The NLRP3 inflammasome protects the host against microbial infections. In this study, Malireddi et al. demonstrate the critical role of TAK1 in restricting RIPK1 signaling to inhibit spontaneous NLRP3 inflammasome activation and cell death, which may be targeted for treatment of myeloid proliferation.
Abstract
The NOD-like receptor (NLR)–P3 inflammasome is a global sensor of infection and stress. Elevated NLRP3 activation levels are associated with human diseases, but the mechanisms controlling NLRP3 inflammasome activation are largely unknown. Here, we show that TGF-β activated kinase-1 (TAK1) is a central regulator of NLRP3 inflammasome activation and spontaneous cell death. Absence of TAK1 in macrophages induced spontaneous activation of the NLRP3 inflammasome without requiring toll-like receptor (TLR) priming and subsequent activating signals, suggesting a distinctive role for TAK1 in maintaining NLRP3 inflammasome homeostasis. Autocrine tumor necrosis factor (TNF) signaling in the absence of TAK1 induced spontaneous RIPK1-dependent NLRP3 inflammasome activation and cell death. We further showed that TAK1 suppressed homeostatic NF-κB and extracellular signal–related kinase (ERK) activation to limit spontaneous TNF production. Moreover, the spontaneous inflammation resulting from TAK1-deficient macrophages drives myeloid proliferation in mice, and was rescued by RIPK1 deficiency. Overall, these studies identify a critical role for TAK1 in maintaining NLRP3 inflammasome quiescence and preserving cellular homeostasis and survival.
Introduction
NOD-like receptor (NLR)–P3 inflammasome activation leads to the maturation of proinflammatory cytokines IL-1β and IL-18, and induction of pyroptotic cell death (Sharma and Kanneganti, 2016). Thus, NLRP3 is central in guarding the host against microbial infections, including bacterial, viral, fungal, and protozoan infections (Anand et al., 2011). Gain-of-function mutations in the NLRP3 gene are associated with inflammatory syndromes collectively known as cyropyrin-associated periodic syndromes (CAPS; http://fmf.igh.cnrs.fr/ISSAID/infevers/; Gurung and Kanneganti, 2016). Conventionally, activation of the NLRP3 inflammasome requires a priming signal and an activating signal. Previous studies demonstrated that the first priming signal—often provided by TLRs—serves to up-regulate NLRP3 and pro–IL-1β (Bauernfeind et al., 2009). Some of the proposed mechanisms for regulating NLRP3 inflammasome activation include potassium efflux, calcium mobilization, mitochondrial damage, and production of ROS (Sharma and Kanneganti, 2016). Molecularly, NEK7 (Schmid-Burgk et al., 2016), cardiolipin (Iyer et al., 2013), and caspase-8/FADD (Gurung et al., 2014) have been shown to directly regulate the NLRP3 inflammasome. Additional studies suggested that deubiquitination of NLRP3 by IRAK proteins is required to assemble the inflammasome complex after receiving the second activation signal (Juliana et al., 2012; Py et al., 2013). Herein, we sought to investigate the role of TAK1, a central signaling molecule, in regulating NLRP3 inflammasome activation and cell death.
Programmed cell death is central to homeostasis and orchestrates normal organismal growth and development. Failure to control cell death programs often results in devastating inflammatory pathologies and disease. TAK1 is a quintessential kinase that plays key roles in cellular homeostasis by positively regulating cell survival and proinflammatory signaling pathways (Yamaguchi et al., 1995; Wang et al., 2001; Ninomiya-Tsuji et al., 2003; Sato et al., 2005; Shim et al., 2005; Wan et al., 2006; Hayden and Ghosh, 2008; Zhang et al., 2017). Whereas inactivation of TAK1 induces apoptosis or necroptosis (Sanna et al., 2002; Mihaly et al., 2014; Guo et al., 2016), hyperactivation of TAK1 under conditions of its enforced expression or TAB2 deletion promotes necroptosis (Morioka et al., 2014). TAK1 is important for lysosomal rupture–induced inflammasome activation (Okada et al., 2014) and hypotonic stimulation (altering cellular volume–induced inflammasome activation; Compan et al., 2012). Currently, there is a tremendous interest in TAK1 inhibition as a therapeutic application for inflammatory disease management and cancer immunotherapy (Sakurai, 2012; Singh et al., 2012; Huang et al., 2015; Kilty and Jones, 2015; Guan et al., 2017). However, prolonged TAK1 inactivation also results in severe inflammation, bone disorders, and cancer development in mice and humans (Shim et al., 2005; Omori et al., 2006; Kajino-Sakamoto et al., 2008, 2010; Tang et al., 2008; Bettermann et al., 2010; Inokuchi et al., 2010; Lamothe et al., 2013; Le Goff et al., 2016; Wade et al., 2016). These findings are paradoxical because TAK1 is a well-accepted upstream kinase that drives inflammation through NF-κB and MAPK signaling cascades (Zhang et al., 2017). Furthermore, inactivation of NF-κB by deletion of IKKβ, NEMO/IKKγ, upstream TAK1-activating TAB proteins, or downstream antiapoptotic cIAP1/2 does not result in similar cell death phenotypes, and often requires priming to induce cell death in vitro (Shim et al., 2005; Vanlangenakker et al., 2011; Dondelinger et al., 2013; Mihaly et al., 2014). Moreover, repression of the deubiquitinase CYLD protects cells from RIPK1-mediated apoptosis in the absence of cIAP1/2 but not in TAK1-inactivated conditions (Dondelinger et al., 2013). Although TAK1 prosurvival function in different cell types is well established, there are conflicting studies regarding the mechanism and nature of cell death observed in TAK1 KO cells. In some studies, both RIPK1 and RIPK3 have been shown to promote necrotic and apoptotic cell death in TAK1-deficient cells (Vanlangenakker et al., 2011; Guo et al., 2016); however, other studies report that RIPK1, RIPK3 or both are dispensable for the cell death observed in TAK1 KO cells (Morioka et al., 2014; Dondelinger et al., 2015; Mihaly et al., 2017). Overall, the molecular mechanisms responsible for hyperactivation of the inflammatory immune response seen in conditions of TAK1 inactivation remain poorly understood. Herein, we sought to investigate the role of TAK1, a central signaling molecule, in regulating NLRP3 inflammasome activation and cell death.
Here, we show that TAK1 is a central regulator of NLRP3 inflammasome homeostasis. Absence of TAK1 in macrophages induced spontaneous activation of the NLRP3 inflammasome without requiring the priming and activating signals, suggesting a distinctive role for TAK1 in maintaining NLRP3 inflammasome homeostasis. Autocrine TNF signaling in the absence of TAK1 induced spontaneous RIPK1-dependent activation of the NLRP3 inflammasome and cell death. Our data further suggested that TAK1 suppresses homeostatic NF-κB and ERK activation to limit spontaneous TNF production. Moreover, the spontaneous inflammation resulting from TAK1-deficient macrophages drove myeloid proliferation in mice, which was rescued by RIPK1 deficiency. Overall, these studies identify a critical paradigm for the maintenance of inflammasome quiescence to preserve myeloid cell homeostasis.
Results and discussion
TAK1 deficiency in myeloid cells results in spontaneous inflammasome activation and secretion of IL-1β and IL-18
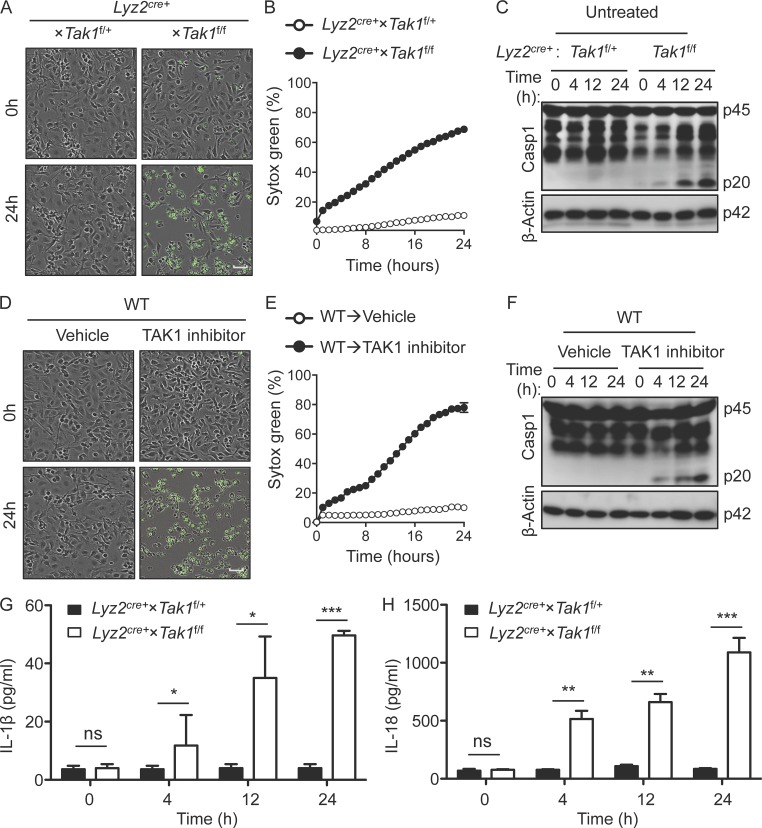
TAK1 deficiency is embryonically lethal in mice (Sato et al., 2005; Shim et al., 2005); thus, to study the function of TAK1, we generated mice lacking TAK1 specifically in the myeloid compartment (Lyz2cre+ × Tak1f/f mice). We observed that TAK1-deficient bone marrow–derived macrophages (BMDMs) underwent spontaneous cell death (Fig. 1, A and B). This was expected, given the important role of TAK1 in the survival of different cell lineages including T cells, B cells, osteoclasts, and hematopoietic stem cells (Sato et al., 2005). Herein, we observed that TAK1-deficient macrophages also induced spontaneous caspase-1 activation in the absence of both priming and activating signals (Fig. 1 C). A two-hit (priming and activation) model is well established and accepted for optimal activation of the inflammasomes (Bauernfeind et al., 2009). However, in certain conditions where the inflammasome sensors have gain-of-function mutations (as observed with NLRP3 [CAPS; Hoffman et al., 2001a,b], NLRC4 [MAS, macrophage activation syndrome; Canna et al., 2014], and Pyrin [FMF, familial Mediterranean fever; French FMF Consortium, 1997; The International FMF Consortium, 1997]), only a priming or an activating signal is sufficient to assemble and activate the inflammasome. Given our data that caspase-1 activation in the TAK1-deficient BMDMs did not require any external stimuli (both priming and activation signals were not required), this demonstrates a previously unknown central regulatory role for TAK1 in maintaining inflammasome quiescence. In agreement with our observations in TAK1-deficient BMDMs, chemical inhibition of TAK1 kinase activity (5Z-7-oxozeaenol, herein referred to as TAK1 inhibitor or TAK1i) in WT macrophages also induced spontaneous cell death and subsequent caspase-1 activation (Fig. 1, D–F). One of the hallmarks of caspase-1 activation is the production of processed cytokines IL-1β and IL-18 (Gurung et al., 2015). Consistently, mature IL-1β and IL-18 were detected in the supernatants from cultured TAK1-deficient macrophages in a steady-state condition (Fig. 1, G and H). In addition, mRNA levels of pro–IL-1β were also up-regulated at steady-state in TAK1-deficient but not WT macrophages (Fig. S2 H), whereas mRNA levels of pro–IL-18, which is constitutively expressed in macrophages, were similarly expressed in both WT and TAK1-deficient macrophages (Fig. S2 I). These data suggested that TAK1 is a central homeostatic regulator of inflammasome activation in macrophages. More importantly, given that TAK1 deficiency promoted spontaneous IL-1β release, which requires a priming signal, our data suggested that TAK1 restricts spontaneous inflammatory signaling to promote cellular quiescence and homeostasis.
Figure 1.
TAK1 deficiency in myeloid cells results in spontaneous inflammasome activation and proinflammatory cytokine production. (A–C) Cell death by Incucyte image analysis, (bar, 40 µm; A), time course quantification of dead cells (B), and immunoblot analysis of pro–caspase-1 (p45) and the active caspase-1 subunit p20 (p20; C) in unstimulated WT control (Lyz2cre+ × Tak1f/+) or TAK1-deficient BMDMs (Lyz2cre+ × Tak1f/f) assessed in culture at the indicated times after differentiation. (D–F) Cell death by Incucyte image analysis, (bar, 40 µm; D), time course quantification of dead cells (E), and caspase-1 activation (F) measured in BMDMs left unstimulated or treated with TAK1i for the indicated times in culture after differentiation. (G and H) Secretion of IL-1β (G) and secretion of IL-18 (H) in unstimulated Lyz2cre+ × Tak1f/f (TAK1 KO) or WT BMDMs left untreated for the indicated times in culture. All data are presented as mean ± SEM (G and H). “p” in Western blots denotes protein molecular weight. P < 0.05 is considered statistically significant. *, P < 0.05; **, P < 0.01; ***, P < 0.001 (two-tailed t test [G and H]). Data are representative of three independent experiments with n = 2 (A–F) and n = 3 in each repeat (G and H).
NLRP3 promotes spontaneous inflammasome activation observed in TAK1-deficient macrophages
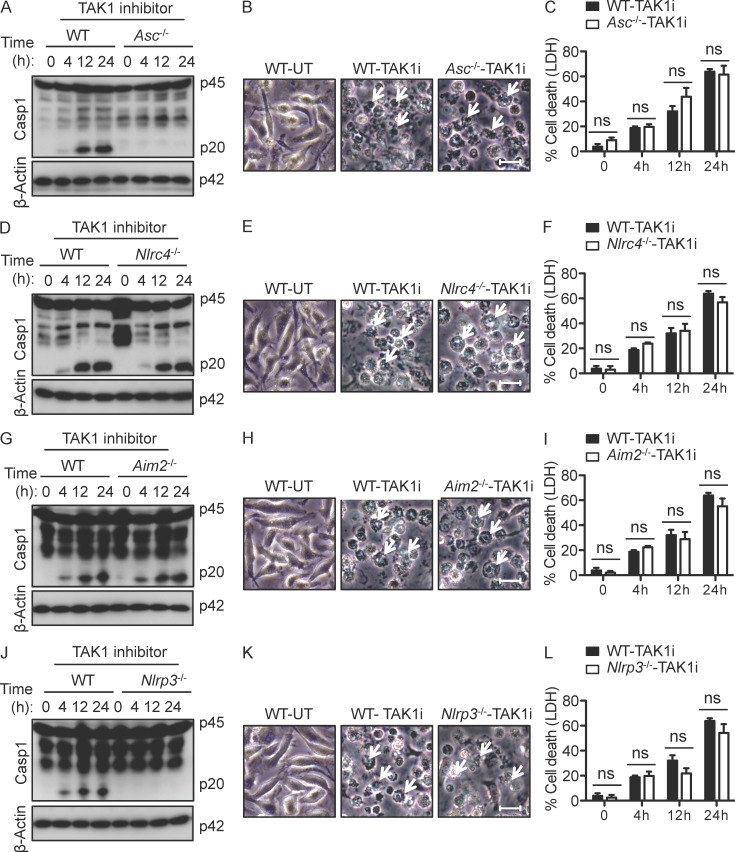
We next asked if this spontaneous caspase-1 activation was dependent on ASC, a central adaptor molecule for inflammasome. We found that TAK1i-induced caspase-1 activation was dependent on ASC (Fig. 2 A). To identify the upstream inflammasome sensor, NLRC4-, AIM2-, and NLRP3-deficient cells were assessed for TAK1i-induced caspase-1 activation. Contrary to NLRC4 and AIM2, NLRP3 proved essential for TAK1i-induced inflammasome activation (Fig. 2, D, G, and J). Given the spontaneous activation of caspase-1 in TAK1-deficient macrophages (Fig. 1), we posited that the cells undergoing pyroptotic cell death could be rescued by the deficiency of NLRP3 inflammasome components. However, TAK1i-treatment induced robust cell death in ASC-deficient BMDMs similar to that observed in WT BMDMs (Fig. 2, B and C). To determine if the inflammasome sensors were involved in the induction of cell death, we treated NLRC4-, AIM2-, and NLRP3-deficient BMDMs with TAK1i. TAK1i-treatment induced similar cell death in both WT and the inflammasome sensor–deficient BMDMs (Fig. 2, E, F, H, I, K, and L).
Figure 2.
NLRP3 promotes spontaneous inflammasome activation observed in TAK1-deficient BMDMs. (A–L) WT or the indicated KO BMDMs were treated with TAK1i for the indicated times. Immunoblot analysis of pro–caspase-1 (p45) and the active caspase-1 subunit p20 (p20; A, D, G, and J), analysis of cell death by microscopy (bars, 20 µm; B, E, H, and K), or LDH secretion (C, F, I, and L) in TAK1i-treated BMDMs assessed at the indicated times after treatment in Asc−⁄− (A–C), Nlrc4−⁄− (D–F), Aim2−⁄− (G–I), and Nlrp3−⁄− (J–L). Arrows indicate dead cells (B, E, H, and K). Data are representative of three independent experiments with n = 3 (A–L). Error bars indicate SEM (C, F, I, and L). “p” in Western blots denotes protein molecular weight. P < 0.05 is considered statistically significant (two-tailed t test [C, F, I, and L]).
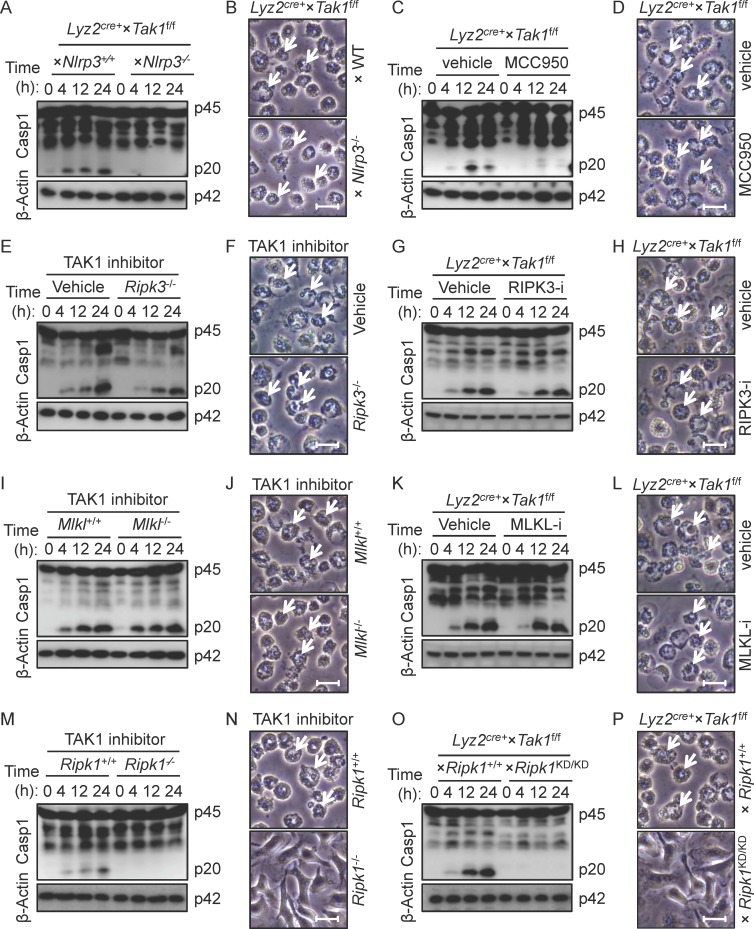
To further establish the role of NLRP3 in TAK1-regulated spontaneous inflammasome activation, we generated BMDMs from mice that lacked both TAK1 and NLRP3 (Lyz2cre+ × Tak1f/f × Nlrp3−⁄− mice). Similar to the results obtained with TAK1i treatment, NLRP3 deficiency prevented spontaneous caspase-1 activation in TAK1-deficient BMDMs (Fig. 3 A). Consistently, treatment of TAK1-deficient BMDMs with MCC950 (a specific inhibitor of the NLRP3 inflammasome) prevented spontaneous caspase-1 activation (Fig. 3 C). Similar to the observation in TAK1i-treated WT and NLRP3-deficient cells (Fig. 2, K and L), genetic deficiency or pharmacological inhibition of NLRP3 did not rescue cell death observed in TAK1-deficient BMDMs (Fig. 3, B and D).
Figure 3.
RIPK1 promotes spontaneous NLRP3 inflammasome activation and cell death in TAK1-deficient BMDMs. (A and B) Analysis of caspase-1 activation (A) and cell death by microscopy (B) in untreated Lyz2cre+ × Tak1f/f (TAK1 KO) compared with Lyz2cre+ × Tak1f/f × Nlrp3−⁄− (TAK1/NLRP3 DKO) assessed at the indicated times after differentiation of BMDMs in culture. (C and D) Lyz2cre+ × Tak1f/f BMDMs were treated with vehicle or MCC950 (specific inhibitor of NLRP3) and probed for caspase-1 activation (C) and cell death (D). (E and F) Caspase-1 immunoblot (E) and cell death analysis (F) in TAK1i-treated WT and Ripk3−⁄− BMDMs at various time points indicated. (G and H) Lyz2cre+ × Tak1f/f BMDMs were treated with vehicle or GSK’872 (RIPK3 inhibitor) and probed for caspase-1 activation (G) and cell death (H). (I and J) Caspase-1 immunoblot (I) and cell death analysis (J) in TAK1i-treated WT and Mlkl−⁄− BMDMs and assessed at the times indicated. (K and L) Lyz2cre+ × Tak1f/f BMDMs were treated with vehicle or GW806742X (MLKL inhibitor) and probed for caspase-1 activation (K) and cell death (L). (M and N) Caspase-1 immunoblot (M) and cell death analysis (N) in WT and Ripk1−⁄− (generated from fetal liver cells) BMDMs treated with TAK1i and assessed at the indicated times. (O and P) Caspase-1 immunoblot (O) and cell death analysis (P) in Lyz2cre+ × Tak1f/f and Lyz2cre+ × Tak1f/f × Ripk1KD/KD BMDMs and assessed at the indicated times. Arrows indicate dead cells. Bars, 20 µm. “p” in Western blots denotes protein molecular weight. Data are representative of three independent experiments with n = 3 in each repeat (A–P).
These results showed that although NLRP3 and ASC deficiency reversed TAK1i-induced spontaneous caspase-1 activation, TAK1i-induced cell death could not be rescued. We have recently shown that IAV-induced cell death consists of all three forms of cell death that include apoptosis, pyroptosis, and necroptosis (Kuriakose et al., 2016). Given that the cells lacking NLRP3 and ASC (and thus pyroptosis) still underwent cell death, we hypothesized that TAK1 deficiency in BMDMs may induce all major forms of cell death that include apoptosis, pyroptosis, and necroptosis. Western blot data for caspase-3, caspase-7, and phospho-MLKL demonstrated that TAK1-deficient macrophages also exhibited the features of apoptotic and necroptotic cell death (Fig. S2, A–C). To this end, we used a combination of inhibitors that specifically block apoptosis, pyroptosis, and necroptosis to rescue spontaneous cell death observed in TAK1-deficient BMDMs. In accordance, we showed that inhibition of apoptosis, pyroptosis, or necroptosis individually was not sufficient to prevent cell death of TAK1-deficient BMDMs (Fig. S1, A–C). Also, the combined inhibition of apoptosis/pyroptosis, pyroptosis/necroptosis, and apoptosis/necroptosis did not completely rescue cell death in TAK1-deficient BMDMs (Fig. S1 D). However, when all cell death pathways were inhibited, TAK1-deficient cells were protected from cell death (Fig. S1 E), suggesting a redundant role for apoptosis, pyroptosis, and necroptosis in inducing cell death in TAK1-deficient BMDMs. Conversely, these data demonstrate that TAK1 plays an essential regulatory role in inhibiting cell death pathways and maintaining cellular homeostasis.
RIPK1 is upstream of spontaneous NLRP3 inflammasome activation and cell death in TAK1-deficient macrophages
Receptor interacting protein kinase (RIPK) 3 has been shown to be involved in regulating NLRP3 inflammasome activation under specific circumstances (Kang et al., 2013; Wang et al., 2014; Lawlor et al., 2015). Our results showed that TAK1i treatment of Ripk3−⁄− BMDMs results in normal NLRP3 inflammasome activation and cell death, similar to WT cells (Fig. 3, E and F). MLKL is a pseudokinase that upon activation intercalates in the plasma membrane to promote necroptosis (Wang et al., 2014). To test the role for MLKL, we treated WT or Mlkl−⁄− BMDMs with TAK1i. MLKL deficiency did not rescue TAK1i-induced caspase-1 activation or cell death (Fig. 3, I and J). To complement these studies, we treated TAK1-deficient BMDMs with RIPK3 or MLKL inhibitor (Fig. 3, G, H, K, and L), and our results showed that RIPK3 and MLKL are dispensable for spontaneous NLRP3 inflammasome activation. Concurrently, the cell death was also not rescued by RIPK3 or MLKL deficiency in TAK1-deficient BMDMs (Fig. 3, F, H, J, and L).
Next, we investigated whether RIPK1, an upstream kinase, was involved in spontaneous NLRP3 inflammasome activation and cell death induction. TAK1 inhibition of WT, but not Ripk1−⁄− macrophages (derived from fetal liver cells because the RIPK1 deficiency in mice causes day 1 postnatal lethality; Kelliher et al., 1998) induced spontaneous NLRP3 inflammasome activation and cell death (Fig. 3, M and N). Furthermore, TAK1-deficient BMDMs lacking RIPK1 kinase activity (Lyz2cre+ × Tak1f/f × Ripk1K45A) did not exhibit spontaneous caspase-1 cleavage or cell death (Fig. 3, O and P). Consistently, the levels of spontaneous IL-1β and IL-18 cytokines observed in Lyz2cre+ × Tak1f/f macrophages were rescued in Lyz2cre+ × Tak1f/f × Ripk1K45A macrophages (Fig. S2, F and G). These results altogether suggest that TAK1 negatively regulates RIPK1 kinase activity independently of RIPK3 and MLKL to control spontaneous NLRP3 inflammasome activation and cell death.
RIPK1 is a well-established regulator of TNF signaling. Thus, we hypothesized that TAK1 deficiency or inhibition may trigger spontaneous activation of the TNF signaling pathway. Indeed, we observed a significant amount of spontaneous TNF secretion in the culture by TAK1-deficient BMDMs (Fig. S2 D) and in the serum of Lyz2cre+ × Tak1f/f mice (Fig. S2 E). To evaluate whether autocrine TNF was the upstream event that induced NLRP3 inflammasome activation and cell death in TAK1-deficient BMDMs, anti-TNF neutralizing antibody was used to block TNF signaling (Fig. S3, A–F). TNF neutralization rescued aberrant caspase-1 activation and cell death in both TAK1-deficient BMDMs and TAK1i-treated WT cells (Fig. S3, A–F). In addition, TNF neutralization also rescued the spontaneous production of IL-1β and IL-18 from TAK1-deficient macrophages (Fig. S2 G). To further examine the role of TNF signaling, we used TNF-deficient and TNFR-deficient BMDMs that were treated with TAK1i. Genetic deficiency of either TNF or TNFR rescued spontaneous caspase-1 activation and cell death responses in TAK1i-treated BMDMs (Fig. S3, G–L). However, TAK1 inhibition–induced caspase-1 activation from Trif−/− and Ifnar1−/− BMDMs was comparable to that observed in the WT BMDMs (Fig. S1 F). Altogether, these data demonstrated that the TNF signaling axes promote NLRP3 inflammasome activation and cell death in TAK1-deficient BMDMs.
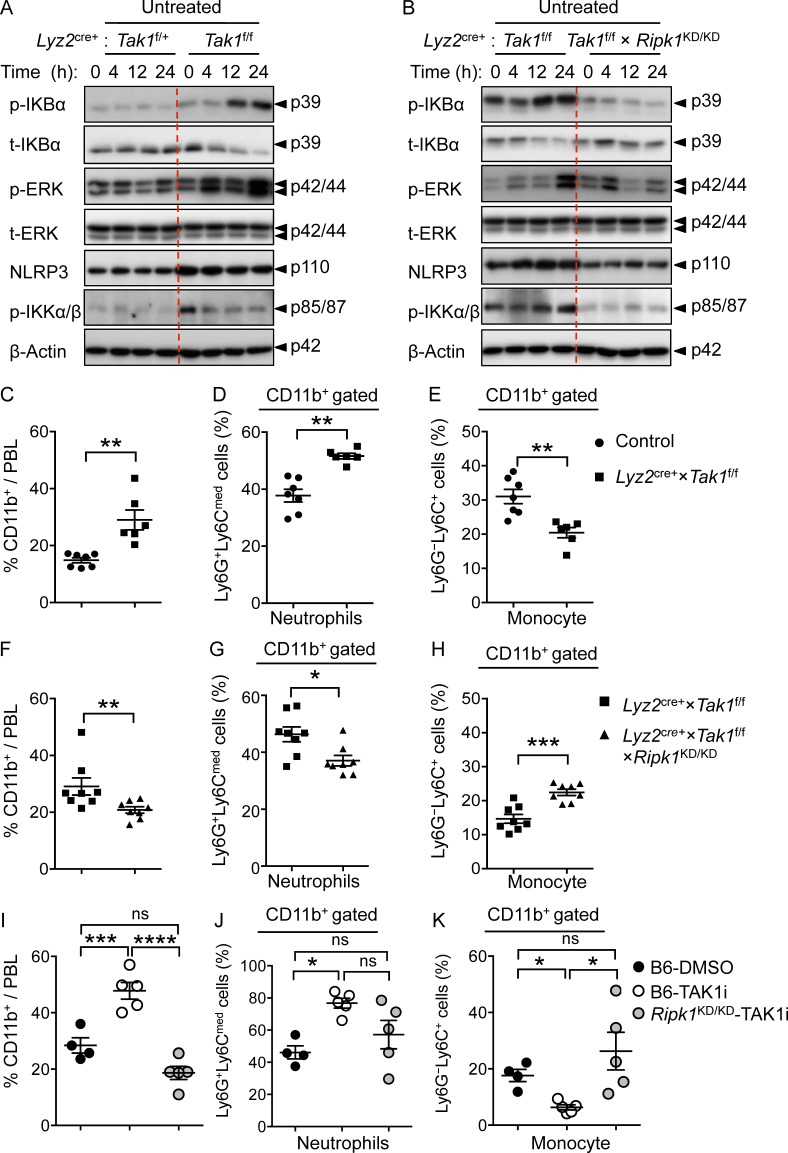
TAK1 restricts RIPK1 kinase–dependent spontaneous NF-κB and ERK activation in macrophages and myeloid proliferation in mice
In addressing the mechanisms by which TAK1 promotes cellular quiescence, we posited that TAK1 deficiency activates inflammatory signaling pathways in the absence of exogenous stimuli, concurrent with our detection of spontaneous NLRP3 inflammasome activation and TNF production by TAK1-deficient BMDMs. In agreement with our hypothesis, we observed increased activation of ERK and NF-κB in TAK1-deficient BMDMs under homeostatic conditions (Fig. 4 A). Similarly, phospho-IKKα/β, upstream regulators of ERK and NF-κB, were also increased basally in TAK1-deficient BMDMs (Fig. 4 A). In concurrence with increased activation, basal protein expression of NLRP3 was also slightly increased in TAK1-deficient BMDMs (Fig. 4 A). These results were unexpected given the established role of TAK1 in promoting ERK and NF-κB activation. More importantly, this aberrant signaling in TAK1-deficient BMDMs was rescued when RIPK1 kinase activity was absent (Fig. 4 B). These data demonstrate that under homeostatic conditions, TAK1 restricts RIPK1-dependent spontaneous NF-κB and ERK activation.
Figure 4.
RIPK1 kinase-dead mouse partially rescues the myeloid phenotype observed in TAK1-deficient mice in vivo. (A) Immunoblot analysis of phospho-IκBα, phospho-ERK, NLRP3, phospho-IKKα/β, and β-actin (loading control) in untreated Tak1f/+ × Lyz2cre+ (HT ctrl) and Tak1f/f × Lyz2cre+ (TAK1 KO) BMDMs assessed at the indicated times after differentiation in culture. (B) Immunoblot analysis as in A in untreated BMDMs from Lyz2cre+ × Tak1f/f (TAK1 KO) and Lyz2cre+ ×Tak1f/f x Ripk1KD/KD (TAK1 KO with kinase-dead RIPK1) mutant mice. (C–H) Flow cytometry analysis of peripheral blood from control (n = 7), Tak1f/f × Lyz2cre+ (n = 6, C–E; n = 8, F–H) and Tak1f/f × Lyz2cre+ × Ripk1KD/KD (n = 8) mice. Littermate controls were used for the experiments, which included Tak1f/f and Tak1f/+ × Lyz2cre+ mice. (C and F) Cumulative dot plots of representing frequencies of CD11b+ cells analyzed by flow cytometry from blood. (D and G) Cumulative dot plots representing frequency of neutrophil population in the CD11b+-gated cells. (E and H) Cumulative dot plots representing frequency of monocyte population in the CD11b+-gated cells. (I–K) Flow cytometry analysis of peripheral blood from control (n = 4) and TAK1i-treated WT (n = 5) and Ripk1KD/KD (n = 5) mice. Cumulative dot plots representing the frequencies of total CD11b+ cells analyzed by flow cytometry from blood (I), and frequency of neutrophil (J) and monocyte (K) populations in the CD11b+-gated cells. All data are presented as mean ± SEM (C–K), and each dot represents a single mouse. “p” in Western blots denotes protein molecular weight. Statistical significance between groups was determined by Mann-Whitney test, and P values less than 0.05 are considered statistically significant. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001. Data are representative of five (A and B) or two (C–H) independent experiments.
Mice with myeloid specific deficiency of TAK1 develop progressive accumulation of neutrophils ultimately displaying signs of myeloid proliferation and death. Consistently, we also observed increased CD11b+ populations (myeloid cells) in the peripheral blood (PBL) of Lyz2cre+ × Tak1f/f mice (Fig. 4 C). A closer examination of CD11b+ cells revealed that whereas neutrophil frequency was increased, monocyte frequency was decreased in Lyz2cre+ × Tak1f/f mice when compared with littermate WT controls (Fig. 4, D and E). Importantly, the increased neutrophil and reduced monocyte populations in the PBL from Lyz2cre+ × Tak1f/f mice were rescued in Lyz2cre+ × Tak1f/f × Ripk1KD/KD mice (Fig. 4, F–H). To further corroborate these findings, we studied the TAK1i-induced acute neutrophilia and monocytopenia in mice (Fig. 4). TAK1i-treatment of WT mice significantly increased the frequency of CD11b+ cells and neutrophils, whereas the frequency of the monocyte population was significantly reduced (Fig. 4, I–K), similar to the mice genetically lacking TAK1 in myeloid compartment (Fig. 4, C–H). Importantly, TAK1i-induced differences in neutrophil and monocyte populations were also dependent on RIPK1 kinase activity (Fig. 4, I–K). Collectively, these data demonstrate a critical role for RIPK1 kinase activity in regulating NLRP3 inflammasome activation and cell death to promote myeloid proliferation in the absence of TAK1 signaling.
The conventional role of TAK1 in propagating NF-κB and MAPK signaling events downstream of several PRR, growth, and cytokine receptors is well established (Ajibade et al., 2013; Zhang et al., 2017). Herein, we describe a previously uncharacterized, paradoxical role for TAK1 in regulating cellular quiescence and homeostasis by inhibiting spontaneous activation of IKKα/β. Early studies demonstrated that inhibition or deletion of IKKα/β activates NLRP3 inflammasome in the presence of priming signal alone (Greten et al., 2007; Zhong et al., 2016). Given these studies that show IKKβ deficiency or inhibition activated the NLRP3 inflammasome, which requires LPS priming, our study is fundamentally different because we demonstrate that TAK1 deficiency leads to enhanced basal activation of IKKα/β to promote TNF release and spontaneous inflammasome activation. This result is completely unexpected given the established role of TAK1 in promoting receptor-induced signaling events (Ajibade et al., 2013; Zhang et al., 2017). The absence of TAK1 in macrophages also induced spontaneous activation of the NLRP3 inflammasome without the requirement for exogenous priming and activation signals, which has not been reported before. Mechanistically, we have clearly demonstrated the role for TNF, TNFR, and RIPK1 in regulating spontaneous NLRP3 inflammasome activation and cell death. Physiologically, enhanced cell death and inflammation resulting from loss-of-function mutations of TAK1 drives myeloid proliferation in mice and humans (Ajibade et al., 2012; Lamothe et al., 2012). TAK1 loss-of-function mutations also cause death of a range of immune and nonimmune cells and disrupt tissue and bone homeostasis (Mihaly et al., 2014; Swarnkar et al., 2015; Le Goff et al., 2016; Wade et al., 2016). Our study identified several important effector molecules driving this cell death and inflammation downstream of TAK1-inactivation and hence potential therapeutic targets. Increased cell death of TAK1-deficeint resident macrophages has also been observed in in vivo mouse models with hematopoietic specific deletion of TAK1 (Sakamachi et al., 2017). Future studies will test whether similar pathways of cell death and inflammasome activation, as established in our study, are at work in these resident macrophages. These findings corroborate and provide a mechanistic explanation for the severe spontaneous inflammatory pathologies in TAK1 KO compared with the mice deficient for other NF-κB family members (Shim et al., 2005; Mihaly et al., 2014). More importantly, we have provided in vivo data targeting RIPK1 kinase activity to rescue the myeloid proliferation phenotype associated with TAK1 deficiency in mice. Our study uncovered previously unidentified functions of TAK1 with potential applications for therapeutically activating the innate immune system and managing myeloid proliferation in specific situations in which TAK1 functions are impaired.
Materials and methods
Mice
Ripk1K45A (Ripk1KD/KD; Berger et al., 2014), Ripk3−⁄− (Newton et al., 2004), Nlrp3−⁄− (Kanneganti et al., 2006), Asc−⁄− (Mariathasan et al., 2004), Casp1−⁄− × Casp11−⁄− (Kayagaki et al., 2011), Tnf−⁄− (Pasparakis et al., 1996), Tnfr−⁄− (Pfeffer et al., 1993), and Mlkl−⁄− (Murphy et al., 2013) were all described previously. Tak1f/f mice were bred with Lyz2cre+ (B6.129P2-Lyz2tm1(cre)Ifo/J; Jackson) mice to generate conditional Tak1 KO mice. C57BL/6 WT (Jackson) and littermate controls were bred at St. Jude Children’s Research Hospital. Animal studies were conducted under protocols approved by St. Jude Children’s Research Hospital on the Use and Care of Animals.
Macrophage differentiation and stimulation
BMDMs were prepared as described previously (Gurung et al., 2012). In brief, bone marrow cells were grown in L cell–conditioned IMDM medium supplemented with 10% FBS, 1% nonessential amino acid, and 1% penicillin-streptomycin for 5 d to differentiate into macrophages. On day 5, BMDMs were counted, and 106 cells were seeded in 12-well cell culture plates in IMDM media containing 10% FBS, 1% nonessential amino acids, and 1% penicillin-streptomycin. For BMDMs generated from Lyz2cre+ × Tak1f/f mice, as the precursor cells differentiate into macrophages, they will express Cre recombinase (under the control of myeloid-specific Lyz2 gene) and delete the floxed Tak1 gene, resulting in TAK1-deficient macrophages.
Where indicated, for pharmacological inhibition, BMDMs were pretreated with chemical inhibitors of apoptosis, pyroptosis, and necroptosis. In other experiments, BMDMs were treated with TAK1i 5Z-7-Oxozeaenol at 0.1 µM to study inflammasome activation and cell death.
Analysis of myeloid proliferation and TAK1i-induced PBL changes in vivo
All flow-cytometric analysis of in vivo myeloid phenotypes was conducted from Lyz2cre+ × Tak1f/f (TAK1 KO) and Lyz2cre+ ×Tak1f/f × Ripk1KD/KD (TAK1 KO with kinase-dead RIPK1) mutant mice. For all in vivo TAK1i treatments, WT or genetically manipulated RIPK1 kinase–dead mice were i.p. injected with DMSO control or TAK1i at 50 mg/kg body weight. Blood samples were collected at 6 h after TAK1i treatment from mouse orbital sinus. PBLs were isolated using standard ACK RBC lysis protocol and stained for flow-cytometric analysis with the indicated antibodies.
Western blotting
Samples for immunoblotting were prepared by combining cell lysates with culture supernatants. Samples were denatured in loading buffer containing SDS and 100 mM DTT and boiled for 5 min. SDS-PAGE–separated proteins were transferred to PVDF membranes and immunoblotted with primary antibodies against caspase-1 (AG-20B-0042; Adipogen), Nlrp3 (AG-20B-0014; Adipogen), GAPDH (D16H11), and β-Actin (13E5; Cell Signaling Technology) followed by secondary anti–rabbit or anti–mouse HRP antibodies (Jackson ImmunoResearch Laboratories), as previously described (Kanneganti et al., 2006).
Lactate dehydrogenase assay
Secreted levels of lactate dehydrogenase from cell supernatants were determined using the CytoTox 96 Non-Radioactive Cytotoxicity Assay according to the manufacturer’s instructions (G1780; Promega).
Flow cytometry
CD11b (M1/70), and Gr-1 (RB6-8C5) antibodies were purchased from eBioscience. LY6C (HK1.4), CD45.2 (104), and LY6G (1A8) were from BioLegend. Flow cytometry data were acquired on an upgraded eight-color FACScan and analyzed using FlowJo software (Tree Star).
Cytokine analysis
Concentrations of cytokines and chemokines were determined by multiplex ELISA (Millipore), or classical ELISA for IL-1β (eBioscience) or IL-18 (MBL International).
Microscope image acquisition
Light microscopy
Differentiated WT and mutant macrophages seeded in 12-well cell culture plates were either left untreated (control) or treated with TAK1i or different cell death inhibitors for the indicated times. Light microscopic images were obtained using an Olympus CKX41 microscope with a 40× objective lens. Digital image recording and image analysis were performed with the INFINITY ANALYZE Software (Lumenera Corp.). The images were processed and analyzed with ImageJ software.
Real-time cell death analysis
Real-time cell death assays were performed using a two-color IncuCyte Zoom in-incubator imaging system (Essen Biosciences). In brief, BMDMs were seeded in 24-well tissue culture vessels (250,000 cells/well) in the presence of 100 nM of the cell-impermeable DNA-binding fluorescent dye Sytox Green (S7020; Life Technologies), which rapidly enter dying cells on membrane permeabilization. Resulting images were analyzed using the software package supplied with the IncuCyte imager, which allows precise analysis of the number of Sytox Green–positive cells present in each image. Experiments were conducted using a minimum of three separate wells for each experimental condition and a minimum of four image fields per well. Dead cell events for each line of BMDMs were acquired via Sytox Green and plotted using GraphPad Prism software.
Statistical analysis
GraphPad Prism 5.0 software was used for data analysis. Data are shown as mean ± SEM. Statistical significance was determined by t tests (two-tailed) for two groups or one-way ANOVA (with Dunnett’s or Tukey’s multiple comparisons tests) for three or more groups.
Online supplemental material
Fig. S1 shows a combination of inhibitors that specifically block apoptosis, necroptosis, and pyroptosis rescue TAK1-deficient BMDMs from cell death. Fig. S2 shows TAK1 deficiency resulting in spontaneous TNF secretion in BMDMs. Fig. S3 shows the critical role of TNF signaling in spontaneous NLRP3 inflammasome activation in TAK1-deficient BMDMs.
Supplementary Material
Acknowledgments
We thank Drs. Peter Gough and John Bertin (both at GlaxoSmithKline) for generously providing Ripk1K45A mice.
This work was supported by National Institutes of Health grants CA163507, AR056296, AI124346, and AI101935 and the American Lebanese Syrian Associated Charities (ALSAC) to T.-D. Kanneganti.
The authors declare no competing financial interests.
Author contributions: R.K.S. Malireddi, P. Gurung, and T.-D. Kanneganti designed the study. H. Chi and J.M. Klco provided necessary reagents and insight for the manuscript. R.K.S. Malireddi, P. Gurung, J. Mavuluri, and T.K. Dasari performed experiments. R.K.S. Malireddi, P. Gurung, and T.-D. Kanneganti analyzed the data. R.K.S. Malireddi, P. Gurung, and T.-D. Kanneganti wrote the manuscript with input from the other authors. T.-D. Kanneganti oversaw the project.
References
- Ajibade A.A., Wang Q., Cui J., Zou J., Xia X., Wang M., Tong Y., Hui W., Liu D., Su B., et al. 2012. TAK1 negatively regulates NF-kappaB and p38 MAP kinase activation in Gr-1+CD11b+ neutrophils. Immunity. 36:43–54. 10.1016/j.immuni.2011.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajibade A.A., Wang H.Y., and Wang R.F.. 2013. Cell type-specific function of TAK1 in innate immune signaling. Trends Immunol. 34:307–316. 10.1016/j.it.2013.03.007 [DOI] [PubMed] [Google Scholar]
- Anand P.K., Malireddi R.K., and Kanneganti T.D.. 2011. Role of the nlrp3 inflammasome in microbial infection. Front. Microbiol. 2:12 10.3389/fmicb.2011.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauernfeind F.G., Horvath G., Stutz A., Alnemri E.S., MacDonald K., Speert D., Fernandes-Alnemri T., Wu J., Monks B.G., Fitzgerald K.A., et al. 2009. Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J. Immunol. 183:787–791. 10.4049/jimmunol.0901363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger S.B., Kasparcova V., Hoffman S., Swift B., Dare L., Schaeffer M., Capriotti C., Cook M., Finger J., Hughes-Earle A., et al. 2014. Cutting Edge: RIP1 kinase activity is dispensable for normal development but is a key regulator of inflammation in SHARPIN-deficient mice. J. Immunol. 192:5476–5480. 10.4049/jimmunol.1400499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettermann K., Vucur M., Haybaeck J., Koppe C., Janssen J., Heymann F., Weber A., Weiskirchen R., Liedtke C., Gassler N., et al. 2010. TAK1 suppresses a NEMO-dependent but NF-kappaB-independent pathway to liver cancer. Cancer Cell. 17:481–496. 10.1016/j.ccr.2010.03.021 [DOI] [PubMed] [Google Scholar]
- Canna S.W., de Jesus A.A., Gouni S., Brooks S.R., Marrero B., Liu Y., DiMattia M.A., Zaal K.J., Sanchez G.A., Kim H., et al. 2014. An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat. Genet. 46:1140–1146. 10.1038/ng.3089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compan V., Baroja-Mazo A., Lopez-Castejon G., Gomez A.I., Martinez C.M., Angosto D., Montero M.T., Herranz A.S., Bazan E., Reimers D., et al. 2012. Cell volume regulation modulates NLRP3 inflammasome activation. Immunity. 37:487–500. 10.1016/j.immuni.2012.06.013 [DOI] [PubMed] [Google Scholar]
- Dondelinger Y., Aguileta M.A., Goossens V., Dubuisson C., Grootjans S., Dejardin E., Vandenabeele P., and Bertrand M.J.. 2013. RIPK3 contributes to TNFR1-mediated RIPK1 kinase-dependent apoptosis in conditions of cIAP1/2 depletion or TAK1 kinase inhibition. Cell Death Differ. 20:1381–1392. 10.1038/cdd.2013.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dondelinger Y., Jouan-Lanhouet S., Divert T., Theatre E., Bertin J., Gough P.J., Giansanti P., Heck A.J., Dejardin E., Vandenabeele P., and Bertrand M.J.. 2015. NF-kappaB-Independent Role of IKKalpha/IKKbeta in Preventing RIPK1 Kinase-Dependent Apoptotic and Necroptotic Cell Death during TNF Signaling. Mol. Cell. 60:63–76. 10.1016/j.molcel.2015.07.032 [DOI] [PubMed] [Google Scholar]
- French FMF Consortium 1997. A candidate gene for familial Mediterranean fever. Nat. Genet. 17:25–31. 10.1038/ng0997-25 [DOI] [PubMed] [Google Scholar]
- Greten F.R., Arkan M.C., Bollrath J., Hsu L.C., Goode J., Miething C., Goktuna S.I., Neuenhahn M., Fierer J., Paxian S., et al. 2007. NF-kappaB is a negative regulator of IL-1beta secretion as revealed by genetic and pharmacological inhibition of IKKbeta. Cell. 130:918–931. 10.1016/j.cell.2007.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan S., Lu J., Zhao Y., Woodfield S.E., Zhang H., Xu X., Yu Y., Zhao J., Bieerkehazhi S., Liang H., et al. 2017. TAK1 inhibitor 5Z-7-oxozeaenol sensitizes cervical cancer to doxorubicin-induced apoptosis. Oncotarget. 8:33666–33675. 10.18632/oncotarget.16895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X., Yin H., Chen Y., Li L., Li J., and Liu Q.. 2016. TAK1 regulates caspase 8 activation and necroptotic signaling via multiple cell death checkpoints. Cell Death Dis. 7:e2381 10.1038/cddis.2016.294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurung P., and Kanneganti T.D.. 2016. Autoinflammatory Skin Disorders: The Inflammasomme in Focus. Trends Mol. Med. 22:545–564. 10.1016/j.molmed.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurung P., Malireddi R.K., Anand P.K., Demon D., Walle L.V., Liu Z., Vogel P., Lamkanfi M., and Kanneganti T.D.. 2012. Toll or Interleukin-1 Receptor (TIR) Domain-containing Adaptor Inducing Interferon-beta (TRIF)-mediated Caspase-11 Protease Production Integrates Toll-like Receptor 4 (TLR4) Protein- and Nlrp3 Inflammasome-mediated Host Defense against Enteropathogens. J. Biol. Chem. 287:34474–34483. 10.1074/jbc.M112.401406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurung P., Anand P.K., Malireddi R.K., Vande Walle L., Van Opdenbosch N., Dillon C.P., Weinlich R., Green D.R., Lamkanfi M., and Kanneganti T.D.. 2014. FADD and caspase-8 mediate priming and activation of the canonical and noncanonical Nlrp3 inflammasomes. J. Immunol. 192:1835–1846. 10.4049/jimmunol.1302839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurung P., Lukens J.R., and Kanneganti T.D.. 2015. Mitochondria: diversity in the regulation of the NLRP3 inflammasome. Trends Mol. Med. 21:193–201. 10.1016/j.molmed.2014.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden M.S., and Ghosh S.. 2008. Shared principles in NF-kappaB signaling. Cell. 132:344–362. 10.1016/j.cell.2008.01.020 [DOI] [PubMed] [Google Scholar]
- Hoffman H.M., Mueller J.L., Broide D.H., Wanderer A.A., and Kolodner R.D.. 2001a Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat. Genet. 29:301–305. 10.1038/ng756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman H.M., Wanderer A.A., and Broide D.H.. 2001b Familial cold autoinflammatory syndrome: phenotype and genotype of an autosomal dominant periodic fever. J. Allergy Clin. Immunol. 108:615–620. 10.1067/mai.2001.118790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H.L., Chiang C.H., Hung W.C., and Hou M.F.. 2015. Targeting of TGF-beta-activated protein kinase 1 inhibits chemokine (C-C motif) receptor 7 expression, tumor growth and metastasis in breast cancer. Oncotarget. 6:995–1007. 10.18632/oncotarget.2739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inokuchi S., Aoyama T., Miura K., Osterreicher C.H., Kodama Y., Miyai K., Akira S., Brenner D.A., and Seki E.. 2010. Disruption of TAK1 in hepatocytes causes hepatic injury, inflammation, fibrosis, and carcinogenesis. Proc. Natl. Acad. Sci. USA. 107:844–849. 10.1073/pnas.0909781107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer S.S., He Q., Janczy J.R., Elliott E.I., Zhong Z., Olivier A.K., Sadler J.J., Knepper-Adrian V., Han R., Qiao L., et al. 2013. Mitochondrial cardiolipin is required for Nlrp3 inflammasome activation. Immunity. 39:311–323. 10.1016/j.immuni.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juliana C., Fernandes-Alnemri T., Kang S., Farias A., Qin F., and Alnemri E.S.. 2012. Non-transcriptional priming and deubiquitination regulate NLRP3 inflammasome activation. J. Biol. Chem. 287:36617–36622. 10.1074/jbc.M112.407130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajino-Sakamoto R., Inagaki M., Lippert E., Akira S., Robine S., Matsumoto K., Jobin C., and Ninomiya-Tsuji J.. 2008. Enterocyte-derived TAK1 signaling prevents epithelium apoptosis and the development of ileitis and colitis. J. Immunol. 181:1143–1152. 10.4049/jimmunol.181.2.1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajino-Sakamoto R., Omori E., Nighot P.K., Blikslager A.T., Matsumoto K., and Ninomiya-Tsuji J.. 2010. TGF-beta-activated kinase 1 signaling maintains intestinal integrity by preventing accumulation of reactive oxygen species in the intestinal epithelium. J. Immunol. 185:4729–4737. 10.4049/jimmunol.0903587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang T.B., Yang S.H., Toth B., Kovalenko A., and Wallach D.. 2013. Caspase-8 blocks kinase RIPK3-mediated activation of the NLRP3 inflammasome. Immunity. 38:27–40. 10.1016/j.immuni.2012.09.015 [DOI] [PubMed] [Google Scholar]
- Kanneganti T.D., Ozoren N., Body-Malapel M., Amer A., Park J.H., Franchi L., Whitfield J., Barchet W., Colonna M., Vandenabeele P., et al. 2006. Bacterial RNA and small antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature. 440:233–236. 10.1038/nature04517 [DOI] [PubMed] [Google Scholar]
- Kayagaki N., Warming S., Lamkanfi M., Vande Walle L., Louie S., Dong J., Newton K., Qu Y., Liu J., Heldens S., et al. 2011. Non-canonical inflammasome activation targets caspase-11. Nature. 479:117–121. 10.1038/nature10558 [DOI] [PubMed] [Google Scholar]
- Kelliher M.A., Grimm S., Ishida Y., Kuo F., Stanger B.Z., and Leder P.. 1998. The death domain kinase RIP mediates the TNF-induced NF-kappaB signal. Immunity. 8:297–303. 10.1016/S1074-7613(00)80535-X [DOI] [PubMed] [Google Scholar]
- Kilty I., and Jones L.H.. 2015. TAK1 selective inhibition: state of the art and future opportunities. Future Med. Chem. 7:23–33. 10.4155/fmc.14.138 [DOI] [PubMed] [Google Scholar]
- Kuriakose T., Man S.M., Malireddi R.K., Karki R., Kesavardhana S., Place D.E., Neale G., Vogel P., and Kanneganti T.D.. 2016. ZBP1/DAI is an innate sensor of influenza virus triggering the NLRP3 inflammasome and programmed cell death pathways. Sci. Immunol. 1:aag2045 10.1126/sciimmunol.aag2045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamothe B., Lai Y., Hur L., Orozco N.M., Wang J., Campos A.D., Xie M., Schneider M.D., Lockworth C.R., Jakacky J., et al. 2012. Deletion of TAK1 in the myeloid lineage results in the spontaneous development of myelomonocytic leukemia in mice. PLoS One. 7:e51228 10.1371/journal.pone.0051228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamothe B., Lai Y., Xie M., Schneider M.D., and Darnay B.G.. 2013. TAK1 is essential for osteoclast differentiation and is an important modulator of cell death by apoptosis and necroptosis. Mol. Cell. Biol. 33:582–595. 10.1128/MCB.01225-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawlor K.E., Khan N., Mildenhall A., Gerlic M., Croker B.A., D’Cruz A.A., Hall C., Kaur Spall S., Anderton H., Masters S.L., et al. 2015. RIPK3 promotes cell death and NLRP3 inflammasome activation in the absence of MLKL. Nat. Commun. 6:6282 10.1038/ncomms7282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Goff C., Rogers C., Le Goff W., Pinto G., Bonnet D., Chrabieh M., Alibeu O., Nistchke P., Munnich A., Picard C., and Cormier-Daire V.. 2016. Heterozygous Mutations in MAP3K7, Encoding TGF-beta-Activated Kinase 1, Cause Cardiospondylocarpofacial Syndrome. Am. J. Hum. Genet. 99:407–413. 10.1016/j.ajhg.2016.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariathasan S., Newton K., Monack D.M., Vucic D., French D.M., Lee W.P., Roose-Girma M., Erickson S., and Dixit V.M.. 2004. Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature. 430:213–218. 10.1038/nature02664 [DOI] [PubMed] [Google Scholar]
- Mihaly S.R., Ninomiya-Tsuji J., and Morioka S.. 2014. TAK1 control of cell death. Cell Death Differ. 21:1667–1676. 10.1038/cdd.2014.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihaly S.R., Sakamachi Y., Ninomiya-Tsuji J., and Morioka S.. 2017. Noncanocial cell death program independent of caspase activation cascade and necroptotic modules is elicited by loss of TGFbeta-activated kinase 1. Sci. Rep. 7:2918 10.1038/s41598-017-03112-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morioka S., Broglie P., Omori E., Ikeda Y., Takaesu G., Matsumoto K., and Ninomiya-Tsuji J.. 2014. TAK1 kinase switches cell fate from apoptosis to necrosis following TNF stimulation. J. Cell Biol. 204:607–623. 10.1083/jcb.201305070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J.M., Czabotar P.E., Hildebrand J.M., Lucet I.S., Zhang J.G., Alvarez-Diaz S., Lewis R., Lalaoui N., Metcalf D., Webb A.I., et al. 2013. The pseudokinase MLKL mediates necroptosis via a molecular switch mechanism. Immunity. 39:443–453. 10.1016/j.immuni.2013.06.018 [DOI] [PubMed] [Google Scholar]
- Newton K., Sun X., and Dixit V.M.. 2004. Kinase RIP3 is dispensable for normal NF-kappa Bs, signaling by the B-cell and T-cell receptors, tumor necrosis factor receptor 1, and Toll-like receptors 2 and 4. Mol. Cell. Biol. 24:1464–1469. 10.1128/MCB.24.4.1464-1469.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ninomiya-Tsuji J., Kajino T., Ono K., Ohtomo T., Matsumoto M., Shiina M., Mihara M., Tsuchiya M., and Matsumoto K.. 2003. A resorcylic acid lactone, 5Z-7-oxozeaenol, prevents inflammation by inhibiting the catalytic activity of TAK1 MAPK kinase kinase. J. Biol. Chem. 278:18485–18490. 10.1074/jbc.M207453200 [DOI] [PubMed] [Google Scholar]
- Okada M., Matsuzawa A., Yoshimura A., and Ichijo H.. 2014. The lysosome rupture-activated TAK1-JNK pathway regulates NLRP3 inflammasome activation. J. Biol. Chem. 289:32926–32936. 10.1074/jbc.M114.579961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omori E., Matsumoto K., Sanjo H., Sato S., Akira S., Smart R.C., and Ninomiya-Tsuji J.. 2006. TAK1 is a master regulator of epidermal homeostasis involving skin inflammation and apoptosis. J. Biol. Chem. 281:19610–19617. 10.1074/jbc.M603384200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasparakis M., Alexopoulou L., Episkopou V., and Kollias G.. 1996. Immune and inflammatory responses in TNF α-deficient mice: A critical requirement for TNF α in the formation of primary B cell follicles, follicular dendritic cell networks and germinal centers, and in the maturation of the humoral immune response. J. Exp. Med. 184:1397–1411. 10.1084/jem.184.4.1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeffer K., Matsuyama T., Kundig T.M., Wakeham A., Kishihara K., Shahinian A., Wiegmann K., Ohashi P.S., Kronke M., and Mak T.W.. 1993. Mice deficient for the 55 kd tumor necrosis factor receptor are resistant to endotoxic shock, yet succumb to L. monocytogenes infection. Cell. 73:457–467. 10.1016/0092-8674(93)90134-C [DOI] [PubMed] [Google Scholar]
- Py B.F., Kim M.S., Vakifahmetoglu-Norberg H., and Yuan J.. 2013. Deubiquitination of NLRP3 by BRCC3 critically regulates inflammasome activity. Mol. Cell. 49:331–338. 10.1016/j.molcel.2012.11.009 [DOI] [PubMed] [Google Scholar]
- Sakamachi Y., Morioka S., Mihaly S.R., Takaesu G., Foley J.F., Fessler M.B., and Ninomiya-Tsuji J.. 2017. TAK1 regulates resident macrophages by protecting lysosomal integrity. Cell Death Dis. 8:e2598 10.1038/cddis.2017.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakurai H. 2012. Targeting of TAK1 in inflammatory disorders and cancer. Trends Pharmacol. Sci. 33:522–530. 10.1016/j.tips.2012.06.007 [DOI] [PubMed] [Google Scholar]
- Sanna M.G., da Silva Correia J., Ducrey O., Lee J., Nomoto K., Schrantz N., Deveraux Q.L., and Ulevitch R.J.. 2002. IAP suppression of apoptosis involves distinct mechanisms: the TAK1/JNK1 signaling cascade and caspase inhibition. Mol. Cell. Biol. 22:1754–1766. 10.1128/MCB.22.6.1754-1766.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato S., Sanjo H., Takeda K., Ninomiya-Tsuji J., Yamamoto M., Kawai T., Matsumoto K., Takeuchi O., and Akira S.. 2005. Essential function for the kinase TAK1 in innate and adaptive immune responses. Nat. Immunol. 6:1087–1095. 10.1038/ni1255 [DOI] [PubMed] [Google Scholar]
- Schmid-Burgk J.L., Chauhan D., Schmidt T., Ebert T.S., Reinhardt J., Endl E., and Hornung V.. 2016. A Genome-wide CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) Screen Identifies NEK7 as an Essential Component of NLRP3 Inflammasome Activation. J. Biol. Chem. 291:103–109. 10.1074/jbc.C115.700492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma D., and Kanneganti T.D.. 2016. The cell biology of inflammasomes: Mechanisms of inflammasome activation and regulation. J. Cell Biol. 213:617–629. 10.1083/jcb.201602089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim J.H., Xiao C., Paschal A.E., Bailey S.T., Rao P., Hayden M.S., Lee K.Y., Bussey C., Steckel M., Tanaka N., et al. 2005. TAK1, but not TAB1 or TAB2, plays an essential role in multiple signaling pathways in vivo. Genes Dev. 19:2668–2681. 10.1101/gad.1360605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A., Sweeney M.F., Yu M., Burger A., Greninger P., Benes C., Haber D.A., and Settleman J.. 2012. TAK1 inhibition promotes apoptosis in KRAS-dependent colon cancers. Cell. 148:639–650. 10.1016/j.cell.2011.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swarnkar G., Karuppaiah K., Mbalaviele G., Chen T.H., and Abu-Amer Y.. 2015. Osteopetrosis in TAK1-deficient mice owing to defective NF-kappaB and NOTCH signaling. Proc. Natl. Acad. Sci. USA. 112:154–159. 10.1073/pnas.1415213112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang M., Wei X., Guo Y., Breslin P., Zhang S., Zhang S., Wei W., Xia Z., Diaz M., Akira S., and Zhang J.. 2008. TAK1 is required for the survival of hematopoietic cells and hepatocytes in mice. J. Exp. Med. 205:1611–1619. 10.1084/jem.20080297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The International FMF Consortium 1997. Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. The International FMF Consortium. Cell. 90:797–807. 10.1016/S0092-8674(00)80539-5 [DOI] [PubMed] [Google Scholar]
- Vanlangenakker N., Vanden Berghe T., Bogaert P., Laukens B., Zobel K., Deshayes K., Vucic D., Fulda S., Vandenabeele P., and Bertrand M.J.. 2011. cIAP1 and TAK1 protect cells from TNF-induced necrosis by preventing RIP1/RIP3-dependent reactive oxygen species production. Cell Death Differ. 18:656–665. 10.1038/cdd.2010.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade E.M., Daniel P.B., Jenkins Z.A., McInerney-Leo A., Leo P., Morgan T., Addor M.C., Ades L.C., Bertola D., Bohring A., et al. 2016. Mutations in MAP3K7 that Alter the Activity of the TAK1 Signaling Complex Cause Frontometaphyseal Dysplasia. Am. J. Hum. Genet. 99:392–406. 10.1016/j.ajhg.2016.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan Y.Y., Chi H., Xie M., Schneider M.D., and Flavell R.A.. 2006. The kinase TAK1 integrates antigen and cytokine receptor signaling for T cell development, survival and function. Nat. Immunol. 7:851–858. 10.1038/ni1355 [DOI] [PubMed] [Google Scholar]
- Wang C., Deng L., Hong M., Akkaraju G.R., Inoue J., and Chen Z.J.. 2001. TAK1 is a ubiquitin-dependent kinase of MKK and IKK. Nature. 412:346–351. 10.1038/35085597 [DOI] [PubMed] [Google Scholar]
- Wang X., Jiang W., Yan Y., Gong T., Han J., Tian Z., and Zhou R.. 2014. RNA viruses promote activation of the NLRP3 inflammasome through a RIP1-RIP3-DRP1 signaling pathway. Nat. Immunol. 15:1126–1133. 10.1038/ni.3015 [DOI] [PubMed] [Google Scholar]
- Yamaguchi K., Shirakabe K., Shibuya H., Irie K., Oishi I., Ueno N., Taniguchi T., Nishida E., and Matsumoto K.. 1995. Identification of a member of the MAPKKK family as a potential mediator of TGF-beta signal transduction. Science. 270:2008–2011. 10.1126/science.270.5244.2008 [DOI] [PubMed] [Google Scholar]
- Zhang Q., Lenardo M.J., and Baltimore D.. 2017. 30 Years of NF-kappaB: A Blossoming of Relevance to Human Pathobiology. Cell. 168:37–57. 10.1016/j.cell.2016.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Z., Umemura A., Sanchez-Lopez E., Liang S., Shalapour S., Wong J., He F., Boassa D., Perkins G., Ali S.R., et al. 2016. NF-kappaB Restricts Inflammasome Activation via Elimination of Damaged Mitochondria. Cell. 164:896–910. 10.1016/j.cell.2015.12.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.