Abstract
Prosthetic valve endocarditis due to Cardiobacterium hominis is rare and recommended therapy includes a third generation cephalosporin. We report a case of Cardiobacterium hominis endocarditis post transcatheter aortic valve replacement in a patient with significant beta-lactam antimicrobial sensitivities who was successfully treated with ciprofloxacin monotherapy in conjunction with surgery.
Keywords: Cardiobacterium, Endocarditis, Ciprofloxacin, Fluoroquinolones
Case report
A 78-year-old man was referred to the hospital by his primary care physician for intravenous antibacterial therapy after 2 sets of blood cultures grew Cardiobacterium hominis. One week earlier he had been hospitalized for exertional chest tightness radiating into his jaw, bilateral peripheral edema, and severe anemia due to lower gastrointestinal blood loss. Troponin was mildly elevated at 0.2 ng/mL, BNP was 671 pg/mL and electrocardiogram showed sinus rhythm with nonspecific repolarization changes. His hemoglobin was 6.7 g/dL and he received 2 units of packed cells. During the transfusion he developed a fever of 38.9 °C, so 2 sets of peripheral blood cultures were drawn. He had no additional fevers, received no antimicrobials during that hospital stay, and was discharged. Both blood culture sets grew Cardiobacterium hominis, so the patient was asked to return to the hospital.
On readmission he reported a history of intermittent low grade fevers, chills, increasing fatigue, worsening anemia, and bilateral leg swelling unresponsive to diuretics over the last 4 months. He had a significant cardiac history which included non-Q wave myocardial infarction in 2010, coronary angioplasty and stent of proximal left circumflex in 2013, cardiac catheterization with intervention to the left anterior descending in 2013, repeat cardiac catheterization in 2015 with drug eluting stent to the left circumflex, and aortic stenosis with transcatheter aortic valve replacement (TAVR) with a SAPIEN (Edwards Lifesciences Corporation) valve in 2015. In addition he had a history of chronic systolic and diastolic congestive heart failure, hypertension, hyperlipidemia, and prostate cancer status post radiation treatments.
Vital signs on admission included a temperature of 36.9 °C, heart rate of 94 beats per minute, respiratory rate of 18 breaths per minute, blood pressure of 132/57 mm Hg. Oxygen saturation was 99% on room air. On physical exam a systolic murmur was noted with no peripheral signs of endocarditis. The white blood cell count was 9.4 × 103/uL, hemoglobin: 8.6 g/dL, and platelets were 210 × 103/uL. The sedimentation rate was 75 mm/h, and C-reactive protein of 11.4 mg/dL. The blood urea nitrogen (BUN) was elevated at 37 mg/dL with a serum creatinine of 1.25 mg/dL. A transesophageal echocardiogram (TEE) revealed a small vegetation or mass on the aortic valve with a mild to moderate perivalvular leak and no abscess.
Repeat blood cultures drawn prior to the start of antimicrobials grew Cardiobacterium hominis. Because the patient reported a history of tongue swelling on cefazolin and a rash on penicillin, ciprofloxacin 400 mg intravenously every 12 h was begun. The isolate was sent to a reference laboratory for sensitivity testing. Minimum inhibitory concentration for the following antimicrobials was reported: ampicillin: 0.25 ug/mL (beta-lactamase negative), ceftriaxone: 1 ug/mL, ciprofloxacin: ≤0.12 ug/mL, levofloxacin: ≤0.06 ug/mL, meropenem: 0.12 ug/mL, trimethoprim-sulfamethoxazole: 0.5/9.5 ug/mL. Repeat blood cultures were negative 4 days after the initiation of ciprofloxacin therapy.
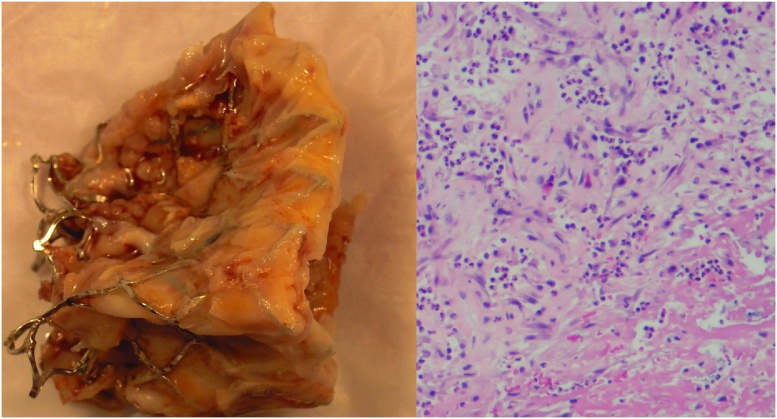
On day 6 of hospitalization, the patient experienced chest pressure radiating into his jaw. This occurred 3 days after clopidogrel and aspirin had been held for esophagogastroduodenoscopy and colonoscopy to work up gastrointestinal bleeding. Troponin was 0.08 ng/mL and electrocardiogram showed a myocardial infarction with anterolateral ST elevation. Emergent cardiac catheterization revealed severe left main and right coronary artery stenosis of 99%. The patient underwent emergent cardiac surgery consisting of removal of the SAPIEN valve, coronary artery bypass graft × 3, and aortic valve replacement. The surgeon stated that the SAPIEN valve was very difficult to remove due to many small vegetations on all of the leaflets, as well as below the leaflets and between the native valve and the SAPIEN valve (Fig. 1).
Fig. 1.
Pathology reported a 3.0 × 2.5 × 0.5 cm aggregate of yellow to green, irregular friable tissue. Culture of the valve was negative after 10 days of incubation.
On post-operative day 7 the patient developed a mediastinal and left chest hematoma that led to cardiogenic shock and he was transferred to the intensive care unit. He returned to the operating room for postoperative bleeding where 2 liters of blood were removed from the right chest. He remained in the intensive care unit for 8 days. On post-operative day 15, the antibacterial was converted to oral ciprofloxacin 500 mg twice daily. This was administered for an additional 4 weeks, resulting in a total of a 6.5 weeks (6 weeks post- surgery) of treatment. He received no other antimicrobials during hospitalization with the exception of vancomycin for surgical prophylaxis. After a 2.5 week hospital stay he was discharged to a rehabilitation center. Fourteen months later, the patient is home, clinically stable with no signs of recurrence. He did not experience any adverse events associated with ciprofloxacin therapy. Levofloxacin was recommended for dental prophylaxis.
Discussion
Cardiobacterium hominis is a gram negative coccobacillus and a member of the HACEK (Haemophilis species, Aggregatibacter species, Cardiobacterium hominis, Eikenella corrodens and Kingella species) group of bacteria known for their slow growing nature and insidious onset [1]. HACEK organisms are the causative pathogens in <10% of cases of community acquired infectious endocarditis, excluding infections in intravenous drug users [2]. This percentage may increase with the advent of matrix assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF) technology that augments a laboratory’s ability to detect this pathogen [3].
The American Heart Association/Infectious Disease Society of America endocarditis guidelines recommend ceftriaxone or another third or fourth-generation cephalosporin for treatment of HACEK endocarditis [2]. Patients with endocarditis who are unable to tolerate first line therapy can be treated with a fluoroquinolone (ciprofloxacin, levofloxacin, or moxifloxacin) for 6 weeks based on limited evidence [2]. There are only six published case reports of Cardiobacterium hominis that utilize ciprofloxacin as part of combination therapy or as salvage therapy [[4], [5], [6], [7], [8], [9]] (Table 1). Clinical cure was achieved in 5 of the 6 patients [[4], [5], [6], [7], [8]] with surgical intervention in 3 patients [[7], [8], [9]]. In 4 cases, ciprofloxacin was combined with either rifampin, ceftriaxone, ceftriaxone and gentamicin, or penicillin, gentamicin, and imipenem-cilastatin [[5], [6], [8], [9]]. Our case report is unique in that ciprofloxacin monotherapy was used for the entire course of therapy, including step-down to oral ciprofloxacin to complete 6 weeks of treatment avoiding the long term use of a peripherally inserted central line.
Table 1.
Current literature of ciprofloxacin as treatment for Cardiobacterium hominis infective endocarditis.
| Age/Gender | Type of Valve | Treatment regimen (reason for ciprofloxacin treatment) | Ciprofloxacin MIC (ug/mL) | Duration of Total Therapy, weeks (Duration of Ciprofloxacin Therapy, weeks) | Surgery | Outcome (follow up in months) |
|---|---|---|---|---|---|---|
| 78/M | AorticSAPIEN | ciprofloxacin 400 mg IV twice daily to 500 mg PO twice daily (Penicillin and cephalosporin allergy) | ≤0.12 | 6.5 | Yes | Cured (14) |
| 43/NS [4] | NS | mezlocillin and tobramycin switched to mezlocillin 4 g IV q8h for unknown duration switched to ciprofloxacin 400 mg IV for 1 dose, then 200 mg IV twice daily (renal dysfunction) | 0.06 | NS (5) | NS | Cured (NS) |
| 61/M [5] | Aortic Homograft | ceftriaxone 2 g IV daily for 3 weeks, then ciprofloxacin 750 mg PO twice daily and rifampin 450 mg PO twice daily (Ceftriaxone-induced agranulocytosis) | 0.012 | 24 (21) | No | Cured (8)a |
| 63/M [6] | Porcine Aortic | ceftriaxone and ciprofloxacin PO (combination therapy) | NS | 27 (27) | No | Cured (NS) |
| 66/F [7] | Native Aortic | ceftriaxone 2 g IV twice daily for 3weeks, then ciprofloxacin 400 mg IV twice daily (ceftriaxone allergy) | 0.5 | 6 (1) | Yes Post antibiotic treatment | Cured (8) |
| 66/F [8] | Tissue aortic valve | ceftriaxone 2 g IV twice daily, gentamicin 7 mg/kg/day, ciprofloxacin 400 mg IV twice daily (combination therapy) | NS | NS | Yes | Curedb (NS) |
| 75/M [9] | Porcine aortic valve/native mitral valve | penicillin, gentamicin, ciprofloxacin, imipenem-cilastatin (combination therapy) | NS | 20 days (20 days) | Yes | Died |
NS: Not stated IV: intravenous PO: oral.
Vegetation present at 8 months.
Post surgery experienced complete heart block and stroke.
Susceptibility testing for Cardiobacterium hominis is not readily available at most institutions. In our case the organism was sent to a reference laboratory and was found to be sensitive to all antimicrobials tested including ciprofloxacin with an MIC of ≤0.12 ug/mL. This is well below the Clinical and Laboratory Standards Institute (CLSI) breakpoint of ≤1 ug/mL [10]. It is also in the range of MIC values 0.012–0.5 ug/mL reported in the literature [[4], [5], [7]]. In the case report by Vogt et al., the authors performed a killing curve assay using the patient’s serum after receiving ciprofloxacin 200 mg combined with 5 × 105 cfu/mL of organisms. With ciprofloxacin peak and trough concentrations of 0.74 ug/mL and 0.14 ug/mL bacterial counts were undetectable within 2 and 4 h respectively [4].
Cardiobacterium hominis has a strong association with aortic valve infection and is known to produce large friable vegetations [1]. Surgical intervention is required in 30–50% of patients [[1], [11]]. Peripheral and central nervous system emboli are reported in 51 and 21% of cases respectively [11]. Our patient did not have any evidence of peripheral or central nervous system emboli. Acute coronary syndrome is a rare manifestation of endocarditis, but has been reported with other HACEK organisms, including two cases with Cardiobacterium hominis [[8], [12]]. In a case series of patients with endocarditis that presented with acute coronary syndrome, Courand et al. recommended consideration of septic coronary embolism in patients with acute coronary syndrome, elevation of inflammatory biomarkers, a normal coronary artery, and unusual regurgitant valvulopathy [12]. Interestingly in our case the patient presented with acute coronary syndrome that may have been related to septic emboli, although he had an extensive cardiac history.
HACEK endocarditis is associated with a 93% cure rate and 4% rate of hospital mortality [[1], [11]]. Our patient responded well to a 6 week course of ciprofloxacin therapy given first intravenously and then by mouth, in combination with surgical intervention. He also did not experience any adverse reactions that can be associated with long term fluoroquinolone therapy such as QTc prolongation, peripheral neuropathy, or tendon rupture [13].
Conclusion
Monotherapy with intravenous ciprofloxacin followed by oral step down therapy for 6 weeks combined with valve replacement was successful in the treatment of prosthetic aortic valve endocarditis with possible septic coronary emboli in a patient allergic to penicillins and cephalosporins.
Funding and conflict of interest
LA, CF & MH have nothing to disclose.
Contributor Information
Lisa M. Avery, Email: lisa.avery@sjhsyr.org.
Muhammad Hasan, Email: muhammad.hasan@sjhsyr.org.
References
- 1.Chambers S.T., Murdoch D., Morris A. HACEK infective endocarditis: characteristics and outcomes from a large, multi-national cohort. PLoS One. 2013;8:e63181. doi: 10.1371/journal.pone.0063181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baddour L.M., Wilson W.R., Bayer A.S., American Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young, Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Stroke Council Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 3.Gatselis N., Malli E., Papadamou G., Petinaki E., Dalekos G.N. Direct detection of Cardiobacterium hominis in serum from a patient with infective endocarditis by broad-range bacterial PCR. J Clin Microbiol. 2006;44:669–672. doi: 10.1128/JCM.44.2.669-672.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vogt K., Klefisch F., Hahn H., Schmutzler H. Antibacterial efficacy of ciprofloxacin in a case of endocarditis due to Cardiobacterium hominis. Zentralbl Bakteriol. 1994;281:80–84. doi: 10.1016/s0934-8840(11)80640-7. [DOI] [PubMed] [Google Scholar]
- 5.Braun D., Horovitz A., Bertea M., Jenni R., Günthard H.F. Aortic homograft endocarditis caused by Cardiobacterium hominis and complicated by agranulocytosis due to ceftriaxone. BMJ Case Rep. 2010;(November) doi: 10.1136/bcr.04.2010.2894. pii: bcr0420102894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnold D.M., Smaill F., Warkentin T.E., Christjanson L., Walker I. Cardiobacterium hominis endocarditis associated with very severe thrombocytopenia and platelet autoantibodies. Am J Hematol. 2004;76:373–377. doi: 10.1002/ajh.20127. [DOI] [PubMed] [Google Scholar]
- 7.Lu P.L., Hsueh P.R., Hung C.C., Teng L.J., Jang T.N., Luh K.T. Infective endocarditis complicated with progressive heart failure due to beta-lactamase-producing Cardiobacterium hominis. J Clin Microbiol. 2000;38:2015–2017. doi: 10.1128/jcm.38.5.2015-2017.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donovan J., Hatcher J., Riddell A., Tiberi S. Back pain, leg swelling and a cardiac arrest: an interesting case of endocarditis. BMJ Case Rep. 2014;(May) doi: 10.1136/bcr-2013-202215. pii: bcr2013202215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldberg M.H., Katz J. Infective endocarditis caused by fastidious oro-pharyngeal HACEK micro-organisms. J Oral Maxillofac Surg. 2006;64:969–971. doi: 10.1016/j.joms.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 10.Clinical and Laboratory Standards Institute (CLSI) Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria: Approved standard, CLSI document M45; 3rd Wayne, PACLSI; 2015. [Google Scholar]
- 11.Malani A.N., Aronoff D.M., Bradley S.F., Kauffman C.A. Cardiobacterium hominis endocarditis: two cases and a review of the literature. Eur J Clin Microbiol Infect Dis. 2006;25:587–595. doi: 10.1007/s10096-006-0189-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Courand P.Y., Mouly-Bertin C., Thomson V., Lantelme P. Acute coronary syndrome revealed Cardiobacterium hominis endocarditis. J Cardiovasc Med (Hagerstown) 2012;13:216–221. doi: 10.2459/JCM.0b013e32833daf81. [DOI] [PubMed] [Google Scholar]
- 13.Cipro ® [Package Insert] Bayer Healthcare Pharmaceuticals Inc. Whippany, NJ, 7/2016.