Abstract
Background
The impact of flooding on mental health is exacerbated due to secondary stressors, although the mechanism of action is not understood. We investigated the role of secondary stressors on psychological outcomes through analysis of data collected one-year after flooding, and effect modification by sex.
Methods
We analysed data from the English National Study on Flooding and Health collected from households flooded, disrupted and unexposed to flooding during 2013–14. Psychological outcomes were probable depression, anxiety and post-traumatic stress disorder (PTSD). Parsimonious multivariable logistic regression models were fitted to determine the effect of secondary stressors on the psychological outcomes. Sex was tested as an effect modifier using subgroup analyses.
Results
A total of 2006 people participated (55.5% women, mean age 60 years old). Participants reporting concerns about their personal health and that of their family (concerns about health) had greater odds of probable depression (adjusted odds ratio [aOR] 1.77, 95% CI 1.17–2.65) and PTSD (aOR 2.58, 95% CI 1.82–3.66). Loss of items of sentimental value was associated with probable anxiety (aOR 1.82, 95% CI 1.26–2.62). For women, the strongest associations were between concerns about health and probable PTSD (aOR 2.86, 95% CI 1.79–4.57). For men, the strongest associations were between ‘relationship problems’ and probable depression (aOR 3.25, 95% CI 1.54–6.85).
Conclusions
Concerns about health, problems with relationships and loss of sentimental items were consistently associated with poor psychological outcomes. Interventions to reduce the occurrence of these secondary stressors are needed to mitigate the impact of flooding on probable psychological morbidity.
Introduction
Flooding is the most common natural disaster and the incidence of flood-related disasters is increasing.1–3 Over the past 10 years, flood events in Europe have resulted in over 900 deaths, affected almost 4 million people and caused economic damage of US $51 billion.4 Flooding results in long lasting severe damage on infrastructure and human health.5
Increases in adverse mental health effects such as post-traumatic stress disorder (PTSD), anxiety and depression have been shown in populations affected by flooding,6–9 have been shown to manifest within weeks,10 or months11 and can last up to years afterwards.12 The English National Study on Flooding and Health has shown elevated rates of psychological morbidity among participants affected by flooding 1 year after the event.13
Previous studies have found that after flooding adults whose property had flooded had a four times higher relative risk of psychological distress.11 After the summer floods of 2007 in England, the prevalence of psychological distress, probable anxiety, probable depression and probable PTSD were found to be two to five times higher in those affected by flood water in their home.6
It has been suggested that psychological morbidity after flooding can be caused by a complex combination of primary and secondary stressors.14 Primary stressors can be identified as arising directly from the flood event such as being injured or your home being flooded. Secondary stressors are more indirect consequences of the event such as personal or financial losses, or difficulties with insurance and compensation, and may be amenable to public health action in order to reduce their impact. Studies have identified a variety of individual secondary stressors associated with adverse mental health outcomes, including: acute unemployment,15 financial loss,6,16,17 problems with insurers17 and concerns about health.6 However, systematic reviews have highlighted limitations of current research including a lack of medium to long-term follow-up and difficulties separating the effects of primary and secondary stressors.9,14
It has been postulated that the impact of disasters is worse among women and results in poorer psychological outcomes.18,19 To date no research has shown whether the impact of secondary stressors experienced after flooding on mental health is different among men and women.
This study was designed to investigate the impact of secondary stressors on psychological outcome following flooding, and the existence of any differential impact of sex as an effect modifier on psychological outcome.
Methods
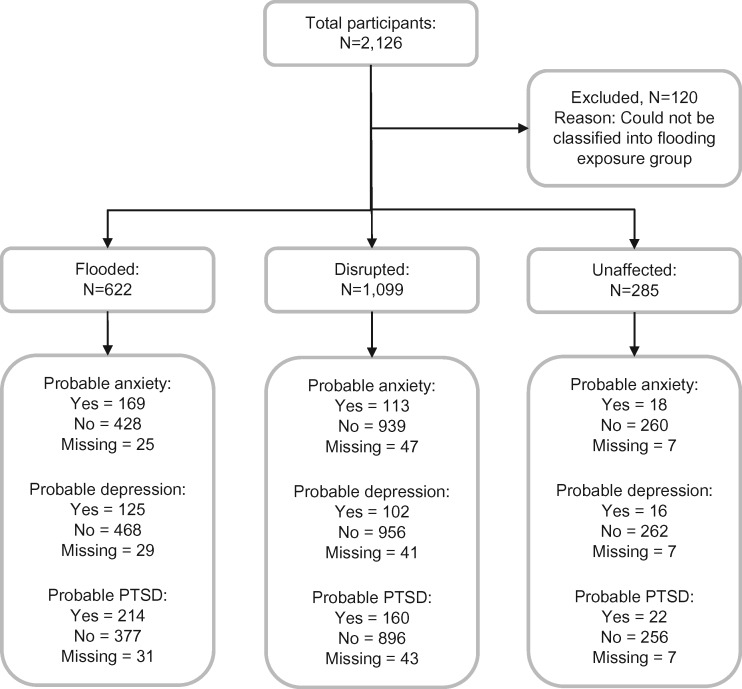
We conducted a secondary analysis of cross-sectional survey data from the English National Study on Flooding and Health. The study has been reported consistent with the STROBE checklist and a flow chart is presented.20
Study design
The study design, sampling procedure and recruitment are described in detail elsewhere.13 Participants from areas affected by the winter floods from 1st December 2013 to 31st March 2014 were recruited 1 year after flooding.
Eligible participants (individuals aged 18 and over) were recruited using a bespoke questionnaire that included questions on mental health outcomes and exposure to secondary stressors.13 Public Health England collected postcodes of flooded homes from six local authorities and used the Royal Mail Postcode Address Finder (PAF) to identify all addresses within the postcodes. Thus the sampling frame was formed of areas both affected and unaffected by the floods. Study invitation packs including the questionnaire were sent to the household addresses identified in January 2015. Two reminders were sent to non-responsive households. Completed paper questionnaires were double entered and validated prior to joining with responses submitted electronically. Participants were categorized into three exposure groups; flooded (i.e. entry of water into a liveable room of the home), disrupted by flooding but without entry of water into a liveable room, and unaffected by flooding. Mental health outcomes were measured using validated tools integrated into the questionnaire and defined as the presence or absence of probable depression, anxiety and PTSD and measured using the PHQ-2 (cut-off ≥3),21 GAD-2 (cut-off ≥3)22 and PCL-6 (cut-off ≥14)23 scales, respectively. We refer to the mental health outcomes as ‘probable’ since the tools are screening instruments and not clinically diagnostic.
Based on prior studies,6,9,14–17 18 individual secondary stressors were specified in the questionnaire, including; financial difficulties, problems with the home and self-reported concerns about their personal health and that of their family (concerns about health; full list of secondary stressors Supplementary table S1).
Data analysis
We performed descriptive statistical analyses of respondent demographics, the exposure to flooding, exposure to secondary stressors, and the mental health outcomes of probable depression, anxiety and PTSD. Participants were excluded from the analysis if they could not be categorized into one of the three overall flooding exposure groups. Participants were also excluded from a particular mental health outcome group if their outcome status could not be assessed for that outcome. Missing data were calculated across demographic characteristics, exposure to secondary stressors and mental health outcomes. The distributions of missing data across exposure and outcome variables were assessed as to whether data was missing at random and were explored for patterns of systematic bias.
Crude logistic regression models were fitted to examine associations between each individual secondary stressor and the outcomes. The secondary stressors that were found to approach statistical significance (P < 0.1) were included in multivariable analyses.
A parsimonious forward stepping approach using a likelihood ratio statistic to identify covariates that explained differences was carried out for each outcome (P < 0.05). The effect of clustering by geographical lower super output area (LSOA) was examined using a sensitivity analysis that aggregated per LSOA was carried out as with robust standard errors, adjusted for clustering. Two subgroup analyses were carried out for men and women independently to assess for differences by sex. Nine a priori potential confounding variables were identified and included in the multivariable analyses: age group, sex, local authority, ethnicity, marital status, education level, employment and deprivation score.13 These variables were specified as potential confounders through expert opinion of the national flooding study group. In addition the variable for overall flooding exposure group was included in the multivariable analyses. Missing data from any of the a priori confounding variables or from the secondary stressors were recoded as ‘missing’ to allow their inclusion in logistic regression analyses.
All statistical analyses were also performed separately for women and men. Analyses were undertaken using Stata Version 13 (StataCorp, College Station, TX, USA).
Ethical approval
This study was a secondary analysis of an existing dataset and not subject to a requirement for ethical approval. The English National Study on Flooding and Health was granted ethical approval by the Psychiatry, Nursing and Midwifery Research Ethics Subcommittee at King’s College London [Reference PNM 1314 152]. All study respondents provided written consent to participate.
Results
Descriptive analysis
Questionnaires were returned from 2014 different households, with a total of 2126 individual participants (response rate 23%). There were 120 participants (4.3%) who could not be classified into an overall flooding exposure group and were excluded from further analyses, see figure 1 for the STROBE flowchart.
Figure 1.
STROBE flowchart
The majority of participants were classified as ‘disrupted’ by flooding (54.8%), followed by ‘flooded’ (31.0%); the remaining 14.2% were assessed as ‘unaffected’ after exposure to flooding. Overall, 12.1% of all the participants were classified as having probable depression, 15.5% having probable anxiety and 19.7% having probable PTSD (Supplementary table S2). Missing values totalled less than 5% across each outcome variable.
Out of the 18 secondary stressor exposures, those most frequently experienced were: concerns about their house value (1107, 55.2%), additional financial burden (891, 44.4%), repairing their home (882, 44.0%) and finding jobs or chores around the house more difficult (858, 42.8%) (table 1). The proportion of missing values for the secondary stressors ranged from 2.7% (additional financial burden; n = 54) to 5.6% (changes in your child/children’s wellbeing or education; n = 113).
Table 1.
Depression: Final multivariable modelsa for main effects, subgroup of women, and subgroup of men
| Secondary stressor | Univariable model | Final multivariable model | Final model in women only | Final model in men only | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Probable depression | Probable depression | Probable depression | Probable depression | |||||||||
| OR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | |
| Additional financial burden | 2.98 | (2.17 to 4.09) | <0.001 | Not included in final model | Not included in final model | 0.80 | (0.39 to 1.67) | 0.555 | ||||
| Additional work pressure | 2.09 | (1.45 to 3.02) | <0.001 | Not included in final model | Not included in final model | 2.76 | (1.18 to 6.45) | 0.019 | ||||
| Loss of sentimental items | 3.41 | (2.47 to 4.70) | <0.001 | 1.67 | (1.10 to 2.55) | 0.016 | 2.20 | (1.29 to 3.77) | 0.004 | Not included in final model | ||
| Concerns about health | 3.80 | (2.72 to 5.31) | <0.001 | 1.77 | (1.15 to 2.72) | 0.009 | 2.62 | (1.48 to 4.64) | 0.001 | Not included in final model | ||
| Childrens wellbeing/education | 2.76 | (1.69 to 4.52) | <0.001 | 1.10 | (0.59 to 2.03) | 0.763 | Not included in final model | 0.26 | (0.06 to 1.16) | 0.079 | ||
| Relationship problems | 3.34 | (2.44 to 4.58) | <0.001 | 1.76 | (1.17 to 2.65) | 0.007 | Not included in final model | 3.25 | (1.54 to 6.85) | 0.002 | ||
| Disagreements with neighbours | 2.80 | (1.88 to 4.16) | <0.001 | Not included in final model | 2.17 | (1.20 to 3.93) | 0.011 | Not included in final model | ||||
| Separated from family | 2.67 | (1.79 to 3.98) | <0.001 | 1.44 | (0.87 to 2.38) | 0.151 | Not included in final model | 1.46 | (0.56 to 3.79) | 0.44 | ||
| Concerns about pets | 2.14 | (1.52 to 3.00) | <0.001 | Not included in final model | Not included in final model | 0.96 | (0.46 to 2.00) | 0.908 | ||||
Each final model also adjusted for: exposure to flooding, age, deprivation (IMD quintile), Local Authority, educational attainment, employment status, ethnicity, marital status, and pre-existing illness (not shown). Final overall main effects model also adjusted for sex.
Notes: Secondary stressors displayed are those statistically significant in increasing the model fit of the data. Those not increasing goodness of fit of the model are displayed as “Not included in final model”.
Of the 81.8% of women who experienced a secondary stressor (n = 911), 32.7% of these were also classified with any of the probable mental health outcomes. Of the 18.2% of women who did not experience any secondary stressors, 11.8% were classified with any of the probable mental health outcomes. 78.0% of men experienced a secondary stressor (n = 665), of these 26.8% were classified with any of the probable mental health outcomes. Of the 22.0% of men who did not experience any secondary stressors, 10.6% were classified with any of the probable mental health outcomes (Supplementary table S3).
For men who had probable depression, anxiety or PTSD, 65.3, 70.8 and 74.6%, respectively, had experienced concerns about their house value after the exposure to flooding. For women who had probable depression or probable PTSD, 73.6 and 75.3%, respectively, had experienced concerns about health after exposure to flooding. Of women who had probable anxiety, 73.7% had experienced concerns about their house value after the flooding.
Logistic regression modelling
Crude logistic regression showed that for each of the secondary stressors, participants who had experienced a secondary stressor had higher odds of adverse mental health outcome than participants that had not experienced the stressor. All associations between experiencing a secondary stressor and having an adverse mental health outcome were statistically significant. Concerns about health (OR 3.80, 95% CI 2.72–5.31), loss of sentimental items (OR 3.41, 95% CI 2.47–4.70) and relationship problems (OR 3.34, 95% CI 2.44–4.58) were the three largest associations with depression (table 1). Loss of sentimental items (OR 3.69, 95% CI 2.76–4.93), relationship problems (OR 3.60, 95% CI 2.71–4.80) and concerns about pets (OR 3.09, 95% CI 2.26–4.21) were the largest associations with anxiety (table 2). Concerns about health (OR 5.43, 95% CI 4.10–7.20), relationship problems (OR 4.65, 95% CI 3.57–6.06) and loss of sentimental items (OR 4.32, 95% CI 3.30–5.66) were the largest associations with PTSD (table 3).
Table 2.
Anxiety: final multivariable modelsa for main effects, subgroup of women, and subgroup of men
| Secondary stressor | Univariable model | Final multivariable model | Final model in women only | Final model in men only | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Probable anxiety | Probable anxiety | Probable anxiety | Probable anxiety | |||||||||
| OR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | |
| Loss of sentimental items | 3.69 | (2.76 to 4.93) | <0.001 | 1.82 | (1.26 to 2.62) | 0.001 | 1.77 | (1.12 to 2.81) | 0.014 | Not included in final model | ||
| Childrens wellbeing/education | 2.95 | (1.91 to 4.55) | <0.001 | 1.29 | (0.76 to 2.19) | 0.343 | Not included in final model | 0.34 | (0.09 to 1.27) | 0.108 | ||
| Relationship problems | 3.60 | (2.71 to 4.80) | <0.001 | 1.73 | (1.20 to 2.50) | 0.004 | 1.66 | (1.06 to 2.61) | 0.027 | 2.97 | (1.55 to 5.68) | 0.001 |
| Disagreements with neighbours | 2.64 | (1.82 to 3.83) | <0.001 | 1.62 | (1.04 to 2.51) | 0.032 | Not included in final model | 2.61 | (1.20 to 5.65) | 0.015 | ||
| Concerns about pets | 3.09 | (2.26 to 4.21) | <0.001 | 1.68 | (1.15 to 2.45) | 0.007 | 2.10 | (1.31 to 3.37) | 0.002 | Not included in final model | ||
Each final model also adjusted for: exposure to flooding, age, deprivation (IMD quintile), Local Authority, educational attainment, employment status, ethnicity, marital status, and pre-existing illness (not shown). Final overall main effects model also adjusted for sex.
Notes: Secondary stressors displayed are those statistically significant in increasing the model fit of the data. Those not increasing goodness of fit of the model are displayed as “Not included in final model”.
Table 3.
PTSD: final multivariable modelsa for main effects, subgroup of women, and subgroup of men
| Secondary stressor | Univariable model | Final multivariable model | Final model in women only | Final model in men only | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Probable PTSD | Probable PTSD | Probable PTSD | Probable PTSD | |||||||||
| OR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | |
| Loss of sentimental items | 4.32 | (3.30 to 5.66) | <0.001 | 1.75 | (1.24 to 2.48) | 0.002 | Not included in final model | Not included in final model | ||||
| Concerns about health | 5.43 | (4.10 to 7.20) | <0.001 | 2.58 | (1.82 to 3.66) | <0.001 | 2.86 | (1.79 to 4.57) | <0.001 | 2.58 | (1.49 to 4.47) | 0.001 |
| Relationship problems | 4.65 | (3.57 to 6.06) | <0.001 | 2.19 | (1.57 to 3.05) | <0.001 | 1.95 | (1.26 to 3.02) | 0.003 | 2.42 | (1.34 to 4.37) | 0.003 |
| Disagreements with neighbours | 3.10 | (2.19 to 4.40) | <0.001 | Not included in final model | Not included in final model | 2.30 | (1.15 to 4.57) | 0.018 | ||||
| Separated from family | 3.23 | (2.28 to 4.59) | <0.001 | Not included in final model | 2.17 | (1.27 to 3.73) | 0.005 | Not included in final model | ||||
| Concerns about pets | 3.55 | (2.67 to 4.71) | <0.001 | 1.60 | (1.13 to 2.28) | 0.008 | 1.85 | (1.16 to 2.94) | 0.01 | 1.54 | (0.86 to 2.76) | 0.144 |
Each final model also adjusted for: exposure to flooding, age, deprivation (IMD quintile), Local Authority, educational attainment, employment status, ethnicity, marital status, and pre-existing illness (not shown). Final overall main effects model also adjusted for sex.
Notes: Secondary stressors displayed are those statistically significant in increasing the model fit of the data. Those not increasing goodness of fit of the model are displayed as “Not included in final model”.
For all three mental health outcomes the final parsimonious multivariable models included loss of sentimental items and relationship problems; other secondary stressors differed between the models. For depression, after adjustment for separation from family and a child’s wellbeing, concerns about health (aOR 1.77, 95% CI 1.15–2.72), relationship problems (aOR 1.76, 95% CI 1.17–2.65) and loss of sentimental items (aOR 1.67, 95% CI 1.10–2.55) were retained in the model. For anxiety, after adjustment for a child’s wellbeing, loss of sentimental items (aOR 1.82, 95% CI 1.26–2.62), relationship problems (aOR 1.73, 95% CI 1.20–2.50), concerns about pets (aOR 1.68, 95% CI 1.15–2.45) and disagreements with neighbours (aOR 1.62, 95% CI 1.04–2.51) were retained in the model. For PTSD, loss of sentimental items (aOR 1.75, 95% CI 1.24–2.48), concerns about health (aOR 2.58, 95% CI 1.82–3.66), relationship problems (aOR 2.19, 95% CI 1.57–3.05) and concerns about pets (aOR 1.60, 95% CI 1.13–2.28) were retained in the model.
Subgroup and sensitivity analyses
For women, those who reported concerns about health had the strongest association with probable depression (aOR 2.62, 95% CI 1.48–4.64) and with probable PTSD (aOR 2.86, 95% CI 1.79–4.57) whereas those who had concerns about pets had the strongest association with probable anxiety (aOR 2.10, 95% CI 1.31–3.37); see tables 1–3.
For men, those who experienced relationship problems had the strongest association with probable depression (aOR 3.25, 95% CI 1.54–6.85) and with probable anxiety (aOR 2.97, 95% CI 1.55–5.68), whereas those who experienced concerns about health had the strongest association with probable PTSD (aOR 2.58, 95% CI 1.49–4.47); see tables 1–3.
After carrying out all sensitivity analyses on each outcome no differences were reported in the direction of the effects and only modest differences in the magnitude of the effects found.
Discussion
To our knowledge, this is the first study to explore the associations between a comprehensive list of secondary stressors and probable mental health outcomes after flooding, including subgroup analyses by sex. We found that the secondary stressors most strongly associated with each mental health outcome varied across each final parsimonious model and by sex. Participants who experienced concerns about health had the strongest associations with probable depression and PTSD, whereas those who experienced the loss of items of sentimental value had the strongest association with probable anxiety.
The strengths and limitations of the research design, the outcome measurement tools used and the generalizability of the study population of the English National Study of Flooding and Health have been discussed elsewhere.13 Strengths and limitations that are specific to this study are discussed here. The questionnaire used asked about secondary stressors experienced during or in the immediate aftermath of flooding (between December 2013 and March 2014); any experiences of these stressors after March 2014 could also partly account for variation in the mental health outcomes. Our analyses controlled for a number of a priori confounders and also adjusted for the primary stressor of being affected by flooding.13 Our model building method meant that any issues with multicollinearity from similar secondary stressors were avoided as we focused only on those that best improved model fit.
This study strengthens previous findings that both primary and secondary stressors after flooding can be associated with adverse mental health outcomes, but also that after adjustment for a primary stressor, the association remains between secondary stressors and outcomes.6,14 We found the experience of concerns about health after flooding was present in all final models, consistent with prior research showing that after adjustment for other factors, experiencing concerns about their own health related to flooding increased mental health symptoms by 2–4 times.6 Previous research on post-flooding secondary stressors has focused either on specific individual associations or stressors grouped together, rather than the production of predictive models of outcome.
We found different secondary stressors were present in our predictive models by sex. Women did not have significantly higher odds of probable depression or anxiety than men, whereas a small significant increase in PTSD was seen. This contrasts with evidence showing that women have poorer mental health outcomes post-disaster.6,16,24–26 However, it has been suggested that women subjectively experience greater threat than men during disasters18 and are more vulnerable than men to specific types of events.27 Therefore, differences may not be seen in flooding events that cause primarily property damage over threat to life.
The public health response to flooding should recognize the potential contribution of secondary stressors to adverse mental health outcomes and adapt preventative interventions accordingly. This study can be used to strengthen multi-agency emergency response and recovery plans. We advocate that these plans consider the important role of secondary stressors to mitigate their impact. For example, such plans could include providing advice about keeping sentimental items safe from floodwater by placing them high up within the household, information from animal charities and rescue shelters about what local temporary arrangements are possible for pets in the event of a flood, and community initiatives to promote social cohesiveness and support after flooding.
Commissioners and providers of health services should be aware that people reporting concerns about their health or the health of their family are more likely to suffer adverse mental health outcomes. Primary care and out of hours services should work to allay such concerns by providing information about the potential risk to health after flooding and what steps to take to protect health. Websites should be kept updated and social media could be used to promote key health messages. Such communication should be tailored to both the immediate aftermath of flooding and its long-term implications. Primary care should also be aware of the potential unrecognized burden of mental health after flooding within communities, and could provide support services such as drop in information services through GP practices and pharmacies.
The results of the predictive models constructed in this study may not be valid for areas experiencing flooding that are markedly different in age, ethnic, or deprivation structures. Our findings require validation through further studies, and additional work is needed to develop predictive models for potentially numerous subgroups in the aftermath of future flooding events. Future work should include studying the impact of interventions targeted to mitigate secondary stressors on the risk of probable mental health outcomes. As the English National Study of Flooding and Health continues, we advocate further analysis of the associations between secondary stressors and probable mental health outcomes as further time elapses post-flooding.
Conclusion
This study has used people’s experiences of secondary stressors after exposure to flooding to produce predictive models for adverse mental health outcomes. We have shown that different secondary stressors are associated with probable depression, anxiety and PTSD in the aftermath of flooding. We highlight two secondary stressors (reporting concerns about health and the loss of items of sentimental value) that should be the focus of preventative action in order to mitigate their effects in future flooding events. Our results also demonstrate the variation in experience of secondary stressors by sex; public health policy makers should ensure emergency response plans for flooding recognize such differences. Clinical services should promote key messages relating to health in the aftermath of flooding.
Funding
Funding for this study was provided by Public Health England. We acknowledge the support of the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London (BC).
Supplementary data
Supplementary data are available at EURPUB online.
Conflicts of interest: None declared.
Key points
We present the first study to explore the association between secondary stressors and probable mental health outcomes after flooding, including subgroup analyses by sex.
We show that participants reporting concerns about their personal health and that of their family had greater odds of depression and PTSD.
For women, the strongest associations were between concerns about health and probable PTSD. For men, the strongest associations were between ‘relationship problems’ and probable depression.
We advocate that preventive interventions should be adapted to mitigate the impact of secondary stressors. Communications tailored to the immediate aftermath and longer-term implications after flooding could promote key health messages.
Primary care should be aware of a potentially unrecognized burden of mental health after flooding and could provide support services.
Supplementary Material
Acknowledgements
We acknowledge respondents to the England National Study on Flooding and Health for providing data used in our study. We thank members of the England National Study on Flooding and Health for supporting this study and providing advice. The members of the English National Study on Flooding and Health Study Group are Thomas David Waite, Charles R. Beck, Angie Bone, Richard Amlôt, Sari Kovats, Ben Armstrong, Giovanni Leonardi, G James Rubin, Isabel Oliver. This study was partly supported by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Evaluation of Interventions at the University of Bristol in partnership with Public Health England (PHE), the NIHR HPRU Emergency Preparedness and Response at King’s College London in partnership with PHE and the NIHR HPRU in Environmental Change and Health at the London School of Hygiene and Tropical Medicine in partnership with PHE. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, the Department of Health or PHE.
References
- 1.Centre for Research on the Epidemiology of Disasters (CRED) and United Nations Office for Disasters Risk Reduction (UNISDR). The Human Cost of Weather Related Disasters 1995-2015;2015.
- 2. Smith KR, Woodward A, Campbell-Lendrum D, Chadee D, et al. Human health: impacts, adaptation, and co-benefits In: Climate Change 2014: Impacts, Adaptation, and Vulnerability Part A: Global and Sectoral Aspects Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press, 2014;709–54. [Google Scholar]
- 3. Kovats RS, Valentini R, Bouwer LM, et al. Europe In: Climate Change 2014: Impacts, Adaptation, and Vulnerability Part B: Regional Aspects Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press, 2014;1267–326. [Google Scholar]
- 4. EM-DAT. Disaster Profiles [Internet]. The International Disaster Database. 2016http://www.emdat.be/database (21 September 2016, date last acessed).
- 5. Menne B, Murray V Floods in the WHO European region: health effects and their prevention. Copenhagen; 2013. http://www.euro.who.int/en/health-topics/environment-and-health/Climate-change/publications/2013/floods-in-the-who-european-region-health-effects-and-their-prevention.
- 6. Paranjothy S, Gallacher J, Amlot R, et al. Psychosocial impact of the summer 2007 floods in England. BMC Public Health 2011;11:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lowe D, Ebi KL, Forsberg B. Factors increasing vulnerability to health effects before, during and after floods. Int J Environ Res Public Health 2013;10:7015–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stanke C, Murray V, Amlôt R, et al. The effects of flooding on mental health: outcomes and recommendations from a review of the literature. PLoS Curr 2012;4:e4f9f1fa9c3cae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fernandez A, Black J, Jones M, et al. Flooding and mental health: a systematic mapping review. PLoS One 2015;10:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alderman K, Turner LR, Tong S. Floods and human health: a systematic review. Environ Int 2012;47:37–47. [DOI] [PubMed] [Google Scholar]
- 11. Reacher M, McKenzie K, Lane C, et al. Health impacts of flooding in Lewes: a comparison of reported gastrointestinal and other illness and mental health in flooded and non-flooded households. Commun Dis Public Health 2004;7:39–46. [PubMed] [Google Scholar]
- 12. Tapsell SM, Tunstall SM. “I wish I’d never heard of Banbury”: the relationship between “place” and the health impacts from flooding. Heal Place 2008;14:133–54. [DOI] [PubMed] [Google Scholar]
- 13. Waite TD, Chaintarli K, Beck CR, et al. The English national cohort study of flooding and health: cross-sectional analysis of mental health outcomes at year one. BMC Public Health 2017;17:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lock S, Rubin GJ, Murray V, et al. Secondary stressors and extreme events and disasters: a systematic review of primary research from 2010-2011. PLOS Currents Disasters. 2012. Edition 1. doi: 10.1371/currents.dis.a9b76fed1b2dd5c5bfcfc13c87a2f24f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Joseph NT, Matthews KA, Myers HF. Conceptualizing health consequences of Hurricane Katrina from the perspective of socioeconomic status decline. Heal Psychol 2014;33:139–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Galea S, Brewin CR, Gruber M, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry 2007;64:1427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tunstall S, Tapsell S, Green C, et al. The health effects of flooding: Social research results from England and Wales. J Water Health 2006;4:365–80. [DOI] [PubMed] [Google Scholar]
- 18. Bonanno GA, Brewin CR, Kaniasty K, Greca AML. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychol Sci Public Interest 2010;11:1–49. [DOI] [PubMed] [Google Scholar]
- 19. Norris FH, Perilla JL, Ibañez GE, Murphy AD. Sex differences in symptoms of posttraumatic stress: does culture play a role? J Trauma Stress 2001;14:7–28. [Google Scholar]
- 20. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:1623–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res 2005;58:163–71. [DOI] [PubMed] [Google Scholar]
- 22. Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50:613–21. [DOI] [PubMed] [Google Scholar]
- 23. Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther 2005;43:585–94. [DOI] [PubMed] [Google Scholar]
- 24. DeSalvo KB, Hyre AD, Ompad DC, et al. Symptoms of posttraumatic stress disorder in a New Orleans workforce following Hurricane Katrina. J Urban Heal 2007;84:142–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Garfin DR, Silver RC, Ugalde FJ, et al. Exposure to rapid succession disasters: a study of residents at the epicenter of the Chilean Bío Bío earthquake. J Abnorm Psychol 2014;123:545–56. [DOI] [PubMed] [Google Scholar]
- 26. Frankenberg E, Friedman J, Gillespie T, et al. Mental health in Sumatra after the tsunami. Am J Public Health 2008;98:1671–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Phifer JF. Psychological distress and somatic symptoms after natural disaster: differential vulnerability among older adults. Psychol. Aging 1990;5:412–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.