Abstract
Background
Little is known about the clinical care experiences of HIV-infected persons in St. Petersburg who have experience with incarceration. To address this question, we conducted a capture-recapture study to identify individuals who had been diagnosed with HIV infection while incarcerated and who subsequently presented for medical care in St. Petersburg, Russia following release from prison.
Methods
We matched 292 HIV-positive prisoners tested by the prison system in 2010 to the medical records at the St. Petersburg AIDS Center in the following 4 years.
Results
The data analysis shows that as many as half of HIV+ prisoners fail to seek treatment in the community upon release. Of those who had sought care post-release, only 36% were receiving HAART. Of the 109 individuals for whom tuberculosis testing was indicated post-release, 36.7% were found to be reactive.
Conclusion
Despite the limitations of the data, this study is the first of its kind to review records documenting HIV care among prisoners in Russia post-incarceration. In addition to providing important descriptive information about this marginalized population, the findings from this study highlight areas where HIV control efforts could be improved in order to address the HIV epidemic in the Russian Federation.
Introduction
With a population incarceration rate of 607 per 100 000 persons, Russia incarcerates more individuals than every other country except the USA.1 Russia’s expansive penitentiary system (containing prisons and ‘correctional colonies’) has medical facilities at each institution, many of which are in poor condition.2 According to the Administration of Federal Penitentiary Services of Russia (UFSIN), in January 2015, these facilities housed 671 700 individuals, the vast majority of whom—like others whose health status reflects the consequences of social marginalization—are suffering health problems.3
The Russian HIV epidemic was initially driven by injection drug use (IDU); in 2014, people who inject drugs (PWID) comprised 57.3% of registered HIV cases and 72.4% of cases with an attributable transmission route.4 Surveillance data indicate great regional differences in HIV prevalence among PWID, ranging from 3 to 64%.5–7
Depending on the source of the reports, official data regarding the numbers of incarcerated persons with HIV or other health problems are widely divergent, ranging from a low of 4% of prisoners infected with tuberculosis (TB) and 9% of prisoners infected with HIV in 20143 to a high estimate that 90% of prisoners in 2010 had TB, HIV, or hepatitis, either as a standalone diagnosis or in coinfection.4 By 2014, it was known that there were 59 532 HIV+ inmates,3 representing ∼6.2% of the 907 607 Russians known to be HIV+.8 Although most HIV+ inmates acquired their infection before incarceration,9 as many as 90% may have learned of their status when they were HIV tested upon entry to prison.10 Some estimates indicate that as many as one in four incarcerated persons in Leningradskaya Oblast is HIV+9; more recent data show that, of 1000 inmates HIV tested in the first half of 2015, 60.2% were infected.11 Interestingly, reports from the end of 2015 indicate only 132.4 cases per 1000 tested.12
Given reporting discrepancies, it is virtually impossible to estimate the actual disease burden in Russian prisons. However, it is clear that there are insufficient resources to provide testing and medical care for these individuals. Although inmates represent a sizeable percentage of the nation’s HIV+ individuals, only 1% of the Federal AIDS budget is dedicated to care for inmates2; the Prosecutor General’s Office estimates that only 24% of the funds necessary are actually available.4
HIV testing is mandatory upon entry into Russian correctional facilities for those whose HIV status is unknown as a result of prior testing within the penal system. Thus, incarceration offers an opportunity to identify and provide medical care to HIV+ individuals who may not normally engage with community-based providers. Russian federal law guarantees that individuals receiving HAART in specialized federal medical institutions (including prisons) are guaranteed HAART access for the entire period of follow-up (including post-release for inmates).13 Ideally, the clinical benefit achieved during incarceration could be maintained through appropriate linkage to community-based care and adherence to treatment.14,15 There are currently no published data on the number of formerly incarcerated HIV+ persons who have successfully continued treatment upon release, nor are there data on HAART adherence in former prisoners in any locality in Russia. Treatment failure and suboptimal adherence post-release compromise individual health outcomes and may result in development of drug resistance (thereby limiting treatment options) and continued sexual, parenteral, and perinatal transmission. Widespread non-adherence may contribute to spread of drug-resistant HIV and maintenance of high community viral load. Therefore, estimating the rate at which HIV+ persons receiving HAART in prison successfully transition to community-based care would serve as an important first step in determining the nature and scope of interventions to facilitate continuity of care for HIV+ prisoners.
St. Petersburg is an appropriate venue to explore these issues, as it has over 50 000 confirmed HIV diagnoses,16 the majority of which are attributable to IDU.17 Prevalence among samples of PWID has increased from 11% in 200018 to 59% in 2010.19 A recent cross-sectional survey conducted in 2013–14 found that 33.7% of the 811 PWID reported incarceration histories.20 Since inmates are given a month’s supply of HAART upon release from [prison, it is imperative that they go to the St. Petersburg AIDS Center, the city’s only comprehensive HIV surveillance and care facility, within 1 month to avoid treatment interruption. Initiation and maintenance of care is critical given that this population is extremely marginalized and may not be linked to medical or other health services outside of the correctional system.
Ideally, understanding incarceration experience and linkage to care post-release would involve the examination of medical records from both the prison system and from community-based sources of HIV care. Although we were not permitted to access prison medical records, we were granted access to the medical records of a subset of the AIDS Center patient population who were tested and diagnosed with HIV in 2010 during their incarceration. This exploratory study identified patients with incarceration histories and, through retrospective review of medical charts, determined: (i) rates of successful linkage to care at the AIDS Center post-release, (ii) receipt of HAART and (iii) presence 7of HIV-related comorbid conditions.
Methods
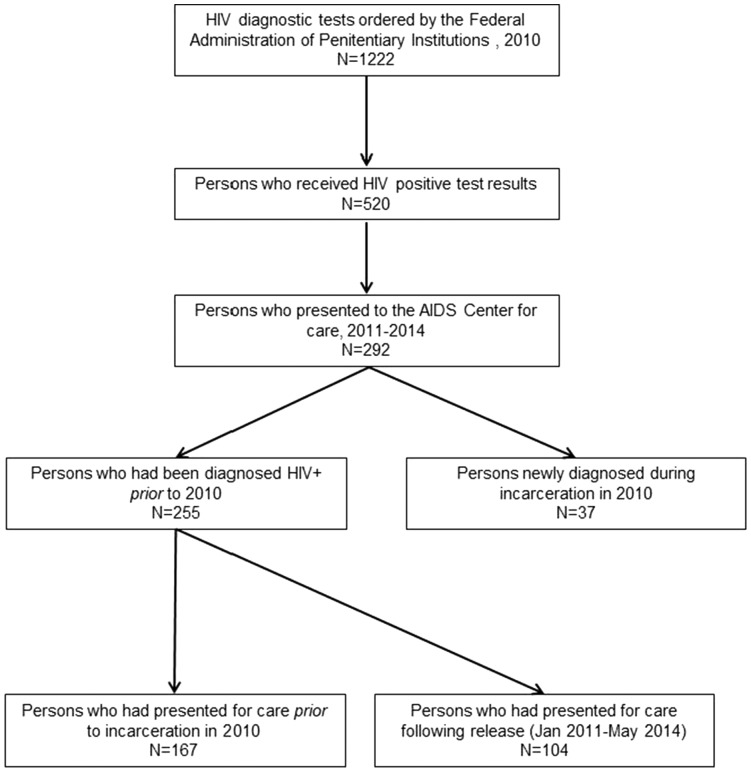
We employed a capture-recapture approach using archived medical records at the St. Petersburg AIDS Center (figure 1). Two specific medical records databases were used, the first being the record of HIV testing conducted in 2010 by the AIDS Center for UFSIN. These records provided data for the development of a roster of HIV+ St. Petersburg residents entering correctional facilities during that year who would be eligible for HIV care both in prison and at the AIDS Center post-release. These individuals represent the ‘capture’ phase of patient identification.
Figure 1.
Sampling methodology for identification of HIV-infected persons with histories of incarceration
The ‘recapture’ stage was 2-fold. First, we identified patients who presented to the AIDS Center prior to incarceration in 2010, i.e. they were already diagnosed HIV+ but were retested by UFSIN. This was done by matching the names on the prisoner roster described above records listing patients who were registered at/had presented to the AIDS Center at least once for care prior to 2010. Second, we identified patients who had been newly diagnosed while incarcerated in 2010 and who presented to the AIDS Center post-release. This was done by matching the names from the prisoner roster to a database of individuals who had received ambulatory and/or inpatient services at the AIDS Center at any time in the follow-up period from January 2011 to May 2014 (inclusive). This second set of patients was defined as having received clinical care post-release. Data from both sets of patients—those diagnosed pre-2010 and those diagnosed in 2010—were used to examine utilization of care post-release.
Data abstraction from patients’ medical charts was conducted to identify treatment course and comorbidities. Data collected included date of initial HIV diagnosis, HAART treatment received during this time period, medication adherence information, hepatitis C virus and TB status, and substance use history. The members of the research team from the AIDS Center completed the chart review and data abstraction, stripping the dataset of all personal identifiers. Analyses were limited to descriptive statistics due to the small sample size. By Russian research ethics standards, this research using de-identified data was considered exempt from review.
Results
During 2010, there were 7088 HIV+ individuals incarcerated in St. Petersburg. In that same year, UFSIN ordered HIV diagnostic testing of 1222 individuals who were entering the correctional facility. These tests were conducted by the AIDS Center. Of these 1222 individuals tested in 2010, 520 (42.5%) were HIV+.
Review of AIDS Center records identified 292 of the 520 individuals tested in 2010 who were registered at AIDS Center. Available demographic characteristics are presented in table 1. The 228 who were not registered may represent individuals who were still incarcerated or had been released from prison and, for whatever reasons, chose not to seek care at the AIDS Center. Per the residence information noted in the medical records, 96.2% of the 292 individuals lived in St. Petersburg. Three individuals indicated that they were homeless, six lived in the adjacent Leningrad Oblast, and two lived outside of the St. Petersburg region.
Table 1.
Demographic characteristics of registered patients at the AIDS Centre, St. Petersburg, with histories of incarceration (n = 292)
| Variable | n (%) |
|---|---|
| Location of residence | |
| St. Petersburg City | 281 (96.2%) |
| Outside St. Petersburg | 2 (0.7%) |
| Leningrad Oblast | 6 (2.3%) |
| Homeless | 3 (1.0%) |
| Time of initial HIV diagnosis | |
| Prior to incarceration | 255 (87.3%) |
| At time of incarceration | 37 (12.7%) |
| Disease stage at time of presentation for care at the AIDS Center (as indicated in medical chart) | |
| Primary infection (Stage 1) | 73 (25.0%) |
| Clinically asymptomatic or minimal symptoms (Stages 2 and 3) | 167 (57.2%) |
| Symptomatic (Stage 4) | 33 (11.3%) |
| No data in chart | 19 (6.5%) |
| Clinical diagnosis of AIDS | |
| No | 247 (84.6%) |
| Yes | 45 (15.4%) |
Of the 292 patients registered at the AIDS Center, 37 (12.7%) were first diagnosed HIV+ during their incarceration in 2010. The remaining 255 (87.3%) had been diagnosed HIV+ prior to incarceration but were retested by UFSIN in 2010.
Using WHO criteria,21 disease staging of the 292 patients within the prison system revealed 73 individuals (25%) with Stage 1 (primary) HIV infection, 167 (57.2%) who had either Stage 2 (clinically asymptomatic) or Stage 3 (clinically symptomatic) disease, and 33.(11.3%) who had Stage 4 disease. Nineteen individuals (6.5%) had no disease staging information in their medical record. Forty-five (15.4%) had clinical AIDS diagnoses.
Care utilization characteristics are presented in table 2. Of the 255 individuals registered at the AIDS Center prior to 2010, 167 (65.4%) completed an initial clinical visit at the AIDS Center prior to incarceration. Of these, 104 (62.3%) sought care sometime within the follow-up period. The remaining 63 (37.7%) had not presented for care, indicating that they were lost to follow up or still incarcerated.
Table 2.
Care utilization among HIV-positive patients with histories of incarceration
| Variable | n (%) |
|---|---|
| Among those who were registered at the AIDS Center prior to incarceration (n = 255) | |
| Presented for care at the AIDS Center prior to incarceration | |
| No | 88 (34.5%) |
| Yes | 167 (65.4%) |
| Sought care in the period between January 2011 and May 2014 | |
| No | 63 (37.7%) |
| Yes | 104 (62.3%) |
| Among those who were ‘not’ registered at the AIDS Center prior to incarceration (n = 125) | |
| Presented for care at the AIDS Center following release | |
| No | 23 (18.4%) |
| Yes | 102 (81.6%) |
| Among total sample (n = 292) | |
| Received care at AIDS Center between January 2011 and May 2014 | |
| No | 86 (29.5%) |
| Yes | 206 (70.5%) |
| Receiving HAART | |
| No | 185 (63.4%) |
| Yes | 107 (36.6%) |
Of the 125 HIV+ individuals not registered at the AIDS Center prior to 2010, 102 had a clinical care visit within the follow-up period. Thus, a total of 206 (70.5%) of the 292 individuals received at least some clinical care in 2011–14. However, treatment information from medical charts indicated that that only 107 (36.6% of 292) were receiving HAART. Thirty-five (12%) had died by May 2014; cause of death was not listed in their medical charts.
TB diagnostic tests were performed for 109 of the 292 patients post-release. Of these 109, 40 (36.7%) were positive.
Patients’ substance use histories were not uniformly recorded in medical charts. Of 292 individual charts, only 136 (46.6%) had any information detailing a patient history of substance use, with data on specific drugs only available for a subset of individuals. Opioids (n = 49) and heroin (n = 41) were the most frequently mentioned, with 4 individuals indicating use of methadone, which can only be obtained illicitly. Five individuals indicated ephedrine or other stimulant use. Although almost all opioids and stimulants are administered intravenously, only 18 individuals had records indicating intravenous injection. Nine individuals reported combined alcohol and opiate abuse, while six reported simultaneous consumption of several drugs.
Discussion
This study is one of the first to examine the clinical histories of HIV+ persons in St. Petersburg, Russia, with histories of incarceration. These descriptive data provide a snapshot of the limitations of the clinical data collection system as well as useful information on incarcerated individuals’ utilization of community-based clinical care and HAART access following release from prison.
There are several data limitations that must be addressed that are indicative of the problems faced in attempting to understand and improve the systems for transitioning patients from prison to HIV care upon release and the overall system of patient record keeping. The first pertains to difficulties in accessing data on HIV+ individuals in the correctional system. Because we could not access prison medical records, we could not examine the issue of incarceration history and linkage to care among the larger population of 7088 HIV+ persons incarcerated in 2010. Additionally, because HIV testing is mandated upon entry into the penal system and medical records of incarcerated individuals are not transferred from non-penal medical services, all newly incarcerated individuals are HIV tested upon arrival. Since we did have access to a list of persons diagnosed HIV+ during their incarceration in 2010, we cross-linked the list with the AIDS Center records to find the 292 individuals who ultimately became our sample. Future efforts examining this issue will require closer collaboration with the correctional system so that medical records for incarcerated persons can be made available, even in de-identified form to ensure confidentiality.
The second limitation was the lack of access to other forms of data relevant to our inmate sample. We did not have access to death data so it is possible that some of the 228 individuals who were identified as HIV+ in 2010 but who did not present to the AIDS Center had died and, therefore, would not have medical records post-2010. Similarly, we did not have access to information about inmates’ release dates, so we cannot be certain that all of those tested and diagnosed in 2010 had been released and, thus, were able to present for community-based care. Our findings represent estimates of those who successfully linked to care following release from incarceration.
Additionally, there were difficulties in identifying from AIDS Center medical records which patients had incarceration histories because such information was infrequently noted in patients’ medical charts, precluding a more straightforward strategy of examining all patient records and selecting those whose charts indicated incarceration histories. In order to address this, we employed the capture-recapture method described earlier. It is very likely that the actual number of AIDS Center patients with incarceration histories is far greater than what we found. More research, better record keeping, and better integration of community and correctional medical records systems are needed to obtain accurate estimates of the size of the HIV+ population in St. Petersburg’s correctional colonies and their linkage to care post-release.
On this last point, we have no denominator for the prisoners in our set of 292 individuals who were released in the 3-year follow-up period, making it impossible to determine the proportion of patients who successfully linked to care. Additionally, we do not know how many of those individuals who did not receive HAART after presenting at the AIDS Center would have been eligible under the treatment initiation guidelines that existed at that time (CD4+ ≤350 per mm).22 Current AIDS Center guidelines would recommend that all of these individuals initiate HAART.
Another limitation pertains to the availability and quality of medical chart data regarding substance use and comorbidities. It is probable that the majority of the individuals identified in this study had histories of substance use, as the number of charts indicating substance use experience is surprisingly low compared with other data about substance use histories (particularly injection) in prison populations.7,20 This may reflect inadequate assessments of patients’ health and risk behavior histories or patients’ underreporting of substance use and other risk behaviors for fear of stigma, judgment, discrimination, or denial of HAART. In our case, the available data were not sufficient to provide comprehensive information about individuals’ substance use behavior other than a snapshot of individuals’ drugs of choice.
Similarly, there was a surprising lack of information in the medical charts about disease comorbidities. The lack of consistent information about TB testing could reflect poor data collection by health care providers (e.g. not asking about prior TB and/or hepatitis screenings, infections and treatment) when taking patients’ medical histories. However, the lack of data could also indicate that the 183 individuals for whom TB tests weren’t ordered had already received a TB diagnosis or had tested negative. This information is relevant to the provision of comprehensive clinical care but was not noted in the charts. This absence of data may reflect the siloed medical care delivery systems that are common in post-Soviet Russia and demonstrates the need for integrated clinical care across medical specialties and disciplines. Additionally, greater efforts are needed among health care providers to standardize the process of taking patients’ medical histories so care can be better integrated. This would facilitate future efforts to examine incidence and prevalence of HIV-associated comorbidities among larger cohorts of individuals receiving care.
Despite these limitations, there are several strengths to this study, the most notable being that we provide information that can be used as a first step in understanding the gap between the need for and access to HIV care among formerly incarcerated HIV+ persons in St. Petersburg. With substance use as a core driver of HIV and incarceration in Russia, it is disconcerting that so little is known about the HIV care trajectories of people with incarceration histories. Our finding that only a third of the patients were receiving HAART is troubling and may be attributable to a number of factors, including not meeting treatment eligibility requirements for that time or regulations discouraging HAART initiation among active PWID who had not previously completed a 6-month abstinence from substance use. Regardless of whether or not these restrictions were justified, they did affect who had HAART access. Our findings reflect what is happening more broadly in the Russian context. Leaders at the Federal AIDS Center have stated that, with rising HIV rates in the country, at least 70% of patients need to be on HAART to slow disease spread. As of 2015, only 157 000 out of 516 000 registered patients in Russia are treated regularly, which is barely over 30% of those infected.23 Recent reports of additional cuts to the HIV medicines budget by the Russian Ministry of Health will likely result in further limitations to HAART access.24
A second strength of this study is that it illuminates the urgent need for more effective systems to link formerly incarcerated individuals to community-based health care and services. This is critical given that many individuals have multiple incarcerations over a life time, risking repeated disruptions in clinical care. The low quality of medical care provision for HIV+ people, lack of appropriate nutrition, and absence of other crucial conditions for maintaining health are of great concern.25 According to international guidelines, the right to medical care in prison includes HAART provision in the context of comprehensive HIV clinical care26 as well as the provision of care consistent with the standards of care available in the community.27 With already low HAART access and further constraints to care potentially occurring because of governmental budget cuts, having complementary community-based services that can help HIV+ persons maintain their health will be critical to efforts to contain the HIV epidemic in Russia. Programmes providing community-based support and care are needed, as well as programmes to ensure linkage to and retention in such services for incarcerated persons transitioning back to communities post-release. Further research and intervention efforts are warranted, as untreated or undertreated HIV infection is deleterious both for infected individuals and for achieving and maintaining low community viral load.
Acknowledgements
The authors would like to thank the medical records personnel at the St. Petersburg AIDS Center for their assistance in locating and abstracting the data from the medical records included in this study.
Funding
This work was supported by a grant from the National Institute on Drug Abuse (R01DA031649; PI: M.S. Ruiz) and an AIDS International Training and Research Programme award from Fogarty International Center (5D43TW001028; PI: R. Heimer).
Conflicts of interest: None declared.
Key points
This study is one of the first to examine the clinical histories of HIV-infected persons in St. Petersburg, Russia, who have histories of incarceration.
Of these 1222 individuals tested for HIV in prison in 2010, 520 (42.5%) received positive test results. Only a third of HIV-infected patients were receiving HAART following release from incarceration. Of the individuals examined for tuberculosis infection post-release, 36.7% were found to be positive.
These data provide useful information on incarcerated individuals’ utilization of community-based clinical care and HAART access following release from prison, and highlight the urgent need for more effective systems to link formerly incarcerated individuals to community-based health care and social services.
References
- 1. Hartney C. Fact Sheet: US rates of incarceration: a global perspective. National Council of Crime and Delinquency, November 2006. Available at: http://www.nccd-crc.org/nccd/pubs/2006nov_factsheet_incarceration.pdf (28 November 2015, date last accessed).
- 2. Parfitt T. Crime and unjust punishment in Russia. Lancet 2010;376:1815–6. [DOI] [PubMed] [Google Scholar]
- 3. Federal Penitentiary Services of Russia (UFSIN). Report on Main Domains and Results of Activities of Federal Penitentiary Services of Russia (UFSIN), 2015. Available at: http://fsin.su/structure/inspector/iao/Doklad/DROND%202015-2017.pdf (3 February 2016, date last accessed).
- 4.The Prosecutor General’s Office of the Russian Federation. Prosecutor General's Office checked the fulfillment of requirements of the legislation on ensuring the rights of prisoners and persons in custody, to qualified medical care. 11 August 2010. Available at: http://www.genproc.gov.ru/smi/news/genproc/news-58618/ (31 July 2016, date last accessed).
- 5. Niccolai LM, Toussova OV, Verevochkin SV, et al. High HIV prevalence, suboptimal HIV testing, and low knowledge of HIV-positive serostatus among injection drug users in St. Petersburg, Russia. AIDS Behav 2010;14:932–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rhodes T, Lowndes C, Judd A, et al. Explosive spread and high prevalence of HIV infection among injecting drug users in Togliatti City, Russia. AIDS 2002;16:F25–31. [DOI] [PubMed] [Google Scholar]
- 7. Rhodes T, Platt L, Maximova S, et al. Prevalence of HIV, hepatitis C and syphilis among injecting drug users in Russia: a multi-city study. Addiction 2006;101:252–66. [DOI] [PubMed] [Google Scholar]
- 8. Pokrovskiy VV. Fact sheet: HIV-infection in the Russian Federation as of December 31, 2014. Federal Scientific-Methodological Center for Prevention and Combating AIDS, 12 March 2015. Available at: http://hivrussia.org/files/spravkaHIV2014.pdf (18 July 2015, date last accessed).
- 9.Federal Service for Surveillance of Consumer Rights Protection and Human Well-Being of the Russian Federation and UNAIDS. Country Progress Report of the Russian Federation on the Implementation of the Declaration of Commitment on HIV/AIDS. Reporting period: January 2008 – December 2009. Moscow: Federal Service for Surveillance of Consumer Rights Protection and Human Well-Being of the Russian Federation and UNAIDS, 2010. Available at: http://www.fzr-eng.ru/uploads/national_report_russia_eng_2008-2009_to_cd.pdf (22 November 2015, date last accessed no longer available online).
- 10. Mahova L. Medical Department of the Central Office of Federal Penitentiary Service for St. Petersburg and Leningradskaya Region (FSIN). Data presented at the official meeting of the Coordination Council on HIV/AIDS under the St. Petersburg Government on November 12, 2008. Published November 14, 2008. http://www.epidemiolog.ru/news/detail.php?ELEMENT_ID=1685 (22 November 2015, date last accessed).
- 11.St. Petersburg AIDS Center. Informational Bulletin of HIV Infection in St. Petersburg as of July 1, 2015. www.hiv-spb.ru/assets/docs/ib/Informacionnyj%20bjulleten'%20CSPID%20za%206%20mesjacev%202015%20goda.pdf (14 October 2016, date last accessed).
- 12.St. Petersburg AIDS Center. Informational Bulletin of HIV Infection in St. Petersburg as of 1 January 2016. Available at: www.hiv-spb.ru/assets/docs/ib/Informacionnyj%20bjulleten%27%20CSPID%20za%202015%20god.pdf (14 October 2016, date last accessed).
- 13.Russian Federation Government Resolution dated December 27, 2004 No 856: “On Approval of Rules of providing free medicines for the treatment of HIV infection in an outpatient setting in the federal specialized medical institutions”, taken in accordance with Article 4 of the Federal Law “On Prevention of Spread of the disease caused by the human immunodeficiency virus (HIV)” (Collection of legislation of the Russian Federation, 1995, number 14, st.1212, 2004, no. 35, st.3607). Available at: http://www.garant.ru/hotlaw/federal/113134/ (13 July 2016, date last accessed).
- 14. Devereux PG, Whitley R, Ragavan A. Discharge planning for inmates with HIV/AIDS: Can it help increase adherence to medical treatment and lower recidivism? Corrections Today 2002;127–9. [Google Scholar]
- 15. Althoff AL, Zelenev A, Meyer JP, et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behavior 2013;17(Suppl 2):S156–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Panteleeva OV, Vinogradova TN HIV-Monitoring at Risk-Groups in St. Petersburg. St. Petersburg AIDS Center. Suzdal, Russia: Russian National AIDS Conference, 13 March 2014.
- 17. Pokrovsky VV, Ladnaya NN, Sokolova EV, Buravcova EV HIV-infection. Federal AIDS Center, Bulletin #35, Moscow, 2011. Available at: http://hivrussia.org/files/bul_35.pdf (4 April 2015, date last accessed).
- 18. Abdala N, Carney JM, Durante AJ, et al. Estimating the prevalence of syringe-borne and sexually transmitted diseases among injection drug users in St. Petersburg, Russia. Intl J STD AIDS 2003; 14:697–703. [DOI] [PubMed] [Google Scholar]
- 19. Eritsyan K, Heimer R, Barbour R, et al. Individual-, network-, and city-level factors associated with HIV prevalence among people who inject drugs in eight Russian cities. BMJ Open 2013;3:e002645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cepeda JA, Niccolai LM, Lyubimova A, et al. High-risk behaviors after incarceration among people who inject drugs in St. Petersburg, Russia. Drug Alcohol Depend 2014;147:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization. WHO Case Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIV-Related Disease in Adults and Children; 2007. Available at: http://www.who.int/hiv/pub/vct/hivstaging/en/. (21 June 2017, date last accessed).
- 22. Bobrik A, Danishevski K, Eroshina K, McKee M. Prison health in Russia: the larger picture. J Public Health Policy 2005;26:30–59. [DOI] [PubMed] [Google Scholar]
- 23. Rozhdestvensky I. Awash in AIDS How Russia’s economic crisis is skyrocketing HIV infections again. Meduza 15 September 2015. Available at: https://meduza.io/en/feature/2015/09/15/awash-in-aids#/en/feature/2015/09/15/awash-in-aids (14 July 2016, date last accessed).
- 24. Mishina V, Manuylova A AIDS is challenged for budget resistance. Funding for HAART is abridged. 12 July 2016. Available at: http://www.kommersant.ru/doc/3036186 (16 July 2016, date last accessed).
- 25. Human Rights in Russia. В связи с гибелью ВИЧ-позитивных заключенных правозащитники просят генпрокурора провести проверку УФСИН по Карелии. Human Rights in Russia website (Права человека в России), 5 December 2010. http://www.hro.org/node/8161 (4 April 2015, date last accesed).
- 26. WHO/UNODC/UNAIDS. Interventions to Address HIV in Prisons: HIV Care, Treatment and Support. Geneva: World Health Organization, 2007. [Google Scholar]
- 27. Jürgens R, Betteridge G. Prisoners who inject drugs: public health and human rights imperatives. Health Hum Rights 2005;8:46–74. [PubMed] [Google Scholar]