Abstract
Background
Physician multisite practicing may affect access to care. However, study measuring the degree of multisite practicing is generally lacking. This study aimed to describe physician multisite practicing patterns in Georgia and to assess its impact on access to care.
Methods
Using data from the Georgia Medicaid Management Information System, the American Medical Association Physician Masterfile, and the US Census, mean number of practice sites per physician was calculated. Counts of sites per physician were then modeled in a negative binomial regression. Local differences in spatial accessibility were assessed based on single-site verse multisite practice locations.
Results
Among 20,116 physicians (mean age, 49.4 years; 30.5% female) in Georgia, 63.2% reported multiple practice sites. The average practice sites per physician was 3.3 overall, 2.6 for primary care physicians, and 3.6 for other physicians. Younger age, male sex, and practicing in group practice setting were associated with a higher number of practice sites per physician. Spatial accessibility index changed substantially when controlling for multiple practice sites.
Conclusions
Physician multisite practicing was prevalent and affected geographic access to care. More research and investment into health workforce information infrastructure seem warranted to accommodate changing physician practice patterns in data collection and dissemination.
Keywords: Access to Health Care, American Medical Association, Census, Georgia, Group Practice, Medicaid, Primary Care Physicians
An estimated 72% of land mass in the United States are currently designated as primary care health professional shortage areas, with >105 million individuals residing in these areas.1 Accurate physician practice location information is therefore important to assess health care accessibility and conduct health workforce planning. However, collection of data regarding physician practice locations has been inconsistent, mixed with public/private initiatives with variable completeness and data quality.2–5 National estimates are insufficient to assess the specific future workforce needs of state and local areas. For planners and policymakers, the correct identification of physicians’ practice locations is critical, yet tremendous uncertainty endures in their use of existing national workforce data sets. The collection and geocoding of health workforce data reveal 3 uncertainty issues of particular concern in the derivation of correct physician practice locations: (1) uncertainty in survey results, such as the accuracy of address information collected6–8; (2) uncertainty in the road network data, which are the source for geocoding and deriving latitude and longitude from address information9,10; and (3) uncertainty about whether the addresses are practice addresses or home addresses.11–13 However, an additional layer of spatial uncertainty exists in physician practice locations: multisite practicing. Most of the literature has focused on the first 3 issues and largely ignored multisite practicing; there is a general lack of study on multisite practicing, largely because of the dearth of workforce data capturing such practice patterns.
Physician multisite practicing attained international attention when it became a focal point in China’s recent health care reform.14 Because physicians generally practice in a single hospital in China, allowing physicians to practice in multiple sites seems to raise many interesting questions regarding topics such as health care access and equitable distribution of health care services. However, physician multisite practicing is common in the United States. Many physicians have multiple hospital privileges and others serve in multisite group practices.15,16 Multisite practicing adds a new layer of spatial uncertainty to physician practice location. It raises concerns about overestimating or underestimating physician availability in specific areas, potentially resulting in misinformed and poorly defined intervention and public policy. However, very few studies have examined physician multisite practicing. Cromley and Albertsen17 found that multisite practice was common and affected distribution of services. They mailed a questionnaire to all urologists practicing in north-central Connecticut and adjacent communities in September 1990. They based their study on branching as a strategy for physicians when capacity cannot be increased at a current location that remains a valuable service site or when the ability to serve new and existing markets can be improved or sustained by locating second-order service sites. However, the study is nearly 3 decades old and was based on a single specialty among 17 practices with 33 physicians. Their findings may not be generalizable to other physicians nor to other areas of the nation. In 2015, 860,939 physicians were actively practicing in the United States.18
Another recent policy relevant to multiple practice locations is the electronic health record (EHR) certification from the Centers for Medicare & Medicaid Services (CMS).19 CMS rules state that 50% of an eligible professional’s total patient encounters must be at a location where certified EHR technology is available. They must base all meaningful use measures only on the encounters that occur at those locations. We did not find any new study on multisite practice in the more current medical literature, most likely because of scarce data availability on physician multisite practicing. The degree of physicians having multiple practice locations and its impact on population spatial accessibility remain woefully unexplored, given its assumed impacts on health care access and health workforce planning and projections.
The enactment of the Affordable Care Act (ACA) made it possible for some states to collect more complete data on multiple practice locations. Georgia is one such state that collects provider data on multiple practice locations. The Georgia Department of Community Health Medicaid Management Information System (MMIS) collects data regarding the service locations of registered health care providers in the state per ACA requirements. This unique data set provides insights to the prevalence of multisite practicing among health care providers, including physicians. This study assesses the prevalence of multisite practicing among physicians in Georgia and its impact on spatial accessibility to physician services. The study also examined whether multisite practicing varies based on physician characteristics and assessed the impact of multisite practicing on local spatial accessibility.
Methods
Data Sources
Most providers in Georgia traditionally have enrolled in the Georgia Medicaid program to furnish covered services to Medicaid beneficiaries and to submit claims for such services. However, the ACA requires physicians and other eligible practitioners to enroll in the Medicaid Program in order to order, prescribe, and refer (OPR) items or services for Medicaid beneficiaries, even when they do not submit claims to Medicaid.20–22 Effective April 1, 2013, physicians and other practitioners who OPR items or services for Medicaid beneficiaries but who choose not to submit claims to Medicaid began enrolling in the Georgia Medicaid OPR Provider program. Providers are required to be enrolled at each physical service location where they see patients. The Georgia MMIS provides fee-for-service and OPR-only provider enrollment data to the public free of charge; it is the statewide information management system that handles Medicaid claims. The provider list tallies registered health care providers and provides their national provider identifier (NPI) along with each physical service location where they see patients.
We obtained the September 30, 2016, Georgia MMIS data snapshot.23 Physicians who were fee-for-service providers (n = 24,296) and OPR-only providers (n = 1,936) were included in this study. Georgia MMIS data were linked to CMS NPI data (October 9, 2016, data snapshot) and the 2016 American Medical Association (AMA) Physician Masterfile (December 31, 2016, data snapshot). CMS began to issue NPIs in 2006, and beginning in May 2008, physicians were required to include their NPI on claims in order to receive payment for Medicare services from CMS. An NPI is permanently associated with a specific individual regardless of any changes in practice location or additional specialty training. The role of CMS in issuing NPIs is independent of its role as a payer for Medicare services, and health care providers are required to have an NPI—regardless of whether they bill Medicare for services—in order to transfer claims and other health care information electronically.24 The AMA Masterfile includes data on all current physicians residing in the United States who meet the educational and credentialing requirements to be recognized as physicians.25 This data set provides a nearly complete list of US physicians and includes not only physicians’ addresses, but also practice type, specialty, age, sex, employment settings, primary professional activities, and other data.
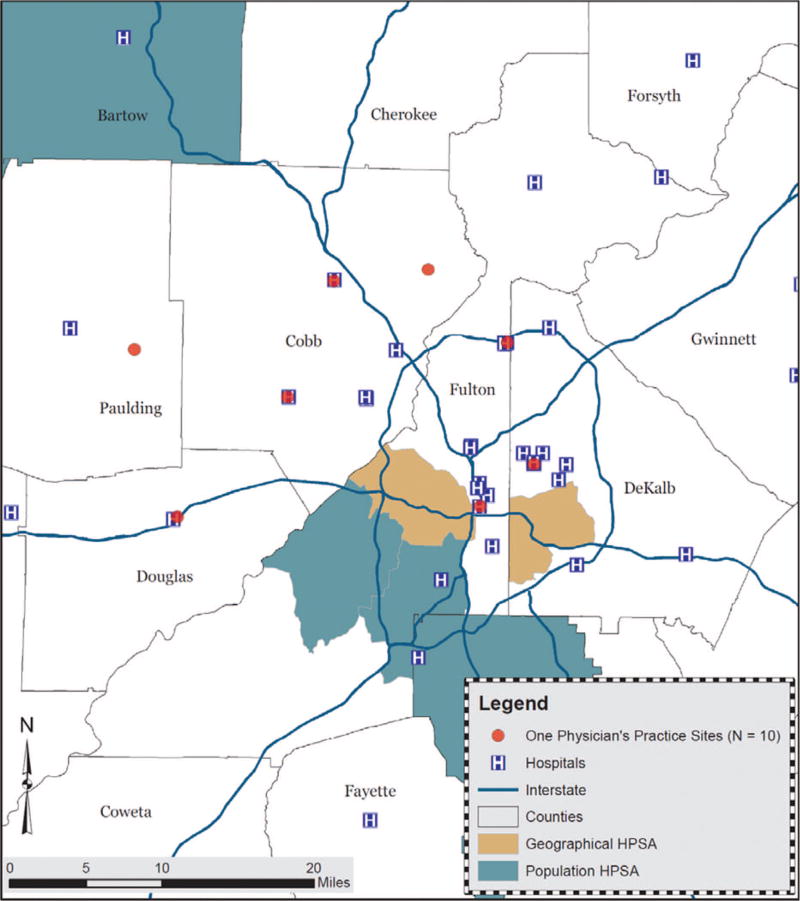
The NPI and AMA Masterfile data provide information for only 1 practice location, whereas in the Georgia MMIS data, a physician could have multiple practice locations. Figure 1 illustrates the multisite practice locations of 1 physician. The map shows the 10 service sites of a urologist who also specializes female urology/pelvic medicine and reconstructive surgery in Atlanta metropolitan area. For this provider, we verified all location addresses with an existing medical practice or hospital locations through online research. The 10 practice sites include 2 cancer treatment centers, 2 hospitals, 3 imaging centers, and 3 urology group practices at 10 different locations across 5 counties.
Figure 1.
An example of 10 practice locations of a urologist who also subspecializes in female urology/pelvic medicine and reconstructive surgery in the Atlanta metropolitan area. Data are based on the Georgia Medicaid Management Information System. The 10 practice sites include 2 cancer treatment centers, 2 hospitals, 3 medical imaging centers, and 3 urologic treatment centers in 10 different locations across 5 counties. HPSA, primary care health professional shortage area (snapshot as of February 8, 2014).
MMIS data were geocoded with the 2013 North America StreetMap database.26 Descriptive statistics were used to describe the number of multiple practice sites stratified by physician characteristics such as age, sex, specialty, international medical graduate (IMG) status, and primary employment setting. The physician characteristics were obtained from the AMA Physician Masterfile.
Statistical Analysis
We calculated mean, median, and 75th, 90th, and 95th percentiles for the number of practice sites per physician by physician characteristics. We also modeled the number of practice sites per physician by physician characteristics via the negative binomial regression model. Negative binomial regression is often used to model count variables, especially for overdispersed count outcome variables. It can be considered as a generalization of Poisson regression because it has the same mean structure as Poisson regression, with an extra parameter to model the overdispersion.
Spatial Analysis
We calculated drive time (up to 60 minutes) among population-weighted centroids of census block groups in Georgia (n = 5533). Drive time calculation is necessary to analyze spatial accessibility. Block group was used as the basic geographic unit for spatial accessibility analysis because physician data were geocoded and aggregated at the block group level, and it is a more meaningful proxy for local communities. Population-weighted block group centroids were obtained by computing the weighted coordinates based on block-level population data—the smallest geographic unit that census tabulates data. Using the population-weighted centroids to represent the block group location is considered to be more accurate than simply using the geographic centroids. The differences between them can be significant, particularly in rural and remote areas, where populations tend to concentrate in a limited space.27–29
Changes in spatial accessibility index were calculated from single-site practice locations compared with that from weighted multisite practice locations. Spatial accessibility is calculated with the 2-step floating catchment area (2SFCA) method, with a 30-minute drive time threshold.27,30 This method is a special case of the classical gravity model. The “floating catchment area” method was first used by Peng31 to study urban job accessibility. Luo and Wang27 built on that method to account for both supply and demand in 2SFCA. The general 2SFCA method starts with generating a provider-to-population ratio in each provider location, such as a census block group centroid. The total number of providers in that census block group is assigned to the census block group centroid. The total number of providers assigned to the census block group centroid is then divided by the population living within that centroid’s catchment areas within a threshold value (eg, 30-minute drive time). This ratio computation is repeated for all census block groups. Population points are the focus in the second step. For each population point (eg, a census block group centroid), a spatial accessibility value is obtained by summing the provider-to-population ratios of all the provider catchments that overlie the point, as determined in the first step. The summed supply ratios obtained in this way are assigned to the entire census block group area represented by the population point.
To calculate the spatial accessibility index with single-site practice locations, 1 Georgian address was randomly selected for physicians with multiple locations. To calculate spatial accessibility index with multisite practice locations, equal weights were assumed for physicians with multiple service locations; for physicians with N locations, each location is weighted down by a factor of 1/N. Therefore, the total number of providers are equal in 2 spatial accessibility calculations. We summarized population between areas with improved spatial accessibility and those with worsened spatial accessibility across the state for the rural population, black population, and population aged ≥65 years. We used census block group population data from the 2015 American Community Survey 5-year Estimates as the base population.32 Statistical analysis was conducted with SAS 9.3 (SAS Institute, Inc., Cary, NC) and thematic map was created with ArcGIS 10.2 (ESRI, Redlands, CA).
Results
A total of 6116 registered physicians in MMIS had no service location inside Georgia. Excluding these physicians left 20,116 physicians for subsequent analysis (mean age, 49.4 years; 30.5% female). Of these remaining physicians, 639 (3.2%) were not found in the AMA Masterfile. With regard to service locations, 36.8% (n = 7394) of the physicians practiced at a single site; 20% (4,026) had 2 service locations, 13.9% (n = 2793) had 3 service locations, 8.9% (n = 1799) had 4 service locations, 5.9% (n = 1193) had 5 offices, and the remaining 14.5% (n = 2911) had ≥6 locations. The average number of practice locations per physician was 3.3 (Table 1). However, the average number of service locations decreased as physician age increased: physicians aged <40 years had a mean of 3.6 service locations per physician; this number dropped to 2.7 service locations per physician for physicians aged ≥60 years. Female physicians had a lower mean number of service locations than male physicians (3 vs 3.4 service locations/physician). The same was true for IMGs (3.2) versus non-IMGs (3.3). Physicians employed in a group practice setting (3.5) tended to have a higher number of sites per physician than those employed in solo (2.1) or 2-physician practices (2.4).
Table 1.
Number of Practice Sites per Physician Based on Registered Physician Provider Data from Georgia Medicaid Management Information System
| Percentiles | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Number of Physicians | Mean | Median | 75th | 90th | 95th | |
| All | 20,116 | 3.3 | 2 | 4 | 7 | 9 |
| Age (years) | ||||||
| <40 | 4,651 | 3.6 | 2 | 4 | 7 | 9 |
| 40–49 | 6,140 | 3.5 | 2 | 4 | 7 | 9 |
| 50–59 | 4,514 | 3.2 | 2 | 4 | 6 | 9 |
| ≥60 | 4,155 | 2.7 | 2 | 3 | 6 | 7 |
| Unknown | 656 | 3.1 | 2 | 3 | 6 | 8 |
| Sex | ||||||
| Male | 13,332 | 3.4 | 2 | 4 | 7 | 9 |
| Female | 6,136 | 3 | 2 | 4 | 6 | 8 |
| Unknown | 648 | 3.1 | 2 | 4 | 6 | 8 |
| IMG status | ||||||
| IMG | 4,397 | 3.2 | 2 | 4 | 7 | 9 |
| Non-IMG | 15,080 | 3.3 | 2 | 4 | 7 | 9 |
| Unknown | 639 | 3.1 | 2 | 4 | 6 | 8 |
| Present employment setting | ||||||
| Self-employed solo practice | 2,170 | 2. 1 | 1 | 2 | 4 | 6 |
| Two-physician practice | 572 | 2.4 | 2 | 3 | 5 | 6 |
| Group practice | 8,694 | 3.5 | 2 | 4 | 7 | 9 |
| Medical school | 355 | 3.4 | 2 | 4 | 6 | 8 |
| State/local | 2,408 | 3.3 | 2 | 4 | 6 | 8 |
| Federal | 113 | 3.2 | 2 | 4 | 7 | 9 |
| Other | 5,804 | 3.4 | 2 | 4 | 7 | 9 |
| Primary specialty | ||||||
| Non-primary care | 12,982 | 3.6 | 2 | 4 | 7 | 10 |
| Primary care | 6,495 | 2.6 | 2 | 3 | 6 | 7 |
| Family medicine | 2,202 | 2.8 | 2 | 3 | 6 | 8 |
| General practice | 95 | 2 | 1 | 2 | 4 | 5 |
| Internal medicine | 2,643 | 2.6 | 2 | 3 | 5 | 7 |
| Pediatrics | 1,555 | 2.6 | 2 | 3 | 6 | 7 |
| Unknown | 639 | 3.1 | 2 | 4 | 6 | 8 |
| Other select specialties | ||||||
| Anesthesiology | 894 | 3.5 | 2 | 4 | 7 | 10 |
| Cardiovascular diseases | 582 | 4.5 | 4 | 6 | 9 | 10 |
| Diagnostic radiology | 716 | 8.7 | 4 | 9 | 25 | 41 |
| Endocrinology, diabetes and metabolism | 121 | 1.9 | 1 | 2 | 3 | 4 |
| Emergency medicine | 1,093 | 2.9 | 2 | 4 | 5 | 6 |
| Gastroenterology | 393 | 3.3 | 2 | 5 | 7 | 8 |
| General surgery | 614 | 2.7 | 2 | 4 | 5 | 7 |
| Nephrology | 341 | 6 | 4 | 8 | 14 | 20 |
| Neurology | 309 | 2.7 | 2 | 4 | 5 | 7 |
| Neuroradiology | 104 | 11.7 | 6 | 14 | 34 | 44 |
| Obstetrics and gynecology | 1,077 | 2.7 | 2 | 4 | 5 | 7 |
| Orthopedic surgery | 524 | 3.2 | 2 | 4 | 7 | 8 |
| Otolaryngology | 278 | 4 | 3 | 5 | 7 | 13 |
| Psychiatry | 508 | 1.8 | 1 | 2 | 3 | 4 |
| Plastic surgery | 137 | 2 | 1 | 2 | 4 | 7 |
| Urology | 249 | 3.3 | 2 | 5 | 8 | 9 |
| Vascular and interventional radiology | 109 | 7.9 | 5 | 9 | 18 | 30 |
IMG, international medical graduate.
The number of service locations also varied by physician specialty. Subspecialists had, on average, a higher number of practice locations than primary care physicians (3.6 vs 2.6 locations/physician). Overall, some specialties had a much higher than average number of locations per physician; for instance, neuroradiologists (n = 104) had, on average, 11.7 service locations per physician; diagnostic radiologists (n = 716) had 8.7 service locations per physician; and vascular and vascular interventional radiologists (n = 109) had 7.9 service locations per physician. On the other hand, some specialties had a lower than average number of offices per physician: Psychiatrists (n = 508) had, on average, 1.8 service locations per physician; endocrinologists (n = 121) had 1.9 service locations per physician; and plastic surgeons (n = 137) had 2 service locations per physician.
Negative binomial regression results similarly suggest a negative association between physician age and the number of practice sites per physician (Table 2). Female physicians still tended to have a smaller number of practice sites compared with male physicians, even when controlling for other factors such as age, specialty, and employment setting. Controlling for other factors, IMGs did not differ significantly from non-IMGs. Those in medical school and a federal institution setting had a similar number of sites per physician compared with those in a group practice setting, whereas those in solo or 2-physician practice settings tended to have a smaller number of practice sites per physician than did physicians in group practice. Physician specialty continued to be an important predictor of the number of practice sites per physician, even when controlling for other physician characteristics.
Table 2.
Negative Binomial Regression Predicting the Number of Practice Sites per Physician
| Estimate | SE | 95% LCLM | 95% UCLM | P Value | |
|---|---|---|---|---|---|
| Intercept | 1.1833 | 0.0159 | 1.1521 | 1.2144 | <.0001 |
| Age (years) | |||||
| <40 | 0.2884 | 0.0205 | 0.2482 | 0.3287 | <.0001 |
| 40–49 | 0.2704 | 0.0181 | 0.235 | 0.3058 | <.0001 |
| 50–59 | 0.1591 | 0.0189 | 0.122 | 0.1962 | <.0001 |
| ≥60 | Reference | ||||
| Sex | |||||
| Male | Reference | ||||
| Female | −0.1544 | 0.0139 | −0.1816 | −0.1273 | <.0001 |
| IMG status | |||||
| IMG | 0.0268 | 0.015 | −0.0026 | 0.0562 | .0735 |
| Non-IMG | Reference | ||||
| Present employment setting | |||||
| Self-employed solo practice | −0.4138 | 0.0225 | −0.4579 | −0.3696 | <.0001 |
| Two-physician practice | −0.32 | 0.0394 | −0.3973 | −0.2427 | <.0001 |
| Group practice | Reference | ||||
| Medical school | −0.0603 | 0.0457 | −0.1499 | 0.0293 | .1873 |
| State/local | −0.0749 | 0.0196 | −0.1132 | −0.0366 | .0001 |
| Federal | −0.1233 | 0.081 | −0.2819 | 0.0354 | .1279 |
| Others | −0.0662 | 0.0162 | −0.0979 | −0.0345 | <.0001 |
| Primary Specialty | |||||
| Non–primary care | Reference | ||||
| Primary care | −0.2781 | 0.0138 | −0.3052 | −0.2511 | <.0001 |
| Dispersion | 0.409 | 0.0066 | 0.3963 | 0.4221 |
A total of 19,451 cases were used; 665 cases were excluded because of missing values.
IMG, international medical graduate; LCLM, Lower Confidence Limit; SE, standard error; UCLM, Upper Confidence Limit.
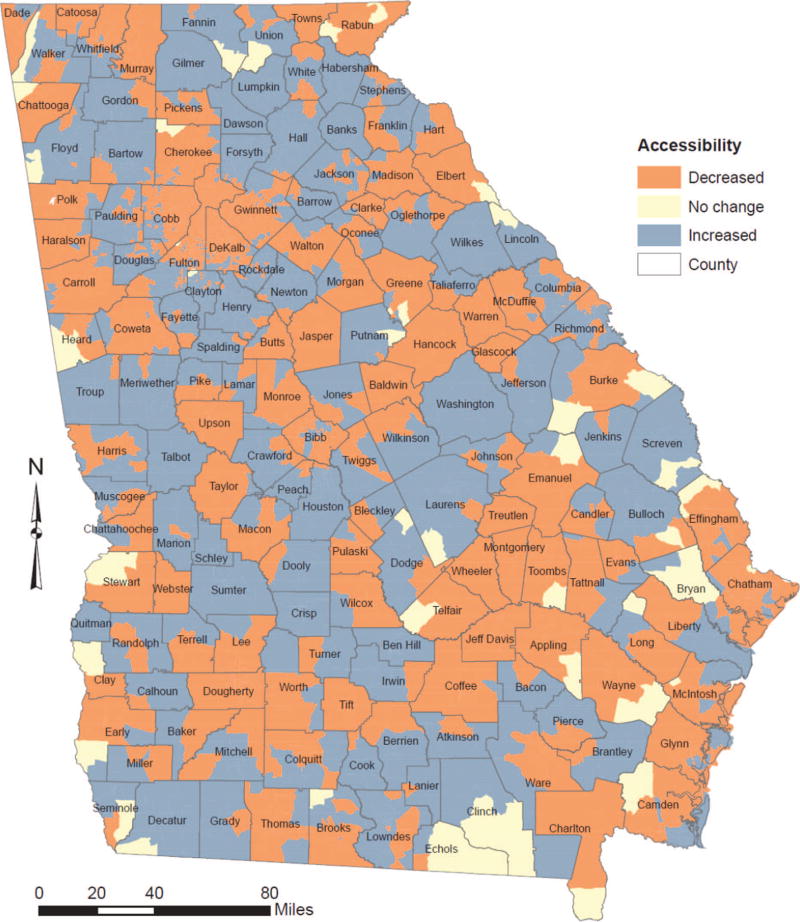
Adjusting for the multisite locations of physicians resulted in visible changes in local spatial accessibility. The accessibility index improved for 41% and decreased for 58% of Georgia’s estimated 10 million population. In a similar way, the accessibility index improved for 42% of population aged ≥65 years and 43% of the black population; it decreased for 57% of both of these populations. Changes in rural areas were more evenly split: half of the rural population had improved accessibility and the other half had decreased accessibility. By contrast, urban areas experienced a larger decrease in spatial accessibility to physicians. The change in spatial accessibility had a very regional pattern: the mid-central and southeastern parts of the state experienced larger decreases in spatial accessibility, whereas the northern and east-central areas of the state saw improvements (Figure 2).
Figure 2.
Map of change in local spatial accessibility after adjusting for the multiple practice sites.
Discussion
Georgia MMIS data provided an opportunity to study multisite practicing patterns among physicians. The physicians in Georgia MMIS data (n = 20,116) are close to the active number of physicians reported in the AMA Masterfile (n = 22,303).33 The AMA Masterfile was believed to overestimate supply, especially for older active physicians, because of lags in posting physician retirements.34 This study found that two thirds of the physicians in Georgia practiced in >1 service location. Certain specialties had a much higher mean number of locations per physician. Furthermore, the pattern also varied by physician age, sex, and IMG status. Overall, male physicians, younger physicians, and those in a group practice setting tended to have higher mean number of practice locations per physician.
In this time of health care reform and a looming physician workforce shortages35, accurate information on physician practice location has tremendous policy implications and may affect the designation of medically underserved areas, because access to physician services is becoming more important for realizing the benefits of the insurance coverage increases. Studying multisite practicing may help lead to more efficient and equitable allocation of medical resources.
This study also highlights the infrastructure needs around US health workforce information. Traditional databases of the physician workforce, such as the AMA Masterfile, NPI, and state licensure data, are based on storing information of a single practice location. The Georgia MMIS data provide a unique opportunity to study how to acquire, store, and distribute multisite practice location data. The Georgia data collection effort is a state-led initiative in a direct response to the enactment of ACA. What Georgia did could be replicated in other states, although Medicaid administration varies from state to state. Once such efforts are made to collect multisite practicing information for health care providers, better health workforce data will help allocate precious resources more equitably, and better workforce planning could also become easier to achieve. As EHR adoption rises36,37, data on patient encounters can also be more easily linked to the actual point of service delivery. This information can be used to scientifically assess the actual availability of physician services in a given geographic area.
Furthermore, while half of the state’s population experienced increase in spatial accessibility to physician services, multisite practicing seems to affect certain areas more profoundly, especially urban areas. Continued attention to obtaining accurate data on practice location is therefore important to understand better the effect of multisite physician practices on health care access. However, the gaps in data quality introduce spatial uncertainty about actual provider service locations and may thus lead to biased estimates of local accessibility; for instance, they could lead to ineffective designation of medically underserved areas.
Nevertheless, this study provides novel insights into physician service delivery trends. It showcases the limitations of traditional data sources with a single practice location for workforce planning and assessment. The findings call for national dialog on public-private collaborations to create and maintain a modern and up-to-date health workforce information infrastructure by way of harnessing information from EHRs, as well as health insurance data, claims data, and administrative data, to provide to the general public, research communities, and policymakers more accurate, timely, accessible, and easy-to-use health workforce data.
This study has a number of limitations. First, the generalizability of finding may be limited. Whether multisite practicing is similar in other states remains to be explored. Second, equal weights for multiple practice sites were assumed. Because allocation of work hours among physician practice sites is unknown, we randomly choose 1 site for the spatial accessibility computation based on a single site. Similarly, we assigned equal weights for the spatial accessibility computation based on multiple sites. This may not realistically reflect actual health service delivery patterns. Third, uncertainty exists as to whether some physicians’ locations were simply patient sign-up locations for the health care systems to which the physicians may belong. However, the existence of locations where these physicians could deliver their services can influence patient access and is therefore worth exploring.
Conclusions
This study determined the prevalence of multisite practicing among physicians in Georgia. The majority of physicians engaged in multisite practicing. On average, physicians practiced at 3 different sites. Young, male, and subspecialist physicians, as well as those in group practice, had a higher number of practice sites per physician. Adjusting for physician multisite practice locations differentially affected spatial accessibility across the state. Given the prevalence of multisite practicing among physicians and its impact on public access to health care, more research is needed on its effects on service distribution. Improvement of health workforce information infrastructure to accommodate the changing physician practice patterns also seems warranted.
Acknowledgments
Funding: This work was supported in part by the National Cancer Institute (grant 1CA182874). The sponsor had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. This work was completed while Dr. Xierali was with the Association of American Medical Colleges, Washington, DC.
Footnotes
Conflict of interest: none declared.
Disclaimer: The content of this article is solely the responsibility of the author and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
References
- 1.Xierali IM, Fair MA, Johnson S, et al. Do free clinic experiences enhance medical student commitment to underserved areas? [Accessed June 6, 2016];Analysis in Brief. 2016 16(2) Available from: https://www.aamc.org/download/454750/data/february2016dofreeclinicexperiencesenhancemedicalstudentcommitm.pdf. [Google Scholar]
- 2.Armstrong D, Moore J Health Workforce Technical Assistance Center. The Health Workforce Minimum Data Set (MDS): what you need to know. [Accessed December 13, 2016];Resource brief. 2015 Jan; Available from: http://www.healthworkforceta.org/wp-content/uploads/2016/08/MDS_Resource_Brief.pdf.
- 3.World Health Organization; University of Technology Sydney. [Accessed December 13, 2016];WHO human resources for health minimum data set. Available from: http://www.who.int/hrh/documents/hrh_minimum_data_set.pdf.
- 4.Staiger DO, Auerbach DI, Buerhaus PI. Comparison of physician workforce estimates and supply projections. JAMA. 2009;302:1674–80. doi: 10.1001/jama.2009.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DesRoches CM, Barrett KA, Harvey BE, et al. The results are only as good as the sample: assessing three national physician sampling frames. J Gen Intern Med. 2015;30(Suppl 3):S595–601. doi: 10.1007/s11606-015-3380-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi W. Principles of modeling uncertainties in spatial data and spatial analyses. Boca Raton, FL: CRC Press; 2010. [Google Scholar]
- 7.Lam NS. Geospatial methods for reducing uncertainties in environmental health risk assessment: challenges and opportunities. Ann Assoc Am Geogr. 2012;102:942–50. [Google Scholar]
- 8.Zandbergen PA, Hart TC, Lenzer KE, Camponovo ME. Error propagation models to examine the effects of geocoding quality on spatial analysis of individual-level datasets. Spat Spatiotemporal Epidemiol. 2012;3:69–82. doi: 10.1016/j.sste.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bell S, Wilson K, Shah TI, Gersher S, Elliott T. Investigating impacts of positional error on potential health care accessibility. Spat Spatiotemporal Epidemiol. 2012;3:17–29. doi: 10.1016/j.sste.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Shi X, Alford-Teaster J, Onega T, Wang D. Spatial access and local demand for major cancer care facilities in the United States. Ann Assoc Am Geogr. 2012;102:1125–34. [Google Scholar]
- 11.Shumsky NL, Bohland J, Knox P. Separating doctors’ homes and doctors’ offices: San Francisco, 1881–1941. Soc Sci Med. 1986;23:1051–7. doi: 10.1016/0277-9536(86)90263-7. [DOI] [PubMed] [Google Scholar]
- 12.McLafferty S, Freeman VL, Barrett RE, Luo L, Shockley A. Spatial error in geocoding physician location data from the AMA Physician Masterfile: implications for spatial accessibility analysis. Spat Spatiotemporal Epidemiol. 2012;3:31–8. doi: 10.1016/j.sste.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Shi X, Xue B, Xierali IM. Identifying the uncertainty in physician practice location through spatial analytics and text mining. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13090930. Pii: E930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu K, Sun Z, Rui Y, Gu S. Multisite licence to practise medicine in China. Lancet. 2014;384:743. doi: 10.1016/S0140-6736(14)61434-3. [DOI] [PubMed] [Google Scholar]
- 15.Clinton C, Schmittling G, Stern TL, Black RR. Hospital privileges for family physicians: a national study of office based members of the American Academy of Family physicians. J Fam Pract. 1981;13:361–71. [PubMed] [Google Scholar]
- 16.Rauch DA Committee on Hospital Care; Section on Hospital Medicine. Medical staff appointment and delineation of pediatric privileges in hospitals. Pediatrics. 2012;129:784–7. doi: 10.1542/peds.2011-3866. [DOI] [PubMed] [Google Scholar]
- 17.Cromley EK, Albertsen PC. Multiple-site physician practices and their effect on service distribution. Health Serv Res. 1993;28:503–22. [PMC free article] [PubMed] [Google Scholar]
- 18.Association of American Medical Colleges. [Accessed May 26, 2017];Active physicians in the largest specialties, 2015. Table 1.1 Number of active physicians in the largest specialties by major professional activity, 2015. Available from: https://www.aamc.org/data/workforce/reports/458480/1–1-chart.html.
- 19.Centers for Medicare & Medicaid Services. [Accessed May 26, 2017];Guide for eligible professionals practicing in multiple locations (EHR incentive programs in 2015 through 2017) Updated: March 2016. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2016_EPMultipleLocations.pdf.
- 20.FAQ: new Medicaid requirements for ordering, prescribing or referring providers: an overview. Atlanta: Georgia Department of Community Health; [Accessed December 26, 2016]. Available from: https://www.mmis.georgia.gov/portal/Portals/0/StaticContent/Public/ALL/NOTICES/OPR%20FAQ%2020-08-2013%20163045%2020-03-2015%20163053.pdf. [Google Scholar]
- 21. [Accessed December 26, 2016];Title 42 - Public Health, chapter IV (10–1-11 edition). Section 455–410: enrollment and screening of providers. Available from: https://www.gpo.gov/fdsys/pkg/CFR-2011-title42-vol4/pdf/CFR-2011-title42-vol4-sec455–410.pdf.
- 22. [Accessed December 26, 2016];Title 42 - Public Health, chapter IV (10–1-11 edition). Section 455.440: national provider identifier. Available from: https://www.gpo.gov/fdsys/pkg/CFR-2011-title42-vol4/pdf/CFR-2011-title42-vol4-sec455–440.pdf.
- 23.Georgia Medicaid Management Information System (MMIS) Atlanta: Georgia Department of Community Health; [Accessed October 19, 2016]. Available from: https://dch.georgia.gov/medicaid-management-information-system-mmis. [Google Scholar]
- 24.Bindman AB. Using the national provider identifier for health care workforce evaluation. Medicare Medicaid Res Rev. 2013;3 doi: 10.5600/mmrr.003.03.b03. pii: mmrr.003.03.b03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.AMA physician masterfile. Chicago: American Medical Association; [Accessed April 12, 2015]. Available from: http://www.ama-assn.org/ama/pub/about-ama/physician-data-resources/physician-masterfile.page. [Google Scholar]
- 26.U.S. and Canada StreetMap. ESRI data & maps. Redland, CA: ESRI; 2014. [Google Scholar]
- 27.Luo W, Wang F. Measures of spatial accessibility to healthcare in a GIS environment: synthesis and a case study in Chicago region. Environ Plan B Urban Anal City Sci. 2003;30:865–84. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jia P, Xierali IM, Wang F. Evaluating and re-demarcating the hospital service areas in Florida. Appl Geogr. 2015;60:248–53. [Google Scholar]
- 29.Jia P, Wang F, Xierali IM. Using a Huff-based model to delineate hospital service areas. Prof Geogr. 2017;69:522–30. [Google Scholar]
- 30.Wang F. Measurement, optimization, and impact of health care accessibility. Ann Assoc Am Geogr. 2012;102:1104–12. doi: 10.1080/00045608.2012.657146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng Z. The jobs-housing balance and urban commuting. Urban Stud. 1997;34:1215–35. [Google Scholar]
- 32.American Community Survey (ACS): summary data file. 5-Year estimates. Washington, DC: U.S. Department of Commerce; [Accessed March 17, 2017]. Available from: https://www.census.gov/programs-surveys/acs/data/summary-file.html. [Google Scholar]
- 33.Georgia physician workforce profile. Washington, DC: Association of American Medical Colleges; 2015. [Accessed May 26, 2017]. Available from: https://www.aamc.org/download/447164/data/georgiaprofile.pdf. [Google Scholar]
- 34.Kletke PR. Physician workforce data: when the best is not good enough. Health Serv Res. 2004;39:1251–6. doi: 10.1111/j.1475-6773.2004.00288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dall T, Chakrabarti R, Iacobucci W, Hansari A, West T. IHS Markit. [Accessed May 26, 2017];2017 Update: the complexities of physician supply and demand: projections from 2015 to 2030. Final report. 2017 Feb 28; Available from: https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565–14ec-48fb-974b–99fafaeecb00/aamc_projections_update_2017.pdf.
- 36.Xierali IM, Hsiao CJ, Puffer JC, et al. The rise of electronic health record adoption among family physicians. Ann Fam Med. 2013;11:14–9. doi: 10.1370/afm.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsiao C-J, Hing E. NCHS data brief no. 143. Hyattsville, MD: National Center for Health Statistics; 2014. [Accessed May 26, 2017]. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2013. Available from: https://www.cdc.gov/nchs/data/databriefs/db143.pdf. [PubMed] [Google Scholar]