Sir,
We would like to share our experience of using the Oxygen Reserve Index™ (ORi™) (Masimo, Irvine, California, USA) in a neonate. The ORi™, a new continuous and non-invasive measurement supplementing routine pulse oximetry, provides a unit-less index ranging from 1 (increased reserve) to 0 (no reserve), predicting impending desaturation before any drop in saturation occurs.[1] In addition, a positive correlation has been shown between the ORi™ value and the arterial oxygen tension.[2] A 13-day neonate, an operated case of tracheoesophageal fistula with suspected mediastinal leak was posted for re-exploration. Preoperatively, the child was tachypnoeic maintaining saturation (SpO2) of 90% on 0.6 inspired oxygen concentration (FiO2) delivered through a high flow nasal cannula. On shifting to the operating room, standard monitors were attached along with the ORi™ and child was pre-oxygenated with 100% oxygen with face mask. Initial slight improvement of SpO2 was noted to 99% with the ORi™ value remaining at 0.
Following induction SpO2 rapidly dropped to 76%, increasing after successful endotracheal intubation. Subsequently, there were frequent desaturation episodes occurring during surgery with lung retraction. Throughout this period ORi™ values remained at 0 despite maintaining FiO2 of between 0.8 and 1.0. Intraoperatively, the surgical team noticed a tracheal rent. Following successful repair of the tracheal rent and improvement in ventilation, appearance of the ORi™ was observed with a dramatic rise to 1.0. Following this increase, FiO2 was then titrated to 0.4–0.5 to maintain an ORi™ value of between 0 and 0.3 and SpO2 above 97%. Surgery proceeded uneventfully with no further desaturation episodes and stable ORi™ values between 0 and 0.3 [Figure 1].
Figure 1.
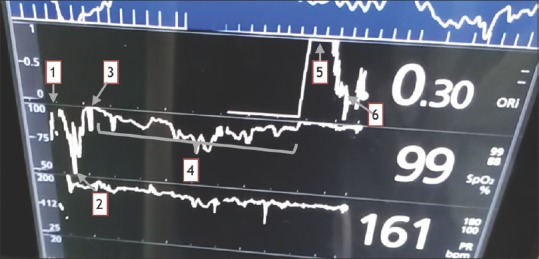
Trends in ORi™ and O2 saturation displayed on the Masimo SET® Monitor. Preoxygenation (1), Desaturation after induction (2), Improvement after intubation (3), Intraoperative desaturation episodes (4), Appearance of ORi™ after repair of tracheal rent (5), FiO2 titrated to ORi™ values (6)
Neonates represent a precarious group requiring careful titration of oxygen therapy, with excessive oxygen being associated with complications such as retinopathy of prematurity, bronchopulmonary dysplasia and periventricular leucomalacia.[3] On the other hand, due to lower reserve and increased oxygen consumption, they tend to desaturate rapidly especially during thoracic surgeries.[4] Using the ORi™, we observed that initially though SpO2 was 100% ORi™ remained 0, and rapid desaturation occurred after induction of anaesthesia correlating with the baby's low reserve. Perhaps use of apnoeic oxygenation techniques during laryngoscopy (such as high flow nasal cannula or deep pharyngeal insufflation) could have prevented this drop in saturation. As the surgery progressed, loss of ventilation through the tracheal rent compounded by the lateral position and frequent lung retraction led to multiple desaturation episodes correlating with the ORi™ value of 0. Repair of the rent and improvement in ventilation was visible with improvements in the SpO2, decreased oxygen requirement and appearance of the ORi™ measurement. Titrating the FiO2 to ORi™ values helped us avoid excessive oxygenation while maintaining a marginal reserve in anticipation of further possible desaturation episodes. The accuracy of ORi™ may be affected by vasoconstriction, hypothermia and poor perfusion states.[5]
In conclusion, the ORi™ is a new monitoring tool, and further studies are needed to explore its utility in different clinical situations and elucidate the factors which may affect its value. Observing the trends in the ORi™ value would help to titrate oxygen therapy in vulnerable patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Szmuk P, Steiner JW, Olomu PN, Ploski RP, Sessler DI, Ezri T, et al. Oxygen reserve index: A Novel noninvasive measure of oxygen reserve – A pilot study. Anesthesiology. 2016;124:779–84. doi: 10.1097/ALN.0000000000001009. [DOI] [PubMed] [Google Scholar]
- 2.Applegate RL, 2nd, Dorotta IL, Wells B, Juma D, Applegate PM. The relationship between oxygen reserve index and arterial partial pressure of oxygen during surgery. Anesth Analg. 2016;123:626–33. doi: 10.1213/ANE.0000000000001262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perrone S, Bracciali C, Di Virgilio N, Buonocore G. Oxygen use in neonatal care: A Two-edged sword. Front Pediatr. 2016;4:143. doi: 10.3389/fped.2016.00143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tobias JD. Anaesthesia for neonatal thoracic surgery. Best Pract Res Clin Anaesthesiol. 2004;18:303–20. doi: 10.1016/j.bpa.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Scheeren TW, Belda FJ, Perel A. The oxygen reserve index (ORI): A new tool to monitor oxygen therapy. J Clin Monit Comput. 2017 Aug 8; doi: 10.1007/s10877-017-0049-4. [Epub ahead of print] Review. PubMed PMID: 28791567. [DOI] [PMC free article] [PubMed] [Google Scholar]


