Abstract
Purpose of the Study:
To compare the number of chronic conditions among a list of 12 and their association with physical function among postmenopausal non-Veteran and Veteran women with diabetes.
Design and Methods:
Among women with diabetes from the Women’s Health Initiative, we compared the average number of chronic conditions between non-Veterans and Veterans and the association between total number of chronic conditions on subsequent RAND-36 physical function. To examine associations between each condition and subsequent physical function, we compared women with diabetes plus one chronic condition to women with diabetes alone using linear regression in separate models for each condition and for non-Veterans and Veterans.
Results:
Both non-Veterans ( N = 23,542) and Veterans ( N = 618) with diabetes had a median of 3 chronic conditions. Decreases in physical function for each additional condition were larger among Veterans than non-Veterans (−6.3 vs. −4.1 points). Decreases in physical function among women with diabetes plus one chronic condition were greater than that reported for diabetes alone for all combinations and were more pronounced among Veterans (non-Veterans: −11.1 to −24.2, Veterans: −16.6 to −40.4 points). Hip fracture, peripheral artery disease, cerebrovascular disease, and coronary disease in combination with diabetes were associated with the greatest decreases in physical function.
Implications:
Chronic conditions were common among postmenopausal women with diabetes and were associated with large declines in physical function, particularly among Veterans. Interventions to prevent and reduce the impact of these conditions and facilitate coordination of care among women with diabetes may help them maintain physical function.
Keywords: Physical function, Diabetes, Veterans, Women’s issues, Chronic illness
Diabetes affects one fifth of older adults and is a consistently strong predictor of poor physical function ( Kalyani, Saudek, Brancati, & Selvin, 2010 ; Ryerson et al., 2003 ; Wray, Ofstedal, Langa, & Blaum, 2005 ), particularly in older women ( Gregg et al., 2000 ). One putative explanation for the decrease in physical function associated with diabetes is the heavy burden of additional chronic conditions among people with diabetes ( Volpato et al., 2002 ), as 90% of adults with diabetes have at least one additional chronic illness ( Clarke & Meiris, 2007 ).
Among those with diabetes, chronic conditions may be conceptualized as concordant or discordant ( Kerr et al., 2007 ; Piette & Kerr, 2006 ). Concordant conditions reflect a similar pathophysiologic process or management strategy and include common diabetes complications such as neuropathy, nephropathy, and retinopathy (microvascular), as well as cardiovascular disease (macrovascular). Discordant conditions are those not necessarily related to the pathogenesis or management of diabetes but associated with diabetes in prior research, such as hip fracture, cancer, and depression. In previous investigations, concordance or discordance, and not just the number of chronic conditions, influenced diabetes self-management and prioritization ( Kerr et al., 2007 ), suggesting that concordance may be an important consideration when assessing associations of additional conditions on outcomes.
A number of studies have investigated the role of chronic conditions in the association between diabetes and physical impairment, reporting that adjustment for concordant and discordant chronic conditions attenuated observed associations ( Kalyani et al., 2010 ; Ryerson et al., 2003 ; Wray et al., 2005 ). However, few studies have examined associations of specific chronic conditions on function. Physical function is a critical component of successful and healthy aging ( Depp & Jeste, 2006 ), as it is required for older adults to maintain independence and active engagement within their communities ( Ford et al., 2000 ). Declining physical function is also associated with increased mortality ( Cooper, Kuh, & Hardy, 2010 ). With the projected growth in the population of older individuals in the United States ( Colby & Ortman, 2014 ) and concurrent increases in diabetes ( Boyle et al., 2001 ), identifying particular chronic conditions that result in the greatest decrements in physical function could highlight important targets for prevention and care coordination for individuals affected by diabetes.
No studies have investigated a broad array of chronic conditions or determined the influence of chronic conditions on physical function among women Veterans with diabetes. The prevalence of diabetes among women 65+ years of age who use Department of Veterans Affairs (VA) health care (“VA users”) is slightly higher than among the general population at 22% (vs. 20%), making it one of the most common conditions among this group of VA users ( Centers for Disease Control and Prevention, 2013 ; Frayne et al., 2014 ). Women Veterans with diabetes may be at particularly elevated risk of impaired physical function due to their higher overall burden of chronic disease and health risk factors compared to non-Veterans, including cardiovascular disease, depressive disorder, obese/overweight, tobacco use, and inactivity ( Lehavot, Hoerster, Nelson, Jakupcak, & Simpson, 2012 ). Furthermore, compared to non-Veteran women, women Veterans are more likely to report frequent poor health and limited activities due to physical, mental, or emotional problems ( Lehavot et al., 2012 ), which may have implications for both the development of chronic conditions and physical function.
Conceptual Model
Differences in the impact of chronic conditions on physical function between non-Veteran and Veteran women with diabetes may be understood within the framework of the adapted Biopsychosocial Model of Health and Aging ( Seeman & Crimmins, 2001 ). The model conceptualizes that macrolevel physical and sociocultural factors result in a network of personal factors, social relationships, individual socioeconomic status, and community-level social characteristics ( Seeman and Crimmins, 2001 ). These physical and sociocultural factors, along with individual genetic factors, physiologic reserve, and allostatic resources (the ability to maintain stability through ongoing life stresses) are impacted by regulated or dysregulated mediation by the neuroendocrine system, autonomic nervous system, and the immune system or allostasis ( McEwen, 2003 ). When the systems are in balance, stability and resilience are the result. When mediation mechanisms become taxed, are overactive and dysregulated, intermediate health outcomes, such as diabetes development, are exacerbated, and the risk for developing additional chronic conditions is increased. With increasing chronic conditions, we postulate declines in physical function.
Our adapted model also incorporates the potential effects of military service on health and aging, including personal factors related to enlistment in the military, such as physical fitness, socioeconomic status, and adverse childhood experiences ( Katon et al., 2015 ; National Center for Veterans Analysis and Statistics, 2011 ; Segal, Segal, Bachman, Freedman-Doan, & O’Malley, 1998 ) as well as military exposures or stressors, including military sexual trauma ( Stern et al., 2000 ) and exposure to violence ( Fontana, Schwartz, & Rosenheck, 1997 ). All of these factors may have unique influences on development of chronic physical and mental health conditions for women Veterans. This conceptual framework is depicted and further discussed in the first editorial in this issue ( Reiber & LaCroix, 2015 ).
Therefore, among postmenopausal non-Veteran and Veteran women with diabetes we sought to: (a) compare the total number of chronic conditions, among a list of 12, and the effect on subsequent physical function; (b) determine the prevalence of each chronic condition in combination with diabetes; and (c) estimate associations of each chronic condition plus diabetes on physical function compared to diabetes alone. We hypothesized that Veterans with diabetes would have more chronic comorbid conditions overall and that decrements in physical function associated with the chronic conditions would be greater than in non-Veterans. To address these aims, we utilized data from the Women’s Health Initiative (WHI), a longitudinal study of 161,808 postmenopausal women aged 50–79 years, which includes detailed health information on one of the largest samples of older women Veterans.
Design and Methods
WHI participants were recruited between 1993 and 1998 from 40U.S. clinical centers ( Anderson et al., 2003 ). WHI included an Observational Study (OS) and four randomized clinical trials—the Estrogen + Progestin (E + P) and Estrogen-Alone (E-Alone) hormone therapy trials, the Dietary Modification trial (DM), and the Calcium + Vitamin D trial (CaD). Data collection for the main study ended in 2005. Participants who remained alive and consented were followed in Extension Study 1 (ES1) between 2005 and 2010, and consenting ES1 participants are continuing to be followed in Extension Study 2 (ES2) from 2010 to 2015. WHI collected data through various mechanisms, including in-person or mailed self-reported questionnaires, in-person or phone interviews, and in-person clinical measurements conducted by trained staff at the clinical centers. WHI collected some data annually, including updated medical histories, and others only at baseline or at intervals throughout the main and extension studies. Main WHI study outcomes were adjudicated (coronary heart disease [CHD], stroke, breast cancer, colorectal cancer, hip fracture, pulmonary embolism, death).
Measures
Physical Function
Physical function was measured using the 10-item physical function subscale from the RAND 36-item Short Form Health Survey (SF-36) ( Ware, Snow, Kosinski & Gandek, 1993 ). Scores ranged from 0 to 100, with higher scores indicating better physical functioning. Assessment occurred multiple times throughout the WHI study, including at baseline for all participants and annually for all ES1 and ES2 participants (regardless of study assignment). Physical function as an outcome was defined as the most recently reported SF-36 physical function measure during ES1 or ES2 (e.g., the last available measure); women without a measurement in these windows were excluded. Baseline physical function was also examined as a covariate in some analyses, as described below.
Veteran Status
Veteran status was defined by baseline response to the question “Have you served in the U.S. armed forces on active duty for a period of 180 days or more?” Participants responding affirmatively were classified as Veterans and those negatively as non-Veterans; women missing this information were excluded ( N = 16,258).
Diabetes
Diabetes was defined as self-report of physician diagnosis at baseline or self-report of an incident prescription of medications or insulin for diabetes at follow-up, which is an acceptable indicator of diagnosed diabetes when compared with medication inventories and fasting glucose ( Jackson et al., 2014 ; Margolis et al., 2008 ).
Chronic Conditions
We ascertained the presence of select concordant and discordant chronic conditions assessed at baseline and follow-up, primarily through self-report of physician diagnosis (Rillamas-Sun et al., in press). The characterization of diabetes and the additional chronic conditions used data that were available through August 2014. These conditions could be reported prior to, at the time of, or after the diabetes diagnosis, as the purpose of our analyses was to examine the co-occurrence of a condition with diabetes, and not the timing of their development. Only concordant and discordant conditions reported prior to this last physical function measure were included in order to establish temporality between the exposures and outcomes.
Concordant Chronic Conditions
Concordant conditions were selected from those available in WHI that are considered common microvascular or macrovascular complications of diabetes ( Aung et al., 2015 ; Fowler, 2008 ; Kerr et al., 2007 ), including coronary disease (congestive heart failure, coronary revascularization, clinical myocardial infarction [MI], definite silent MI, or death due to definite or possible CHD [only during follow-up]); cerebrovascular disease (stroke, transient ischemic attack, carotid artery disease [only during follow-up], or carotid endarterectomy/angioplasty); eye disease (glaucoma, cataracts, and macular degeneration [follow-up only]); peripheral artery disease (PAD); and dialysis for kidney failure . Because components of the metabolic syndrome—elevated waist circumference, triglycerides, blood pressure, and fasting glucose, and reduced high density lipoprotein—are a set of commonly clustering risk factors for diabetes with a prevalence of 80% ( Marchesini et al., 2004 ), we did not examine them as chronic conditions herein.
Discordant Chronic Conditions
Conditions not considered to be common diabetes complications, but for which associations between diabetes and the condition have been reported, were examined as discordant conditions, including cancer (excluding nonmelanoma skin cancer) ( Suh & Kim, 2011 ); hip fracture ( Janghorbani, Van Dam, Willett, & Hu, 2007 ); osteoarthritis ( Schett et al., 2013 ); depression (score ≥0.06 on the Burnam Depression Scale or self-reported treatment for depression) ( Burnam, Wells, Leake, & Landsverk, 1988 ; Nouwen et al., 2010 ); cognitive impairment (self-report of physician diagnosis of dementia or Alzheimer’s disease or a Modified Mini-Mental State score of <89) ( Espeland et al., 2006 ; Luchsinger, 2012 ); frequent falls (self-report of ≥2 falls within 12 months prior to the last physical function assessment) ( Schwartz et al., 2002 ); and urinary incontinence (urine leakage that was perceived as very or extremely bothersome) ( Lifford, Curhan, Hu, Barbieri, & Grodstein, 2005 ). During follow-up coronary disease, cerebrovascular disease, cancer, and hip fracture were confirmed by examination of participant medical records by trained physician adjudicators, as these were primary or secondary outcomes for WHI ( Curb et al., 2003 ).
Total Conditions and Chronic Condition Categories
We calculated the total number of chronic conditions for each individual (possible range: 0–12) to reflect burden of chronic conditions and also created 12 chronic condition categories consisting of diabetes plus one additional condition (Rillamas-Sun et al., in press). We examined whether report of the other condition in conjunction with diabetes occurred anytime from baseline to follow-up, up to the time of their last available physical function measurement.
Covariates
Additional covariates of interest included the baseline variables age, race/ethnicity, educational attainment, income, marital status, body mass index (BMI), smoking status, alcoholic drinks consumed per week, physical activity (metabolic equivalent time—hours per week of leisure-time physical activity [ Ainsworth et al., 1993 ]), self-reported use of pills for high cholesterol, self-reported use of pills for hypertension, self-reported use of insulin, and study assignment (OS, E-Alone intervention, E-Alone control, E + P intervention, E + P control, DM intervention, DM control). We also examined control of hypertension using a combination of self-reported use of pills and measured hypertension (systolic ≥ 140 and diastolic ≥ 90) to define individuals as: no medication/not hypertensive, no medications/hypertensive, medications/not hypertensive, and medications/hypertensive. We also accounted for duration of follow-up.
Data Analysis
We first examined the sociodemographic characteristics of the non-Veteran and Veteran participants. We compared the average follow-up time between groups with the Wilcoxon rank-sum test due to nonnormality of follow-up time ( Wilcoxon, 1945 ), and we used Pearson’s chi-squared test to examine differences in the proportion of women who had their last physical function measure in ES1 and ES2. For both non-Veterans and Veterans, we obtained the prevalence of diabetes alone and of having each of the other 12 chronic conditions concurrently with diabetes. For diabetes alone and all 12 disease combinations, we computed the age-adjusted means and standard deviations of the physical function score using linear regression.
Total Number of Conditions
We examined the distribution of number of chronic conditions among non-Veterans and Veterans with diabetes separately. Using Poisson regression to obtain average differences in counts and the corresponding 95% confidence intervals (CIs), we statistically compared the number of chronic conditions between non-Veterans and Veterans ( Supplementary Appendix 1, Equation 1 ).
Association Between Total Number of Conditions and Physical Function
Using linear regression with robust SE estimates, we estimated the association between the burden of chronic conditions (total number of chronic conditions) and subsequent physical function, including an interaction term between Veteran status and number of conditions ( Supplementary Appendix 2, Equation 2 ). The interaction allowed for testing of whether the effect of total number of conditions on physical function differed between non-Veterans and Veterans. We excluded women with more than seven chronic conditions because of small sample size in Veterans ( n ≤ 1).
Association Between Each Co-occurring Chronic Condition and Physical Function
In linear regression models fit separately for non-Veterans and Veterans, we examined associations of each chronic condition in combination with diabetes on subsequent physical function. The exposure in these regressions was an indicator variable (0 for diabetes only and 1 for diabetes plus one other condition), with women with diabetes only serving as the reference group ( Supplementary Appendix 2, Equation 3 ). The coefficient for the indicator variable reflected the average difference in physical function score associated with having diabetes plus the chronic condition compared to having diabetes only. Because of the small sample sizes particularly among Veteran women ( n = 2), we excluded kidney dialysis from these analyses, resulting in 11 linear regression models for non-Veterans and 11 for non-Veterans. To formally test for statistically significant differences between non-Veterans and Veterans in the association between each condition and physical function, we re-fit the linear regression models with an interaction term between the indicator for the chronic condition and Veteran status ( Supplementary Appendix 1, Equation 4 ). However, we had limited power to detect interactions due to small cell sizes among Veterans.
All regression analyses were adjusted for baseline age (continuous), race (non-white/white, dichotomous), education (ordinal), smoking status (nominal), BMI (continuous), physical activity (continuous), use of pills for hypertension (no/yes), and use of pills for hypercholesterolemia (no/yes). These covariates were selected based on a priori knowledge of their associations with exposures and outcomes ( Greenland & Neutra, 1980 ; Hernán, Hernández-Díaz, Werler, & Mitchell, 2002 ; Robins, 2001 ; Rothman & Greenland, 1998 ). Additional adjustment was made for duration of follow-up since longer observation in the study increased the exposure period in which a woman could develop a chronic condition or have lower physical functioning. Analyses with physical function as the outcome were adjusted for baseline physical function (continuous).
All analyses were conducted using Stata 13 (Stata Corp, College Station, TX) and we used an alpha .05 level for all hypothesis tests.
Results
Of the 144,684 women with information on diabetes and Veteran status, 16.7% of both non-Veterans and Veterans had diabetes, leading to a study sample of 23,542 non-Veteran women and 618 Veteran women. Approximately 85% of women had complete data to identify the presence of all the chronic conditions from our list. Compared to non-Veterans, Veteran women were older, more educated, more likely to have ever smoked, less likely to be married or in a marriage-like relationship, and to be a racial/ethnic minority ( Table 1 ). Half of women were taking pills for hypertension and using insulin at baseline. Non-Veterans and Veterans with diabetes had similar average follow-up time (~15 years, p = .12) and proportion of physical function scores ascertained in ES2 (non-Veterans: 26%, Veterans: 23%, p = .18; data not shown).
Table 1.
Baseline Characteristics of Non-Veteran and Veteran Women With Diabetes in the Women’s Health Initiative
| Non-Veterans | Veterans | |||
|---|---|---|---|---|
| N | % | N | % | |
| Total | 23,524 | 618 | ||
| Baseline | ||||
| Age | ||||
| 50–59 | 7,412 | 31.5 | 148 | 23.9 |
| 60–69 | 11,281 | 48.0 | 217 | 35.1 |
| 70+ | 4,831 | 20.5 | 253 | 40.9 |
| Race/ethnicity | ||||
| American Indian/Alaskan native | 194 | 0.8 | 8 | 1.3 |
| Asian/Pacific Islander | 751 | 3.2 | 10 | 1.6 |
| Black/African American | 3,854 | 16.4 | 76 | 12.3 |
| Hispanic/Latina | 1,286 | 5.5 | 23 | 3.7 |
| White | 17,053 | 72.5 | 485 | 78.5 |
| Other | 324 | 1.4 | 13 | 2.1 |
| Education | ||||
| Less than high school | 1,907 | 8.1 | 17 | 2.8 |
| High school diploma/GED | 4,521 | 19.2 | 68 | 11.0 |
| Some college or vocational/training school | 9,331 | 39.7 | 270 | 43.7 |
| College graduate or more | 7,610 | 32.3 | 261 | 42.2 |
| Income | ||||
| <20,000 | 5,037 | 21.4 | 126 | 20.4 |
| 20,000–<50,000 | 10,113 | 43.0 | 287 | 46.4 |
| 50,000–<75,000 | 3,884 | 16.5 | 105 | 17.0 |
| 75,000+ | 3,038 | 12.9 | 65 | 10.5 |
| Marital status | ||||
| Never married | 1,014 | 4.3 | 70 | 11.3 |
| Divorced/separated | 4,184 | 17.8 | 117 | 18.9 |
| Widowed | 4,576 | 19.5 | 141 | 22.8 |
| Married/marriage-like relationship | 13,653 | 58.0 | 289 | 46.8 |
| Body mass index | ||||
| Underweight | 82 | 0.3 | 5 | 0.8 |
| Normal | 3,810 | 16.2 | 124 | 20.1 |
| Overweight | 7,185 | 30.5 | 184 | 29.8 |
| Obese | 12,234 | 52.0 | 302 | 48.9 |
| Smoking status | ||||
| Never | 11,860 | 50.4 | 274 | 44.3 |
| Former | 9,630 | 40.9 | 271 | 43.9 |
| Current | 1,703 | 7.2 | 62 | 10.0 |
| Alcohol intake | ||||
| Nondrinker | 3,329 | 14.2 | 51 | 8.3 |
| Past drinker | 6,427 | 27.3 | 188 | 30.4 |
| <1 drink per week | 7,917 | 33.7 | 206 | 33.3 |
| 1+ drinks per week | 5,652 | 24.0 | 166 | 26.9 |
| Physical activity (MET-hours/week) | ||||
| Inactive (0–1.7) | 6,814 | 29.0 | 173 | 28.0 |
| Low (>1.7–<8.4) | 7,203 | 30.6 | 169 | 27.3 |
| Medium (8.4–<20.0) | 5,696 | 24.2 | 154 | 24.9 |
| High (20.0+) | 3,730 | 15.9 | 119 | 19.3 |
| Physical function score | ||||
| 0–<25 | 890 | 3.8 | 21 | 3.4 |
| 25–<50 | 2,569 | 10.9 | 87 | 14.1 |
| 50–<75 | 5,070 | 21.6 | 117 | 18.9 |
| 75–100 | 14,466 | 61.5 | 369 | 59.7 |
| Pills for high cholesterol | ||||
| No | 18,258 | 77.6 | 451 | 73.0 |
| Yes | 4,936 | 21.0 | 158 | 25.6 |
| BP control a | ||||
| No medications, normal BP | 9,919 | 42.2 | 253 | 40.9 |
| No medications, high BP | 2,241 | 9.5 | 68 | 11.0 |
| Medications, normal BP | 6,508 | 27.7 | 160 | 25.9 |
| Medications, high BP | 4,636 | 19.7 | 125 | 20.2 |
| Insulin use | ||||
| No | 12,961 | 55.1 | 327 | 52.9 |
| Yes | 10,463 | 44.5 | 287 | 46.4 |
| Study assignment | ||||
| Observational Study | 12,763 | 54.3 | 351 | 56.8 |
| Estrogen-Alone intervention | 1,096 | 4.7 | 29 | 4.7 |
| Estrogen-Alone control | 1,134 | 4.8 | 31 | 5.0 |
| Estrogen + Progestin intervention | 1,232 | 5.2 | 32 | 5.2 |
| Estrogen + Progestin control | 1,216 | 5.2 | 32 | 5.2 |
| Dietary Modification intervention | 2,358 | 10.0 | 60 | 9.7 |
| Dietary Modification control | 3,725 | 15.8 | 83 | 13.4 |
| Through follow-up | ||||
| Number of chronic conditions b | ||||
| 0 | 1,397 | 7.0 | 36 | 6.9 |
| 1 | 3,836 | 19.2 | 77 | 14.9 |
| 2 | 5,414 | 27.1 | 131 | 25.3 |
| 3 | 4,596 | 23.0 | 126 | 24.3 |
| 4+ | 4,759 | 23.8 | 148 | 28.6 |
| Number of concordant chronic conditions b | ||||
| 0 | 1,331 | 6.7 | 23 | 4.4 |
| 1 | 6,022 | 30.1 | 142 | 27.4 |
| 2 | 8,504 | 42.5 | 227 | 43.8 |
| 3 | 3,134 | 15.7 | 90 | 17.4 |
| 4+ | 1,011 | 5.1 | 36 | 6.9 |
| Number of discordant chronic conditions b | ||||
| 0 | 4,135 | 20.7 | 101 | 19.5 |
| 1 | 6,846 | 34.2 | 171 | 33.0 |
| 2 | 5,233 | 26.2 | 141 | 27.2 |
| 3 | 2,653 | 13.3 | 67 | 12.9 |
| 4+ | 1,135 | 5.7 | 38 | 7.3 |
Notes: BP, blood pressure; GED, general educational development; MET, metabolic equivalent time.
a Systolic BP ≥140mm Hg or diastolic BP ≥90mm Hg considered high.
b Among women with no missing data on chronic conditions; assessed up until last physical function measure in the Extension Studies.
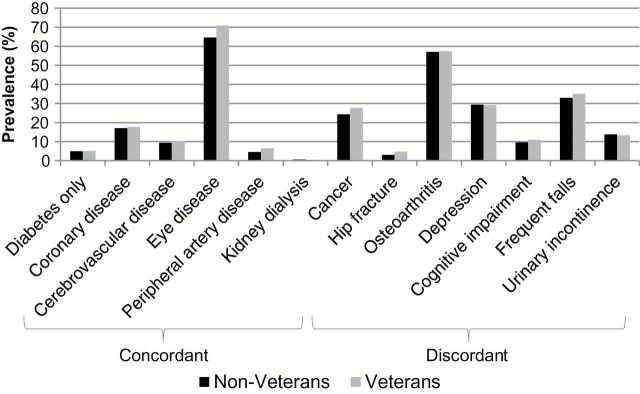
Among non-Veterans, 4.9% had diabetes alone, compared to 5.2% in Veterans, with corresponding age-adjusted physical function scores of 72.0 and 78.9, respectively ( Figure 1 ; Table 2 ). The most common conditions were eye disease, osteoarthritis, frequent falls, and depression, and prevalence of each condition was generally slightly higher in Veterans. Aside from women with diabetes alone, Veterans had slightly lower age-adjusted mean physical function scores with the presence of most conditions ( Table 2 ).
Figure 1.
Unadjusted prevalence of concordant and discordant chronic conditions among Non-Veteran and Veteran women with diabetes. The most common chronic conditions among Non-Veteran and Veteran women with diabetes were eye disease, osteoarthritis, and frequent falls. The prevalence of each chronic condition was slightly higher in Veterans than Non-Veterans for all but kidney dialysis, depression, and urinary incontinence.
Table 2.
Age-Adjusted Average Physical Function Scores Among Non-Veteran and Veteran Women With Diabetes Alone and With Additional Chronic Conditions a
| Chronic conditions | Non-Veterans | Veterans | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Median number of chronic conditions b | Mean | SD | Median number of chronic conditions b | |
| Diabetes only | 72.0 | 1.2 | 0 | 78.9 | 3.4 | 0 |
| Diabetes and concordant conditions | ||||||
| Coronary disease | 43.5 | 0.5 | 4 | 40.3 | 3.8 | 4 |
| Cerebrovascular disease | 42.5 | 0.8 | 4 | 42.5 | 4.8 | 4 |
| Eye disease | 52.7 | 0.3 | 3 | 50.9 | 1.9 | 3 |
| Peripheral artery disease | 39.4 | 1.0 | 4 | 31.2 | 4.5 | 4 |
| Kidney dialysis | 45.0 | 3.0 | 5 | 62.9 | 0.0 | 5 |
| Discordant conditions | ||||||
| Cancer | 51.4 | 0.5 | 3 | 51.3 | 2.7 | 3 |
| Hip fracture | 39.8 | 1.6 | 4 | 37.8 | 6.8 | 4 |
| Osteoarthritis | 51.9 | 0.3 | 3 | 52.2 | 1.9 | 3 |
| Depression | 48.6 | 0.4 | 4 | 46.2 | 2.5 | 4 |
| Cognitive impairment | 46.7 | 0.9 | 4 | 45.2 | 6.2 | 4 |
| Frequent falls | 48.6 | 0.4 | 3 | 45.2 | 2.4 | 4 |
| Urinary incontinence | 46.7 | 0.6 | 4 | 42.1 | 3.8 | 4 |
Notes: a At mean age of 63.3 years.
b Observed, unadjusted median number of chronic conditions, including concordant or discordant condition specified in row.
Total Number of Conditions
Among women with diabetes, non-Veterans and Veterans had a median of three chronic conditions, with a range of 0–9. In fully adjusted Poisson regression, in which we examined differences between Veterans and non-Veterans in the total number of chronic conditions, there was no evidence that the groups differed (difference = 0.01, 95% CI: −0.05, 0.07; Table 3 ).
Table 3.
Difference in Number of Chronic Conditions Between Veterans and Non-Veterans
| Veterans compared to non-Veterans | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Veterans | Veterans | 95% CI | |||||||||
| N | Median | Min | Max | N | Median | Min | Max | Diff. a | LB | UB | p value |
| 14,296 | 3 | 0 | 9 | 372 | 3 | 0 | 9 | 0.01 | −0.05 | 0.07 | .68 |
Notes: CI, confidence interval; diff., difference; LB, lower bound; UB, upper bound.
a Adjusted for baseline age, race, education, smoking, body mass index, physical activity, hypertension, hypercholesterolemia, and duration of follow-up.
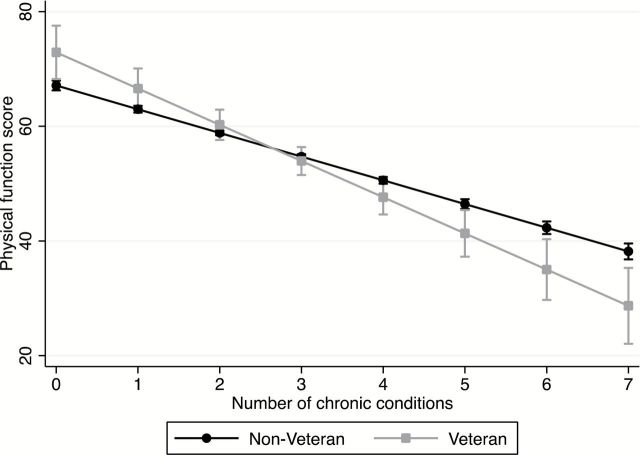
Association Between Total Number of Conditions and Physical Function
In both non-Veterans and Veterans with diabetes, the burden of chronic conditions was inversely associated with physical function in linear regression. Physical function score decreased by 4.1 points (95% CI: −4.4, −3.8) per additional condition in non-Veterans and 6.3 (95% CI: −7.8, −4.9) in Veterans ( Figure 2 ; Supplementary Table 2 ), which was significantly different when examining the interaction between Veteran status and the total number of chronic conditions ( p value for interaction = .004).
Figure 2.
Adjusted association between number of chronic conditions and physical function among Non-Veteran and Veteran women with diabetes. Among Non-Veterans, physical function scores decreased by 4.1 points (95% CI: −4.4, −3.8) per additional condition in Non-Veterans and 6.3 (95% CI: −7.8, −4.9) in Veterans, which was significantly different ( p value for interaction = .004). Analyses were adjusted for baseline age, race, education, smoking, body mass index, physical activity, baseline physical function, use of pills for hypertension, use of pills for hypercholesterolemia, and duration of follow-up.
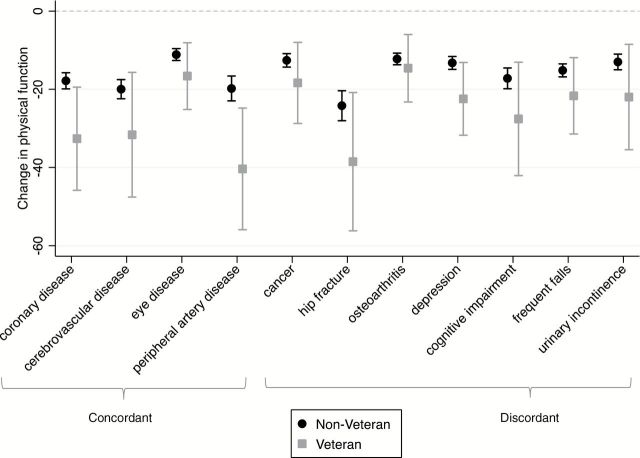
Association Between Each Co-occurring Chronic Condition and Physical Function
In analyses stratified by Veteran status, having any of the comorbid conditions in addition to diabetes led to greater decrements in physical function compared to diabetes alone for both non-Veterans and Veterans. In non-Veterans, the adjusted decreases were between 11 and 24 points across conditions ( Figure 3 ; Supplementary Table 3 ). Among Veterans, decreases were more pronounced, ranging from 17 to 40 points. In both groups, the greatest decreases were observed for diabetes in combination with the concordant conditions, PAD, cerebrovascular disease, and coronary disease, and the discordant condition, hip fracture. When we analyzed the data using interaction terms in order to examine differences in the effect of each chronic condition on physical function by Veteran status, only diabetes plus depression was statistically significant ( p value = .04). However, decreases in physical function score were larger among Veterans for all conditions, consistent with the stratified analyses ( Supplementary Table 4 ).
Figure 3.
Mean difference in physical function score for participants with diabetes plus an additional concordant or discordant chronic condition compared to diabetes alone, stratified by Veteran status. Compared to women with diabetes alone, women with each chronic condition had greater impairments in physical function, among both Non-Veterans and Veterans. Across all chronic conditions, the decrements in physical function were larger among Veterans compared to Non-Veterans. The largest decreases in physical function among both groups were seen for hip fracture, peripheral artery disease, coronary disease, and cerebrovascular disease. Models were adjusted for baseline age, race, education, smoking, body mass index, physical activity, physical function, use of pills for hypertension, use of pills for hypercholesterolemia, and duration of follow-up.
Discussion
In the current study population, half of women with diabetes had three or more chronic conditions, highlighting the heavy disease burden in this group. These findings are consistent with prior studies examining additional chronic conditions among adults with diabetes ( Kerr et al., 2007 ; Wolff, Starfield, & Anderson, 2002 ). Among individuals with diabetes, this issue is particularly important, as additional chronic conditions are associated with reduced quality of life ( Maddigan, Feeny, & Johnson, 2005 ), increases in health care utilization ( Struijs, Baan, Schellevis, Westert, & van den Bos, 2006 ), impaired self-management, lower prioritization of diabetes management ( Kerr et al., 2007 ), and increased mortality ( Lynch, Gebregziabher, Zhao, Hunt, & Egede, 2014 ). However, impacts on diabetes outcomes may vary depending on whether conditions are concordant or discordant with diabetes ( Kerr et al., 2007 ).
Veteran women with diabetes had slightly higher prevalence of most concordant and discordant chronic conditions; however, differences were fairly small. The most prevalent chronic conditions among both non-Veterans and Veterans included eye disease (concordant) and osteoarthritis, frequent falls, and depression (discordant). Other investigations in women with diabetes have reported high prevalence of hypertension, coronary disease, and arthritis, as well as peripheral nerve dysfunction ( Gregg et al., 2002 ; Maty et al., 2004 ; Volpato et al., 2003 ), but differences in study populations and included conditions make comparisons difficult. Consistent with previous investigations, we also observed that with an increasing number of chronic conditions, physical function declined ( Caruso, Silliman, Demissie, Greenfield, & Wagner, 2000 ; Der-Martirosian, Cordasco, & Washington, 2013 ; Rillamas-Sun et al., in press). With each additional condition, physical function scores decreased by 4 points among non-Veterans and 6 points among non-Veterans.
In all women, we observed that physical function was impaired to a greater extent in women with each of the selected chronic conditions compared to women with diabetes alone regardless of whether conditions were concordant or discordant. These decreases were quite pronounced, ranging from 11 to 40 points. In a previous examination of the effect of differences in physical function on mortality, a 1-point decrease in physical function conferred a 6%–9% increase in 2-year mortality risk among individuals with diabetes, suggesting the decreases we observed herein could impact mortality ( Bjorner, Lyng Wolden, Gundgaard, & Miller, 2013 ). Among both non-Veterans and Veterans, the greatest declines were observed for the concordant chronic conditions, PAD, coronary disease, and cerebrovascular disease, and the discordant chronic condition, hip fracture, indicating they are important targets for prevention for both groups of women. When we looked at the total burden of chronic conditions among women with each chronic condition in addition to diabetes, a higher burden among women with these four conditions could not explain our findings (e.g., we observed a similar median number of conditions among women with diabetes plus coronary disease as women with diabetes plus urinary incontinence).
Although the chronic conditions were associated with declines in physical function among both non-Veterans and Veterans, the effects were 2–21 points higher across conditions in Veterans. Furthermore, the greatest differences between non-Veterans and Veterans were observed in the four conditions associated with the greatest declines in both groups (PAD, coronary disease, cerebrovascular disease, and hip fracture). Given that differences of this magnitude could lead to meaningful disparities in mortality, our findings may partially explain the increased mortality reported among Veterans compared to non-Veterans ( Weitlauf et al., 2015 ).
The reasons for the greater decreases among Veterans are unclear. Distributions of a number of demographic characteristics and health behavior practices that fit within the Adapted Biopsychosocial Model of Health and Aging and that are associated with both physical function and disability were similar among non-Veterans and Veterans, ( Bruce, Davis, & Davis, 2005 ) and adjustment for these variables did not eliminate differences. Veterans with diabetes may also have more severe disease or poorer disease management, leading to greater decreases in physical function. Self-reported use of insulin and pills for hypercholesterolemia, as well as hypertension control, were similar at baseline, suggesting comparable treatment levels at least across these measures ( Joish, Malone, Wendel, Draugalis, & Mohler, 2005 ). However, measures of glycemic control are not available for all WHI participants, and thus we cannot rule out the possibility that poorer disease control might account for these findings. Furthermore, contrary to our expectation, we observed that the total number of chronic conditions was similar between non-Veterans and Veterans, and therefore disparities in chronic condition burden likely cannot account for differences by Veteran status. The lack of differences in total number of conditions may be explained by the study population of WHI, which included generally healthy women at study entry in contrast to previous population-based studies that report differences between non-Veterans and Veterans ( Lehavot et al., 2012 ).
Additional factors that could potentially explain the larger declines in physical function associated with each chronic condition among Veterans may include those related to military-specific exposures outlined in the Adapted Biopsychosocial Model of Health and Aging. Military sexual or physical trauma and witnessing violence are both associated with decreases in physical function ( Sadler, Booth, Mengeling, & Doebbeling, 2004 ). These and other military experiences may contribute to development of posttraumatic stress disorder ( Yaeger, Himmelfarb, Cammack, & Mintz, 2006 ) and depression ( Boyd, Bradshaw, & Robinson, 2013 ), which also impair physical function ( Dobie et al., 2004 ; Tomey et al., 2010 ). Differences prior to or at entry into the military may also play a role in these findings. However, we did not have detailed data on military mental or physical stressors or historical information on participants prior to their entry into the military, as outlined in the Adapted Biopsychosocial Model of Health and Aging, and therefore we could not examine the contribution of these factors on the observed differences in association between chronic conditions and physical function among Veterans and non-Veterans.
Strengths and Limitations
Strengths of this study include the use of one of the largest and most diverse study populations of older Veteran women and inclusion of a broad array of both concordant and discordant chronic conditions. Furthermore, this is one of the only studies to examine differences between non-Veteran and Veteran women in the health effects of co-occurring chronic conditions. We were not able to examine some common chronic conditions, including nephropathy and neuropathy; however, we made use of proxy variables, where possible (e.g., kidney dialysis for nephropathy). In analyses examining the association between total number of chronic conditions and physical function, we used a simple count, which did not take into account severity or potential differential influences on physical function. However, our approach was similar to other common indices reflecting burden of chronic conditions, such as Elixhauser’s Comorbidity Measure ( Elixhauser, Steiner, Harris, & Coffey, 1998 ). We were also underpowered to detect differences between non-Veterans and Veterans in the association between each chronic condition and physical function due to small sample sizes among women Veterans. As a result, almost all formal tests of interactions were not statistically significant. However, the consistency of larger decrements in physical function score among Veterans relative to non-Veterans in both stratified and interaction analyses cannot be ignored. Furthermore, we executed 22 statistical tests across the stratified analysis, which may have inflated our Type I error rate (false positives). However, using the Bonferroni-corrected p value of .0023 (.05/22 tests), all estimates in the stratified analyses would remain significant ( Bland & Altman, 1995 ). We were also limited by the lack of information on duration of military service or type of job performed in the military among women Veterans, which could potentially be related to the development of chronic conditions, as well as physical function. Therefore, we could not examine the contribution of these variables to our findings, and results may differ among other samples of women Veterans with different service characteristics. Lastly, many of the Veterans in this sample likely served in pre-Vietnam conflicts (e.g., WWII), thus the extent to which these findings can be generalized to current midlife or younger women Veterans is not known.
Implications for Practice and Policy
Given the large decreases in physical function associated with chronic conditions, efforts to prevent or delay development of these conditions or to more seamlessly integrate care of existing chronic conditions in women with diabetes should be a priority. Despite the prevalence of chronic conditions among people with diabetes, guidelines on clinical approaches to chronic conditions in general and on discordant conditions in particular are limited ( Lugtenberg, Burgers, Clancy, Westert, & Schneider, 2011 ). For concordant chronic conditions, achieving recommended hemoglobin A1c, cholesterol, and blood pressure targets, as well as improvements in diet and physical activity, reduce risk of macrovascular and microvascular complications ( American Diabetes Association, 2015 ), which can impair physical function above and beyond diabetes. In line with these recommended targets, use of blood glucose–lowering agents and blood pressure–lowering medications is 80% among adults with diabetes, and 60% use a lipid-lowering medication ( Wong, Ong, Cheung, & Cheung, 2014 ). However, strategies for discordant chronic conditions are less clear and potentially at odds with diabetes care. For example, hypoglycemia, a possible side effect of insulin and oral diabetes medications, may increase the risk of falls ( Schwartz et al., 2008 ), and some oral medications may also increase the risk of fracture, particularly among women ( Loke, Singh, & Furberg, 2009 ).
For VA users, the recently adopted Patient-Centered Medical Home (PCMH) may facilitate comprehensive, coordinated care for patients with diabetes. This patient centric approach is supported by a primary care team of providers, nurse care managers, and clinical and administrative staff ( Rosland et al., 2013 ). Among individuals with diabetes, the PCMH has been associated with better quality of care, including A1c, blood pressure, and cholesterol targets, reductions in emergency room and inpatient admissions, and improvements in patient satisfaction ( Bojadzievski & Gabbay, 2011 ). However, no investigations have examined whether this approach specifically prevents development of chronic conditions or facilitates coordinated care for prevalent conditions. Future research should investigate the role of the PCMH and other organizational factors in reducing the incidence of chronic conditions, mitigating declines in physical function, and improving the quality of care beyond diabetes-specific care in patients with both concordant and discordant chronic conditions, particularly for women Veterans.
Funding
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services (grant numbers HHSN268201100046C, HHSN268201100001C, HHSN268201 100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C).
WHI Investigators— Program Office : Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller (National Heart, Lung, and Blood Institute, Bethesda, MD). Clinical Coordinating Center : Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg (Fred Hutchinson Cancer Research Center, Seattle, WA). Investigators and Academic Centers : JoAnn E. Manson (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA); Barbara V. Howard (MedStar Health Research Institute/Howard University, Washington, DC); Marcia L. Stefanick (Stanford Prevention Research Center, Stanford, CA); Rebecca Jackson (The Ohio State University, Columbus, OH); Cynthia A. Thomson (University of Arizona, Tucson/Phoenix, AZ); Jean Wactawski-Wende (University at Buffalo, Buffalo, NY); Marian Limacher (University of Florida, Gainesville/Jacksonville, FL); Robert Wallace (University of Iowa, Iowa City/Davenport, IA); Lewis Kuller (University of Pittsburgh, Pittsburgh, PA); and Sally Shumaker (Wake Forest University School of Medicine, Winston-Salem, NC). Women’s Health Initiative Memory Study : Sally Shumaker (Wake Forest University School of Medicine, Winston-Salem, NC). For a list of all the investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf This work was also supported by the U.S. Department of Veterans Affairs Health Services Research & Development Program (Postdoctoral Fellowship TPP 61-029 to K. E. Gray); U.S. Department of Veterans Affairs Office of Patient Care, Women’s Health Services; and the VA Puget Sound Center of Innovation for Veteran-Centered and Value-Driven Care (to J. G. Katon). This work was also supported by the Department of Veterans Affairs Health Services Research and Development VA HSR&D FOP 14-439; the VA Office of Womenʼs Health; and a VA HSR&D Senior Research Career Scientist Award (Project RCS 98-353 to G. E. Reiber).
Supplementary Material
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
References
- Ainsworth B. E. Haskell W. L. Leon A. S. Jacobs D. R. Jr. Montoye H. J. Sallis J. F. , & Paffenbarger R. S. Jr . ( 1993. ). Compendium of physical activities: Classification of energy costs of human physical activities . Medicine and Science in Sports and Exercise , 25 , 71 – 80 . [DOI] [PubMed] [Google Scholar]
- American Diabetes Association . ( 2015. ). (6) Glycemic targets . Diabetes Care , 38 ( Suppl. 1 ), S33 – S40 . doi: 10.2337/dc15-S009 [DOI] [PubMed] [Google Scholar]
- Anderson G. L. Manson J. Wallace R. Lund B. Hall D. Davis S. , … Prentice R. L . ( 2003. ). Implementation of the Women’s Health Initiative study design . Annals of Epidemiology , 13 ( Suppl. 9 ), S5 – S17 . doi: 10.1016/S1047-2797(03)00043-7 [DOI] [PubMed] [Google Scholar]
- Aung E. Donald M. Coll J. Dower J. Williams G. M. , & Doi S. A . ( 2015. ). The impact of concordant and discordant comorbidities on patient-assessed quality of diabetes care . Health Expectations , 18 , 1621 – 1632 . doi: 10.1111/hex.12151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorner J. B. Lyng Wolden M. Gundgaard J. , & Miller K. A . ( 2013. ). Benchmarks for interpretation of score differences on the SF-36 health survey for patients with diabetes . Value Health , 16 , 993 – 1000 . doi: 10.1016/j.jval.2013.06.022 . [DOI] [PubMed] [Google Scholar]
- Bland J. M. , & Altman D. G . ( 1995. ). Multiple significance tests: The Bonferroni method . British Medical Journal , 310 , 170 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojadzievski T. , & Gabbay R. A . ( 2011. ). Patient-Centered Medical Home and diabetes . Diabetes Care , 34 , 1047 – 1053 . doi: 10.2337/dc10-1671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd M. A. Bradshaw W. , & Robinson M . ( 2013. ). Mental health issues of women deployed to Iraq and Afghanistan . Archives of Psychiatric Nursing , 27 , 10 – 22 . doi: 10.1016/j.apnu.2012.10.005 [DOI] [PubMed] [Google Scholar]
- Boyle J. P. Honeycutt A. A. Narayan K. M. Hoerger T. J. Geiss L. S. Chen H. , & Thompson T. J . ( 2001. ). Projection of diabetes burden through 2050: Impact of changing demography and disease prevalence in the U.S . Diabetes Care , 24 , 1936 – 1940 . doi: 10.2337/diacare.24.11.1936 [DOI] [PubMed] [Google Scholar]
- Bruce D. G. Davis W. A. , & Davis T. M . ( 2005. ). Longitudinal predictors of reduced mobility and physical disability in patients with type 2 diabetes: The Fremantle Diabetes Study . Diabetes Care , 28 , 2441 – 2447 . doi: 10.2337/diacare.28.10.2441 [DOI] [PubMed] [Google Scholar]
- Burnam M. A. Wells K. B. Leake B. , & Landsverk J . ( 1988. ). Development of a brief screening instrument for detecting depressive disorders . Medical Care , 26 , 775 – 789 . [DOI] [PubMed] [Google Scholar]
- Caruso L. B. Silliman R. A. Demissie S. Greenfield S. , & Wagner E. H . ( 2000. ). What can we do to improve physical function in older persons with type 2 diabetes? The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences , 55 , M372 – M377 . doi: 10.1093/gerona/55.7.M372 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health Interview Statistics . ( 2013. ). Rate per 100 of civilian, noninstitutionalized population with diagnosed diabetes, females, by age, United States, 1980–2011 . Retrieved from http://www.cdc.gov/diabetes/statistics/prev/national/tprevfemage.htm
- Clarke J. L. , & Meiris D. C . ( 2007. ). Building bridges: Integrative solutions for managing complex comorbid conditions . American Journal of Medical Quality , 22 ( Suppl. 2 ), 5S – 16S . doi: 10.1177/1062860607299242 [DOI] [PubMed] [Google Scholar]
- Colby S. L. , & Ortman J. M . ( 2014. ). Projections of the size and composition of the U.S. population: 2014 to 2050. Current population reports (P25-1143) . Washington, DC: : U.S. Census Bureau; . [Google Scholar]
- Cooper R. Kuh D. , & Hardy R . ( 2010. ). Objectively measured physical capability levels and mortality: Systematic review and meta-analysis . British Medical Journal , 341 , c4467 . doi: 10.1136/bmj.c4467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curb J. D. McTiernan A. Heckbert S. R. Kooperberg C. Stanford J. Nevitt M. , … Daugherty S .; WHI Morbidity and Mortality Committee . ( 2003. ). Outcomes ascertainment and adjudication methods in the Women’s Health Initiative . Annals of Epidemiology , 13 ( Suppl. 9 ), S122 – S128 . doi: 10.1016/S1047-2797(03)00048-6 [DOI] [PubMed] [Google Scholar]
- Depp C. A. , & Jeste D. V . ( 2006. ). Definitions and predictors of successful aging: A comprehensive review of larger quantitative studies . American Journal of Geriatric Psychiatry , 14 , 6 – 20 . doi: 10.1097/01.JGP.0000192501.03069.bc [DOI] [PubMed] [Google Scholar]
- Der-Martirosian C. Cordasco K. M. , & Washington D. L . ( 2013. ). Health-related quality of life and comorbidity among older women veterans in the United States . Quality of Life Research , 22 , 2749 – 2756 . doi: 10.1007/s11136-013-0424-7 [DOI] [PubMed] [Google Scholar]
- Dobie D. J. Kivlahan D. R. Maynard C. Bush K. R. Davis T. M. , & Bradley K. A . ( 2004. ). Posttraumatic stress disorder in female veterans: Association with self-reported health problems and functional impairment . Archives of Internal Medicine , 164 , 394 – 400 . doi: 10.1001/archinte.164.4.394 [DOI] [PubMed] [Google Scholar]
- Espeland M. A. Rapp S. R. Robertson J. Granek I. Murphy C. Albert M. , & Bassford T . ( 2006. ). Benchmarks for designing two-stage studies using modified mini-mental state examinations: Experience from the Women’s Health Initiative Memory Study . Clinical Trials , 3 , 99 – 106 . doi: 10.1191/1740774506cn140oa [DOI] [PubMed] [Google Scholar]
- Elixhauser A. Steiner C. Harris D. R. , & Coffey R. M . ( 1998. ). Comorbidity measures for use with administrative data . Medical Care , 36 , 8 – 27 . [DOI] [PubMed] [Google Scholar]
- Fontana A. Schwartz L. S. , & Rosenheck R . ( 1997. ). Posttraumatic stress disorder among female Vietnam veterans: A causal model of etiology . American Journal of Public Health , 87 , 169 – 175 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford A. B. Haug M. R. Stange K. C. Gaines A. D. Noelker L. S. , & Jones P. K . ( 2000. ). Sustained personal autonomy: A measure of successful aging . Journal of Aging and Health , 12 , 470 – 489 . [DOI] [PubMed] [Google Scholar]
- Fowler M. J . ( 2008. ). Microvascular and macrovascular complications of diabetes . Clinical Diabetes , 26 , 77 – 82 . doi: 10.2337/diaclin.26.2.77 [Google Scholar]
- Frayne S. M. Phibbs C. S. Saechao F. Maisel N. C. Friedman S. A. Finlay A. , … Haskell S . ( 2014. ). Sourcebook: Women Veterans in the Veterans health administration. Volume 3. Sociodemographics, utilization, costs of care, and health profile . Washington, DC: : Women’s Health Evaluation Initiative, Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs; . [Google Scholar]
- Greenland S. , & Neutra R . ( 1980. ). Control of confounding in the assessment of medical technology . International Journal of Epidemiology , 9 , 361 – 367 . [DOI] [PubMed] [Google Scholar]
- Gregg E. W. Beckles G. L. Williamson D. F. Leveille S. G. Langlois J. A. Engelgau M. M. , & Narayan K. M . ( 2000. ). Diabetes and physical disability among older U.S. adults . Diabetes Care , 23 , 1272 – 1277 . doi: 10.2337/diacare.23.9.1272 [DOI] [PubMed] [Google Scholar]
- Gregg E. W. Mangione C. M. Cauley J. A. Thompson T. J. Schwartz A. V. Ensrud K. E. , & Nevitt M. C . ( 2002. ). Diabetes and incidence of functional disability in older women . Diabetes Care , 25 , 61 – 67 . doi: 10.2337/diacare.25.1.61 [DOI] [PubMed] [Google Scholar]
- Hernán M. A. Hernández-Díaz S. Werler M. M. , & Mitchell A. A . ( 2002. ). Causal knowledge as a prerequisite for confounding evaluation: An application to birth defects epidemiology . American Journal of Epidemiology , 155 , 176 – 184 . doi: 10.1093/aje/155.2.176 [DOI] [PubMed] [Google Scholar]
- Jackson J. M. DeFor T. A. Crain A. L. Kerby T. J. Strayer L. S. Lewis C. E. , … Margolis K. L . ( 2014. ). Validity of diabetes self-reports in the Women’s Health Initiative . Menopause , 21 , 861 – 868 . doi: 10.1097/gme.0000000000000189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janghorbani M. Van Dam R. M. Willett W. C. , & Hu F. B . ( 2007. ). Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture . American Journal of Epidemiology , 166 , 495 – 505 . doi: 10.1093/aje/kwm106 [DOI] [PubMed] [Google Scholar]
- Joish V. N. Malone D. C. Wendel C. Draugalis J. R. , & Mohler M. J . ( 2005. ). Development and validation of a diabetes mellitus severity index: A risk-adjustment tool for predicting health care resource use and costs . Pharmacotherapy , 25 , 676 – 684 . [DOI] [PubMed] [Google Scholar]
- Kalyani R. R. Saudek C. D. Brancati F. L. , & Selvin E . ( 2010. ). Association of diabetes, comorbidities, and A1C with functional disability in older adults: Results from the National Health and Nutrition Examination Survey (NHANES), 1999-2006 . Diabetes Care , 33 , 1055 – 1060 . doi: 10.2337/dc09-1597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon J. G. Lehavot K. Simpson T. L. Williams E. C. Barnett S. B. Grossbard J. R. , … Reiber G. E . ( 2015. ). Adverse childhood experiences, military service, and adult health . American Journal of Preventive Medicine , 49 , 573 – 582 . doi: 10.1016/j.amepre.2015.03.020 [DOI] [PubMed] [Google Scholar]
- Kerr E. A. Heisler M. Krein S. L. Kabeto M. Langa K. M. Weir D. , & Piette J. D . ( 2007. ). Beyond comorbidity counts: How do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? Journal of General Internal Medicine , 22 , 1635 – 1640 . doi: 10.1007/s11606-007-0313-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K. Hoerster K. D. Nelson K. M. Jakupcak M. , & Simpson T. L . ( 2012. ). Health indicators for military, veteran, and civilian women . American Journal of Preventive Medicine , 42 , 473 – 480 . doi: 10.1016/j.amepre.2012.01.006 [DOI] [PubMed] [Google Scholar]
- Lifford K. L. Curhan G. C. Hu F. B. Barbieri R. L. , & Grodstein F . ( 2005. ). Type 2 diabetes mellitus and risk of developing urinary incontinence . Journal of the American Geriatrics Society , 53 , 1851 – 1857 . doi: 10.1111/j.1532-5415.2005.53565.x [DOI] [PubMed] [Google Scholar]
- Loke Y. K. Singh S. , & Furberg C. D . ( 2009. ). Long-term use of thiazolidinediones and fractures in type 2 diabetes: A meta-analysis . Canadian Medical Association Journal , 180 , 32 – 39 . doi: 10.1503/cmaj.080486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchsinger J. A . ( 2012. ). Type 2 diabetes and cognitive impairment: Linking mechanisms . Journal of Alzheimer’s Disease , 30 , S185 – S198 . doi: 10.3233/JAD-2012–111433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugtenberg M. Burgers J. S. Clancy C. Westert G. P. , & Schneider E. C . ( 2011. ). Current guidelines have limited applicability to patients with comorbid conditions: A systematic analysis of evidence-based guidelines . PLoS One , 6 , e25987 . doi: 10.1371/journal.pone.0025987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch C. P. Gebregziabher M. Zhao Y. Hunt K. J. , & Egede L. E . ( 2014. ). Impact of medical and psychiatric multi-morbidity on mortality in diabetes: Emerging evidence . BMC Endocrine Disorders , 14 , 68 . doi: 10.1186/1472-6823-14-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddigan S. L. Feeny D. H. , & Johnson J. A . ( 2005. ). Health-related quality of life deficits associated with diabetes and comorbidities in a Canadian National Population Health Survey . Quality of Life Research , 14 , 1311 – 1320 . doi: 10.1007/s11136-004-6640-4 [DOI] [PubMed] [Google Scholar]
- Marchesini G. Forlani G. Cerrelli F. Manini R. Natale S. Baraldi L. , … Melchionda N . ( 2004. ). WHO and ATPIII proposals for the definition of the metabolic syndrome in patients with Type 2 diabetes . Diabetic Medicine , 21 , 383 – 387 . doi: 10.1111/j.1464-5491.2004.01115.x [DOI] [PubMed] [Google Scholar]
- Margolis K. L. Lihong Q. Brzyski R. Bonds D. E. Howard B. V. Kempainen S. , … Phillips L. S . ( 2008. ). Validity of diabetes self-reports in the Women’s Health Initiative: Comparison with medication inventories and fasting glucose measurements . Clinical Trials , 5 , 240 – 247 . doi: 10.1177/1740774508091749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maty S. C. Fried L. P. Volpato S. Williamson J. Brancati F. L. , & Blaum C. S . ( 2004. ). Patterns of disability related to diabetes mellitus in older women . The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences , 59 , 148 – 153 . doi: 10.1093/gerona/59.2.M148 [DOI] [PubMed] [Google Scholar]
- McEwen B. S . ( 2003. ). Interacting mediators of allostasis and allostatic load: Towards an understanding of resilience in aging . Metabolism , 52 ( Suppl. 2 ), 10 – 16 . doi: 10.1016/S0026-0495(03)00295-6 [DOI] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics . ( 2011. ). America’s women veterans: Military service history and VA benefit utilization statistics . Washington, DC: : National Center for Veterans Analysis and Statistics, Department of Veterans Affairs; . [Google Scholar]
- Nouwen A. Winkley K. Twisk J. Lloyd C. E. Peyrot M. Ismail K. , & Pouwer F . ( 2010. ). Type 2 diabetes mellitus as a risk factor for the onset of depression: A systematic review and meta-analysis . Diabetologia , 53 , 2480 – 2486 . doi: 10.1007/s00125-010-1874-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette J. D. , & Kerr E. A . ( 2006. ). The impact of comorbid chronic conditions on diabetes care . Diabetes Care , 29 , 725 – 731 . doi: 10.2337/diacare.29.03.06.dc05-2078 [DOI] [PubMed] [Google Scholar]
- Reiber G. E. , & LaCroix A. Z. ( 2015. ). Special Supplement: Older women Veterans in the Women’s Health Initiative . The Gerontologist , 2015. doi: 10:1093/geront/gnv673 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rillamas-Sun E. LaCroix A. Z. Bell C. L. Ryckman K. K. Ockene J. K. , & Wallace R. B. (in press). The impact of multimorbidity and coronary disease comorbidity on physical function in women aged 80 and older: The Women’s Health Initiative . Journals of Gerontology, Series A: Biological Sciences and Medical Sciences . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins J. M . ( 2001. ). Data, design, and background knowledge in etiologic inference . Epidemiology , 12 , 313 – 320 . [DOI] [PubMed] [Google Scholar]
- Rosland A. M. Nelson K. Sun H. Dolan E. D. Maynard C. Bryson C. , … Schectman G . ( 2013. ). The Patient-Centered Medical Home in the Veterans Health Administration . The American Journal of Managed Care , 19 , e263 – e272 . [PubMed] [Google Scholar]
- Rothman K. J. , & Greenland S . ( 1998. ). Precision and validity in epidemiologic studies . In Rothman K. J., Greenland S. (Eds.), Modern epidemiology ( 2 nd ed., pp. 120 – 125 ). Philadelphia, PA: : Lippincott-Raven; . [Google Scholar]
- Ryerson B. Tierney E. F. Thompson T. J. Engelgau M. M. Wang J. Gregg E. W. , & Geiss L. S . ( 2003. ). Excess physical limitations among adults with diabetes in the U.S. population, 1997-1999 . Diabetes Care , 26 , 206 – 210 . doi: 10.2337/diacare.26.1.206 [DOI] [PubMed] [Google Scholar]
- Sadler A. G. Booth B. M. Mengeling M. A. , & Doebbeling B. N . ( 2004. ). Life span and repeated violence against women during military service: Effects on health status and outpatient utilization . Journal of Women’s Health , 13 , 799 – 811 . doi: 10.1089/jwh.2004.13.799 . [DOI] [PubMed] [Google Scholar]
- Schett G. Kleyer A. Perricone C. Sahinbegovic E. Iagnocco A. Zwerina J. , … Kiechl S . ( 2013. ). Diabetes is an independent predictor for severe osteoarthritis: Results from a longitudinal cohort study . Diabetes Care , 36 , 403 – 409 . doi: 10.2337/dc12-0924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz A. V. Hillier T. A. Sellmeyer D. E. Resnick H. E. Gregg E. Ensrud K. E. , … Cummings S. R . ( 2002. ). Older women with diabetes have a higher risk of falls: A prospective study . Diabetes Care , 25 , 1749 – 1754 . doi: 10.2337/diacare.25.10.1749 [DOI] [PubMed] [Google Scholar]
- Schwartz A. V. Vittinghoff E. Sellmeyer D. E. Feingold K. R. de Rekeneire N. Strotmeyer E. S. , … Harris T. B . ( 2008. ). Diabetes-related complications, glycemic control, and falls in older adults . Diabetes Care , 31 , 391 – 396 . doi: 10.2337/dc07-1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T. E. , & Crimmins E . ( 2001. ). Social environment effects on health and aging: Integrating epidemiologic and demographic approaches and perspectives . Annals of the New York Academy of Sciences , 954 , 88 – 117 . doi: 10.1111/j.1749-6632.2001.tb02749.x [DOI] [PubMed] [Google Scholar]
- Segal M. W. Segal D. R. Bachman J. G. Freedman-Doan P. , & O’Malley P. M . ( 1998. ). Gender and the propensity to enlist in the U.S. military . Gender Issues , 16 , 65 – 87 . doi: 10.1007/s12147-998-0022-0 [Google Scholar]
- Stern A. Wolfe J. Daley J. Zaslavsky A. Roper S. F. , & Wilson K . ( 2000. ). Changing demographic characteristics of women veterans: Results from a national sample . Military Medicine , 165 , 773 – 780 . [PubMed] [Google Scholar]
- Struijs J. N. Baan C. A. Schellevis F. G. Westert G. P. , & van den Bos G. A . ( 2006. ). Comorbidity in patients with diabetes mellitus: Impact on medical health care utilization . BMC Health Services Research , 6 , 84 . doi: 10.1186/1472-6963-6-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh S. , & Kim K. W . ( 2011. ). Diabetes and cancer: Is diabetes causally related to cancer? Diabetes & Metabolism Journal , 35 , 193 – 198 . doi: 10.4093/dmj.2011.35.3.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomey K. Sowers M. R. Harlow S. Jannausch M. Zheng H. , & Bromberger J . ( 2010. ). Physical functioning among mid-life women: Associations with trajectory of depressive symptoms . Social Science & Medicine , 71 , 1259 – 1267 . doi: 10.1016/j.socscimed.2010.06.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpato S. Blaum C. Resnick H. Ferrucci L. Fried L. P. , & Guralnik J. M . ( 2002. ). Comorbidities and impairments explaining the association between diabetes and lower extremity disability: The Women’s Health and Aging Study . Diabetes Care , 25 , 678 – 683 . doi: 10.2337/diacare.25.4.678 [DOI] [PubMed] [Google Scholar]
- Volpato S. Ferrucci L. Blaum C. Ostir G. Cappola A. Fried L. P. , … Guralnik J. M . ( 2003. ). Progression of lower-extremity disability in older women with diabetes: The Women’s Health and Aging Study . Diabetes Care , 26 , 70 – 75 . doi: 10.2337/diacare.26.1.70 [DOI] [PubMed] [Google Scholar]
- Ware J. E. Snow K. K. Kosinski M. , & Gandek B . ( 1993. ). SF-36 health survey: Manual and interpretation guide . Boston, MA: : The Health Institute, New England Medical Center; . [Google Scholar]
- Weitlauf J. C. Lacroix A. Z. Bird C. E. Woods N. F. Washington D. L. Katon J. G. , … Stefanick M. L . ( 2015. ). Prospective analysis of health and mortality risk in Veteran and non-Veteran participants in the Women’s Health Initiative . Women’s Health Issues , 25 , 648 – 656 . doi: 10.1016/j.whi.2015.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcoxon F . ( 1945. ). Individual comparisons by ranking methods . Biometrics , 1 , 80 – 83 . doi: 10.2307/3001968 . [Google Scholar]
- Wolff J. L. Starfield B. , & Anderson G . ( 2002. ). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly . Archives of Internal Medicine , 162 , 2269 – 2276 . doi: 10.1001/archinte.162.20.2269 [DOI] [PubMed] [Google Scholar]
- Wong H. K. Ong K. L. Cheung C.-L. , & Cheung B. M. Y . ( 2014. ). Utilization of glucose, blood pressure, and lipid lowering medications among people with type II diabetes in the United States, 1999–2010 . Annals of Epidemiology , 24 , 516 – 521 . e511 . doi: 10.1016/j.annepidem.2014.05.001 [DOI] [PubMed] [Google Scholar]
- Wray L. A. Ofstedal M. B. Langa K. M. , & Blaum C. S . ( 2005. ). The effect of diabetes on disability in middle-aged and older adults . The journals of gerontology, Series A: Biological Sciences and Medical Sciences , 60 , 1206 – 1211 . doi: 10.1093/gerona/60.9.1206 [DOI] [PubMed] [Google Scholar]
- Yaeger D. Himmelfarb N. Cammack A. , & Mintz J . ( 2006. ). DSM-IV diagnosed posttraumatic stress disorder in women veterans with and without military sexual trauma . Journal of General Internal Medicine , 21 ( Suppl. 3 ), S65 – S69 . doi: 10.1111/j.1525-1497.2006.00377.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.