The number of women in the military has been increasing steadily over the past 30 years and their roles are expanding. By 2016 women will be eligible to serve in all military positions including previously limited combat roles ( U.S. Government Accountability Office, 2015 ). To join the military, women need to be at least 17 years of age, have no more than two dependents, have successfully completed education and aptitude tests, and meet physical, mental, and moral standards. Military women serve around the globe and with each assignment, deployment, and conflict, they are introduced to opportunities and risks. When individuals complete discharge documents and separate from the military, they transition to Veteran status and are thus eligible to receive VA health care services and other benefits based on their service, disabilities, and financial need.
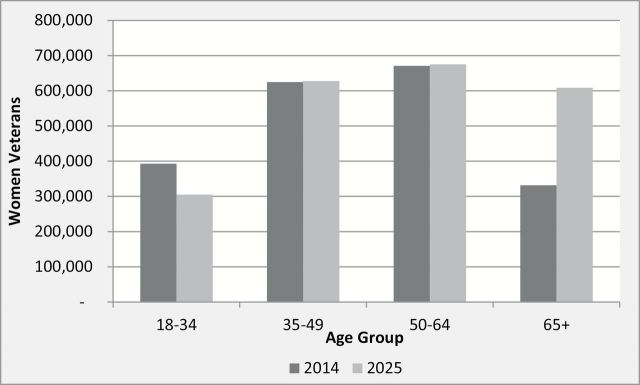
Today, more than 2 million of the almost 22 million U.S. Veterans are women who have earned America’s gratitude and respect for their military contributions. Included are the 400,000 women serving during the World War II era, the 120,000 serving during the Korean conflict and the 265,000 who volunteered to serve during the Vietnam era ( America’s Women Veterans, 2012 ; Women in Military Service, 2015 ). Their early military roles were in nursing, technical, mechanical, communication, clerical, and service positions. The absolute number of women Veterans older than 65 years is expected to grow rapidly in the next 10 years. Figure 1 shows the projected 10% increase in all women Veterans from 2014 to 2025 and the striking 83% increase in women Veterans older than 65 years (from 332,000 women Veterans in 2014 to more than 608,000 in 2025) (U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics, 2014).
Figure 1.
Age distribution of women Veterans in 2014 and 2025
Over the past two decades, Congress tasked the Department of Veterans Affairs (VA) to identify women Veterans’ health-related needs and improve their health care. As a result, the number of unique programs and services available to women Veterans through the VA has increased, driven by a growing body of research focused specifically on women Veterans’ health care needs. Among women Veterans, 32% are enrolled to receive health care in the Veterans Health Administration (VHA), and among those using VA care, the majority are older than 45 years. Despite the growing evidence base, there is still a recognized gap in knowledge regarding women Veterans, aging, and the potential impact of military service on aging processes. ( Yano et al., 2011 ). The articles contained in this supplement describe unique findings that advance our knowledge on older women Veterans in the areas of menopause and reproductive health, chronic disease and comorbidities, healthy aging, and premature mortality.
Women’s Health Initiative
The Women’s Health Initiative (WHI) is one of the largest U.S. prevention studies and the largest, most ethnically, and geographically diverse study of older women in the United States. In 1992, the WHI was funded by the National Institutes of Health (NIH) to address the most common causes of death, disability, and impaired quality of life in postmenopausal women. The WHI Program included a Clinical Trial (CT) component (three overlapping prevention trials testing Hormone Therapy, Dietary Modification and Calcium and Vitamin D supplementation), and a large Observational Study (OS). The WHI CT and OS enrolled women at the same 40 clinical centers located in major population centers across the United States. A single Clinical Coordinating Center (WHI CCC) at the Fred Hutchinson Cancer Research Center managed clinical operations, data collection, and analysis. Key WHI Principal and Co-Investigators from the CCC and clinical sites who were instrumental to the entire research enterprise are listed at the end of this editorial. Study design details are described elsewhere ( Anderson et al., 2003 ; Women’s Health Initiative Study Group, 1998 ). WHI established standardized methods across all study sites to collect the extensive self-reported, clinical, laboratory, and imaging assessments. Specific definitions and diagnostic criteria were provided for primary study endpoints (heart disease, breast cancer, and hip fracture) and for major secondary endpoints (stroke, pulmonary embolism, endometrial cancer, colo-rectal cancer, and death from other causes). All primary and secondary outcomes were adjudicated using hospital records, electrocardiogram readings, laboratory findings, and death certificates.
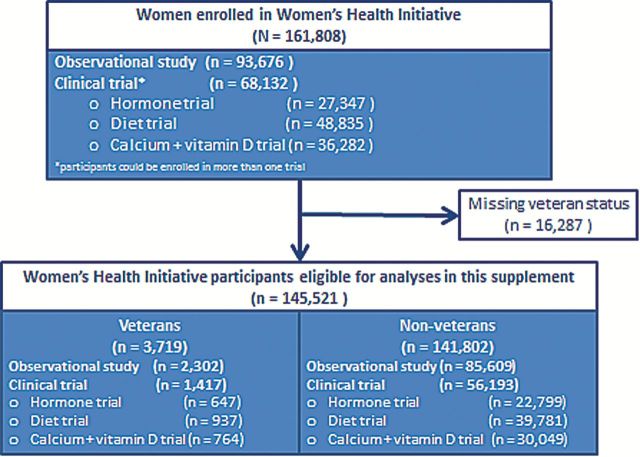
The 5-year recruitment period for the CT/OS began in September 1993 and ended in December, 1998. There were 161,808 postmenopausal women aged 50–79 who enrolled in the WHI. At baseline, 3,719 of these women affirmatively answered the question, “Have you served in the U.S. armed forces on active duty for a period of 180 days or more?” Detailed military service and exposures data were not available. Women with a missing response were excluded from analyses for this supplement. Figure 2 illustrates the WHI participants by Veteran and non-Veteran status.
Figure 2.
Women’s Health Initiative Veteran and non-Veteran participants.
WHI women were followed through 2005 initially and then re-consented for continued follow-up through two extension periods covering 2005–2010 and 2010–2015. More than 90,000 WHI participants are alive and are being followed nationwide. The massive WHI database and biospecimen repository, available to all researchers, now include up to 22 years of follow-up information. Researchers’ use of WHI data on women Veterans allows the ability to characterize and compare older women Veterans in WHI to a control population of older women without military exposures. The initial WHI analysis comparing women Veterans to non-Veterans identified that after adjustment for age and known health risk factors, women Veterans had a significantly elevated risk for all-cause mortality ( Weitlauf et al., 2015 ). This finding compelled the investigation of how and why women Veterans’ health differs from their WHI counterparts without military service. Teams of VA and non-VA researchers from around the country asked and answered important questions using this database to shed light on the similarities and differences between Veterans and non-Veteran WHI participants and to investigate possible explanations to the extent of the available data.
Conceptual Framework
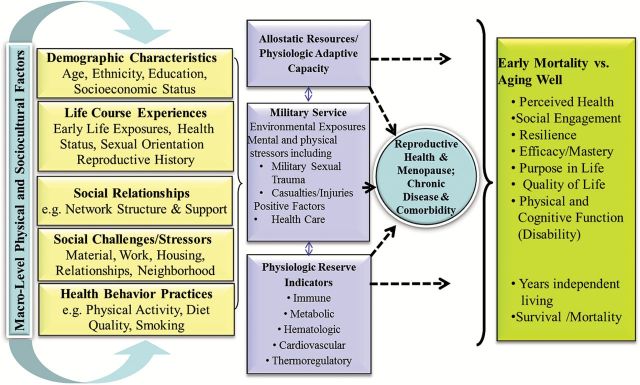
To better understand the impact of military service on aging, we used an adaptation of the Biopsychosocial Model of Health and Aging ( Seeman & Crimmins, 2001 ). This model posits that early life exposures such as socio-demographic factors, adverse childhood experiences, and young adult health and behavior influence the choice of joining the military as well as subsequent health and disease ( Figure 3 ) ( McEwen, 2002 , 2003 ). Women’s early life experiences and health prior to joining the military may interact both positively and negatively with their military experience to influence their health as they age. Military selection criteria for women, women’s expanding military roles and exposures, and the broader influences on health risks and preventive health factors have all changed over time. While military service can expose women to numerous stressors ( Magruder et al., 2015 ), they can also benefit from support, a sense of shared purpose, and health care. Thus, experiences and exposures that are unique to military service are categorized in this model as having either a positive or negative impact on adult health and longevity through a variety of complex mechanisms and pathways. Each article in this supplement “Older Women Veterans in the Women’s Health Initiative” compares findings between women Veterans their non-Veteran reference group in three important areas: reproductive health and menopause, chronic disease and comorbidity, and early mortality/healthy aging.
Figure 3.
Women Veterans aging well life course model (adapted from Seeman & Crimmins, 2001 ).
Reproductive Health and Menopause
Women’s reproductive health and their experience of menopausal symptoms are influenced by genetic, hormonal, and health-related factors such as depression, smoking, and obesity. Changes in ovarian hormone secretion give rise to vasomotor symptoms in many midlife women which may subsequently impact health-related quality of life. Other common and salient menopausal symptoms of great concern for postmenopausal women are insomnia and poor sleep quality. Aberrant sleep patterns are associated with increased cardio-metabolic risk and linked to smoking, obesity, hypertension, diabetes, and mental health conditions ( Rissling et al., 2015 ). Thus, menopausal symptoms may influence or be markers for health later in life and mortality risk.
Peri-menopausal symptoms such as fibroids, abnormal bleeding, and pelvic pain may be reduced or eliminated through hysterectomy (removal of the uterus) and bilateral salpingo oophorectomy (BSO) (removal of the ovaries) ( Cheong, Smotra, & Williams, 2014 ; Marjoribanks, Lethaby, & Farquhar, 2006 ). In more recent years, shifts toward delayed childbearing and development of treatments for these conditions that preserve the uterus and/or ovaries have led to a decrease in rates of hysterectomy and BSO nationally. However, prior evidence suggests that women Veterans are more likely to undergo these procedures than their non-veteran peers ( Gardella, Johnson, Dobie, & Bradley, 2005 ). Removal of the ovaries results in early surgical menopause, which can increase long-term health risks. Understanding the frequency of these procedures among women Veterans can help to identify specific health concerns and needs.
Chronic Disease and Comorbidity
The impact of early life exposures, socioeconomic status, and lifestyle choices on later life risks of chronic disease and comorbidity is well documented ( Seeman & Crimmins, 2001 ). Although the greater prevalence of chronic disease and comorbidity among male veterans relative to their non-veteran peers has been a topic of research for many years, less is known about differences among women. Differences in health behaviors between women Veterans and non-Veterans, such as smoking, physical activity, and diet, may contribute to increased risk for health risks and certain chronic diseases later in life. Furthermore, evidence suggests that, similar to men, women often join the military to escape unfavorable or dysfunctional home lives. Additional stressors accumulated during the course of military service may interact with this history of early life adversity to amplify the negative impact of chronic disease, making women Veterans more prone to developing comorbidities and less able to engage in self-care for management of chronic diseases such as diabetes. Nevertheless, some of the positive aspects of military service, such as access to health care, and high levels of occupational attainment may make individuals more resilient initially in the face of cognitive decline and development of chronic disease. In order to tailor disease prevention programs and screening for women Veterans, it is important to understand the role of military service in the development of chronic disease and illness and the impacts on physical function and quality of life.
Early Mortality versus Healthy Aging
The Biopsychosocial Model of Health and Aging postulates that socio-demographic characteristics interact to influence psychological characteristics and behavioral factors. These relationships are influenced by broader effects of the sociocultural and physical environments across each individual’s life course, and these domains ultimately influence health outcomes, including mortality ( Washington et al., 2015 ). The combined impact of early life exposures and adult health can lead to decreased longevity and influence mortality. Prior studies have documented robust good health and decreased risk of all-cause mortality among women Veterans relative to the general population, but recently published higher mortality rates among WHI women Veterans compared to non-Veterans raise concern ( Weitlauf, 2015 ). Increased mortality may be of particular concern among sexual minority women and those with substance use disorders who may have the highest exposure to stressors early in life and during military service. Notably, some of the stressors experienced by women in the military have changed over time and thus there may be cohort effects of military service on mortality that deserve continued study.
Declining mortality rates during the past century are resulting in a growing number of older people, especially women. Survivors in their 80, 90s, and 100s vary widely in their abilities to live independently and continue to enjoy life. Constructs included in healthy aging are longevity, avoidance of disease and maintaining physical and cognitive function even when diseases cannot be avoided. Psychosocial parameters of aging well include perceived quality of life, capacity for autonomous living, and capacity for social engagement (requiring cognitive function and emotional well-being). Healthy aging is influenced by psychological characteristics such as sense of efficacy and mastery and behavioral habits such as smoking, alcohol intake, and diet ( McEwen, 2003 ). Both psychological characteristics and behavioral habits may differ between those who join the military and those who do not. For example, the spirit of adventure that moved women to join the military may increase their sense of self-efficacy in later life. Their greater independence and self-reliance and their embracing of nontraditional occupational roles may have decreased their likelihood of marriage and childbearing during the life course. In later life, these decisions may result in fewer social supports and greater social isolation. In addition to these selection factors, women’s military service may involve occupational exposures to repetitive physical and psychological stress, to which the body may not be able to respond efficiently. Over the life course, the accumulated impact from the body’s inability to respond to daily life stressors can affect the aging process, resulting in early mortality as noted above or survival with a greater burden of disease and disability. Women Veteran’s health behaviors including physical activity, smoking, alcohol use, and diet, combined with exposure to hazardous environments and other live events, may limit their ability to adapt to repeated stress and negatively impact their likelihood of healthy aging.
In summary, the opportunity to conduct the research in this supplement builds on the strengths and organization of the WHI and the women who volunteered their time to advance research in older women. Senior WHI and VA investigators worked with VA postdoctoral fellows and junior faculty who led 8 of our 13 manuscript teams, a strategy designed to strengthen the cadre of future women Veterans researchers. Our findings indicate that older women Veterans today are a special population with certain risks that are higher than their WHI counterparts. While our data do not allow us to identify all of the causes of the health disparities, the findings clearly indicate areas of focus for research and for improving preventive services and health care for current and future generations of women Veterans. These implications are described in the editorial by Dr. Bastian ( Bastian et al., 2016 ). We thank the involved women Veterans for their service to their country as well as their contributions to WHI. We commit ourselves to protecting and preserving the health of women Veterans by improving our understanding of the long-term health effects of military service now and in future generations of women who serve.
Funding
The WHI program is funded by the National Heart, Lung and Blood Institute, National Institute of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201 100003C, HHSN268201100004C, and HHSN271201100004C.
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller
Clinical Coordinating Center: Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg.
Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker.
Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker.
For a list of all the investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
This work was also supported by the Department of Veterans Affairs Health Services Research and Development VA HSR&D FOP 14–439 and the VA Office of Women’s Health. Dr. Reiber’s effort was supported by a VA HSR&D VA Senior Research Career Scientist Award (Project #RCS 98–353).
Acknowledgments
The views expressed in this editorial are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- America’s Women Veterans . ( 2012. ). U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Retrieved from http://www.va.gov/vetdata/docs/specialreports/final_womens_report_3_2_12_v_7.pdf [Google Scholar]
- Anderson G. L. Manson J. Wallace R. Lund B. Hall D. Davis S. ,… Prentice R. L . ( 2003. ). Implementation of the Women’s Health Initiative study design . Annals of Epidemiology , 13 ( 9 Suppl ), S5 – S17 . [DOI] [PubMed] [Google Scholar]
- Bastian L. Hayes P. Haskell S. G. Atkins D. Reiber G LaCroix A. Z. , & Yano E. M . ( 2016. ) Improving our understanding of health issues in older women Veterans . The Gerontologist , 56 , S10 – S13 . doi:10.1093/geront/gnv672 [DOI] [PubMed] [Google Scholar]
- Cheong Y. C. Smotra G. , & Williams A. C . ( 2014. ). Non-surgical interventions for the management of chronic pelvic pain . The Cochrane Database of Systematic Reviews , 3 , CD008797 . doi: 10.1002/14651858.CD008797.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardella C. Johnson K. M. Dobie D. J. , & Bradley K. A . ( 2005. ). Prevalence of hysterectomy and associated factors in women Veterans Affairs patients . The Journal of Reproductive Medicine , 50 , 166 – 172 . [PubMed] [Google Scholar]
- Magruder K. Serpi T. Kimmerling R. Kilbourne A. M. Collins J. F. Cypel Y. ,… Kang H . ( 2015. ). Prevalence of posttraumatic stress disorder in Vietnam-Era Women Veterans: The Health of Vietnam-Era Women’s Study (HealthVIEWS) . JAMA Psychiatry , E1–E8. doi: 10.1001/jamapsychiatry.2015.1786 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marjoribanks J. Lethaby A. , & Farquhar C . ( 2006. ). Surgery versus medical therapy for heavy menstrual bleeding . Cochrane Database of Systematic Reviews , CD003855 . doi: 10.1002/14651858.CD003855 . [DOI] [PubMed] [Google Scholar]
- McEwen B. S . ( 2002. ). Sex, stress and the hippocampus: allostasis, allostatic load and the aging process . Neurobiology of Aging , 23 ( 5 ), 921 – 939 . [DOI] [PubMed] [Google Scholar]
- McEwen B. S . ( 2003. ). Interacting mediators of allostasis and allostatic load: Towards an understanding of resilience in aging . Metabolism , 52 ( 10 Suppl 2 ), 10 – 16 . [DOI] [PubMed] [Google Scholar]
- Rissling M.B. Gray K. Ulmer C. Martin J. Zaslavsky O. Gray S.L. ,… Weitlauf J. C . ( 2015. ). Sleep disturbance, diabetes and cardiovascular disease in postmenopausal Veteran women . The Gerontologist . 56 , S54 – S56 . doi:10.1093/geront/gnv668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T. , & Crimmins E . ( 2001. ). Social environmental effects on health and aging. Integrating epidemiologic and demographic approaches and perspectives . Annals of the New York Academy of Sciences , 954 , 88 – 117 . [DOI] [PubMed] [Google Scholar]
- U.S. Government Accountability Office . ( 2015. ). Report to Congressional Committees. Military Personnel: DOD is Expanding Combat Service Opportunities for Women, but Should Monitor Long-Term Integration Progress. GAO-15–589.
- Veteran Population Projection Model . ( 2014. ). (VetPop2014) Retrieved September 1, 2015 from http://www.va.gov/vetdata/veteran_population.asp
- Washington D. L. Bird C. E. LaMonte M. J. Goldstein K. M. Rillamas-Sun E Stefanick M. L. ,… Weitlauf J. C . ( 2015. ). Military generation and its relationship to mortality in women Veterans in the Women’s Health Initiative . The Gerontologist . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitlauf J. C. LaCroix A. Z. Bird C. E. Woods N. F. Washington D. L. Katon J. G. ,… Stefanick M. L . ( 2015. ). Prospective analysis of health and mortality risk in veteran women in the Women’s Health Initiative . Women’s Health Issues , 25 , 648 – 656 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Women’s Health Initiative Study Group . ( 1998. ). Design of the Women’s Health Initiative clinical trial and observational study . Control Clin Trials , 19 , 61 – 109 . [DOI] [PubMed] [Google Scholar]
- Women in Military Service for American Memorial Foundation, Inc . ( 2015. ) Retrieved September 1, 2015 from http://chnm.gmu.edu/courses/rr/s01/cw/students/leeann/historyandcollections/boiler/siteindex.htm
- Yano E. M. Bastian L. A. Bean-Mayberry B. Eisen S. Frayne S. Hayes P. ,… Washington D. L . ( 2011. ). Using research to transform care for women veterans: advancing the research agenda and enhancing research-clinical partnerships . Women’s Health Issues , 21 ( 4 Suppl ), S73 – S83 . doi: 10.1016/j.whi.2011.04.002 [DOI] [PubMed] [Google Scholar]