Abstract
Purpose of the Study
A structured interview was conducted with Medicare patients readmitted to a private, tertiary teaching hospital from skilled nursing facilities (SNFs) to assess their perspectives of readmission preventability and their role in the readmission.
Design and Methods
Data were collected at Vanderbilt University Medical Center using a 6-item interview administered at the bedside to Medicare beneficiaries with unplanned hospital readmissions from 23 SNFs within 60 days of a previous hospital discharge. Mixed analytical methods were applied, including a content analysis that evaluated factors contributing to hospital readmission as perceived by consumers.
Results
Among 208 attempted interviews, 156 were completed, of which 53 (34%) respondents rated their readmission as preventable. 28.3% of the 53 consumers attributed the readmission to hospital factors, 52.8% attributed it to the SNF, and 18.9% believed both sites could have prevented the readmission. The primary driver of the readmission was a family member/caregiver in 31 cases and the patient in 24 of the 156 cases, amounting to 55 (35.3%) consumer-driven readmissions. Contributing factors included: premature hospital discharge (16.3%); poor discharge planning (16.3%); a clinical issue not resolved in the hospital (14.3%); inadequate treatment at the SNF (69.4%); improper medication management at the SNF (20.4%); and poor decision-making regarding the transfer (14.3%).
Conclusions and Implications
Interviewing readmitted patients provides information relevant to reducing readmissions that may otherwise be omitted from hospital and SNF records. Consumers identified quality issues at both the hospital and SNF and perceived themselves as initiating a significant number of readmissions.
Keywords: Person-centered care, Continuum of care, Quality of care, Care transition, Post-acute care, Medicare, Mixed-methods, Rehospitalization
Hospitals discharge more Medicare beneficiaries to skilled nursing facilities (SNFs) than to any other post-acute care setting (Mor, Intrator, Feng, & Grabowski, 2010). A significant portion of SNF patients (22%–25%) return to the hospital within 30 days (Levinson, 2013a; Levinson, 2014; Mor et al., 2010). Researchers estimate the preventability of hospital readmissions among patients discharged to all locations to range between 5% and 79%, with a median of 27.1% (Van Walraven, Bennett, Jennings, Austin, & Forster, 2011). Preventability, however, has largely been estimated based on physician-led clinical reviews of medical records or through the use of administrative, claims, and registry data (Auerbach et al., 2016; Goldfield et al., 2008; Lavenberg et al., 2014; Ouslander et al., 2010).
For example, Levinson (2014) described a clinical review approach employed by the Office of the Inspector General (OIG) in which physicians examined SNF medical records to identify documented triggers that reflected a potential adverse event. In these triggered cases, the OIG rated the preventability and degree of harm caused by the event. This approach estimated that 33% of SNF patients suffered an adverse or temporary harm event, with 59% of these events rated as preventable. Furthermore, over half of the patients who experienced harm were readmitted to the hospital, amounting to $2.8 billion spent on additional hospital care during 2011 (Levinson, 2014).
Similarly, a second approach to identifying potentially avoidable readmissions uses hospital diagnostic coding, such as the International Classification of Diseases (ICD) codes, from which readmission preventability is ascertained by expert consensus (Donzé, Aujesky, Williams, & Schnipper, 2013; Kansagara et al., 2011). Some investigations have implemented a more complex approach using claims data and algorithms based on hospital admission diagnoses to estimate preventability (Kramer, Fish, & Min, 2013). Researchers have yet to apply this approach to the SNF care setting. Lavenberg and colleagues (2014) described in detail the limitations and advantages of these existing approaches as they pertain to the measurement of readmission preventability.
One method that has not traditionally been used to estimate readmission preventability is to directly ask consumers—patients and/or their respective family members or caregivers who experienced both hospitalizations—to provide their perspective about factors that contributed to their readmission. Some studies that have interviewed rehospitalized consumers were limited by small sample sizes (Enguidanos, Coulourides, Schreibeis-Baum, Lendon, & Lorenz, 2015; Stevenson, Pori, Payne, Black, & Taylor, 2015; White et al., 2014) and did not include older adults discharged to SNFs (Howard-Anderson et al., 2014; Kangovi et al., 2012). One study with a larger sample included a small number of patients discharged to post-acute care but did not report data for this group separately (Auerbach et al., 2016; Greysen et al., 2016).
To our knowledge, no study has described the perceived role of the consumer in making the decision to return to the hospital. A consumer interview approach may provide insights into the preventability of hospital readmissions not captured with more traditional review methods used in prior studies. This includes clinical care not captured in SNF or hospital records that may highlight deficits in quality (Schnelle, Bates-Jensen, Chu, & Simmons, 2004), as well as patient factors or social circumstances that can go unrecognized from a review of medical records (Ouslander et al., 2010). Furthermore, the role of the consumer in the readmission decision may be more apparent in an interview with the patient, family member, or caregiver.
This mixed-methods study evaluates the perspectives of a sample of patients and/or their respective family members/caregivers who were readmitted to the discharging hospital from SNFs within 60 days. The study aims to measure the frequency of consumer-reported barriers to recovery, and to further describe the consumer’s perception of readmission causes and their role in the readmission decision. The following questions were addressed:
What percent of readmitted consumers rate their readmission as preventable?
What percent of readmissions rated as preventable are perceived by consumers to be due to hospital care, SNF care, or both?
How often do consumers report that the decision to return to the hospital was made by the consumer as opposed to a health care provider?
What are the main issues that contribute to preventable readmissions from the consumer’s perspective?
Design and Methods
Setting, Participants, and Eligibility
Data were collected at Vanderbilt University Medical Center, which is a private, tertiary teaching hospital, as part of a larger longitudinal quality improvement project funded by the Centers for Medicare & Medicaid Services (CMS) from January 2013 to June 2015. The larger project aimed to reduce hospital readmissions and improve the quality of care transitions for Medicare beneficiaries discharged to 23 area SNFs, of which one was nonprofit. Standardized hospital discharge documentation and telephone follow-up completed by project nurses within 24hr of SNF admission and 1 week later were key components of the larger project and were present for the time period during which the readmission data reported in this paper were collected. System-level practice changes implemented by Vanderbilt University Hospital and the SNFs in response to quality improvement findings occurred after the conclusion of the project and, thus, did not influence study results. The 23 SNFs were located in the middle Tennessee area and had an average total bed capacity of 118 (short + long-stay beds) and average total staffing (licensed nurses + nurse aides) of 4.18 hours per resident per day (hprd). Both bed capacity and staffing levels were slightly higher than the average for SNFs throughout the state (TN state average = 114 beds and 3.97 total hprd) based on publicly reported data during the project period (http://www.medicare.gov/nursinghomecompare).
A multi-disciplinary team including hospitalists, gerontologists, transitional care advocates (nurse practitioners and registered nurses), and a research coordinator developed a six-question, semi-structured rehospitalization interview, which was conducted with a subset of patients who had unplanned hospital readmissions from SNFs within 60 days of hospital discharge. The purpose of the interview was to identify factors that consumers perceived as contributing to the readmission, to gauge whether something could have been done differently at the hospital or SNF to avoid the readmission, and to identify the primary decision-maker who initiated the transfer back to the hospital. The interview included four close-ended questions to collect quantitative data regarding the course of the readmission, and an additional two open-ended questions to identify issues that potentially contributed to the readmission. Interview questions were modified from an instrument used by a prior mixed-methods study (Auerbach, et al., 2016; Greysen et al., 2016), which administered a similar but longer questionnaire.
The university-affiliated Institutional Review Board waived the requirement for written consent. Instead, eligible participants were provided with a description of the project and had the right to refuse the interview. Interviews were attempted for all patients who were discharged from the hospital to one of the 23 participating SNFs and were otherwise eligible according to the eligibility criteria of the larger CMS-funded study.
Eligibility criteria for the data presented here as part of this sub-study included the following: (a) Medicare beneficiary; (b) discharged from the hospital to one of 23 area SNFs; (c) unplanned inpatient readmission from SNF within 60 days of hospital discharge; and (d) understood and spoke English. Patients who discharged from a SNF to home and were subsequently readmitted to the hospital were not included in this sample. Rehospitalized patients who were not readmitted to the original discharging hospital were also excluded from this sample, as it was not possible to interview this group upon hospital readmission due to delays in notification about the transfer.
Prior research has highlighted the need to include the perspectives of readmitted patients with cognitive limitations and their caregivers, as their exclusion may limit the generalizability of findings to the larger SNF population (Greysen et al., 2016). Consequently, all cognitively-impaired participants in the sample were included if a family member or caregiver was jointly available for the interview and knowledgeable about the care transition. Cognitive impairment was assessed using the Brief Interview for Mental Status (BIMS), a short, objective screening tool designed to measure cognitive function among nursing home residents (Chodosh et al., 2008; Saliba et al., 2012). The BIMS total score ranges from 0 to 15 (0–7: severe impairment; 8–12: moderate impairment; 13–15: cognitively intact). A patient with a score of 12 or less was categorized as cognitively impaired (Saliba et al., 2012).
Interview Protocol
Trained research personnel administered in-person interviews at the bedside during the rehospitalization event. Due to time constraints, responses were not audiotape-recorded or returned to participants for review, but instead were documented by research staff using Research Electronic Data Capture (REDCap; Harris et al., 2009). This approach veered from traditional qualitative methodology but did allow for a content analysis of the consumer responses. For the purpose of this analysis, four interview questions were analyzed: (1) “What is your understanding of why you were transferred back to the hospital?”; (2) “Who is the main person who thought you (or your family member) needed to be transferred back to the hospital?”; (3) “Do you think that anything could have been done better during your previous hospitalization to prevent your transfer back to hospital?”; and (4) “Do you think that anything could have been done differently in [name of SNF] to prevent your transfer back to the hospital?”. For the purposes of this study, answering “yes” to either question 3 or 4 indicated that the rehospitalization was potentially preventable. Additionally, if a participant answered “yes” or “unsure” to question 3 or 4, the interviewer probed for more information as to what could have potentially prevented the rehospitalization. If a participant answered “no” to both questions 3 and 4, they were not further questioned. Data were subsequently exported from the REDCap database and a mixed-methods approach was applied to perform descriptive, quantitative, and content analyses. All analyses were performed using Microsoft Excel (Microsoft Office Professional 2010, version 14.0.7166.5000) and SPSS statistical software (IBM SPSS Statistics for Windows, version 23.0).
Analysis of Open-Ended Participant Commentary
A content analysis (Hsieh & Shannon, 2005) was applied to analyze participants’ responses to the open-ended interview questions, in order to explore the causal factors that consumers perceived as contributing to the readmission. The endorsement of each factor was later quantified into frequencies in order to prioritize quality improvement efforts as part of the larger study. All interview responses were examined for participants who endorsed that something could have been done differently to prevent their transfer back to the hospital or who were unsure (i.e., a “yes” or “unsure” response to question 3 or 4). Commentary generated by participants who responded that they were “unsure” if anything could have been done differently were subsequently determined to have inconclusive commentary and, therefore, excluded from the overall analysis. Research personnel who administered the interviews did not participate in the content analysis.
Initially, three members of the research team conducted a blinded review of the interview data. Each of these staff independently reviewed all interview commentary and examined the content for text related to care transition issues (e.g., “I should not have been discharged so soon”). Each reviewer then classified the interview responses into themes and made revisions as new themes emerged in the commentary. After coding multiple interviews, prior data was recoded as appropriate before continuing to code the remaining interviews. New categories continued to be created as novel issues were encountered that were not already captured in the coding structure. This iterative process continued until all interviews were reviewed and no new themes were identified in an effort to achieve data saturation.
Subsequently, the reviewers met as a team to reach agreement on the content of the themes, as well as to refine the classifications of each comment, until a preliminary thematic coding structure for categorization of consumer responses was developed and agreed upon by the group. Commentary that generated inter-rater disagreement among the initial group of three reviewers was flagged for further review by two additional independent research team members, neither of whom had participated in the initial review process. These additional reviewers were provided with the original dataset of consumers’ responses along with the preliminary coding structure, but they were blind to the disparate ratings of the original reviewers. They each then independently reviewed the same data and used the preliminary thematic coding structure to independently categorize each consumer comment. Lastly, all five reviewers reconvened to compare the original categorizations to those of the additional two reviewers. Remaining discrepancies were discussed as a group until inter-rater agreement was achieved for each response, and final revisions were made to the coding structure to accurately reflect all commentary.
For the purposes of this study, participant commentary is described for interviews in which consumers indicated that something could have been done to avoid the rehospitalization. As commentary made by consumers “unsure” of readmission preventability was often inconclusive, it was examined separately but not included in the central analysis. Because each participant was permitted to describe more than one quality issue that may have prevented their readmission, endorsement of themes was not mutually exclusive in that a single interview comment could receive multiple thematic codes.
Results
From March 2013 to April 2015, interviews were attempted for 208 unplanned inpatient readmissions from 23 SNFs within 60 days of a previous hospital discharge. Of those 208 readmissions, 156 rehospitalization interviews (75%) were completed, whereas 52 (25%) could not be obtained due to the following reasons: (a) patient too ill to participate (12.5%); (b) patient deceased in the hospital (5.3%); (c) insufficient time prior to discharge (5.3%); and (d) patient refusal (1.9%). Of the 156 completed interviews, 100 (64.1%) were completed solely with the patient, 29 (18.6%) were completed solely with a family member/caregiver, and 27 (17.3%) were conducted jointly with both the patient and the respective family member/caregiver. The interview required 10 to 20min per person to administer.
Participants (N = 156) had a mean age of 74.5 (±11.1) years and were 51.9% female and 84.6% non-Hispanic white (Table 1). The median length of stay was 8 days for the initial hospitalization and 6 days for the readmission. The median length of time between the initial hospital discharge and readmission from SNF was 10.5 days.
Table 1.
Baseline Characteristics of Study Sample
| Characteristic | N = 156 |
|---|---|
| Age, in years, mean (±SD) | 74.5 (±11.1) |
| Sex, n (%) | |
| Female | 81 (51.9%) |
| Race, n (%) | |
| White | 132 (84.6%) |
| African American | 23 (14.7%) |
| Other | 1 (0.6%) |
| Brief Interview for Mental Status (BIMS), n (%) | |
| Cognitively Intact (score 13–15) | 82 (52.6%) |
| Moderately Impaired (score 8–12) | 32 (20.5%) |
| Severely Impaired (score 0–7) | 5 (3.2%) |
| Missing (due to inability to participate, refusal, or insufficient time) | 37 (23.7%) |
| Time intervals, in days, median (interquartile range) | |
| Length of stay during initial hospitalization | 8 (5 to 12) |
| Time between initial hospital discharge and readmission | 10.5 (4 to 20) |
| Time between readmission and rehospitalization interview | 2 (1 to 4) |
| Length of stay during readmission | 6 (4 to10) |
The average BIMS score for the sample with valid data (119 out of 156) was 13.03 (±2.73). Among 156 participants 52.6% were cognitively intact (BIMS score 13–15), 20.5% were moderately impaired (score 8–12), and 3.2% were severely impaired (score 0–7). A BIMS total score could not be calculated for the remaining 37 participants due to the patient’s inability to respond, refusal, or insufficient time prior to discharge. Family members/caregivers provided proxy interview responses for severely impaired patients, though most participants in the sample had sufficient cognitive functioning to answer the interview questions.
Results were analyzed according to patient demographics including age, sex, race, ethnicity, and cognitive status; however, differences were only identified for cognitive status. Consumers who were “unsure” as to whether something could have been done differently to avoid the rehospitalization in one or both care settings were more likely to be cognitively impaired (55% cognitively intact) than participants who responded to these questions with a “yes” or “no” (84.8% cognitively intact). However, open-ended commentary among “unsure” consumers was not excluded on the basis of the participants’ cognitive status but, rather, on the inconclusive nature of their remarks. For example, some consumers were simply undecided as to whether or not the readmission was preventable, such as one patient who expressed it was “hard to tell.” Many participants who were “unsure” were unable to identify the specifics surrounding the circumstances of the transfer, providing responses such as “I just don’t know. I don’t really know what they did.” Other participants were unable to provide clear responses but, instead, provided more tangential or nonsensical commentary that could not be coded.
Consumers’ Role in the Decision to Transfer
Across all 156 completed interviews, 92 (59%) consumers reported that the decision to return to the hospital for readmission was made by someone at the SNF. In nine (5.8%) cases, the participant could not identify the primary decision-maker who initiated the transfer. In 31 (19.9%) cases, the primary decision-maker who triggered the transfer was reported by the consumer to be the family member or caregiver, and in 24 (15.4%) cases the patient reported that s/he insisted on the transfer. Thus, a total of 55 (35.3%) cases reflected consumer-driven readmissions.
Consumers’ Endorsement of Preventability
A total of 53 (34%) consumers endorsed that something could have been done differently to avoid the rehospitalization in one or both care settings, with 15 (28.3%) indicating the hospital, 28 (52.8%) indicating the SNF, and 10 (18.9%) indicating that both sites could have prevented the readmission. Among the 55 (35.3%) consumers who responded that they were “unsure” if the hospital and/or SNF could have prevented the readmission, 23 (41.8%) consumers responded they were “unsure” solely in regard to the hospital’s role, 15 (27.3%) were “unsure” solely in regard to the SNF, and 17 (30.9%) responded that they were “unsure” with respect to both care settings. Commentary made by consumers who were “unsure” was ultimately excluded from the central content analysis because, under separate analysis, 43.6% of these comments were rated by all research team members as “inconclusive.”
Consumers’ Perspectives of Preventability Themes
Of the 53 consumers who endorsed some level of preventability, 49 interviews (92.5%) included commentary that was analyzed for thematic categorization. The remaining four included commentary that was rated by all research team members as “inconclusive,” thus this commentary was excluded.
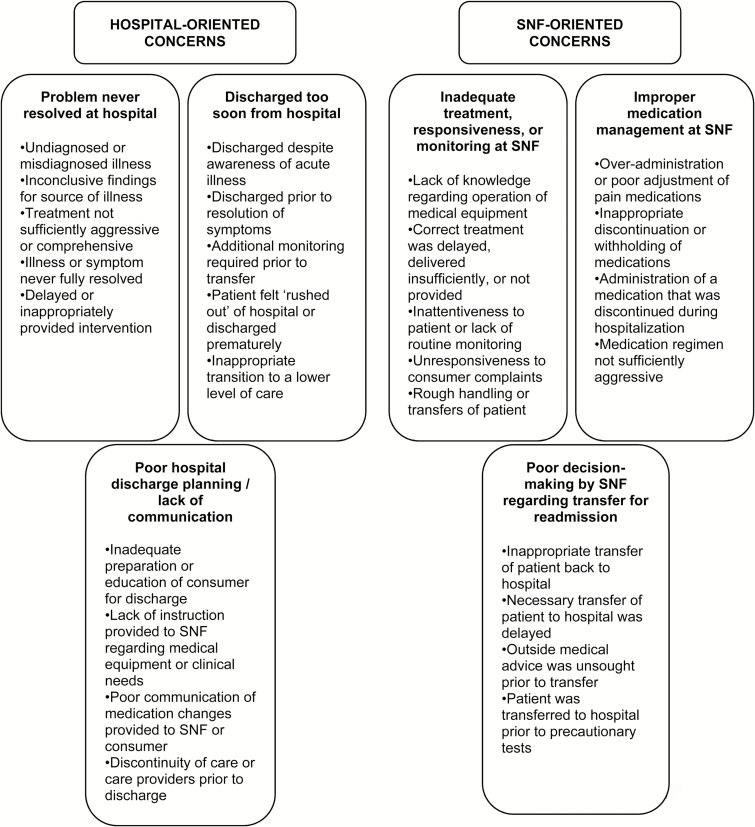
Table 2 shows the content analysis of consumer commentary from the 49 interviews, which revealed six themes that contributed to readmissions, as referenced by the consumers. Themes that reflected quality issues during the previous hospitalization included: premature hospital discharge, poor hospital discharge planning or lack of communication between the hospital and patient or SNF providers, and a clinical problem that was never resolved during the initial hospitalization. In contrast, themes that implicated the SNF comprised: inadequate treatment including poor SNF staff responsiveness to patient complaints and/or poor symptom monitoring, improper medication management, and poor decision-making regarding the transfer from the SNF back to the hospital. The frequencies with which consumers endorsed the issues were quantified in order to prioritize findings for quality improvement practice. Frequencies are shown with the content analysis in an effort to describe which issues patients reported most often. On average, participants endorsed 1.5 of these six themes, which were not mutually exclusive. Excerpts of consumer commentary from the rehospitalization interview are provided in Table 2 in order to demonstrate each theme. Subthemes identified within each category are also described in Figure 1.
Table 2.
Themes Perceived by Consumers as Contributing to Preventable Readmissions (N = 49)
| Site of concern | Preventability themea and consumers’ representative quotations | Endorsement n (%) |
|---|---|---|
| Hospital | Problem never resolved at hospital | 7 (14.3%) |
| Nobody knew about the GI bleed. | ||
| They never found the cause of her pain. | ||
| Discharged too soon from hospital | 8 (16.3%) | |
| They could have kept me longer in the hospital. I feel safer at the hospital; you can take better care of me here. | ||
| The stay here last time could have been extended to be sure she was over the illness last time. | ||
| Poor hospital discharge planning/ lack of communication | 8 (16.3%) | |
| [I] wished they had told me and my wife about the medication before they took me off it. | ||
| They should have made sure that where they sent my mother they knew about the TEP, and how to clean it and what to do for it. | ||
| SNF | Improper medication management at SNF | 10 (20.4%) |
| When I asked about my water pill and informed them I had not had it for 13–18 days, I felt like I was being blown off. | ||
| As soon as the Butrans patch arrived they were supposed to discontinue the hydrocodone, but they kept giving it even after I questioned it. | ||
| Inadequate treatment, responsiveness, or monitoring at SNF | 34 (69.4%) | |
| They didn’t know what to do with my drain and feeding tube. They started up the feeding “in” and never connected the “out” to a bag like I told them. | ||
| She was neglected. No one went in to check on her and her health declined to the point she had to come back to the hospital. | ||
| Poor decision-making by SNF regarding transfer for readmission | 7 (14.3%) | |
| They told me I needed to go back to the hospital and I begged them not to send me. I had stopped bleeding by then but the nurse said I scare them out there. | ||
| They could have trusted me when I told them it was bad. I had to call my own doctor and he told me to get to the ER. |
Notes: ER = emergency room; GI = lower gastrointestinal; SNF = skilled nursing facility; TEP = tracheoesophageal puncture.
aThemes were not mutually exclusive in that one consumer comment could be coded as pertaining to more than one theme.
Figure 1.
Subthemes perceived by consumers as contributing to preventable readmissions (N = 49).
Hospital-Oriented Concerns
Approximately 16% of the 49 interviews pointed to being discharged too quickly from the hospital to the SNF. One patient (male; age 82) who was readmitted to the medical intensive care unit within 2 days of discharge described how he had “felt rushed out of the hospital,” and that he “was anxious and not feeling well” on the day of his previous hospital discharge. In contrast, some participants (14.3%) believed that a condition went unnoticed or unresolved during the initial hospitalization, regardless of the discharge timing. The son of one patient (female; over age 89) reflected on a missed diagnosis during his mother’s previous hospital admission stating that:
Nobody knew about the lower GI [gastrointestinal] bleed…and they did not do [body] weights or [fluid] input/output during her stay…I was concerned about orders not being followed. I asked to see the MD and never got to see the MD. [They] changed doctors a lot – four doctors in seven days. I felt the continuity of care was a problem.
Similarly, 16% described how their readmission may have been related to the hospital’s lack of communication during the discharge process, both with the patient and the SNF, as well as poor patient education and clinical planning in preparation for the transfer. For example, one patient (male; age 73) reported that the hospital did not communicate with him regarding the discontinuation of the medication Ranexa, stating that he “wished they [the hospital] had told me and my wife about the medication before they took me off it.” Likewise, one mother whose daughter (female; age 44) was readmitted within 2 days of hospital discharge for abdominal pain described the lack of hospital communication with the SNF. She said that the hospital “needed to give better instructions to the SNF about how to run the tube feeding. They [the SNF] were letting the tube feeding run too fast and she was in extreme pain.”
SNF-Oriented Concerns
Consumers most frequently attributed their readmission to treatment at the SNF, expressing concern about staff responsiveness and the degree of symptom monitoring (69.4%). For instance, one patient (female; age 77) who was rehospitalized for urine retention, leukocytosis, and altered mental status, reported along with her daughter that she was “never put on a bedpan or offered to be put on a bedpan [at the SNF]…and was left lying in urine-soaked pads for hours.” They stated they were informed by the SNF staff that she “would be changed every 2hr as needed,” but that this was “more like every 4 to 6hr.” They also described how she was discharged from the hospital with ointment to be used at the SNF but claimed that the ointment was never applied by SNF staff to her perineal area as ordered.
Patients often cited issues with medication management at SNFs (20.4%) and, more specifically, the overuse of pain medications during post-acute care. One participant (female; age 77) who claimed she “never got out of bed or had any physical therapy” reported that the SNF staff had also given her pain medicine “with every medication pass even though [she] never asked for it.” Another participant (female; age 54) readmitted for delirium related to polypharmacy described a similar issue:
I got to [the SNF]…then I may have taken too many pain medications and it affected me. I was confused. I was dreaming crazy dreams, then I fell on the floor, then they upped the pain meds and I couldn’t think straight…I still had Lyrica and Celexa - too much for my brain…they could have adjusted my pain meds more slowly.
A total of 14.3% of consumers also described what they deemed to be poor decision-making regarding their transfer from the SNF back to the hospital. Some patients believed they had been transferred back to the hospital unnecessarily. One participant (male; age 76) attested that:
My blood count was low…I had just started eating and did not feel that the test results were as bad as they [the SNF] said. I should not have been sent back here [to the hospital]. They [the SNF] needed to repeat the lab or they should have called [the doctor’s] office before sending me to the emergency room.
In contrast, another patient (male; age 66) indicated that he should have been transferred back to the emergency room (ER) for reevaluation sooner.
I called my private physician on the phone and he told me to get to the ER no matter what the people there [at the SNF] said, so I did. They could have trusted me when I told them it was bad. I had to call my own doctor and he told me to get to the ER.
Discussion
Overall, 53 (34%) of the 156 hospital readmissions from SNFs were perceived by consumers as preventable. Interviews revealed that patients and family members/caregivers perceived themselves to be the primary drivers of transfers in over one third of readmissions. Although consumers who endorsed preventability more frequently implicated aspects of SNF care, they described quality issues at both the SNF and the hospital. Inadequate treatment or responsiveness by the SNF staff, improper medication management at the SNF, premature hospital discharge, and poor hospital discharge planning were the largest areas of concern expressed by consumers in this study. To our knowledge, this is the first consumer perspectives study to focus on patients readmitted from SNFs, but problems with hospital discharge and care transitions have also been reported for other patient populations (Auerbach et al., 2016; Enguidanos et al., 2015; Howard-Anderson et al., 2014; Kangovi et al., 2012).
Dissatisfaction with SNF care quality appeared to be a major contributing factor, given that 30% of readmissions were reported as self-initiated by consumers. Interview commentary from the content analysis revealed that many consumers requested their own readmission because they were concerned about the capabilities of SNF staff to provide coordinated and timely quality care. This is not an unexpected result and reflects recent reports of care plan quality problems in SNFs and ongoing concerns about the adequacy of staffing in nursing home care settings (Levinson, 2013a; Levinson, 2013b; Levinson, 2014; Thomas, Mor, Tyler, & Hyer, 2012). Recent data also indicate that SNFs with lower staffing levels have higher readmission rates, and that lower retention rates among licensed nurses in SNFs are significantly associated with higher 30-day rehospitalization rates (Levinson 2013a; Thomas et al., 2012). Furthermore, poor hospital discharge communication may be straining SNFs’ already hampered ability to provide timely, appropriate care (Kind & Smith, 2008; King et al., 2013). Unfortunately, the system-level problems with SNF care and staffing do not lend themselves to an intervention that can be easily implemented in the short term. However, if consumers are driving some readmissions, at least partially due to unrealistic expectations about SNF care or inaccurate perceptions of SNF quality, then interventions to reduce readmissions could be more feasibly initiated by the hospital and SNF. Educating consumers about the capacity of SNF care, providing anticipatory guidance as to the normal course of their disease (e.g., dizziness might be expected), and engaging them in discussions about their readiness for hospital discharge may increase their confidence in the ability of SNF staff to effectively manage their care.
Consumer education and patient activation become increasingly important given the finding that 35.3% of consumers in this sample were “unsure” as to whether the hospital and/or SNF could have done anything differently to prevent their rehospitalization, which suggests that these consumers were unaware of the specific circumstances surrounding their transfer. This consumer uncertainty raises important questions about the extent of patient education and engagement during care transitions, particularly among a population with relatively high levels of cognitive impairment, and merits further study. Likewise, commentary collected in this study often revealed a lack of patient empowerment or self-advocacy throughout the course of the care transition which, if bolstered, may hold promise in preventing inappropriate transfers or expediting necessary ones. These patient-centered initiatives should be viewed as a crucial aspect of any multicomponent intervention to reduce readmissions and complement the findings from previous work examining the efficacy of multifaceted interventions that include patient and caregiver education (Hansen, Young, Hinami, Leung, & Williams, 2011; Kripalani, Theobald, Anctil, & Vasilevskis, 2013).
The findings from this study have potential implications for how SNF readmission data should be interpreted and used on a regulatory level and how interventions to reduce readmissions should be designed in future studies. It has been debated whether hospitals or SNFs should be penalized for readmissions that are driven primarily by consumer preference, even though one could argue that it is the responsibility of both hospitals and SNFs to educate patients and families about this issue (Lavenberg et al., 2014). Directly asking readmitted consumers about who made the decision to transfer them back to the hospital and which aspects of care were most problematic is the most efficient way to measure the consumer role in the transfer process, and such measures should be incorporated into the satisfaction interviews already conducted by many hospitals and SNFs. These consumer interviews, when combined with other methods used to identify potentially avoidable readmissions as reviewed in this paper, would provide a more comprehensive data base useful for improvement.
The regulatory implications of these data are particularly timely because 30-day readmission rates from SNFs will soon be publicly-reported by CMS as a quality indicator (Medicare Program, 2015). The implicit assumption that these rates may reflect the quality of SNF care is leading to policy initiatives that link readmission rates with SNF financial incentives (Burke et al., 2016). This assumption of SNF responsibility for readmissions is not without merit based on the consumer perspectives reported in this study, as well as other data showing associations between low overall SNF staffing levels and hospital readmissions rates (Levinson, 2013a). Addressing staffing issues is an important long term solution that should be part of broader efforts to reduce SNF responsibility for avoidable hospital readmissions.
However, the findings of this study also suggest that a substantial proportion of readmissions are due to factors more under the control of the discharging hospital than the receiving SNF. In particular, the perception that patients were discharged too quickly suggests that hospital providers may have had an unrealistic expectation of the capabilities of the SNF to manage the patient’s clinical care or erroneously concluded that the patient was ready for discharge. In either case, the results of this study suggest that overall readmission data should not be considered as a quality measure of SNF care only, but rather as a quality indicator of both hospital and SNF care jointly and the transition process between these two care settings. Arguments can be made that the new SNF readmission indicators to be published by CMS (Medicare Program, 2015) should be reported separately for those cases when consumers perceived the hospital, the SNF, or both as the locus of the problem. This type of reporting would reflect the responsibility of both sites for a successful transition and provide incentives for both sites to develop more effective methods of communication and transfer.
In addition to the limitation that this study took place in only one hospital, the analytical exclusion of commentary by participants “unsure” of readmission preventability may bias the findings, even though this exclusion was implemented due to difficulty in categorizing the “unsure” consumer comments. The use of audiotaped interviews would likely have provided further insight into participant commentary, and the use of other qualitative methods that do not rely on team consensus, such as a quantitative content analysis that uses an objective count of key word frequencies, may have been helpful in the interpretation of data. We also acknowledge that consumer perceptions of reasons for readmission or their role in the readmission decision may not have been objective. For example, in some cases, it is possible that decisions to transfer a patient back to the hospital resulted from meetings between consumers and SNF staff in which the decision to transfer was more of a joint decision than implied by consumers in their interview comments. However, even if consumer perceptions are biased, it does not detract from their importance as measures of factors that should be addressed in a successful hospital discharge or SNF-to-hospital readmission process. Moreover, a study by Boulding and colleagues (Boulding, Glickman, Manary, Schulman, & Staelin, 2011) that examined perceptions of patients across 2,562 hospitals found that higher satisfaction with inpatient care and discharge planning was significantly associated with lower 30-day readmission rates, and patients’ perceptions were more predictive of clinical quality than objective clinical performance measures.
Other limitations of this study are that consumers may have felt pressure to not criticize the quality of the hospital care because interviews took place in the hospital setting. It’s also possible that consumers who had negative opinions of the discharging hospital requested to be rehospitalized elsewhere and were, thus, not represented in the readmission sample included in this study. However, interviewing consumers transferred to other hospitals is difficult because SNFs do not routinely alert the original discharging hospital when patients are discharged from their SNF to other locations. Furthermore, there may be wide geographic dispersion of hospitals in many regions. Finally, patient complaints about the quality of SNF care may not represent the perceptions of all patients discharged to SNFs because we only interviewed patients who were readmitted to the hospital from a SNF.
In conclusion, this study demonstrates the value and feasibility of interviewing consumers about factors that contributed to their hospital readmission from a SNF. Strengths of the study included a focus on the SNF population, the measurement of consumer-driven readmissions, and the inclusion of participants with cognitive impairment. The interview process was relatively inexpensive in terms of staff time (10–20min), potentially yielding a higher participation rate among patients, and identified actionable factors that may have been traditionally overlooked (both at the SNF and hospital) to prevent readmissions. The consumer interview offers a unique perspective of the readmission process that may enhance medical record reviews and produces data with clear policy and intervention implications that supplement chart review-based analyses of factors contributing to hospital readmissions.
Funding
This work was supported by the Department of Health and Human Services, Centers for Medicare & Medicaid Services (grant number 1C1CMS331006 to J. F. Schnelle); the National Institute on Aging of the National Institutes of Health (award number K23AG040157 to E. E. Vasilevskis); and the National Center for Advancing Translational Sciences (CTSA award No. UL1TR000445). Support was also provided by the Department of Veterans’ Affairs through the Clinical Research Center of Excellence and through the Geriatric Research, Education and Clinical Center. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies, the National Institutes of Health, the National Center for Advancing Translational Sciences or the Department of Veterans’ Affairs.
Acknowledgments
Each co-author contributed significantly to the manuscript. None of the authors have significant conflicts of interest to report related to this project or the results reported within this manuscript.
References
- Auerbach A. D. Kripalani S. Vasilevskis E. E. Sehgal N. Lindenauer P. L. Metlay J. P.,…Schnipper J. L (2016). Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Internal Medicine, 176, 484–493. doi:10.1001/jamainternmed.2015.7863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulding W. Glickman S. W. Manary M. P. Schulman K. A., & Staelin R (2011). Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. American Journal of Managed Care, 17, 41–48. Retrieved from http://www.ajmc.com/journals/issue/2011/2011-1-vol17-n1/AJMC_11jan_Boulding_41to48/ [PubMed] [Google Scholar]
- Burke R. E. Whitfield E. A. Hittle D. Min S. J. Levy C. Prochazka A. V.,…Ginde A. A (2016). Hospital readmission from post-acute care facilities: Risk factors, timing, and outcomes. Journal of the American Medical Directors Association, 17, 249–255. doi:10.1016/j.jamda.2015.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chodosh J., Edelen M. O., Buchanan J. L., Yosef J. A., Ouslander J. G., Berlowitz D. R., …Saliba D. (2008). Nursing home assessment of cognitive impairment: Development and testing of a brief instrument of mental status. Journal of the American Geriatrics Society, 56, 2069–2075. doi:10.1111/j.1532-5415.2008.01944.x [DOI] [PubMed] [Google Scholar]
- Donzé J. Aujesky D. Williams D., & Schnipper J. L (2013). Potentially avoidable 30-day hospital readmissions in medical patients: Derivation and validation of a prediction model. JAMA Internal Medicine, 173, 632–638. doi:10.1001/jamainternmed.2013.3023 [DOI] [PubMed] [Google Scholar]
- Enguidanos S. Coulourides K. Schreibeis-Baum H. Lendon J., & Lorenz K (2015). “Because I was sick”: Seriously ill veterans’ perspectives on reason for 30-day readmissions. Journal of the American Geriatrics Society, 63, 537–542. doi:10.1111/jgs.13238 [DOI] [PubMed] [Google Scholar]
- Goldfield N. I., McCullough E. C., Hughes J. S., Tang A. M., Eastman B., Rawlins L. K., Averill R. F. (2008). Identifying potentially preventable readmissions. Health Care Financing Review, 30, 75–91. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19040175 [PMC free article] [PubMed] [Google Scholar]
- Greysen S. R. Harrison J. D. Kripalani S. Vasilevskis E. Robinson E. Metlay J.,…Auerbach A. D (2016). Understanding patient-centred readmission factors: A multi-site, mixed-methods study. BMJ Quality and Safety. Advance online publication. doi:10.1136/bmjqs-2015-004570 [DOI] [PubMed] [Google Scholar]
- Hansen L. O. Young R. S. Hinami K. Leung A., & Williams M. V (2011). Interventions to reduce 30-day rehospitalization: A systematic review. Annals of Internal Medicine, 155, 520–528. doi:10.7326/0003-4819-155-8-201110180-00008 [DOI] [PubMed] [Google Scholar]
- Harris P. A. Taylor R. Thielke R. Payne J. Gonzalez N., & Conde J. G (2009). Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. doi:10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard-Anderson J. Lonowski S. Vangala S. Tseng C. H. Busuttil A., & Afsar-Manesh N (2014). Readmissions in the era of patient engagement. JAMA Internal Medicine, 174, 1870–1872. doi:10.1001/jamainternmed.2014.4782 [DOI] [PubMed] [Google Scholar]
- Hsieh H. F., & Shannon S. E (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277–1288. doi:10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Kangovi S. Grande D. Meehan P. Mitra N. Shannon R., & Long J. A (2012). Perceptions of readmitted patients on the transition from hospital to home. Journal of Hospital Medicine, 7, 709–712. doi:10.1002/jhm.1966 [DOI] [PubMed] [Google Scholar]
- Kansagara D. Englander H. Salanitro A. Kagen D. Theobald C. Freeman M., & Kripalani S (2011). Risk prediction models for hospital readmission: a systematic review. JAMA, 306, 1688–1698. doi:10.1001/jama.2011.1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind A. J. H., & Smith M. A (2008). Documentation of mandated discharge summary components in transitions from acute to subacute care. In Henriksen K., Battles J. B., Keyes M. A.et al. (Eds.), Advances in patient safety: New directions and alternative approaches (vol. 2: Culture and redesign) (pp. 179–188). Rockville, MD: Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- King B. J. Gilmore-Bykovskyi A. L. Roiland R. A. Polnaszek B. E. Bowers B. J., & Kind A. J (2013). The consequences of poor communication during transitions from hospital to skilled nursing facility: A qualitative study. Journal of the American Geriatrics Society, 61, 1095–1102. doi:10.1111/jgs.12328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer A. Fish R., & Min S (2013). Community discharge and rehospitalization outcome measures (fiscal year 2011). Requisition Number MED 12P0061. Washington, DC: Medicare Payment Advisory Commission; Retrieved from http://www.medpac.gov/documents/contractor-reports/apr13_communitydischarge_contractor.pdf [Google Scholar]
- Kripalani S. Theobald C. N. Anctil B., & Vasilevskis E. E (2013). Reducing hospital readmission rates: Current strategies and future directions. Annual Review of Medicine, 14, 471–485. doi:10.1146/annurev-med-022613-090415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavenberg J. G. Leas B. Umscheid C. A. Williams K. Goldmann D. R., & Kripalani S (2014). Assessing preventability in the quest to reduce hospital readmissions. Journal of Hospital Medicine, 9, 598–603. doi:10.1002/jhm.2226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson D. R. (2013. a). Medicare nursing home resident hospitalization rates merit additional monitoring. Report No. OEI-06-11-00040. Washington, DC: US Department of Health and Human Services, Office of Inspector General; Retrieved from http://oig.hhs.gov/oei/reports/oei-06-11-00040.pdf [Google Scholar]
- Levinson D. R. (2013. b). Skilled nursing facilities often fail to meet care planning and discharge planning requirements. Report No. OEI-02-09-00201. Washington, DC: US Department of Health and Human Services, Office of Inspector General; Retrieved from http://oig.hhs.gov/oei/reports/oei-02-09-00201.pdf [Google Scholar]
- Levinson D. R. (2014). Adverse events in skilled nursing facilities: National incidence among Medicare beneficiaries. Report No. OEI-06-11-00370. Washington, DC: US Department of Health and Human Services, Office of Inspector General; Retrieved from http://oig.hhs.gov/oei/reports/oei-06-11-00370.pdf [Google Scholar]
- Medicare.gov Nursing Home Compare (n.d.) Retrieved from http://www.medicare.gov/nursinghomecompare/results.html#loc=37205&lat=36.1030036&lng=-86.8722146
- Medicare Program (2015). Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities (SNFs) for FY 2016, SNF Value-Based Purchasing Program, SNF Quality Reporting Program, and Staffing Data Collection; Final Rule, 80 Fed. Reg. 46390 (to be codified at 42 C.F.R. pt. 483). [PubMed]
- Mor V. Intrator O. Feng Z., & Grabowski D. C (2010). The revolving door of rehospitalization from skilled nursing facilities. Health Affairs, 29, 57–64. doi:10.1377/hlthaff.2009.0629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander J. G. Lamb G. Perloe M. Givens J. H. Kluge L. Rutland T.,…Saliba D (2010). Potentially avoidable hospitalizations of nursing home residents: Frequency, causes, and costs. Journal of the American Geriatrics Society, 58, 627–635. doi:10.1111/j.1532-5415.2010.02768.x [DOI] [PubMed] [Google Scholar]
- Saliba D. Buchanan J. Edelen M. O. Streim S. Ouslander J. Berlowitz D., & Chodosh J (2012). MDS 3.0: Brief interview for mental status. Journal of the American Medical Directors Association, 13, 611–617. doi:10.1016/j.jamda.2012.06.004 [DOI] [PubMed] [Google Scholar]
- Schnelle J. F. Bates-Jensen B. M. Chu L., & Simmons S. F (2004). Accuracy of nursing home medical record information about care-process delivery: Implications for staff management and improvement. Journal of the American Geriatrics Society, 52, 1378–1383. doi:10.1111/j.1532-5415.2004.52372.x [DOI] [PubMed] [Google Scholar]
- Stevenson C. W. Pori D. Payne K. Black M., & Taylor V. E (2015). Hearing the veteran’s voice in congestive heart failure readmissions. Professional Case Management, 20, 177–185. doi:10.1097/NCM.0000000000000080 [DOI] [PubMed] [Google Scholar]
- Thomas K. S., Mor V., Tyler D. A., Hyer K. (2012). The relationships among licensed nurse turnover, retention, and rehospitalization of nursing home residents. The Gerontologist, 53, 211–221. doi:10.1093/geront/gns082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Walraven C. Bennett C. Jennings A. Austin P. C., & Forster A. J (2011). Proportion of hospital readmissions deemed avoidable: A systematic review. CMAJ, 183, E391–E402. doi:10.1503/cmaj.101860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White C. L. Brady T. L. Saucedo L. L. Motz D. Sharp J., & Birnbaum L. A (2014). Towards a better understanding of readmissions after stroke: Partnering with stroke survivors and caregivers. Journal of Clinical Nursing, 24, 1091–1100. doi:10.1111/jocn.12739 [DOI] [PubMed] [Google Scholar]