Abstract
Purpose:
Active aging is a concept that lacks consensus. The WHO defines it as a holistic concept that encompasses the overall health, participation, and security of older adults. Fernández-Ballesteros and colleagues propose a similar concept but omit security and include mood and cognitive function. To date, researchers attempting to validate conceptual models of active aging have obtained mixed results. The goal of this study was to examine the validity of existing models of active aging with epidemiological data from Canada.
Methods:
The WHO model of active aging and the psychological model of active aging developed by Fernández-Ballesteros and colleagues were tested with confirmatory factor analysis. The data used included 799 community-dwelling older adults between 65 and 74 years old, recruited from the patient lists of family physicians in Saint-Hyacinthe, Quebec and Kingston, Ontario.
Results:
Neither model could be validated in the sample of Canadian older adults. Although a concept of healthy aging can be modeled adequately, social participation and security did not fit a latent factor model. A simple binary index indicated that 27% of older adults in the sample did not meet the active aging criteria proposed by the WHO.
Implications:
Our results suggest that active aging might represent a human rights policy orientation rather than an empirical measurement tool to guide research among older adult populations. Binary indexes of active aging may serve to highlight what remains to be improved about the health, participation, and security of growing populations of older adults.
Keywords: Active aging, Gerontology, Health promotion, Factor analysis
Global aging has fostered the development of a positive discourse about aging, including healthy, successful, or active aging. Aging is no longer presented as an unavoidable period of decline that requires withdrawal from active life (Rowe & Kahn, 1997). Of all the existing concepts accompanying this positive vision of aging, this article focuses on active aging because it is a more holistic and inclusive concept that encompasses the economic and physical security of older adults (Foster & Walker, 2014). In this article, we propose to test and compare two models of active aging using epidemiological data collected among older adults in Canada.
Competing definitions for the concept of active aging coexist and there remains overlap between active and successful aging. Although active aging is sometimes used as a proxy to designate either productive or physically active elders, most authors dismiss unidimensional measures in favor of a more holistic definition that encompasses physical, mental, and social functions (Boudiny, 2012). In this study, we focus specifically on a multidimensional concept of active aging that takes into account the impact of the social context on aging. The World Health Organization (WHO, 2002) defines active aging as “the process of optimizing opportunities for health, participation and security in order to enhance quality of life as people age” (emphasis added, p.12). The WHO proposes a broad concept that is influenced by gender and culture, and that is composed of behavioral, personal, physical, social, and economic determinants, as well as health and social services. Another perspective about active aging is proposed by Fernández-Ballesteros, Robine, Walker, and Kalache (2013) in the field of psychology. They define active aging as a low probability of illness and disability, high physical fitness, high cognitive functioning, positive mood and coping with stress, and being engaged with life. Important differences between these two models are that the concept proposed by the WHO takes into account the physical and economic security of older adults as part of a human rights based approach to social and health policy in the face of population aging, while Fernández-Ballesteros focuses on psychological aspects such as cognition and mood. Underlying the WHO inclusion of security in the concept of active aging is the proposition that conditions of poverty and violence in many countries of the world are barriers to active aging, because lack of financial security or personal safety hampers quality of life for older adults.
Although research and policy initiatives aiming to promote the health and participation of older populations have been multiplying over the last decade, there remains a considerable lack of conceptual clarity about active aging. Unfortunately, active ageing is often used interchangeably with subtly divergent notions such as successful aging, quality of life, and healthy aging, hampering the development of empirical measurement. Bowling (2008) compared lay perceptions of active aging in a sample of 337 people aged more than 65, with the results of previous research about successful aging (Bowling, 2005) and quality of life (Bowling, Banister, Sutton, Evans, & Windsor, 2002). The most common descriptions of active aging reported by participants were “maintaining physical health and functioning (43%), leisure and social activities (34%), mental functioning and activity (18%), and social relationships and contacts (15%)” (Bowling, 2008, p. 294). There was remarkable similarity in the themes mentioned across the different concepts, although healthy aging and quality of life were generally viewed as end points and “states of being.”
Previous studies have had mixed results when attempting to verify the validity of conceptual models of active aging. Paul, Ribeiro, and Teixeira (2012) tested a model using the determinants of active aging that were proposed by the WHO. They used confirmatory factor analysis on the data collected during interviews conducted among 1,322 seniors in Portugal. Their analysis failed to confirm the WHO conceptual model insofar as some of the determinants were deeply intertwined (Paul et al., 2012). They rather obtained a model that accounted for more than 50% of the variance present in the data and that included six factors: health, psychological components, cognitive performance, social relationships, bio-behavioral components, and personality. They concluded that psychological factors play a larger role in their data than acknowledged in the WHO model (Paul et al., 2012). However, their analysis can be criticized for proposing a measurement model based on the determinants of active aging rather than on indicators of the concept (Fernández-Ballesteros, 2008).
A lack of conceptual clarity is by no means unique to the notion of active aging. Despite a growing interest in successful aging among gerontologists, as evidenced by a recent special issue of The Gerontologist devoted to the topic, there are fundamental differences in definitions and concepts among research groups, health care providers and seniors, themselves. A comprehensive review of research about successful aging identified 29 different definitions of this concept (Depp & Jeste, 2006). These definitions and models range from the purely biomedical with a focus on longevity and the delaying of morbidity, through preservation of cognitive function, to an emphasis on well-being and life satisfaction (Lupien & Wan, 2004). Moreover, the validity of successful aging models has also been challenged when using confirmatory factor analysis methods. Lee, Lan, and Yen (2011) tested a very similar model to the one proposed by Fernández-Ballesteros and colleagues, but labeled it as successful aging, and erroneously accepted a measurement model that poorly captured the variance of the items included in the model. Alternatively, fairly simple indexes have been suggested to measure the presence or absence of components of both active and successful aging (Hank, 2011; McLaughlin, Connell, Heeringa, Li, & Roberts, 2010; Zasimova & Sheluntcova, 2014). These indexes tend to be difficult to compare because they imply arbitrary cutoff points, and they are not standardized in terms of the variables that are considered.
In Canada, there is a paucity of research about active aging. Until now, the few studies conducted about positive notions of aging in Canada have focused on lay perceptions of successful aging rather than on the validity of empirical measurement (Tate, Lah, & Cuddy, 2003; Tate, Swift, & Bayomi, 2013). In one of these studies, researchers analyzed the responses of 2,783 Canadian seniors to the open-ended question: “What do you think makes people live long and keep well?” (Bassett, Bourbonnais, & McDowell, 2007). The authors conclude that individual behaviors, primarily nutrition and physical activity, figure prominently in respondents’ justifications for successful aging (Bassett et al., 2007). Overall, it remains unclear whether existing models of active aging are valid in a Canadian context. In order to address this research gap, we propose to review and test empirically different definitions of active aging using data collected among a sample of older Canadian adults that took part in a large international epidemiological study on mobility and aging.
The goal of this study was to examine the validity of existing models of active aging using epidemiological data from Canada. Our hypothesis was that a latent reflective measurement model for active aging as defined by the WHO (2002) or by Fernández-Ballesteros and colleagues (2013) could be validated in Canadian populations of older adults. Reflective models are developed to measure a latent, unobserved concept, such as intelligence, which can only be quantified through other observed variables (Kline, 2011). The variables that form a latent factor are expected to covary and to be interchangeable because they represent a common underlying concept. Conceptually, reflective measurement models differ from formative models, which have cause indicators. An example of formative model would be socioeconomic status, whereby someone can have a high level of education but be unemployed. Cause indicators do not need to covary and part of the concept is lost when omitting one of them (Kline, 2011).
Design and Methods
Study Population and Recruitment Methods
This study used data collected in 2012 from a sample of 799 community-dwelling Canadian adults aged 65–74 who had been recruited for the International Mobility in Aging Study (IMIAS) (Sousa et al., 2014). Half of the participants were living in Saint-Hyacinthe, Quebec, whereas the other half were residents of Kingston, Ontario. The samples were drawn from primary care clinics rosters. Due to Ethics Committees requirements at Queens University and University of Montreal, participants could not be contacted directly. Instead, older adults were invited to participate in the IMIAS study via a letter from their family physician. Potential participants were instructed to contact our field coordinator to obtain information about the study. Around 30% of persons who had received an invitation called to obtain information about the study, and among them 95% agreed to participate. In Saint-Hyacinthe, the invitations were stratified by sex and neighbourhood, and as such, according to the 2006 Canadian Census the resulting sample of participants was representative of the residents of Saint-Hyacinthe’s population for this age group, in terms of education, income, and marital status. In Kingston, according to the same census, the study sample was representative of the population aged between 65 and 74 in terms of income and marital status. However, the sample over-represented the population with a university-level education.
Data Collection
At all sites, study procedures were carried out at the participant’s home. The questionnaires, the data collection documents, and manuals of procedures are available in English and in French.
Ethical Requirements
Ethical approval for this project was obtained from Queen’s University and the Research Centre of the University of Montreal Hospital Complex.
Variables
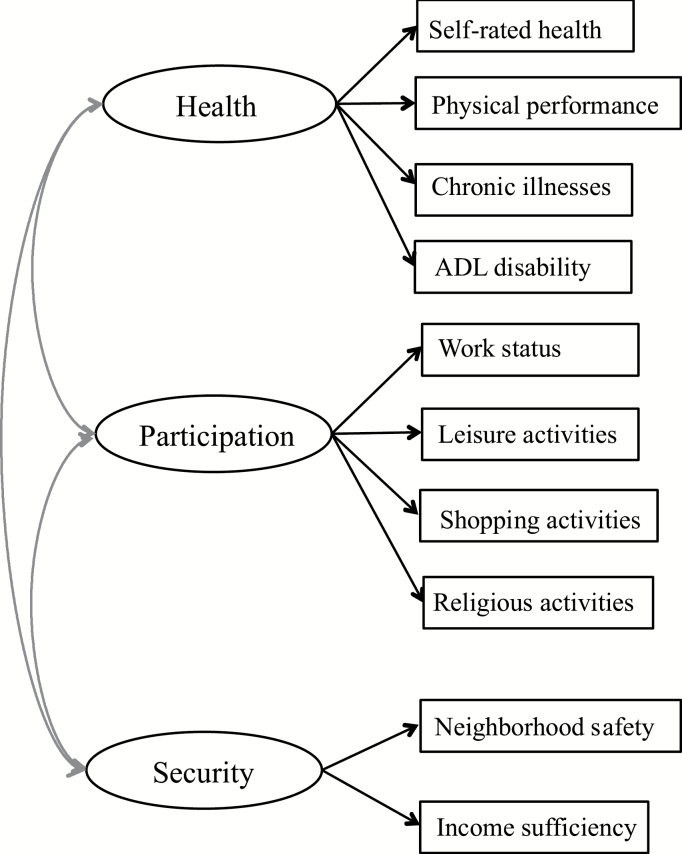
The validity of the two conceptual models of active aging was assessed by creating two measurement models of active aging using the relevant variables from the IMIAS 2012 baseline data set. In both models, the factors creating the construct of active aging were allowed to covary freely. Figure 1 presents the variables that were hypothesized as part of the factors of health, participation, and security for the WHO model of active aging. Note that the arrows flow from the latent constructs to the observed variables and that these would be reversed if a formative model had been hypothesized.
Figure 1.
Hypothesized WHO model active aging in Canada.
The “health factor” consisted of self-rated health (Likert scale from 1 [very poor] to 5 [very good]), a physical performance score (12-point score on the SPPB) (Guralnik et al., 1994), the number of frequent chronic illnesses between 0 and 7 (including hypertension, diabetes, heart disease, chronic respiratory disease, cerebrovascular accident, arthritis, and cancer), and the total self-reported score on the presence of disability in seven basic activities of daily living such as getting out of bed, dressing, and bathing (0–7). The “participation factor” is composed of a binary work status, and of three variables about the frequency of community activities, shopping activities, and religious activities (Likert scale from 0 [never] to 5 [everyday]). The “security factor” comprised two items, namely perceived income security (measured with a single question using a 4-point response scale) and neighbourhood safety (measured with a single question—whether or not participants felt safe when they were walking in their neighbourhood—using a 3-point scale).
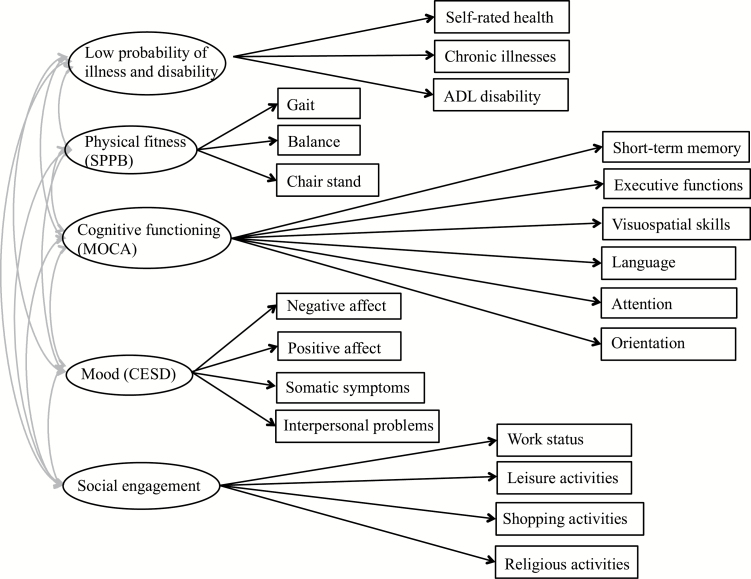
Figure 2 presents the hypothesized model of active aging following the definition proposed by Fernández-Ballesteros and colleagues (2013). The five-factor structure encompasses health, physical fitness, cognitive function, mood, and social engagement. In this model, “health factor” and “physical fitness factor” are hypothesized to be two different latent factors, with the former including self-rated health, ADL disability, and chronic illnesses, whereas the latter is the short physical performance battery (SPPB) score composed of measures of gait speed, balance, and the chair-stand test, each on a 4-point scale (Guralnik et al., 1994). The “cognitive function factor” was measured with the Montreal Cognitive Assessment scale (MOCA) (Nasreddine et al., 2005). The MOCA is composed of six dimensions according to existing research, namely short-term memory (0–5), executive functions (0–4), visuospatial skills (0–4), language (0–5), attention (0–6), and orientation (0–6; Freitas, Simões, Marôco, Alves, & Santana, 2011). The “mood factor” was measured with the Centre for Epidemiological Studies Depression scale (CES-D) (Radloff, 1977), which comprises 20 Likert-scale items (0–3 points each). Following previous work done by Irwin, Artin, and Oxman (1999), we grouped the items according to negative affect (7 items), positive affect (4 items), somatic symptoms (7 items), and interpersonal problems (2 items). Finally, the “social engagement factor” was measured with the same items as social participation used in the WHO model.
Figure 2.
Hypothesized Fernandez Ballesteros et al. model of active aging in Canada.
Data Analyses
Before fitting the models, the multivariate normality of the data was assessed by performing skewness and kurtosis tests. Most of the variables included in the models were highly skewed and failed the multivariate normality tests. For this reason, the models were estimated with an asymptotically distribution-free estimation method that relaxes the normality assumptions in structural equation modeling (Kline, 2011). To ensure a valid measurement model, we then examined closely the correlation matrices and the Cronbach’s alpha as an indicator of internal consistency for each of the factors in the hypothesized models. These results guided us in testing the hypothesized models using confirmatory factor analysis, which is a covariance-based estimation method. Kline (2011) warns against fitting models when the correlations between items are low: he suggests .50 as a minimum benchmark for adequate use of this method. This is an important prerequisite for confirmatory factor analysis, and one that has been overlooked by previous authors in the field (e.g., Lee et al., 2011). For each of the fitted models, we thus excluded items that had low correlations with other items in the same hypothesized factor, because this implied that they did not represent a common, reflective latent factor and might be better suited for other conceptual models such as formative models or indexes (Edwards & Bagozzi, 2000). The final fitted models are presented in the results section. We opted to report unstandardized parameter estimates, because the variables are not normally distributed and we wanted to preserve the scales of variables such as the number of chronic conditions. The size of the factor loadings therefore cannot be directly compared in the models, and we report each individual item’s explained variance because the error terms for individual items are not as informative with unstandardized coefficients.
Model Fit Evaluation
The fitted models are accompanied by several goodness-of-fit indexes in order to assess the validity of the models. The first indicator of fit, chi-square, represents a badness-of-fit statistic comparing the observed and expected covariance matrices; we thus hope for a nonsignificant result that would fail to reject the hypothesized model. This test is however sensitive to sample size, so that we are more likely to reject model fit with large sample sizes (Hu & Bentler, 1999; Steiger, 2007). To complement this strict model fit statistic, we present the root mean square error of approximation (RMSEA), the standardized root mean square residual (SRMR), and the comparative fit index (CFI). Both the RMSEA and the SRMR range between 0 and 1, and smaller values indicate better model fit (Kline, 2011). An acceptable fit is found when the former is .06 or less, and the latter is .08 or less. The CFI also range from 0 to 1, but larger values indicate a better fit, and we are aiming for a value of .90 or larger as an acceptable model fit. The coefficient of determination is the R2 statistics provided for the models. We then present some simple descriptive binary indexes for the concept of active aging, as proposed by previous authors (Zasimova & Sheluntcova, 2014). All of the statistical analyses were performed using Stata 12.
Results
A Confirmatory Factor Analysis of the WHO Model of Active Aging
Table 1 shows the correlations between the items hypothesized to fit the WHO model of active aging in Canadian IMIAS database. It is very clear that many of the variables are not highly correlated and as such cannot be considered to represent a common latent factor. Our hypothesis about the validity of a latent, reflective measurement model for active aging as defined by the WHO can be rejected on the basis of this result in our Canadian data. The correlation between the four items composing the “health factor” are acceptable and mostly close to the .50 recommended value. The Cronbach’s alpha for this factor is also acceptable at .66 (Kline, 2011). In terms of the “participation factor,” however, the correlations are much lower than needed and the Cronbach’s alpha is .22. In fact, it appears that the older adults who participate in a given activity, such as shopping, tend to participate less in another, such as religious activities. A latent factor is therefore not an appropriate model to capture the variance for these items; items with negative correlations cannot be estimated under a common factor. The items of the latent factor “security” are also poorly correlated and do not represent an overarching concept of security. Overall, the data collected did not support the hypothesized three-factor WHO model. Only the “health factor” could be estimated with the data.
Table 1.
Correlation of Hypothesized Items for the WHO Model of Active Aging
| Health | Self-rated health | SPPB | Chronic illnesses | ADL disability |
|---|---|---|---|---|
| Self-rated health | 1 | |||
| SPPB | 0.39 | 1 | ||
| Chronic illnesses | 0.44 | 0.32 | 1 | |
| ADL disability | 0.39 | 0.47 | 0.25 | 1 |
| Cronbach's alpha: 0.66 | ||||
| Participation | Work status | Community activities | Shopping activities | Religious activities |
| Work status | 1 | |||
| Community | −0.04 | 1 | ||
| Shopping | −0.07 | 0.15 | 1 | |
| Religious | −0.02 | 0.14 | −0.03 | 1 |
| Cronbach's alpha: 0.23 | ||||
| Security | Neighborhood safety | Income sufficiency | ||
| Neighborhood safety | 1 | |||
| Income sufficiency | 0.14 | 1 |
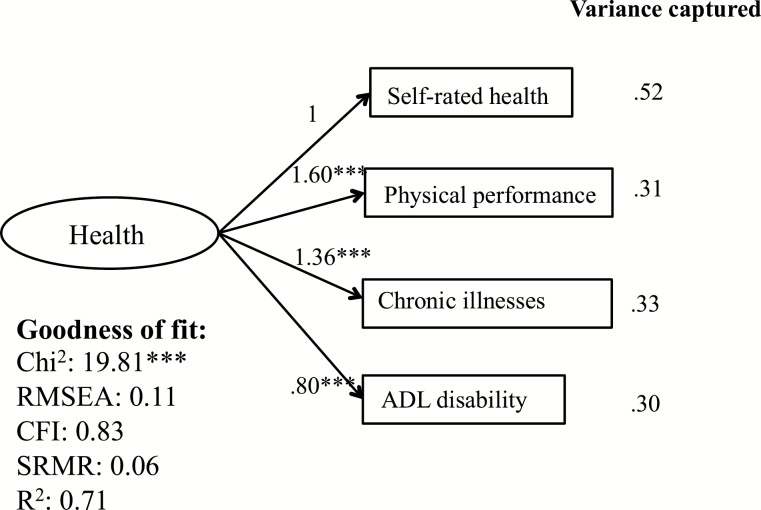
Figure 3 reports the unstandardized values obtained when fitting the “health factor” from the WHO model of active aging. All of the items are significantly related to the latent factor. The variance explained for the individual items remained low, suggesting that a large portion of unique variances in these items is not captured within this common factor. As far as the goodness-of-fit statistics are concerned, for the “health factor” only, the chi-square is significant but still fairly small considering the sample size. Although the RMSEA is above an acceptable value at .11, both the SRMR and the CFI suggest an acceptable model fit, at .06 and .83, respectively. To conclude, we were unable to validate the WHO model of active aging within the Canadian IMIAS data. We could only estimate a concept of healthy aging without the “participation” and “security” factors, and it does not successfully capture the variance of the individual items, namely in terms of self-rated health, the number of chronic illnesses, SPPB, and the number of ADL disabilities.
Figure 3.
Fitted health factor of WHO model of active aging in Canada.
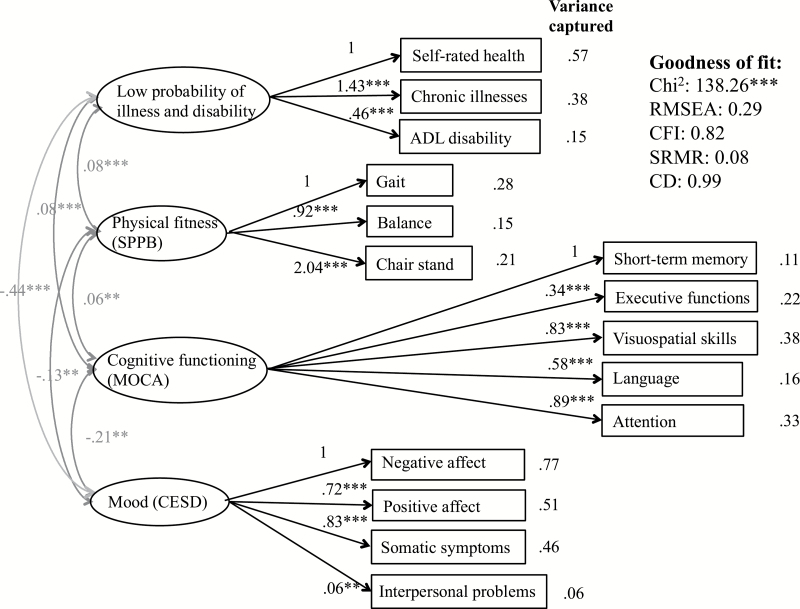
A Confirmatory Factor Analysis of the Model of Active Aging Proposed by Fernández-Ballesteros and Colleagues
Table 2 describes the correlation between the items hypothesized for the model of active aging as developed by Fernández-Ballesteros and colleagues (2013). We had already determined that the items included in the “social engagement factor” did not meet the correlation levels necessary to fit a latent factor structure, so this aspect of the model was omitted. The orientation variable was also removed from the “cognitive functioning factor,” because it was not highly correlated with other items in their factor. In fact, there was little variance in this item among the sample under study. Figure 4 reports the unstandardized factor loadings obtained after fitting the four remaining factors. The variance of individual items that is captured by the factors remains particularly problematic for all of the factors. Moreover, this model of active aging does not offer a satisfactory model fit. Although the RMSEA is excellent, the goodness-of-fit statistics are particularly mediocre when considering the χ2, the SRMR, and the CFI. In summary, the active aging model proposed by Fernández-Ballesteros and colleagues does not fit the Canadian IMIAS data either.
Table 2.
Correlation of Hypothesized Items for Model of Active Aging According to Fernandez-Ballesteros and Colleagues
| Illness and disability | Self-rated health | Chronic illnesses | ADL disability | |||
|---|---|---|---|---|---|---|
| Self-rated health | 1 | |||||
| Chronic illnesses | 0.44 | 1 | ||||
| ADL disability | 0.39 | 0.25 | 1 | |||
| Cronbach’s alpha: 0.59 | ||||||
| Physical fitness (SPPB) | Gait | Balance | Chair rise | |||
| Gait | 1 | |||||
| Balance | 0.29 | 1 | ||||
| Chair rise | 0.38 | 0.23 | 1 | |||
| Cronbach’s alpha: 0.51 | ||||||
| Mood (CES-D) | Negative affect | Positive affect | Somatic symptoms | Interpersonal problems | ||
| Negative affect | 1 | |||||
| Positive affect | 0.66 | 1 | ||||
| Somatic symptoms | 0.69 | 0.53 | ||||
| Interpersonal problems | 0.4 | 0.35 | 0.32 | 1 | ||
| Cronbach’s alpha: 0.77 | ||||||
| Cognitive Function (MOCA) | Short-term memory | Executive function | Visuospatial skills | Language | Attention | Orientation |
| Short-term memory | 1 | |||||
| Executive function | 0.18 | 1 | ||||
| Visuospatial skills | 0.22 | 0.30 | 1 | |||
| Language | 0.21 | 0.18 | 0.31 | 1 | ||
| Attention | 0.17 | 0.29 | 0.35 | 0.28 | 1 | |
| Orientation | 0.05 | 0.09 | 0.10 | 0.14 | 0.13 | 1 |
| Cronbach’s alpha: 0.53 |
Figure 4.
Fitted Fernandez Ballesteros et al. model of active aging in Canada.
Descriptive Binary Index of Active Aging in Canada
We proceeded to create a simple binary index to provide a portrait of the state of active aging in Canada according to the WHO definition. It is considered that older adults meet the criteria for active aging only if they do not report any of the problems that are presented in Table 3 in the domains of health, participation, or security. Respondents did not fulfill the requirements of the health domain if they report any of the following: poor or very poor self-rated health, a physical performance (SPPB) score below 8, disability in more than two activities of daily living, and more than three common chronic illnesses. Although participants who were employed met the requirement of participation, those who were not on the labor market did not achieve a desired level of participation if they also either did not have any monthly social contact with friends and family members, or if they were not taking part in any of the three types of social activities that were measured. Finally, for the security component of the index older adults who reported either feeling unsafe to walk in their neighbourhood or having an insufficient income did not meet the criteria of active aging. When choosing these cutoff points in a very simple binary index, 27% of the IMIAS sample of 799 Canadian older adults could not be considered as aging actively because of a problem in at least one of the three domains. More than half of these older adults reported problems in more than one domain. Having more than three common chronic illnesses was the most common problem reported in the sample and thus represented the biggest barriers to aging actively following this definition.
Table 3.
Binary Index WHO Model of Active Aging in Canada
| % Inactive | |
|---|---|
| Healtha | 17.15 |
| Poor/very poor self-rated health | 2.26 |
| Physical performance score below 8 | 7.26 |
| Disability in more than 2 activities of daily living | 6.01 |
| More than 3 chronic illnesses | 10.51 |
| Participationa | 7.01 |
| Not working and no monthly social contact | 2.38 |
| Not working and no participation in social activities | 5.01 |
| Securitya | 8.64 |
| Feel unsafe when walking in neighbourhood | 2.75 |
| Insufficient income | 6.38 |
| Total inactivea | 27.03 |
aReporting problems for one or more criteria.
Discussion
This article aimed to assess the validity of two models of active aging among a Canadian sample of older adults using confirmatory factor analysis. The results of this study did not allow us to validate either the WHO model of active aging or the psychological model of active aging developed by Fernández-Ballesteros and colleagues (2013). Our findings suggest that active aging cannot be readily operationalized to guide research with older adult populations. As such, active aging might represent a policy orientation rather than a concept that can be measured empirically. This interpretation is also supported by the sheer variety of measurement models that are developed by researchers when attempting to carry out empirical research about successful and active aging (McLaughlin et al., 2010; Paul et al., 2012; Pruchno, Wilson-Genderson, & Cartwright, 2010).
Beyond rejecting the validity of the models that were specified, it is important to reflect on the value of active aging as a concept if it does not differ from existing models of successful aging. The most commonly used definition remains the one suggested by Rowe and Kahn (1997), “a low probability of disease and disease-related disability, high cognitive and physical functional capacity, and active engagement with life” (p. 433). This definition is strikingly similar to the one proposed by Fernández-Ballesteros and colleagues, with the exception of positive mood. In fact, by incorporating concerns about the material realities of older adults, the WHO attempted to move active aging away from individual determinants and to address a prominent criticism of successful aging as inaccessible and overlooking social inequalities (Martinson & Berridge, 2015). In a recent article, Martin and colleagues (2015) emphasize the need to reach consensus on a definition by reconciling different models of successful aging. We conclude that active aging is encountering a similar challenge, and add that going back and forth between theory and empirical data is useful to further our conceptual models and put them to the test.
Moreover, we wish to comment on the pitfalls of using confirmatory factor analysis to assess the validity of measurement models. It is important to specify models that are theoretically sound and to make sure that the items proposed as factors are highly correlated and indeed represent a common latent construct. Otherwise, we run the risk of estimating models that do poorly at capturing the variance of individual items (Lee et al., 2011), which is the primary purpose of the development of measurement models. Our results further confirm that capturing the social participation of older adults is particularly challenging. Previous studies also reported lower variance explained for those items (Lee et al., 2011; Paul et al., 2012), suggesting that older adults are likely to be highly involved in only one type of social activities. From a theoretical perspective, active aging may be better suited for a conceptual model with different assumptions from those of the reflective, latent measurement models commonly used in psychology. For example, a formative measurement model would imply that active aging is formed by cause indicators, with each of them representing an important component of the composite concept that cannot be interchanged without losing part of the concept. The goodness of fit of formative models however remains difficult to ascertain with existing statistical methods (Kline, 2011).
At a policy level, indexes following the WHO model active aging may also be useful to highlight what remains to be improved about the health, social participation, and social and economic security of our growing populations of older adults. A major challenge with simple indexes is to develop more sophisticated weighing of the items that are representative of their importance, as well as to agree on meaningful cutoff points that can be compared across populations. There is an inherent arbitrariness in the cutoff points used when creating binary indexes, so the state of active aging in populations can seem dire or excellent depending on the choice being made. Whether the presence of chronic illnesses precludes active aging even if symptoms are well-controlled remains to be debated given the high prevalence of chronic illnesses across elderly populations. The recently developed Active Aging Index offers a more sophisticated weighted index to rank countries with regards to active aging at the population rather than at an individual level (Zaidi et al., 2013). However, because 35% of the concept refers to labor market participation of different age groups, and another 35% targets nonpaid productive activities such as caregiving and volunteering, it remains an index that is heavily weighted towards productive activities to the detriment of other forms of social participation (Foster & Walker, 2014).
The development of a comprehensive and flexible concept of active aging that can capture its multidimensional nature endures as a very real challenge. Foster and Walker’s description of the concept summarizes the task at hand: “active ageing means creating opportunities for staying in the labor market longer, for contributing to society through unpaid work in the community as volunteers or passing on their skills to younger people, and in their extended families, and for living autonomously and in dignity for as much and as long as possible” (2014, p 4). It is worth mentioning that our measures of social participation had limitations because many domains, such as volunteering and caregiving were not assessed as part of the IMIAS study. Previous work has documented the complexity of capturing the participation among older adults, whereby as many as 13 distinct activity domains have been identified (Putnam et al., 2014). Future research should differentiate between different types of productive activities, such as work, volunteering, and caregiving, and types of leisure activities including physical, intellectual, religious, social activities. Developing a measure of the extent to which older adults feel involved in activities that are meaningful for them may also represent a better variable to capture social participation as a latent factor.
In conclusion, our work does not provide empirical support for the acceptance of either the WHO model or the psychological model of active aging in Canadian older adult populations. There remains a lot of work to be done before active aging can be operationalized and validated as a measurement model for empirical studies.
Funding
The IMIAS study was supported by a grant from the Canadian Institutes of Health Research (CIHR). The first author received a scholarship from the Fonds de recherche du Québec-Santé to complete this work.
References
- Bassett R. Bourbonnais V., & McDowell I (2007). Living long and keeping well: Elderly Canadians account for success in aging. Canadian Journal on Aging / La Revue Canadienne Du Vieillissement, 26, 113–126. doi:10.3138/cja.26.2.113 [DOI] [PubMed] [Google Scholar]
- Boudiny K. (2012). “Active ageing”: From empty rhetoric to effective policy tool. Ageing and Society, 1–22. doi:10.1017/S0144686X1200030X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A. (2005). What is successful ageing and who should define it? BMJ, 331, 1548–1551. doi:10.1136/bmj.331.7531.1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A. (2008). Enhancing later life: How older people perceive active ageing? Aging & Mental Health, 12, 293–301. doi:10.1080/13607860802120979 [DOI] [PubMed] [Google Scholar]
- Bowling A. Banister D. Sutton S. Evans O., & Windsor J (2002). A multidimensional model of the quality of life in older age. Aging & Mental Health, 6, 355–371. doi:10.1080/1360786021000006983 [DOI] [PubMed] [Google Scholar]
- Depp C. A., & Jeste D. V (2006). Definitions and predictors of successful aging: A comprehensive review of larger quantitative studies. The American Journal of Geriatric Psychiatry, 14, 6–20. doi:10.1097/01.JGP.0000192501.03069.bc [DOI] [PubMed] [Google Scholar]
- Edwards J. R., & Bagozzi R. P (2000). On the nature and direction of relationships between constructs and measures. Psychological Methods, 5, 155–174. doi:10.1037/1082-989x.5.2.155 [DOI] [PubMed] [Google Scholar]
- Fernández-Ballesteros R. (2008). Active aging: The contribution of psychology. Toronto: Hogrefe Publishing. [Google Scholar]
- Fernández-Ballesteros R. Robine J. M. Walker A., & Kalache A (2013). Active aging: A global goal. Current Gerontology and Geriatrics Research, 298012. doi:10.1155/2013/298012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster L., & Walker A (2014). Active and successful aging: A European policy perspective. The Gerontologist, 55, 83–90. doi:10.1093/geront/gnu028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freitas S. Simões M. R. Marôco J. Alves L., & Santana I (2011). Construct validity of the Montreal Cognitive Assessment (MoCA). Journal of the International Neuropsychological Society, 18, 242–250. doi:10.1017/S1355617711001573 [DOI] [PubMed] [Google Scholar]
- Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G., et al. (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49, M85–M94. doi:10.1093/geronj/49.2.m85 [DOI] [PubMed] [Google Scholar]
- Hank K. (2011). How “successful” do older Europeans age? Findings from SHARE. Journal of Gerontology: Social Sciences, 66, 230–236. doi:10.1093/geronb/gbq089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L. T., & Bentler P. M (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. doi:10.1080/10705519909540118 [Google Scholar]
- Irwin M. Artin K. H., & Oxman M. N (1999). Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Archives of Internal Medicine, 159, 1701–1704. doi:10.1001/archinte.159.15.1701 [DOI] [PubMed] [Google Scholar]
- Lee P.-L. Lan W., & Yen T.-W (2011). Aging successfully: A four-factor model. Educational Gerontology, 37, 210–227. doi:10.1080/03601277.2010.487759 [Google Scholar]
- Lupien S. J., & Wan N (2004). Successful ageing: From cell to self. Philosophical Transactions of the Royal Society B: Biological Sciences, 359, 1413–1426. doi:10.1098/rstb.2004.1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). New York: Guilford Press. [Google Scholar]
- Martin P. Kelly N. Kahana B. Kahana E. Willcox B. J. Willcox D. C., & Poon L. W (2015). Defining successful aging: A tangible or elusive concept? The Gerontologist, 55, 14–25. doi:10.1093/geront/gnu044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinson M., & Berridge C (2015). Successful aging and its discontents: A systematic review of the social gerontology literature. The Gerontologist, 55, 58–69. doi:10.1093/geront/gnu037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin S. J. Connell C. M. Heeringa S. G. Li L. W., & Roberts J. S (2010). Successful aging in the United States: Prevalence estimates from a national sample of older adults. Journal of Gerontology: Social Sciences, 65, 216–226. doi:10.1093/geronb/gbp101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasreddine Z. S., Phillips N. A., Bedirian V., Charbonneau S., Whitehead V., Collin I., Cummins J. L., Chertkow H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53, 695–699. doi:10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Paul C. Ribeiro O., & Teixeira L (2012). Active ageing: An empirical approach to the WHO model. Current Gerontology and Geriatrics Research, 2012, 1–10. doi:10.1186/1477-7525-9-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruchno R. A. Wilson-Genderson M., & Cartwright F (2010). A two-factor model of successful aging. Journals of Gerontology Series B-Psychological Sciences and Social Sciences, 65, 671–679. doi:10.1093/geronb/gbq051 [DOI] [PubMed] [Google Scholar]
- Putnam M. Morrow-Howell N. Inoue M. Greenfield J. C. Chen H., & Lee Y (2014). Suitability of public use secondary data sets to study multiple activities. The Gerontologist, 54, 818–829. doi:10.1093/geront/gnt074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Rowe J. W., & Kahn R. L (1997). Successful aging. The Gerontologist, 37, 433–440. doi:10.1093/geront/37.4.433 [DOI] [PubMed] [Google Scholar]
- Sousa A. C. Guerra R. O. Thanh Tu M. Phillips S. P. Guralnik J. M., & Zunzunegui M. V (2014). Lifecourse adversity and physical performance across countries among men and women aged 65–74. PLoS One, 9, e102299. doi:10.1371/journal.pone.0102299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger J. H. (2007). Understanding the limitations of global fit assessment in structural equation modeling. Personality and Individual Differences, 42, 893–898. doi:10.1016/j.paid.2006.09.017 [Google Scholar]
- Tate R. B. Lah L., & Cuddy T. E (2003). Definition of successful aging by elderly Canadian males: The Manitoba follow-up study. The Gerontologist, 43, 735–744. doi:10.1093/geront/43.5.735 [DOI] [PubMed] [Google Scholar]
- Tate R. B. Swift A. U., & Bayomi D. J (2013). Older men’s lay definitions of successful aging over time: The Manitoba follow-up study. International Journal of Aging & Human Development, 76, 297–322. doi:10.1093/geront/43.5.735 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2002). Active aging: A policy framework (pp. 1–60). Retrieved from http://whqlibdoc.who.int/hq/2002/who_nmh_nph_02.8.pdf [Google Scholar]
- Zaidi A., Gasior K., Hofmarcher M. M., Lelkes O., Marin B., Rodrigues R., et al. (2013). Active Ageing Index 2012: Concept, methodology and final results. Vienna, Austria: European Centre Vienna. [Google Scholar]
- Zasimova L., & Sheluntcova M (2014). Measuring active aging for government policy planning: A case of Russia. Working Paper from the National Research University Higher School of Economics (HSE). 1–30.