Abstract
Background:
Maxillofacial tumours in children and adolescents have been documented worldwide; however, few studies were reported from Africa, especially sub-Saharan Africa. In Nigeria, most of the studies emanated from the Southwest region.
Aim:
To present an audit of clinicopathologic features and treatment of orofacial tumours in children and adolescents in Sokoto, Northwest Nigeria.
Patients and Methods:
Clinicopathologic records of the Departments of Dental and Maxillofacial Surgery, Paediatrics and Histopathology, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria, were reviewed for all the oral and maxillofacial tumours managed in children <19 years from January 2011 to December 2015.
Results:
Two hundred and twenty-two tumours were noted in all age groups during the study duration and 75 (33.8%) of these occurred in children and adolescents. A total of 45 (60%) males and thirty (40%) females constitute the patient population with a male to female ratio of 1.5:1. There are 32 (42.7%) benign tumours and 43 (57.3%) malignant tumours. Burkitt's lymphoma was the most common malignant tumour in 24 cases (55.8%), whereas pleomorphic adenoma was the most common benign soft tissue tumour in 4 cases (30.8%) and fibro-osseous lesions were the most common benign jaw tumours in 10 cases (52.6%). Chemotherapy alone was the treatment modality in 24 cases of malignant tumour whereas 13 cases had combination chemotherapy and irradiation.
Conclusions:
Our findings established that oral and maxillofacial tumours in children and adolescents are quite common in Sokoto, Northwest region of Nigeria, particularly the malignant types. There is a need for improved universal healthcare insurance for all citizens to adequately manage these children effectively.
Keywords: Adolescents, Burkitt's lymphoma, chemoradiation, chemotherapy, children, orofacial, pleomorphic adenoma, tumours
INTRODUCTION
Orofacial tumours are a diverse group of pathologic disorders with various histological types and clinical behaviour.[1] They are said to be seen in all age groups and gender and can include hamartomas, congenital overgrowth or true neoplasms.[2] These tumours might result in the destruction of facial bone with compromise to the airway and digestive system and adjacent structures when neglected.[3] Environmental factors such as viral infection, chronic malnutrition, trauma, alcohol and tobacco intake have been fingered in the aetiopathogenesis of these maxillofacial tumours;[4] however, genetic background has been suggested.[5] About 3%–10% of head and neck tumours have been reported to occur in children and adolescents worldwide.[2,6,7]
Several reports of maxillofacial tumours in children and adolescents have been documented worldwide;[2,8,9,10,11] however, few studies were reported from Africa, especially sub-Saharan Africa.[8,12,13] In Nigeria, most of the studies emanated from the Southwest region.[4,13]
To the best of our knowledge, no data on clinicopathologic features and treatment of orofacial tumours in children and adolescents in Sokoto, Northwest of Nigeria. The current study analysed 75 cases of these neoplasms regarding the age and gender distribution, incidence, histopathologic type, site of tumour and treatment.
PATIENTS AND METHODS
The histopathology and clinical records of the Departments of Dental and Maxillofacial Surgery, Paediatrics and Histopathology, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria, were reviewed for all the oral and maxillofacial tumours seen and managed in children and adolescent <19 years from January 2011 to December 2015. Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria is the biggest tertiary referral centre in Sokoto state. It served a largely remote rural population of over six million people in Sokoto and other neighbouring states of Kebbi, Zamfara, Niger and Katsina and two neighbouring Countries (the Republic of Benin and the Republic of Niger) with land mass spanning more than 25.973 km2. In addition, the hospital has a functional linear accelerator radiotherapy machine with consultants’ radio-oncologists and nuclear physicists.
The data were subjected to analysis of age, sex, site of tumour, histopathologic type and treatment given. The age of the patients was divided into four groups: Group 1 (0–5 years), Group 2 (6–10 years), Group 3 (11–15 years) and Group 4 (16–19 years) as described by authors of similar studies.[4,12] Data were analysed using SPSS for Window version 20.0 (Armonk, NY: IBM Corporation, NY, USA). Results were presented as simple frequencies and descriptive statistics. Cross tabulation was done to find differences between groups. P < 0.05 was considered statistically significant.
RESULTS
Based on the findings, 222 tumours were noted in all age groups during the study duration and 75 (33.8%) of these occurred in children and adolescents. A total of 45 (60%) males and thirty (40%) females constitute the patient population with a male to female ratio of 1.5:1. Only age group of 15–19 had fewer male patients i.e., seven (38.9%); all other age groups have more boys than girls [Table 1]. Patient's ages ranged from 2 years to 19 years. There was a higher incidence of malignant maxillofacial tumours in both sexes (25 [55.6%] males and 18 [60%] females). The age group of 10–14 had the highest cases of malignant maxillofacial tumours i.e., 23 (76.7%), whereas the age group of 15–19 had the highest cases of benign tumours 16 (88.9%) [Table 2]. Burkitt's lymphoma was the most common malignant tumour in the series with 14 (58.3%) cases in the age group of 5–9 and ten (41.7%) cases in the age group of 10–14. Rhabdomyosarcoma was the second most common malignant tumour with seven (70%) cases in the age group of 10–14, two (20%) cases in the age group of 5–9 and one (10%) case in the age group of 0–4 [Table 3]. Only five cases of mucoepidermoid carcinoma presented with three (60%) cases in the 10–14 age group and two (40%) cases in the 15–19 age group [Table 3]. There was statistically significant difference between age and type of tumour (P = 0.000) as malignant tumours are more common in the age groups of 10–14 years. However, there is no significant difference between sex and tumour types (P = 0.703). Pleomorphic adenoma was the most common benign soft tissue tumour in four cases (30.8%) and three cases were seen in the adolescent age group of 15–19 years and only one case in the age group of 5–9 years [Table 4]. Fibro-osseous lesions constitute the most common benign jaw tumours seen in our series with five (26.3%) cases each of fibrous dysplasia and ossifying fibroma. Four (80%) cases of fibrous dysplasia presented in the age group of 5–9 years, while only one (20%) case presented in the 10–14 years age group. All the five (26.3%) cases of ossifying fibroma presented in the 15–19 years age group [Table 5]. Only four (21.1%) cases of odontogenic tumours presented, with three (15.8%) cases of ameloblastoma (one case each in the 5–9 years, 10–14 years and 15–19 years age groups) and only one (5.3%) case of adenomatoid odontogenic tumour [Table 5].
Table 1.
Distribution of age group and sex of patients
| Age group | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| 0-4 | 2 (100.0) | 0 | 2 (100) |
| 5-9 | 16 (64.0) | 9 (36.0) | 25 (100) |
| 10-14 | 20 (66.7) | 10 (33.3) | 30 (100) |
| 15-19 | 7 (38.9) | 11 (61.1) | 18 (100) |
| Total | 45 (60.0) | 30 (40.0) | 75 (100) |
Table 2.
Distribution of sex and age group with tumour type
| Benign (%) | Malignant (%) | Total (%) | |
|---|---|---|---|
| Sex | |||
| Male | 20 (44.4) | 25 (55.6) | 45 (100) |
| Female | 12 (40.0) | 18 (60.0) | 30 (100) |
| Total | 32 (42.7) | 43 (57.3) | 75 (100) |
| Age group | |||
| 0-4 | 1 (50.0) | 1 (50.0) | 2 (100) |
| 5-9 | 8 (32.0) | 17 (68.0) | 25 (100) |
| 10-14 | 7 (23.3) | 23 (76.7) | 30 (100) |
| 15-19 | 16 (88.9) | 2 (11.1) | 18 (100) |
| Total | 32 (42.6) | 43 (57.4) | 75 (100) |
Table 3.
Age group distribution of 43 maxillofacial malignant jaw tumours
| Tumours | Age groups (years) | Total (%) | |||
|---|---|---|---|---|---|
| 0-4 | 5-9 | 10-14 | 15-19 | ||
| Lymphomas | |||||
| Burkitt’s lymphoma | 0 | 14 | 10 | 0 | 24 (55.8) |
| Sarcomas | |||||
| Rhabdomyosarcomas | 1 | 2 | 7 | 0 | 10 (23.3) |
| Osteosarcomas | 0 | 0 | 3 | 0 | 3 (7.0) |
| Carcinomas | |||||
| Mucoepidermoid carcinoma | 0 | 0 | 3 | 2 | 5 (11.6) |
| Others | |||||
| Malignant peripheral nerve sheath tumour | 0 | 1 | 0 | 0 | 1 (2.3) |
| Total | 1 | 16 | 23 | 2 | 43 (100.0) |
Table 4.
Age group distribution of 13 maxillofacial benign soft tissue tumours
| Tumours | Age group (years) | Total (%) | |||
|---|---|---|---|---|---|
| 0-4 | 5-9 | 10-14 | 15-19 | ||
| Vascular | |||||
| Capillary haemangioma | 0 | 0 | 1 | 0 | 1 (7.7) |
| Angiofibroma | 0 | 0 | 1 | 0 | 1 (7.7) |
| Salivary gland | |||||
| Pleomorphic adenoma | 0 | 1 | 0 | 3 | 4 (30.8) |
| Others | |||||
| Heck’s disease | 1 | 1 | 0 | 0 | 2 (15.3) |
| Chronic inflammation | 0 | 1 | 0 | 0 | 1 (7.7) |
| Fibroepithelial polyp | 0 | 0 | 1 | 0 | 1 (7.7) |
| Fibrous epulis | 0 | 0 | 0 | 1 | 1 (7.7) |
| Pyogenic granuloma | 0 | 0 | 0 | 1 | 1 (7.7) |
| Plasma cell mucositis | 0 | 0 | 0 | 1 | 1 (7.7) |
| Total | 1 | 3 | 3 | 6 | 13 (100) |
Table 5.
Age group distribution of 19 benign jaw tumours
| Tumours | Age group (years) | Total (%) | |||
|---|---|---|---|---|---|
| 0-4 | 5-9 | 10-14 | 15-19 | ||
| Odontogenic tumour | |||||
| Ameloblastoma | 0 | 1 | 1 | 1 | 3 (15.8) |
| Adenomatoid odontogenic tumour | 0 | 0 | 1 | 0 | 1 (5.3) |
| Odontogenic cyst | |||||
| Dentigerous cyst | 0 | 0 | 2 | 1 | 3 (15.8) |
| Odontogenic keratocyst | 0 | 0 | 0 | 2 | 2 (10.5) |
| Fibro-osseous lesions | |||||
| Fibrous dysplasia | 0 | 4 | 0 | 1 | 5 (26.3) |
| Ossifying fibroma | 0 | 0 | 0 | 5 | 5 (26.3) |
| Total | 0 | 5 | 4 | 10 | 19 (100.0) |
Among the 75 cases of maxillofacial tumours recorded, there are 32 (42.7%) benign tumours and 43 (57.3%) malignant tumours. Burkitt's lymphoma was the most common malignant tumour 24 (55.8%) whereas pleomorphic adenoma was the most common benign soft tissue tumour four (30.8%) and fibro-osseous lesions were the most common benign jaw tumours ten (52.6%). The most common odontogenic tumour was ameloblastoma, whereas dentigerous cyst was the most common odontogenic cyst.
There were more cases of malignant tumours in the mandible and maxilla i.e., 22 (66.7%) and 16 (66.7%), respectively, as compared to benign tumours i.e., 11 (33.3%) and 8 (33.3%), respectively. All the cases of pleomorphic adenoma were seen in the parotid gland [Table 6].
Table 6.
Site distribution of maxillofacial benign and malignant tumours
| Site | Benign (%) | Malignant (%) | Total (%) |
|---|---|---|---|
| Cheek | 1 (100.0) | 0 | 1 (100) |
| Gingivae | 2 (100.0) | 0 | 2 (100) |
| Labial mucosa | 2 (100.0) | 0 | 2 (100) |
| Lower lip | 4 (100.0) | 0 | 4 (100) |
| Mandible | 11 (33.3) | 22 (66.7) | 33 (100) |
| Mandible + abdomen | 0 | 2 (100.0) | 2 (100) |
| Maxilla | 8 (33.3) | 16 (66.7) | 24 (100) |
| Maxilla + abdomen | 0 | 1 (100.0) | 1 (100) |
| Maxilla + orbit | 0 | 2 (100.0) | 2 (100) |
| Parotid | 4 (100.0) | 0 | 4 (100) |
| Total | 32 (42.7) | 43 (57.3) | 75 (100) |
Chemotherapy alone was the treatment modality in 24 cases of malignant tumour whereas 13 cases had combination chemotherapy and irradiation. This was statistically significant as most of the malignant cases were treated (P = 0.000). All the six patients that were discharged against medical advice are cases of malignancies [Table 7]. The two cases of resection done were the case of ameloblastoma in the adolescence age groups. Silver nitrate application was used in the treatment of the two cases of Heck's disease. All the cases of ossifying fibroma were treated with shelling out of lesion. The fibrous dysplasia that presented in the age group of 5–9 years were observed while that in the age group of 15–19 years was paired down.
Table 7.
Distribution of treatment modalities of maxillofacial tumours
| Treatment | Benign (%) | Malignant (%) | Total (%) |
|---|---|---|---|
| Chemo-radiation | 0 | 13 (100.0) | 13 (100) |
| Chemo-therapy | 0 | 24 (100.0) | 24 (100) |
| Discharged against medical advice | 0 | 6 (100.0) | 6 (100) |
| Enucleation and curettage | 7 (100.0) | 0 | 7 (100) |
| Excision | 10 (100.0) | 0 | 10 (100) |
| Observation | 5 (100.0) | 0 | 5 (100) |
| Pairing down | 1 (100.0) | 0 | 1 (100) |
| Resection | 2 (100.0) | 0 | 2 (100) |
| Shelling out | 5 (100.0) | 0 | 5 (100) |
| Silver nitrate application | 2 (100.0) | 0 | 2 (100) |
| Total | 32 (42.7) | 43 (57.3) | 75 (100) |
DISCUSSION
Information on clinical features of pathologic disorders such as tumours including primary site, age, sex distribution and treatment given is important for overall patient management. It is also necessary for review of treatment options and prognosis. Studies have been carried out in other regions of Nigeria on oral and maxillofacial tumours in children and adolescents; however, to the best of our knowledge, data on oral and maxillofacial neoplasms in these age groups are not available in Sokoto, Northwest Nigeria. We found that 254 tumours were noted in all age groups with 75 (33.9%) occurring in children and adolescents. This percentage is higher than that published by Aregbesola et al.[4] and Arotiba[13] from Southwest of Nigeria where they reported 28% and 20%, respectively. Other researchers have reported lower percentages ranging from 7% to 17%.[14,15,16] The reasons for this difference are fairly due to the diverse age and pathologic lesions included because in some studies, reactive and viral lesions are considered as neoplasm.[11,15,17] This high percentage recorded in this region of Nigeria could not be explained; however, we opined that influx of other nationals into this region of the country may be a contributing factor.
Several studies[9,15,18] have reported a male preponderance while others have disagreed.[2,14] We found an overall male preponderance of ratio 1.4:1 which agrees to findings of Aregbesola et al.[4] Most reports[9,10,11,13,14,19] have found a higher percentage of benign tumours in the child and adolescence age groups; however, we found a high percentage of malignant tumour (57.3%) in our series. This finding agrees with some studies in Nigeria where malignant tumours are more than benign tumours.[4,18] The reason for this high malignant tumour in African populations is due to the high prevalence of endemic Burkitt's lymphoma among paediatric patients.[4,15,18] Similar to earlier reports from Nigeria,[4,15] Burkitt's lymphoma constitutes the highest number of malignant tumours (58.3%) seen from the current study. Rhabdomyosarcoma was the other common malignant neoplasm seen in this series constituting 23.3% of all cases of malignancy in the paediatric population. This finding has also been reported by Aregbesola et al.[4] and Jaafari-Ashkavandi and Ashraf.[1] Rhabdomyosarcoma has been thought to have predilection for the head and neck region in paediatric population.[20]
Our result showed that pleomorphic adenoma was the most frequent benign nonodontogenic soft tissue tumour in paediatric age group with location in the parotid gland only. This finding has been reported in African population by Elarbi et al.[10] in Libyan paediatric population and Aregbesola et al.[4] in Nigerian paediatric population. This finding, however, is in contrary to other studies from Western countries where vascular anomalies, especially haemangiomas were most frequent.[7,9,21] Vascular malformations are considered developmental by some authorities[22] while some regard them as hamartomas of blood vessels.[23] The rarity of vascular malformations in African population is still a subject of research.
In agreement with other Nigerian studies,[12,13,15] ameloblastoma was the most frequent odontogenic tumour seen in this series. This, however, differs from other studies were odontoma was the most common odontogenic tumour.[9,11,16] Odontomas are often regarded as dental hamartomas, rather than odontogenic neoplasms.[9,24] Most odontomas are symptomless and usually discovered on routine radiographs.[25] Genetic factors have been suggested as a possible reason.[4] Odontogenic tumours in children are known to have predilection for the mandible,[11,15,16] this was corroborated by our findings. Ulmansky et al.[14] found out that odontogenic myxoma was the most common odontogenic tumour in children in their series. It was also observed from our series that all the odontogenic tumours and cysts occurred in children above the age of 5 years with majority in the adolescent age group. This finding is consistent with other studies.[9,16] Since odontogenic tumours are thought to arise from tooth germs,[3] and crown formation terminates at 4 or 5 years of age in most of the fully formed crowns.[16] This reinforced the idea that the bulk of odontogenic tumours arise from dormant remnants of the tooth germ.[9]
Fibrous dysplasia and ossifying fibroma were the most common benign nonodontogenic jaw tumour accounting for ten (52.6%) of all the benign jaw tumours. This finding agrees with earlier reports.[4,26] Majority of the fibrous dysplasia occurred in the 5–9 years age group, while all the cases of ossifying fibroma occurred in the age group of 15–19 years. Since fibrous dysplasia is a developmental lesion in the fibro-osseous lesion group[27] secondary to mutations in the gene (GNAS I) encoding for the α-subunit of a signal transducing G-protein (Gs-α) leading to increased c-AMP production affecting proliferation and differentiation of preosteoblasts,[28,29,30] one will expect them to present early. This has been confirmed by our series and other studies.[1,4,26] Ossifying fibroma, on the other hand, is a true neoplasm.[31] Although chromosome translocations have been identified in a few cases of ossifying fibroma, genetic studies have been insufficient to determine the molecular mechanisms that underlie the development of this tumour.[31] Therefore, they are expected to present in the adolescent age group which was corroborated by our study and others.[1,4,26] One case of aggressive juvenile ossifying fibroma was treated by shelling out of the lesion [Figure 1a and b], with temporary ligation of the left external carotid artery [Figure 1c] to minimise intra-operative haemorrhage. This procedure has been reported in the literature to minimise haemorrhage in major oral and maxillofacial surgical procedures.[32]
Figure 1.
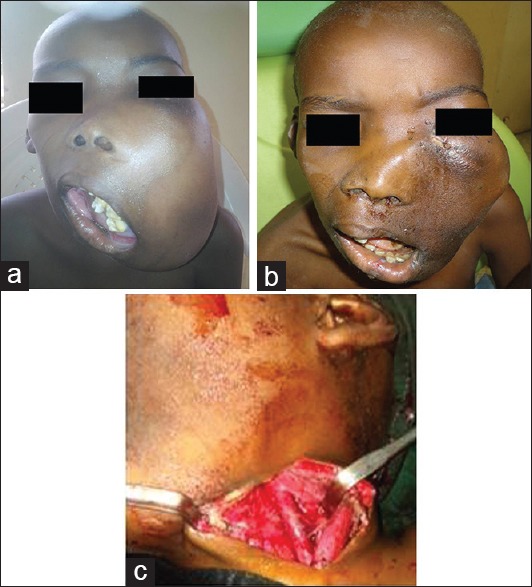
(a) Clinical photograph of patient with aggressive juvenile ossifying fibroma. (b) Five days postoperative clinical photograph. (c) External carotid artery ligation
Malignant tumours in this series had the highest presentation in the 10–14 age group (76.7%) closely followed by 5–9 age group (68.0%). This agrees with the findings of Olweny[33] who saw lesser cases after the 15th year of age. All cases of tumours beyond the maxillofacial region into the orbit [Figure 2a and b] and abdomen [Figure 3] were malignant cases. In addition, all the malignant cases were treated with chemotherapy alone of combination chemoradiation therapy. This was because most patients present in advance disease conditions were salvage surgery may be challenging because of co-morbid conditions. Reasons for this delay in presentation might be attributed to the user fee-based health system with few on health insurance, long distance from the rural referring centres, self-medication, ignorance and patronage of unorthodox medical practitioners. Six patients with malignant tumours discharged themselves against medical advice due to financial reasons. The rationale for this is that most of the patients are from low socioeconomic class as reflected from their parent's occupation. Based on the socioeconomic classification scheme by Oyedeji[34] for occupation [Table 8], these patients are in class IV and V and so cannot afford the treatment protocol for these malignant cases. Patients that were able to undergo treatment were supported by welfare funds donated by philanthropists and other nongovernmental organisations. Clegg et al.[35] in 2009 reported that socioeconomic patterns in incidence vary for specific cancers and such patterns were mostly associated with lower socioeconomic status. Despite advances in knowledge about risk factor reduction and improvements in the early detection and management of several cancers, socioeconomic imbalance persists in cancer incidence, morbidity, mortality and survival.[35,36] In addition, this excessive dependence on the ability to pay through out-of-pocket payment reduces healthcare consumption, worsens the already inequitable access to quality care and exposes households to the financial risk of expensive illness in low-income settings.[37]
Figure 2.
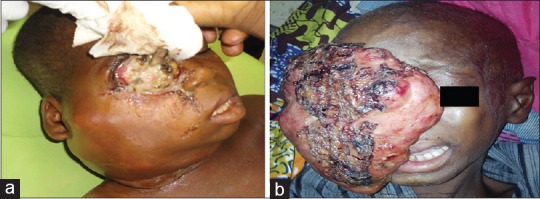
(a) Orbito-maxillofacial tumour presentation. (b) Orbito-maxillofacial tumour presentation
Figure 3.

Maxillofacial and abdominal tumour presentation
Table 8.
Socioeconomic classification by Oyedeji for occupation
| Class | Occupation |
|---|---|
| I | Senior public servants, professionals, managers, large-scale traders, businessmen and contractors |
| II | Intermediate grade public servants and senior school teachers |
| III | Junior school teachers, professional drivers and artisans |
| IV | Petty traders, labourers and messengers |
| V | Unemployed, full-time homemakers, students and subsistence farmers |
CONCLUSIONS
Our findings established that the orofacial tumours in children and adolescents are quite common in the Northwest region of Nigeria, with influx of patients from two neighbouring countries of Benin and Niger Republics. Most of these tumours are also of the malignant types emphasising the need for improved universal healthcare insurance for all citizens to adequately manage these children effectively.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to thank Medical records unit of Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria.
REFERENCES
- 1.Jaafari-Ashkavandi Z, Ashraf MJ. A clinico-pathologic study of 142 orofacial tumors in children and adolescents in Southern Iran. Iran J Pediatr. 2011;21:367–72. [PMC free article] [PubMed] [Google Scholar]
- 2.Bhaskar SN. Oral tumors of infancy and childhood. A survey of 293 cases. J Pediatr. 1963;63:195–210. doi: 10.1016/s0022-3476(63)80330-3. [DOI] [PubMed] [Google Scholar]
- 3.Regezi JA, Sciubbaj J, Jordan RC. Odontogenic tumors. 5th ed. Philadelphia: Saunders; 2008. Oral Pathology-Clinical Pathologic Correlations; p. 261. [Google Scholar]
- 4.Aregbesola SB, Ugboko VI, Akinwande JA, Arole GF, Fagade OO. Orofacial tumours in suburban Nigerian children and adolescents. Br J Oral Maxillofac Surg. 2005;43:226–31. doi: 10.1016/j.bjoms.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Neville BW, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology. 3rd ed. Philadelphia: Saunders; 2009. [Google Scholar]
- 6.Keszler A, Guglielmotti MB, Dominguez FV. Oral pathology in children. Frequency, distribution and clinical significance. Acta Odontol Latinoam. 1990;5:39–48. [PubMed] [Google Scholar]
- 7.Khademi B, Taraghi A, Mohammadianpanah M. Anatomical and histopathological profile of head and neck neoplasms in Persian pediatric and adolescent population. Int J Pediatr Otorhinolaryngol. 2009;73:1249–53. doi: 10.1016/j.ijporl.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 8.Adebayo ET, Ajike SO, Adekeye EO. Odontogenic tumours in children and adolescents: A study of 78 Nigerian cases. J Craniomaxillofac Surg. 2002;30:267–72. doi: 10.1016/s1010-5182(02)90288-x. [DOI] [PubMed] [Google Scholar]
- 9.Al-Khateeb T, Al-Hadi Hamasha A, Almasri NM. Oral and maxillofacial tumours in North Jordanian children and adolescents: A retrospective analysis over 10 years. Int J Oral Maxillofac Surg. 2003;32:78–83. doi: 10.1054/ijom.2002.0309. [DOI] [PubMed] [Google Scholar]
- 10.Elarbi M, El-Gehani R, Subhashraj K, Orafi M. Orofacial tumors in Libyan children and adolescents. A descriptive study of 213 cases. Int J Pediatr Otorhinolaryngol. 2009;73:237–42. doi: 10.1016/j.ijporl.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka N, Murata A, Yamaguchi A, Kohama G. Clinical features and management of oral and maxillofacial tumors in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:11–5. doi: 10.1016/s1079-2104(99)70186-1. [DOI] [PubMed] [Google Scholar]
- 12.Ajayi OF, Ladeinde AL, Adeyemo WL, Ogunlewe MO. Odontogenic tumors in Nigerian children and adolescents- a retrospective study of 92 cases. World J Surg Oncol. 2004;2:39. doi: 10.1186/1477-7819-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arotiba GT. A study of orofacial tumors in Nigerian children. J Oral Maxillofac Surg. 1996;54:34–8. doi: 10.1016/s0278-2391(96)90299-2. [DOI] [PubMed] [Google Scholar]
- 14.Ulmansky M, Lustmann J, Balkin N. Tumors and tumor-like lesions of the oral cavity and related structures in Israeli children. Int J Oral Maxillofac Surg. 1999;28:291–4. [PubMed] [Google Scholar]
- 15.Adebayo ET, Ajike SO, Adekeye EO. Tumours and tumour-like lesions of the oral and perioral structures of Nigerian children. Int J Oral Maxillofac Surg. 2001;30:205–8. doi: 10.1054/ijom.2001.0052. [DOI] [PubMed] [Google Scholar]
- 16.Sato M, Tanaka N, Sato T, Amagasa T. Oral and maxillofacial tumours in children: A review. Br J Oral Maxillofac Surg. 1997;35:92–5. doi: 10.1016/s0266-4356(97)90682-3. [DOI] [PubMed] [Google Scholar]
- 17.Jones AV, Franklin CD. An analysis of oral and maxillofacial pathology found in children over a 30-year period. Int J Paediatr Dent. 2006;16:19–30. doi: 10.1111/j.1365-263X.2006.00683.x. [DOI] [PubMed] [Google Scholar]
- 18.Asamoa EA, Ayanlere AO, Olaitan AA, Adekeye EO. Paediatric tumours of the jaws in Northern Nigeria. Clinical presentation and treatment. J Craniomaxillofac Surg. 1990;18:130–5. doi: 10.1016/s1010-5182(05)80330-0. [DOI] [PubMed] [Google Scholar]
- 19.Tanrikulu R, Erol B, Haspolat K. Tumors of the maxillofacial region in children: Retrospective analysis and long-term follow-up outcomes of 90 patients. Turk J Pediatr. 2004;46:60–6. [PubMed] [Google Scholar]
- 20.Green DM. Developments in Oncology. In: Green DM, editor. Diagnosis and management of malignant solid tumours in infants and children. Boston: Martins Nijhoff; 1985. pp. 1–5. [Google Scholar]
- 21.Maitra A, Kumar V. Robbin's Basic Pathology. In: Kumar V, Cotran R, Robbins A, editors. Genetic and pediatrics diseases. 7th ed. Philadelphia: Saunders; 2003. p. 251. [Google Scholar]
- 22.Shklar G, Meyer I. Vascular tumors of the mouth and jaws. Oral Surg Oral Med Oral Pathol. 1965;19:335–58. doi: 10.1016/0030-4220(65)90046-0. [DOI] [PubMed] [Google Scholar]
- 23.Cawson RA, Langdon JD, Eveson JW. Surgical pathology of the mouth and jaws. Oxford: Wright. 1996:279–81. [Google Scholar]
- 24.Budnick SD. Compound and complex odontomas. Oral Surg Oral Med Oral Pathol. 1976;42:501–6. doi: 10.1016/0030-4220(76)90297-8. [DOI] [PubMed] [Google Scholar]
- 25.Mosqueda-Taylor A, Ledesma-Montes C, Caballero-Sandoval S, Portilla-Robertson J, Ruíz-Godoy Rivera LM, Meneses-García A. Odontogenic tumors in Mexico: A collaborative retrospective study of 349 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:672–5. doi: 10.1016/s1079-2104(97)90371-1. [DOI] [PubMed] [Google Scholar]
- 26.Ajagbe HA, Daramola JO. Primary tumors of the jaw in Nigerian children. J Natl Med Assoc. 1982;74:157–61. [PMC free article] [PubMed] [Google Scholar]
- 27.Eversole LR. Craniofacial fibrous dysplasia and ossifying fibrous. Oral Maxillofac Surg Clin North Am. 1997;9:625–42. [Google Scholar]
- 28.Barnes L, Eveson JW, Reichart P, Sidransky D. Lyon: International Agency for Research on Cancer (IARC) Press; 2005. The WHO Classification of Head and Neck Tumours. [Google Scholar]
- 29.Chen FL, Shi WJ, Wang S, Zhang Q, Hu RM WHO. A novel, complex heterozygous mutation within Gsalpha gene in patient with McCune-Albright syndrome. Endocrine. 2002;18:121–8. doi: 10.1385/ENDO:18:2:121. Head and Neck TumoursSong HD. [DOI] [PubMed] [Google Scholar]
- 30.Pollandt K, Engels C, Kaiser E, Werner M, Delling G. Gsalpha gene mutations in monostotic fibrous dysplasia of bone and fibrous dysplasia-like low-grade central osteosarcoma. Virchows Arch. 2001;439:170–5. doi: 10.1007/s004280100453. [DOI] [PubMed] [Google Scholar]
- 31.Regezi JA, Sciubba J, Jordan RC. Benign non-odontogenic tumours. In: Oral Pathology-Clinical Pathologic Correlations. 5th ed. Stewart J, editor. Philadelphia: Saunders; 2008. p. 283. [Google Scholar]
- 32.Bouloux GF, Perciaccante VJ. Massive hemorrhage during oral and maxillofacial surgery: Ligation of the external carotid artery or embolization? J Oral Maxillofac Surg. 2009;67:1547–51. doi: 10.1016/j.joms.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 33.Olweny CL. Neoplastic diseases. Diseases of Children in the Subtropics and Tropics. In: Stanfield P, Bructon M, Chan M, Parkin M, Waterson T, editors. London: Edward Arnold; 1991. pp. 875–80. [Google Scholar]
- 34.Oyedeji GA. Socioeconomic and cultural background of hospitalised children in Ilesha. Niger J Paediatr. 1985;12:111–7. [Google Scholar]
- 35.Clegg LX, Li FP, Hankey BF, Chu K, Edwards BK. Cancer survival among US whites and minorities: A SEER (Surveillance, Epidemiology, and End Results) Program population-based study. Arch Intern Med. 2002;162:1985–93. doi: 10.1001/archinte.162.17.1985. [DOI] [PubMed] [Google Scholar]
- 36.Jemal A, Clegg LX, Ward E, Ries LA, Wu X, Jamison PM, et al. Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 37.Onwujekwe OE, Uzochukwu BS, Obikeze EN, Okoronkwo I, Ochonma OG, Onoka CA, et al. Investigating determinants of out-of-pocket spending and strategies for coping with payments for healthcare in southeast Nigeria. BMC Health Serv Res. 2010;10:67. doi: 10.1186/1472-6963-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]


