Abstract
Introduction
Particulate matter and air pollution in Korea are becoming worse. There is a lack of research regarding the impact of particulate matter on patients with COPD. Therefore, the purpose of this study was to investigate the effects of various air pollution factors, including particulate matter, on the incidence rate of severe acute exacerbations of COPD (AECOPD) events.
Methods
We analyzed the relationship between air pollutants and AECOPD events that required hospitalization at Guro Hospital in Korea from January 1, 2015 to May 31, 2017. We used general linear models with Poisson distribution and log-transformation to obtain adjusted relative risk (RR). We conducted further analysis through the Comprehensive Air-quality Index (CAI) that is used in Korea.
Results
Among various other air pollutants, particulate matter was identified as a major source of air pollution in Korea. When the CAI score was over 50, the incidence rate of severe AECOPD events was statistically significantly higher [RR 1.612, 95% CI, 1.065–2.440, P=0.024]. Additionally, the particulate matter levels 3 days before hospitalization were statistically significant [RR 1.003, 95% CI, 1.001–1.005, P=0.006].
Conclusion
Particulate matter and air pollution increase the incidence rate of severe AECOPD events. COPD patients should be cautioned against outdoor activities when particulate matter levels are high.
Keywords: air pollution, particulate matter, air quality index, acute exacerbation, COPD
Introduction
Air pollution is a global environmental issue.1 Among the many air pollutants, the problem of particulate matter (PM) in China is causing global concern.2 PM is a complex mixture of extremely small solid and liquid particles (diameter of less than 10 µm) floating in air. Similarly, concerns regarding PM have also grown in Korea over the past several years.3 According to some surveys, the capital of Korea, Seoul, is a city with a high concentration of PM. Currently, the Korean government and organizations are preparing various policies and regulations regarding PM.
Many countries and government agencies are using the air quality index (AQI) in assessing the degree of air pollution.4 Air is a mixture of various gases, and AQI is obtained by integrating the pollution degree of various gases, like PM, ozone (O3), nitrogen dioxide (NO2), sulfur dioxide (SO2), and carbon monoxide (CO). Korea uses the Comprehensive Air-quality Index (CAI). The CAI is used to analyze and prevent the effects of air pollution on public health.5 However, there is an insufficiency of research about clinical adverse effects of PM and air pollution in Korea.
PM is thought to cause direct damage to the lungs, bronchi and skin6,7 as well as an abnormal inflammatory response and coagulopathy, resulting in various diseases.8,9 PM can have a more harmful impact on patients with pulmonary diseases, such as COPD.10 However, studies regarding the harmful effects of PM on COPD and acute exacerbation of COPD (AECOPD) are lacking. There has been recent study in Korea showing that the concentration of PM was associated with hospitalization for asthma, acute bronchitis, and acute rhinitis.11 However most studies on PM in Korea have focused on asthma or cardiovascular disease.12,13 Therefore, the purpose of this study was to investigate the harmful impact of various air pollution factors, including PM, on the incidence rate of severe AECOPD events.
Materials and methods
Collection of patient data
We found AECOPD events that required hospitalization at Korea University Guro Hospital by searching the hospital’s electronic records. This study was approved by the Institutional Review Board of Korea University Guro Hospital (approval number KUGH16131-002). The study is a retrospective analysis, so did not need patient consent. We maintain the confidentiality of patient information. According to inclusion and exclusion criteria, 375 severe AECOPD events were identified. We defined severe AECOPD events as those that required hospitalization.14
Patients were included if they: 1) had undergone a pulmonary function test within 1 year that showed an obstructive pattern (a ratio of forced expiratory volume in the first second [FEV1] to forced vital capacity [FVC] of less than 70%)14 before the admission event; 2) had been hospitalized for “an acute worsening of respiratory symptoms that result in additional therapy, like short-acting inhaled beta2-agonists, maintenance therapy with long-acting bronchodilators, systemic corticosteroids, oxygen therapy, and antibiotics”;15 3) had been hospitalized through an emergency room or an outpatient clinic between January 1, 2015 and May 31, 2017; and 4) were over 40 years old.
Patients were excluded if: 1) they had cancer, an autoimmune disease, or an immune deficiency; or 2) the cause of admission was not AECOPD, but was, for example, acute heart failure, acute pulmonary edema, acute pulmonary embolism, pneumothorax, or arrhythmia.
Collection of air pollution and climate data
Air pollution and climate data were provided by the government of the Republic of South Korea and the city of Seoul. The air pollution measuring station was located in Guro, where the hospital is located; Guro is an area in Seoul.
We collected data on representative gases related to air pollution: PM with a diameter of less than 10 µm (PM10), PM with a diameter of less than 2.5 µm (PM2.5), ozone (O3), nitrogen dioxide (NO2), sulfur dioxide (SO2), and carbon monoxide (CO). We also received temperature and humidity data. All data included hourly, daily, weekly, and monthly average values.
Comprehensive Air-quality Index in Korea
We conducted further analysis through the CAI used in Korea. The CAI is a way of describing ambient air quality based on the level of health risks associated with the level of air pollution. The CAI has values of 0 through 500, which are divided into four categories. The higher the CAI value is, the greater the level of air pollution. We calculated the score for each air pollutant and used the highest score as the representative value. If there were two or more cases for which the calculated score was higher than the C grade, we added 50 points to the highest score. Detailed information regarding the CAI is shown in Tables 1 and 2.
Table 1.
Comprehensive Air-quality Index (CAI)
| Category | Description | Values | Health effects |
|---|---|---|---|
| A | Good | 0–50 | A level that will not impact patients suffering from diseases related to air pollution |
| B | Moderate | 51–100 | A level that may have minimal impact on patients in cases of chronic exposure |
| C | Unhealthy | 101–250 | A level that may have harmful impacts on patients and members of sensitive groups, and that may also cause the general public unpleasant side effects |
| D | Very unhealthy | 251–500 | A level that may require emergency measures for patients and members of sensitive groups, and that may have harmful impacts on the general public |
Table 2.
The relationship between CAI value and air pollutants
| Category
|
A
|
B
|
C
|
D
|
|---|---|---|---|---|
| Description
|
Good
|
Moderate
|
Unhealthy
|
Very unhealthy
|
| Values | 0–50 | 51–100 | 101–250 | 251–500 |
| PM10 (µg/m3) | 0–30 | 31–80 | 81–150 | 151–600 |
| PM2.5 (µg/m3) | 0–15 | 16–50 | 51–100 | 101–500 |
| O3 (ppm) | 0–0.030 | 0.031–0.090 | 0.091–0.150 | 0.150–0.600 |
| NO2 (ppm) | 0–0.030 | 0.031–0.060 | 0.061–0.200 | 0.201–2 |
| SO2 (ppm) | 0–0.020 | 0.021–0.050 | 0.051–0.150 | 0.151–1 |
| CO (ppm) | 0–2 | 2.01–9 | 9.01–15 | 15.01–50 |
Abbreviations: CAI, Comprehensive Air-quality Index; PM10, particulate matter with a diameter of less than 10 µm; PM2.5, particulate matter with a diameter of less than 2.5 µm; O3, ozone; NO2, nitrogen dioxide; SO2, sulfur dioxide; CO, carbon monoxide.
Statistical analysis
Data were analyzed using SPSS 20 software (SPSS for windows, IBM Corporation, Armonk, NY, USA). Data points are reported as mean ± SD. The association between the incidence rate of severe AECOPD events and PM10 concentration or CAI score was analyzed by the application of general linear models with a Poisson distribution. General linear models with a Poisson distribution and log-transformation were used to analyze frequency or incidence rate in previous studies; this method is called Poisson regression analysis.11,16,17
The atmosphere is a complex system, which is influenced by various air pollutant gases and weather. To evaluate various air pollutant gases, we used the CAI, which combines six main air pollutants. Additionally, we analyzed the temperature and humidity in a Poisson regression analysis to adjust for the effect of weather. And, we also adjusted for day of the week (DOW) and holiday (Saturdays, Sundays, and public holidays) in a Poisson regression. A 95% CI was calculated using the Poisson regression analysis, and the CI range was defined as statistically significant when it was greater than 1.
Results
Air pollution and climate data in Korea
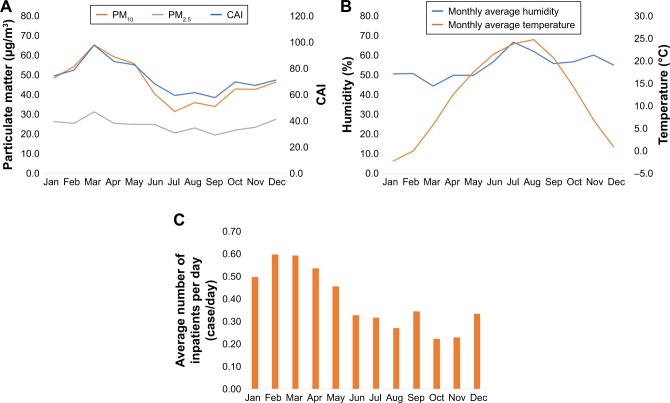
In Korea, PM10 and PM2.5 were identified as major air pollutants. There was no seasonal variation found for PM2.5. However, seasonal variation was found for PM10. PM10 was high between January and May every year. As a result, the CAI score also tended to increase during these months (Figure 1A). Korea has four distinct seasons; thus, the temperature and humidity showed distinct annual variation. Humidity was low in winter and high in summer and autumn (Figure 1B). The incidence rate of severe AECOPD events was found to be high in winter and spring (Figure 1C). Detailed monthly average data on levels of six air pollutant gases, temperature, and humidity are presented in Table 3.
Figure 1.
Monthly average data related to air pollutants and number of inpatients per day. (A) Monthly average CAI, PM10, and PM2.5. (B) Monthly average humidity and temperature. (C) Monthly average number of inpatients (patients admitted to hospital for AECOPD) per day.
Notes: The average from January to May is from 2015 to 2017; the average from June to December is from 2015 to 2016.
Abbreviations: CAI, Comprehensive Air-quality Index; PM10, particulate matter with a diameter of less than 10 µm; PM2.5, particulate matter with a diameter of less than 2.5 µm.
Table 3.
Monthly average data related to air pollutants
| CAI | PM10 (µg/m3) |
PM2.5 (µg/m3) |
O3 (ppm) |
NO2 (ppm) |
SO2 (ppm) |
CO (ppm) |
Temperature (°C) |
Humidity (%) |
|
|---|---|---|---|---|---|---|---|---|---|
| Jan | 77.1±29.3 | 50.2±18.9 | 27.4±11.7 | 0.012±0.006 | 0.031±0.011 | 0.006±0.001 | 0.7±0.2 | −2.0±4.2 | 54.7±12.4 |
| Feb | 81.5±45.0 | 56.2±41.6 | 26.3±10.7 | 0.016±0.006 | 0.030±0.010 | 0.007±0.002 | 0.6±0.2 | 0.4±3.6 | 54.9±13.5 |
| Mar | 101.2±50.2 | 67.6±28.2 | 32.4±12.4 | 0.024±0.007 | 0.031±0.011 | 0.007±0.002 | 0.6±0.2 | 6.7±4.0 | 47.9±11.9 |
| Apr | 88.3±34.8 | 61.3±26.4 | 26.3±10.0 | 0.031±0.010 | 0.027±0.008 | 0.006±0.002 | 0.6±0.1 | 14.0±2.8 | 53.8±16.5 |
| May | 85.8±41.3 | 57.8±27.3 | 25.8±10.7 | 0.038±0.008 | 0.023±0.007 | 0.007±0.001 | 0.5±0.1 | 19.3±2.7 | 53.7±14.6 |
| Jun | 70.9±10.6 | 42.1±13.6 | 25.8±8.7 | 0.039±0.007 | 0.023±0.006 | 0.006±0.001 | 0.4±0.1 | 22.5±23.6 | 61.3±11.5 |
| Jul | 66.8±17.9 | 32.5±14.8 | 21.3±10.2 | 0.034±0.015 | 0.020±0.006 | 0.005±0.001 | 0.4±0.1 | 23.9±26.0 | 72.0±11.3 |
| Aug | 62.1±16.2 | 37.4±15.1 | 24.0±11.2 | 0.034±0.011 | 0.020±0.007 | 0.006±0.001 | 0.4±0.1 | 28.3±27.1 | 66.8±6.7 |
| Sep | 63.3±13.8 | 35.3±13.9 | 20.2±9.4 | 0.028±0.008 | 0.024±0.009 | 0.005±0.001 | 0.4±0.1 | 24.6±22.7 | 60.4±10.8 |
| Oct | 58.1±37.9 | 44.4±23.4 | 22.8±15.1 | 0.019±0.006 | 0.028±0.011 | 0.006±0.001 | 0.5±0.2 | 18.7±15.8 | 61.3±11.4 |
| Nov | 79.1±26.0 | 44.2±20.1 | 24.3±12.4 | 0.012±0.007 | 0.029±0.009 | 0.006±0.001 | 0.6±0.2 | 4.3±7.8 | 65.0±12.6 |
| Dec | 70.0±27.8 | 48.0±16.5 | 28.5±11.8 | 0.009±0.006 | 0.032±0.009 | 0.006±0.001 | 0.7±0.2 | 4.1±1.4 | 59.5±12.4 |
Notes: The average from January to May is from 2015 to 2017; the average from June to December is from 2015 to 2016. Numbers are presented as mean ± SD.
Abbreviations: CAI, Comprehensive Air-quality Index; PM10, particulate matter with a diameter of less than 10 µm; PM2.5, particulate matter with a diameter of less than 2.5 µm; O3, ozone; NO2, nitrogen dioxide; SO2, sulfur dioxide; CO, carbon monoxide.
Comprehensive Air-quality Index
When classified as CAI categories, 0.26 cases were hospitalized per day in category A, and 0.45 cases were hospitalized per day in category B. However, there was no significant difference between categories B and C (Table 4). In addition, we analyzed the adjusted relative risk (RR) using the CAI 50, which is the distinguishing value between Categories A and B, and 100, which is the distinguishing value between Categories B and C. When analyzed on the cutoff value of 50, the incidence rate of severe AECOPD events was statistically significantly higher in the group with CAI values higher than 50 (RR 1.612, 95% CI 1.065–2.440, P=0.024). However, when analyzed on the cutoff value of 100, there was no statistically significant difference between the two groups (Table 5).
Table 4.
The association between CAI and severe AECOPD events
| CAI category
|
A
|
B
|
C
|
D
|
Total |
|---|---|---|---|---|---|
| CAI description | Good | Moderate | Unhealthy | Very unhealthy | |
| Total number of days | 94 | 696 | 82 | 10 | 882 |
| Total number of inpatients (cases) | 24 | 311 | 33 | 6 | 374 |
| Average number of inpatients per day (cases/day) | 0.26 | 0.45 | 0.40 | 0.60 |
Abbreviations: CAI, Comprehensive Air-quality Index; AECOPD, acute exacerbations of chronic obstructive pulmonary disease.
Table 5.
Risk of severe AECOPD events with cutoff values of CAI 50 and 100
| Cutoff value | Factors | RR | 95% CI | P-value |
|---|---|---|---|---|
| CAI 50 | CAI≤50 | 1 | ||
| CAI>50 | 1.612 | 1.065–2.440 | 0.024 | |
| Temperature (°C) | 0.989 | 0.979–0.999 | 0.034 | |
| Humidity (%) | 0.994 | 0.986–1.001 | 0.110 | |
| CAI 100 | CAI≤100 | 1 | ||
| CAI>100 | 1.025 | 0.736–1.429 | 0.882 | |
| Temperature (°C) | 0.989 | 0.979–0.999 | 0.033 | |
| Humidity (%) | 0.993 | 0.986–1.001 | 0.074 |
Abbreviations: AECOPD, acute exacerbations of chronic obstructive pulmonary disease; CAI, Comprehensive Air-quality Index; RR, adjusted relative risk.
Relationship between exposure time of air pollutant and hospitalization
We assessed the time at which PM and air pollution have the greatest effect on AECOPD events. PM10 levels 3 days before hospitalization were statistically significant (RR 1.003, 95% CI 1.001–1.005, P=0.006) (Figure 2A). Similarly, the CAI value 3 days before hospitalization was statistically significant (RR 1.002, 95% CI 1.000–1.004, P=0.019) (Figure 2B). In addition, the adjusted relative risk increased by 1.05 for every 10 µg/m3 of increased PM10 average level from the day of hospitalization to 3 days before hospitalization (P=0.020).
Figure 2.
Association of PM10, CAI and severe AECOPD events after adjustment for humidity and temperature. (A) The association of PM10 and severe AECOPD events. (B) The association of CAI and severe AECOPD events.
Abbreviations: PM10, particulate matter with a diameter of less than 10 µm; CAI, Comprehensive Air-quality Index; AECOPD, acute exacerbations of chronic obstructive pulmonary disease.
Discussion
Our study is the first study in Korea to investigate how PM and air pollution affect the incidence rate of severe AECOPD events. We analyzed six gases (PM10, PM2.5, CO, O3, NO2, and SO2) that are considered to be representative air pollutants.18 Additionally, we used an AQI called the CAI, which is used in Korea.19 Because air pollutant concentration and clearance rate vary depending on weather, we analyzed temperature and humidity together, using Poisson regression analysis.20 In addition, we adjusted for DOW and holidays in a Poisson regression analysis. In Korea, the main reason for choosing a particular hospital is the distance to the hospital from the patient’s house; therefore, the spatial location is based on the Guro area, where the hospital is located. Daily, weekly, and monthly analyses were performed. According to our results, PM and air pollution increase the incidence rate of severe AECOPD events in Korea.
Air pollution is a major global problem affecting health.21 PM is the most serious source of air pollution in Korea.11 Our study did not find high concentrations of other air pollutants (CO, O3, NO2, and SO2). For many years, large amounts of PM from China have been flowing into Korea.22,23 PM is generated in various ways in Korea, such as through the construction industry, automobile use, and heating systems.24,25 The number of PM warnings has also steadily increased in Korea since 2013. According to our results, PM10 and PM2.5 levels have not decreased for several years. Also, PM10 appears to increase during winter and spring each year. In Korea, COPD patients should pay attention to daily activities in winter and spring when there are high levels of PM. For example COPD patients should avoid outdoor activities, use masks, and keep windows closed at home when PM levels are high.
PM acts as an irritant at the moment of respiration, and damages the lungs, bronchi, and mucous membranes.26 In addition to acute damage, PM enters the body and causes abnormal inflammatory responses and coagulopathy.9 Recent study shows that PM2.5 contributes to abnormal airway inflammation through various signaling pathways, such as epidermal growth factor receptor (EGFR), mitogen-activated protein kinase (MAPK), nuclear factor (NF)-kB and the interleukin pathway.27–29 Also, PM2.5 affects the fractional concentration of exhaled nitric oxide (FeNO), which can lead to airway inflammation in COPD patients.30 These abnormal inflammatory responses and signaling pathways are related to a variety of diseases, such as myocardial infarction, stroke, embolism, and cancer.31–33 Furthermore, when PM is absorbed into the body it can produce oxidative stress.34 PM directly increases reactive oxygen species, which cause DNA damage.35 Transition metals or organic compounds may modulate mitochondria or nicotinamide adenine dinucleotide phosphate (NADPH)-oxidase, which deteriorates their function.36 Our results showed that PM10 and CAI levels at 3 days before hospitalization had the greatest correlation with admission rate for severe AECOPD events. We estimate that this is due to abnormal inflammatory response and oxidative stress. Because of these responses, it is necessary to consider not only acute periods, but also sub-acute and chronic periods, in the study of PM.
Various epidemiological studies related to PM have been conducted, mainly in China. Several systematic reviews and meta-analyses have shown that PM exposure is associated with mortality, hospitalization and emergency department visits in COPD patients.37–39 These results were confirmed with both PM10 and PM2.5. PM may be related to various respiratory diseases, such as lung cancer, COPD, asthma, bronchiectasis and chronic cough.40,41 There is also a relationship with the prognosis and mortality of the general public.42,43 It is possible that not only AECOPD, but also acute exacerbation of asthma and bronchiectasis, may increase.44 If air pollution becomes worse, it may become a major cause of COPD, along with smoking.45 Long-term studies related to the occurrence of COPD are needed to better understand the disease.
Most guidelines and government policies about PM and air pollution are based on the general public, not COPD patients.46,47 However, patients with pulmonary disease can be seriously affected by lower levels of PM which may not affect healthy people. Our study also showed a significant difference in incidence rate in CAI 50, not in CAI 100, which is the standard for the general public in Korea. Specific guidelines and government support for COPD patients are needed.
Our study has some limitations. First, this study is a single center study. Guro is one of the regions in Korea where the PM level is high. Analysis in areas with low PM levels is required. Secondly, only hospitalized events were analyzed. It is unclear whether the incidence rate of AECOPD events that do not require hospitalization will increase as well. A study encompassing both types of AECOPD events is needed. Third, the causes of AECOPD were not analyzed. The causes of AECOPD can be classified as either infectious or non-infectious. Infectious causes include bacteria or viruses; non-infectious causes include air pollution, drugs, cold temperatures, allergens, smoking and emotional stress. Further analysis of laboratory findings after admission or history taking will help determine the cause of AECOPD. However, this study is a retrospective study; some of the patients’ in-hospital data were insufficient and we could not analyze the causes of AECOPD. Fourth, as representative data of air pollution, we used ambient pollutant concentrations from a monitoring station in Guro. This may be different to individual PM exposure, and this might lead to underestimation or overestimation of the RR.
However, we adjusted various factors that could affect air pollution through Poisson regression analysis, such as the temperature, humidity, DOW and holiday; and we conducted analysis including six representative air pollution gases and the AQI. In addition, we performed a time analysis of the most influential exposure periods. In the future, large-scale studies will be needed on air pollution and AECOPD in various regions.
Conclusion
PM and air pollution increase the incidence rate of severe AECOPD events. PM and air pollution are considered to be major non-infectious causes of AECOPD events. COPD patients should be cautioned against outdoor activities when PM levels are high.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Colao A, Muscogiuri G, Piscitelli P. Environment and health: not only cancer. Int J Environ Res Public Health. 2016;13(7):724. doi: 10.3390/ijerph13070724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang J, Zhao B, Wang S, et al. Particulate matter pollution over China and the effects of control policies. Sci Total Environ. 2017;584-585:426–447. doi: 10.1016/j.scitotenv.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 3.Kamimura A, Armenta B, Nourian M, Assasnik N, Nourian K, Chernenko A. Perceived environmental pollution and its impact on health in China, Japan, and South Korea. J Prev Med Public Health. 2017;50(3):188–194. doi: 10.3961/jpmph.17.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thach TQ, Tsang H, Cao P, Ho LM. A novel method to construct an air quality index based on air pollution profiles. Int J Hyg Environ Health. 2018;221(1):17–26. doi: 10.1016/j.ijheh.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Choi G, Heo S, Lee JT. Assessment of environmental injustice in Korea using synthetic air quality index and multiple indicators of socioeconomic status: A cross-sectional study. J Air Waste Manag Assoc. 2016;66(1):28–37. doi: 10.1080/10962247.2015.1107657. [DOI] [PubMed] [Google Scholar]
- 6.Wang C, Cai J, Chen R, et al. Personal exposure to fine particulate matter, lung function and serum club cell secretory protein (Clara) Environ Pollut. 2017;225:450–455. doi: 10.1016/j.envpol.2017.02.068. [DOI] [PubMed] [Google Scholar]
- 7.Kim KE, Cho D, Park HJ. Air pollution and skin diseases: Adverse effects of airborne particulate matter on various skin diseases. Life Sci. 2016;152:126–134. doi: 10.1016/j.lfs.2016.03.039. [DOI] [PubMed] [Google Scholar]
- 8.Bind MA, Baccarelli A, Zanobetti A, et al. Air pollution and markers of coagulation, inflammation, and endothelial function: associations and epigene-environment interactions in an elderly cohort. Epidemiology. 2012;23(2):332–340. doi: 10.1097/EDE.0b013e31824523f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu C, Cai J, Qiao L, et al. The acute effects of fine particulate matter constituents on blood inflammation and coagulation. Environ Sci Technol. 2017;51(14):8128–8137. doi: 10.1021/acs.est.7b00312. [DOI] [PubMed] [Google Scholar]
- 10.Ni L, Chuang CC, Zuo L. Fine particulate matter in acute exacerbation of COPD. Front Physiol. 2015;6:294. doi: 10.3389/fphys.2015.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jo EJ, Lee WS, Jo HY, et al. Effects of particulate matter on respiratory disease and the impact of meteorological factors in Busan, Korea. Respir Med. 2017;124:79–87. doi: 10.1016/j.rmed.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Park JW, Lim YH, Kyung SY, et al. Effects of ambient particulate matter on peak expiratory flow rates and respiratory symptoms of asthmatics during Asian dust periods in Korea. Respirology. 2005;10(4):470–476. doi: 10.1111/j.1440-1843.2005.00728.x. [DOI] [PubMed] [Google Scholar]
- 13.Hwang SH, Lee JY, Yi SM, Kim H. Associations of particulate matter and its components with emergency room visits for cardiovascular and respiratory diseases. PLoS One. 2017;12(8):e0183224. doi: 10.1371/journal.pone.0183224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report: GOLD Executive Summary. Eur Respir J. 2017;49(3):1700214. doi: 10.1183/13993003.00214-2017. [DOI] [PubMed] [Google Scholar]
- 15.Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi: 10.1016/S0140-6736(07)61382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nastos PT, Matzarakis A. Weather impacts on respiratory infections in Athens, Greece. Int J Biometeorol. 2006;50(6):358–369. doi: 10.1007/s00484-006-0031-1. [DOI] [PubMed] [Google Scholar]
- 17.Panagiotakos DB, Chrysohoou C, Pitsavos C, et al. Climatological variations in daily hospital admissions for acute coronary syndromes. Int J Cardiol. 2004;94(2–3):229–233. doi: 10.1016/j.ijcard.2003.04.050. [DOI] [PubMed] [Google Scholar]
- 18.Kang SH, Heo J, Oh IY, et al. Ambient air pollution and out-of-hospital cardiac arrest. Int J Cardiol. 2016;203:1086–1092. doi: 10.1016/j.ijcard.2015.11.100. [DOI] [PubMed] [Google Scholar]
- 19.Oh T, Kim M, Lim J, et al. A real-time monitoring and assessment method for calculation of total amounts of indoor air pollutants emitted in subway stations. J Air Waste Manag Assoc. 2012;62(5):517–526. doi: 10.1080/10962247.2012.660558. [DOI] [PubMed] [Google Scholar]
- 20.D’Amato G, Pawankar R, Vitale C, et al. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res. 2016;8(5):391–395. doi: 10.4168/aair.2016.8.5.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brook RD, Newby DE, Rajagopalan S. The global threat of outdoor ambient air pollution to cardiovascular health: time for intervention. JAMA Cardiol. 2017;2(4):353–354. doi: 10.1001/jamacardio.2017.0032. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Ying Q, Hu J, Zhang H. Spatial and temporal variations of six criteria air pollutants in 31 provincial capital cities in China during 2013–2014. Environ Int. 2014;73:413–422. doi: 10.1016/j.envint.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 23.Song C, Wu L, Xie Y, et al. Air pollution in China: Status and spatiotemporal variations. Environ Pollut. 2017;227:334–347. doi: 10.1016/j.envpol.2017.04.075. [DOI] [PubMed] [Google Scholar]
- 24.Ogundele LT, Owoade OK, Hopke PK, Olise FS. Heavy metals in industrially emitted particulate matter in Ile-Ife, Nigeria. Environ Res. 2017;156:320–325. doi: 10.1016/j.envres.2017.03.051. [DOI] [PubMed] [Google Scholar]
- 25.Zhang X, Staimer N, Tjoa T, et al. Associations between microvascular function and short-term exposure to traffic-related air pollution and particulate matter oxidative potential. Environ Health. 2016;15(1):81. doi: 10.1186/s12940-016-0157-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Del Donno M, Verduri A, Olivieri D. Air pollution and reversible chronic respiratory diseases. Monaldi Arch Chest Dis. 2002;57(3–4):164–166. [PubMed] [Google Scholar]
- 27.Jeong SC, Cho Y, Song MK, Lee E, Ryu JC. Epidermal growth factor receptor (EGFR)-MAPK-nuclear factor(NF)-kappaB-IL8: A possible mechanism of particulate matter(PM) 2.5-induced lung toxicity. Environ Toxicol. 2017;32(5):1628–1636. doi: 10.1002/tox.22390. [DOI] [PubMed] [Google Scholar]
- 28.Kim HJ, Choi MG, Park MK, Seo YR. Predictive and prognostic biomarkers of respiratory diseases due to particulate matter exposure. J Cancer Prev. 2017;22(1):6–15. doi: 10.15430/JCP.2017.22.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yan Z, Jin Y, An Z, Liu Y, Samet JM, Wu W. Inflammatory cell signaling following exposures to particulate matter and ozone. Biochim Biophys Acta. 2016;1860(12):2826–2834. doi: 10.1016/j.bbagen.2016.03.030. [DOI] [PubMed] [Google Scholar]
- 30.Chen R, Qiao L, Li H, et al. Fine particulate matter constituents, nitric oxide synthase dna methylation and exhaled nitric oxide. Environ Sci Technol. 2015;49(19):11859–11865. doi: 10.1021/acs.est.5b02527. [DOI] [PubMed] [Google Scholar]
- 31.McGuinn LA, Ward-Caviness C, Neas LM, et al. Fine particulate matter and cardiovascular disease: Comparison of assessment methods for long-term exposure. Environ Res. 2017;159:16–23. doi: 10.1016/j.envres.2017.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tian Y, Xiang X, Wu Y, et al. Fine particulate air pollution and first hospital admissions for ischemic stroke in Beijing, China. Sci Rep. 2017;7(1):3897. doi: 10.1038/s41598-017-04312-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoek G, Brunekreef B, Fischer P, van Wijnen J. The association between air pollution and heart failure, arrhythmia, embolism, thrombosis, and other cardiovascular causes of death in a time series study. Epidemiology. 2001;12(3):355–357. doi: 10.1097/00001648-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 34.Risom L, Moller P, Loft S. Oxidative stress-induced DNA damage by particulate air pollution. Mutat Res. 2005;592(1–2):119–137. doi: 10.1016/j.mrfmmm.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 35.Bates JT, Weber RJ, Abrams J, et al. Reactive oxygen species generation linked to sources of atmospheric particulate matter and cardiorespiratory effects. Environ Sci Technol. 2015;49(22):13605–13612. doi: 10.1021/acs.est.5b02967. [DOI] [PubMed] [Google Scholar]
- 36.Holland NA, Fraiser CR, Sloan RC, 3rd, Devlin RB, Brown DA, Wingard CJ. Ultrafine particulate matter increases cardiac ischemia/reperfusion injury via mitochondrial permeability transition pore. Cardiovasc Toxicol. 2017;17(4):441–450. doi: 10.1007/s12012-017-9402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax. 2014;69(7):660–665. doi: 10.1136/thoraxjnl-2013-204492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DeVries R, Kriebel D, Sama S. Outdoor air pollution and COPD-related emergency department visits, hospital admissions, and mortality: a meta-analysis. COPD. 2017;14(1):113–121. doi: 10.1080/15412555.2016.1216956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu R, Chen Y, Wu S, Deng F, Liu Y, Yao W. The relationship between particulate matter (PM10) and hospitalizations and mortality of chronic obstructive pulmonary disease: a meta-analysis. COPD. 2013;10(3):307–315. doi: 10.3109/15412555.2012.744962. [DOI] [PubMed] [Google Scholar]
- 40.Gharibvand L, Lawrence Beeson W, Shavlik D, et al. The association between ambient fine particulate matter and incident adenocarcinoma subtype of lung cancer. Environ Health. 2017;16(1):71. doi: 10.1186/s12940-017-0268-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bloemsma LD, Hoek G, Smit LA. Panel studies of air pollution in patients with COPD: Systematic review and meta-analysis. Environ Res. 2016;151:458–468. doi: 10.1016/j.envres.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 42.Shang Y, Sun Z, Cao J, et al. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ Int. 2013;54:100–111. doi: 10.1016/j.envint.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 43.Sifaki-Pistolla D, Lionis C, Koinis F, Georgoulias V, Tzanakis N. Cancer Registry of C. Lung cancer and annual mean exposure to outdoor air pollution in Crete, Greece. Eur J Cancer Prev. 2017;26:S208–S214. doi: 10.1097/CEJ.0000000000000407. [DOI] [PubMed] [Google Scholar]
- 44.Pothirat C, Tosukhowong A, Chaiwong W, Liwsrisakun C, Inchai J. Effects of seasonal smog on asthma and COPD exacerbations requiring emergency visits in Chiang Mai, Thailand. Asian Pac J Allergy Immunol. 2016;34(4):284–289. doi: 10.12932/AP0668. [DOI] [PubMed] [Google Scholar]
- 45.Huls A, Schikowski T. Ambient particulate matter and COPD in China: a challenge for respiratory health research. Thorax. 2017;72(9):771–772. doi: 10.1136/thoraxjnl-2016-209687. [DOI] [PubMed] [Google Scholar]
- 46.Wong CM, Vichit-Vadakan N, Vajanapoom N, et al. Part 5. Public health and air pollution in Asia (PAPA): a combined analysis of four studies of air pollution and mortality. Res Rep Health Eff Inst. 2010;(154):377–418. [PubMed] [Google Scholar]
- 47.Kutlar Joss M, Eeftens M, Gintowt E, Kappeler R, Kunzli N. Time to harmonize national ambient air quality standards. Int J Public Health. 2017;62(4):453–462. doi: 10.1007/s00038-017-0952-y. [DOI] [PMC free article] [PubMed] [Google Scholar]