Abstract
Purpose of the Study:
This study examined whether caregiving has a differential effect on the well-being of sibling caregivers relative to other caregiving groups and whether race moderates this effect.
Design and Methods:
Using the National Survey of Midlife Development in the United States, 631 family caregivers (including 61 sibling caregivers) and 4,944 noncaregivers were identified. Hierarchical regression analyses were conducted to estimate the effect of the caregiver-care recipient relationship and its interaction with race on caregivers’ well-being (i.e., depressive symptoms, self-rated health, life satisfaction, and perceived control over life).
Results:
Caregivers in general reported poorer well-being than noncaregivers, but sibling caregivers were less affected by caregiving than parent or spouse caregivers. Among sibling caregivers, caregiving took a significantly greater toll on non-Hispanic White caregivers than those from minority groups with respect to depressive symptoms and life satisfaction.
Implication:
The findings suggest that the experience of sibling caregivers is significantly shaped by their cultural background.
Keywords: Race, Caregiving-informal, Caregiving stress, Kinship relationship, Sibling caregivers
Introduction
A growing body of research on the long-term effects of caregiving consistently finds evidence for the toll of caregiving. However, among caregivers, the role of siblings has received little attention. Typically in studies of family caregiving, siblings have been treated as “other” caregivers (Litwin, Stoeckel, & Roll, 2014; Marks, Lambert, & Choi, 2002). Yet, it is important to study sibling caregivers as a distinct group, as they are likely to play a larger caregiving role in the future given two population trends: (i) the increased longevity of individuals with disabilities who now often outlive their parents but have lifelong needs for care (Bittles et al., 2002) and (ii) changes in marital patterns of baby boomers—higher rates of divorce and fewer marriages compared with earlier cohorts (Kreider, 2005). Further, there is growing evidence that there are differential effects of caregiving depending on the race/ethnicity of a caregiver (Dilworth-Anderson et al., 2005). Thus, the present study examined whether caregiving has a differential effect on the well-being of sibling caregivers relative to other caregiving groups and whether race moderates this effect.
Caregivers’ Well-being and Their Kinship Relationship to Care Recipients
Most of the comparative research on caregiving by kinship relationship has contrasted spouse versus adult child caregivers. Based on a meta-analysis of 168 empirical studies comparing caregiving spouses with adult children or children-in-law, Pinquart and Sörensen (2011) found that spouse caregivers reported higher levels of depressive symptoms, greater financial and physical burden, and lower levels of psychological well-being than adult child or child-in-law caregivers. However, there is some conflicting evidence. Chumbler, Grimm, Cody, and Beck (2003) found no difference in the level of burden between spouse and adult child caregivers based on a random sample of family caregivers of elders with cognitive impairment, and Chappell, Dujela, and Smith (2014), in a study of family caregivers of elders with dementia, reported higher levels of caregiving burden and more negative outcomes among adult child caregivers compared with spouse caregivers.
A second less extensive body of comparative caregiving research has examined whether caregiving takes a greater toll on parents caring for children with disabilities than adult children or spouses caring for frail elders. Studies based on representative samples in Europe (Survey of Health Ageing and Retirement in Europe; Litwin, et al., 2014) and in the United States (Midlife Development in the United States; Zehner Ourada & Walker, 2014) found higher levels of depressive symptoms and poorer physical health experienced by parent caregivers than adult child caregivers, presumably due to the longer-term nature of their caregiving responsibilities. However, other studies comparing parental caregivers of children with disabilities to spouse caregivers found that parental caregivers perceive their health as better and report higher levels of life satisfaction and lower levels of depression (e.g., McPherson, Pentland, & McNaughton, 2000).
The Well-being of Sibling Caregivers
Only recently have studies compared sibling caregivers with other groups of family caregivers. A number of studies suggest that sibling caregivers fare better than other caregivers. Penning and Wu (2015) found that among middle-aged and older caregivers, caring for a sibling was associated with less stress and better mental health than caring for a spouse or a child. Based on data from 19 countries participating in the WHO Mental Health Surveys, Viana and colleagues (2013) found that among caregivers of individuals with chronic physical and mental health conditions, siblings reported fewer burdens than caregivers of spouses, children, or parents. In an analysis of those respondents aged 50 and older in the above-mentioned WHO Surveys, Shahly and colleagues (2013) reported that spouse and parent caregivers reported higher levels of burden than sibling and adult child caregivers.
Studies of caregivers of a brother or sister with a mental illness (MI) also suggest that caregiving may take less of a toll on sibling caregivers compared with parental caregivers (Chen & Lukens, 2011; Hsiao & Tsai, 2015). The lower likelihood that sibling caregivers co-reside with the care recipients and thus are less exposed to behavior problems that caregivers find stressful may partially explain their better well-being. In addition, siblings may feel a greater choice in taking on the caregiving role than parents, adult children, or spouses, and therefore caregiving may be less likely to lead to an erosion of feelings of personal mastery (Pearlin, Mullan, Semple, & Skaff, 1990).
However, there are several theoretical reasons for hypothesizing that siblings may experience considerable distress from the caregiving role. First, by midlife, siblings are likely to have significant competing work and family responsibilities, and thus additional obligations to provide care for their brother or sister can be physically, emotionally, and financially daunting (Hatfield & Lefley, 2005; Lohrer, Lukens, & Thorning, 2007). Second, research suggests that non-normative life events are more stressful than normative ones (Bell & Lee, 2008). In our society, caregiving for an aging spouse, child, or parent is a more normative role than caring for a sibling, as supported by the research of Reinhard and Horwitz (1995) who found evidence that siblings interpret caregiving as more non-normative than parents. Third, professionals may fail to involve siblings in the patient’s care because, in part, there is not the same expectation that siblings will take on an active caregiving role. Hatfield and Lefley (2005) found that mental health providers were less willing to share information about their patient with a sibling caregiver than a spouse or parent caregiver, even if he or she was the primary caregiver. Therefore, compared with other caregivers, siblings may experience countervailing factors, some of which lower their level of burden (e.g., living apart from the care receiver) and others that increase their level of burden (e.g., assuming a non-normative role, less support from the service system).
Several trends suggest that sibling caregiving might become a more normative role in the future. Data indicate that baby boomers not only have an increased rate of divorce but fewer marry compared with earlier cohorts (Kreider, 2005). As a result, fewer baby boomers have children or a spouse in the household who could provide care. Thus, baby boomers in unprecedented numbers may be turning to their siblings for support in old age. The role of siblings also may become more prevalent with the increased life expectancy of individuals with disabilities (Bittles et al., 2002). Growing numbers of siblings will likely take over caregiving responsibilities when their aging parents are no longer able to continue in this role. Thus, understanding the toll on siblings of assuming the caregiving role will have increasing public health relevance.
Differential Caregiving Effects by Race
According to the stress process model (Pearlin et al., 1990), race is one of the most important structural factors that moderate the effect of caregiving on individual outcomes. Race is closely linked to cultural norms that influence family expectations about caregiving. For example, many ethnic minority families (i.e., African American, Hispanics) have long-standing cultural traditions of providing care to family members, which may affect the degree to which they experience family caregiving as stressful (Dilworth-Anderson et al., 2005). The racial difference in caregiving expectations may be particularly evident with respect to sibling caregiving as minorities are more likely than Whites to have stronger bonds with extended families such as siblings (Goldscheider & Bures, 2003; Miner & Uhlenberg, 1997; White, 2001). Older African American brothers and sisters were more likely to maintain positive relationships with their siblings than older Whites, to have more positive attitudes toward their siblings, and to show greater interest in providing support for them (Gold, 1990). In addition, the lower marriage rate and higher divorce rate among African Americans may make sibling caregiving more pertinent to this population group (Copen, Daniels, Vespa, & Mosher, 2012).
The existing research comparing White caregivers to ethnic minority caregivers suggest that caregiving takes a particular toll on the psychological well-being of White caregivers. Several studies found lower perceived burden and better psychological well-being in African American caregivers than their White counterparts (Dilworth-Anderson, Williams, & Gibson, 2002; Dilworth-Anderson et al., 2005). Pinquart and Sörensen (2005) found that African American caregivers of frail elders had lower levels of caregiver burden and depression than their White counterparts. In studies of parents of adults with developmental disabilities or other chronic conditions, the greater vulnerability of Whites is also evident in the comparison with their African American or Hispanic counterparts (Magaña & Smith, 2006; Valentine, McDermott, & Anderson, 1998). An exception to this pattern was found by Pruchno and her colleagues (1997) who did not find that race had either direct or indirect effects on caregiving outcomes.
In contrast to the effects on psychological well-being, previous studies found that caregiving takes a greater toll on the physical health of racial or ethnic minority caregivers than on Whites. Pinquart and Sörensen (2005) found that minority caregivers reported worse physical health outcomes than White caregivers. This was also the case in a study of Latina mothers of adults with developmental disabilities, where these caregivers had poorer physical health than their White peers (e.g., Magaña, Seltzer & Krauss, 2004). However, as far as we know, no study has examined the differential caregiving effect on siblings by race.
The Present Study
The major aim of this study was to examine the well-being of sibling caregivers relative to other family caregivers (i.e., spouse, adult child, and parental caregivers) and a comparison group of noncaregivers. In addition, we examined whether the caregiver’s race or ethnicity moderates the impact of caregiving. By using data from the National Survey of Midlife Development in the United States (MIDUS), a nationally representative random sample, this study further advances previous research by filling major gaps in caregiving studies, including the need for studies using a national probability sample; the importance of examining both positive and negative consequences of caregiving; and the need to include a broad range of caregivers. Also, this study overcomes an additional methodological limitation in past caregiving studies by comparing sibling caregivers to a comparison group of noncaregivers.
Based on our conceptualization of sibling caregiving as a non-normative role and the differential effects of caregiving by race, we tested the following hypotheses. (i) Sibling caregivers would report lower levels of well-being than respondents in the comparison group without caregiving responsibilities, but they would be less negatively affected by caregiving than other types of family caregivers. (ii) Race or ethnicity would moderate the association between caregiver-care recipient relationship and well-being outcomes. For sibling caregivers who are members of minority groups, the toll of caregiving would be evident in the domain of physical health whereas the toll of caregiving would be most evident in the domain of psychological well-being for White sibling caregivers.
Design and Methods
Study Sample
The study sample was drawn from the MIDUS Study, a nationally representative sample of English-speaking, non-institutionalized adults. The original cohort was aged 25–74 years when the study began in 1995–1996 (MIDUS I). The MIDUS II follow-up was conducted in 2004–2006 when the respondents ranged from age 35 to 86 years. In addition to the 4,963 respondents who participated both in MIDUS I and MIDUS II, as a part of MIDUS II, 592 African Americans aged 35 to 86 from Milwaukee, WI were recruited using area probability sampling methods. Additionally, in 2011, with an emphasis on investigating how the recent economic recession in 2008 affected the lives of American adults, MIDUS expanded its study with an additional 2,660 participants aged 25–64 years. This “Refresher” cohort also consists of a nationally representative random sample (n = 2,152) as well as a random sample of African Americans in Milwaukee (n = 508). For the purpose of this study, the data from MIDUS II and the Refresher cohorts (including the Milwaukee sample) were combined. Data from MIDUS I were not included in the current analysis because questions about the respondent’s caregiving responsibilities were not asked in MIDUS I. Only those aged 35 or older in the Refresher samples were included in this analysis (n = 1,818) to match the age range of participants in the MIDUS II sample. The Refresher and MIDUS II samples differed on several background variables. There was a higher percentage of racial or ethnic minorities in the Refresher cohort relative to the MIDUS II sample (31.4% vs 22.3%). Also, the Refresher cohort was less likely to be currently married (61.9% vs 68.2%) and employed (66.5% vs 83.4%), but had higher levels of education (14.6 years of schooling vs 14.4 years). These differences were controlled in the analysis.
A respondent was identified as a caregiver if he or she reported providing personal care to a sibling, spouse, child, or parent because of a physical or mental condition, illness, or disability during the past 12 months. Those providing short-term care (i.e., for less than 4 weeks) or less than 1 hour of care per week (n = 104, 15.9% of caregivers) during the past year were excluded as the focus of the study was on those providing at least moderate amounts of care over an extended period of time. A comparison group of noncaregivers consisted of respondents who reported that they had not provided any personal care to a family member during the past 12 months. We excluded from the comparison group respondents who provided care to a family member more than 12 months ago (n = 1,447).
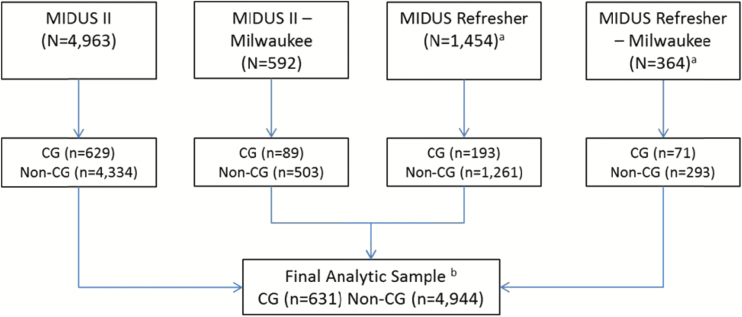
We identified four groups of caregivers. Respondents who provided care to a brother, sister, brother-in-law, and sister-in-law were classified as sibling caregivers. Spouse caregivers had to be currently married to the care recipient. Those providing care to their son, daughter, son-in-law, or daughter-in-law were categorized as parental caregivers. Respondents who provided care to their father, mother, father-in-law, or mother-in-law were classified as adult child caregivers. Based on these selection criteria, our final sample consisted of 631 caregivers (61 sibling caregivers, 99 spouse caregivers, 105 parent caregivers, and 366 adult child caregivers) and 4,944 noncaregivers. Figure 1 summarizes the criteria and procedure to select this analytic sample by MIDUS data source.
Figure 1.
Sample selection criteria and procedure. a The sample is limited to those aged 35 years and older. bExcluded were (i) caregivers of a family member or friend other than a spouse, child, parent, or sibling; (ii) caregivers who provided care less than 4 weeks and/or less than 1 hour per week; (iii) unmarried spouse caregivers; and (iv) noncaregivers during the past 12 months but who had been caregivers in the past more than 12 months ago. CG = caregiver; non-CG = noncaregiver.
Measures
Outcome Variables
We included four outcome variables: depressive symptoms, self-rated physical health, life satisfaction, and perceived control. All respondents were asked if they had experienced a period of at least 2 weeks of either depressed mood or anhedonia. If they responded affirmatively, they were asked if they experienced any one of six additional symptoms (e.g., appetite change, sleep problems, low energy). Depressive symptoms were measured by counting the total number of depressive symptoms experienced by a respondent (ranged from 0 to 7). Respondents were asked to rate their physical health on a 5-point scale with 1 = poor and 5 = excellent. Life satisfaction was measured by a single item asking respondents to rate their life satisfaction on a 4-point scale. Scores were recoded so that a higher score represented a higher level of life satisfaction (1 = not at all satisfied, 4 = very satisfied). Perceived control over one’s life was measured by a single item asking respondents to report how much control they felt over their life in general. The original responses were recoded so that a higher score indicated greater control (1 = no control, 4 = a lot of control). Research has shown that these single-item variables have excellent validity and are strong predictors of respective outcomes measured by multiple, psychometrically established items (Cheung & Lucas, 2014; Cleary, 1997; Menec & Chipperfield, 1997).
Predictors
The primary independent variables were the respondents’ minority status (0 = non-Hispanic White, 1 = member of minority groups) and the caregiver’s kinship relationship to the care recipient. Categorical variables were created for each of the caregiving kinship groups (i.e., sibling caregivers, spouse caregivers, parent caregivers, and adult child caregivers), with noncaregivers serving as the reference group.
Sociodemographic Variables
These included the respondents’ age (in years), gender (1 = female, 0 = male), marital status (1 = married, 0 = unmarried), employment status (1 = employed, 0 = not employed), and education (in years).
Caregiving Context Variables
To describe how the caregiving context of sibling caregivers varied from that of other caregiver groups, we included several additional variables: whether the care recipient co-resided with the caregiver (0 = no, 1 = yes), the number of weeks of care provided during the past 12 months, and the average number of hours of care provided per week. Additionally, the reason care was needed was probed in an open-ended question asking the respondent to identify the condition, illness, or disability that caused the individual to need personal care. These open-ended responses were independently coded into one of three categories: (i) a medical condition including dementia, (ii) a developmental disability (DD) or MI, or (iii) other, which included “old age” or “accident or injury” that could not be classified into one of the other two categories. Finally, a caregiver reported whether he/she provided the following four types of care: (i) bathing, dressing, eating, or going to the bathroom; (ii) getting around inside the house or going outside; (iii) shopping, cooking, housework, or laundry; and (iv) managing money, making phone calls, or taking medication. Each of the four types of care was coded “1” if a caregiver provided that type of care and was coded zero otherwise.
Analysis Plans
We investigated differences between the caregivers as a group versus noncaregivers, using analysis of covariance (ANCOVA), controlling for significant sociodemographic variables between the groups. We also used ANCOVA to identify mean level differences in the well-being outcomes across the four groups of caregivers as well as noncaregivers. Significant differences in proportions for the binary variables between the groups were assessed using chi-square tests. Post hoc t tests were conducted when the overall F ratio was significant. Hierarchical linear regression was used to estimate the association between the type of caregiver-care recipient kinship relationship and well-being outcomes (Model 1), with an interaction term added on the second step (Model 2) to examine whether a caregiver’s race modified the association between the caregiver-care recipient relationship and well-being outcomes.
Results
Group Comparisons
As shown in Table 1, caregivers and noncaregivers differed with respect to gender and employment status. Caregivers were more likely to be women and less likely to be employed than noncaregivers. Caregivers also had more depressive symptoms, perceived their health as poorer, and had lower levels of life satisfaction and perceived control over their lives, net of gender and employment status.
Table 1.
Comparison of Caregivers and Noncaregivers
| Caregivers | Noncaregivers | x 2 or F | |
|---|---|---|---|
| (n = 631) | (n = 4,944) | ||
| Sociodemographic characteristics | |||
| Female: n (%) | 408 (64.7) | 2,431 (49.2) | 53.71*** |
| Minority status: n (%) | 167 (26.6) | 1,134 (23.1) | 3.62 |
| Age: M (SD) | 52.72 (10.65) | 51.94 (12.71) | 2.36 |
| Married: n (%) | 420 (66.6) | 3,286 (66.5) | 0.00 |
| Employed: n (%) | 377 (59.5) | 3,361 (69.9) | 13.34*** |
| Education: M (SD) | 14.29 (2.43) | 14.31 (2.67) | 0.03 |
| Well-being | |||
| Depressive symptoms: M (SD) | 1.19 (2.31) | 0.57 (1.66) | 55.06*** |
| Self-rated health: M (SD) | 3.39 (1.07) | 3.54 (1.05) | 4.96* |
| Life satisfaction M (SD) | 3.40 (0.75) | 3.56 (0.66) | 27.26*** |
| Perceived control M (SD) | 3.52 (0.71) | 3.64 (0.63) | 13.25*** |
Notes. Number of missing cases: age (1), race (44), employed (31), education (9), self-rated physical health (1), life satisfaction (5), and perceived control (7).
F tests of well-being measures were conducted after controlling for gender and employment status differences between caregivers and noncaregivers.
*p ≤ .05. **p ≤ .01. ***p ≤ .001.
Table 2 provides descriptive information on how the four groups of caregivers differed from one another and from the comparison group. Post hoc analyses showed that a higher proportion of the sibling caregivers were members of minority groups (47.5%) compared with the other groups of caregivers and noncaregivers. Spouse caregivers were older (60 years) than other caregivers and noncaregivers. All spouses were married; sibling caregivers were less likely to be married (47.5%) than noncaregivers (66.5%) and adult child caregivers (62.8%). Sibling caregivers (49.1%) and spouse caregivers (43.4%) were less likely to be employed than adult child caregivers or noncaregivers. There were no differences in levels of education between the four caregiver groups and the comparison group.
Table 2.
Well-being, Sociodemographic, and Caregiving Characteristics of Sample by Caregiving Group
| (a) | (b) | (c) | (d) | (e) | x 2 or F | ||
|---|---|---|---|---|---|---|---|
| Sibling caregivers | Spouse caregivers | Parent caregivers | Adult child caregivers | Noncaregivers | |||
| (n = 61) | (n = 99) | (n = 105) | (n = 366) | (n = 4,944) | |||
| Sociodemographic characteristics | |||||||
| Female: n (%) | 43 (70.5) | 65 (65.7) | 72 (68.6) | 338 (62.3) | 2,431 (49.2) | 56.05*** | a, b, c, d > e |
| Minority status: n (%) | 29 (47.5) | 21 (21.2) | 28 (26.7) | 89 (24.5) | 1,134 (23.1) | 21.02*** | a > b, c, d, e |
| Age: M (SD) | 52.31 (10.70) | 59.98 (11.94) | 51.62 (12.08) | 51.13 (8.93) | 51.94 (12.07) | 11.72*** | b > a, c, d, e |
| Married: n (%) | 29 (47.5) | 99 (100.0) | 62 (59.0) | 230 (62.8) | 3,286 (66.5) | 64.51*** | a, c, d, e < b |
| a < d, e | |||||||
| Employed: n (%) | 31 (49.1) | 43 (43.4) | 62 (59.0) | 241 (65.7) | 3,316 (66.9) | 33.93*** | a, b < d, e; b < c |
| Education: M (SD) | 14.16 (2.75) | 14.12 (2.34) | 14.40 (2.60) | 14.33 (2.35) | 14.31 (2.67) | 0.22 | |
| Well-being | |||||||
| Depressive symptoms: M (SD) | 1.72 (2.78) | 0.97 (2.04) | 1.30 (2.34) | 1.13 (2.28) | 0.57 (1.66) | 5.08*** | a, b, c, d > e |
| Self-rated health: M (SD) | 3.16 (1.08) | 3.44 (1.12) | 3.12 (1.14) | 3.49 (1.01) | 3.53 (1.05) | 14.07*** | c < b, d, e |
| Life satisfaction: M (SD) | 3.31 (0.83) | 3.38 (0.67) | 3.14 (0.92) | 3.50 (0.68) | 3.56 (0.66) | 8.34*** | b, c < d, e; c < a |
| Perceived control: M (SD) | 3.44 (0.74) | 3.47 (0.73) | 3.43 (0.77) | 3.58 (0.67) | 3.64 (0.63) | 3.50*** | b, c < d, e |
| Caregiving context | |||||||
| Reason for care: n (%) | 206.72*** | c < a, b, d; a < b, d | |||||
| Medical condition | 41 (67.2) | 92 (92.9) | 34 (33.7) | 287 (80.4) | |||
| DD or MI | 15 (24.6) | 2 (2.0) | 53 (52.5) | 6 (1.7) | |||
| Other | 5 (8.2) | 5 (5.1) | 14 (13.9) | 64 (17.9) | |||
| Weeks of care past year: M (SD) | 21.11 (18.56) | 29.55 (21.40) | 35.47 (19.66) | 29.10 (19.15) | 7.05*** | ||
| Weekly caregiving hours: M (SD) | 19.66 (28.46) | 30.58 (30.16) | 31.03 (30.16) | 23.41 (25.94) | 4.13** | ||
| Help bath/dress/eat: n (%) | 26 (42.6) | 65 (65.7) | 59 (56.2) | 225 (61.5) | 9.83* | b, d > a | |
| Help getting around: n (%) | 30 (50.0) | 70 (70.7) | 39 (37.1) | 271 (74.0) | 56.38*** | b, d > a, c; a > c | |
| Help shopping/housework: n (%) | 51 (83.6) | 86 (86.9) | 87 (82.9) | 318 (86.9) | 1.44 | ||
| Help money/phone/med: n (%) | 36 (60.0) | 76 (76.8) | 91 (86.8) | 286 (78.1) | 15.02** | b, c, d > a | |
| Coresidence: n (%) | 14 (23.0) | 97 (98.0) | 80 (76.2) | 143 (39.1) | 153.67*** | b, c > a, d; b > c; d > a | |
Notes. Number of missing cases: age (1), race (44), employed (31), education (9), self-rated physical health (1), life satisfaction (5), perceived control (7), reason for care (13), help getting around (1), and help money/phone/med (1).
F tests of well-being measures were conducted after controlling for sociodemographic differences across the four caregiver groups as well as the group of noncaregivers.
Post hoc test results are noted when there is a significant difference (p ≤ .05) from (a) sibling caregivers; (b) spouse caregivers; (c) parent caregivers; (d) adult child caregivers; and (e) noncaregivers.
DD = developmental disability; MI = mental illness.
*p ≤ .05. **p ≤ .01. ***p ≤ .001.
As shown in Table 2, the five groups differed significantly with respect to levels of depressive symptoms, self-rated physical health, life satisfaction, and perceived control. All four groups of caregivers had more depressive symptoms than noncaregivers. Spouse and parent caregivers reported lower levels of life satisfaction and perceived control than the comparison group and adult child caregivers. Parent caregivers reported poorer self-rated health than spouse and adult child caregivers as well as noncaregivers.
We observed the expected differences in the reasons the care recipient needed care. Post hoc analysis revealed that sibling caregivers were significantly more likely than spouse or adult child caregivers to be caring for a family member with a DD or MI. Also, parent caregivers were significantly less likely to be caring for a family member with a medical condition than sibling, spouse, and adult child caregivers. There was an overall difference among the four groups of caregivers in both the length and intensity of caregiving provided. Although the post hoc comparisons were not statistically significant, sibling caregivers provided fewer hours of care per week than the other caregiving groups, showing a trend-level difference (p < .10). Sibling caregivers were less likely than spouse or adult child caregivers to provide assistance with bathing, dressing, eating; getting around; managing money, making phone calls, or taking medications. Spouse, parent, and adult child caregivers provided similar levels of help with activities of daily living except in the area of helping the care recipient get around in which parent caregivers reported providing less help than spouse and adult child caregivers. There were no differences among the four caregiver groups in the percent helping with shopping or housework. Almost all of the spouse caregivers co-resided with their husband or wife (98%) whereas sibling caregivers were least likely to co-reside with their brother or sister to whom they provide care (23%).
Effects of the Kinship Relationship on Caregivers’ Well-being: Moderating Effect of Race/Ethnicity
Table 3 shows the results of the hierarchical linear regression analyses examining the effects of caregiving on caregivers’ well-being by the kinship relationship between caregivers and care recipients (Model 1), and the differences in the effects by caregivers’ minority status (Model 2). In Model 1, controlling for sociodemographic characteristics, sibling caregivers reported greater depressive symptoms than noncaregivers but did not differ in their health, life satisfaction, or perceived control. Spouse caregivers reported significantly more depressive symptoms as well as lower levels of life satisfaction and perceived control than noncaregivers, and adult child caregivers reported higher levels of depression than noncaregivers. Parent caregivers had the greatest level of vulnerability, with significantly higher levels of depression, poorer self-rated health, less life satisfaction, and lower levels of perceived control than noncaregivers. Thus, our first hypothesis was supported with sibling caregivers reporting higher levels of depression than noncaregivers, but sibling caregivers were less affected than spouse and parent caregivers.
Table 3.
Multivariate Effects of Caregiving Relationship on Caregivers’ Well-being
| Depressive symptoms | Self-rated health | Life satisfaction | Perceived control | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Sociodemographics | ||||||||
| Femalea | .27*** | .27*** | .06* | .06* | .02 | .02 | −.02 | .02 |
| Minorityb | −.17** | −.14* | −.26*** | −.25*** | .01 | .01 | .01 | −.01 |
| Age | −.02*** | −.02*** | −.01*** | −.01*** | .01*** | .01*** | .01*** | .01*** |
| Marriedc | −.25*** | −.25*** | −.18*** | .19*** | .31*** | .31*** | .05** | .05** |
| Employedd | −.46*** | −.46*** | .40*** | .40*** | .14*** | .14*** | .13*** | .13*** |
| Education | −.03*** | −.03*** | .08*** | .08*** | .01* | .01* | −.00 | −.00 |
| Caregiver groupse | ||||||||
| Sibling caregivers | .86*** | 1.27*** | −.14 | −.10 | −.15† | −.35** | −.12 | −.15 |
| Spouse caregivers | .50** | .57** | −.02 | .12 | −.33*** | −.30*** | −.22*** | −.23*** |
| Parent caregivers | .65*** | .73*** | −.37*** | −.37*** | −.39*** | −.38*** | −.19** | −.19** |
| Adult child caregivers | .49*** | .50*** | −.04 | −.02 | −.06 | −.05 | −.05 | −.09* |
| Caregiver group × Race | ||||||||
| Sibling × Minority | −.88* | −.09 | .44** | .08 | ||||
| Spouse × Minority | −.36 | −.64** | −.12 | .07 | ||||
| Parent × Minority | −.30 | .02 | −.03 | .02 | ||||
| Adult child × Minority | −.06 | −.05 | −.01 | .18* | ||||
| Constant | 1.67 | 1.67 | 2.94 | 2.94 | 3.13 | 3.13 | 3.27 | 3.28 |
| N | 5,492 | 5,492 | 5,491 | 5,491 | 5,489 | 5,489 | 5,487 | 5,487 |
| Adjusted r2 | .0475 | .0477 | .1398 | .1403 | .0793 | .0799 | .0263 | .0265 |
Notes. Reference group is amale, bnon-Hispanic White, cunmarried, dunemployed, and enoncaregivers.
† p < .10. *p ≤ .05. **p ≤ .01. ***p ≤ .001.
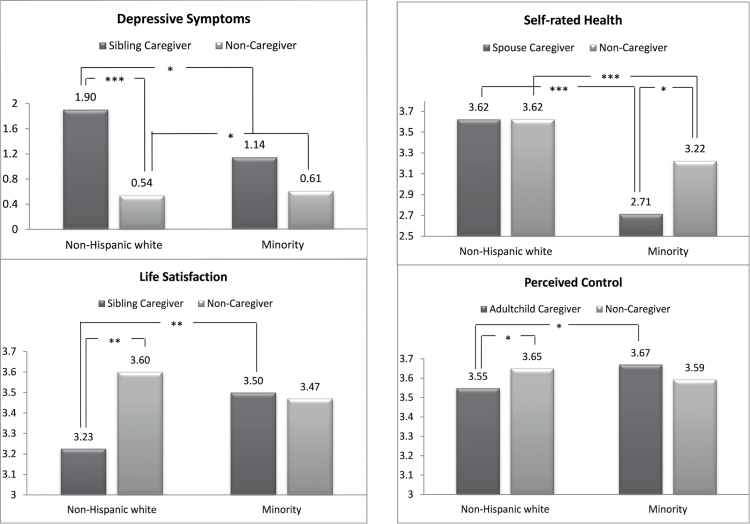
Model 2 shows the interaction effect of minority status in predicting the effects of caregiving for siblings, spouses, children, or parents. As shown in the upper left panel of Figure 2, White sibling caregivers experienced greater depressive symptoms (predicted mean = 1.90) than White noncaregivers (predicted mean = 0.54, F = 17.21, p < .001), whereas for those from minority groups, levels of depression were not significantly different between sibling caregivers and noncaregivers. Also, White sibling caregivers had higher levels of depression than sibling caregivers from minority groups (predicted mean = 1.14, F = 5.36, p < .05). However, among the noncaregivers, those from minority groups (predicted mean = 0.61) had higher levels of depression than White noncaregivers (F = 5.50, p < .05).
Figure 2.
The moderating effect of race on well-being. *p ≤ .05. **p ≤ .01. ***p ≤ .001.
A similar pattern for sibling caregivers was found for life satisfaction. White sibling caregivers reported significantly lower levels of life satisfaction (predicted mean = 3.23) than White noncaregivers (predicted mean = 3.60, F = 9.43, p < .01). Also, White sibling caregivers had lower levels of satisfaction than sibling caregivers from minority groups (predicted mean = 3.50, F = 7.16, p < .01). However, among sample members from minority groups, there was no difference between sibling caregivers and sibling noncaregivers.
Minority status also moderated the effect of caregiving on a sense of perceived control for adult children. White adult child caregivers reported lower levels of perceived control (predicted mean = 3.55) than White noncaregivers (predicted mean = 3.65, F = 5.37, p < .05). Overall, caregivers from minority groups (predicted mean = 3.67) reported higher levels of perceived control than White caregivers (F = 4.82, p < .05). However, there was no difference in perceived control among caregivers and noncaregivers from minority groups.
There was some evidence that among individuals from minority groups, the toll of caregiving was seen in the domain of physical health, but only for spouse caregivers. The physical health of caregiving spouses who were from minority groups was most affected by caregiving (see the upper right panel of Figure 2). Among those from minority groups, spouse caregivers (predicted mean = 2.71) had significantly poorer physical health than noncaregivers (predicted mean = 3.22, F = 5.95, p < .05). There were no significant differences in health between White spouse caregivers (predicted mean = 3.62) and White noncaregivers (predicted mean = 3.62).
Discussion
Given the complex dynamics of family caregiving, it is important to understand how caregivers’ kinship relationship to care recipients, caregiver race, and those interactions are associated with caregiver well-being. In this study, we shed new light on this question by expanding the range of kinship relationships to include siblings, a group which has rarely been studied in prior research, and by exploring whether race moderates the effect of kinship relationship on well-being.
Consistent with prior research, caregivers in general, including sibling caregivers, reported worse physical and psychological well-being than noncaregivers, net of their socioeconomic characteristics. Among sibling caregivers, caregiving took a significantly greater toll on non-Hispanic White caregivers than those from minority groups. There are several possible explanations for why we found that White sibling caregivers reported higher levels of depressive symptoms and lower levels of life satisfaction than minority sibling caregivers. First, these findings are consistent with the work of Dilworth-Anderson and colleagues (2005), who proposed that differences between ethnic groups in the strength of the cultural norm surrounding family care help explain the racial or ethnic differences found in the caregiving literature. The closer relationship between siblings in minority communities may explain, in part, the better well-being of the minority sibling caregivers relative to their White counterparts (Miner & Uhlenberg, 1997; White, 2001). Second, White caregivers of siblings were more likely to be married than sibling caregivers from minority groups (66% vs 28% respectively, p < .01). Consequently, it is possible that White sibling caregivers were more likely to be simultaneously providing care to another family member, be a spouse or parent-in-law. Third, as the care networks of African Americans are more expansive than Whites (Dilworth-Anderson et al., 2005), minority sibling caregivers may receive more informal assistance with caregiving than White sibling caregivers. The MIDUS survey did not include questions about cultural norms, multiple caregiving roles or secondary caregivers, which would have allowed us to explore these possible explanations.
We did not find that race moderated the effects of caregiving on psychological well-being for either spouse or parental caregivers, consistent with prior research (Jessup, Bakas, McLennon, & Weaver, 2015; Kang, 2006). As in our research, these studies did not find that African American and non-African American spouse caregivers differed in levels of depressive symptoms or emotional strains. One possible explanation of these findings is that there is a stronger societal expectation that parents and spouses, regardless of an individual’s race or ethnicity, will provide care than is the case for siblings and adult children.
The greater toll of caregiving on physical health was evident only for minority spouse caregivers. This is consistent with a study of older couples which found African American caregivers were in poorer physical health than White caregivers (Wallsten, 2000). Sörensen and Pinquart (2005) also found that African American and Hispanic spouses caring for Alzheimer’s patients, but not White spouses, had worse perceived physical health than other caregivers. Spouse caregivers are often older and therefore frailer, and have fewer alternative roles to give them a social outlet (Pinquart & Sörensen, 2011). This effect may be even more pronounced among older minorities because of their higher morbidity related to health inequalities and lifestyle factors (Boslaugh, 2008). Minority spouse caregivers may also experience greater physical consequences as a result of their limited economic resources that both prevent them from utilizing paid services to assist them with caregiving as well as limit their ability to seek preventative medical care for their own health needs (Pinquart & Sörensen, 2005).
Our finding that parents caring for children with disabilities are a particularly vulnerable group is consistent with a growing body of research on the challenges faced by midlife and older parents caring for children with a DD and MI. Studies showed that parents of adults with the chronic conditions have poorer physical and mental health and lower levels of functional abilities than similarly aged parents of healthy adult children (Aschbrenner, Greenberg, & Seltzer, 2009; Seltzer, Floyd, Song, Greenberg, & Hong, 2011). Due to behavioral problems of the affected children and the associated social stigma and isolation, parents of children with a DD or MI experience lifelong caregiving stress, and the stress is known to have cumulative effects on health (Seltzer et al., 2011).
Our study findings have important implications for gerontological practice. First, there has been little recognition in the practice literature of sibling caregivers and their unique challenges. There is a need to increase the awareness among practitioners of the growing numbers of sibling caregivers and to develop outreach services to meet their needs for information and support. In-service agency training could emphasize the role of sibling caregivers and how their caregiving experience may differ from that of other family caregivers. In addition, support groups and psychoeducation programs, which have been developed for adult children and spouses, could be adapted to meet the unique challenges faced by sibling caregivers. Second, and most importantly, relevant federal and state laws often fail to include siblings in the definition of “family.” It was only recently that the Department of Labor added “siblings” in its dissemination of materials that identify those family members eligible under the Family Medical Leave Act (U.S. Department of Labor, 2015). Gerontological practitioners have a role to play in advocating that written state and federal statutes affecting services to caregivers include “siblings” in the definition of family caregivers eligible for services and supports.
The present study has limitations that should be considered when interpreting the results. First, certain subgroups including spouse, parent, and sibling minority caregivers had small cell sizes (n = less than 30), and thus data may have the insufficient power to detect certain effects. Second, we did not have an adequate number of minority caregivers to examine variations in the effects of caregiving among specific racial or ethnic groups. Lastly, there was considerable heterogeneity in the reasons care was needed, and therefore, we were not able to examine within-group variation in the effects of specific diagnostic categories on caregiver well-being.
Juxtaposed with these limitation are the study strengths that include data drawn from a nationally representative sample, the inclusion of a comparison group of noncaregivers, and the ability to capture a wide range of caregivers with respect to life course stage, kinship relationship, and race. With the aging of the population and shifts in the ethnic composition of the United States, future generations of caregivers will be characterized by greater diversity not only along the dimension of race or ethnicity but also in terms of their kinship relationship to the care recipient. Sibling caregivers will be among the most rapidly growing groups of family caregivers.
Funding
This work was supported by the National Institute on Aging (grant P01-AG020166) to conduct a longitudinal follow-up of the MIDUS investigation. The original study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. Support for this research was provided by the Office of the Vice Chancellor for Research and Graduate Education at the University of Wisconsin–Madison with funding from the Wisconsin Alumni Research Foundation. Support was also provided by a grant (P30 HD03352) to the Waisman Center at the University of Wisconsin–Madison.
References
- Aschbrenner K. A., Greenberg J. S., Seltzer M. M. (2009). Parenting an adult child with bipolar disorder in later life. The Journal of Nervous and Mental Disease, 197, 298–304. doi:10.1097/NMD.0b013e3181a206cc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell S., Lee C. (2008). Transitions in emerging adulthood and stress among young Australian women. International Journal of Behavioral Medicine, 15, 280–288. doi:10.1080/10705500802365482 [DOI] [PubMed] [Google Scholar]
- Bittles A. H. Petterson B. A. Sullivan S. G. Hussain R. Glasson E. J., & Montgomery P. D (2002). The influence of intellectual disability on life expectancy. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 57, M470–M472. doi:10.1093/gerona/57.7.M470 [DOI] [PubMed] [Google Scholar]
- Boslaugh S. (2008). African American health issues. In Boslaugh S.(Ed.), Encyclopedia of epidemiology (pp. 5–11). Thousand Oaks, CA: Sage. [Google Scholar]
- Chappell N. L. Dujela C., & Smith A (2014). Spouse and adult child differences in caregiving burden. Canadian Journal on Aging, 33, 462–472. doi:10.1017/S0714980814000336 [DOI] [PubMed] [Google Scholar]
- Chen W.-Y., & Lukens E (2011). Well-being, depressive symptoms, and burden among parent and sibling caregivers of persons with severe and persistent mental illness. Social Work in Mental Health, 9, 397–416. doi:10.1080/15332985.2011.575712 [Google Scholar]
- Cheung F., & Lucas R. E (2014). Assessing the validity of single-item life satisfaction measures: Results from three large samples. Quality of Life Research, 23, 2809–2818. doi:10.1007/s11136-014-0726-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chumbler N. R., Grimm J. W., Cody M., Beck C. (2003). Gender, kinship and caregiver burden: The case of community-dwelling memory impaired seniors. International Journal of Geriatric Psychiatry, 18, 722–732. doi:10.1002/gps.912 [DOI] [PubMed] [Google Scholar]
- Cleary P. D. (1997). Subjective and objective measures of health: Which is better when? Journal of Health Services Research & Policy, 2, 3–4. [DOI] [PubMed] [Google Scholar]
- Copen C. E. Daniels K. Vespa J., & Mosher W. D (2012). First marriages in the United States: Data from the 2006–2010 National Survey of Family Growth. National health statistics reports (Report no. 49). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Dilworth-Anderson P. Brummett B. H. Goodwin P. Williams S. W. Williams R. B., & Siegler I. C (2005). Effect of race on cultural justifications for caregiving. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60B, S257–S262. doi:10.1093/geronb/60.5.S257 [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P. Williams I. C., & Gibson B. E (2002). Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000). The Gerontologist, 42, 237–272. doi:10.1093/geront/42.2.237 [DOI] [PubMed] [Google Scholar]
- Gold D.T. (1990). Late-life sibling relationships: Does race affect typological distribution? The Gerontologist, 30, 741–748. doi:10.1093/geront/30.6.741 [DOI] [PubMed] [Google Scholar]
- Goldscheider F. K., & Bures R. M (2003). The racial crossover in family complexity in the United States. Demography, 40, 569–587. doi:10.1353/dem.2003.0022 [DOI] [PubMed] [Google Scholar]
- Hatfield A. B., & Lefley H. P (2005). Future involvement of siblings in the lives of persons with mental illness. Community Mental Health Journal, 41, 327–338. doi:10.1007/s10597-005-5005-y [DOI] [PubMed] [Google Scholar]
- Hsiao C. Y., Tsai Y. F. (2015). Factors of caregiver burden and family functioning among Taiwanese family caregivers living with schizophrenia. Journal of Clinical Nursing, 24, 1546–1556. doi:10.1111/jocn.12745 [DOI] [PubMed] [Google Scholar]
- Jessup N. M., Bakas T., McLennon S. M., Weaver M. T. (2015). Are there gender, racial or relationship differences in caregiver task difficulty, depressive symptoms and life changes among stroke family caregivers? Brain Injury, 29, 17–24. doi:10.3109/02699052.2014.947631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S. Y. (2006). Predictors of emotional strain among spouse and adult child caregivers. Journal of Gerontological Social Work, 47, 107–131. doi:10.1300/J083v47n01_08 [DOI] [PubMed] [Google Scholar]
- Kreider R. M. (2005, February). Number, timing, and duration of marriages and divorces: 2001, current population reports (Report No. P70-97). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Litwin H., Stoeckel K. J., Roll A. (2014). Relationship status and depressive symptoms among older co-resident caregivers. Aging & Mental Health, 18, 225–231. doi:10.1080/13607863.2013.837148 [DOI] [PubMed] [Google Scholar]
- Lohrer S. P., Lukens E. P., Thorning H. (2007). Economic expenditures associated with instrumental caregiving roles of adult siblings of persons with severe mental illness. Community Mental Health Journal, 43, 129–151. doi:10.1007/s10597-005-9026-3 [DOI] [PubMed] [Google Scholar]
- Magaña S., Seltzer M. M., Krauss M. W. (2004). Cultural context of caregiving: Differences in depression between Puerto Rican and non-Latina White mothers of adults with mental retardation. Mental Retardation, 42, 1–11. doi:10.1352/0047-6765(2004)42<1:CCOCDI>2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Magaña S., Smith M. J. (2006). Health outcomes of midlife and older Latina and black American mothers of children with developmental disabilities. Mental Retardation, 44, 224–234. doi:10.1352/0047-6765(2006)44[224:HOOMAO]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Marks N. F. Lambert J. D., & Choi H (2002). Transitions to caregiving, gender, and psychological well-being: A prospective U.S. national study. Journal of Marriage and Family, 64, 657–667. doi:10.1111/j.1741-3737.2002.00657.x [Google Scholar]
- McPherson K. M. Pentland B., & McNaughton H. K (2000). Brain injury—The perceived health of carers. Disability & Rehabilitation, 22, 683–689. doi:10.1080/096382800445489 [DOI] [PubMed] [Google Scholar]
- Menec V. H., & Chipperfield J. G (1997). The interactive effect of perceived control and functional status on health and mortality among young-old and old-old adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 52, P118–P126. doi:10.1093/geronb/52B.3.P118 [DOI] [PubMed] [Google Scholar]
- Miner S., & Uhlenberg P (1997). Intragenerational proximity and the social role of sibling neighbors after midlife. Family Relations, 46, 145–153. doi:10.2307/585038 [Google Scholar]
- Pearlin L. L. Mullan J. T. Semple S. J., & Skaff M. T (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30, 583–594. doi:10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Penning M. J., & Wu Z (2015). Caregiver stress and mental health: Impact of caregiving relationship and gender. The Gerontologist, doi:10.1093/geront/gnv038 [DOI] [PubMed] [Google Scholar]
- Pinquart M., & Sörensen S (2005). Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist, 45, 90–106. doi:10.1093/geront/45.1.90 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2011). Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging, 26, 1–14. doi:10.1037/a0021863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruchno R. A. Patrick J. P., & Burant C. J (1997). African American and White mothers of adults with chronic disabilities: Caregiving burden and satisfaction. Family Relations, 46, 335–346. doi:10.2307/585094 [Google Scholar]
- Reinhard S. C., & Horwitz A. V (1995). Caregiver burden: Differentiating the content and consequences of family caregiving. Journal of Marriage & Family, 57, 741–750. doi:10.2307/353928 [Google Scholar]
- Shahly V. Chatterji S. Gruber M. J. Al-Hamzawi A. Alonso J. Andrade L. H. … Kessler R. C (2013). Cross-national differences in the prevalence and correlates of burden among older family caregivers in the World Health Organization World Mental Health (WMH) Surveys. Psychological Medicine, 43, 865–879. doi:10.1017/S0033291712001468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer M. M., Floyd F., Song J., Greenberg J., Hong J. (2011). Midlife and aging parents of adults with intellectual and developmental disabilities: Impacts of lifelong parenting. American Journal on Intellectual and Developmental Disabilities, 116, 479–499. doi:10.1352/1944-7558-116.6.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sörensen S., Pinquart M. (2005). Racial and ethnic differences in the relationship of caregiving stressors, resources, and sociodemographic variables to caregiver depression and perceived physical health. Aging & Mental Health, 9, 482–495. doi:10.1080/13607860500142796 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor Wage and Hour Division (2015, July). Fact sheet #28B: FMLA leave for birth, placement, bonding, or to care for a child with a serious health condition on the basis of an “in loco parentis” relationship. Retrieved January 25, 2016, from http://www.dol.gov/whd/regs/compliance/whdfs28B.pdf
- Valentine D. P. McDermott S., & Anderson D (1998). Mothers of adults with mental retardation: Is race a factor in perceptions of burdens and gratifications? Families in Society, 79, 577–584. doi:10.1606/1044–3894.861 [Google Scholar]
- Viana M. C. Gruber M. J. Shahly V. Alhamzawi A. Alonso J. Andrade L. H., … Kessler R. C (2013). Family burden related to mental and physical disorders in the world: Results from the WHO World Mental Health (WMH) surveys. Revista Brasileira de Psiquiatria, 35, 115–125. doi:10.1590/1516-4446-2012-0919 [DOI] [PubMed] [Google Scholar]
- Wallsten S. S. (2000). Effects of caregiving, gender, and race on the health, mutuality, and social supports of older couples. Journal of Aging & Health, 12, 90–111. doi:10.1177/089826430001200105 [DOI] [PubMed] [Google Scholar]
- White L. (2001). Sibling relationships over the life course: A panel analysis. Journal of Marriage and Family, 63, 555–568. doi:10.1111/j.1741-3737.2001.00555.x [Google Scholar]
- Zehner Ourada V. E., & Walker A. J (2014). A comparison of physical health outcomes for caregiving parents and caregiving adult children. Family Relations, 63, 163–177. doi:10.1111/fare.12046 [Google Scholar]