Abstract
Purpose of the Study:
Older homeless adults living in shelters have high rates of geriatric conditions, which may increase their risk for acute care use and nursing home placement. However, a minority of homeless adults stay in shelters and the prevalence of geriatric conditions among homeless adults living in other environments is unknown. We determined the prevalence of common geriatric conditions in a cohort of older homeless adults, and whether the prevalence of these conditions differs across living environments.
Design and Methods:
We interviewed 350 homeless adults, aged 50 and older, recruited via population-based sampling in Oakland, CA. We evaluated participants for common geriatric conditions. We assessed living environment using a 6-month follow-back residential calendar, and used cluster analysis to identify participants’ primary living environment over the prior 6 months.
Results:
Participants stayed in 4 primary environments: unsheltered locations (n = 162), multiple locations including shelters and hotels (n = 88), intermittently with family/friends (n = 57), and, in a recently homeless group, rental housing (n = 43). Overall, 38.9% of participants reported difficulty performing 1 or more activities of daily living, 33.7% reported any falls in the past 6 months, 25.8% had cognitive impairment, 45.1% had vision impairment, and 48.0% screened positive for urinary incontinence. The prevalence of geriatric conditions did not differ significantly across living environments.
Implications:
Geriatric conditions were common among older homeless adults living in diverse environments, and the prevalence of these conditions was higher than that seen in housed adults 20 years older. Services that address geriatric conditions are needed for older homeless adults living across varied environments.
Keywords: Homeless persons, Functional status, Sensory impairment, Cognitive impairment, Epidemiology
Introduction
The median age of the U.S. homeless population is increasing (Hahn, Kushel, Bangsberg, Riley, & Moss, 2006). Currently, half of single homeless adults are aged 50 and older (Culhane, Metraux, Byrne, Stino, & Bainbridge, 2013), compared to 11% in 1990 (Hahn et al., 2006). Homeless people are thought to experience “accelerated aging” relative to the general population (Cohen, 1999; Gelberg, Linn, & Mayer-Oakes, 1990). Homeless adults have disproportionately high rates of chronic illnesses and poor health status (Garibaldi, Conde-Martel, & O’Toole, 2005; Gelberg, Linn, & Mayer-Oakes, 1990; Kimbler, DeWees, & Harris, 2015), premature age-adjusted mortality rates (Baggett et al., 2013; Hwang, Orav, O’Connell, Lebow, & Brennan, 1997), and high rates of geriatric conditions in individuals in their 50s and early 60s (Brown, Kiely, Bharel, & Mitchell, 2012).
Geriatric conditions, such as functional impairment, falls, and urinary incontinence, typically first occur in housed adults aged 75 and older (Inouye, Studenski, Tinetti, & Kuchel, 2007) and are strongly associated with adverse health outcomes including acute care use, institutionalization, and death (Inouye et al., 1998; Inouye, Studenski, Tinetti, & Kuchel, 2007; Tschanz et al., 2004). Environmental factors play a central role in older adults’ ability to adapt to these conditions. Older adults who live in stable housing may be able to modify their environment to adapt to geriatric impairments (Szanton et al., 2011; Wahl, Fange, Oswald, Gitlin, & Iwarsson, 2009). In contrast, older homeless adults may have great difficulty changing their environment, leading to a mismatch between their abilities and environment. As suggested by Lawton and Nahemow’s environmental press model, this mismatch may make it more difficult to function independently, and may be most severe in older homeless adults living in more demanding environments, such as individuals staying in unsheltered places or moving frequently between different locations (Kushel, 2012; Lawton & Nahemow, 1973).
In previous work, we found that geriatric conditions were common among older homeless adults recruited from homeless shelters (Brown et al., 2012). However, this study did not sample unsheltered individuals or those living temporarily with family or friends. These individuals make up the majority of homeless people nationally (Opening Doors: Federal Strategic Plan to Prevent and End Homelessness Update 2013, 2014) and may be at high risk for poor outcomes associated with geriatric conditions (Bamberger & Dobbins, 2014; Nyamathi, Leake, & Gelberg, 2000). Understanding how the prevalence of geriatric conditions varies among homeless persons living in differing environments is critical for targeting limited resources and planning appropriate services and programs for older homeless adults. Therefore, we examined the prevalence of common geriatric conditions in a population-based sample of older homeless adults, and determined whether the prevalence of geriatric conditions differed by living environment. We hypothesized that the prevalence of geriatric conditions would be higher among homeless individuals living in more demanding environments, such as unsheltered places, as these individuals may experience a larger mismatch between their abilities and environment.
Design and Methods
Design Overview
We interviewed homeless adults, aged 50 and older, recruited via population-based sampling in Oakland, CA. These interviews were part of a cohort study, Health Outcomes in People Experiencing Homelessness in Older Middle agE (HOPE HOME). We developed the study methods in consultation with a community advisory board. The institutional review board of the University of California, San Francisco, approved the study.
Sample and Recruitment
Similar to our prior research with homeless adults living in San Francisco (Weiser et al., 2013), we sampled homeless individuals from low cost meal programs and shelters. We extended the sampling frame to include recycling centers and places where unsheltered people stayed. Sampling sites included all overnight homeless shelters in Oakland that served single adults over age 25 (n = 5), all low-cost meal programs that served homeless individuals at least 3 meals per week (n = 5), a recycling center, and places where unsheltered homeless adults stayed. For the latter, we randomly selected days to accompany an outreach team that served unsheltered homeless people. We set total sampling goals for each sampling frame based on best estimates of the number of unique individuals who visited that site, or were unsheltered, annually. The study team randomly selected individuals at each site to meet these sampling goals. Individuals who met a brief eligibility screen were invited to participate in an enrollment interview.
The study team conducted enrollment and baseline interviews from July 2013 to June 2014 at St. Mary’s Center, a non-profit community-based center in Oakland that serves low-income older adults. Individuals were eligible to participate if they were aged 50 or older, able to communicate in English, and currently homeless as defined in the federal Homeless Emergency Assistance and Rapid Transitions to Housing (HEARTH) Act (Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009). Individuals who were unable to communicate due to severe hearing impairment were excluded.
After determining eligibility, study staff used a teach-back method to obtain informed consent (Dunn & Jeste, 2001) and excluded individuals unable to provide consent. Study staff conducted in-depth structured baseline interviews with eligible participants. Individuals received a $25 gift card for completing the eligibility and baseline interviews.
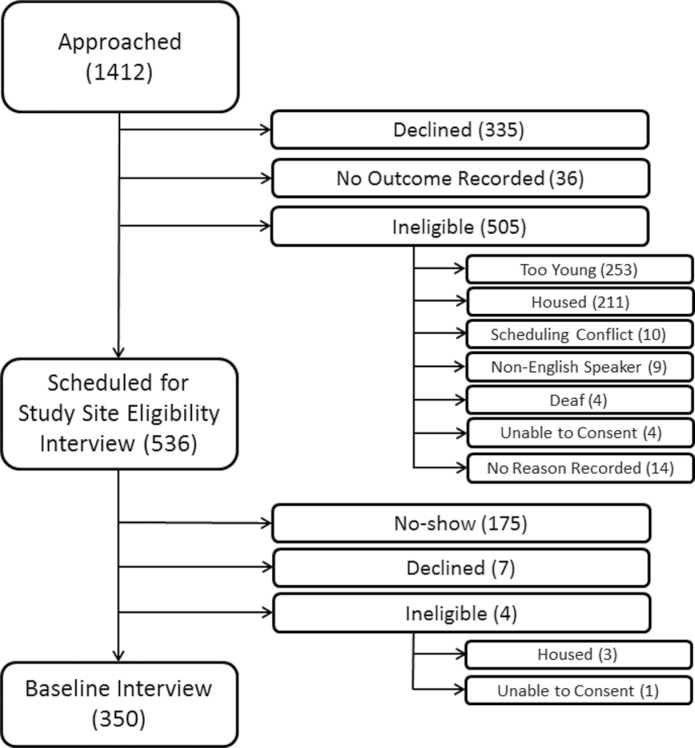
Of 1,412 people approached for eligibility screening, 536 met preliminary eligibility criteria and were scheduled for an enrollment interview (Figure 1). Another 505 were ineligible, and 335 declined to participate before we assessed eligibility. Of 536 people scheduled for an enrollment interview, 350 attended and were enrolled, 4 were ineligible, 7 declined, and 175 did not attend. People who declined to participate or did not attend the interview were similar to enrolled participants by sex, but were more likely to be African-American by observed race/ethnicity (82.3 vs. 79.7%, p =.04) and more likely to be recruited from meal programs (55.3 vs. 49.1%) and from unsheltered areas or recycling centers (20.1 vs. 15.7%, overall p = .003).
Figure 1.
Flow-chart of recruitment of 350 older homeless adults. This figure shows the number of individuals approached, assessed for eligibility, and enrolled in the study, noting specific reasons for inability to enroll. Values represent the number of individuals in each group. Participants who declined after being approached (335) declined before being assessed for eligibility. Therefore, the number of participants who were ineligible for the study may have been higher than the numbers presented in this table.
Measures
Geriatric Conditions
Participants reported if they had difficulty performing 5 activities of daily living (ADLs; bathing, dressing, eating, transferring, toileting) (Katz, 1983), and six instrumental activities of daily living (IADLs; taking transportation, managing medications, managing money, applying for benefits, setting up a job interview, finding a lawyer) (Sullivan, Dumenci, Burnam, & Koegel, 2001). We assessed IADLs using the Brief Instrumental Functioning Scale, a validated instrument developed for use in homeless persons (Sullivan, Dumenci, Burnam, & Koegel, 2001). We defined ADL impairment as difficulty performing 1 or more ADLs; we defined IADL impairment similarly.
We defined mobility impairment as self-reported difficulty walking across a room (Katz, 1983). Participants reported how many times they had fallen over the past 6 months and whether they had required medical treatment (Health and Retirement Survey (HRS), 2012).
We assessed cognition using the Modified Mini-Mental State Examination (Bland & Newman, 2001). A licensed neuropsychologist trained research staff to administer this instrument and observed random interviews to ensure adherence to the protocol. We defined cognitive impairment as a score below the 7th percentile (i.e., 1.5 standard deviations below a reference cohort mean) or inability to complete the assessment (Bland & Newman, 2001; Bravo & Hebert, 1997).
We defined visual impairment as a corrected visual acuity worse than 20/40 on a Snellen chart (“Screening for impaired visual acuity in older adults: U.S. Preventive Services Task Force recommendation statement,” 2009). We defined hearing impairment as self-reported difficulty hearing (Moyer, 2012). Participants reported if they used a hearing aid. We assessed urinary incontinence using the three Incontinence Questions adapted for a 6-month period (incontinence defined as reporting having leaked urine during the prior 6 months) (Brown et al., 2006). We assessed depressive symptoms using the Center for Epidemiologic Studies Depression Scale (range 0–60; symptoms of major depression defined as a score >16) (Radloff, 1977).
Living Environment
We assessed living environment using a follow-back residential calendar (Tsemberis, McHugo, Williams, Hanrahan, & Stefancic, 2007). Each participant reported where he or she had stayed over the previous 6 months and the number of days spent in each location, including homeless shelters, unsheltered places, housing belonging to family/friends, transitional housing, hotels or single room occupancy units, rented rooms or apartments, homes they owned, medical facilities, drug treatment facilities, and jail or prison. We identified each participant’s primary living environment using cluster analysis.
Participants also reported where they had stayed each night during the 2 weeks before the interview and the date when they last had stable housing, defined as living in non-institutional housing for at least 12 months.
Participant Characteristics
Sociodemographic Variables
Sociodemographic characteristics included age, gender, race/ethnicity (African-American, white, Latino, multiracial/other), marital/partner status, and highest level of education. Participants reported the age at which they first experienced homelessness as an adult.
Health Status
We assessed self-rated general health (fair or poor versus good, very good, or excellent) (Ware, Kosinski, & Keller, 1996). Participants reported if a health care provider had ever told them that they had hypertension, coronary artery disease or myocardial infarction, congestive heart failure, stroke, diabetes, chronic obstructive pulmonary disease or asthma, arthritis, or HIV/AIDS (National Health and Nutrition Examination Survey (NHANES), 2009).
We assessed history of mental health problems using measures adapted from the National Survey of Homeless Assistance Providers and Clients (Burt et al., 1999) and the Addiction Severity Index (McLellan et al., 1992). Participants reported if they had ever experienced serious anxiety, depression, difficulty controlling violent behavior, hallucinations that were not a result of substance use; had attempted suicide; or had been prescribed medication by a doctor for psychiatric problems. We defined a history of mental health problems as having experienced any of these issues (Burt et al., 1999). Participants reported if they had ever been hospitalized for a psychiatric problem.
Health-Related Behaviors
Participants reported their history of cigarette smoking using questions from the California Tobacco Survey (never smoker, former, current) (Al-Delaimy, Edland, Pierce, Mills, & White, 2011). We defined a history of alcohol use problems as reporting drinking to get drunk three or more times a week, and a history of drug use problems as reporting using drugs three or more times a week (Burt et al., 1999). We assessed alcohol use disorders in the past 6 months using the Alcohol Use Disorders Identification Test adapted for a 6-month period (range, 0–20; alcohol problem defined as a score ≥8) (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). We assessed illicit drug use in the past 6 months using the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test adapted for a 6-month period (range 0–39; drug problem defined as a score ≧4 for use of either cocaine, amphetamines, or opioids) (Humeniuk, Henry-Edwards, Ali, Poznyak, & Monteiro, 2010).
Health Care Access
Participants reported if they had a regular location to obtain health care other than the emergency department (National Health Interview Survey (NHIS, 2012). Adult Access to Health Care and Utilization. 2012).
Statistical Analyses
We described geriatric conditions and participant characteristics using descriptive statistics. To identify the primary environment where each participant stayed, we used cluster analysis, which identifies existing patterns within data to generate similar groups of participants (Everitt, Landau, Leese, & Stahl, 2011; Kohn et al., 2010; Lee et al., 2016). Participants were assigned to a housing group based on the total number of days they reported staying in each location over the previous 6 months. For those with recent homelessness, these locations could include places where they had been housed.
We chose to use cluster analysis rather than other methods of categorizing the data for several reasons. In an effort to best approximate a sample of older adults experiencing homelessness in Oakland, our study sampled homeless individuals from homeless shelters, unsheltered places, meal lines, and recycling centers. Similarly, we used a follow-back residential calendar to capture variability in living environment over a 6-month period, rather than assessing living environment cross-sectionally based on an individual’s location at the time of recruitment. Rather than categorizing this complex data using a priori living environment categories determined based on studies with narrower sampling frames, we used cluster analysis to identify naturally occurring groups within the data that we might not have otherwise predicted.
We used two cluster methods to identify living environment groups. For our primary analysis, we used Ward’s linkage to minimize the sum of squares difference within groups (Ward, 1963). We performed visual analysis of a dendrogram representing the data structure to select an optimal number of clusters, and used bivariable matrices to confirm that we could identify natural groupings. We then verified these cluster classifications using k-medians cluster analysis for a set number of 3–8 clusters (Calinski & Harabasz, 1974; Hair, Black, Babin, & Anderson, 1987). To measure the distinctness of the groups generated by these two cluster methods, we used the pseudo-t2 and pseudo-F stopping rules (Calinski & Harabasz, 1974). To confirm that there were significant distinctions between groups, we performed one-way ANOVA.
To test for differences in geriatric conditions and participant characteristics across housing groups, we used the Kruskal–Wallis test of medians and chi-square tests for categorical variables.
We used multivariable logistic regression models to determine how the association of living environment with each geriatric condition changed after adjusting for key factors including age, sex, alcohol, and drug use problems. Where differences in association were found, we wished to assess whether they were reflective of underlying vulnerabilities in the population or whether they persisted even after adjustment. We used separate models for each condition and treated living environment as an indicator variable in which one group was the referent. We considered sex as a potential effect modifier of the association between environment and each geriatric condition, as men are more likely to live in unsheltered environments than are women (North & Smith, 1993).
As living environment may reflect the length of time an individual has been homeless, we conducted separate unadjusted logistic regression analyses substituting time since last stable housing (modeled as a linear variable) in place of environment. Analyses were conducted using SAS version 9.2 (SAS Institute, Cary, North Carolina) and Stata version 11 (StataCorp).
Results
Participant Characteristics
The median age of the cohort was 58 years (IQR, 54, 61), 77.1% were male, and 79.7% were African American (Table 1). Nearly half (43.6%) experienced their first episode of adult homelessness at age 50 or older. The majority of participants (55.7%) reported poor or fair health status; chronic medical conditions were common. Nearly three-quarters (71.3%) had a history of mental health problems. Most participants smoked tobacco (65.4%) and more than half had a lifetime alcohol and/or drug use problem.
Table 1.
Baseline Characteristics of Homeless Adults Aged 50 and Older in Oakland, CA (N = 350), by Living Environment
| Characteristic | All participants (n = 350) | Unsheltered (n = 162) | Multiple location users (n = 88) | Cohabiters (n = 57) | Recently homeless (n = 43) | P valuea |
|---|---|---|---|---|---|---|
| Sociodemographics | ||||||
| Age, median years (IQR) | 58 (54, 61) | 57 (54, 61) | 58 (54, 61) | 56 (53, 61) | 59 (56, 63) | 0.07 |
| Male, No. (%) | 270 (77.1) | 139 (85.8) | 71 (80.7) | 31 (54.4) | 29 (67.4) | <.001 |
| Race/ethnicity, No. (%) | 0.39 | |||||
| African American | 278 (79.7) | 133 (82.1) | 71 (80.7) | 45 (79.0) | 30 (69.8) | |
| White | 38 (10.9) | 16 (9.9) | 10 (11.4) | 4 (7.0) | 8 (18.6) | |
| Latino | 16 (4.6) | 8 (4.9) | 4 (4.6) | 3 (5.3) | 1 (2.3) | |
| Other | 17 (4.9) | 5 (3.1) | 3 (3.4) | 3 (8.8) | 4 (9.3) | |
| Currently married or partnered, No. (%) | 30 (8.6) | 13 (8.0) | 8 (9.1) | 5 (8.8) | 4 (9.3) | 0.12 |
| Less than high school education, No. (%) | 90 (25.7) | 45 (27.8) | 24 (27.3) | 12 (21.1) | 9 (20.9) | 0.87 |
| First episode of adult homelessness age 50 or older, No. (%) | 152 (43.6) | 58 (35.8) | 34 (38.6) | 32 (56.1) | 26 (60.5) | .003 |
| Health status | ||||||
| Fair or poor, No. (%) | 195 (55.7) | 97 (60.0) | 45 (51.1) | 27 (47.4) | 26 (60.5) | 0.27 |
| Chronic medical conditions, No. (%) | ||||||
| Hypertension | 195 (56.0) | 85 (52.5) | 58 (66.7) | 31 (55.4) | 21 (48.8) | 0.12 |
| Coronary artery disease or myocardial infarction | 32 (9.1) | 15 (9.3) | 6 (6.8) | 6 (10.5) | 5 (11.6) | 0.79 |
| Congestive heart failure | 25 (7.1) | 12 (7.4) | 5 (5.7) | 4 (7.0) | 4 (9.3) | 0.90 |
| Diabetes | 49 (14.0) | 16 (9.9) | 15 (17.1) | 11 (19.3) | 7 (16.7) | 0.21 |
| Stroke | 39 (11.2) | 12 (7.5) | 15 (17.1) | 9 (15.8) | 3 (7.0) | 0.06 |
| Chronic obstructive pulmonary disease or asthma | 92 (26.3) | 41 (25.3) | 25 (28.4) | 17 (29.8) | 9 (20.1) | 0.73 |
| Arthritis | 156 (44.6) | 71 (43.8) | 46 (52.3) | 27 (47.4) | 12 (27.9) | 0.07 |
| HIV/AIDS | 19 (5.5) | 5 (3.1) | 8 (9.4) | 2 (3.6) | 4 (9.8) | 0.11 |
| Mental health status | ||||||
| History of mental health problem, No. (%)b | 249 (71.3) | 115 (71.4) | 65 (73.9) | 44 (77.2) | 25 (58.1) | 0.18 |
| History of psychiatric hospitalization, No. (%) | 66 (18.9) | 27 (16.7) | 21 (23.9) | 9 (15.8) | 9 (20.9) | 0.49 |
| Health-related behaviors | ||||||
| Current smoker, No. (%) | 229 (65.4) | 114 (70.4) | 53 (60.2) | 35 (61.4) | 27 (62.8) | 0.46 |
| Alcohol use problem, lifetime, No. (%)c | 206 (59.5) | 92 (57.9) | 56 (64.4) | 32 (56.1) | 26 (60.5) | 0.73 |
| Alcohol use problem, past 6 months, No. (%)d | 90 (25.8) | 51 (31.7) | 17 (19.3) | 15 (26.3) | 7 (16.3) | 0.08 |
| Illicit drug use problem, lifetime, No. (%)e | 206 (58.9) | 98 (60.5) | 53 (60.2) | 30 (52.6) | 25 (58.1) | 0.76 |
| Illicit drug use problem, past 6 months, No. (%)f | 177 (50.6) | 91 (56.2) | 43 (48.9) | 28 (49.1) | 15 (34.5) | 0.09 |
| Health service use and access | ||||||
| Has regular location to obtain health care, No. (%) | 252 (72.0) | 108 (66.7) | 74 (84.1) | 42 (73.7) | 28 (65.1) | 0.02 |
a P value calculated using Kruskal–Wallis nonparametric test for comparison of medians and chi-square tests for comparison of proportions.
bHistory of mental health problems defined as self-reported history of serious anxiety, depression, trouble controlling violent behavior, hallucinations that were not a result of substance use; had attempted suicide; or had been prescribed medication by a doctor for psychiatric or emotional problems.
cLife-time alcohol use problem defined a self-reported history of drinking to get drunk three or more times a week.
dAlcohol use problem, past 6 months defined as an Alcohol Use Disorders Identification Test score ≥8 (range 0–20; higher scores indicate more problems).
eLifetime drug use problem defined as self-reported use of drugs three or more times a week.
fDrug use problem, past 6 months defined as a World Health Organization Alcohol, Smoking and Substance Involvement Screening Test score for either cocaine, amphetamines, or opioids of ≥4 (range 0–39; higher scores indicate more problems).
Participant characteristics including health status and health-related behaviors did not differ significantly across housing groups, with the exception of sex, having a first episode of adult homelessness at age 50 or older, and having a regular location to obtain health care (Table 1).
Living Environment Based on Cluster Analysis
Cluster analysis of the locations where participants stayed over the previous 6 months yielded 4 groupings, as previously reported (Lee et al., 2016). The first group of participants spent most of their time unsheltered (“unsheltered,” n = 162). The second moved between multiple locations including homeless shelters, unsheltered places, hotels, and jails (“multiple location users,” n = 88). The third spent most of their time staying with family and/or friends (“cohabiters,” n = 57). The fourth group had only recently become homeless, and prior to becoming homeless had spent most of their time in rental housing (“recently homeless,” n = 43).
Unsheltered participants spent on average 85.6% of nights unsheltered; multiple location users spent 39.4% of their nights in shelters, 15.8% unsheltered, 13.2% in hotels, and 8.1% in jail/prison; cohabiters spent 71.2% of nights staying with family/friends; and recently homeless individuals spent 80.2% of nights in rental housing. Additional group characteristics are reported elsewhere (Lee et al., 2016).
At the time of the interview, 46.9% of participants reported that they had stayed exclusively in an unsheltered location over the previous 2 weeks, 33.1% had stayed exclusively in a homeless shelter, 8.0% had stayed in both a homeless shelter and an unsheltered location, 2.9% had stayed in transitional housing, 2.6% had stayed with family/friends, 1% had stayed in a hotel, and, in recently homeless individuals, 6.0% had stayed in their own apartment or house. The median time since participants had stable housing was 2.1 years (IQR, 0.6, 5.8).
Geriatric Conditions Overall and by Living Environment
Over a third of participants (38.9%) reported difficulty performing 1 or more ADLs and 49.4% reported difficulty performing 1 or more IADLs (Table 2). Nearly one-fifth (17.1%) had difficulty performing three or more ADLs. More than one-quarter of participants (26.9%) reported difficulty walking, and 33.7% reported one or more falls in the past 6 months; 14.3% fell three or more times. Of participants who reported falling, one-third required medical treatment. One-quarter of participants (25.8%) screened positive for cognitive impairment. Visual impairment was present among 45.1% of participants and hearing impairment was reported by 35.6%, yet only three participants had a hearing aid. Nearly half of participants (48.0%) screened positive for urinary incontinence and 38.3% reported symptoms of major depression.
Table 2.
Comparison of Geriatric Conditions Among Older Homeless Adults in Oakland, CA (N = 350), by Living Environment
| Geriatric conditions, No. (%) | Total (n = 350) | Unsheltered (n = 162) | Multiple location users (n = 88) | Cohabiters (n = 57) | Recently homeless (n = 43) | p valuea |
|---|---|---|---|---|---|---|
| ADL impairmentb,c | 136 (38.9) | 64 (29.5) | 36 (40.9) | 25 (43.9) | 11 (25.6) | .26 |
| IADL impairmentb,d | 173 (49.4) | 85 (52.5) | 48 (54.6) | 23 (40.4) | 17 (39.5) | .17 |
| Mobility impairmente | 94 (26.9) | 42 (25.9) | 25 (28.4) | 18 (31.6) | 9 (20.9) | .66 |
| One or more falls in past 6 monthsf | 118 (33.7) | 55 (34.0) | 35 (39.8) | 17 (29.8) | 11 (25.6) | .38 |
| Cognitive impairmentg | 90 (25.8) | 46 (28.6) | 25 (28.4) | 11 (19.3) | 8 (18.6) | .48 |
| Visual impairmenth | 150 (45.1) | 82 (53.3)i | 30 (35.7) | 23 (42.6) | 15 (36.6) | .04 |
| Hearing impairmentj | 124 (35.6) | 60 (37.3) | 29 (33.0) | 22 (39.3) | 13 (30.2) | .72 |
| Urinary incontinencek | 167 (48.0) | 75 (46.6) | 45 (51.7) | 30 (52.6) | 17 (39.5) | .50 |
| Depressionl | 133 (38.3) | 61 (38.1) | 33 (37.9) | 23 (40.4) | 16 (37.2) | .82 |
aType 3 Wald chi square P value for effect of the housing group variable.
bADL, activities of daily living; IADL, instrumental activities of daily living.
cADL impairment defined as self-reported difficulty performing one or more ADLs.
dIADL impairment defined as self-reported difficulty performing one or more IADLs.
eMobility impairment defined as self-reported difficulty walking across a room.
fFalls were self-reported.
gCognitive impairment defined as a Modified Mini-Mental State Examination score below the 7th percentile (i.e., 1.5 standard deviations below the demographically-adjusted cohort mean).
hVisual impairment defined as a corrected visual acuity worse than 20/40 on a Snellen chart.
iThe standardized residuals for the 4 living environment groups were 2.80 for unsheltered, −1.99 for multiple location users, −0.40 for cohabiters, and −1.16 for recently homeless.
jHearing impairment defined as self-reported difficulty hearing.
kUrinary incontinence assessed using the three Incontinence Questions.
lSymptoms of major depression defined as a Center for Epidemiologic Studies Scale score of >16 (range, 0–60; higher scores indicate more problems).
The prevalence of each geriatric condition did not differ significantly across housing groups. The exception was vision impairment, which was more prevalent in unsheltered participants than in other groups (p =.04, Table 2; standardized residual for unsheltered group, 2.80).
In analyses to determine if age, sex, or substance use problems confounded the relationship between environment and each geriatric condition, the odds of each condition changed less than 10% after adding these variables to the model (data not shown). In analyses to determine if sex modified the association between environment and geriatric conditions, the interaction term for sex and environment was significant only in the model for ADL impairment (unadjusted p for interaction =.04; p adjusted for age, sex, and substance use = .01). Based on the adjusted model including the interaction term, we estimated odds ratios for ADL impairment in women (versus men) in each environment. Women renters, cohabiters, and multiple location users had a higher odds of ADL impairment than men, although the odds ratios for women renters and cohabiters crossed 1. Unsheltered women had a lower odds of ADL impairment than men, though the odds ratio crossed 1 (data not shown).
Duration of time since last stable housing was not significantly associated with the presence of each geriatric condition (data not shown).
Implications
We found that the prevalence of geriatric conditions was high in a population-based sample of older homeless adults. Despite a median age of 58 years, participants had rates of geriatric conditions similar to or higher than adults in the general population with a median age of nearly 80 years (Kelsey et al., 2010; Leveille et al., 2008). Our findings are consistent with earlier research showing that geriatric conditions are common in older homeless people recruited from homeless shelters (Brown et al., 2012), but extend this earlier work through population-based sampling that includes people who meet the federal HEARTH definition of homelessness (Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009). We did not find differences in the prevalence of geriatric conditions across different environments, contrary to our hypothesis (Nyamathi, Leake, & Gelberg, 2000). Our findings suggest that services to address geriatric conditions are needed for older homeless adults living in a range of environments.
Consistent with previous work (Brown et al., 2012), we found that despite this cohort’s relatively younger age, the prevalence of most geriatric conditions was higher compared to both the general older population and the older population living in poverty. Compared to a population-based cohort of adults with a median age of 79 years, rates of several conditions were higher in the older homeless cohort, including ADL impairment (38.9% older homeless vs. 22.6% general older population), IADL impairment (49.4% vs. 40.4%), cognitive impairment (25.8% vs. 12.0%), visual impairment (45.1% vs. 13.8%), and urinary incontinence (48.0% vs. 41.1%) (Brown et al., 2012; Kelsey et al., 2010, Leveille et al., 2008). Although few data are available on the prevalence of geriatric conditions in older adults living in poverty, results from a cohort of community-dwelling adults aged 65 and older (mean age 71.7 years) with income less than 200% of the federal poverty level are similar. Older homeless adults had a higher prevalence of falls (33.7% older homeless adults vs. 21.9% older adults living in poverty), visual impairment (45.1% vs. 12.0%), urinary incontinence (48.0% vs. 29.5%), and depression (38.3% vs. 11.3%) (Counsell et al., 2007).
While the overall prevalence of geriatric conditions in the cohort was disproportionately high compared to older individuals in the general population, the prevalence of geriatric conditions did not differ across living environments. The similar prevalence of geriatric conditions in each environment may reflect several factors. First, it is possible that we lacked power to detect a difference in prevalence due to the relatively small size of the environment subgroups. However, relatively small differences in prevalence are unlikely to be important for clinical practice or policy, and geriatric conditions were prevalent in all subgroups. Second, older homeless people who develop geriatric conditions that are influenced by the person-environment interaction may seek the environment that best fits their abilities, resulting in a “leveling” of the prevalence of geriatric conditions across environments. Survival bias may contribute to this leveling, as older people who are unsheltered and have geriatric conditions may be more likely to be admitted to nursing homes or to die. Finally, the prevalence of key risk factors for geriatric conditions was similar across environments; the similar distribution of risk factors may contribute to the similar prevalence of geriatric conditions.
Different homeless environments pose different challenges in managing geriatric conditions. Adaptive equipment such as glasses or walkers may be lost, damaged, or stolen in any environment, but this risk may be highest in unsheltered environments. These challenges may have contributed to the significantly higher prevalence of vision impairment in unsheltered people; differing access to regular medical care may have also played a role. Our finding that sex modified the association of living environment and ADL impairment may reflect a greater tendency for women with ADL impairment to seek out sheltered environments versus men.
The high prevalence of geriatric conditions in homeless people living in diverse environments has implications for planning services and care. In the general population, approaches to managing geriatric conditions include rehabilitation, environmental modification, and addressing polypharmacy; such interventions reduce adverse outcomes associated with geriatric conditions, including acute care use and institutionalization (Counsell et al., 2007; Gill et al., 2002; Tinetti et al., 1994). However, these interventions are difficult to implement in the environments in which homeless individuals live. This difficulty points to the need for broader solutions that address both geriatric conditions and homelessness.
Permanent supportive housing, defined as subsidized housing with closely linked or on-site supportive services, maintains housing and may reduce acute care utilization among homeless adults (Sadowski, Kee, VanderWeele, & Buchanan, 2009; Stergiopoulos & Herrmann, 2003; Stergiopoulos et al., 2015). Currently, many older homeless adults who have functional impairment and other geriatric conditions may be placed in nursing homes due to a lack of other appropriate options (Bamberger & Dobbins, 2014). However, permanent supportive housing may be able to meet the needs of the aging homeless population, with modifications including personal care attendants and environmental adaptations. Further study is needed to determine if such adapted housing programs could allow formerly homeless individuals to age in place, delaying or preventing the need for nursing home care.
This study has several limitations. We excluded individuals with severe hearing impairment (n = 4) and those unable to provide informed consent (n = 5), potentially leading to an underestimation of the prevalence of hearing and cognitive impairment. Measures of function may not appropriately measure function in vulnerable groups (Tennant et al., 2004). However, we used an IADL assessment tool specifically developed for use in homeless populations (Sullivan et al., 2001). We assessed living environment over the prior 6 months using self-reports, which may be less accurate among persons with cognitive impairment. However, we employed a follow-back residential calendar technique validated for use in homeless populations (Tsemberis et al., 2007). Because the study was conducted in one city, our findings may not be generalizable to other areas. However, participant characteristics were similar to those in nationally representative data (Opening Doors: Federal Strategic Plan to Prevent and End Homelessness Update 2013, 2014).
As the population of older homeless adults continues to grow, developing appropriate services for this group is increasingly important. These services must address the high prevalence of geriatric conditions in older homeless adults living across a range of environments. Housing programs that incorporate interventions to address geriatric conditions provide a promising model of care for this vulnerable and growing population.
Funding
This work was supported by grants from the National Institute on Aging (NIA) at the National Institutes of Health (NIH) [grant numbers K23AG045290 to R.B., K24AG046372 to M.K., R01AG041860 to M.K., P30AG044281 to R.B.]; the NIH National Center for Advancing Translational Sciences through the University of California, San Francisco, Clinical and Translational Science Institute [grant number KL2TR000143 to R.B.]; and a Medical Student in Aging Research Program award from the American Federation for Aging Research and the NIA at NIH to K.H. These funding sources had no role in the preparation, review, or approval of the manuscript. Dr. Brown is an employee of the San Francisco VA Medical Center. The opinions expressed in this manuscript may not represent those of the Department of Veterans Affairs.
Acknowledgements
The authors gratefully acknowledge their colleagues Angela Allen, Pamela Olsen, Nina Fiellin, Tauni Marin, and Kenneth Perez for their invaluable contributions to the HOPE HOME study. The authors also thank the staff at St. Mary’s Center and the HOPE HOME Community Advisory Board for their guidance and partnership. R.B. is a member of the Board of Directors of Hearth, Inc., a non-profit organization dedicated to ending homelessness among the elderly. No other relevant conflicts of interest were reported.
References
- Al-Delaimy W. K. Edland S. Pierce J. P. Mills A. L., & White M. M (2011). California Tobacco Survey (CTS): 2008. California Department of Health Services. California Department of Health Services. Retrieved from http://www.cdph.ca.gov/programs/tobacco/Documents/CTCPCaliforniaAdultTobaccoSurvey2008.pdf
- Babor T. F. Higgins-Biddle J. C. Saunders J. B., & Monteiro M. G (2001). The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care: World Health Organization. Retrieved from http://www.talkingalcohol.com/files/pdfs/WHO_audit.pdf
- Baggett T. P. Hwang S. W. O’Connell J. J. Porneala B. C. Stringfellow E. J. Orav E. J., … Rigotti N. A (2013). Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med, 173, 189–195. doi:10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamberger J. D., & Dobbins S (2014). Long-term cost effectiveness of placing homeless seniors in permanent supportive housing. San Francisco, CA: Federal Reserve Bank of San Francisco; Retrieved from http://www.frbsf.org/community-development/files/wp2014-01.pdf [Google Scholar]
- Bland R. C., & Newman S. C (2001). Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3MS) as a screen for dementia. Canadian Journal of Psychiatry, 46, 506–510. [DOI] [PubMed] [Google Scholar]
- Bravo G., & Hebert R (1997). Age-and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. International Journal of Geriatric Psychiatry, 12, 1008–1018. doi:10.1002/(SICI)1099–1166(199710)12:10<1008::AID-GPS676>3.0.CO;2-A [DOI] [PubMed] [Google Scholar]
- Brown J. S. Bradley C. S. Subak L. L. Richter H. E. Kraus S. R. Brubaker L., … Grady D (2006). The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Annals of Internal Medicine, 144, 715–723. doi:10.7326/0003-4819-144-10-200605160-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. T. Kiely D. K. Bharel M., & Mitchell S. L (2012). Geriatric syndromes in older homeless adults. Journal of General Internal Medicine, 27, 16–22. doi:10.1007/s11606-011-1848-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt M. Aran L. Douglas T. Valente J. Lee E., & Iwen B (1999). Homelessness: programs and the people they serve: findings from the national survey of homeless assistance providers and clients, Technical Report. Washington, DC: The Urban Institute. [Google Scholar]
- Calinski T., & Harabasz J (1974). A dendrite method for cluster analysis. Communications in Statistics, 3, 1–27. doi:10.1080/03610927408827101 [Google Scholar]
- Cohen C. I. (1999). Aging and homelessness. Gerontologist, 39, 5–14. doi:10.1093/geront/39.1.5 [DOI] [PubMed] [Google Scholar]
- Counsell S. R. Callahan C. M. Clark D. O. Tu W. Buttar A. B. Stump T. E., & Ricketts G. D (2007). Geriatric care management for low-income seniors: a randomized controlled trial. JAMA, 298, 2623–2633. doi:10.1001/jama.298.22.2623 [DOI] [PubMed] [Google Scholar]
- Culhane D. P. Metraux S. Byrne T. Stino M., & Bainbridge J (2013). The age structure of contemporary homelessness: evidence and implications for public policy. Analyses of Social Issues and Public Policy, 13, 228–244. doi:10.1111/asap.12004 [Google Scholar]
- Dunn L. B., & Jeste D. V (2001). Enhancing informed consent for research and treatment. Neuropsychopharmacology, 24, 595–607. doi:10.1016/s0893-133x(00)00218-9 [DOI] [PubMed] [Google Scholar]
- Everitt B. S. Landau S. Leese M., & Stahl D (2011). Cluster Analysis. Chichester, UK: Wiley. [Google Scholar]
- Garibaldi B. Conde-Martel A., & O’Toole T. P (2005). Self-reported comorbidities, perceived needs, and sources for usual care for older and younger homeless adults. Journal of General Internal Medicine, 20, 726–730. doi:10.1111/j.1525-1497.2005.0142.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L. Linn L. S., & Mayer-Oakes S. A (1990). Differences in health status between older and younger homeless adults. Journal of the American Geriatrics Society, 38, 1220–1229. doi:10.1111/j.1532–5415.1990.tb01503.x [DOI] [PubMed] [Google Scholar]
- Gill T. M. Baker D. I. Gottschalk M. Peduzzi P. N. Allore H., & Byers A (2002). A program to prevent functional decline in physically frail, elderly persons who live at home. New England Journal of Medicine, 347, 1068–1074. doi:10.1056/NEJMoa020423 [DOI] [PubMed] [Google Scholar]
- Hahn J. A. Kushel M. B. Bangsberg D. R. Riley E., & Moss A. R (2006). BRIEF REPORT: the aging of the homeless population: fourteen-year trends in San Francisco. Journal of General Internal Medicine, 21, 775–778. doi:10.1111/j.1525-1497.2006.00493.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J. F. Black W. C. Babin B. J., & Anderson R. E (1987). Multivariate Data Analysis. New York: Macmillan USA. [Google Scholar]
- Health and Retirement Survey (HRS) (2012). Ann Arbor, MI: National Institute on Aging, University of Michigan Institute for Social Research; Retrieved from: http://hrsonline.isr.umich.edu/modules/meta/2012/core/qnaire/online/03hr12C.pdf [Google Scholar]
- Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009 Definition of homelessness. U.S. Congress (2009). [Google Scholar]
- Humeniuk R. Henry-Edwards S. Ali R. Poznyak V., & Monteiro M (2010). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in primary care. Geneva: World Health Organization. [Google Scholar]
- Hwang S. W. Orav E. J. O’Connell J. J. Lebow J. M., & Brennan T. A (1997). Causes of death in homeless adults in Boston. Annals of Internal Medicine, 126, 625–628. doi:10.7326/0003-4819-126-8-199704150-00007 [DOI] [PubMed] [Google Scholar]
- Inouye S. K. Peduzzi P. N. Robison J. T. Hughes J. S. Horwitz R. I., & Concato J (1998). Importance of functional measures in predicting mortality among older hospitalized patients. JAMA, 279, 1187–1193. doi:10.1001/jama.279.15.1187 [DOI] [PubMed] [Google Scholar]
- Inouye S. K. Studenski S. Tinetti M. E., & Kuchel G. A (2007). Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. Journal of the American Geriatrics Society, 55, 780–791. doi:10.1111/j.1532-5415.2007.01156.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz S. (1983). Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society, 31, 721–727. doi:10.1111/j.1532–5415.1983.tb03391.x [DOI] [PubMed] [Google Scholar]
- Kelsey J. L. Berry S. D. Procter-Gray E. Quach L. Nguyen U. S. Li W., … Hannan M. T (2010). Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and Zest in the Elderly of Boston Study. Journal of the American Geriatrics Society, 58, 2135–2141. doi:10.1111/j.1532-5415.2010.03062.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbler K. J. DeWees M. A., & Harris A. N (2015). Characteristics of the old and homeless: identifying distinct service needs. Aging & Mental Health, 1–9. doi:10.1080/13607863.2015.1088512 [DOI] [PubMed] [Google Scholar]
- Kohn H. F. Steinley D., & Brusco M. J (2010). The p-median model as a tool for clustering psychological data. Psychological Methods, 15, 87–95. doi:10.1037/a0018535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel M. (2012). Older homeless adults: can we do more? Journal of General Internal Medicine, 27, 5–6. doi:10.1007/s11606-011-1925-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton M. P., & Nahemow L (1973). Ecology and the aging process. In Eisdorfer C., Lawton M. P. (Eds.), The psychology of adult development and aging (pp. 619–674). Washington, DC: American Psychological Association. [Google Scholar]
- Lee C. T. Guzman D. Ponath C. Tieu L. Riley E., & Kushel M (2016). Residential patterns in older homeless adults: Results of a cluster analysis. Social Science & Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leveille S. G. Kiel D. P. Jones R. N. Roman A. Hannan M. T. Sorond F. A., … Lipsitz L. A (2008). The MOBILIZE Boston Study: design and methods of a prospective cohort study of novel risk factors for falls in an older population. BMC Geriatrics, 8, 16. doi:10.1186/1471-2318-8-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan A. T. Kushner H. Metzger D. Peters R. Smith I. Grissom G., … Argeriou M (1992). The fifth edition of the addiction severity index. J Subst Abuse Treat, 9, 199–213. doi:10.1016/0740-5472(92)90062-S [DOI] [PubMed] [Google Scholar]
- Moyer V. A. (2012). Screening for hearing loss in older adults: U.S. Preventive Services Task Force recommendation statement. Annals of Intern Medicine, 157, 655–661. doi:10.7326/0003-4819-157-9-201211060-00526 [DOI] [PubMed] [Google Scholar]
- National Health Interview Survey (NHIS) (2012). Adult Access to Health Care and Utilization. Hyattsville, MA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- National Health and Nutrition Examination Survey Questionnaire (NHANES) (2009). Hyattsville, MD: U.S: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- North C. S., & Smith E. M (1993). A comparison of homeless men and women: different populations, different needs. Community Mental Health Journal, 29, 423–431. doi:10.1007/BF00754410 [DOI] [PubMed] [Google Scholar]
- Nyamathi A. M. Leake B., & Gelberg L (2000). Sheltered versus nonsheltered homeless women differences in health, behavior, victimization, and utilization of care. Journal of General Internal Medicine, 15, 565–572. doi:10.1046/j.1525-1497.2000.07007.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opening Doors: Federal Strategic Plan to Prevent and End Homelessness Update 2013 (2014). Washington, DC: United States Interagency Council on Homelessness. [Google Scholar]
- Radloff L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Sadowski L. S. Kee R. A. VanderWeele T. J., & Buchanan D (2009). Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA, 301, 1771–1778. doi:10.1001/jama.2009.561 [DOI] [PubMed] [Google Scholar]
- Screening for impaired visual acuity in older adults: U.S. Preventive Services Task Force recommendation statement (2009). Annals of Intern Medicine, 151, 37–43. doi:10.7326/0003-4819-151-1-200907070-00007 [DOI] [PubMed] [Google Scholar]
- Stergiopoulos V., & Herrmann N (2003). Old and homeless: a review and survey of older adults who use shelters in an urban setting. Canadian Journal of Psychiatry, 48, 374–380. [DOI] [PubMed] [Google Scholar]
- Stergiopoulos V. Hwang S. W. Gozdzik A. Nisenbaum R. Latimer E. Rabouin D., … Goering P. N (2015). Effect of scattered-site housing using rent supplements and intensive case management on housing stability among homeless adults with mental illness: a randomized trial. JAMA, 313, 905–915. doi:10.1001/jama.2015.1163 [DOI] [PubMed] [Google Scholar]
- Sullivan G. Dumenci L. Burnam A., & Koegel P (2001). Validation of the brief instrumental functioning scale in a homeless population. Psychiatric Services, 52, 1097–1099. doi:10.1176/appi.ps.52.8.1097 [DOI] [PubMed] [Google Scholar]
- Szanton S. L. Thorpe R. J. Boyd C. Tanner E. K. Leff B. Agree E., … Gitlin L. N (2011). Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. Journal of American Geriatrics Society, 59, 2314–2320. doi:10.1111/j.1532-5415.2011.03698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennant A. Penta M. Tesio L. Grimby G. Thonnard J. L. Slade A., … Phillips S (2004). Assessing and adjusting for cross-cultural validity of impairment and activity limitation scales through differential item functioning within the framework of the Rasch model: the PRO-ESOR project. Med Care, 42(1 Suppl), I37–48. doi:10.1097/01.mlr.0000103529.63132.77 [DOI] [PubMed] [Google Scholar]
- Tinetti M. E. Baker D. I. McAvay G. Claus E. B. Garrett P. Gottschalk M., … Horwitz R. I (1994). A multifactorial intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine, 331, 821–827. doi:10.1056/nejm199409293311301 [DOI] [PubMed] [Google Scholar]
- Tschanz J. T. Corcoran C. Skoog I. Khachaturian A. S. Herrick J. Hayden K. M., … Breitner J. C (2004). Dementia: the leading predictor of death in a defined elderly population: the Cache County Study. Neurology, 62, 1156–1162. doi:10.1212/01.WNL.0000118210.12660.C2 [DOI] [PubMed] [Google Scholar]
- Tsemberis S. McHugo G. Williams V. Hanrahan P., & Stefancic A (2007). Measuring homelessness and residential stability: the residential time-line Follow-Back Inventory. Journal of Community Psychology, 35, 29–42. doi:10.1002/jcop.20132 [Google Scholar]
- Wahl H. W. Fange A. Oswald F. Gitlin L. N., & Iwarsson S (2009). The home environment and disability-related outcomes in aging individuals: what is the empirical evidence? Gerontologist, 49, 355–367. doi:10.1093/geront/gnp056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward J. H. (1963). Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association, 58, 236–244. doi:10.1080/01621459.1963.10500845 [Google Scholar]
- Ware J. Jr. Kosinski M., & Keller S. D (1996). A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care, 34, 220–233. [DOI] [PubMed] [Google Scholar]
- Weiser S. D. Hatcher A. Frongillo E. A. Guzman D. Riley E. D. Bangsberg D. R., & Kushel M. B (2013). Food insecurity is associated with greater acute care utilization among HIV-infected homeless and marginally housed individuals in San Francisco. Journal of General Internal Medicine, 28, 91–98. doi:10.1007/s11606-012-2176-4 [DOI] [PMC free article] [PubMed] [Google Scholar]