Abstract
Background and Objectives:
Self-perceptions of aging (SPA), or attitudes toward one’s aging experience, have been linked to health through multiple pathways. Few studies, however, have investigated how older adults’ views on aging influence their care-seeking behaviors.
Research Design and Methods:
Using two independent subsamples from the Health and Retirement Study (2011 Health Care Mail Survey: N = 2,866; 2013 Health Care and Nutrition Study: N = 2,474), logistic regression and negative binomial regression were used to examine the association between SPA and health care delay over the next 12 months. Subsequently, we used latent class analysis to identify subgroups reporting different reasons for delay. With multinomial logistic regression, we then examined if, compared with the no delay group, SPA differentiated membership in the delay subgroups.
Results:
In both samples, more negative aging self-perceptions were associated with a higher likelihood of health care delay and more perceived barriers to care, after adjusting for predisposing, enabling, and need factors. Latent class analysis revealed three subgroups characterized by different reasons for delay: (a) limited health care access, (b) too busy to go to the doctor, and (c) dislike of going to the doctor. In fully adjusted models, individuals with more negative SPA were more likely to belong to “limited-access” and “dislike” subgroups compared with the no delay group.
Discussion and Implications:
SPA may affect decision-making processes regarding whether to seek care for worrisome symptoms. Efforts to promote more positive SPA may encourage older adults to be more proactive in addressing their health care needs.
Keywords: Access to and utilization of services, Attitudes and perception toward aging/aged, Health, Physician–patient communication/relationships, Psychosocial, Well-being
Self-perceptions of aging (SPA), or subjective evaluations of one’s own aging experience, have wide-reaching implications for the health of the aging population. According to Levy’s stereotype embodiment theory (Levy, 2009), individuals are exposed to age stereotypes across the life span, and the internalization of these stereotypes as SPA influences health through physiological (Levy, Hausdorff, Hencke, & Wei, 2000), psychological (Levy & Leifheit-Limson, 2009), and behavioral (Levy & Myers, 2004) pathways. Previous research has shown that compared with their more positive counterparts, older adults with more negative SPA have shorter lives (Kotter-Grühn, Kleinspehn-Ammerlahn, Gerstorf, & Smith, 2009; Levy, Slade, Kunkel, & Kasl, 2002), suffer from more functional limitations (Levy, Slade, & Kasl, 2002; Sargent-Cox, Anstey, & Luszcz, 2012), and are less likely to recover from disability (Levy, Slade, Murphy, & Gill, 2012).
How older adults view the aging process affects not only their health status but also their use of health care resources. Evidence from multiple studies of middle-aged and older adults show that individuals with more negative aging self-views are less likely to seek preventive health services (Kim, Moored, Giasson, & Smith, 2014) but more likely to require intensive or emergent care such as hospitalization (Stephan, Sutin, & Terracciano, 2016; Sun, Kim, & Smith, 2017). One explanation for these findings is that older adults with more negative SPA are delaying necessary medical care and suffering from more serious downstream consequences. Few studies, however, have investigated if aging self-perceptions influence older adults’ perceptions of barriers to timely medical care. The purpose of the present study is to examine the association between negative SPA and health care delay as a possible behavioral link between SPA and health services use.
Andersen’s Behavioral Model of Health Services Use
Barriers to primary care are associated with an increased risk of using emergency services, highlighting the importance of timely medical care in reducing the occurrence of serious adverse events (Rust et al., 2008). Andersen’s Behavioral Model of Health Services Use provides a useful framework for studying factors that influence access to care (Andersen, 1995). Predisposing factors (e.g., sociodemographic factors, health beliefs) influence an individual’s propensity to use health care services. Enabling factors (e.g., income, health insurance, regular source of care) are resources that enable or facilitate access to care. Need factors (e.g., disease burden, depressive symptoms) capture how perceived or evaluated health status dictates the use of medical services. Although many studies that use Andersen’s model as a conceptual framework examine factors that increase the likelihood of health care use, the present study uses this theoretical structure for understanding how aging self-perceptions affect short-term health care delay and decrease the likelihood of health care use due to perceived barriers to care. We are interested in the effects of SPA on health care delay above and beyond the influence of known predisposing, enabling, and need predictors of health care utilization.
Within the framework of Andersen’s model, negative SPA may be associated with an increased likelihood to delay care due to (a) lower predisposition to seek care, (b) lack of enabling resources, and (c) lower perceived need for care. As a predisposing factor, SPA may affect older adults’ health beliefs regarding age-related conditions. Goodwin, Black, and Satish (1999) found that individuals who considered arthritis, heart disease, and sleep problems to be a normal part of aging were less likely to receive preventive care services. Negative SPA, therefore, may lower an individual’s propensity to proactively protect their health. Older adults with negative SPA may also lack important enabling resources that facilitate access to care. In one study, older adults who believed nothing could be done to treat age-related conditions were significantly less likely to have a regular physician (Goodwin et al., 1999). Older adults with more negative SPA have also been shown to be less likely to financially plan for retirement (Heraty & McCarthy, 2015). Finally, SPA could be conceptualized as a need factor that affects older adults’ judgments of whether their health problems are of sufficient importance to seek help. In a study of community-dwelling older adults, those who held more negative views of aging were less likely to believe in the importance of discussing age-related issues (e.g., depression, arthritis, memory impairment) with their doctors (Sarkisian, Hays, & Mangione, 2002).
Current Study
In the present study, we use data from the Health and Retirement Study (HRS) to examine whether aging self-perceptions are associated the likelihood of delaying medical care over the next 12 months. HRS collected mail surveys about delay of medical care from two independent subsamples. The first sample completed an in-person HRS interview in 2010 and the Health Care Mail Survey (HCMS) in 2011. The second sample completed an in-person HRS interview in 2012 and the Health Care and Nutrition Study (HCNS) in 2013. We analyzed these two samples separately, performing initial analyses using the 2011 HCMS sample and then replicating our results in the 2013 HCNS sample. We hypothesize that individuals with more negative SPA will be more likely to delay care and report more perceived barriers to care, after adjusting for predisposing, enabling, and need factors.
We also explore the relationship between SPA and the specific reasons for delaying care. Although accessibility issues (e.g., not being able get an appointment soon enough, not having transportation) are important problems to address, we also consider the role of psychosocial factors (e.g., disliking going to the doctor, being afraid of what one might find out) in the decision to postpone care. Previous studies suggest that psychosocial concerns such as physicians’ perceived lack of responsiveness may be a greater disincentive to seeking care than more tangible or practical factors such as medical bills or transportation (Fitzpatrick, Powe, Cooper, Ives, & Robbins, 2004).
Although reporting to be too busy to see the doctor may be related to logistical or scheduling conflicts, it may also serve as an excuse to avoid addressing underlying psychosocial concerns. By shifting causal attributions from an internal stable source (e.g., I do not like going to the doctor) to a more external situational factor (e.g., I am too busy), excuses allow individuals to maintain a positive personal image and a sense of control (Snyder & Higgins, 1988). We, therefore, hypothesize that being too busy will be more closely related to psychosocial rather than access-related reasons for delay.
Instead of analyzing each reason for delay independently, we use latent class analysis to identify unmeasured subgroup membership. We describe the characteristics of each subgroup and then examine if, compared with the no delay group, SPA predicts membership in the delay subgroups. We hypothesize that there will be two distinct delay subgroups: Individuals who delay care due to (a) limited health care access and (b) psychosocial concerns. We predict that SPA will be associated only with membership in the psychosocial subgroup after adjusting for predisposing, enabling, and need factors.
Methods
Participants
The HRS is a nationally representative biennial panel study of U.S. adults aged 51 and older (Sonnega et al., 2014). Respondents who completed an in-person HRS interview also received a self-administered Psychosocial and Lifestyle Leave-Behind Questionnaire that assessed multiple domains of psychosocial functioning, including SPA. The 2011 HCMS and 2013 HCNS examined issues of health care access, including health care delay in the past 12 months. Response rates were 75% and 65% for the HCMS and HCNS, respectively. The final analytic sample size was 2,866 for the 2011 HCMS sample and 2,474 for the 2013 HCNS sample. For a detailed description of the inclusion criteria for both analytic samples, see Supplementary Figures 1 and 2. The HRS protocols are approved by the University of Michigan Health Services Institutional Review Board. The present study was exempted from review because it uses de-identified and publicly available data.
Measures
Self-Perceptions of Aging
In the HRS Psychosocial and Lifestyle Questionnaire, SPA were measured in 2010 and 2012 using an eight-item scale derived from the Philadelphia Morale Scale (Lawton, 1975) and the Berlin Aging Study (http://www.base-berlin.mpg.de/en). On a scale from 1 (strongly disagree) to 6 (strongly agree), respondents indicated the degree to which they endorsed statements such as “Things keep getting worse as I get older” and “So far, I am satisfied with the way I am aging.” Positively worded items were reverse coded, and all items were averaged so that higher scores corresponded to more negative SPA. The final score was set to missing if there were more than four items with missing values. Cronbach’s alpha for the overall scale was 0.82 in 2010 and 0.81 in 2012. For analyses, scores were standardized (μ = 0, σ = 1) to facilitate interpretation and comparison of effect size with other studies of SPA.
Health Care Delay
In the 2011 HCMS and 2013 HCNS, respondents were asked whether they had delayed getting medical care in the last 12 months for any of the following reasons (mark all that apply): (a) I could not get through on the telephone, (b) I could not get an appointment soon enough, (c) Once I get there, I have to wait too long to see the doctor, (d) The clinic/doctor’s office was not open when I could get there, (e) I did not have transportation, (f) I am too busy to go to the doctor, (g) I am afraid of what I might find out, (h) I do not believe in going to doctors, (i) I do not like going to the doctor, and (j) I have not delayed getting medical care in the last 12 months. We expected reasons (a)–(e) to be related to issues of health care access and reasons (f)–(j) to reflect psychosocial concerns. In the 2013 HCNS, additional responses in the “other (specify)” category were coded into existing coding frames or excluded to allow for more direct comparison with the 2011 HCMS. In the 2011 HCMS only, respondents who endorsed delaying care were also asked to mark all types of care delayed: (a) major surgery that would have required a hospital stay of one or more nights, (b) outpatient surgery, (c) seeing the doctor about a symptom or a problem, (d) getting a check-up, (e) routine screening, like a colonoscopy, (f) filling a prescription, and (g) other, specify. Responses in the “other (specify)” category were coded into existing coding frames or excluded from analyses.
Covariates
Covariates from the 2010/2012 in-person interview were included in blocks based on Andersen’s Behavioral Model. Predisposing covariates included sociodemographic variables such as age, gender, race/ethnicity, educational attainment, and living arrangement. Enabling covariates included economic factors such as total household income and health insurance status. Need covariates included health-related factors such as (a) an index of eight chronic conditions (Fisher, Faul, Weir, & Wallace, 2005), (b) an index of eight depressive symptoms, and (c) the number of activities of daily living (ADLs) performed with difficulty (Fonda & Herzog, 2004).
Analysis Strategy
We employed three analytic steps. First, we used logistic regression in Stata 14.0 to examine the association between negative SPA and the likelihood of delaying health care for any of the provided reasons. Respondents were assigned a score of 0 if they marked only the option “I have not delayed getting medical care in the last 12 months” and a score of 1 if they marked at least one of the reasons for delaying medical care. Respondents who indicated that they had not delayed seeking care but also marked one or more reasons for delaying care were excluded due to their conflicting responses (Supplementary Figures 1 and 2). Negative binomial regression was also performed to examine the relationship between negative SPA and the number of reasons given for delaying care. Coefficients were converted to odds ratios (OR) or incidence rate ratios (IRR) for ease of interpretation.
Second, we used MPlus version 7.4 to perform latent class analysis on the subsample of respondents who delayed care to identify subgroups who endorsed similar reasons for postponing care. Binary scores were created to indicate whether respondents did (1) or did not (0) delay care for each reason. Based on a priori hypotheses, one-, two-, and three-class models were tested. Model fit was determined using a combination of information criteria, entropy measures, and likelihood ratio tests (Supplementary Table 1).
Third, respondents were assigned to a delay subgroup based on their highest posterior probability of belonging, and the resulting group memberships were exported to Stata. Using multinomial logistic regression with the no delay group serving as the reference category, we then examined if SPA predicted the likelihood of membership in the three different delay subgroups, after adjusting for blocks of predisposing, enabling, and need factors. Coefficients were converted to relative risk ratios (RRR) for ease of interpretation.
For the logistic, negative binomial, and multinomial logistic regression analyses described previously, we started with an unadjusted model (Model 1) and then created a minimally adjusted model with age and gender (Model 2). Next, we generated models to explore the degree to which additional blocks of predisposing, enabling, and need factors explained the link between SPA and health care delay over and above age and gender. Model 3 included age, gender, and other predisposing variables (race/ethnicity, educational attainment, living arrangement). Model 4 included age, gender, and enabling factors (total household income, health insurance status). Model 5 included age, gender, and need factors (chronic conditions, depressive symptoms, ADL limitations). Finally, Model 6 included all covariates.
Results
Descriptive Analyses
Table 1 shows the descriptive statistics for the 2011 HCMS and 2013 HCNS samples. Both samples were comparable in terms of gender, race, education, health insurance status, and number of depressive symptoms. Respondents in the 2013 HCNS sample, however, were slightly older, had a lower household income, had more chronic conditions, and were more likely to live alone. Over the 1-year follow-up, slightly more respondents in the 2013 HCNS sample reported delaying medical care. In both samples, the most common reasons for delaying care were disliking going to the doctor, being unable to get an appointment soon enough, and being too busy to see the doctor.
Table 1.
Descriptive Statistics From the 2011 HCMS and 2013 HCNS Analytic Study Samplesa
| Study variables | 2011 HCMS (N = 2,866) | 2013 HCNS (N = 2,474) |
|---|---|---|
| Negative SPA, M (SD) | 3.05 (1.04) | 3.13 (1.02) |
| Age, M (SD) | 67.34 (10.32) | 68.18 (9.77) |
| Female, % | 57.92 | 59.50 |
| Race/ethnicity, % | ||
| White | 75.26 | 72.51 |
| Black | 14.03 | 14.92 |
| Hispanic | 8.16 | 9.58 |
| Other | 2.55 | 2.99 |
| Educational attainment, %b | ||
| <High school | 13.22 | 14.96 |
| High school | 57.26 | 54.61 |
| ≥ College | 29.52 | 30.44 |
| Living alone, % | 19.99 | 22.43 |
| Total household income (in thousands), M (SD) | 66.99 (75.01) | 61.50 (87.22) |
| Uninsured, % | 6.07 | 7.28 |
| Chronic illnesses, M (SD) | 2.10 (1.44) | 2.28 (1.48) |
| Depressive symptoms, M (SD) | 1.21 (1.81) | 1.26 (1.85) |
| ADL limitations, M (SD) | 0.25 (0.75) | 0.24 (0.72) |
| Delay for any reason, % | 17.20 | 19.52 |
| I do not like going to the doctor, % | 29.21 | 28.57 |
| I could not get an appointment soon enough, % | 23.53 | 26.71 |
| I am too busy to go to the doctor, % | 22.52 | 23.60 |
| Once I get there, I have to wait too long to see the doctor, % | 18.05 | 15.32 |
| I did not have transportation, % | 15.62 | 13.66 |
| I am afraid of what I might find out, % | 14.20 | 14.49 |
| I could not get through on the telephone, % | 11.16 | 7.45 |
| The clinic/doctor’s office was not open when I could get there, % | 7.91 | 6.83 |
| I do not believe in going to doctors, % | 3.85 | 1.86 |
Note: ADL = activities of daily living; HCMS = Health Care Mail Survey; HCNS = Health Care and Nutrition Study; SPA = self-perceptions of aging.
aUnweighted sample data. bPercentages may not sum to 100% due to rounding.
SPA and Health Care Delay
After adjusting for age, gender, and other predisposing factors (Model 3), each standard deviation (SD) increase in negative SPA was associated with a 49% higher likelihood of health care delay in the 2011 sample and a 57% higher likelihood of health care delay in the 2013 sample (Table 2). Individuals with more negative SPA were not only more likely to delay care overall but also reported more reasons for delay. Although the effect size was somewhat diminished with each block of covariates, the association between SPA and health care delay remained significant across all models. Compared with the minimally adjusted model with age and gender (Model 2), the largest incremental decrease in OR/IRR occurred after adding need factors in Model 5.
Table 2.
Negative Self-Perceptions of Aging and OR for Health Care Delay and IRR for Number of Reasons for Delay for 2011 HCMS and 2013 HCNS Samples
| 2011 (N = 2,866) | 2013 (N = 2,474) | ||||
|---|---|---|---|---|---|
| Delay (yes/no) | Number of reasons | Delay (yes/no) | Number of reasons | ||
| Model | Covariates | OR (95% CI) | IRR (95% CI) | OR (95% CI) | IRR (95% CI) |
| 1 | Unadjusted | 1.36 (1.24–1.50) | 1.40 (1.28–1.54) | 1.47 (1.33–1.63) | 1.41 (1.29–1.55) |
| 2 | Age + gender | 1.49 (1.35–1.65) | 1.50 (1.37–1.65) | 1.60 (1.44–1.78) | 1.47 (1.34–1.60) |
| 3 | Age + gender + predisposinga | 1.49 (1.34–1.65) | 1.50 (1.37–1.65) | 1.57 (1.41–1.75) | 1.45 (1.33–1.59) |
| 4 | Age + gender + enablingb | 1.47 (1.32–1.63) | 1.47 (1.33–1.61) | 1.58 (1.42–1.76) | 1.46 (1.34–1.60) |
| 5 | Age + gender + needc | 1.25 (1.11–1.41) | 1.30 (1.17–1.45) | 1.41 (1.25–1.60) | 1.33 (1.21–1.48) |
| 6 | All covariatesd | 1.25 (1.11–1.42) | 1.31 (1.17–1.46) | 1.40 (1.24–1.59) | 1.33 (1.20–1.47) |
Note: ADL = activities of daily living; CI = confidence interval; HCMS = Health Care Mail Survey; HCNS = Health Care and Nutrition Study; OR = odds ratio; IRR = incidence rate ratio. p < .001 for all analyses.
aPredisposing: race/ethnicity, educational attainment, living arrangement. bEnabling: total household income, health insurance status. cNeed: chronic illnesses, depressive symptoms, ADL limitations. dAll covariates: age, gender, race/ethnicity, educational attainment, living arrangement, total household income, health insurance status, chronic illnesses, depressive symptoms, ADL limitations.
Latent Class Analyses
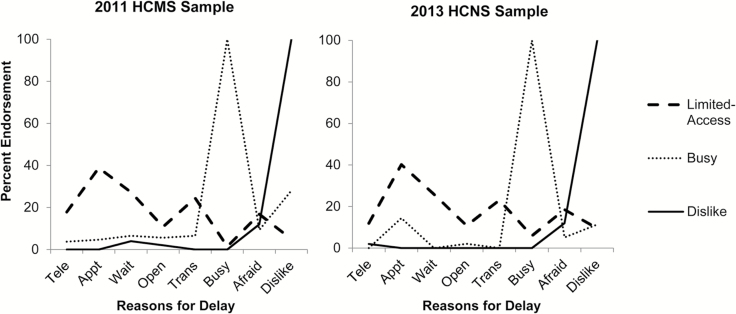
Latent class analysis was used to identify unobservable subgroups in our sample. The reason “I do not believe in going to doctors” was excluded from latent class analyses due to low endorsement (Table 1). Latent class analyses revealed a three-class model to be the best fit to the data among the three models tested (Supplementary Table 1). Figure 1 shows the pattern of endorsement for each of the eight delay reasons by latent subgroup.
Figure 1.
Percent endorsement of each reason for delay by latent subgroup for the 2011 Health Care Mail Survey (HCMS) and the 2013 Health Care and Nutrition Study (HCNS) samples. Tele = I could not get through on the telephone; Appt = I could not get an appointment soon enough; Wait = Once I get there, I have to wait too long to see the doctor; Open = The clinic/doctor’s office was not open when I could get there; Trans = I did not have transportation; Busy = I am too busy to go to the doctor; Afraid = I am afraid of what I might find out; Dislike = I do not like going to the doctor. Limited-access = latent subgroup defined primarily by delay due limited health care access; Busy = latent subgroup defined primarily by delay due to being too busy to go to the doctor; Dislike = latent subgroup defined primarily by delay due to disliking going to the doctor.
The characteristics of the three subgroups were remarkably similar between the two HRS samples. The largest subgroup (>50% of respondents) consisted of individuals who delayed care primarily due to limited health care access. Although each of the five access-related issues were reported by some members of the “limited-access” subgroup, inability to get appointments soon enough and lack of transportation were the most prominent reasons for delay in this subgroup. The other subgroups were predominantly characterized by a single reason for delay. In the “busy” subgroup, all respondents reported being too busy to see the doctor, and all respondents in the “dislike” subgroup reported disliking going to the doctor. These two subgroups were comparable in size, each consisting of roughly 20% of respondents. Interestingly, “being afraid of what I might find out” was similarly endorsed by all three subgroups.
Descriptive Statistics for Subgroups of Delay
Table 3 describes the characteristics of the no delay group and the three delay subgroups. Compared with the no delay group, all three delay subgroups were significantly younger. Respondents in the limited-access subgroup were worse off in almost all respects: more negative SPA, lower household income, lower educational attainment, more chronic conditions, more depressive symptoms, more ADL limitations, and more likely to be uninsured. In terms of race/ethnicity, a larger proportion of minority respondents belonged to the limited-access subgroup. Respondents in the busy subgroup had a wealthier and healthier profile: higher household income, higher educational attainment, and fewer chronic conditions. The busy subgroup, however, was more likely to be uninsured in the 2011 sample. The busy subgroup was the only subgroup with similar levels of SPA compared with the no delay group. Finally, the dislike subgroup differed from the no delay group at a psychological level: more negative SPA and more depressive symptoms. However, the dislike subgroup had fewer chronic conditions in the 2011 sample and was more likely to be uninsured in the 2013 sample.
Table 3.
Descriptive Statistics for Latent Subgroups of Delay in the 2011 HCMS and 2013 HCNS Samplesa
| 2011 HCMS sample | 2013 HCNS sample | |||||||
|---|---|---|---|---|---|---|---|---|
| Covariates | No delay (n = 2,373) | Limited-access (n = 286) | Busy (n = 107) | Dislike (n = 100) | No delay (n = 1,991) | Limited-access (n = 286) | Busy (n = 97) | Dislike (n = 100) |
| Negative SPA, M (SD) | 2.99 (1.02) | 3.41 (1.03) | 3.02 (1.08) | 3.36 (1.05) | 3.05 (1.00) | 3.54 (1.03) | 3.11 (0.99) | 3.51 (1.08) |
| Age, M (SD) | 68.38 (10.14) | 63.31 (10.42) | 59.71 (7.97) | 62.56 (9.01) | 69.30 (9.61) | 64.18 (9.38) | 60.03 (7.30) | 65.20 (8.87) |
| Female, % | 57.61 | 60.14 | 64.49 | 52.00 | 59.02 | 60.84 | 63.92 | 61.00 |
| Race/ethnicity, %b | ||||||||
| White | 76.86 | 59.44 | 74.77 | 83.00 | 74.38 | 56.29 | 78.35 | 76.00 |
| Black | 13.70 | 20.28 | 9.35 | 9.00 | 14.41 | 21.33 | 10.31 | 11.00 |
| Hispanic | 6.78 | 18.18 | 13.08 | 7.00 | 8.49 | 17.13 | 7.22 | 12.00 |
| Other | 2.65 | 2.10 | 2.80 | 1.00 | 2.71 | 5.24 | 4.12 | 1.00 |
| Educational attainment, %b | ||||||||
| <High school | 12.52 | 20.63 | 8.41 | 14.00 | 14.21 | 24.13 | 3.09 | 15.00 |
| High school | 57.99 | 54.90 | 43.93 | 61.00 | 55.20 | 49.30 | 46.39 | 66.00 |
| ≥ College | 29.50 | 24.48 | 47.66 | 25.00 | 30.59 | 26.57 | 50.52 | 19.00 |
| Living alone, % | 20.56 | 19.93 | 12.15 | 15.00 | 21.60 | 27.97 | 21.65 | 24.00 |
| Total household income (in thousands), M (SD) | 67.45 (74.16) | 49.33 (65.99) | 100.80 (98.79) | 70.57 (76.92) | 62.90 (90.75) | 43.83 (50.44) | 102.67 (114.56) | 44.17 (38.79) |
| Uninsured, % | 4.89 | 13.29 | 10.28 | 9.00 | 5.17 | 17.48 | 9.28 | 18.00 |
| Chronic illnesses, M (SD) | 2.10 (1.42) | 2.34 (1.52) | 1.70 (1.30) | 1.69 (1.53) | 2.29 (1.45) | 2.58 (1.58) | 1.58 (1.53) | 1.99 (1.44) |
| Depressive symptoms, M (SD) | 1.05 (1.66) | 2.31 (2.36) | 1.31 (1.87) | 1.66 (2.18) | 1.09 (1.71) | 2.33 (2.38) | 1.33 (1.59) | 1.66 (2.06) |
| ADL limitations, M (SD) | 0.23 (0.71) | 0.49 (1.04) | 0.12 (0.56) | 0.21 (0.70) | 0.22 (0.68) | 0.46 (1.00) | 0.13 (0.61) | 0.21 (0.46) |
Note: ADL = activities of daily living; HCMS = Health Care Mail Survey; HCNS = Health Care and Nutrition Study; SPA = self-perceptions of aging. Busy = latent subgroup defined primarily by delay due to being too busy to go to the doctor; dislike = latent subgroup defined primarily by delay due to disliking going to the doctor; limited-access = latent subgroup defined primarily by delay due limited health care access.
aUnweighted sample data. bPercentages may not sum to 100% due to rounding.
In the 2011 HCMS, respondents who endorsed delaying care in the past 12 months were also asked about the types of care delayed. The most common types of care delayed were seeing the doctor for a symptom or problem (52.13%), getting a check-up (28.80%), and getting routine screening (21.70%). In comparing the three subgroups, the busy subgroup was significantly more likely than the limited-access subgroup to delay preventative care services such as check-ups (40.19% vs 24.48%) and routine screenings (30.84% vs 17.48%; Supplementary Figure 3).
SPA and Delay Subgroup Membership
Table 4 presents the association between negative SPA and delay subgroup membership by model. In the unadjusted model, respondents with more negative SPA were more likely to belong to the limited-access subgroup compared with the no delay group in both the 2011 (RRR = 1.49, 95% CI = 1.32–1.69, p < .001) and 2013 (RRR = 1.61, 95% CI = 1.42–1.83, p < .001) samples. The association between SPA and access-related delay remained significant in all models, including the final model where each SD increase in negative SPA increased the likelihood of belonging to the limited-access subgroup by 18% in 2011 and 36% in 2013.
Table 4.
Negative Self-Perceptions of Aging and RRR of Membership in Latent Subgroups of Delay for 2011 HCMS and 2013 HCNS Samples
| 2011 HCMS sample | 2013 HCNS sample | ||||||
|---|---|---|---|---|---|---|---|
| Limited-access (n = 286) | Busy (n = 107) | Dislike (n = 100) | Limited-access (n = 286) | Busy (n = 97) | Dislike (n = 100) | ||
| Model | Covariates | RRR (95% CI) | RRR (95% CI) | ||||
| 1 | Unadjusted | 1.49 (1.32–1.69)** | 1.02 (0.84–1.24) | 1.43 (1.17–1.74)** | 1.61 (1.42–1.83)** | 1.05 (0.86–1.30) | 1.57 (1.29–1.92)** |
| 2 | Age + gender | 1.61 (1.42–1.82)** | 1.16 (0.96–1.42) | 1.55 (1.27–1.89)** | 1.73 (1.52–1.97)** | 1.20 (0.97–1.47) | 1.68 (1.37–2.05)** |
| 3 | Age + gender + predisposinga | 1.58 (1.39–1.79)** | 1.24 (1.02–1.51)* | 1.52 (1.24–1.86)** | 1.67 (1.46–1.90)** | 1.27 (1.03–1.58)* | 1.61 (1.31–1.98)** |
| 4 | Age + gender + enablingb | 1.50 (1.32–1.71)** | 1.24 (1.01–1.52)* | 1.56 (1.27–1.90)** | 1.65 (1.45–1.88)** | 1.26 (1.02–1.56)* | 1.61 (1.31–1.97)** |
| 5 | Age + gender + needc | 1.18 (1.02–1.38)* | 1.17 (0.93–1.48) | 1.59 (1.25–2.01)** | 1.37 (1.18–1.59)** | 1.27 (1.00–1.61) | 1.75 (1.38–2.21)** |
| 6 | All covariatesd | 1.18 (1.01–1.37)* | 1.23 (0.97–1.56) | 1.55 (1.22–1.97)** | 1.36 (1.17–1.58)** | 1.33 (1.04–1.70)* | 1.67 (1.32–2.12)** |
Note: ADL = activities of daily living; CI = confidence interval; HCMS = Health Care Mail Survey; HCNS = Health Care and Nutrition Study; RRR = relative risk ratio. Busy = latent subgroup defined primarily by delay due to being too busy to go to the doctor; dislike = latent subgroup defined primarily by delay due to disliking going to the doctor; limited-access = latent subgroup defined primarily by delay due limited health care access; reference group = no delay group.
aPredisposing: race/ethnicity, educational attainment, living arrangement. bEnabling: total household income, health insurance status. cNeed: chronic illnesses, depressive symptoms, ADL limitations. dAll covariates: age, gender, race/ethnicity, educational attainment, living arrangement, total household income, health insurance status, chronic illnesses, depressive symptoms, ADL limitations.
*p < .05, **p < .001.
In the unadjusted model, there was no significant association between negative SPA and belonging to the busy subgroup compared with the no delay group, likely due to the relatively similar levels of SPA between the two groups. After adjusting for age, gender, and predisposing factors (Model 3) or enabling factors (Model 4), the relationship between SPA and busy subgroup membership became significant, suggesting the presence of suppression effects. Despite fluctuations in significance across models, the point estimates are relatively similar in magnitude for Models 2–6. A larger sample size may be needed to reveal the degree to which negative SPA is consistently related to busy delay subgroup membership.
Individuals with more negative SPA were more likely to belong to the dislike subgroup in all models. Although there were slight fluctuations in effect size after adjusting for different blocks of covariates, the relationship between SPA and dislike subgroup membership remained robust. After adjusting for all covariates, every SD increase in negative SPA increased the likelihood of belonging to the dislike subgroup by 55% in the 2011 sample and 67% in the 2013 sample.
Discussion
Based on Levy’s stereotype embodiment theory, we explored health care delay as a behavioral explanation for why older adults with more negative aging attitudes experience worse health outcomes. Previous research suggests that total patient delay can be broken down into a series of conceptually distinct stages with unique predictors of delay at each point (Safer, Tharps, Jackson, & Leventhal, 1979). Although SPA may affect earlier stages of delay such as the initial detection of unexplained signs/symptoms to disease inference (e.g., appraisal delay) and disease inference to the decision to seek medical help (e.g., illness delay), the present study examined the association between SPA and utilization delay, or delays in seeing the doctor after determining the need to seek medical attention. Consistent with our hypothesis, individuals with more negative SPA were not only more likely to delay care but also cited more reasons for delaying care, even after adjusting for predisposing, enabling, and need factors based on Andersen’s Behavioral Model of Health Services Use.
We then used a person-centered approach to identify latent subgroups of delay and examined if SPA scores predicted subgroup membership. As hypothesized, one of the subgroups was characterized by limited health care access. Older adults with more negative SPA were more likely to belong to the limited-access subgroup, whose members tended to be more socioeconomically disadvantaged and in poorer health. Although we did not expect SPA to influence the perception of practical barriers to care, it is plausible that individuals with negative SPA are less likely to persevere in the face of daily inconveniences. Endorsement of negative age stereotypes has been associated with the belief that health outcomes are in the control of powerful others or up to chance (Sargent-Cox & Anstey, 2015), and external factors such as prolonged wait times may be a sufficient deterrent for seeking care among those who are nihilistic or fatalistic in their views of aging. Conversely, those with more positive SPA may be more persistent in their efforts and seek additional resources to get their health care needs met.
Counter to expectations, the busy delay subgroup was distinct from both the dislike and limited-access delay subgroups. Although we hypothesized that being too busy served as a psychosocial excuse for delaying care, being busy may not entail an active avoidance of health care encounters but rather a prioritization of other commitments. Individuals may report being too busy to seek care because they perceive an incompatibility between their own availability and the availability of potential sources of health care. A glimpse at the descriptive statistics provides some insight into the characteristics of individuals who say they are too busy to seek care. Although the busy subgroup had similar levels of SPA compared with the no delay group, respondents in the busy subgroup were younger and had higher household incomes, higher educational attainment, and fewer chronic conditions. The busy subgroup may represent older adults who are still functioning at a high level and delaying care because they are actively engaged in work or community activities. Indeed, a significantly larger percentage of respondents in the busy subgroup reported not being retired compared with the other delay subgroups. For these individuals, SPA may only matter in select circumstances and/or play only a small role in their decision-making process regarding whether to seek care.
Finally, older adults with more negative SPA were more likely to belong to the subgroup who disliked going to the doctor. Although only approximately 20% of respondents belonged to the dislike subgroup, disliking going to the doctor was the most cited reason for delaying care among all respondents. The Communication Predicament of Aging Model (Ryan, Giles, Bartolucci, & Henwood, 1986) depicts how negative age stereotypes can influence the quality of interactions between older adults and health professionals, causing older adults to evaluate their health care experience more negatively. Physicians may adopt over-accommodating patterns of speech, sometimes referred to as patronizing communication (Ryan, Hummert, & Boich, 1995) or elderspeak (Kemper, 1994), based on stereotyped expectations about the aging process. Older adults with negative SPA may then embody negative age stereotypes by acting in a dependent manner and inadvertently contribute to the paternalistic behavior displayed by health care professionals. These well-intentioned but overly supportive patterns of speech and behavior by formal/informal care providers can negatively affect the psychological well-being of older adults by activating negative age stereotypes and solidifying the notion that aging is inexorably linked with increased dependence and functional limitations (Kwak, Ingersoll-Dayton, & Burgard, 2014; Williams, Kemper, & Hummert, 2004).
For all three subgroups in the 2011 sample, the most common type of care delayed was seeing the doctor for a symptom or problem. As older adults begin experiencing more age-related declines, they may find it more difficult to distinguish symptoms of “old age” from more worrisome symptoms that may be indicative of serious health conditions. Prior research found that older adults who attributed a recent heart attack/stroke to “old age” were less likely to make lifestyle changes and had higher rates of health care utilization (e.g., hospitalization) over follow-up (Stewart, Chipperfield, Perry, & Hamm, 2016). Promoting more positive aging self-perceptions may help older adults counter automatic old age attributions and take time to more critically evaluate their symptoms. Consequently, older adults with more positive views on aging may interpret new bodily discomforts as cues for seeking medical attention rather than inevitable products of the aging process.
There are several limitations to the present study that should be addressed. First, we used a select sample of respondents who met specific inclusion criteria. HRS does not provide weights for respondents who complete both the Psychosocial and Lifestyle Questionnaire and an off-year study. Although we were unable to weight our analytic samples to represent the U.S. population aged 51 and older, we replicated our results in two distinct samples of older adults, increasing confidence in the robustness of our findings. In predicting delay subgroup membership, we assigned respondents to the subgroup to which they had the highest posterior probability of belonging. Although we did not explicitly account for uncertainty of group membership in our analyses, the average probability of membership was greater than .85 for all groups. Additionally, our measure of health care delay was based on self-report, and thus, may reflect subjective rather than objective assessments of barriers to health care. Perceived barriers to care, however, may be just as important as actual barriers in predicting care-seeking behaviors. Finally, the reasons for delay did not capture all possible barriers to seeking medical care, and future work should examine a broader range of social, psychological, and cognitive factors as contributors to delay.
Despite these limitations, the present study adds to the literature on SPA and health by delving deeper into how aging attitudes affect perceived barriers to timely medical care. On a theoretical level, we emphasize the importance of studying not only the behavior of interest (e.g., health care delay) but also the underlying cognitive and emotional processes that guide health care decision making. We highlight the role of psychosocial reasons in determining health care delay and draw attention to the fact disliking going to the doctor ranks highly among older adults as a justification for postponing care. Understanding the extent to which age stereotypes serve as a basis for these negative feelings toward care providers and/or the health care system will further inform efforts on how to improve doctor-patient communication and prevent the undertreatment or overtreatment of age-related conditions.
From a methodological perspective, the present study measured SPA prior to asking about health care delay and controlled for a comprehensive list of covariates. Many studies interview patients about the timing and reasons for delay after the occurrence of a serious health event such as hospitalization (Weissman, Stern, Fielding, & Epstein, 1991). These negative health events, however, may color how older adults remember the decisions and behaviors that contributed to their current state. By using a prospective design with a 1-year follow-up, we were able to ask about delay in the context of everyday life and infer how SPA affects short-term health care decisions.
The pervasiveness of age stereotypes in contemporary American society is shaping the way in which individuals think, feel, and behave as they enter their later years. With the unprecedented number of Baby Boomers reaching old age, ensuring that the aging population has access to the resources they need to maintain high levels of physical, psychological, and social functioning has become a top priority. Although the current study focuses on the effect of older adults’ aging attitudes on health care use, it is also important to consider how clinicians’ views on aging and ageism within the health care system may interact with older adults’ self-views to influence the delivery of high-quality health care (Davis, Bond, Howard, & Sarkisian, 2011; Meisner, 2012; Ouchida & Lachs, 2015). To help older adults view aging in a more positive light and more effectively manage their own health, policymakers and practitioners must take a multifaceted approach and address the issue of age stereotypes and health care delay from individual, institutional, and societal levels.
Supplementary Material
Supplementary data is available at The Gerontologist online.
Funding
The Health and Retirement Study is conducted by the Institute for Social Research at the University of Michigan, with grants from the National Institute on Aging (U01AG009740) and the Social Security Administration. J. K. Sun’s contribution was partially funded by the National Institute on Aging (T32AG027708). J. Smith’s contribution was partially funded by the National Institute on Aging (U01AG009740 and R01AG040635). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. This paper was published as part of a supplement sponsored and funded by AARP. The statements and opinions expressed herein by the authors are for information, debate, and discussion, and do not necessarily represent official policies of AARP.
Supplementary Material
References
- Andersen R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10. doi:10.2307/2137284 [PubMed] [Google Scholar]
- Davis M. M., Bond L. A., Howard A., & Sarkisian C. A (2011). Primary care clinician expectations regarding aging. Gerontologist, 51, 856–866. doi:10.1093/geront/gnr017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher G. G., Faul J. D., Weir D. R., & Wallace R. B (2005). Documentation of chronic disease measures in the Health and Retirement Study (HRS/AHEAD). Ann Arbor: University of Michigan; Retrieved March 14, 2017, from http://hrsonline.isr.umich.edu/index.php?p=userg [Google Scholar]
- Fitzpatrick A. L., Powe N. R., Cooper L. S., Ives D. G., & Robbins J. A (2004). Barriers to health care access among the elderly and who perceives them. American Journal of Public Health, 94, 1788–1794. doi:10.2105/AJPH.94.10.1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonda S., & Herzog A. R. 2004. Documentation of physical functioning measures in the Health and Retirement Study and the Asset and Health Dynamics among the Oldest Old Study. Ann Arbor: University of Michigan; Retrieved March 14, 2017, from http://hrsonline.isr.umich.edu/index.php?p=userg [Google Scholar]
- Goodwin J. S., Black S. A., & Satish S (1999). Aging versus disease: The opinions of older Black, Hispanic, and Non-Hispanic White Americans about the causes and treatment of common medical conditions. Journal of the American Geriatrics Society, 47, 973–979. doi:10.1111/j.1532–5415.1999.tb01293.x [DOI] [PubMed] [Google Scholar]
- Heraty N., & McCarthy J (2015). Unearthing psychological predictors of financial planning for retirement among late career older workers: Do self-perceptions of aging matter? Work, Aging and Retirement, 1, 274–283. doi:10.1093/workar/wav008 [Google Scholar]
- Kemper S. (1994). Elderspeak: Speech accommodations to older adults. Aging, Neuropsychology, and Cognition, 1, 17–28. doi:10.1080/09289919408251447 [Google Scholar]
- Kim E. S., Moored K. D., Giasson H. L., & Smith J (2014). Satisfaction with aging and use of preventive health services. Preventive Medicine, 69, 176–180. doi:10.1016/j.ypmed.2014.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter-Grühn D., Kleinspehn-Ammerlahn A., Gerstorf D., & Smith J (2009). Self-perceptions of aging predict mortality and change with approaching death: 16-year longitudinal results from the Berlin Aging Study. Psychology and Aging, 24, 654–667. doi:10.1037/a0016510 [DOI] [PubMed] [Google Scholar]
- Kwak M., Ingersoll-Dayton B., & Burgard S (2014). Receipt of care and depressive symptoms in later life: The importance of self-perceptions of aging. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69, 325–335. doi:10.1093/geronb/gbt128 [DOI] [PubMed] [Google Scholar]
- Lawton M. P. (1975). The Philadelphia geriatric center morale scale: A revision. Journal of Gerontology, 30, 85–89. doi:10.1093/geronj/30.1.85 [DOI] [PubMed] [Google Scholar]
- Levy B. R. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332–336. doi:10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B. R., Hausdorff J. M., Hencke R., & Wei J. Y (2000). Reducing cardiovascular stress with positive self-stereotypes of aging. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 55, 205–213. doi:10.1093/geronb/55.4.P205 [DOI] [PubMed] [Google Scholar]
- Levy B. R., & Leifheit-Limson E (2009). The stereotype-matching effect: Greater influence on functioning when age stereotypes correspond to outcomes. Psychology and Aging, 24, 230–233. doi:10.1037/a0014563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B. R., & Myers L. M (2004). Preventive health behaviors influenced by self-perceptions of aging. Preventive Medicine, 39, 625–629. doi:10.1016/j.ypmed.2004.02.029 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Slade M. D., & Kasl S. V (2002). Longitudinal benefit of positive self-perceptions of aging on functional health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57, 409–417. doi:10.1093/geronb/57.5.P409 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Slade M. D., Kunkel S. R., & Kasl S. V (2002). Longevity increased by positive self-perceptions of aging. Journal of Personality and Social Psychology, 83, 261–270. doi:10.1037/0022-3514.83.2.261 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Slade M. D., Murphy T. E., & Gill T. M (2012). Association between positive age stereotypes and recovery from disability in older persons. JAMA, 308, 1972–1973. doi:10.1001/jama.2012.14541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisner B. A. (2012). Physicians’ attitudes toward aging, the aged, and the provision of geriatric care: A systematic narrative review. Critical Public Health, 22, 61–72. doi:10.1080/09581596.2010.539592 [Google Scholar]
- Ouchida K. M., & Lachs M. S (2015). Not for doctors only: Ageism in healthcare. Generations, 39, 46–57. Retrieved March 14, 2017, from http://www.asaging.org/generations-journal-american-society-aging [Google Scholar]
- Ryan E. B., Giles H., Bartolucci G., & Henwood K (1986). Psycholinguistic and social psychological components of communication by and with the elderly. Language & Communication, 6, 1–24. doi:10.1016/0271-5309(86)90002–9 [Google Scholar]
- Ryan E. B., Hummert M. L., & Boich L. H (1995). Communication predicaments of aging patronizing behavior toward older adults. Journal of Language and Social Psychology, 14, 144–166. doi:10.1177/0261927X95141008 [Google Scholar]
- Rust G., Ye J., Baltrus P., Daniels E., Adesunloye B., & Fryer G. E (2008). Practical barriers to timely primary care access: Impact on adult use of emergency department services. Archives of Internal Medicine, 168, 1705–1710. doi:10.1001/archinte.168.15.1705 [DOI] [PubMed] [Google Scholar]
- Safer M. A., Tharps Q. J., Jackson T. C., & Leventhal H (1979). Determinants of three stages of delay in seeking care at a medical clinic. Medical Care, 17, 11–29. doi:10.1097/00005650-197901000-00002 [DOI] [PubMed] [Google Scholar]
- Sargent-Cox K., & Anstey K. J (2015). The relationship between age-stereotypes and health locus of control across adult age-groups. Psychology & Health, 30, 652–670. doi:10.1080/08870446.2014.974603 [DOI] [PubMed] [Google Scholar]
- Sargent-Cox K. A., Anstey K. J., & Luszcz M. A (2012). The relationship between change in self-perceptions of aging and physical functioning in older adults. Psychology and Aging, 27, 750–760. doi:10.1037/a0027578 [DOI] [PubMed] [Google Scholar]
- Sarkisian C. A., Hays R. D., & Mangione C. M (2002). Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. Journal of the American Geriatrics Society, 50, 1837–1843. doi:10.1046/j.1532-5415.2002.50513.x [DOI] [PubMed] [Google Scholar]
- Snyder C. R., & Higgins R. L (1988). Excuses: Their effective role in the negotiation of reality. Psychological Bulletin, 104, 23–35. doi:10.1037//0033-2909.104.1.23 [DOI] [PubMed] [Google Scholar]
- Sonnega A., Faul J. D., Ofstedal M. B., Langa K. M., Phillips J. W., & Weir D. R (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43, 576–585. doi:10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y., Sutin A. R., & Terracciano A (2016). Feeling older and risk of hospitalization: Evidence from three longitudinal cohorts. Health Psychology, 35, 634–637. doi:10.1037/hea0000335 [DOI] [PubMed] [Google Scholar]
- Stewart T. L., Chipperfield J. G., Perry R. P., & Hamm J. M (2016). Attributing heart attack and stroke to “old age”: Implications for subsequent health outcomes among older adults. Journal of Health Psychology, 21, 40–49. doi:10.1177/1359105314521477 [DOI] [PubMed] [Google Scholar]
- Sun J. K., Kim E. S., & Smith J (2017). Positive self-perceptions of aging and lower rate of overnight hospitalization in the US population over age 50. Psychosomatic Medicine, 79, 81–90. doi:10.1097/psy.0000000000000364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman J. S., Stern R., Fielding S. L., & Epstein A. M (1991). Delayed access to health care: Risk factors, reasons, and consequences. Annals of Internal Medicine, 114, 325–331. doi:10.7326/0003-4819-114-4-325 [DOI] [PubMed] [Google Scholar]
- Williams K., Kemper S., & Hummert M. L (2004). Enhancing communication with older adults: Overcoming elderspeak. Journal of Gerontological Nursing, 30, 17–25. doi:10.3928/0098-9134-20041001-08 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.