Abstract
Background and Aims:
Airway used in prone position should be efficacious and safe. The Streamlined Liner of the Pharynx Airway (SLIPA™) and Laryngeal Mask Airway-ProSeal (PLMA) provide better airway seal and protection against aspiration. We planned to evaluate the performance of SLIPA™, PLMA and endotracheal tube (ETT) in prone position.
Methods:
114 adult patients undergoing elective surgery in prone position under general anaesthesia were randomised into Group-T (ETT), Group-S (SLIPA™) and Group-P (PLMA). Airways were inserted in supine position and patients turned prone subsequently. Airway characteristics, ventilatory parameters and complications were noted. One-way analysis of variance, Mann–Whitney U-test and Chi-square or Fisher's exact test were used.
Results:
Tidal volumes, peak airway pressure and compliance were comparable at all times. Leak pressure was significantly higher (P < 0.001) in Group-T (mean leak pressure = 40 cmH2O) when compared to Group-S and Group-P at all the times of recording, and there was no significant difference between Group-S and Group-P. The number of patients requiring airway/neck manipulation in prone position was significantly higher (P < 0.001) in Group-S (19 [55.9%]) when the three groups were compared (none in Group-T) and in comparison with Group-P (5 [14.7%], P < 0.001). On airway removal, the incidence of complications and airway reaction was significantly higher in Group-T. Group-S had a significantly higher incidence of dysphagia at 2 h postoperatively.
Conclusion:
ETT was most efficacious. SLIPA™ and PLMA were efficacious, safe and less stimulating to the airway during removal. More patients required SLIPA™ airway/neck manipulation.
Key Words: Anaesthesia, positive-pressure respiration, prone position, ventilation
INTRODUCTION
Effective and safe airway management is a major concern in anaesthesia in the prone position, and airway used should be as efficacious and safe as in supine position. Endotracheal tube (ETT) is considered the 'gold standard' for airway management. Among the many advantages, an ETT provides the most reliable and definitive airway and adequate ventilation and protects against aspiration. However, haemodynamic responses, coughing, bronchospasm, failed intubation and postoperative sore throat are among the concerns. These problems led to the invention and subsequent introduction of supraglottic airways (SGAs) into clinical practice which resulted in a paradigm shift in airway management during anaesthesia from a two-choice (face mask vs. ETT) to a three-choice (face mask vs. SGA vs. ETT) model.
The laryngeal mask airway (LMA)[1] has many advantages over ETT such as faster and easier placement, improved oxygen saturation and lower frequency of coughing during emergence, reduced anaesthetic requirement for airway tolerance and lower incidence of sore throat.[2,3,4] An improved version LMA-ProSeal (PLMA) provides adequate seal[5,6] and offers protection against regurgitation,[7] aspiration and gastric insufflation.
A relatively new airway device, the Streamlined Liner of the Pharynx Airway (SLIPA™), which is uncuffed, offers an alternative to the cuffed LMA.[8] The SLIPA™ effects a seal because its anatomical shape seals the outlet from the pharynx at the base of the tongue and also the entrance to the oesophagus because of the resilience of the material used in manufacture.[9] Protection against aspiration is claimed on account of the hollow structure that allows some storage of the regurgitated fluid.
Modifications in the design providing a higher leak pressure[10] and a gastric drain tube make the second-generation SGAs more suitable and reliable for positive pressure ventilation in prone position. There are only a few studies on PLMA during anaesthesia in the prone position, and no prospective studies on SLIPA™.
Therefore, we designed a prospective study to evaluate the performance of SLIPA™ and PLMA and compare it to that of ETT in anaesthetised paralysed patients undergoing elective surgery in prone position. We hypothesised that the efficacy of SLIPA™ and PLMA would be different from ETT.
METHODS
Approval for this prospective, randomised study was obtained from the Institute Ethical Committee. Patients of either sex aged 18–65 years belonging to the American Society of Anesthesiologists (ASA) grades I–III scheduled for elective urology, plastic surgery, lumbar and lower thoracic spine procedures in prone position under general anaesthesia were included, from February 2016 to May 2017. Written, informed consent was obtained from the patients after pre-anaesthetic evaluation. Exclusion criteria were surgeries with anticipated extensive blood loss or postoperative mechanical ventilation, anticipated difficult airway, gastro-oesophageal reflux, reactive airway, obesity (body mass index ≥30 kg/m2), present history of sore throat or dysphagia, allergy to anaesthetic medications in use, pregnant or lactating women and those who declined to participate. Age, gender, weight, height, modified Mallampati score and thyroid cartilage width of the patients were recorded. Patients were kept fasted as per the current ASA guidelines in force[11] and received oral diazepam 0.15 mg/kg and ranitidine 150 mg the night before and on the morning of surgery.
On arrival to the operating room, the patients were allocated into Group-T (ETT), Group-S (SLIPA™) and Group-P (PLMA) by computer-generated random numbers using block randomisation technique with varying block sizes and serially numbered sealed envelopes. After initiating monitoring, an intravenous access was secured. A pre-procedure self-testing of the anaesthesia workstation (Avance CS2, Datex-Ohmeda, Inc., General Electric Company, Madison, USA) with confirmation of circuit leak <100 ml/min was ensured. A standard technique of general anaesthesia was used. Intraoperative monitoring included electrocardiogram, non-invasive oscillometric blood pressure, pulse oximeter (SpO2), end-tidal carbon dioxide (ETCO2), neuromuscular transmission and nasopharyngeal temperature. The patients were pre-oxygenated with 100% oxygen for 3 min. Anaesthesia was induced with intravenous (IV) fentanyl 2 μg/kg and propofol titrated to loss of verbal contact. Neuromuscular blockade was achieved with IV vecuronium 0.1 mg/kg. Lungs were ventilated manually with a facemask and pressure limit set to 15 cm H2O. The respective airway was inserted upon achieving train-of-four (TOF) count zero. Anaesthesia was maintained with IV propofol infusion (50–150 μg/kg/h), supplemental boluses of IV fentanyl 1 μg/kg, vecuronium as required and positive pressure ventilation with 33% oxygen in N2O.
ETT (7 mm for females and 8.5 mm for males) was inserted under direct laryngoscopy using Macintosh blade. The size of SLIPA™ was selected by matching the thyroid cartilage width,[12] and the insertion was facilitated by jaw thrust provided by an assistant. PLMA size selection was based on body weight (size 3 if <50 kg, size 4 if 51–70 kg or size 5 if 71–100 kg) and insertion was guided by gum elastic bougie under direct laryngoscopy.[13] Both SLIPA™ and PLMA were lubricated with water-soluble gel before insertion. The cuffs of ETT were inflated with the volume of air appropriate to avoid palpable leak. PLMA was inflated according to the recommended amount of air for respective size. A maximum of three attempts at insertion were allowed for SLIPA™ and PLMA. Anaesthesiologists and trainees with at least 1 year of experience were allowed to insert the airway. Insertion of SLIPA™ and PLMA was performed by only those who had prior experience (at least 10 successful insertions in patients) of inserting these devices, and the presence of the experienced anaesthesiologist was ensured during airway insertion and the conduct of these cases.
Insertion was deemed 'successful' if controlled ventilation produced an adequate chest excursion, bilateral equal air entry and a square-wave capnogram at leak pressure (inspiratory pressure at which leak of respiratory gases was detected by palpation over the anterior neck) ≥15 cmH2O. Following each 'unsuccessful' attempt, face mask ventilation was resumed for at least 1 min before the next attempt. The number of attempts at insertion (maximum of 3) and time taken for 'successful' insertion (from removal of face mask until airway insertion deemed 'successful') were noted immediately.
Manipulation of the airway or neck position (flexion/extension/rotation) was allowed to improve the fit of airway (if the initial leak pressure <15 cmH2O) following each attempt. Only those patients with 'successful' airway placement were turned prone and managed as per the study protocol subsequently. If airway insertion was 'unsuccessful' even after three attempts, the patient received an ETT as rescue airway and was excluded from the study for further analysis.
After 'successful' placement, the airway was secured with adhesive plaster. A 14 Fr gastric drain tube was inserted in Group-P which was suctioned and left open to drain any gastric content into a glove. Subsequently, the patients were mechanically ventilated in volume control mode with an inspired tidal volume (VTi) = 6–10 ml/kg of ideal body weight (IBW), respiratory rate (RR) =10–16/min, inspiratory-expiratory ratio (I: E) = 1:2 and positive end-expiratory pressure (PEEP) = 5 cmH2O. VT and RR were adjusted to achieve an ETCO2< 45 mmHg. Ability to achieve an expired tidal volume (VTe) of at least 6 ml/kg of IBW without leak and ETCO2 < 45 mmHg was considered 'adequate ventilation'. After achieving 'adequate ventilation', the cuff pressure of ETT was adjusted to 25 cmH2O and that of PLMA to 60 cmH2O.
The following parameters were noted 5 min after 'successful' placement of the airway (T1) (after adjusting the cuff pressure) after adjusting the VTe to 6 ml/kg of IBW: (1) VTi(ml), (2) VTe(ml), (3) RR (cycles/min), (4) expired minute volume (MVe, L), (5) peak airway pressure (Ppeak, cmH2O), (6) mean airway pressure (Pmean, cmH2O), (7) compliance (ml/cmH2O) and (8) leak pressure (cmH2O). The parameters 1–7 were recorded from the display of the ventilator. The 'leak pressure' was estimated using 'manometric stability' method[14] as follows. The expiratory valve of the circle breathing system was closed and fresh gas flow adjusted to 3 L/min. As the pressure in the breathing system increased (maximum allowed 40 cmH2O), the airway pressure at which the manometer dial reached stability (i.e., the leak is in equilibrium with the fresh gas flow) was noted.
Subsequently, patients were turned prone with the head turned slightly to one side with no external pressure on the neck. The chest and pelvis were adequately supported to keep the abdomen free of any direct pressure. The above-mentioned ventilator parameters were noted 5 min after re-establishing monitoring and mechanical ventilation in prone position (T2) and subsequently at 30 min (T3) and 60 min after assuming prone position (T4). TOF count of zero, cuff pressure of ETT = 25 cmH2O and that of PLMA = 60 cmH2O and VTe= 6 ml/kg of IBW were ensured before recording parameters at each of these intervals. Manipulation of the airway or neck position (flexion/extension/rotation) was allowed to improve the fit of airway (if leak pressure <15 cmH2O) and the same was noted.
Surgical manipulations were paused while recording the parameters. Intraoperative complications such as airway dislodgement, obstruction, desaturation (SpO2< 94%) or ETCO2 >45 mmHg, if any, were recorded. During the surgery, endotracheal intubation performed in prone or after turning supine at the discretion of the attending anaesthesiologist was the proposed rescue technique for the SLIPA™ and PLMA group for loss of airway or any severe compromise in ventilation as judged by the anaesthesiologist.
Intravenous diclofenac 1 mg/kg or tramadol 1 mg/kg and ramosetron 0.3 mg were administered 30 min before the end of surgery. Propofol infusion and N2O were discontinued 10 min before the expected completion of surgery. Neuromuscular blockade was reversed with neostigmine 50 μg/kg and glycopyrrolate 10 μg/kg. The airway was removed in prone position after the patients started breathing spontaneously and regained consciousness. The time duration from turning the patient prone till the patient regained spontaneous ventilation was considered the 'duration of prone ventilation'. The following were noted upon airway removal: airway reaction (coughing, breath-holding, laryngospasm and bronchospasm), airway injury, blood on device, regurgitation/aspiration (presence/staining of devices with gastric juice) and damage to the airway device.
The patients were turned supine soon after the airway device removal and transferred to the post-anaesthesia care unit (PACU) subsequently. Intravenous morphine 0.1 mg/kg was administered if the patient complained of pain during the PACU stay. Intravenous diclofenac 1 mg/kg or tramadol 1 mg/kg was administered q12h in the ward. An investigator not aware of the airway device used assessed the following: sore throat, dysphagia, hoarseness of voice and postoperative nausea and vomiting (PONV), by asking about general well-being first and then the leading questions, at 1 h (in PACU) and 24 h postoperatively.
The primary objective was efficacy of the three airway devices with respect to the leak pressure and ventilatory parameters (tidal volume, respiratory rate, minute volume, peak and mean airway pressures and compliance). The secondary objective was safety assessed in terms of the number of attempts at insertion, time taken for insertion, failure of device, number of airway/neck manipulations, and intraoperative, post-airway removal and postoperative complications.
Continuous data were presented as mean (standard deviation [SD]) or median (interquartile range), as appropriate. Normality of the quantitative data was checked by measures of Kolmogorov–Smirnov tests of normality. For normally distributed data, means of the groups were compared using one-way analysis of variance followed by post hoc multiple comparisons. For skewed data or ordinal data, Kruskal–Wallis test followed by Mann–Whitney U-test for two groups was applied. Qualitative or categorical variables were described as frequencies and proportions. Proportions were compared using Chi-square or Fisher's exact test whichever is applicable.
A pilot study of 10 cases each in prone position showed a leak pressure of 31 ± 5 cmH2O for PLMA and >40 cmH2O for ETT. We considered the reported[15] mean leak pressure of 27.3 cmH2O for SLIPA™. Assuming an equal SD for both, PLMA and SLIPA™, the sample size estimated was 29 patients per group. In the same pilot study, the mean dynamic compliance was 25.4 and 22.0 ml/cmH2O for PLMA and ETT, respectively. Assuming an equal SD of 5 ml/cmH2O, the sample size estimated was 34 patients per group at a power of 80% and confidence interval (CI) of 95%. Therefore, we included a total of 114 patients (38 in each group) assuming a possible drop out of 10%. All analyses were performed using IBM SPSS statistics version 22.0 (Statistical Packages for the Social Sciences, Chicago, IL) and a P < 0.05 was considered statistically significant.
RESULTS
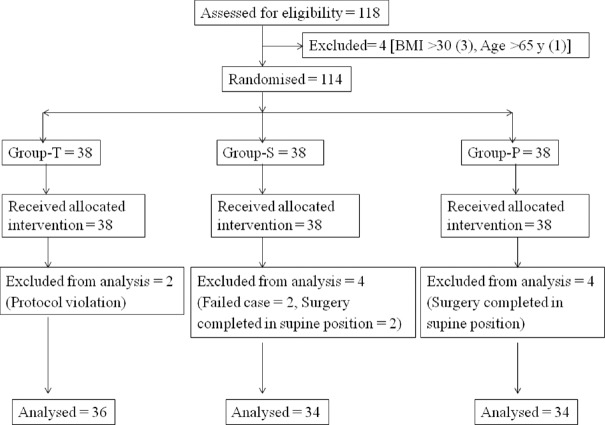
One hundred and fourteen patients were randomised into three groups. Two patients in Group-T (protocol violation) and four each in Group-S (failed case = 2, surgery completed in supine position = 2) and Group-P (surgery completed in supine position) were excluded from the study [Figure 1]. Data of 104 patients were analysed. Totally, eight qualified anaesthesiologists and nine eligible trainees inserted the airway devices.
Figure 1.
Consort patient flow diagram
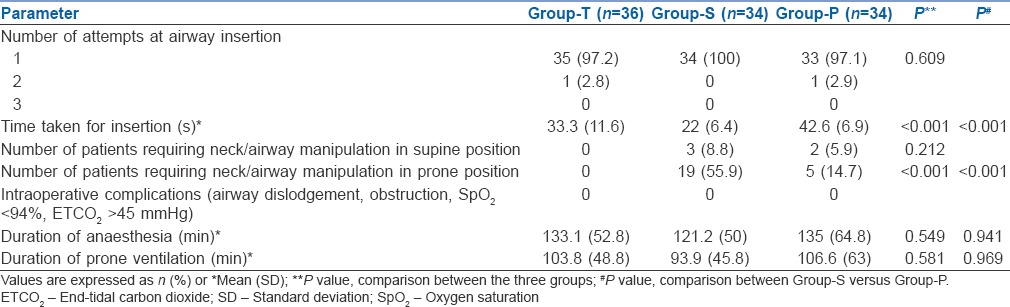
Patient characteristics were similar in all the three groups [Table 1]. The number of attempts at airway insertion, airway manipulation in supine position, intraoperative complications and the duration of anaesthesia and prone ventilation were comparable between the three groups [Table 2]. The mean time taken for airway insertion was significantly higher (P < 0.001) in Group-P (42.6 ± 6.9 s), when the three groups were compared and in comparison with Group-S (22 ± 6.4 s, P < 0.001). The number of patients requiring airway manipulation in prone position was significantly higher (P < 0.001) in Group-S (19 [55.9%], when the three groups were compared and in comparison with Group-P (5 [14.7%], P < 0.001). No patient in Group-T required any airway manipulation in prone position.
Table 1.
Patient characteristics
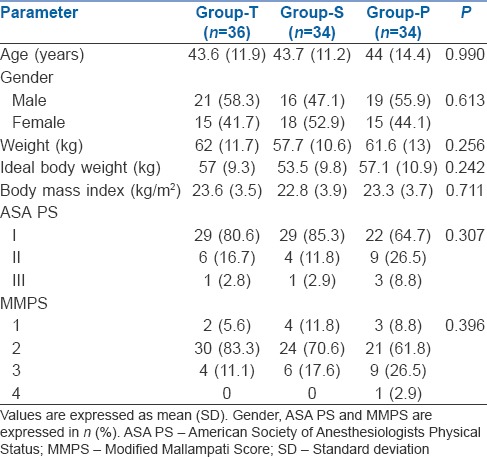
Table 2.
Airway characteristics, intraoperative airway complications, duration and analgesics
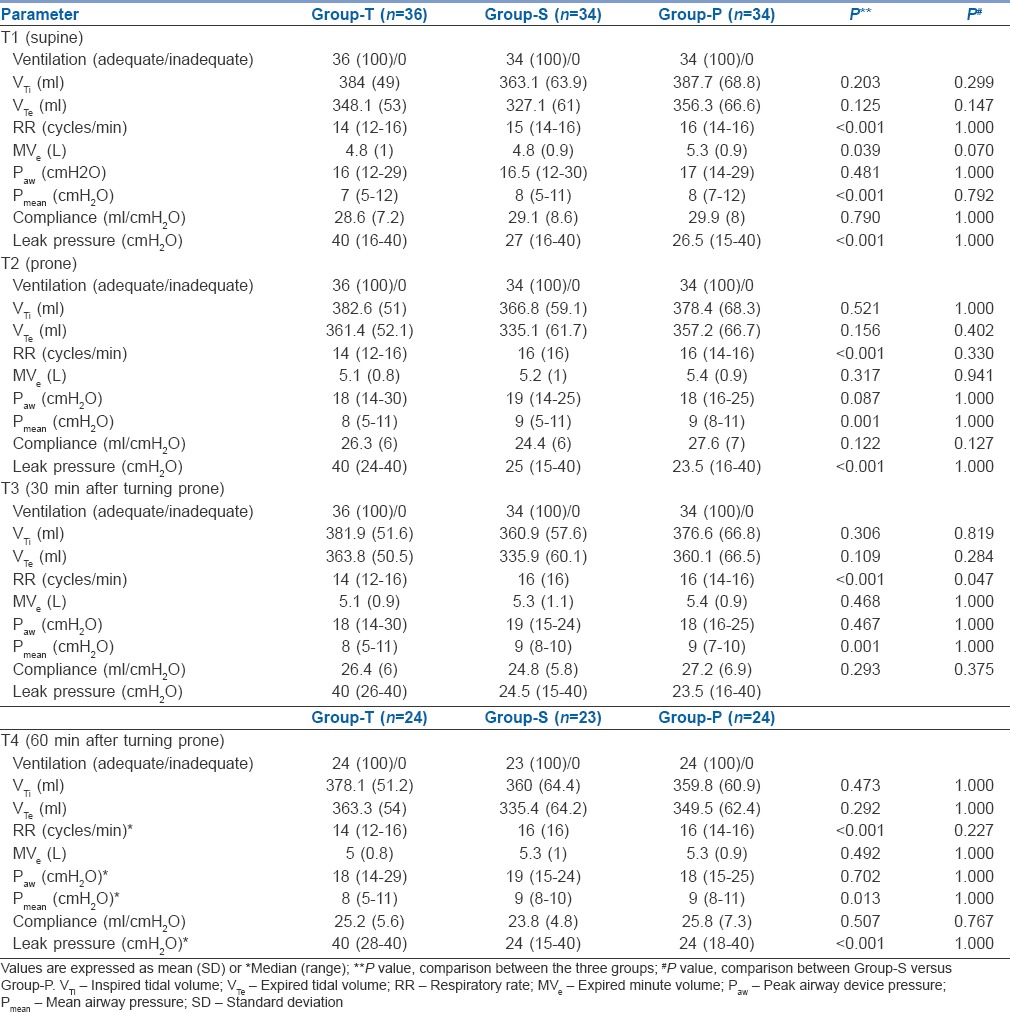
Ventilation was deemed 'adequate' in all the patients at all the times of recording in all the three groups. The VTi, VTe, Paw and compliance were comparable between the three groups at all the times of recording [Table 3]. The RR was significantly lower (P < 0.001) in Group-T at all the times of recording when the three groups were compared, whereas the difference between Group-S and Group-P was not significant, except at T3(P = 0.047). There was no difference in MVe between the three groups at all the times of recording, except at T1(P = 0.039). However, the difference in MVe between Group-S and Group-P at T1 was not significant. Pmean was significantly lower in Group-T at all the times of recording. The leak pressure was significantly higher (P < 0.001) in Group-T (mean leak pressure = 40 cmH2O) when compared to Group-S and Group-P at all the times of recording, and there was no significant difference between Group-S and Group-P at any of these times of recording. There was no intraoperative inadequate ventilation, desaturation, airway obstruction or dislodgement of airway in any of the three groups.
Table 3.
Ventilatory parameters
The incidence of complications upon airway device removal was significantly higher (P = 0.002) in Group-T when compared to the other two groups [Table 4]. However, the same was not significantly different between Group-S and Group-P. Among the complications, airway reaction (coughing) was significantly higher in Group-T (P < 0.001) with no significant difference between Group-S and Group-P. There was no significant difference with respect to airway injury and blood on device. No patient experienced breath-holding, laryngospasm, bronchospasm or regurgitation/aspiration. There was no damage to any of the airway devices.
Table 4.
Complications upon airway removal
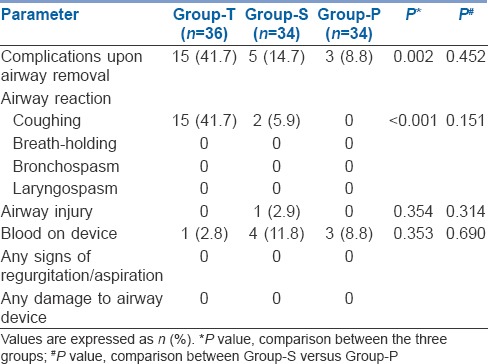
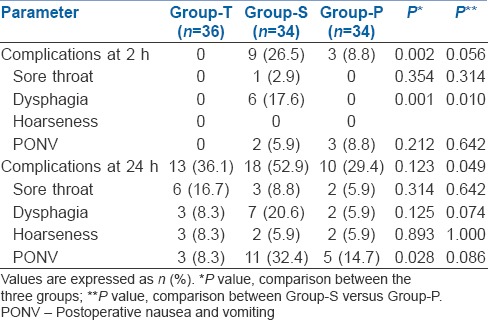
At 2 h postoperatively, there was a significant difference (P = 0.002) in the overall incidence of complications (sore throat, dysphagia, hoarseness and PONV) with Group-S having the highest number of complications [Table 5]. However, there was no significant difference between Group-S and Group-P. Six patients in only Group-S complained of dysphagia which was significant (P = 0.001). At 24 h postoperatively, there was no difference (P = 0.123) in the overall incidence of complications between the three groups. However, Group-T had significantly lower incidence (P = 0.028) of PONV when compared to Group-S and Group-P. No patient required rescue endotracheal intubation intraoperatively or airway assistance after the airway device removal in prone position.
Table 5.
Postoperative morphine consumption and complications
DISCUSSION
We found that all the three airways provided 'adequate ventilation' in all the patients even though ETT provided a significantly higher mean leak pressure than SLIPA™ and PLMA. SLIPA™ and PLMA were similar with regard to leak pressure and other ventilatory parameters.
Significantly, lower RR in Group-T could be because of the minor leaks associated with SLIPA™ and PLMA during positive pressure ventilation. The significantly higher Pmean observed in Group-P and Group-S could be because of the resistance offered by the larynx to respiratory gases while ventilating with SGAs. However, these statistically significant differences in RR and Pmean may not be clinically significant. The mean leak pressure recorded in Group-P in prone [Table 3] are slightly less than that reported in the previous studies (31–36 cmH2O).[15,16,17] The mean leak pressure recorded in Group-S in supine position was similar to that reported earlier (23.4–30 cmH2O).[7,18,19,20,21]
In terms of safety, the three devices were found safe in general even though there were differences in a few aspects such as the time taken for insertion, number of intraoperative neck/airway manipulations, post-airway device removal complications and postoperative complications. The time taken for insertion was shortest in Group-S and highest in Group-P. Insertion of SLIPA™ did not involve direct laryngoscopy, and there was no time required for inflation of the cuff as it is a cuffless airway. We chose the bougie-guided insertion of PLMA under direct laryngoscopy as it has been demonstrated to be superior to both the standard digital and the introducer tool techniques.[13] Hence, it required more time than ETT and SLIPA™ for insertion. Studies have used different definitions for the time taken for insertion. This explains the slightly higher time taken for insertion of the devices in our study.
Even though there were no intraoperative complications (inadequate ventilation, desaturation, airway obstruction and dislodgement of airway) in any of the three groups, Group-S had a significantly higher number of patients requiring neck/airway manipulations in prone position. This may indicate that the SLIPA™ is less stable compared to ETT and PLMA in prone position with neck slightly turned to one side. Placement of a gastric drain tube in Group-P may have helped in keeping the PLMA in place during change of position and in prone position. The slight rotation of the neck to one side may cause leaks with SLIPA™ during positive pressure ventilation because of its relatively rigid, preformed, and cuffless design and a change in dimensions of the pharynx with neck rotation even though its shape is similar to pharynx. On the other hand, PLMA might conform to the shape of the pharynx better in altered neck positions. There are conflicting findings with regard to perilaryngeal leakage with a change in head position with PLMA and SLIPA™. One study reported an increased incidence of leakage with the PLMA versus the SLIPA™,[18] while the other study found similar rates for both devices.[19] A change in the cuff pressure of PLMA which was not monitored while N2O was used has been proposed as one of the reasons for increased perilaryngeal leak with PLMA versus SLIPA™.[18] ETT is less susceptible to such displacements and such minor displacements may not manifest in ventilator parameters requiring adjustments.
A notable finding was the complications upon airway removal in Group-T with a significantly higher incidence of airway reaction compared to Group-S and Group-P. Removal of ETT is known to be more stimulating than the SGAs. The higher incidence of dysphagia in Group-S at 2 h postoperatively did not persist at 24 h. This may be attributed to the relatively stiff 'toe' and an uncuffed design and a larger size of SLIPA™ at the time of insertion leading to a greater force being used during insertion. We also monitored the intracuff pressures of ETT and PLMA which could have prevented mucosal ischaemia.[22]
The incidence of aspiration with the LMA has been estimated at 0.02%,[23] which is similar to ETT in elective patients.[24] The risk of pulmonary aspiration in patients whose lungs were mechanically ventilated through LMA (35,630 procedures) or ETT (30,082 procedures) was compared.[25] The odds ratio for pulmonary aspiration with the LMA was 1.06 (95% CI 0.20–5.62).
Only a few studies have evaluated PLMA during prone anaesthesia[15,16,17,26] and there are no prospective studies on SLIPA™. López et al.[16] compared PLMA with LMA-Supreme in a prospective study. The airway device was inserted following induction of general anaesthesia in prone position. Both the devices were easy to insert with few complications. There was less need for manipulation to achieve optimal position (3% vs. 15%; P = 0.02), and seal pressure was higher with the PLMA (31[4] vs. 27[4] cmH2O; P < 0.01].
A retrospective audit of 245 patients[15] in which the PLMA was inserted in and anaesthesia was maintained in prone position by experienced users reported that PLMA insertion and ventilation was successful in all patients. Correctable partial airway obstruction occurred in three patients, but there was no hypoxia, hypercapnoea, displacement, regurgitation, gastric insufflation or airway reflex activation. The authors suggested that the insertion of and maintenance of anaesthesia with the PLMA is feasible in prone position by experienced users. They also recommended that this technique should only be used by clinicians with considerable experience with the PLMA and prone anaesthesia.
There are a few shortcomings of our study. The study was blinded only for postoperative complications. The operators had variable experience, and they were more experienced with ETT than with PLMA and least with SLIPA™. Uniformity in gastric drain tube insertion was not maintained which may have affected the incidence of dysphagia and sore throat. Only Group-P received a gastric drain tube and Group-T did not to adhere to the routine practice. It is not possible to insert a gastric drain tube with SLIPA™. We had kept the patients' neck turned slightly to one side which might have affected the ventilatory parameters in Group-S and Group-P. Finally, postoperative pain assessment was subjective.
The safety of SLIPA™ and PLMA for prone ventilation needs to be established in studies with larger sample size. Feasibility in the hands of novices under the supervision of experienced users is required before recommendations for extensive usage can be made.
A careful consideration of anticipated airway difficulty, anaesthesiologist's ability to handle the accidental loss of airway in prone position and the type of surgical procedure is a must before selecting the appropriate airway. SGAs may not be suitable for patients undergoing surgery in prone position where the anaesthesiologist does not have access to/control of the head and neck.
CONCLUSION
We found that ETT was the most efficacious airway device for positive pressure ventilation in prone position. The SLIPA™ and PLMA were efficacious, safe and less stimulating to the airway during removal in prone position. However, higher number of patients required SLIPA™ airway/neck manipulation to maintain adequate ventilation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We are thankful to Dr Donald Miller and Dr G D Puri, Professor and Head, Department of Anaesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India, for helping us procure free samples of SLIPA™ for the study. We are grateful to Mrs Kusum L. Chopra for the statistical assistance.
REFERENCES
- 1.Brain AI. The laryngeal mask--a new concept in airway management. Br J Anaesth. 1983;55:801–5. doi: 10.1093/bja/55.8.801. [DOI] [PubMed] [Google Scholar]
- 2.Brimacombe J. The advantages of the LMA over the tracheal tube or facemask: A meta-analysis. Can J Anaesth. 1995;42:1017–23. doi: 10.1007/BF03011075. [DOI] [PubMed] [Google Scholar]
- 3.Hohlrieder M, Brimacombe J, von Goedecke A, Keller C. Postoperative nausea, vomiting, airway morbidity, and analgesic requirements are lower for the ProSeal laryngeal mask airway than the tracheal tube in females undergoing breast and gynaecological surgery. Br J Anaesth. 2007;99:576–80. doi: 10.1093/bja/aem096. [DOI] [PubMed] [Google Scholar]
- 4.Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: A systematic review. J Oral Maxillofac Surg. 2010;68:2359–76. doi: 10.1016/j.joms.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Brain AI, Verghese C, Strube PJ. The LMA 'ProSeal'-A laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 6.Keller C, Brimacombe J. Mucosal pressure and oropharyngeal leak pressure with the ProSeal versus laryngeal mask airway in anaesthetized paralysed patients. Br J Anaesth. 2000;85:262–6. doi: 10.1093/bja/85.2.262. [DOI] [PubMed] [Google Scholar]
- 7.Miller DM, Camporota L. Advantages of ProSeal and SLIPA airways over tracheal tubes for gynecological laparoscopies. Can J Anaesth. 2006;53:188–93. doi: 10.1007/BF03021826. [DOI] [PubMed] [Google Scholar]
- 8.Miller DM, Lavelle M. A streamlined pharynx airway liner: A pilot study in 22 patients in controlled and spontaneous ventilation. Anesth Analg. 2002;94:759–61. doi: 10.1097/00000539-200203000-00052. [DOI] [PubMed] [Google Scholar]
- 9.Miller DM. A proposed classification and scoring system for supraglottic sealing airways: A brief review. Anesth Analg. 2004;99:1553–9. doi: 10.1213/01.ANE.0000134798.00069.2B. [DOI] [PubMed] [Google Scholar]
- 10.Ramachandran SK, Kumar AM. Supraglottic airway devices. Respir Care. 2014;59:920–31. doi: 10.4187/respcare.02976. [DOI] [PubMed] [Google Scholar]
- 11.Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures. An Updated Report by the ASA Task Force. Anesthesiology. 2017;126:376–93. doi: 10.1097/ALN.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 12.Choi GJ, Kang H, Baek CW, Jung YH, Woo YC, Kim SH, et al. Comparison of streamlined liner of the pharynx airway (SLIPA ™) and laryngeal mask airway: A systematic review and meta-analysis. Anaesthesia. 2015;70:613–22. doi: 10.1111/anae.13035. [DOI] [PubMed] [Google Scholar]
- 13.Brimacombe J, Keller C, Judd DV. Gum elastic bougie-guided insertion of the ProSeal laryngeal mask airway is superior to the digital and introducer tool techniques. Anesthesiology. 2004;100:25–9. doi: 10.1097/00000542-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999;82:286–7. doi: 10.1093/bja/82.2.286. [DOI] [PubMed] [Google Scholar]
- 15.Brimacombe JR, Wenzel V, Keller C. The Proseal laryngeal mask airway in prone patients: A retrospective audit of 245 patients. Anaesth Intensive Care. 2007;35:222–5. doi: 10.1177/0310057X0703500211. [DOI] [PubMed] [Google Scholar]
- 16.López AM, Valero R, Hurtado P, Gambús P, Pons M, Anglada T, et al. Comparison of the LMA Supreme™ with the LMA proseal™ for airway management in patients anaesthetized in prone position. Br J Anaesth. 2011;107:265–71. doi: 10.1093/bja/aer104. [DOI] [PubMed] [Google Scholar]
- 17.Taxak S, Gopinath A, Saini S, Bansal T, Ahlawat MS, Bala M, et al. Aprospective study to evaluate and compare laryngeal mask airway ProSeal and i-gel airway in the prone position. Saudi J Anaesth. 2015;9:446–50. doi: 10.4103/1658-354X.159473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woo YC, Cha SM, Kang H, Baek CW, Jung YH, Kim JY, et al. Less perilaryngeal gas leakage with SLIPA™ than with LMA-ProSeal™ in paralyzed patients. Can J Anaesth. 2011;58:48–54. doi: 10.1007/s12630-010-9412-3. [DOI] [PubMed] [Google Scholar]
- 19.Choi YM, Cha SM, Kang H, Baek CW, Jung YH, Woo YC, et al. The clinical effectiveness of the streamlined liner of pharyngeal airway (SLIPA) compared with the laryngeal mask airway ProSeal during general anesthesia. Korean J Anesthesiol. 2010;58:450–7. doi: 10.4097/kjae.2010.58.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Puri GD, Hegde HV, Jayant A, Bhukal I. Haemodynamic and bispectral index response to insertion of the streamlined liner of the pharynx airway (SLIPA™): Comparison with the laryngeal mask airway. Anaesth Intensive Care. 2008;36:404–10. doi: 10.1177/0310057X0803600312. [DOI] [PubMed] [Google Scholar]
- 21.Abdellatif AA, Ali MA. Comparison of streamlined liner of the pharynx airway (SLIPA™) with the laryngeal mask airway ProSeal™ for lower abdominal laparoscopic surgeries in paralyzed, anesthetized patients. Saudi J Anaesth. 2011;5:270–6. doi: 10.4103/1658-354X.84100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin BC, Wu RS, Chen KB, Yang MH, Lo YC, Chiang YY, et al. A comparison of the classic and a modified laryngeal mask airway (OPLAC™) in adult patients. Anesth Analg. 2011;112:539–44. doi: 10.1213/ANE.0b013e31820a5626. [DOI] [PubMed] [Google Scholar]
- 23.Brimacombe JR, Berry A. The incidence of aspiration associated with the laryngeal mask airway: A meta-analysis of published literature. J Clin Anesth. 1995;7:297–305. doi: 10.1016/0952-8180(95)00026-e. [DOI] [PubMed] [Google Scholar]
- 24.Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993;78:56–62. doi: 10.1097/00000542-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Bernardini A, Natalini G. Risk of pulmonary aspiration with laryngeal mask airway and tracheal tube: Analysis on 65 712 procedures with positive pressure ventilation. Anaesthesia. 2009;64:1289–94. doi: 10.1111/j.1365-2044.2009.06140.x. [DOI] [PubMed] [Google Scholar]
- 26.Sharma V, Verghese C, McKenna PJ. Prospective audit on the use of the LMA-supreme for airway management of adult patients undergoing elective orthopaedic surgery in prone position. Br J Anaesth. 2010;105:228–32. doi: 10.1093/bja/aeq118. [DOI] [PubMed] [Google Scholar]