Abstract
Purpose of the Study:
To examine whether Veteran status influences (a) women’s survival to age 80 years without disease and disability and (b) indicators of successful, effective, and optimal aging at ages 80 years and older.
Design and Methods:
The Women’s Health Initiative (WHI) enrolled 161,808 postmenopausal women aged 50–79 years from 1993 to 1998. We compared successful aging indicators collected in 2011–2012 via mailed questionnaire among 33,565 women (921 Veterans) who reached the age of 80 years and older, according to Veteran status. A second analysis focused on women with intact mobility at baseline who could have reached age 80 years by December 2013. Multinominal logistic models examined Veteran status in relation to survival to age 80 years without major disease or mobility disability versus having prevalent or incident disease, having mobility disability, or dying prior to age 80 years.
Results:
Women Veterans aged 80 years and older reported significantly lower perceived health, physical function, life satisfaction, social support, quality of life, and purpose in life scale scores compared with non-Veterans. The largest difference was in physical function scores (53.0 for Veterans vs 59.5 for non-Veterans; p < .001). Women Veterans were significantly more likely to die prior to age 80 years than non-Veteran WHI participants (multivariate adjusted odds ratio = 1.20; 95% confidence interval, 1.04–1.38). In both Veteran and non-Veteran women, healthy survival was associated with not smoking, higher physical activity, healthy body weight, and fewer depressive symptoms.
Implications:
Intervening upon smoking, low physical activity, obesity, and depressive symptoms has potential to improve chances for healthy survival in older women including Veterans.
Keywords: Healthy aging, disability, Quality of life, Women Veterans
Women aged 80 years and older are emerging as a large and critically important demographic group. The U.S. Census estimated that 6.6 million women were aged 80 years and older in 2012, which accounts for 4% of the total female population and 2% of the entire U.S. population ( Ortman, Velkoff, & Hogan, 2014 ). By 2026, the baby boomers will enter their 9th decade as octogenarians; women aged 80 years and older are projected to comprise nearly 12% of the total female population and 6% of the entire population ( Colby & Ortman, 2014 ). Preparing to support the health care and well-being of this growing population is clearly a public health priority.
The growth of women Veterans in these age groups is also on the rise, commensurate with greater opportunities for expanded roles and advancement for women in the military ( Washington, Bean-Mayberry, Hamilton, Cordasco, & Yano, 2013 ). According to the National Center for Veterans Analysis and Statistics veteran population projection model, 2.0 million U.S. women had a history of military service, more than 16% of whom were older than 65 years (National Center for Veterans Analysis and Statistics, 2014). Yet few studies on the health characteristics of older women Veterans, particularly those from World War II and the Korean and Vietnam wars, have been reported ( Bean-Mayberry et al., 2011 ). With a few notable exceptions, most published data focus on women Veterans younger than 65 years ( Washington et al., in press ; Kang et al., 2014 ). Population-based studies of women Veterans that have included older subgroups found that World War II and Korea era women Veterans (with mean ages of 87 and 77 years, respectively) had double the prevalence of fair or poor overall health status compared with Vietnam era women Veterans (whose mean age was 64 years), suggesting significant threats to women Veterans’ healthy aging ( Bean-Mayberry et al., 2011 ; Washington, Bean-Mayberry et al., 2013 ). However, World War II Veterans had a significantly better mental health profile than younger military era cohorts. Currently, active duty forces are 15% women and, with the most recent conflicts in Afghanistan and Iraq being the longest sustained U.S. military operation since the Vietnam War, returning women Veterans are more likely than men to experience depression, musculoskeletal disorders, and adjustment disorders ( Haskell et al., 2011 ). Understanding the predictors of healthy aging among the growing population of women Veterans is critical to preparing family, professional, and health care systems with which these women interact and support.
We have been unable to identify studies that explicitly evaluated whether prior military service affects various indicators of aging well including survival to at least age 80 years, development of incident disease, mobility disability, psychosocial measures of resilience and mastery, or quality of life in older women. The Women’s Health Initiative (WHI) Program enrolled 161,808 postmenopausal women including more than 3,000 with past military service. Since the baseline in 1993–1998, the program has amassed an unprecedented database on health status, incident disease events, health behaviors, and social psychological factors in women who have been under study for 15–20 years.
The overall purpose of this article is to examine whether Veteran status influences an array of healthy aging metrics, including the probability of living to age 80 years without disease and disability and several psychosocial parameters of aging well. Specifically, our study objectives were to (a) compare measures of successful, effective, and optimal aging among women Veterans and non-Veterans at least 80 years of age in the WHI cohort and (b) determine whether the probability and determinants of living to age 80 years without disease and disability differs for Veteran women compared with non-Veteran women.
Conceptual Framework
This analysis is based on an adaptation of the Biopsychosocial Model of Health and Aging ( Seeman and Crimmins, 2001 ) that incorporates the allostatic load concept influencing resilience in aging ( McEwen, 2003 ). This model posits that both the physical and sociocultural environments in which people live and work, along with their personal characteristics, social relationships, and socioeconomic status, influence lifecourse trajectories of health and contribute to consistently observed gradients in health and mortality for variables such as education, socioeconomic status, and social networks. The pathways linking these factors to health-related outcomes include influences on psychological characteristics (e.g., sense of efficacy and mastery) and behavioral habits (e.g., smoking, physical activity, diet) that in turn influence allostatic load (“the cost of adaptation”) through stress-related pathways and physiologic reserve in a variety of biological pathways (e.g., immunity, metabolism, cardiovascular, etc.). Our adapted model also includes the space associated with service in the military that includes possible exposures related to working in or near combat theatres and stresses of military service some of which are unique to women or experienced differently by women (e.g, sexual trauma, casualties, injuries, chemicals, infections, etc.).
Metrics of aging well used in this manuscript were based on three conceptualizations of well aging from the literature: successful aging, effective aging, and optimal aging (Woods et al., JGMS Supplement, under review). Successful aging includes dimensions of longevity, avoidance of disabling morbidity, remaining mobile, and maintaining the ability to live independently ( Depp, Vahia, & Jeste, 2010 ). Effective aging encompasses the adaptation that occurs in response to the development of disease, pain, and/or other common phenomenon in older adults ( Curb et al., 1990 ). Optimal aging refers to the psychological dimensions of well-being irrespective of physical health state ( Ryff, 1982 , 2013 ; Ryff & Keyes 1995 ) including perceptions of happiness, enjoyment of life, and life satisfaction. This conceptual framework is depicted and further discussed in the editorial in this supplement.
Methods
Study Population and Design
The WHI Program is the largest and most diverse cohort of older women in the United States. Women were recruited from 40 clinical centers throughout the United States. From 1993 to 1998, 161,808 postmenopausal women between 50 and 79 years of age were enrolled ( Hays et al., 2003 ). In 2005, participants were invited to enroll in the WHI Extension I Study for five more years of health data collection. A second study extension began in 2010 and continues through 2015 and comprises 93,462 women, 53% of whom are younger than 80 years and 47% of whom are aged 80 and older. Twelve percent of surviving and currently enrolled women are minorities, including American Indians, Asian and Pacific Islanders, African Americans, and Hispanics.
All participants provided informed consent at baseline and for the extension periods. The study protocol and procedures were reviewed and approved by institutional review boards at each clinical center at baseline and for the first extension. The Fred Hutchinson Cancer Research Center became the Institutional Review Board for all participants at the second extension through the present.
Measures
Veteran status
Military service was determined from the baseline assessment. Women were classified as Veterans if they reported serving in the U.S. armed forces on active duty for at least 180 days.
Aging well indicators
In the WHI, successful aging measures included perception of one’s health, living independently (vs in a nursing home), Rand-36 physical function ( Ware & Sherbourne, 1992 ), and absence of disease and disability ( Rillamas-Sun et al., 2014 ). Effective aging indicators are captured in the WHI through metrics of self-control, self-mastery, and environmental mastery from the Perceived Stress Scale ( Cohen, Kamarck, & Mermelstein, 1983 ) and of resilience from the Brief Resilience Scale ( Smith et al., 2008 ). In the WHI, optimal aging was measured using self-ratings of one’s happiness, life enjoyment ( Burnam, Wells, Leake, & Landsverk, 1988 ), and quality of life ( Hadorn & Hays, 1991 ), and scores from the Emotional Well-Being Scale ( Ware & Sherbourne, 1992 ), Satisfaction with Life Scale ( Pavot, Diener, Colin, & Sandvik, 1991 ), MOS Social Support Scale ( Sherbourne & Stewart, 1991 ), and the Purpose in Life and Personal Growth Subscales ( Ryff & Keyes, 1995 ). Except for the absence of disease and disability, which was a created variable (described in Absence of Disease and Disability), these aging well metrics were collected between 2011 and 2012 using a questionnaire administered to participants enrolled in the second WHI Extension Study.
Absence of disease and disability
Methods used to classify the absence of disease and disability were defined in a previous report from WHI ( Rillamas-Sun et al., 2014 ). Briefly, using a birthdate cutoff, a cohort of women who could reach age 80 years by December 2, 2013 were identified and classified into the following mutually exclusive categories: (a) lived to age 80 years without major disease or mobility disability; (b) lived to age 80 years and had disease at baseline but no incident disease or mobility disability during the WHI study follow-up; (c) lived to age 80 years and developed disease but not mobility disability during the WHI study follow-up; (d) lived to age 80 years and developed a mobility disability; and (e) did not live to age 80 years. The major diseases we assessed were coronary disease, stroke, cancer (excluding non-melanoma skin cancer), hip fracture, and type-2 diabetes. Prevalent disease at baseline was ascertained using self-reports of physician diagnoses for each condition. Surveillance of incident disease occurred during study follow-up (including throughout the WHI extension studies) through adjudication of medical records or self-reported physician diagnosis. Mobility disability was characterized as requiring the use of a walking aid (i.e., crutches, walker, or wheelchair) to walk on an even surface and/or limited ability to walk one block or one flight of stairs ( Hays, Serbourne, & Mazel, 1993 ). Deaths were confirmed through adjudication of hospital, autopsy, or death certificate records, and the National Death Index was checked regularly for all participants, including those lost to follow-up.
Covariates
All covariate data for this article were taken from the baseline assessment. Demographic characteristics included age, race/ethnicity, highest education level, annual family income, and marital status. Health behaviors and health status included smoking status, alcohol intake, having depression, physical activity, use of hormone therapy (HT), weight, waist circumference, and body mass index (BMI). Race/ethnicity was self-selected from the following categories: White, African American, Hispanic, Asian or Pacific Islander, American Indian or Alaskan Native, or other. Depression was determined based on a score of at least .06 using the Center for Epidemiologic Studies Depression Scale short form ( Burnam et al., 1988 ). Total recreational physical activity was quantified as metabolic equivalent hours per week (MET-hours/week), computed from data about self-reported duration and frequency of exercise ( Ainsworth et al., 1993 ). Clinic-based measurements of weight and height at baseline were used to calculate BMI using the formula: weight (in kilograms) divided by height (in meters) squared. Standard World Health Organization cutpoints for BMI were used to categorize women as underweight, normal weight, overweight, or obese ( National Institutes of Health [NIH], 1998 ; World Health Organization [WHO], 1998).
Statistical Analysis
All analyses excluded women with missing Veteran status information. Two separate subcohorts were then constructed to examine (a) aging well in Veteran and non-Veteran women who had reached age 80 years or older by 2011–2012 and (b) prospective survival to age 80 years and older for non-Veterans without major disease or mobility disability ( Figure 1 ).
Figure 1.
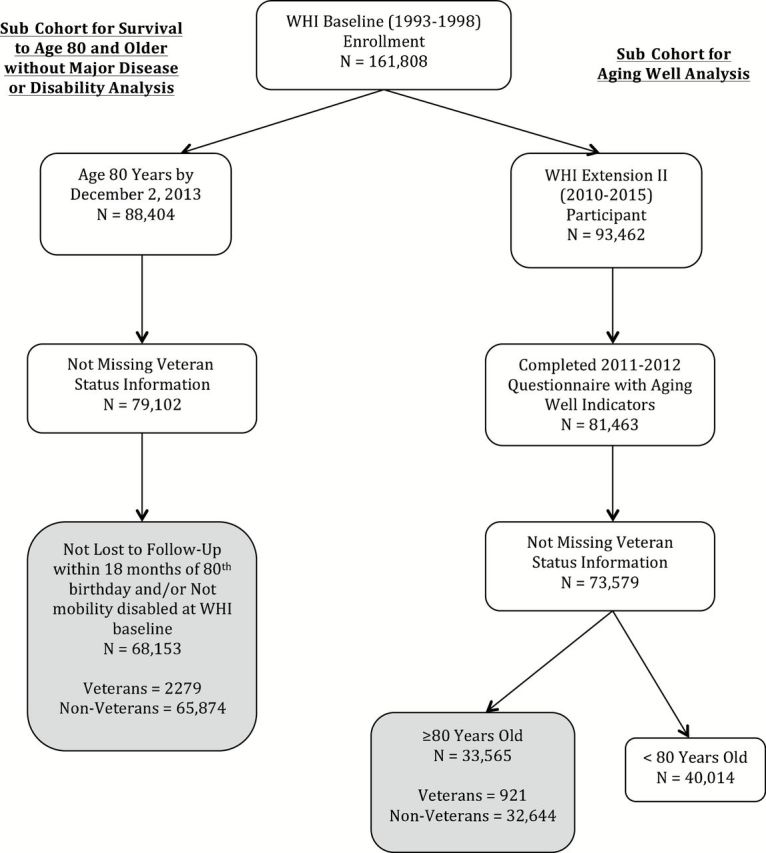
Distribution of survival to age 80 years and older and aging well sub cohorts.
Analysis of aging well in 2011–2012
Aging well indicators were collected in 2011–2012 during the WHI second extension via mailed questionnaire. Among the 81,463 women who completed the questionnaire, 73,579 had Veteran status information ( Figure 1 ). To provide context, we first analyzed all women comparing those aged 80 years and older ( n = 33,565) with those younger than 80 years ( n = 40,014). Then, among women older than 80 years, we compared Veterans ( n = 921) with non-Veterans ( n = 32,644) ( Figure 1 ). For both group comparisons, frequency distributions for categorical indicators and mean scores and standard deviations ( SD ) for continuous indicators were calculated. The Chi-square test for categorical measures and Student’s t test for continuous metrics were used to identify statistically significant group differences defined at α = .05.
Survival to age 80 years and older without major disease or disability
To determine the probability of living to age 80 years without disease and disability, we first identified the sample of women who could have reached their 80th birthday by December 2, 2013, the most recent date that WHI outcomes were available. Of the 88,404 women identified, 9,302 were missing Veteran status information ( Figure 1 ). We then grouped women into the five mutually exclusive outcomes (described earlier) and excluded women who had no study follow-up within 18 months of their 80th birth year ( n = 8,499) or who had mobility disability at baseline ( n = 2,450). A final sample of 68,153 women (2,279 Veterans) remained for this part of the analysis.
To compare across the five survival outcomes, percent distributions or mean ( SD ) values by Veteran status, demographic characteristics, and health behavior and status were estimated. Using women who lived to age 80 years without disease and disability as the reference group, multinomial logistic regression was used to estimate the odd ratios (ORs) and 95% confidence intervals (CIs) of being in one of the other four groups by Veteran status. The crude model adjusted only for age at baseline, whereas the adjusted model also included race/ethnicity, WHI program component (i.e., clinical trial or observational study participant), education, marital status, income, hormone use, smoking status, alcohol use, physical activity, BMI, and depression. Finally, logistic regression was used to assess whether these 11 baseline characteristics predicted the probability of living to age 80 years without disease and disability differently among Veterans compared with non-Veterans using crossproduct terms to evaluate interaction by Veteran status. Statistical significance was defined at α = .05. All analyses were completed using SAS v9.3 (SAS Institute, Cary, NC).
Results
Differences Between Veteran and Non-Veteran Women at Baseline
Among the 68,153 women who could have reached their 80th birthday by December 2013 and who had intact mobility at baseline, women Veterans were older on average than non-Veteran women (71.5 vs 68.8 years), more likely to be Caucasian, and to be college graduates, but less likely to be ever married or to be living with spouse or partner at baseline ( Table 1 ). Women Veterans were significantly more likely to be current or past smokers, to consume alcohol, and reported higher mean physical activity levels. Although mean BMI was similar by Veteran status, women Veterans were less likely to be overweight or obese compared with non-Veteran women. They were also slightly less likely to be classified as depressed compared with their non-Veteran peers ( Table 1 ).
Table 1.
Baseline Characteristics for Survival to Age 80 Years and Older by Veteran Status, n = 68,153
| Characteristic | Veteran | Non-Veteran | p Value |
|---|---|---|---|
| N (%) of women | 2,279 (3.3) | 65,874 (96.7) | |
| Age, years, mean ( SD ) | 71.5 (4.3) | 68.8 (4.3) | <.0001 |
| Race/ethnicity, n (%) | <.0001 | ||
| White | 2,093 (92.3) | 57,296 (87.2) | |
| Black or African American | 92 (4.1) | 4,398 (6.7) | |
| Hispanic/Latina | 32 (1.4) | 1,456 (2.2) | |
| Asian or Pacific Islander | 17 (0.8) | 1,577 (2.4) | |
| American Indian or Alaskan Native | 8 (0.4) | 233 (0.4) | |
| Other | 25 (1.1) | 732 (1.1) | |
| Education, n (%) | <.0001 | ||
| High school or less | 240 (10.6) | 15,967 (24.4) | |
| Some college | 930 (41.0) | 24,990 (38.1) | |
| College graduate | 1,099 (48.4) | 24,566 (37.5) | |
| Family income, n (%) | .1 | ||
| <$50,000 | 1,553 (72.2) | 43,204 (70.6) | |
| $50,000 or more | 597 (27.8) | 17,995 (29.4) | |
| Marital status, n (%) | <.0001 | ||
| Married/living as married | 1,046 (46.0) | 38,221 (58.2) | |
| Divorced/separated | 356 (15.7) | 8,348 (12.7) | |
| Widowed | 649 (28.6) | 16,593 (25.3) | |
| Never married | 222 (9.8) | 2,509 (3.8) | |
| Hormone therapy use, n (%) | 983 (43.7) | 29,534 (45.1) | .19 |
| Smoking behavior, n (%) | <.0001 | ||
| Never smoked | 1,023 (45.9) | 33,923 (52.3) | |
| Past smoker | 1,073 (48.1) | 27,584 (42.5) | |
| Current smoker | 135 (6.1) | 3,406 (5.3) | |
| Alcohol intake, n (%) | <.0001 | ||
| Non drinker | 142 (6.3) | 7,622 (11.7) | |
| Past drinker | 461 (20.4) | 12,247 (18.7) | |
| <1 drink/week | 723 (32.0) | 20,762 (31.8) | |
| ≥1 drink/week | 931 (41.3) | 24,741 (37.9) | |
| Physical Activity, MET-hours per week, mean ( SD ) | 13.6 (13.7) | 12.8 (13.5) | .003 |
| Depression, n (%) | 154 (6.9) | 5,568 (8.7) | .003 |
| Weight, kg, mean ( SD ) | 71.2 (15.4) | 71.7 (15.8) | .09 |
| BMI, kg/m 2 , mean ( SD ) | 27.3 (5.4) | 27.6 (5.6) | .008 |
| BMI category, n (%) | .02 | ||
| Underweight | 29 (1.3) | 633 (1.0) | |
| Normal | 826 (36.6) | 23,049 (35.3) | |
| Overweight | 841 (37.3) | 23,631 (36.2) | |
| Obese | 560 (24.8) | 17,977 (27.5) | |
| Waist circumference, cm, mean ( SD ) | 86.4 (13.2) | 86.3 (13.2) | .74 |
Note: BMI = body mass index; MET = metabolic equivalent.
Comparisons of Women Aged 80 and Older With Younger Women
Metrics of aging well related to successful, effective, and optimal aging were all significantly different among the women at least age 80 years compared with the women younger than age 80 years ( Table 2 ). Large differences were seen in the percentages residing in homes with special services for older people (21.8% vs 8.6%) and in average Rand-36 physical function scores (59.3 vs 75.5) in older compared with younger women, respectively. Modest but significant differences were seen by age group in the percent reporting at least good self-mastery, environmental mastery, and self-control. Although scores were lower than those among the younger women, the majority of older women continued to report being happy and enjoying life most of the time, as well as having a high quality of life.
Table 2.
Aging Well Indicator Scores Among Women by Age Group and Veteran Status
| Aging well constructs and indicators | Theoretical ranges | WHI Extension Study II Cohort a | Subcohort aged ≥80 years | ||||
|---|---|---|---|---|---|---|---|
| N = 73,579 | N = 33,565 | ||||||
| Women aged <80 years ( N = 40,014) | Women aged ≥80 years ( N = 33,565) | p Value | Veteran ( N = 921) | Non-Veteran | p Value | ||
| 1. Successful aging | |||||||
| % responding at least “Good” Perceived Health | NA | 93.4 | 87.2 | <.001 | 84.7 | 87.3 | .02 |
| % residing in place with special services or in nursing home | NA | 8.6 | 21.8 | <.001 | 31.7 | 21.5 | <.001 |
| Mean ( SD ) Physical Functioning Score | 0–100 | 75.5 (23.6) | 59.3 (27.1) | <.001 | 53.0 (28.4) | 59.5 (27.1) | <.001 |
| 2. Effective aging | |||||||
| Mean ( SD ) Adapted Brief Resilience Scale Score | 1–5 | 4.08 (0.81) | 3.97 (0.82) | <.001 | 4.01 (0.84) | 3.97 (0.82) | .25 |
| % with “good” Self-Mastery | NA | 68.2 | 59.0 | <.001 | 58.4 | 59.1 | .72 |
| % with “good” Environmental Mastery | NA | 62.2 | 55.1 | <.001 | 53.9 | 55.1 | .46 |
| % with “good” Self-Control | NA | 77.3 | 74.5 | <.001 | 73.8 | 74.5 | .63 |
| 3. Optimal aging | |||||||
| Mean ( SD ) Emotional Well-Being Score | 1–100 | 80.4 (14.3) | 79.5 (14.2) | <.001 | 79.2 (14.2) | 79.5 (14.2) | .53 |
| % who have Been Happy at least most of the time | NA | 70.1 | 65.6 | <.001 | 63.4 | 65.7 | .15 |
| % who Enjoyed Life at least most of the time | NA | 75.8 | 69.9 | <.001 | 69.8 | 69.9 | .94 |
| Mean ( SD ) Satisfaction with Life Scale Score | 5–35 | 26.8 (6.2) | 26.3 (6.0) | <.001 | 25.7 (6.3) | 26.3 (6.0) | .004 |
| % Extremely Satisfied with Life | NA | 27.1 | 22.8 | <.001 | 21.9 | 22.8 | .52 |
| Mean ( SD ) MOS Social Support Scale | 9–45 | 38.5 (7.3) | 36.8 (7.9) | <.001 | 35.6 (8.6) | 36.8 (7.9) | <.001 |
| Mean ( SD ) Quality of Life Rating | 0–10 | 8.06 (1.53) | 7.54 (1.70) | <.001 | 7.30 (1.88) | 7.55 (1.69) | <.001 |
| % reporting high Quality of Life | NA | 73.4 | 60.3 | <.001 | 54.7 | 60.4 | <.001 |
| Mean ( SD ) Personal Growth Score | 0–28 | 22.0 (4.9) | 20.2 (4.9) | <.001 | 20.1 (5.0) | 20.2 (4.9) | .42 |
| Mean ( SD ) Purpose in Life Score | 0–28 | 20.7 (4.7) | 18.7 (4.7) | <.001 | 18.3 (4.7) | 18.7 (4.7) | .02 |
Notes: NA = not applicable; WHI = Women’s Health Initiative.
a From WHI Extension 2 who completed Form 155 and had non-missing Veteran status.
Aging Well Indicators by Veteran Status
Veterans and non-Veterans differed on several of the successful aging parameters. Among the women aged 80 years and older, those who were Veterans were significantly but modestly less likely to report at least good perceived health compared with non-Veterans (85% vs 87%; p = .02; Table 2 ). Almost one third of women Veterans (32%) were living in a residential environment that provided services for older people compared with only 22% of non-Veteran women. Rand-36 physical function scores averaged 53 in Veteran women compared with 60 in non-Veteran women ( p < .001). Women Veterans compared with non-Veterans did not differ on the health metrics related to effective aging (resilience, self and environmental mastery, self-control) nor did they differ in average levels of several optimal aging indicators including emotional well-being, happiness, enjoyment of life, or personal growth scores. Women Veterans had significantly lower scores on the satisfaction with life, social support, quality of life, and purpose in life scales.
Survival to Age 80 Years Without Disease and Disability by Veteran Status
Overall, 31% of women survived to age 80 years without major disease or mobility disability, 18% lived to age 80 years with baseline disease but no incident disease or mobility disability, whereas 23% developed incident disease, 12% developed mobility disability with or without incident disease, and 16% did not survive to age 80 years. Unadjusted percentages of these endpoints were similar among women Veterans and non-Veterans ( Table 3 ). The probability of death prior to age 80 years was significantly higher among Veteran women compared with non-Veterans after adjustment for age alone (OR = 1.17; 95% CI: 1.03–1.33) and in the full multivariate analysis (OR = 1.20; 95% CI: 1.04–1.38; Table 4 ). ORs were close to null and nonsignificant for all other survival outcomes.
Table 3.
Survival Outcomes for Veteran Women Relative to Non-Veteran Women.
| Veteran | Non-Veteran | Odds ratios (95% confidence intervals) | ||
|---|---|---|---|---|
| Survival outcome | N (%) | N (%) | Crude a | Adjusted b |
| 1. Lived to age 80 years with no disease and with no mobility disability | 744 (32.7) | 20,316 (30.8) | Ref | Ref |
| 2. Lived to age 80 years with baseline disease but no incident disease or mobility disability | 515 (22.6) | 11,630 (17.7) | 1.07 (0.95–1.20) | 1.10 (0.97–1.25) |
| 3. Lived to age 80 years with incident disease but no mobility disability | 452 (19.8) | 15,199 (23.1) | 0.97 (0.86–1.09) | 0.98 (0.86–1.12) |
| 4. Lived to age 80 years with mobility disability, with or without disease | 208 (9.1) | 8,062 (12.2) | 1.03 (0.88–1.21) | 1.01 (0.84–1.21) |
| 5. Did not live to age 80 years | 360 (15.8) | 10,667 (16.2) | 1.17 (1.03–1.33) | 1.20 (1.04–1.38) |
Notes: a Adjusted for baseline age only.
b Adjusted for race/ethnicity, study membership (observational study vs clinical trial), and baseline age, education, marital status, family income, hormone therapy use, smoking status, alcohol use, physical activity, body mass index, and depression.
Table 4.
Baseline Predictors of Living to Age 80 Years with No Disease and No Mobility Disability by Veteran Status
| Veterans | Non-Veterans | |||||
|---|---|---|---|---|---|---|
| N (%) Veterans | Crude OR (95% CI) | Adjusted OR (95% CI) a | N (%) Non-Veterans | Crude OR (95% CI) | Adjusted OR (95% CI) a | |
| Age b | ||||||
| Older than 68 years | 1,697 (74.5) | 1.48 (1.20–1.83) | 1.40 (1.12–1.76) | 31,916 (48.5) | 1.39 (1.35–1.44) | 1.39 (1.34–1.44) |
| 68 Years or younger | 582 (25.5) | Ref | Ref | 33,958 (51.6) | Ref | Ref |
| Race/ethnicity | ||||||
| Not White | 175 (7.7) | 0.76 (0.54–1.08) | 1.00 (0.69–1.45) | 8,396 (12.8) | 0.71 (0.67–0.74) | 0.87 (0.82–0.93) |
| White | 2,093 (92.3) | Ref | Ref | 57,296 (87.2) | Ref | Ref |
| Education | ||||||
| <College graduate | 1,170 (51.6) | 0.98 (0.82–1.16)* | 1.10 (0.91–1.32)* | 40,957 (62.5) | 0.78 (0.76–0.81)* | 0.91 (0.87–0.94)* |
| College graduate | 1,099 (48.4) | Ref | Ref | 24,566 (37.5) | Ref | Ref |
| Family income | ||||||
| <$50,000 | 1,553 (72.2) | 0.89 (0.73–1.08) | 1.02 (0.83–1.26) | 43,204 (70.6) | 0.75 (0.72–0.78) | 0.90 (0.86–0.94) |
| $50,000 or more | 597 (27.8) | Ref | Ref | 17,995 (29.4) | Ref | Ref |
| Marital status | ||||||
| Widowed, divorced/ | 1,227 (54.0) | 0.82 (0.69–0.98) | 0.86 (0.71–1.03) | 27,450 (41.8) | 0.85 (0.82–0.88) | 0.92 (0.89–0.96) |
| separated, never married | ||||||
| Married/living as married | 1,046 (46.0) | Ref | Ref | 38,221 (58.2) | Ref | Ref |
| Hormone therapy use | ||||||
| Yes | 983 (43.7) | 1.18 (0.99–1.41) | 1.15 (0.95–1.38) | 29,534 (45.1) | 1.15 (1.11–1.19) | 1.08 (1.04–1.12) |
| No | 1,265 (56.3) | Ref | Ref | 35,908 (54.9) | Ref | Ref |
| Smoking behavior | ||||||
| Current smoker | 135 (6.1) | 0.35 (0.22–0.57) | 0.31 (0.19–0.52) | 3,406 (5.3) | 0.49 (0.45–0.54) | 0.50 (0.46–0.55) |
| Past smoker | 1,073 (48.1) | 0.85 (0.71–1.02) | 0.80 (0.66–0.97) | 27,584 (42.5) | 0.83 (0.80–0.86) | 0.77 (0.74–0.80) |
| Never smoked | 1,023 (45.9) | Ref | Ref | 33,923 (52.3) | Ref | Ref |
| Alcohol intake | ||||||
| Non drinker | 603 (26.7) | 0.59 (0.48–0.73) | 0.64 (0.51–0.81) | 19,869 (30.4) | 0.67 (0.64–0.69) | 0.71 (0.68–0.74) |
| Drinker | 1,654 (73.3) | Ref | Ref | 45,503 (69.6) | Ref | Ref |
| Physical activity b | ||||||
| ≤9 MET-hours/week | 1,070 (47.0) | 0.72 (0.60–0.86) | 0.85 (0.70–1.03) | 33,346 (50.6) | 0.69 (0.67–0.71) | 0.82 (0.79–0.85) |
| >9 MET-hours/week | 1,209 (53.1) | Ref | Ref | 32,528 (49.4) | Ref | Ref |
| Has depression | ||||||
| Yes | 154 (6.9) | 0.57 (0.38–0.84) | 0.68 (0.45–1.03) | 5,568 (8.7) | 0.57 (0.54–0.61) | 0.65 (0.61–0.70) |
| No | 2,080 (93.1) | Ref | Ref | 58,569 (91.3) | Ref | Ref |
| BMI category | ||||||
| Underweight | 29 (1.3) | 0.78 (0.35–1.72) | 0.89 (0.39–2.04) | 633 (1.0) | 0.73 (0.62–0.87) | 0.77 (0.64–0.93) |
| Normal | 826 (36.6) | Ref | Ref | 23,049 (35.3) | Ref | Ref |
| Overweight | 841 (37.3) | 0.96 (0.79–1.17) | 1.01 (0.82–1.25) | 23,631 (36.2) | 0.83 (0.79–0.86) | 0.86 (0.83–0.90) |
| Obese | 560 (24.8) | 0.48 (0.38–0.61) | 0.53 (0.41–0.68) | 17,977 (27.5) | 0.45 (0.43–0.47) | 0.52 (0.49–0.54) |
Notes: BMI = body mass index; CI = confidence interval; MET = metabolic equivalent; OR = odds ratio.
a Adjusted for all other predictors listed.
b Cutoff at median value of full sample.
* p ≤ .05 for effect modification.
Baseline Predictors of Survival to Age 80 Years in Veteran and non-Veteran Women
Baseline predictors of survival to age 80 years without disease and mobility disability were very similar in women Veterans and non-Veterans ( Table 4 ). Both groups of women were more likely to reach this milestone if they were older at baseline, married, or using HT and less likely to achieve this milestone if they were nondrinkers, were smokers, had lower physical activity levels, had higher levels of depressive symptoms, or were underweight or obese. CIs for the Veteran women’s estimates were wider due to their smaller size but were similar in magnitude to the larger cohort of non-Veteran women. Of the 11 variables evaluated in the interaction analysis, the only variable that appeared to predict survival to age 80 years without disease or mobility disability differently among women Veterans versus non-Veterans was education. Among women Veterans, less than college education did not appear to predict healthy survival, whereas among non-Veteran women, those without a college degree were significantly less likely to be classified in the healthy survivor group ( p value for interaction <.05; Table 4 ). This interaction remained apparent when testing a three-level education variable (high school, some college, and college graduate) and a continuous years of education variable.
In the analysis of women Veterans alone, data are presented using median cutpoints specific to the Veteran subgroup; this resulted in slightly higher cutpoints for age and physical activity than in the analysis that combined Veteran and non-Veteran women. The age- and fully adjusted models revealed that the same variables noted earlier predicted healthy survival ( Table 5 ). The strongest predictors were baseline age above the median, being a nonsmoker, drinking alcohol in moderation, lower levels of depressive symptoms, and healthy body weight.
Table 5.
Baseline Predictors of Living to Age 80 Years with No Disease and No Mobility Disability for WHI Veterans Only, n = 2,279
| N (%) | Crude OR (95% CI) | Adjusted OR (95% CI) a | |
|---|---|---|---|
| Age b | |||
| Older than 72 years | 1,122 (49.2) | 1.44 (1.21–1.72) | 1.41 (1.16–1.71) |
| 72 Years or younger | 1,157 (50.8) | Ref | Ref |
| Race/ethnicity | |||
| Not White | 175 (7.7) | 0.76 (0.54–1.08) | 1.00 (0.69–1.46) |
| White | 2,093 (92.3) | Ref | Ref |
| Education | |||
| <College graduate | 1,170 (51.6) | 0.98 (0.82–1.16) | 1.07 (0.88–1.30) |
| College graduate | 1,099 (48.4) | Ref | Ref |
| Family income | |||
| <$50,000 | 1,553 (72.2) | 0.89 (0.73–1.08) | 1.04 (0.83–1.31) |
| $50,000 or more | 597 (27.8) | Ref | Ref |
| Marital status | |||
| Widowed, divorced/separated, or never married | 1,227 (54.0) | 0.82 (0.69–0.98) | 0.84 (0.68–1.02) |
| Married/living as married | 1,046 (46.0) | Ref | Ref |
| Hormone therapy use | |||
| Yes | 983 (43.7) | 1.18 (0.99–1.41) | 1.16 (0.96–1.41) |
| No | 1,265 (56.3) | Ref | Ref |
| Smoking behavior | |||
| Current smoker | 135 (6.1) | 0.35 (0.22–0.57) | 0.31 (0.18–0.52) |
| Past smoker | 1,073 (48.1) | 0.85 (0.71–1.02) | 0.79 (0.65–0.95) |
| Never smoked | 1,023 (45.9) | Ref | Ref |
| Alcohol intake | |||
| Non drinker | 603 (26.7) | 0.59 (0.48–0.73) | 0.62 (0.49–0.78) |
| Drinker | 1,654 (73.3) | Ref | Ref |
| Physical activity b | |||
| ≤10.5 MET-hours/week | 1,181 (51.8) | 0.72 (0.61–0.86) | 0.85 (0.70–1.03) |
| >10.5 MET-hours/week | 1,098 (48.2) | Ref | Ref |
| Has depression | |||
| Yes | 154 (6.9) | 0.57 (0.38–0.84) | 0.64 (0.42–0.97) |
| No | 2,080 (93.1) | Ref | Ref |
| BMI category | |||
| Underweight | 29 (1.3) | 0.78 (0.35–1.72) | 0.89 (0.39–2.06) |
| Normal | 826 (36.6) | Ref | Ref |
| Overweight | 841 (37.3) | 0.96 (0.79–1.17) | 0.99 (0.80–1.22) |
| Obese | 560 (24.8) | 0.48 (0.38–0.61) | 0.52 (0.40–0.68) |
Notes: BMI = body mass index; WHI = Women’s Health Initiative.
a Adjusted for all other predictors listed.
b Cutoff at median value of veterans sample.
Discussion
Differences Between Women Veterans and non-Veterans
This study highlights many similarities and several important differences between older Veteran and non-Veteran women that relate to aging well. At baseline, among WHI participants who could have reached their 80th birthday by December 2013, prior military service was associated with older age, higher education, higher levels of physical activity, and alcohol consumption but lower likelihood of ever marrying and currently living with a spouse or partner. After adjustment for age alone and for all of these variables, women Veterans were significantly more likely to die before reaching age 80 years compared with non-Veteran WHI participants, but they were no more likely to develop nonfatal incident diseases or mobility disability. Among WHI participants who were aged 80 and older, women with prior military service had lower physical function scores and were more likely to reside in a place with special services for older people. Women Veterans had significantly but modestly lower satisfaction with life and purpose in life scores. They also had significantly lower quality of life ratings and lower social support scores. These findings suggest that prior military service identifies a subgroup of older women with some special risks that need to be better understood.
Previous Evidence on Disability and Mortality in Women Veterans
In the recently reported National Survey of Women Veterans conducted in 2008–2009 (Der-Martirosian, Cordasco, Washington, 2013 ; Washington, in press), levels of SF12 physical and mental component summary scores in women Veterans older than 65 years were found to be similar to those of population norms for older U.S. women published in 1998 (U.S. Population Norms (SF-36), 1998, http://www.sf-36.org/research/sf98norms.pdf ). That survey also revealed that 52% of older U.S. women Veterans today have a college degree, about 13% use VA health care services, 18% served in a combat/war zone, and 5% reported military sexual trauma. Just more than half of the U.S. women Veterans older than 65 years served in and following the Vietnam war (57%), whereas the other 43% served prior to the Vietnam war. Depression was common, reported by 23% of older women Veterans. These data are useful for putting the present WHI findings in context.
A recent retrospective study of 12,000 U.S. women Veterans including 4,734 Vietnam, 2,062 near-Vietnam, and 5,313 nondeployed U.S. military women found that mortality was 11%–15% lower in the two Veteran cohorts compared with the nondeployed group ( Kang et al., 2014 ). Among the women Vietnam Veterans in that study, 80% were nurses whose mortality risk from pancreatic and brain cancer and motor vehicle accidents was elevated compared with nurses in the general population. Overall, these findings are not consistent with the 20% increased risk of not surviving to age 80 observed in the present study. It is possible that among WHI participants, Veterans and non-Veterans are more comparable than in the previous retrospective cohort study allowing the excess risk of death to be revealed. This finding is consistent with an earlier WHI analysis that found an increased risk of all-cause mortality for women Veterans compared with non-Veterans in the entire WHI cohort ( Weitlauf et al., in press ).
Alternative explanations for why aging women Veterans differ from non-Veterans
Why would a history of military service influence healthy survival, physical function and quality of life in older women? Several explanations are possible. First, women who voluntarily select military service may differ importantly from women who do not. A variety of early life course differences are possible that could influence later life survival and functioning including socioeconomic status, family supports, and personality and behavioral differences. Previous studies have noted that women who make the nontraditional career choice of joining the military may have repercussions that influence their future life and social connectedness ( Cotten, Skinner, & Sullivan, 2000 ; Frayne et al., 2006 ). Amongst Veterans using the VA system in 1999, women in every age group were more likely to be unmarried than men. More than 70% of women Veterans older than 65 years were not married and nearly half lived alone and 15%–19% reported that they had no one to take them to a medical appointment ( Cotten, Skinner, & Sullivan, 2000 ; Frayne et al., 2006 ). These findings are consistent with lower rates of ever marrying, currently living with a spouse or partner, and reported social support among women Veterans in the WHI compared with non-Veterans. Greater self-reliance among the WHI women Veterans may also explain why their levels of resilience and mastery, indicators of “effective aging,” were not affected by their poorer physical function and perceived health status.
Second, women who served in the military may have been exposed to experiences that altered their subsequent life course such as military sexual trauma, environmental exposures associated with their military jobs, or posttraumatic stress disorder ( Der-Martirosian et al., 2013 ; Lehavot, Der-Martirosian, Simpson, Sadler, Washington 2013 ; Washington, Davis, Der-Martirosian, & Yano, 2013 ). The WHI data are unable to shed light on the extent to which these factors influenced the findings reported herein. Third, women with prior military service may access and/or receive different health care than non-Veteran women, and this may occur within or outside of the VA system. To the extent that WHI participants are similar to the older women Veterans who responded to the National Survey of Women Veterans, we would expect 87% of them to receive their health care outside of the VA system.
Influence of Education and Other Factors on Healthy Survival on Women Veterans Versus Non-Veterans
Women Veterans in WHI were apparently not protected by having college degrees as there was no association between educational attainment and healthy survival for them, in contrast to better odds of healthy survival among more highly educated non-Veteran women. This finding may be due to chance because 11 risk factor interactions were tested in this analysis. Alternatively, the lack of social support and greater disability of Veteran women may have negated any salutary effect of higher education on healthy survival. Selection factors associated with less versus more education may also differ for Veteran and non-Veteran women. Only 11% of women Veterans had no college education compared with 24% of non-Veteran women. Thus, college education may better identify women of higher socioeconomic status and greater resources among non-Veteran compared with Veteran women.
A few selected findings in the present study, not specifically related to Veteran status, merit comment. The finding that older age at baseline was associated with improved odds of healthy survival appears paradoxical but is likely explained by the study design employed here. Women with baseline mobility disability were excluded from the analytic study population, thus removing more older than younger women in poor health. Older women then had fewer years of survival prior to reaching age 80 years, so less time to develop new incident diseases, mobility disability or to die. Simply put, the closer the women were to age 80 years without mobility disability, the more likely they were to reach age 80 years or older.
HT use at baseline was associated with better odds of healthy survival and this association did not statistically differ by Veteran status. The WHI Hormone Therapy randomized controlled trials do not show an effect of estrogen treatment with or without progestin on reduced mortality in older WHI HT Trial participants ( Manson et al., 2013 ); in fact, risks of total mortality were increased among older women assigned to estrogen alone ( LaCroix et al., 2011 ). Thus, a causal association between baseline HT and improved odds of healthy survival is unlikely. Rather, baseline hormone use likely identifies women who are healthier, have better access to health care or engage in more preventive health behaviors than women not using HT ( Buist, LaCroix, Newton, Keenan, 1999 ; Gleason, Dowling, Friedman, Wharton, & Asthana, 2012 ).
Influence of Modifiable Risk Factors on Healthy Survival
The translational value of the present study is most evident in the finding that the same modifiable risk factors predicted healthy survival in women Veterans and non-Veterans. Specifically, women were less likely to survive to age 80 years without disease and disability if they were current smokers, less physically active, obese, or suffering from depressive symptoms. These risks are all amenable to change by effective interventions ( Farmer, Rose, Riopelle, Lanto, & Yano, 2011 ). Given that older women Veterans report less social support, interventions that include enhanced social support may be particularly beneficial and worthy of evaluation in this special population ( Lehavot, Der-Martirosian, Simpson, Shipherd, Washington, & 2013 ).
Strengths and Weaknesses
Strengths of this study include the large population of diverse postmenopausal women, the vast amount of data available on personal characteristics, risk factors, incident diseases, disability and indicators of well aging, and the inclusion of nearly 2,300 older women Veterans and more than 68,000 WHI participants overall. Given that most past research on older women Veterans has either been restricted to VA users, or been limited to use of survey data to make comparisons with non-VA users, strengths of the WHI cohort also include the prospective design and use of the same methods for data collection in all participants including adjudication of incident disease events and deaths. This study was limited by lack of information on details of women’s military service including duration of service, service era, combat history or deployment to combat zones, military occupations and exposures, and use of VA health care services over time. We are unable to disaggregate the possible explanations for the observed differences between women Veterans and non-Veterans in the discordant measures of well aging. These findings pertain to women aged 80 and older now, and they may or may not generalize to the prospects for healthy aging among younger women Veterans.
Future Directions for Research and Health Care Services to Support Aging Women Veterans
Understanding the aging issues of women Veterans, whether prior service in the U.S. military affects aging well, and the determinants of healthy aging have been identified as priority areas for research by the Veterans Health Administration Women’s Health leadership ( Yano et al., 2011 ). These findings support that goal by showing that women Veterans differ from non-Veterans on several dimensions of aging well, including survival to age 80 years, maintaining physical function, and perceived health and quality of life. Importantly, modifiable risk factors predicting healthy survival were similar regardless of prior military service. This underscores the importance of providing effective behavior change programs targeting smoking cessation and physical activity and establishing healthy body weights to Veteran and non-Veteran women alike. The findings also support evaluation and treatment of depressive symptoms to improve prospects of healthy survival. Learning more about the aging of younger cohorts of women Veterans from post-Vietnam service eras will also be critically important in the light of these findings. Caring for older women Veterans in the future will be influenced by their growing numbers and their greater likelihood of exposure to combat and its associated long-term physical and mental health challenges.
Funding
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller
Clinical Coordinating Center: Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg
Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
For a list of all the investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
This material is based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development (HSR&D) Service FOP14-439 and the VA Office of Women’s Health. Drs. Reiber and Yano were funded through VA HSR&D Senior Research Career Scientist awards (RCS # 98-353 and RCS #05-195, respectively).
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- Ainsworth B. E. Haskell W. L. Leon A. S. Jacobs D. R. Jr Montoye H. J. Sallis J. F. , & Paffenbarger R. S. Jr . ( 1993. ). Compendium of physical activities: Classification of energy costs of human physical activities . Medicine & Science in Sports & Exercise , 25 , 71 – 80 . [DOI] [PubMed] [Google Scholar]
- Bean-Mayberry B. Yano E. M. Washington D. L. Goldzweig C. Batuman F. Huang C. Miake-Lye I. , & Shekelle P. G . ( 2011. ). Systematic review of Women Veterans’ Health: Update on gaps and successes . Women’s Health Issues , 21 , S84 – S97 . doi:10.1016/j.whi.2011.04.022 [DOI] [PubMed] [Google Scholar]
- Buist D. S LaCroix A. Z. Newton K. M. , & Keenan N. L . ( 1999. ). Are long-term hormone replacement therapy users different from short-term and never users? American Journal of Epidemiology , 149 , 275 – 281 . [DOI] [PubMed] [Google Scholar]
- Burnam M. A., Wells K. B., Leake B., Landsverk J . ( 1988. ). Development of a brief screening instrument for detecting depressive disorders . Medical Care , 26 , 775 – 789 . [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R . ( 1983. ). A global measure of perceived stress . Journal of Health and Social Behavior , 24 , 385 – 396 . [PubMed] [Google Scholar]
- Colby S. L. , & Ortman J. M . ( 2014. ). The Baby Boom Cohort in the United States: 2012 to 2060 . (Current Population Reports, P25–1141). Washington, DC: : U.S. Census Bureau; . [Google Scholar]
- Cotten S. R. Skinner K. M. , & Sullivan L. M . ( 2000. ). Social support among women veterans . Journal of Women and Aging , 12 , 39 – 62 . [DOI] [PubMed] [Google Scholar]
- Curb J. D. Guralnik J. M. LaCroix A. Z. Korper S. P. Deeg D. Miles T. , & White L . ( 1990. ). Effective aging: Meeting the challenge of growing older . Journal of the American Geriatrics Society , 38 , 827 – 828 . [DOI] [PubMed] [Google Scholar]
- Depp C. Vahia I. V. , & Jeste D . ( 2010. ). Successful aging: Focus on cognitive and emotional health . Annual Review of Clinical Psychology , 6 , 527 – 550 . doi:10.1146/annurev.clinpsy.121208.131449 [DOI] [PubMed] [Google Scholar]
- Der-Martirosian C. Cordasco K. M. , & Washington D. L . ( 2013. ). Health-related quality of life and comorbidity among older women veterans in the United States . Quality of Life Research , 22 , 2749 – 2756 . doi:10.1007/s11136-013-0424-7 [DOI] [PubMed] [Google Scholar]
- Farmer M. M. Rose D. E. Riopelle D. Lanto A. B. , & Yano E. M . ( 2011. ). Gender differences in smoking and smoking cessation treatment: An examination of the organizational features related to care . Women’s Health Issues , 21 ( Suppl .), S182 – S189 . doi:10.1016/j.whi.2011.04.018 [DOI] [PubMed] [Google Scholar]
- Frayne S. M. Parker V. A. Christiansen C. L. Loveland S. Seaver M. R. Kazis L. E. , & Skinner K. M . ( 2006. ). Health status among 28,000 women veterans. The VA Women’s Health Program Evaluation Project . Journal of General Internal Medicine , 21 ( Suppl. 3 ), S40 – S46 . doi:10.1111/j.1525-1497.2006.00373.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason C. E. Dowling N. M. Friedman E. Wharton W. , & Asthana S . ( 2012. ). Using predictors of hormone therapy use to model the healthy user bias: How does healthy user status influence cognitive effects of hormone therapy? Menopause , 19 , 524 – 533 . doi:10.1097/gme.0b013e318238ff2c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadorn D. C., Hays R. D . ( 1991. ). Multitrait-multimethod analysis of health-related quality-of-life measures . Medical Care , 29 , 829 – 840 . [DOI] [PubMed] [Google Scholar]
- Haskell S. G. Mattocks K. Goulet J. L. Krebs E. E. Skanderson M. Leslie D. , … Brandt C . ( 2011. ). The burden of illness in the first year home: Do male and female VA users differ in health conditions and healthcare utilization . Womens Health Issues , 21 , 92 – 97 . doi:10.1016/j.whi.2010.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays J. Hunt J. Hubbell A. Anderson G. L. Limacher M. Allen C. , & Rossouw J. E . ( 2003. ). The WHI recruitment methods and results . Annals of Epidemiology , 13 , S18 – S77 . [DOI] [PubMed] [Google Scholar]
- Hays R. D. Serbourne C. D. , & Mazel R. M . ( 1993. ). The RAND 36-Item Health Survey 1.0 . Health Economics , 2 , 217 – 227 . [DOI] [PubMed] [Google Scholar]
- Kang H. K. Cypel Y. Kilbourne A. M. Serpi T. Collins J. F. Frayne S. M. , … Spiro A. 3rd . ( 2014. ). HealthViEWS: Mortality study of female US Vietnam era veterans, 1965–2010 . American Journal of Epidemiology , 179 , 721 – 730 . doi:10.1093/aje/kwt319 [DOI] [PubMed] [Google Scholar]
- LaCroix A. Z. Chlebowski R. T. Manson J. E. Aragaki A. K. Johnson K. C. Martin L. , … Wactawski-Wende J .; WHI Investigators . ( 2011. ). Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy: A randomized controlled trial . Journal of the American Medical Association , 305 , 1305 – 1314 . doi:10.1001/jama.2011.382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K. Der-Martirosian C. Simpson T. L. Sadler A. G. , & Washington D. L . ( 2013. ). Barriers to care for women veterans with posttraumatic stress disorder and depressive symptoms . Psychological Services , 10 , 203 – 212 . doi:10.1037/a0031596 [DOI] [PubMed] [Google Scholar]
- Lehavot K. Der-Martirosian C. Simpson T. L. Shipherd J. C. , & Washington D. L . ( 2013. ). The role of military social support in understanding the relationship between PTSD, physical health, and healthcare utilization in women Veterans . Journal of Traumatic Stress , 26 , 772 – 775 . doi:10.1002/jts.21859 [DOI] [PubMed] [Google Scholar]
- Manson J. E. Chlebowski R. T. Stefanick M. L. Aragaki A. K. Rossouw J. E. Prentice R. L. , … Wallace R. B . ( 2013. ). Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials . Journal of the American Medical Association , 310 , 1353 – 1368 . doi:10.1001/jama.2013.278040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B. S . ( 2003. ). Interacting mediators of allostasis and allostatic load: Towards an understanding of resilience in aging . Metabolism , 52 ( Suppl. 2 ), 10 – 16 . [DOI] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics, Department of Veterans Affairs, Washington, DC . (November 2014. ). National Center for Veterans Analysis and Statistics Table 1L: VetPop2014 Living Veterans by Age Group, Gender, 2013–2043 . Retrieved from http://www1.va.gov/vetdata/Veteran_Population.asp (Accessed February 2, 2015 ).
- National Institutes of Health . ( 1998. ). Clinical Guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report . Obes Res , 6 ( Suppl. 2 ), S51S – S209 . [PubMed] [Google Scholar]
- Ortman J. M. Velkoff V. A. , & Hogan H . ( 2014. ). An aging nation: The older population in the United States . (Current Population Reports, P 25 – 1140 ). Washington, DC: : U.S. Census Bureau; . [Google Scholar]
- Pavot W. Diener E. Colin C. R. , & Sandvik E . ( 1991. ). Further validation of the Satisfaction with Life Scale: Evidence for the cross-method convergence of well-being measures . Journal of Personality Assessment , 57 , 149 – 161 . [DOI] [PubMed] [Google Scholar]
- Rillamas-Sun E. LaCroix A. Z. Waring M. E. Kroenke C. H. LaMonte M. J. Vitolins M. Z. , … Wallace R. B . ( 2014. ). Obesity and late-age survival without major disease or disability in older women . JAMA Internal Medicine , 174 , 98 – 106 . doi:10.1001/jamainternmed.2013.12051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff C. D . ( 2013. ). Eudaimonic well-being and health: Mapping consequences of self-realization . In Waterman S. (Ed.), The best within us: Positive psychology perspectives on eudaimonia (pp. 77 – 98 ). Washington, DC: : American Psychological Association; . [Google Scholar]
- Ryff C. D. , & Keyes C. L. M . ( 1995. ). The structure of psychological well-being revisited . Journal of Personality and Social Psychology , 69 , 719 – 727 . [DOI] [PubMed] [Google Scholar]
- Ryff C. D . ( 1982. ). Successful aging: A developmental approach . Gerontologist , 22 , 209 – 214 . [DOI] [PubMed] [Google Scholar]
- Seeman T. E. , & Crimmins E. ( 2001. ). Social environment effects on health and aging: integrating epidemiologic and demographic approaches and perspectives . Annals of the New York Academy of Sciences , 954 , 88 – 117 . [DOI] [PubMed] [Google Scholar]
- Sherbourne S. D., Stewart A. L . ( 1991. ). The MOS social support survey . Social Science & Medicine , 32 , 705 – 714 . [DOI] [PubMed] [Google Scholar]
- Smith B. W. Dalen J. Wiggins K. Tooley E. Christopher P. , & Bernard J . ( 2008. ). The Brief Resilience Scale: Assessing the ability to bounce back . International Journal of Behavioral Medicine , 15 , 194 – 200 . [DOI] [PubMed] [Google Scholar]
- U.S. Population Norms (SF-36) . ( 1998. ). Retrieved from http://www.sf-36.org/research/sf98norms.pdf
- Ware J. , & Sherbourne C . ( 1992. ). The MOS 36-item short-form healthy survey (SF-36). Conceptual framework and item selection . Medical Care , 30 , 473 – 483 . [PubMed] [Google Scholar]
- Washington D. L Bean-Mayberry B. Hamilton A. B. Cordasco K. M. , & Yano E. M . ( 2013. ). Women Veterans’ healthcare delivery preferences and use by military service era: Findings from the National Survey of Women Veterans . Journal of General Internal Medicine , 28 ( Suppl. 2 ), S571 – S576 . doi:10.1007/s11606-012-2323-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington D. L. Farmer M. M. Mor S. S. Canning M. , & Yano E. M . (in press). Assessment of the health care needs and barriers to VA use experienced by women Veterans: Findings from the National Survey of Women Veterans . Med Care . [DOI] [PubMed] [Google Scholar]
- Washington D. L. Davis T. D. Der-Martirosian C. , & Yano E. M . ( 2013. ). PTSD risk and mental health care engagement in a multi-war era community sample of women Veterans . Journal of General Internal Medicine , 28 , 894 – 900 . doi:10.1007/s11606-012-2303-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitlauf J., LaCroix A., Bird C., et al. (in press). Association of women’s military service and physical health: A prospective analysis of long-term health outcomes and mortality in Veteran and non-Veteran participants in the Women’s Health Initiative . Women’s Health Issues . [Google Scholar]
- Women’s Health Initiative Study Group . ( 1998. ). Design of the Women’s Health Initiative clinical trial and observational study . Controlled Clinical Trials , 19 , 61 – 109 . [DOI] [PubMed] [Google Scholar]
- Woods N. F Rillamas-Sun E. Cochrane B. B. La Croix A. Z. Seeman T. E. Tindle H. A. , … Wallace R. B . (under review). Aging well: Observations from the Women’s Health Initiative Study . Journal of Gerontology: Medical Sciences . [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Report of a WHO consultation on obesity . ( 1998. ). Obesity: Preventing and managing a global epidemic . Geneva: : World Health Organization; . [PubMed] [Google Scholar]
- Yano E. M. Bastian L. A. Bean-Mayberry B. Eisen S. Frayne S. Hayes P. , … Washington D. L . ( 2011. ). Using research to transform care for women veterans: Advancing the research agenda and enhancing research–clinical partnership . Women’s Health Issues , 21 , S73 – S83 . doi:10.1016/j.whi.2011.04.002 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau, Current Population Survey, Annual Social and Economic Supplement . ( 2012. ). “The Older Population in the United States, 2012.” Table 1. Population by Age and Sex: 2012 . Retrieved from http://www.census.gov/population/age/data/2012.html(Accessed November 2014) [Google Scholar]


