at age 2,[16] preterm delivery,[4] future emotional disorders,[17] and prolonged labor.[18] Maintaining the mental health of pregnant women is an important factor in the stability of the family and community, and an important strategy in this regard is the contribution of the spouse to this important issue.[19] The study by Karamoozian showed that psychological therapists in health centers can be used to improve the mental health of women during pregnancy.[20] The findings of other studies showed that psycho education training programs can be used to reduce anxiety and depression in pregnant women and promote mental health.[21,22,23,24] Hitherto, the studies in this field have been focused on pregnant women and not enough attention has been paid to their husbands. Researchers, globally, have focused on the participation of men in issues such as family planning, sexually transmitted diseases, and HIV and not enough attention has been paid to their role in other aspects of women's health, such as pregnancy and childbirth.[25] Due to the importance of mental health in pregnancy, the present study was conducted to assess the effects of mental health training program on stress, anxiety, and depression during pregnancy.
Materials and Methods
This clinical trial was conducted with the code IRCT2016012426174N1 on 120 pregnant women referring to health centers in Isfahan, Iran, from September to February 2016. The participants were selected through convenient sampling, and then, randomly divided into three groups of couples (with the presence of the partner), pregnant women (without the presence of the partner), and control group (routine care). Sample size was calculated to be 34 pregnant women in each group, but was increased to 40 individuals considering possible dropouts (β = 0.05), (z1 = 1.96, z2 = 0.84).
The inclusion criteria consisted of primiparity, gestational age of 28–32 weeks, spouses' literacy, adequate physical and physiological health to actively attend the class, and lack of severe problems in obstetrics, chronic diseases, any psychological diseases, and an unwanted pregnancy. The exclusion criteria consisted of absence of the pregnant women or their spouse from educational sessions in the study groups, serious illness or problem during the study, occurrence of a specific disease or problem contraindicating pregnant women's attendance of the study, and the need for complete bed rest.
The content of the mental health training course during pregnancy was prepared based on the available textbooks and literature, and its content validity was determined by midwifery and psychology professors. The training course content included information such as the definition of mental health and its importance during pregnancy, the impact of mental disorders on pregnancy outcome, the role of husbands in the mental health of pregnant women, marital communication skills, problem-solving skills, breathing techniques, muscle relaxation techniques, stages of vaginal delivery, pain-relief methods, physiological delivery and readiness for accepting the role of parents, and newborn care and breast feeding.
In the intervention groups, four training sessions (lasting 2 h) were held during 4 weeks (once a week). At the end of each session, pregnant women were given homework exercises using CDs and pamphlets. Follow-up was conducted by telephone during the week. The control group received routine care in the health care center. Data were collected using the Depression, Anxiety, and Stress Scales (DASS-42) and a demographic characteristics form. The questionnaires were completed in two stages for all participants in the study groups: before the intervention and 2 weeks after the intervention.
Data were collected using the DASS-42. DASS-42 was prepared in 1995 by Lovebird that includes 42 questions that assess stress, anxiety, and depression, each with 14 different questions. Test–retest reliability has been, respectively, reported as 0.80, 0.76, and 0.77 for the depression, anxiety, and stress scales, and Cronbach's alpha of the depression, anxiety, and stress scales have been reported as 0.8, 10.74, and 0.78, respectively. The questions are scored based on a four-point Likert scale ranging from 0 to 3 (from never to always). The maximum score on each scale is equal to 42.[26] After obtaining informed consents from the participants, questionnaires were completed by all subjects before and 2 weeks after the intervention. Data were analyzed using Chi-square test, Kruskal–Wallis test, repeated measures analysis of variance (ANOVA), and one-way ANOVA in Statistical Package for the Social Sciences (SPSS) software (version 18, SPSS Inc., Chicago, IL, USA).
Ethical considerations
The present study was approved by the Ethical Committee of Isfahan University of Medical Sciences, Isfahan IR.MUI.REC.1394.3.556 (394556). The research design, method of education, confidentiality of data, and the study goal were explained to the subjects, and they were asked to sign a written consent form to enter the study. Those who had a score of higher than 18, 9, and 13 in the stress, anxiety, and depression scales, respectively, and those who had suicidal thoughts were excluded from the study and referred to a psychiatrist.
Results
In this study, a total of 16 training sessions were held. ANOVA and Chi-square test showed that there was no significant difference among the three groups in terms of demographic characteristics. One-way ANOVA showed that before the intervention there was no statistically significant difference among the three groups in terms of the mean scores of anxiety, depression, and stress.
There was no significant difference in the mean score of anxiety in the control group before and after the intervention (p = 0.680). However, in the pregnant women group and couples group, the average anxiety score of pregnant women after the intervention was significantly lower than before the intervention (p < 0.001) [Table 1]. In the control group, the mean stress score of pregnant women before and after the intervention was not significantly different (p = 0.77). Nevertheless, in the pregnant women group (p < 0.001) and couples group (p < 0.001), the mean stress score of pregnant women was significantly lower after the intervention compared to before the intervention [Table 2]. Moreover, paired t-test showed that, in the control group, the mean depression score of pregnant women was not significantly different before and after the intervention (p = 0.580). However, in the pregnant women group (p < 0.001) and couples group (p < 0.001), the mean depression score of pregnant women after the intervention was significantly lower than before the intervention [Table 3]. ANOVA showed a significant difference among the three groups after the intervention. Least significant difference (LSD) showed that after the intervention, mean anxiety score of the pregnant women group was significantly lower than that of the control group (p = 0.002) and this score was significantly lower in the couples group than that in the pregnant women group (p = 0.045) [Table 1].
Table 1.
Comparison of anxiety scores before and after the intervention between and within groups
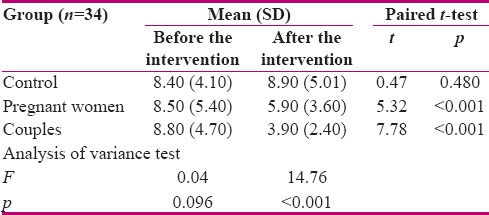
Table 2.
Comparison of stress scores before and after the intervention between and within groups
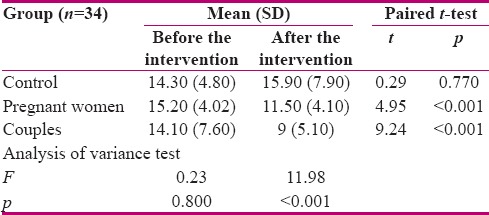
Table 3.
Comparison of depression scores before and after the intervention between and within groups
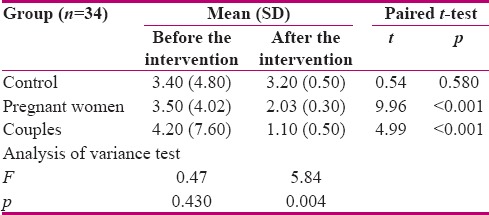
Furthermore, LSD showed that after the intervention the mean stress score of the pregnant women group was significantly lower than the control group (p = 0.003) and in the couples group it was significantly lower than the pregnant women group (p = 0.038) [Table 2]. In addition, the mean depression score differed significantly among the three groups (p = 0.004). LSD showed that after the intervention the mean depression score of the pregnant women group (p = 0.028) and the couples group (p = 0.001) was significantly lower than the control group. However, no significant difference was observed between the two intervention groups in terms of mean depression score (p = 0.140) [Table 3].
Discussion
This study was conducted to compare the effect of mental health training during pregnancy on stress, anxiety, and depression in two groups of couples and pregnant women. The results of this study showed that the mentioned training in the intervention groups, especially the couples group, significantly improved the domains of mental health of pregnant women. The mean score of anxiety, stress, and depression in the two intervention groups was significantly lower after the intervention compared to before the intervention.
In explanation of these results, it can be said that most pregnant women have many fears and concerns during pregnancy which cause anxiety and stress.[20] Moreover, the experience of pregnancy in a woman's life can be considered as a situation tension. Anxiety in pregnant women can cause problems for the mother and fetus. This applies especially to nulliparous women who are not well prepared for these problems.[21] In the training sessions, the researchers tried to present skills which can improve mental health. The participants stated that if their mental health problems during pregnancy are resolved, they will experience lower stress levels during pregnancy. This finding was in agreement with that of the study by Bloom et al.[27] Researchers performed a mental health intervention among 235 pregnant women in Belgium and found that the implementation of this intervention resulted in the improvement of women's anxiety.[28] Moreover, in the present study, anxiety and stress were significantly lower in the couples group than the pregnant women group after the intervention; however, no significant difference was observed between these two groups in terms of depression.
In explanation of these results, it can be said that, in the couples group, the presence of the husband reinforced learning and the correct functioning of the educational materials. The findings of the present research were consistent with the results of the studies by Shobeiri et al.,[24] Delaram and Shams,[8] Seyed Ahmadi Nejad et al.,[18] and Jabbari et al.[22] In this regard, a psychological intervention was conducted in Australia on 1410 pregnant women and improved their mental health.[29] The findings of this study were consistent with that of the study by Karamoozian.[20]
Although mental health training interventions improved stress and anxiety in pregnant women group, the mean score of anxiety and stress was higher in the couples group after the intervention. Therefore, the researchers suggest that couples educational programs should be considered by health provider as a means to reduce the psychological stress of pregnancy. According to this study, it seems that support from the husband is effective in the promotion of mental health in pregnant women. A limitation of this study was the possible effect of individual differences on stress, depression, and anxiety, though the researchers tried to control the impact of individual differences to some extent through random assignment.
Conclusion
Based on the results of this study, it can be concluded that educational interventions during pregnancy, especially in couples, improve maternal mental health during pregnancy through decreasing anxiety, stress, and depression. It is suggested that greater emphasis be placed on the impact of mental health program training on stress, anxiety, and depression during pregnancy, especially with the presence of the husband.
Financial support and sponsorship
Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
Nothing to declare.
Acknowledgement
This article was derived from a Master Degree thesis with project Cod:13943556, Isfahan University of Medical Sciences, Isfahan, Iran.
References
- 1.Sharifi N, Jalili L, Najar S, Yazdizadeh H, Haghighizadeh MH. Survey of general health and related factors in menopausal women in Ahvaz city, 2012 ;21:59-65. Razi Journal of Medical Sciences. 2015;21:59–65. [In Persian] [Google Scholar]
- 2.Rubertsson C, Hellström J, Cross M, Sydsjö G. Anxiety in early pregnancy: Prevalence and contributing factors. Arch Womens Ment Health. 2014;17:221–8. doi: 10.1007/s00737-013-0409-0. [DOI] [PubMed] [Google Scholar]
- 3.Basharpoor S, Heydarirad H, Atadokht A, Daryadel SJ, Nasiri-Razi R. The role of health beliefs and health promoting lifestyle in predicting pregnancy anxiety among pregnant women. Iranian Journal of Health Education and Health Promotion. 2015;3:171–80. [In Persian] [Google Scholar]
- 4.Giardinelli L, Innocenti A, Benni L, Stefanini M, Lino G, Lunardi C, et al. Depression and anxiety in perinatal period: Prevalence and risk factors in an Italian sample. Arch Womens Ment Health. 2012;15:21–30. doi: 10.1007/s00737-011-0249-8. [DOI] [PubMed] [Google Scholar]
- 5.Karami K, Mardani A, ShakeriNejad G, Saki A. Effectiveness of a codified educational behavioral program on the mental health of pregnant women. The Journal of Shahid Sadoughi University of Medical Sciences. 2015;23:879–89. [In Persian] [Google Scholar]
- 6.Sajadi H, Vameghi M, Setare forozan A, Rafiey H, Ohgheghee Kamal S, Nosrat abadi M. Prevalence, risk factors and interventions of depression during pregnancy in Iranian studies (1997-2011): A systematic review. Journal of North Khorasan University of Medical Sciences. 2013;5:521–30. [In Persian] [Google Scholar]
- 7.Abdollahzade Rafi M, Hassanzadeh M, Ahmadi S, Taheri M, Hosseini M. Relationship between social support with depression and anxiety during third trimester pregnancy. Iranian Journal of Nursing Research. 2012;7:1–10. [In Persian] [Google Scholar]
- 8.Delaram M, Shams S. The effect of foetal movement counting on maternal anxiety: A randomised, controlled trial. J Obstet Gynaecol. 2016;36:39–43. doi: 10.3109/01443615.2015.1025726. [DOI] [PubMed] [Google Scholar]
- 9.Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women and Birth. 2015;28:179–93. doi: 10.1016/j.wombi.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Schetter CD, Tanner L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25:141. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35. doi: 10.1016/j.bpobgyn.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Dolatian M, Mirabzadeh A, Forouzan AS, Sajjadi H, Majd HA, Moafi F. Preterm delivery and psycho-social determinants of health based on World Health Organization Model in Iran: A narrative review. Global J Health Sci. 2013;5:52. doi: 10.5539/gjhs.v5n1p52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ding XX, Wu YL, Xu SJ, Zhu RP, Jia XM, Zhang SF, et al. Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103–10. doi: 10.1016/j.jad.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 14.Darwin Z, McGowan L, Edozien LC. Antenatal mental health referrals: Review of local clinical practice and pregnant women' s experiences in England. Midwifery. 2015;31:e17–22. doi: 10.1016/j.midw.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Bayrami M, Zahmatyar H, Bahadori KJ. Prediction strategies to coping with stress in the pregnancy women with first experience on the based factors hardiness and social support. 2013 [In Persian] [Google Scholar]
- 16.Davis EP, Sandman CA. Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology. 2012;37:1224–33. doi: 10.1016/j.psyneuen.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sabooteh SS, Sharifirad GH, Hassanzadeh A. Fathers' subjective norms, normative beliefs and motivation to comply regarding prevention of children tendency toward addictive drugs. J Health Syst Res. 2014:1746–56. [In Persian] [Google Scholar]
- 18.Seyed Ahmadi Nejad FS, Golmakani N, Shakeri MT. Effect of progressive muscle relaxation on depression, anxiety, and stress of primigravid women. Evidence Based Care. 2015;5:67–76. [In Persian] [Google Scholar]
- 19.Mortazavi F, Mirzaii K. Reason of, barriers to, and outcomes of husbands' involvement in prenatal and intrapartum care program based on midwives' experiences: A qualitative study. Arak Medical University Journal. 2012;15:104–15. [In Persian] [Google Scholar]
- 20.Karamoozian M. Effectiveness of cognitive-behavioral stress management intervention on anxiety and depression during pregnancy. Journal of Kerman University of Medical Sciences. 2014;20:606–21. [In Persian] [Google Scholar]
- 21.Rafiee B, Akbarzade M, Asadi N, Zare N. Comparison of attachment and relaxation training effects on anxiety in third trimester and postpartum depression among primipara women. Journal of Hayat. 2013;19:76, 88. [In Persian] [Google Scholar]
- 22.Jabbari Z, Hashemi H, Haghayegh SA. Survey on effectiveness of cognitive behavioral stress management on the stress, anxiety, and depression of pregnant women. 2012 [In Persian] [Google Scholar]
- 23.Mahmoodi H, Babazadeh T, Shirzadi S, Mohammadi Y, Sharifi-Saqezi P, Mulodirad N. Health promotion behavior in pregnant women referred to prenatal care unit of Imam Khomeini Hospital of Saqqez. Journal of Education and Community Health. 2015;1:58–65. [In Persian] [Google Scholar]
- 24.Shobeiri F, Taravati-Javad M, Soltani F, Karami M. Effects of progressive muscle relaxation counseling on anxiety among primigravida women referred to health care centers in Hamadan. Journal of Education and Community Health. 2015;2:1, 9. [In Persian] [Google Scholar]
- 25.Rabieipoor S, Khodaei A, Radfar M. The relationship between husbands' participation in prenatal care and mental health of pregnant women referred to health centers in Urmia, 1392. Journal of Urmia Nursing And Midwifery Faculty. 2015;13:338, 47. [In Persian] [Google Scholar]
- 26.Pahlavanzadeh S, Yazdani M. The effect of psycho-education on depression, anxiety and stress in family caregivers of patients with mental disorders. Journal of Kermanshah University of Medical Sciences. 2010;14 [In Persian] [Google Scholar]
- 27.Bloom TL, Bullock LF, Parsons L. Rural pregnant women's stressors and priorities for stress reduction. Issues Ment Health Nurs. 2012;33:813–9. doi: 10.3109/01612840.2012.712087. [DOI] [PubMed] [Google Scholar]
- 28.Bogaerts A, Devlieger R, Nuyts E, Witters I, Gyselaers W, Van den Bergh B. Effects of lifestyle intervention in obese pregnant women on gestational weight gain and mental health: A randomized controlled trial. Int J Obes (Lond) 2013;37:814–21. doi: 10.1038/ijo.2012.162. [DOI] [PubMed] [Google Scholar]
- 29.Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. Effects of a midwife psycho-education intervention to reduce childbirth fear on women's birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;15:284. doi: 10.1186/s12884-015-0721-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


