Abstract
Purpose of the Study:
Trajectories of physical activity (PA) and sedentary time (ST) after military separation are likely important determinants of women’s health outcomes later in life, because low PA and high ST are known contributors to premature mortality risk. Our objective was to compare longitudinal trajectories of recreational PA and ST between Veteran and non-Veteran postmenopausal women from the Women’s Health Initiative (WHI).
Design and Methods:
Women Veteran ( n = 3,719) and non-Veteran ( n = 141,800) WHI participants were included. Self-reported participation in recreational PA, converted to metabolic equivalent (MET)-hours/week, was prospectively assessed over 8 years. Self-reported ST, defined as hours/day sitting or lying down, was collected at baseline and at Years 3 and 6. Generalized estimating equations were used to compare trajectories of PA and ST between Veterans and non-Veterans, adjusted for demographics and lifestyle behaviors.
Results:
Veterans had higher baseline PA than non-Veterans (13.2 vs 12.5 MET-hours/week, p = .03). PA declined for both groups, with a steeper decline among Veterans (change/visit year −0.19 vs −0.02 MET-hours/week; interaction p < .001). At baseline, Veterans and non-Veterans had similar levels of ST (107.2 vs 105.9 hours/week, p = 0.42). Over time, ST remained stable among Veterans but declined slightly among non-Veterans (change/visit year −0.19 vs −0.49 hours/week; interaction p = .01).
Implications:
The less favorable longitudinal trajectories of PA and ST we observed for women Veterans may contribute to worse health among these individuals later in life. Understanding barriers to enhancing PA and reducing ST in women Veterans could lead to more effective approaches to intervening on these health behaviors.
Keywords: Women Veterans, Health behavior, Physical activity, Sedentary lifestyle, Sedentary behavior, Health trajectory, Longitudinal Study, Postmenopausal
Concurrent with the growing participation of women in the U.S. military (with women now comprising 14% of the active duty force), there is increasing clinical practice, policy, and research attention to women Veterans’ health risks and outcomes ( Bastian, Bosworth, Washington, & Yano, 2013 ; Batuman et al., 2011 ; Bean-Mayberry et al., 2011 ; Defense Manpower Research, 2015 ; Washington, Farmer, Mor, Canning, & Yano, 2015 ). In population-based studies, active duty women had better physical health, whereas women Veterans had worse health, compared with non-Veteran civilian women ( Lehavot, Hoerster, Nelson, Jakupcak, & Simpson, 2012 ). Entry into the military requires a baseline level of physical fitness, and retention in the military requires maintenance of those standards ( Department of Defense, 2004 ). Even after military service, in cross-sectional studies, Veterans are more likely than non-Veterans to meet physical activity (PA) recommendations ( Littman, Forsberg, & Koepsell, 2009 ). However, both men and women Veterans often gain weight around the time of military discharge, and they have similar levels of obesity as non-Veterans ( Koepsell, Littman, & Forsberg, 2012 ; Littman, Jacobson, Boyko, Powell, & Smith, 2013 ). Development of obesity may signal an underlying decline in health behavior. It is unclear how changes in recreational PA and sedentary time (ST) may contribute to this trend among women Veterans. Though health behaviors of male Veterans have been studied in comparison with non-Veteran men, only limited evidence is available on women Veterans’ health behaviors compared with the general population ( Lehavot et al., 2012 ).
Inadequate PA and high levels of ST are distinct constructs that each independently contribute to premature mortality risk ( Seguin et al., 2014 ; Owen, Healy, Matthews, & Dunstan, 2010 ). However, in combination, the risk is augmented, with the highest cardiovascular disease risk being in inactive women (≤1.7 metabolic equivalent [MET]-hours/week) who spend 10 or more hours per day sitting ( Chomistek et al., 2013 ). Maintaining a physically active lifestyle and decreasing ST is a U.S. disease prevention and health promotion guideline (U.S. Department of Health and Human Services [DHHS], 2008). Trajectories toward a healthier lifestyle may be associated with cumulative long-term health benefits. For example, older adults who commence moderate-intensity PA have reduced rates of major mobility disability ( Pahor et al., 2014 ). Conversely, trajectories toward less healthy lifestyle behaviors may be associated with increased long-term adverse effects. Some groups are less physically active than others; for example, 43% of U.S. women in contrast to 52% of U.S. men meet PA guidelines (Centers for Disease Control and Prevention, 2014). Little is known about maintenance of PA or development of ST among women Veterans after military service has ended. We hypothesize that women Veterans may follow more adverse PA and ST trajectories compared with non-Veterans, related to the compounding physical and mental health effects of military service. Characterizing and contrasting these trajectories may inform our understanding of relationships among Veteran status, health risks, and health outcomes.
The primary objective of this article is to address the question of whether postmenopausal women Veterans and non-Veterans differ in their longitudinal trajectories of recreational PA and of ST. To better understand how PA and ST varies with age, our secondary objective is to compare baseline PA and ST as a function of age and Veteran status.
Conceptual Framework
The biopsychosocial model of health and aging ( Seeman & Crimmins, 2001 ) is the conceptual framework that guided our examination of health behavior trajectories by Veteran status. That model describes a dynamic array of factors that influence life course trajectories of health. It suggests that aging well is related to macrolevel physical and sociocultural factors, and individual attributes of demographic characteristics (e.g., age, race/ethnicity, education, and income), life course experiences (including military experiences), social relationships and challenges (represented by social support measures), and health behavior practices (e.g., diet quality and tobacco use). In the model, chronic diseases and conditions are in the causal pathway toward aging well and health services outcomes. LaCroix and Reiber (in press) adapted this model by incorporating military service corollaries to the individual attributes of the original model, in order to highlight unique influences on aging well and health services outcomes for women Veterans ( Supplementary Figure 1 ). A 2011 systematic review on the health effects of military service on women Veterans describes the scientific literature that supports inclusion of these life course experiences of military service exposures and stressors ( Batuman et al., 2011 ). Veteran status, therefore, serves as a proxy for known military-related exposures such as combat and physical injury, stressors such as military sexual trauma, and potentially mutable Veteran-associated characteristics that predict health behavior trajectories ( Hoggatt, Williams, Der-Martirosian, Yano, & Washington, 2015 ; Washington, Bean-Mayberry, Hamilton, Cordasco, & Yano, 2013 ; Washington et al., 2015 ).
Design and Methods
To address the objectives, we utilized data from the Women’s Health Initiative (WHI), a longitudinal study on the determinants of health and disease among postmenopausal women aged 50–79 years at recruitment. Participants were recruited from 40 clinical centers around the United States between 1993 and 1998 for the observational study (OS) or for one or more randomized clinical trials (CTs). Details on recruitment and eligibility criteria for each study component have been described in detail elsewhere ( Hays et al., 2003 ; Women’s Health Initiative Study Group, 1998).
The main study collected data on 161,808 CT and OS participants until 2005. Participant data were collected via self-administered forms, interviews (in-person or by telephone), and in-person clinical measurements (e.g., blood pressure, height, weight, grip strength, and clinical breast examination) by trained staff at the Clinical Centers. Frequency of data collection and the specific information collected varied by study enrollment (Women’s Health Initiative Study Group, 1998).
Study Variables
Veteran Status
Veteran status was defined based on responses to the question, “Have you served in the U.S. armed forces on active duty for a period of 180 days or more?” Women responding “yes” were classified as Veterans and those responding “no” as non-Veterans. Women with a missing response ( n = 16,287) were excluded from analyses.
Physical Activity and Sedentary Time
Recreational PA was assessed with a validated self-reported questionnaire ( Meyer, Evenson, Morimoto, Siscovick, & White, 2009 ). The questionnaire asked about walking behaviors, including the frequency of walking outside the home for more than 10 minutes without stopping, the average number of minutes walked per episode, and the usual speed of walking (miles per hour, mph). The questionnaire also solicited information on the number of episodes per week and duration per episode of strenuous or very hard exercise (e.g., aerobics, jogging, tennis, and swimming), moderate exercise (e.g., biking, calisthenics, and popular/folk dancing), and mild exercise (e.g., slow dancing, bowling, and golf). METs that reflect intensity of the activity were assigned to walking casually/strolling (<2 mph), average/normal walking (2–3 mph), fast (3–4 mph), and very fast walking (>4 mph) as 2.0, 3.0, 4.0, and 5.0 METs, respectively; and 3.0, 4.5, and 7.0 METs for mild, moderate, and strenuous or very hard exercise, respectively ( Ainsworth et al., 1993 ; Nguyen et al., 2013 ; The Women’s Health Initiative Study Group, 1998). Total weekly recreational PA was summarized as MET-hours per week by multiplying the number of hours per week performing each activity by the activity-specific MET value, and summing across all activities (hereafter referred to as “PA”). Among OS participants, PA was assessed at baseline and follow-up visit Years 3 through 8; for CT participants, it was assessed at baseline and follow-up visit Years 1, 3, 6, and 9.
ST was assessed only in OS participants at baseline and follow-up visit Years 3 and 6. Two questions contributed to the ST measure. Participants were asked about the number of hours spent sitting during a usual day and night (sitting component of measure) and were directed to include time spent sitting at work, sitting at the table eating, driving or riding in a car or bus, and sitting up watching TV or talking. In order to capture napping and watching TV while lying down, they were also asked about the number of hours in a usual day spent sleeping or lying down with their feet up (sleeping/lying down component of measure), including time spent sleeping or trying to sleep at night, napping, and lying down watching TV. For both questions, participants selected their responses from the categories <4, 4–5, 6–7, 8–9, 10–11, 12–13, 14–15, or 16+ hours. To examine ST as a continuous variable, first, for each component, we assigned the midpoint of each participants’ response category (e.g., assigning 4.5 to the category 4–5) and assigned discrete values of 2 and 16.5 hours for those reporting <4 or 16+ hours, respectively. Next, we calculated total ST by adding the sitting and the sleeping/lying down components for each participant, which has moderate test–retest reliability (intraclass correlation coefficient = .60; Schneider et al., 2014 ); we then multiplied by 7 to convert ST to units of hours per week.
Time typically spent sleeping each night over the last 4 weeks was assessed as an independent measure in OS participants at baseline and at Year 3 (sleep-only measure). Participants selected their responses from the categories 5 or less hours, 6 hours, 7 hours, 8 hours, 9 hours, or 10+ hours. We assigned values of 2.5 and 10.5 for those reporting ≤5 or 10+ hours, respectively. Because sleep time was not measured in all years, it could not be removed from the ST measure (which combines sitting plus sleeping/lying down). Sitting plus lying down time (sitting/lying down measure) was calculate by subtracting sleep-only time (converted to sleep-only time per week) from total ST.
Covariates
Informed by our conceptual framework, additional covariates of interest were for the domains of demographic characteristics, social relationships, and health characteristics and health behavior practices. Demographic and social relationship characteristics included baseline self-reported age; race/ethnicity; highest level of education; whether currently employed; annual income; and marital status. Baseline social support was examined using the 9-item Medical Outcomes Study social support questionnaire, which provides a total score from questions about four types of support: emotional/informational, affection, tangible, and positive social interaction ( Sherbourne & Stewart, 1991 ). The total ranges from 9 to 45 with higher scores indicating more social support.
Health characteristics and health behavior practices included smoking status. Baseline dietary intake was obtained with the self-reported WHI Food Frequency Questionnaire ( Patterson et al., 1999 ), from which overall diet quality was assessed with the Healthy Eating Index 2005, with a maximum of 100 reflecting optimal quality ( Guenther, Reedy, Krebs-Smith, & Reeve, 2008 ). Baseline body mass index (BMI) was calculated from measured height and weight. Historical PA reported at baseline was also of interest, which included dichotomous responses (no/yes) to questions about whether the participant engaged in strenuous or very hard exercise ≥3 times a week at ages 18, 35, and 50. Finally, study assignment was included as a covariate.
Data Analysis
We first examined the baseline characteristics separately for Veteran and non-Veteran WHI participants who had PA or ST available at baseline. We chose individual characteristics that are postulated by the conceptual model to influence PA and ST as variables for comparison ( Table 1 ). Baseline PA and ST categories were those used in prior WHI analyses, with PA categories corresponding to levels used in federal guidelines (e.g., with accumulating 150 minutes/week of moderate-intensity exercise—the minimum recommended by the federal government—being equivalent to at least 8.4 MET-hours/week; Elsawy & Higgins, 2010 ).
Table 1.
Baseline Demographic, Social Relationship and Health Behavioral Characteristics of Veteran and Non-Veteran Women in the Women’s Health Initiative
| Veterans | Non-Veterans | |||
|---|---|---|---|---|
| N a | % a | N a | % a | |
| Total | 3,719 | 100.0 | 141,800 | 100.0 |
| Age (years) | ||||
| 50–59 | 785 | 21.1 | 46,366 | 32.7 |
| 60–69 | 1,081 | 29.1 | 64,642 | 45.6 |
| 70–79 | 1,853 | 49.8 | 30,792 | 21.7 |
| Race/ethnicity | ||||
| American Indian/Alaskan Native | 25 | 0.7 | 606 | 0.4 |
| Asian/Pacific Islander | 46 | 1.2 | 3,986 | 2.8 |
| Black/African American | 263 | 7.1 | 12,873 | 9.1 |
| Hispanic/Latino | 86 | 2.3 | 5,671 | 4.0 |
| White | 3,239 | 87.1 | 116,616 | 82.2 |
| Unknown | 47 | 1.3 | 1,675 | 1.2 |
| Education | ||||
| Less than high school | 64 | 1.7 | 7,482 | 5.3 |
| High school diploma/GED | 379 | 10.2 | 24,225 | 17.1 |
| Some college or vocational/training school | 1,522 | 40.9 | 53,196 | 37.5 |
| College graduate or higher | 1,740 | 46.8 | 55,975 | 39.5 |
| Currently employed | ||||
| No | 2,712 | 72.9 | 88,258 | 62.2 |
| Yes | 995 | 26.8 | 52,909 | 37.3 |
| Income | ||||
| <$20,000 | 629 | 16.9 | 21,822 | 15.4 |
| $20,000 to <$50,000 | 1,728 | 46.5 | 58,777 | 41.5 |
| $50,000 to <$75,000 | 630 | 16.9 | 26,489 | 18.7 |
| $75,000+ | 527 | 14.2 | 25,310 | 17.8 |
| Insurance status | ||||
| None | 59 | 1.6 | 5,243 | 3.7 |
| Any | 3,640 | 97.9 | 135,766 | 95.7 |
| Marital status | ||||
| Never married | 381 | 10.2 | 6,061 | 4.3 |
| Divorced/separated | 686 | 18.4 | 22,709 | 16.0 |
| Widowed | 835 | 22.5 | 24,358 | 17.2 |
| Married/marriage-like relationship | 1,807 | 48.6 | 88,189 | 62.2 |
| Social support score b | ||||
| 9–17 | 134 | 3.6 | 3,504 | 2.5 |
| 18–26 | 499 | 13.4 | 14,576 | 10.3 |
| 27–35 | 1,031 | 27.7 | 37,440 | 26.4 |
| 36–44 | 1,457 | 39.2 | 61,096 | 43.1 |
| 45 | 483 | 13.0 | 21,447 | 15.1 |
| Smoking status | ||||
| Never | 1,631 | 43.9 | 71,573 | 50.5 |
| Former | 1,693 | 45.5 | 58,838 | 41.5 |
| Current | 317 | 8.5 | 9,552 | 6.7 |
| Healthy Eating Index 2005 quintiles c | ||||
| 1 (<57.9) | 716 | 19.3 | 27,848 | 19.6 |
| 2 (57.9 to <65.5) | 707 | 19.0 | 27,979 | 19.7 |
| 3 (65.5 to <71.5) | 725 | 19.5 | 28,213 | 19.9 |
| 4 (71.5 to <77.1) | 758 | 20.4 | 28,647 | 20.2 |
| 5 (77.1+) | 804 | 21.6 | 28,905 | 20.4 |
| Body Mass Index | ||||
| Underweight (BMI < 18.5kg/m 2 ) | 44 | 1.2 | 1,248 | 0.9 |
| Normal (BMI 18.5–24.9kg/m 2 ) | 1,247 | 33.5 | 48,639 | 34.3 |
| Overweight (BMI 25–29.9kg/m 2 ) | 1,321 | 35.5 | 48,523 | 34.2 |
| Obese (BMI ≥ 30kg/m 2 ) | 1,068 | 28.7 | 42,082 | 29.7 |
| Hard exercise ≥3 times/week at age 18 | ||||
| No | 1,548 | 41.6 | 73,696 | 52.0 |
| Yes | 2,036 | 54.7 | 62,546 | 44.1 |
| Hard exercise ≥3 times/week at age 35 | ||||
| No | 1,804 | 48.5 | 74,784 | 52.7 |
| Yes | 1,777 | 47.8 | 61,814 | 43.6 |
| Hard exercise ≥3 times/week at age 50 | ||||
| No | 2,142 | 57.6 | 86,111 | 60.7 |
| Yes | 1,473 | 39.6 | 51,737 | 36.5 |
| Physical activity (MET-hours/week) d | ||||
| Inactive (0 to 1.7) | 783 | 21.1 | 31,297 | 22.1 |
| Low (>1.7 to <8.4) | 997 | 26.8 | 39,838 | 28.1 |
| Medium (8.4 to <20) | 1,077 | 29.0 | 39,704 | 28.0 |
| High (20+) | 853 | 22.9 | 30,551 | 21.5 |
| Sedentary time (hours per week) | ||||
| 0 to 28 | 19 | 0.5 | 1,312 | 0.9 |
| >28 to <32 | 57 | 1.5 | 2,090 | 1.5 |
| 32 to 44 | 385 | 10.4 | 14,922 | 10.5 |
| 44+ | 1,806 | 48.6 | 66,372 | 46.8 |
| Study assignment | ||||
| Observational study | 2,302 | 61.9 | 85,607 | 60.4 |
| Estrogen-Alone intervention | 113 | 3.0 | 4,455 | 3.1 |
| Estrogen-alone control | 137 | 3.7 | 4,440 | 3.1 |
| Estrogen + progestin intervention | 204 | 5.5 | 6,955 | 4.9 |
| Estrogen + progestin control | 193 | 5.2 | 6,949 | 4.9 |
| Dietary modification intervention | 335 | 9.0 | 13,377 | 9.4 |
| Dietary modification control | 435 | 11.7 | 20,017 | 14.1 |
Notes: BMI = body mass index; GED = General Educational Development; MET = metabolic equivalent.
a Numbers may not add to totals or percents to 100 due to missing data.
b Range 9–45 with higher scores indicating more social support.
c Maximum 100, reflecting optimal diet quality.
d 150 minutes/week of exercise is equivalent to at least 8.4 MET-hours/week of physical activity.
We then examined the unadjusted average PA and ST at baseline among Veterans and non-Veterans. To assess whether there were differences between the groups in either of these baseline outcomes, we employed linear regression using robust standard error estimates with Veteran status as the exposure. Model estimates reflected mean differences in PA or ST in Veterans compared with non-Veterans. To determine the effect of age on the association of Veteran status and baseline PA and ST, we repeated the analyses including an interaction term between Veteran status and age modeled continuously. We used Wald tests of the interaction term to determine whether the cross-sectional association between age and the outcomes differed between Veterans and non-Veterans. To facilitate interpretation, we divided age at baseline by 5 to reflect changes in PA or ST per 5-year difference in age.
To examine longitudinal trajectories of PA and ST in Veterans and non-Veterans, we employed a generalized estimating equations (GEEs) approach to linear regression with robust standard error estimates ( Liang & Zeger, 1986 ; Zeger & Liang, 1986 ). GEE allows all observations to be included in an analysis even if a participant does not have data at all visit years. We used discrete visit year modeled linearly as the time variable for analyses with baseline as visit year zero, which imposes a linear change over time in the outcomes. We included an interaction between Veteran status and visit year to allow the trajectories in Veterans and non-Veterans to differ (e.g., to have different slopes). We examined Wald tests of the interaction terms to evaluate whether the trajectories differed between Veterans and non-Veterans. We obtained estimates of the average change in PA and ST per visit year for Veterans and non-Veterans, which reflected the slope of the trajectory. To determine whether a linear change over time was appropriate, we also modeled visit year nominally, which permitted the change in outcome from one visit year to another to vary over time (e.g., nonconstant slope) and graphically compared the results. Graphical examination of PA and of ST modeled nominally indicated that the patterns were consistent with a linear change over time in both Veterans and non-Veterans, therefore only the linear models are presented.
Sensitivity analyses were conducted to examine the effect of only sitting plus lying down time. This longitudinal trajectory that excluded sleep time extended only through Year 3.
We adjusted all analyses for baseline age (continuous), race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 score (continuous), BMI (continuous), and study assignment (nominal, for PA analysis only). For the analysis of ST, we also examined a model adjusted for whether the participant was employed (no/yes), which was assessed at baseline and visit Years 3 and 6 in the OS participants, and thus was treated as a time-varying covariate. Because it was not assessed in CT participants, we did not include employment as a covariate in PA analyses. Because incident chronic conditions may be in the causal pathways for both PA and ST, and physical function is a time-varying covariate that is correlated with these constructs ( Seguin et al., 2012 ), they were not included in the models.
Results
Sample Characteristics and Baseline PA and ST
Baseline characteristics of the 145,519 women comprising our analytic sample (Veterans n = 3,719; non-Veterans n = 141,800) are described in Table 1 . Veterans were older than non-Veterans and were more likely to be white, never married, a college graduate, currently not employed, current or former smokers, and to have previously participated in strenuous or very hard exercise 3 or more times/week. At baseline, approximately half of both Veterans (51.9%) and non-Veterans (49.5%) achieved PA levels of ≥8.4 MET-hours/week ( Table 1 ). Baseline ST was skewed toward >77 hours per week for both groups ( Table 1 ).
The mean level of PA at baseline was 13.2 MET-hours/week (standard deviation [ SD ] = 14.2) among Veterans and 12.5 MET-hours/week ( SD = 13.7) among non-Veterans ( Table 2 ). Veterans had 0.7 additional MET-hours/week of PA (95% confidence interval [CI] 0.24, 1.16) compared with non-Veterans in unadjusted analyses. After adjustment, the difference decreased to 0.53 MET-hours/week (95% CI 0.06, 1.01).
Table 2.
Baseline Differences in Physical Activity and Sedentary Time Between Veteran and Non-Veteran Women
| Veterans a | Non-Veterans a | Unadjusted | Adjusted b | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean ( SD ) | N | Mean ( SD ) | Diff | 95% CI | p Value | Diff | 95% CI | p Value | |
| Physical activity (MET-hours/week) | 3,278 | 13.2 (14.2) | 124,853 | 12.5 (13.7) | 0.70 | (0.24, 1.16) | .003 | 0.53 | (0.06, 1.01) | .03 |
| Sedentary time (hours/week) c | 1,992 | 107.2 (28.4) | 74,064 | 105.9 (29.2) | 1.08 | (−0.12, 2.28) | .08 | 0.51 | (−0.73, 1.76) | .42 |
Notes: BMI = body mass index; CI = confidence interval; Diff = difference; MET = metabolic equivalent; SD = standard deviation.
a Numbers and means reflect those from adjusted analyses.
b Adjusted for age (continuous), race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), BMI (continuous), and study assignment (nominal; for physical activity only).
c Among Observational Study participants only.
The mean amount of ST at baseline was 107.2 hours/week ( SD = 28.4) among Veterans and 105.9 hours/week (SD=29.2) among non-Veterans ( Table 2 ). In unadjusted comparisons, Veterans had slightly greater ST, but the difference was not statistically significant (difference = 1.08, 95% CI −0.12, 2.28). After adjustment, the difference was attenuated (difference = 0.51, 95% CI −0.73, 1.76). In the sensitivity analyses that examined sitting plus lying down time, results were similar, with no differences between Veterans and non-Veterans (adjusted difference 0.52; 95% CI −0.76, 1.79; Supplementary Table 1 ).
Age Differences in Baseline PA and ST
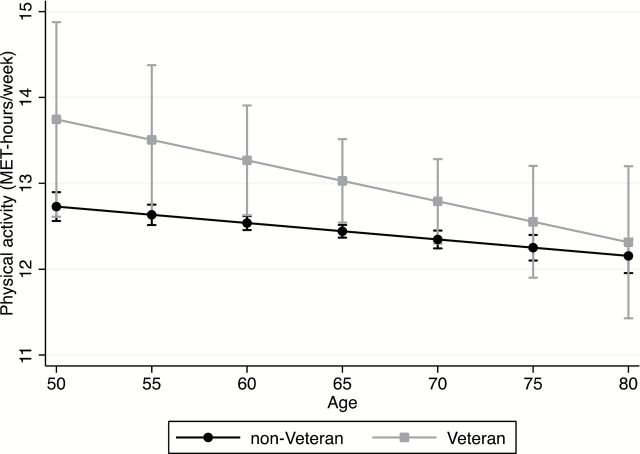
Among non-Veterans, there was a statistically significant inverse association between baseline age and PA, such that older women reported less PA ( Table 3 ). Adjusting for demographic characteristics, social relationships, health behavior practices, and study arm, PA decreased by −0.10 MET-hours/week (95% CI −0.15, −0.04) among non-Veterans, for every 5-year increment in age. Among Veterans, the effect was more pronounced ( Figure 1 ; difference per 5 years of age −0.24); however, the estimate did not reach statistical significance (95% CI −0.52, 0.06). There was no evidence that the relationship between baseline age and PA differed between Veterans and non-Veterans ( p value for interaction = .35).
Table 3.
Age Differences in Baseline Physical Activity and Sedentary Time Among Veteran and Non-Veteran Women
| Veterans | Non-Veterans | ||||||
|---|---|---|---|---|---|---|---|
| Difference per 5 years of age a | 95% CI | p Value | Difference per 5 years of age a | 95% CI | p Value | Interaction p value | |
| Physical activity (MET-hours/week) | −0.24 | (−0.54, 0.06) | .12 | −0.10 | (−0.15, −0.04) | <.001 | .35 |
| Sedentary time (hours/week) b | −0.16 | (−0.27, −0.05) | .004 | −0.17 | (−0.19, −0.15) | <.001 | .87 |
Notes: BMI = body mass index; CI = confidence interval; MET = metabolic equivalent.
a Adjusted for baseline race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), BMI (continuous), and study assignment (nominal; for physical activity only).
b Among Observational Study participants only.
Figure 1.
Association between baseline age and physical activity (metabolic equivalent-hours/week) among Veteran and non-Veteran women. Adjusted for baseline race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), body mass index (continuous), and study assignment. Error bars are 95% confidence intervals. p Value for interaction .35.
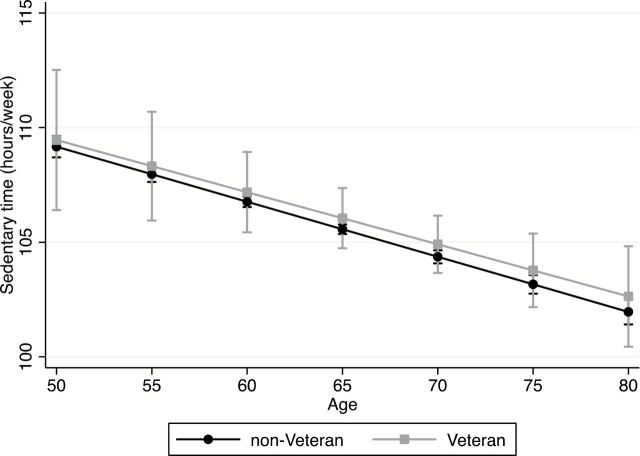
For ST at baseline, there was an inverse association between age and ST for both Veterans and non-Veterans, such that older women had less adjusted ST ( Figure 2 ). For every 5-year increment in age, ST decreased among non-Veterans by 0.17 hours per week (95% CI −0.19, −0.15), ( Table 3 ); the effect was similar in Veterans (difference = −0.16, 95% CI −0.27, −0.05). There was no evidence that the association with age differed between Veterans and non-Veterans ( p value for interaction = .87).
Figure 2.
Association between baseline age and sedentary time (hours/week) among Veteran and non-Veteran women. Adjusted for baseline race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), body mass index (continuous), and study assignment. p Value for interaction .87.
Trajectories in PA and ST
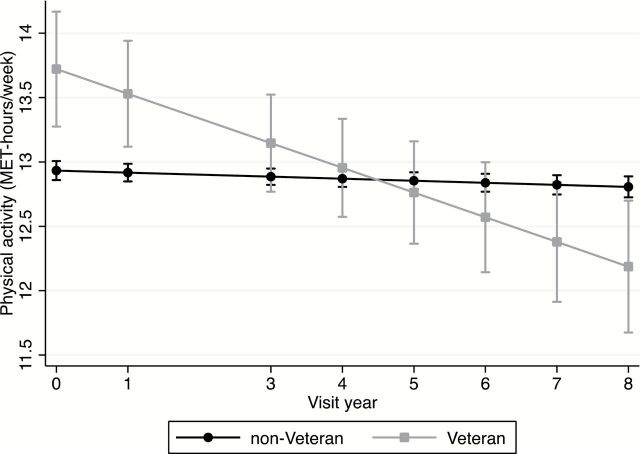
Trajectories in PA and in ST are described by Veteran status in Table 4 . After adjusting for demographic characteristics, social relationships, health behavior practices, and study arm, PA decreased by 0.02 MET-hours/week for each visit year in non-Veterans (95% CI −0.03, −0.005). In Veterans, the decline over time was more pronounced, with decreases of 0.19 MET-hours/week for each visit year (95% CI −0.27, −0.12). The difference in PA trajectories between Veterans and non-Veterans was statistically significant ( Figure 3 ; p value for interaction < .001).
Table 4.
Trajectories in Physical Activity and Sedentary Time Among Veteran and Non-Veteran Women
| Veterans | Non-Veterans | ||||||
|---|---|---|---|---|---|---|---|
| Change per visit year a | 95% CI | p Value | Change per visit year a | 95% CI | p Value | Interaction p value | |
| Physical activity (MET-hours/week) | −0.19 | (−0.27, −0.12) | <.001 | −.02 | (−0.03, −0.005) | .005 | <.001 |
| Sedentary time (hours/week) b | −0.19 | (−0.42, 0.03) | .09 | −.49 | (−0.53, −0.46) | <.001 | .01 |
Notes: BMI = body mass index; CI = confidence interval; MET = metabolic equivalent.
a Adjusted for baseline age (continuous), race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), BMI (continuous), and study assignment (nominal; for physical activity only).
b Among Observational Study participants only
Figure 3.
Trajectories of physical activity (metabolic equivalent-hours/week) among Veteran and non-Veteran women. Models were adjusted for baseline age (continuous), race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), body mass index (continuous), and study assignment. p Value for interaction <.001.
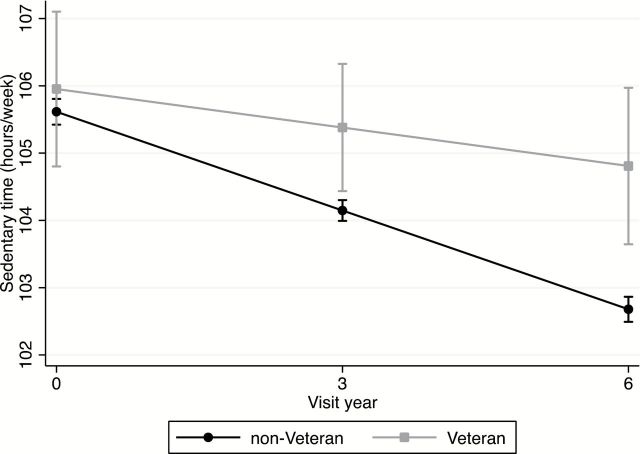
For ST trajectories, there was a decrease in adjusted ST of 0.49 hours/week for each visit year among non-Veterans (95% CI −0.53, −0.46). The decrease was less pronounced among Veterans, with a decline of 0.19 hours/week for each visit year, which was not significant (95% CI −0.42, 0.03). The difference in trajectories between Veterans and non-Veterans was significant ( Figure 4 ; p value for interaction = .01). When also adjusting for employment as a time-varying covariate, the declines per visit year in ST were less pronounced, but interpretations remained consistent (data not shown).
Figure 4.
Trajectories of sedentary time (hours/week) among Veteran and non-Veteran women. Models were adjusted for baseline age (continuous), race/ethnicity (non-white/white), education (ordinal), income (ordinal), marital status (nominal), social support (continuous), smoking status (nominal), Healthy Eating Index 2005 (continuous), body mass index (continuous), and study assignment. p Value for interaction .01.
When examining sitting plus lying down time ( Supplementary Table 2 ), compared with the longitudinal trajectories in ST, there were larger decreases per visit year in both Veterans (−0.66; 95% CI −1.10, −0.22) and non-Veterans (−0.92; 95% CI −0.99, −0.85) but there were no significant differences between Veterans and non-Veterans ( p value for interaction = .25).
Discussion
This study is one of the few longitudinal assessments of PA and ST in women Veterans. It sought to characterize women Veterans’ trajectories of these two behaviors and to contrast them against trajectories for the larger population of non-Veteran women in the national WHI cohort. We found that women Veterans developed more adverse PA trajectories than non-Veteran women, with women Veterans having an average decline in PA per visit year of 0.19 MET-hours/week. By contrast, earlier studies of women from the WHI OS found that recreational PA in postmenopausal women is stable over 8 years of follow-up ( Nguyen et al., 2013 ). The PA trajectory we described for non-Veteran women (an annual change of −0.02 MET-hours/week) is in keeping with that earlier study, however different than the temporal trends seen in population surveillance studies on older adults ( Brownson, Boehmer, & Luke, 2005 ).
There are several potential explanations for our findings. WHI was a select population that tended to be of higher socioeconomic status and healthier than the general population. The Veteran/non-Veteran differences we observed could be attributed to a true effect in a postmenopausal female population that is largely healthier than the general population (e.g., with half of the WHI cohort meeting PA recommendations in contrast to 43% of the general population). Alternately, it could be attributable to differences between women Veterans and non-Veterans that might not be as apparent in the general population that includes individuals in poorer health who likely did not have the early life health advantages of Veterans. Regardless of which is true, the findings suggest the need for additional longitudinal studies in other diverse cohorts of women with past military service to confirm these present findings, which suggest that women Veterans are particularly susceptible to PA declines over time.
The annual decline we observed in women Veterans’ PA is approximately similar in magnitude to the differences in level of PA at baseline that are associated with 5-year increases in age. Extrapolated over the 8-year follow-up period, that annual decline in PA is equivalent to a reduction of 1.5 MET-hours/week. From a population health perspective, modest deficits in health behavior such as this contribute to patterns of health determinants over the life course that have a cumulative negative impact on the health of the population, and modest increases in health behavior have a positive impact ( Kindig & Stoddart, 2003 ; Lloyd-Jones et al., 2010 ; Rose, 1981 ). For example, in the Nurses’ Health Study, among women who did not engage in vigorous exercise, those who expended approximately 1.7 MET-hour/week walking had 31% less age-adjusted risk of coronary events compared with those who expended 0 MET-hour/week ( Manson et al., 1999 ).
In contrast to their less favorable health behavior trajectories, women Veterans had more favorable baseline PA profiles compared with non-Veteran women. This is not surprising given the physical requirements for military service. Women Veterans were more likely to report that earlier in life they participated in hard exercise three or more times per week. However, these Veteran/non-Veteran differences narrowed from age 18 to age 50, which could potentially reflect the cumulative effects of active duty on disability. For example, in a 7-year longitudinal assessment of recently returning women Veterans in that age range, the prevalence of painful musculoskeletal conditions increased each year after deployment ( Haskell et al., 2012 ). At the time of WHI enrollment, Veterans had an adjusted 0.53 additional MET-hours/week of PA compared with non-Veterans, an advantage that dissipated by Year 5 of follow-up. Though women Veterans may have had a behavioral disposition toward PA earlier in life, our findings suggest that factors beyond behavioral disposition influenced Veterans after military service. A key question that future research should address is what the determinants of this trajectory are. In the general population, correlates of PA include environmental factors related to both physical and social environments and individual factors such as age and previous PA ( Bauman et al., 2012 ). Among U.S., Iraq, and Afghanistan Veterans, mental health and somatic symptom severity are associated with reduced PA ( Hoerster, Jakupcak, McFall, Unützer, & Nelson, 2012 ). Women Veterans differ from non-Veterans in having military exposures such as military sexual trauma, and having a higher prevalence of selected physical and mental health disorders ( Batuman, 2011 ; Bean-Mayberry, 2011 ; Lehavot et al., 2012 ). Future research should ascertain whether these or other modifiable characteristics of women Veterans are predictive of their decline in PA, and to what extent this influences healthy aging and clinical disease manifestations.
We found that at baseline Veterans and non-Veterans had similar levels of ST, with each group averaging over 15 hours/day of this behavior. Age at the time of study entry was inversely correlated with baseline ST, though it is unclear whether this is an artifact of including sleep time in the measure. There is sparse comparative data that found modestly higher ST with age ( Harvey, Chastin, & Skelton, 2013 ). As noted by Elsawy, the 2008 PA Guidelines for Americans advises older adults to avoid inactivity while striving to be as physically active as their abilities allow ( Elsawy & Higgins, 2010 ; U.S. DHHS, 2008). Despite this recommendation, our findings, similar to those of others, were notable for relatively few older adults achieving this recommended minimum ( Elsawy & Higgins, 2010 ; Shay et al., 2012 ). Over time, adjusting for differences in age, other demographic characteristics and lifestyle behaviors, Veterans developed a somewhat less favorable ST trajectory compared with non-Veterans, with ST declining among non-Veterans but remaining stable among Veterans. Adjusting for employment as a time-varying covariate attenuated the declines per visit year in ST. An understanding of the correlates of this trajectory may help inform preventive action. Prior research found that correlates of greater sitting time in a predominantly male Veteran cohort were depression symptoms, BMI, functional impairment, and self-rated health, whereas greater recreational PA and being employed were associated with less sitting time (Millstein et al., in press). It is possible that additional exposures and health conditions that are related to military service may be contributing to the less favorable trajectories for women Veterans.
Some limitations of the present study should be noted. PA and ST were each self-reported, and may have been subject to recall bias or to social desirability bias, and thus misclassification of either or both behavior. Our measure of ST was unable to distinguish between potentially health promoting ST (including sleep, social interactions, and intellectual engagement) and ST considered detrimental to health, though sensitivity analyses that excluded sleep time were similar to findings for ST. ST was calculated by adding the midpoint of several ranges, and this may have also contributed to measurement error. We did not have detailed information about women Veterans’ military service, and therefore could not ascertain the influence of specific military exposures on the trajectories that we described. Though WHI participants may not be entirely representative of the cross-section of women in the United States, and may also differ substantially from more recent war cohorts, the baseline characteristics of the WHI Veteran cohort are similar to that described for older women in the population-based National Survey of Women Veterans ( Der-Martirosian, Cordasco, & Washington, 2013 ; Washington et al., 2013 ; Washington et al., 2015 ). Strengths of this study include the prospective design, large size, high follow-up rate, and the detailed assessments of PA, ST, and potential confounding factors.
Implications
This study contributes to an understanding of the health risk profile of older women Veterans. The longitudinal declines in women Veterans’ PA that we found, coupled with their maintenance of high levels of ST, create an adverse health behavior trajectory for women Veterans that may explain in part the excess Veteran mortality risk that has been described in some studies of older women Veterans ( Cypel & Kang, 2008 ; Weitlauf et al., 2015 ). The biopsychosocial model of health and aging ( Seeman & Crimmins, 2001 ) as it relates to women Veterans (LaCroix & Reiber, 2015; Supplementary Figure 1 ) identifies mutable health behavior practices as contributors to aging well and achieving optimal health services outcomes. This model, while providing a framework for guiding our examination of health behavior trajectories by Veteran status, can also inform recommendations for clinical practice and research that stem from the findings. Our findings affirm the importance of initiation and maintenance of PA in older women, and the reduction of ST, as important health priorities. Initiatives such as the Exercise is Medicine ( American College of Sports Medicine, 2015 ), global health initiative to encourage healthcare providers to include PA when designing treatment plans for patients, could be incorporated into Veterans Health Administration (VA) and non-VA health care settings that care for women Veterans. Macrolevel physical and sociocultural factors are identified in the adapted biopsychosocial model of health and aging as foundational in providing the context for health behavior practices and for understanding military service experiences and other influences on aging well and outcomes. Applied to women Veterans, this suggests that embedding PA interventions and other health promotion activities into Veteran service organizations and community organizations with large Veteran constituencies may be useful strategies to reach and engage women Veterans (Belza & the PRC-HAN Physical Activity Conference Planning Workgroup, 2007; Centers for Disease Control and Prevention, 2011). The VA has model programs at some sites aimed at increasing PA in the older individuals; future research should evaluate the reach of these programs, their effectiveness, and factors impacting wider implementation.
The health behavior trajectories we reported on were likely established well before women entered the WHI study. Therefore, interventions to monitor, promote, and maintain PA in women Veterans should be aimed at both older women Veterans and younger women Veterans who are earlier in their life course trajectories. In summary, increasing efforts by VA and other Veteran service organization to promote activity among women Veterans will have a substantial public health impact, potentially addressing their excess functional limitations, morbidity, and mortality ( Lehavot et al., 2012 ).
Funding
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201 100003C, HHSN268201100004C, and HHSN271201100004C.
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, MD) Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller
Clinical Coordinating Center: Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg
Investigators and Academic Centers: (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
For a list of all investigators who have contributed to the WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
This research was also supported by Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service FOP14-439 and the VA Office of Women’s Health.
Supplementary Material
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- Ainsworth B. E., Haskell W. L., Leon A. S., Jacobs D. R., Jr, Montoye H. J., Sallis J. F., Paffenbarger R. S., Jr . ( 1993. ). Compendium of physical activities: Classification of energy costs of human physical activities . Medicine and Science in Sports and Exercise , 25 , 71 – 80 . [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine . ( 2015. ). Exercise is medicine . Indianapolis, IN: : American College of Sports Medicine; . Retrieved from http:exerciseismedicine.org [Google Scholar]
- Bastian L. A. Bosworth H. B. Washington D. L. , & Yano E. M . ( 2013. ). Setting the stage: Research to inform interventions, practice and policy to improve women Veterans’ health and health care . Journal of General Internal Medicine , 28 ( Suppl. 2 ), S491 – S494 . doi: 10.1007/s11606-013-2470-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batuman F. Bean-Mayberry B. Goldzweig C. Huang C. Miake-Lye I. M. Washington D. L. , … Shekelle P. G . ( 2011. ) Health Effects of Military Service on Women Veterans (VA Evidence-based Synthesis Program Reports #05-226) . Washington, DC: : Department of Veterans Affairs; . [PubMed] [Google Scholar]
- Bauman A. E., Reis R. S., Sallis J. F., Wells J. C., Loos R. J., Martin B. W .; Lancet Physical Activity Series Working Group . ( 2012. ). Correlates of physical activity: Why are some people physically active and others not? Lancet (London, England) , 380 , 258 – 271 . doi: 10.1016/S0140-6736(12)60735-1 [DOI] [PubMed] [Google Scholar]
- Bean-Mayberry B. Yano E. M. Washington D. L. Goldzweig C. Batuman F. Huang C. … Shekelle P. G . ( 2011. ). Systematic review of women veterans’ health: Update on successes and gaps . Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health , 21 ( 4 Suppl .), S84 – S97 . doi: 10.1016/j.whi.2011.04.022 [DOI] [PubMed] [Google Scholar]
- Belza & the PRC-HAN Physical Activity Conference Planning Workgroup . ( 2007. ). Moving ahead: Strategies and tools to plan, conduct, and maintain effective community-based physical activity programs for older adults . Atlanta, GA: : Centers for Disease Control and Prevention; . [Google Scholar]
- Brownson R. C., Boehmer T. K., Luke D. A . ( 2005. ). Declining rates of physical activity in the United States: What are the contributors? Annual Review of Public Health , 26 , 421 – 443 . doi: 10.1146/annurev.publhealth.26.021304.144437 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . ( 2011. ). Strategies to prevent obesity and other chronic diseases: The CDC guide to strategies to increase physical activity in the community . Atlanta, GA: : U.S. Department of Health and Human Services; . [Google Scholar]
- Centers for Disease Control and Prevention . ( 2014. ). Facts about physical activity . Atlanta, GA: : U.S. Department of Health and Human Services; . Retrieved from http://www.cdc.gov/physicalactivity/data/facts.html [Google Scholar]
- Chomistek A. K. Manson J. E. Stefanick M. L. Lu B. Sands-Lincoln M. Going S. B. … Eaton C. B . ( 2013. ). Relationship of sedentary behavior and physical activity to incident cardiovascular disease: Results from the Women’s Health Initiative . Journal of the American College of Cardiology , 61 , 2346 – 2354 . doi: 10.1016/j.jacc.2013.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cypel Y., Kang H . ( 2008. ). Mortality patterns among women Vietnam-era veterans: Results of a retrospective cohort study . Annals of Epidemiology , 18 , 244 – 252 . doi: 10.1016/j.annepidem.2007.11.009 [DOI] [PubMed] [Google Scholar]
- Defense Manpower Research . ( 2015. ). Demographics of Active Duty U.S. Military . April 12, 2015. Retrieved from http://www.statisticbrain.com/demographics-of-active-duty-u-s-military/ . Accessed April 27, 2015 .
- Department of Defense . ( 2004. ). Department of Defense Physical Fitness and Body Fat Program Procedures (Directive Number 1308.1) . Washington, DC: : Department of Defense; . [Google Scholar]
- Der-Martirosian C., Cordasco K. M., Washington D. L . ( 2013. ). Health-related quality of life and comorbidity among older women veterans in the United States . Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation , 22 , 2749 – 2756 . doi: 10.1007/s11136-013-0424-7 [DOI] [PubMed] [Google Scholar]
- Elsawy B., Higgins K. E . ( 2010. ). Physical activity guidelines for older adults . American Family Physician , 81 , 55 – 59 . [PubMed] [Google Scholar]
- Guenther P. M. Reedy J. Krebs-Smith S. M. , & Reeve B. B . ( 2008. ). Evaluation of the Healthy Eating Index-2005 . Journal of General Internal Medicine , 108 , 1854 – 1864 . doi: 10.1016/j.jada.2008.08.011 [DOI] [PubMed] [Google Scholar]
- Haskell S. G., Ning Y., Krebs E., Goulet J., Mattocks K., Kerns R., Brandt C . ( 2012. ). Prevalence of painful musculoskeletal conditions in female and male veterans in 7 years after return from deployment in Operation Enduring Freedom/Operation Iraqi Freedom . The Clinical Journal of Pain , 28 , 163 – 167 . doi: 10.1097/AJP.0b013e318223d951 [DOI] [PubMed] [Google Scholar]
- Harvey J. A., Chastin S. F., Skelton D. A . ( 2013. ). Prevalence of sedentary behavior in older adults: A systematic review . International Journal of Environmental Research and Public Health , 10 , 6645 – 6661 . doi: 10.3390/ijerph10126645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays J. Hunt J. R. Hubbell F. A. Anderson G. L. Limacher M. Allen C. , & Rossouw J. E . ( 2003. ). The Women's Health Initiative recruitment methods and results . Annals of Epidemiology , 13 , S18 – S77 . doi: 10.1016/S1047-2797(03)00042-5 [DOI] [PubMed] [Google Scholar]
- Hoerster K. D., Jakupcak M., McFall M., Unützer J., Nelson K. M . ( 2012. ). Mental health and somatic symptom severity are associated with reduced physical activity among US Iraq and Afghanistan veterans . Preventive Medicine , 55 , 450 – 452 . doi: 10.1016/j.ypmed.2012.08.017 [DOI] [PubMed] [Google Scholar]
- Hoggatt K. J., Williams E. C., Der-Martirosian C., Yano E. M., Washington D. L . ( 2015. ). National prevalence and correlates of alcohol misuse in women veterans . Journal of Substance Abuse Treatment , 52 , 10 – 16 . doi: 10.1016/j.jsat.2014.12.003 [DOI] [PubMed] [Google Scholar]
- Kindig D., Stoddart G . ( 2003. ). What is population health? American Journal of Public Health , 93 , 380 – 383 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koepsell T. D., Littman A. J., Forsberg C. W . ( 2012. ). Obesity, overweight, and their life course trajectories in veterans and non-veterans . Obesity (Silver Spring, Md.) , 20 , 434 – 439 . doi: 10.1038/oby.2011.2 [DOI] [PubMed] [Google Scholar]
- LaCroix A. Z., Reiber G . ( 2015. ). Older women Veterans in the Women’s Health Initiative . The Gerontologist . Advanced online publication. doi:10:1093/geront/gnv673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K., Hoerster K. D., Nelson K. M., Jakupcak M., Simpson T. L . ( 2012. ). Health indicators for military, veteran, and civilian women . American Journal of Preventive Medicine , 42 , 473 – 480 . doi: 10.1016/j.amepre.2012.01.006 [DOI] [PubMed] [Google Scholar]
- Liang K. Y. , & Zeger S. L . ( 1986). Longitudinal data analysis using generalized linear models . Biometrika , 73 , 13 – 22 . [Google Scholar]
- Littman A. J., Forsberg C. W., Koepsell T. D . ( 2009. ). Physical activity in a national sample of veterans . Medicine and Science in Sports and Exercise , 41 , 1006 – 1013 . doi: 10.1249/MSS.0b013e3181943826 [DOI] [PubMed] [Google Scholar]
- Littman A. J., Jacobson I. G., Boyko E. J., Powell T. M., Smith T. C .; Millennium Cohort Study Team . ( 2013. ). Weight change following US military service . International Journal of Obesity (2005) , 37 , 244 – 253 . doi: 10.1038/ijo.2012.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Jones D. M. Hong Y. Labarthe D. Mozaffarian D. Appel L. J. Van Horn L. … Rosamond W. D . ( 2010. ). Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond . Circulation , 121 , 586 – 613 . doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- Manson J. E. Hu F. B. Rich-Edwards J. W. Colditz G. A. Stampfer M. J. Willett W. C. … Hennekens C. H . ( 1999. ). A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women . The New England Journal of Medicine , 341 , 650 – 658 . doi: 10.1056/NEJM199908263410904 [DOI] [PubMed] [Google Scholar]
- Meyer A. M., Evenson K. R., Morimoto L., Siscovick D., White E . ( 2009. ). Test-retest reliability of the Women’s Health Initiative physical activity questionnaire . Medicine and Science in Sports and Exercise , 41 , 530 – 538 . doi: 10.1249/MSS.0b013e31818ace55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millstein R. A. Hoerster K. D. Rosenberg D. E. Nelson K. M. Reiber G. , & Saelens B. E . (in press). Individual, social, and neighborhood associations with sitting time among Veterans . Journal of Physical Activity & Health . [DOI] [PubMed] [Google Scholar]
- Nguyen H. Q. Herting J. R. Kohen R. Perry C. K. LaCroix A. Adams-Campbell L. L. … Tinker L . ( 2013. ). Recreational physical activity in postmenopausal women is stable over 8 years of follow-up . Journal of Physical Activity & Health , 10 , 656 – 668 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen N., Healy G. N., Matthews C. E., Dunstan D. W . ( 2010. ). Too much sitting: The population health science of sedentary behavior . Exercise and Sport Sciences Reviews , 38 , 105 – 113 . doi: 10.1097/JES.0b013e3181e373a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahor M. Guralnik J. M. Ambrosius W. T. Blair S. Bonds D. E. Church T. S. , … Williamson J. D . ( 2014. ). Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial . The Journal of the American Medical Association , 311 , 2387 – 2396 . doi: 10.1001/jama.2014.5616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson R. E., Kristal A. R., Tinker L. F., Carter R. A., Bolton M. P., Agurs-Collins T . ( 1999. ). Measurement characteristics of the Women’s Health Initiative food frequency questionnaire . Annals of Epidemiology , 9 , 178 – 187 . [DOI] [PubMed] [Google Scholar]
- Rose G . ( 1981. ). Strategy of prevention: Lessons from cardiovascular disease . British Medical Journal (Clinical research ed.) , 282 , 1847 – 1851 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider K. L. Andrews C. Hovey K. M. Seguin R. A. Manini T. Lamonte M. J. … Pagoto S. L . ( 2014. ). Change in physical activity after a diabetes diagnosis: Opportunity for intervention . Medicine and Science in Sports and Exercise , 46 , 84 – 91 . doi: 10.1249/MSS.0b013e3182a33010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T. E., Crimmins E . ( 2001. ). Social environment effects on health and aging: Integrating epidemiologic and demographic approaches and perspectives . Annals of the New York Academy of Sciences , 954 , 88 – 117 . [DOI] [PubMed] [Google Scholar]
- Seguin R. Buchner D. M. Liu J. Allison M. Manini T. Wang C. Y. … Lacroix A. Z . ( 2014. ). Sedentary behavior and mortality in older women: The Women’s Health Initiative . American Journal of Preventive Medicine , 46 , 122 – 135 . doi: 10.1016/j.amepre.2013.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seguin R. Lamonte M. Tinker L. Liu J. Woods N. Michael Y. L. … Lacroix A. Z . ( 2012. ). Sedentary behavior and physical function decline in older women: Findings from the Women’s Health Initiative . Journal of Aging Research , 2012 , 271589 . doi: 10.1155/2012/271589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay C. M. Ning H. Allen N. B. Carnethon M. R. Chiuve S. E. Greenlund K. J. … Lloyd-Jones D. M . ( 2012. ). Status of cardiovascular health in US adults: Prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008 . Circulation , 125 , 45 – 56 . doi: 10.1161/CIRCULATIONAHA.111.035733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne C. D., Stewart A. L . ( 1991. ). The MOS social support survey . Social Science & Medicine (1982) , 32 , 705 – 714 . [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . ( 2008. ). 2008 Physical activity guidelines for Americans . Washington, DC: : U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; . [Google Scholar]
- Washington D. L., Bean-Mayberry B., Hamilton A. B., Cordasco K. M., Yano E. M . ( 2013. ). Women veterans’ healthcare delivery preferences and use by military service era: Findings from the National Survey of Women Veterans . Journal of General Internal Medicine , 28 ( Suppl. 2 ), S571 – S576 . doi: 10.1007/s11606-012-2323-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington D. L., Farmer M. M., Mor S. S., Canning M., Yano E. M . ( 2015. ). Assessment of the healthcare needs and barriers to VA use experienced by women veterans: Findings from the national survey of women Veterans . Medical Care , 53 ( 4 Suppl. 1 ), S23 – S31 . doi: 10.1097/MLR.0000000000000312 [DOI] [PubMed] [Google Scholar]
- Weitlauf J. C. LaCroix A. Z. Bird C. E. Woods N. F. Washington D. L. Katon J. G. , … Stefanick M. L . ( 2015. ). Prospective analysis of health and mortality risk in Veteran and non-Veteran participants in the Women’s Health Initiative . Women’s Health Issues , 25 , 648 – 656 . doi: 10.1016/j.whi.2015.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Women’s Health Initiative Study Group . ( 1998. ). Design of the Women’s Health Initiative clinical trial and observational study . Controlled Clinical Trials , 19 , 61 – 109 . doi: 10.1016/S0197-2456(97)00078-0 [DOI] [PubMed] [Google Scholar]
- Zeger S. L., Liang K. Y . ( 1986. ). Longitudinal data analysis for discrete and continuous outcomes . Biometrics , 42 , 121 – 130 . [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.