Abstract
Purpose of the Study
The study identifies differences in age-expectations between older adults from Korean, Chinese, Latino, and African American backgrounds living in the United States.
Design and Methods
This study uses baseline demographic, age-expectation, social, and health data from 229 racial/ethnic minority seniors in a stroke-prevention intervention trial. Unadjusted regression models and pair-wise comparisons tested for racial/ethnic differences in age-expectations, overall, and across domain subscales (e.g., physical-health expectations). Adjusted regression models tested whether age-expectations differed across racial/ethnic groups after controlling for demographic, social, and health variables. Regression and negative binomial models tested whether age-expectations were consistently associated with health and well-being across racial/ethnic groups.
Results
Age-expectations differed by race/ethnicity, overall and for each subscale. African American participants expected the least age-related functional decline and Chinese American participants expected the most decline. Although African American participants expected less decline than Latino participants in unadjusted models, they had comparable expectations adjusting for education. Latino and African American participants consistently expected less decline than Korean and Chinese Americans. Acculturation was not consistently related to age-expectations among immigrant participants over and above ethnicity. Although some previously observed links between expectations and health replicated across racial/ethnic groups, in adjusted models age-expectations were only related to depression for Latino participants.
Implications
With a growing racial/ethnic minority older population in the United States, it is important to note older adults’ age-expectations differ by race/ethnicity. Moreover, expectation-health associations may not always generalize across diverse samples.
Keywords: Attitudes and Perceptions toward Aging/aged, Diversity and Ethnicity, Health, Sociology of aging/social Gerontology
Perceptions of aging (age stereotypes and perceptions of one’s own aging) have been linked to older adults’ physical, cognitive, and social function (Levy, Zonderman, Slade, & Ferrucci, 2011; Menkin, Robles, Gruenewald, Tanner, & Seeman, 2016; Sarkisian, Hays, Berry, & Mangione, 2002). Stereotype embodiment theory posits perceptions of aging act as self-fulfilling prophecies (Levy, 2009). For example, expecting health decline to be part of aging is associated with lower perceived importance of seeking health care treatment (Sarkisian, Hays, & Mangione, 2002); this fatalism may undermine health.
Despite clinical relevance of perceptions of aging, relatively little research examines their determinants. Moreover, although some associations between perceptions of aging and health have replicated abroad (Kim, 2009), most work linking perceptions of aging to health has come from homogeneous, predominantly non-Latino white, samples. Research on intra-national racial/ethnic differences in perceptions of aging is rare.
The present study tests whether expectations regarding aging (i.e., age-expectations) differ across older adults from African American, Latino, Korean, and Chinese backgrounds living in greater Los Angeles. Specifically, high age-expectations refer to expectations of achievement and maintenance of high physical, mental, and cognitive functioning with aging (for self and others); low age-expectations are expectations of decline with age (Sarkisian, Hays, Berry, et al., 2002). Aside from the African American participants, most participants were immigrants and Los Angeles is a diverse metropolitan area with many ethnic enclaves facilitating continued cultural variation. In addition to identifying links between race/ethnicity, acculturation, and age-expectations, we also tested whether previously observed associations between age-expectations and health replicate or vary in strength for older adults of different races/ethnicities.
Factors Shaping Perceptions of Aging
Bringing together fragmented research on determinants of perceptions of aging, Kornadt and Rothermund (2015) proposed a model highlighting societal context, individual experiences, and biological changes as primary factors shaping domain-specific perceptions. Society may shape age-expectations both through differential exposure to negative images of aging and through cultural values influencing attention to this negative information. Given that age-expectations cover multiple domains (e.g., physical vs cognitive), and biological changes are also expected to shape perceptions, culture may influence some perceptions more than others (Löckenhoff et al., 2009).
Societal Context: Heritage Culture
While there have been no direct cross-cultural comparisons of age-expectations specifically, comparisons of broader perceptions of aging in Eastern and Western cultures have yielded mixed findings. Initially, Eastern cultures’ tradition of respect for elders led researchers to posit that East Asian adults have more positive perceptions of aging than those from Western societies (e.g., Levy & Langer, 1994). However, other studies find no cross-cultural differences (e.g., Boduroglu, Yoon, Luo, & Park, 2006), and a growing number show that East Asian respondents have more negative perceptions of aging (e.g., Harwood et al., 2001). Some differences may be due to sampling variability in small samples. A recent meta-analysis found respondents from East Asian countries had more negative perceptions of aging than those from Western societies. Yet, there was heterogeneity within regions. For example, South Korean participants had more negative perceptions of aging than participants from Western countries, but Chinese participants’ overall perceptions did not differ significantly from Western participants’ (North & Fiske, 2015). These studies compare perceptions of aging across countries; our study compares older adults from African American, Latino, Korean, and Chinese backgrounds living in the United States.
Levy (2009) suggests that we internalize age stereotypes based on exposure to messages about aging in media and everyday culture. Structural influences (e.g., population age composition; Löckenhoff et al., 2009) and cultural influences (e.g., individualism vs collectivism; North & Fiske, 2015) may shape age-expectations. Because we compare participants of different ethnicities living in the United States who are currently exposed to comparable structural influences, we focus on the persistent influence of culture on age-expectations.
Growing up in different cultures may not only shape exposure to different representations of aging but also how we process this information. North and Fiske’s (2015) meta-analysis found cultural individualism predicted more positive perceptions of aging. They theorize individualism facilitates acknowledging older adults’ contributions and valuing their experiences, while in collectivistic societies, older adults may be seen as a burden. Another possible explanation emerges from Fung’s (2013) framework that people internalize cultural values, which shape their goals and affect behavior and development. Individualistic values promote bias toward positive and away from negatively valenced information, especially in later life. Conversely, negative information (e.g., noticing an angry face) is useful within East Asian interdependent cultures, so this attentional bias (i.e., negativity avoidance) is rarely observed among older adults in East Asia. Differential attention to negative information about aging (e.g., from media portrayals) in more individualistic vs interdependent/collectivistic cultures may manifest in differential perceptions of aging.
Notably, this framework compares Western and East Asian cultures. Latino culture is also collectivistic. However, Campos and Kim (2017) posit that collectivism in Latino culture promotes greater positive affect as part of familial obligations, while East Asian collectivism focuses more on emotional balance and harmony. Respect for elders (i.e., respeto) encourages people to value and seek older adults for advice (Beyene, Becker, & Mayen, 2002), and these social functions are expected to be emotionally positive (Campos & Kim, 2017). Emphasis on positive affect within Latino culture may encourage attention to positive information and away from negative information more than among East Asian adults, facilitating higher age-expectations.
Oyserman, Coon, and Kemmelmeier (2002) found African Americans were more individualistic than European Americans; Latino/Hispanic Americans did not differ from European Americans, but Asian Americans were slightly less individualistic. Although we do not have individualism/collectivism data in our study, we expect similar patterns in our sample. Thus, given the link between individualism and attention to negative information, these findings suggest Chinese and Korean Americans would have the lowest age-expectations, followed by Latino Americans, with African Americans reporting the highest age-expectations.
The only study to our knowledge that has examined racial/ethnic differences in age-expectations within the United States compared non-Latino white, African American, and Latino older adults (Sarkisian, Shunkwiler, Aguilar, & Moore, 2006). Non-Latino white and African American participants had similar expectations of functional decline with age. Latino participants expected greater decline overall but had comparable expectations to the other participants adjusting for education, which was associated with higher age-expectations. (It is unclear why education is related to age-expectations and whether it is a proxy for cognitive resources, financial resources, socioeconomic status, or acculturation. We cannot differentiate among these interpretations in our study, so we include education as a covariate, to compensate for differential levels of education in our convenience sample, without focusing on theoretical interpretation.)
Extending this research to Asian American participants, based on the aforementioned link between collectivism and attention to negative information, we would expect participants with Korean or Chinese backgrounds to have lower age-expectations than the other participants. Korean American participants were expected to potentially score even lower than Chinese American participants because South Korea scored slightly lower in individualism than China (Hofstede, Hofstede, & Minkov, 2010). Moreover, Korean participants had more negative perceptions of aging than Chinese participants in previous multinational studies (e.g., Löckenhoff et al., 2009; North & Fiske, 2015). Consistent with Sarkisian et al. (2006), we also expected African American participants in our study to have higher age-expectations than Latino, Chinese, and Korean American participants (i.e., to expect less functional decline), but expected some of these differences might be accounted for by differences in education level.
Hypothesis 1: Age-expectations differ across racial/ethnic groups.
Societal Context After Immigration: Acculturation
If U.S. culture (e.g., individualism) promotes more positive views of aging (e.g., as suggested by North & Fiske, 2015), then greater acculturation in this context is expected to be associated with higher age-expectations. Past research with Korean American older adults found greater acculturation was associated with more positive self-perceptions of aging (Kim, Jang, & Chiriboga, 2012). However, Chinese American older adults who had lived in the United States for at least 15 years still had less positive perceptions of their own aging than Anglo-Americans (Tien-Hyatt, 1986). Immigrants’ perceptions of aging are likely shaped by both their heritage and current society’s culture.
Hypothesis 2: Greater acculturation is associated with higher age-expectations.
Domain Differences: Societal Context vs Biological Changes
The multidimensional nature of perceptions of aging may also contribute to mixed cross-cultural findings. Aging is associated with positively and negatively valenced stereotypes (e.g., senility vs wisdom) and with expected changes across a variety of domains (e.g., physical, cognitive, and socio-emotional changes). For example, participants tend to perceive declines in physical and cognitive function in later life, but perceive relative stability in social and emotional outcomes (e.g., Boduroglu et al., 2006; Harwood et al., 2001). Attention to variability across domains of age-expectations is important.
Furthermore, societal context, individual experiences, and biological changes may exert differential influence across domains of age-expectations. Perceptions about physical and cognitive changes may be more consistent across cultures if biological changes have more influence in those domains. Conversely, perceptions about social and emotional changes are especially likely to vary based on societal and individual context. Löckenhoff and colleagues (2009) proposed this idea and indeed found that, among college students, culture-level measures were more often related to perceptions of socioemotional aging than to perceived cognitive changes. None of their culture-level variables were significantly associated with expected changes in physical aging.
Hypothesis 3: Race/ethnicity explains more variance in older adults’ expectations about emotional and social outcomes than in expectations about physical or cognitive function.
Links From Perceptions of Aging to Health
Consistent with stereotype embodiment theory (Levy, 2009), American and Canadian participants’ age-expectations have been linked to their physical- and mental-health-related quality of life, depression, and physical activity (Meisner, Weir, & Baker, 2013; Sarkisian, Prohaska, Wong, Hirsch, & Mangione, 2005; Sarkisian, Steers, Hays, & Mangione, 2005). One study found people with lower age-expectations had more comorbidities and limitations in activities of daily living (e.g., needing help bathing; Sarkisian, Hays, Berry, et al., 2002).
Links between age-expectations and health have been replicated in some international, homogeneous samples. Korean participants with lower age-expectations reported worse health-related quality of life and less physical activity (Kim, 2009). Middle-aged adults in Singapore with higher age-expectations reported better health and fewer depressive symptoms (Joshi, Malhotra, Lim, Ostbye, & Wong, 2010). However, there has been no direct comparison of strength of these expectation-health associations across racial/ethnic groups and there may be variability in these associations across cultures. Fung (2013) highlights that while optimism is related to better health in Western samples, having more negative expectations about one’s future was beneficial for older Chinese adults’ wellbeing over time.
Hypothesis 4a: Age-expectations are linked to health in this racially/ethnically diverse sample.
Exploratory Hypothesis 4b: Previously reported associations between age-expectations and health-relevant outcomes from homogeneous samples may vary in strength across racial/ethnic groups.
Design and Methods
Participants
Participants were recruited for a randomized controlled trial promoting walking to reduce stroke risk among adults age 60 years or older with hypertension from African American, Latino, Korean, and Chinese backgrounds (see Kwon et al., 2015). Participants (N = 233) were recruited from near four Los Angeles, community-based, senior-service organizations. The current study uses data from participants’ baseline, individual, in-person, pre-randomization study visits. Four participants were excluded for missing data on age-expectations. Demographic and health characteristics for the remaining 229 participants are described in Table 1. Among the African American participants, all but three were born in the United States. Other participants (with the exception of three Latino participants) were born outside the United States. Instruments were forward- and back-translated into Spanish, Korean, and Chinese. All African American participants and three Latino participants completed the interview in English; all other Latino participants completed the interview in Spanish. Korean and Chinese American participants were interviewed in Korean or Mandarin Chinese, respectively.
Table 1.
Baseline Characteristics of Study Participants (N = 229)
| Racial/Ethnic Background | ||||||
|---|---|---|---|---|---|---|
| Characteristic | Overall (N = 229) | African American (n = 52) | Latino (n = 63) | Korean (n = 60) | Chinese (n = 54) | p value |
| Age, mean ± SD (range) | 73.9 ± 6.6 (60–96) | 73.0 ± 7.2 (61–87) |
72.4 ± 5.8 (62–87) |
76.2 ± 6.7 (60–96) |
74.2 ± 6.5 (63–86) | .011 |
| Female, n (%) | 157 (69%) | 39 (75%) | 49 (78%) | 36 (60%) | 33 (61%) | .075 |
| Physical-health-related quality of life, mean ± SD | 42.3 ± 10.0 | 43.1 ± 9.7 | 43.2 ± 10.1 | 42.1 ± 9.9 | 40.5 ± 10.3 | .465 |
| Mental-health related quality of life, mean ± SD | 50.5 ± 9.9 | 53.4 ± 10.6 | 50.5 ± 10.8 | 48.5 ± 8.6 | 49.9 ± 8.9 | .070 |
| Unable to perform ≥ 2 ADLs, n (%) | 40 (17%) | 11 (21%) | 11 (17%) | 6 (10%) | 12 (22%) | .301 |
| Number of comorbidities, mean ± SD | 2.0 ± 2.2 | 2.2 ± 2.1 | 1.4 ± 2.4 | 1.5 ± 1.8 | 2.8 ± 2.4 | .004 |
| Possible depression (PHQ9 score ≥ 10), n (%) | 37 (16%) | 7 (13%) | 13 (21%) | 10 (17%) | 7 (13%) | .653 |
| Perceived supporta, mean ± SD | 2.7 ± 1.1 | 3.4 ± 1.2 | 3.1 ± 1.1 | 1.9 ± 0.6 | 2.4 ± 0.7 | <.001 |
| Highest grade of formal education completed, n (%) | ||||||
| ≤8 | 61 (27%) | 1 (2%) | 32 (51%) | 9 (15%) | 19 (35%) | <.001 |
| 9–12 | 81 (35%) | 19 (37%) | 20 (32%) | 29 (48%) | 13 (24%) | .050 |
| Some college | 87 (38%) | 32 (62%) | 11 (17%) | 22 (37%) | 22 (41%) | <.001 |
| Years living in the United Statesb, mean ± SD | N/A | 37.1 ± 11.6 | 27.8 ± 11.2 | 23.1 ± 11.0 | <.001 | |
| Maintenance of heritage culturec, mean ± SD | N/A | 7.5 ± 1.2 | 7.0 ± 1.0 | 6.8 ± 0.8 | .002 | |
| Acculturation towards mainstream culturec, mean ± SD | N/A | 6.7 ± 1.6 | 5.2 ± 1.2 | 5.4 ± 1.3 | <.001 | |
| Overall expectations regarding aging scale, mean ± SD | 30.5 ± 21.6 | 48.3 ± 19.6 | 36.7 ± 21.2 | 22.8 ± 15.0 | 14.8 ± 13.6 | <.001 |
| Physical health subscale, mean ± SD | 27.3 ± 23.1 | 43.1 ± 22.6 | 35.5 ± 21.7 | 19.4 ± 17.7 | 11.3 ± 15.5 | <.001 |
| Mental health subscale, mean ± SD | 37.0 ± 28.4 | 60.6 ± 27.1 | 41.8 ± 27.7 | 27.8 ± 19.9 | 19.0 ± 20.4 | <.001 |
| Cognitive function subscale, mean ± SD | 27.3 ± 23.1 | 41.3 ± 22.8 | 32.8 ± 23.1 | 21.1 ± 17.1 | 14.0 ± 19.7 | <.001 |
Notes. Test of significance for difference between racial/ethnic groups was derived using a chi-square test for categorical variables and analysis of variance for the continuous variables. ADLs = activities of daily living, SD = standard deviation. Acculturation measures were not administered to African American participants.
aItem missing for one participant. bItem missing for six (3%) participants. cItem missing for 15 (8%) participants.
Measures
Age-Expectations
The Expectations Regarding Aging short-form scale (ERA-12; Sarkisian, Steers, et al., 2005) assessed participants’ expected age-related changes across three subscales: physical health, mental health, and cognitive function (The mental health subscale included items reflecting social and emotional changes, specifically expectations of loneliness, social withdrawal, worry, and depression.) Participants rated statements describing age-related declines such as “Having more aches and pains is an accepted part of aging,” or “It’s normal to be depressed when you are old,” as definitely true, somewhat true, somewhat false, or definitely false. Scores were transformed to a 0–100 scale with higher scores indicating expectations of greater physical function, social and emotional wellbeing, and cognitive function in later life. We computed transformed scores for the overall ERA-12 scale (α = 0.90) and separate transformed scores for each subscale (physical health α = 0.74, mental health α = 0.85, cognitive function α = 0.83). Eight participants were missing one item per subscale; the item score was imputed using the mean of the remaining subscale item scores. Four participants missing multiple items within a subscale were excluded.
Social and Demographic Variables
Participants self-reported race/ethnicity, age, and gender. Education was categorized as the highest grade completed: below 8th, 9–12th, or higher education. We used the overall perceived support score from a scale validated for use with ethnically diverse samples (Wong, Nordstokke, Gregorich, & Pérez-Stable, 2010); one participant did not respond.
Acculturation
The Vancouver Acculturation Index assesses acquisition of American mainstream culture and maintenance of heritage culture; higher mainstream scores and lower heritage scores reflect greater orientation toward American culture (Ryder, Alden, & Paulhus, 2000). We also measured number of years participants had lived in the United States. Acculturation measures were not administered to African American participants. Three Latino and three Chinese American participants did not report the number of years they lived in the United States, and one Latino, six Korean, and eight Chinese American participants skipped the Acculturation Index.
Physical and Mental Health
The Medical Outcomes Study 12-item Short Form (SF-12; Ware, Kosinski, & Keller, 1996) yielded separate standardized physical- and mental-health-related quality of life scores, comparing sample participants to the mean and standard deviation of the general U.S. population. Higher scores indicated better health-related quality of life. The interview also assessed number of medical comorbidities (Charlson comorbidity scale modified for self-administration; Katz, Chang, Sangha, Fossel, & Bates, 1996) and limitations in activities of daily living (ADLs; Gill, McGloin, Gahbauer, Shepard, & Bianco, 2001). Depression severity was assessed with the Patient Health Questionnaire (PHQ9; Kroenke & Spitzer, 2002).
Health Behavior
We totaled self-reported minutes of physical activity (i.e., walking, moderate, and vigorous exercise) from the International Physical Activity Questionnaire (Craig et al., 2003). Because the distribution was strongly positively skewed, we rounded to the nearest number of minutes and treated the variable as a count.
Data Analysis
Racial/Ethnic Differences in Age-Expectations
Our first aim was to test whether age-expectations differed across racial/ethnic groups. Unadjusted regression models tested whether race/ethnicity (dummy-coded) accounted for significant variance in age-expectations (N = 229). Pair-wise comparisons with a Sidak adjustment identified which groups were different from each other. Multivariate regression models tested whether race/ethnicity predicted age-expectations over and above covariates (age, gender, perceived support, physical-health-related quality of life, mental-health-related quality of life, and education; N = 228). Perceived support, physical health, mental health, and education have been linked to age-expectations (Menkin et al., 2016; Sarkisian, Steers, et al., 2005; Sarkisian et al., 2006) (Depression was highly correlated with mental-health related quality of life, and number of ADL limitations and comorbidities were highly correlated with physical-health related quality of life, so they were excluded for parsimony and ease of model interpretation.)
Acculturation
Acculturation was not included in the full-sample model because the measures were not administered to African American participants. Instead, we ran parallel models to those described above with the Latino, Chinese, and Korean American subsample, adding acculturation to the unadjusted and adjusted models to test whether exposure to U.S. culture was related to age-expectations over and above ethnicity. Latino-American participants on average had greater exposure to U.S. culture than the Chinese and Korean American participants (Table 1) and had higher age-expectations, so these models also allowed us to verify ethnic differences were not due to differences in the samples’ acculturation.
Domain Differences
Our third aim was to identify whether race/ethnicity accounted for more variance in expectations about mental health than about physical and cognitive function. We compared the effect sizes (adjusted R2) of unadjusted regression models linking race/ethnicity to the respective age-expectations subscales. We also looked at pair-wise comparisons for unadjusted and adjusted models predicting each expectation subscale in order to test whether the patterns of racial/ethnic differences varied by domain. (We analyzed the full sample, and thus did not include acculturation. If acculturation measures were tested as predictors in addition to ethnicity, only greater mainstream acculturation was associated with higher mental health expectations over and above ethnicity, b = 3.84, SE = 1.38, p = .006. None of the acculturation measures accounted for significant variance in any of the other age-expectation subscales over and above ethnicity.)
Expectation-Health Link Across Racial/Ethnic Groups
We tested whether links between age-expectations and health-related outcomes observed in homogeneous samples replicated in this diverse sample, and whether the links’ strength differed across racial/ethnic groups. Overall age-expectations were treated as a predictor of health-related outcomes. We ran regression models predicting physical- and mental-health-related quality of life and depression, and tested negative binomial models predicting number of ADL limitations, comorbidities, and minutes of physical activity. After testing unadjusted models, we adjusted for demographics, education, perceived support, and physical- and mental-health-related quality of life. (For models predicting mental- and physical-health-related quality of life, the corresponding covariate was dropped from the adjusted model.) Next we checked whether adding a set of interaction terms between race/ethnicity (dummy-coded) and overall age-expectations significantly improved the model fit, using R2 change tests (for continuous outcomes) or likelihood ratio tests comparing deviance scores (for count outcomes) from models with and without the interaction terms as predictors. First, we added the interaction terms to a model only including age-expectations and race/ethnicity; second, we added the interaction terms to the adjusted model. If interaction terms improved model fit, we compared the age-expectations betas from regression models, shifting which race/ethnicity was the referent group.
Results
Racial/Ethnic Differences in Age-Expectations
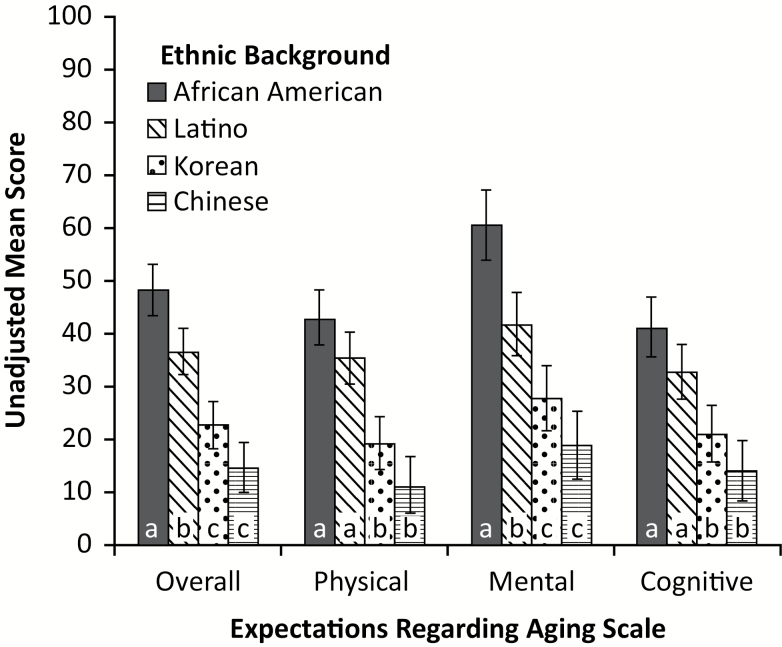
Overall age-expectation scores differed across racial/ethnic groups. In an unadjusted model, race/ethnicity accounted for significant variance in age-expectations, F(3, 225) = 38.30, p ≤ .001. African American participants had the highest overall age-expectations followed in descending order by Latino, Korean, and Chinese American participants (Figure 1). Pair-wise comparisons indicated that, although Korean and Chinese American participants did not differ (p = .095), all other racial/ethnic groups had different age-expectations (p’s ≤ .003). In the adjusted model, the only change was that African American and Latino participants no longer had different age-expectations (Table 2); the difference was not significant over and above education.
Figure 1.
Unadjusted mean expectation regarding aging scores for overall scale and each subscale by race/ethnicity. Bars represent unadjusted 95% confidence intervals. Within each dependent variable scale, racial/ethnic group means that are significantly different from each other, based on pair-wise comparisons with Sidak corrections, are identified with different letters.
Table 2.
Characteristics Associated with Higher Age-Expectations
| Outcome | Variable | Parameter Estimate (SE) | |
|---|---|---|---|
| Unadjusted (N = 229) | Adjusted (N = 228) | ||
| Overall expectations | Intercept | 36.71 (2.23)*** | 34.77 (15.24)* |
| African American | 11.63 (3.31)*** | 3.73 (3.46) | |
| Korean American | –13.94 (3.19)*** | –13.92 (3.46)*** | |
| Chinese American | –21.95 (3.28)*** | –21.56 (3.27)*** | |
| Age (per year) | –0.25 (0.17) | ||
| Male | –5.63 (2.47)* | ||
| Perceived support | 1.15 (1.16) | ||
| Physical-health-related quality of life | 0.18 (0.11) | ||
| Mental-health-related quality of life | 0.38 (0.11)*** | ||
| Education (grade) | |||
| <or= to 8 | –14.40 (3.16)*** | ||
| 9–12 | –5.90 (2.64)* | ||
| Physical-health expectations | Intercept | 35.49 (2.47)*** | 43.07 (17.46)* |
| African American | 7.62 (3.67)* | 2.87 (3.96) | |
| Korean American | –16.05 (3.54)*** | –13.82 (3.97)*** | |
| Chinese American | –24.23 (3.63)*** | –22.58 (3.74)*** | |
| Age (per year) | –0.31 (0.20) | ||
| Male | –8.78 (2.83)** | ||
| Perceived support | 0.98 (1.33) | ||
| Physical-health-related quality of life | 0.24 (0.13)† | ||
| Mental-health-related quality of life | 0.21 (0.13) | ||
| Education (grade) | |||
| <or= to 8 | –9.41 (3.62)** | ||
| 9–12 | –6.70 (3.03)* | ||
| Mental-health expectations | Intercept | 41.80 (3.03)*** | 34.63 (20.41)† |
| African American | 18.78 (4.51)*** | 7.15 (4.63) | |
| Korean American | –14.02 (4.34)*** | –14.61 (4.64)** | |
| Chinese American | –22.82 (4.46)*** | –23.13 (4.37)*** | |
| Age (per year) | –0.35 (0.23) | ||
| Male | –4.72 (3.31) | ||
| Perceived support | 1.46 (1.55) | ||
| Physical-health-related quality of life | 0.12 (0.15) | ||
| Mental-health-related quality of life | 0.72 (0.15)*** | ||
| Education (grade) | |||
| <or= to 8 | –20.00 (4.23)*** | ||
| 9–12 | –7.17 (3.54)* | ||
| Cognitive-function expectations | Intercept | 32.85 (2.62)*** | 26.59 (18.77) |
| African American | 8.50 (3.90)* | 1.17 (4.26) | |
| Korean American | –11.74 (3.75)** | –13.32 (4.26)** | |
| Chinese American | –18.81 (3.86)*** | –18.96 (4.02)*** | |
| Age (per year) | –0.09 (0.21) | ||
| Male | –3.39 (3.05) | ||
| Perceived support | 1.02 (1.43) | ||
| Physical-health-related quality of life | 0.17 (0.14) | ||
| Mental-health-related quality of life | 0.22 (0.14) | ||
| Education (grade) | |||
| <or= to 8 | –13.78 (3.89)*** | ||
| 9–12 | –3.83 (3.26) | ||
Notes: Latino participants are the race/ethnicity reference group, and some college is the education reference group.
*p ≤ .05, **p ≤ .01, ***p ≤. 001.
Acculturation
Neither living longer in the United States (b = 0.06, SE = 0.12) nor maintaining/rejecting heritage culture (b = 1.26, SE = 1.35) were associated with age-expectations over and above ethnicity (p’s > .35). Greater adoption of mainstream culture was correlated with higher overall age-expectations (b = 2.68, SE = 0.97, p = .007) independent of ethnicity. Ethnic differences in overall age-expectations persisted after controlling for mainstream acculturation. (In fact, because of fewer pair-wise comparisons, in the subsample the Korean American participants had significantly higher age-expectations than the Chinese Americans.) After adjusting for other covariates, the ethnic differences in age-expectations persisted but adoption of mainstream culture was no longer significantly associated with age-expectations (b = 1.44, SE = 0.96). (Conclusions were identical with and without the Latino participants born in the United States. There was also no evidence that acculturation moderated the relationship between ethnicity and age-expectations (i.e., acculturation to U.S. culture did not trump the effects of heritage culture on age-expectations.))
Domain Differences
In unadjusted models, race/ethnicity accounted for significant variance in each subscale of age-expectations: physical health F(3, 225) = 30.22, mental health F(3, 225) = 30.48, and cognitive function F(3, 225) = 18.47 (p’s ≤ .001). Comparing effect sizes, race/ethnicity accounted for the most variance in overall age-expectations scores (adjusted R2 = 0.33) vs the subscales. Race/ethnicity accounted for 28% of variance in both physical-health age-expectations and in mental-health age-expectations, but only 19% of variance in cognitive-function age-expectations.
The patterns of racial/ethnic differences were identical for physical-health and cognitive-function age-expectations. Pair-wise comparisons showed that African American and Latino participants had higher physical-health and cognitive-function expectations than Korean and Chinese Americans (p’s ≤ .012). African American and Latino participants did not differ in their physical-health or cognitive-function expectations (p ≥ .169), nor did Korean and Chinese American participants (p ≥ .152). The adjusted models produced parallel conclusions.
There were more differences among racial/ethnic groups for mental-health expectations. Pair-wise comparisons showed all racial/ethnic groups had significantly different expectations (p’s ≤ .009) except Chinese and Korean Americans (p = .277; Figure 1). In adjusted models, the only change was that African American and Latino participants no longer had different expectations (Table 2) over and above education.
Expectation-Health Link Across Racial/Ethnic Groups
Physical-Health-Related Outcomes
In unadjusted models, age-expectations positively correlated with physical-health-related quality of life, b = 0.08, SE = 0.03, p = .011. However, there was no association after adjusting for demographics, perceived support, education, and mental-health-related quality of life, b = 0.06, SE = 0.04, p = .115. Moreover, age-expectations were not related to ADL limitations nor comorbidities in unadjusted or adjusted models (p’s ≥ .127). Yet, age-expectations were positively correlated with physical activity, in unadjusted b = 0.01, SE = 0.003, p = .001; and adjusted models b = 0.01, SE = 0.004, p = .003. Adding age-expectation and race/ethnicity interaction terms did not improve model fit for any of these outcomes (unadjusted or adjusted, p’s ≥ .131).
Mental-Health-Related Outcomes
Age-expectations scores were positively correlated with mental-health-related quality of life, in unadjusted b = 0.12, SE = 0.03, p < .001; and adjusted models b = 0.13, SE = 0.04, p = .001. Adding age-expectation and race/ethnicity interaction terms did not improve model fit (unadjusted or adjusted, p’s ≥ .489).
Age-expectations were negatively correlated with depression severity, in unadjusted b = –0.06, SE = 0.02, p < .001; and adjusted models b = –0.08, SE = 0.02, p < .001. Although adding interaction terms for age-expectations and race/ethnicity to the unadjusted model did not significantly improve model fit (p = .079), adding the interaction terms to the adjusted model did, F(13, 214) = 4.53, p < .001. There was no association between age-expectations and depression for Chinese, Korean, and African American participants, but Latino participants with lower age-expectations reported greater depression, age-expectation b = –0.16, SE = 0.03, p < .001.
Discussion
Expectations regarding aging differed substantially across racial/ethnic groups. As hypothesized, African American participants overall expected less functional decline with age than participants with Latino, Korean, or Chinese backgrounds. However, as in Sarkisian et al. (2006), once education differences were accounted for, African American and Latino participants’ age-expectations no longer differed. Higher education was associated with higher age-expectations (i.e., less expected decline with age) for Latino participants, and Latino participants overall had lower levels of education than African American participants. Further research is needed to explain this link between education and age-expectations (e.g., whether it is a proxy for financial vs cognitive resources). Still, after controlling for demographic, social, and health covariates, both African American and Latino participants consistently had higher age-expectations than Korean and Chinese American participants.
We observed similar differences between East Asian immigrants and American-born participants as previously found between native residents in East Asian and Western societies. African American participants having higher age-expectations than Korean and Chinese American participants was consistent with the meta-analysis indicating people from more individualistic societies tend to have more positive perceptions of aging than those from more collectivistic societies (North & Fiske, 2015) possibly due to differences in attention to negative information. Notably, our racial/ethnic groups differed in endorsement of declines with age. Perceptions of positive changes may be more consistent across racial/ethnic groups. There is greater bias toward positive and away from negative information in individualistic cultures, but positive information captures attention more than neutral information cross-culturally (e.g., Fung, 2013).
Race/ethnicity (proxy for heritage culture) and adoption of mainstream U.S. culture independently accounted for variance in age-expectations, but acculturation was less consistently linked to age-expectations. This suggests that early cultural influences may shape age-expectations more than recent exposure to new cultural context, consistent with Levy’s (2009) hypothesis that we are more vulnerable to internalizing age stereotypes when they are not yet self-relevant. Notably, the vast majority of participants in this analysis were born outside the United States, limiting acculturation variability. Acculturation may be more consistently linked to age-expectations when comparing U.S. natives with immigrants of the same race/ethnicity.
Consistent with Kornadt and Rothermund (2015), we found evidence for domain specificity in age-expectations. Our hypothesis that race/ethnicity would affect expectations about socio-emotional changes more than expectations about physical or cognitive changes was partially supported. Race/ethnicity accounted for more variance in mental-health than cognitive-function age-expectations, but race/ethnicity accounted for the same amount of variance in physical- and mental-health age-expectations. Social and emotional age-related changes appear sensitive to cultural context, but items from the physical-health subscale assessing expectations about energy/vitality may be more open to cultural interpretation than previously-studied physical age-stereotypes (e.g., changes in appearance; Löckenhoff et al., 2009).
In line with stereotype embodiment theory (Levy, 2009), we found links between age-expectations and physical- and mental-health-related quality of life, depression, and physical activity in our diverse sample. We found no association between age-expectations and comorbidities or ADL limitations. Past studies linking age-expectations to these outcomes have used the long-form Expectations Regarding Aging scale (ERA-38; Sarkisian, Hays, Berry, et al., 2002) and these associations have not yet replicated with the short-form scale (ERA-12; e.g., Sarkisian, Steers, et al., 2005). Thus, the lack of replication may be due to using different forms of the scale, or possibly our sample’s history of hypertension, rather than due to differences in the samples’ racial/ethnic composition.
Previous research linking age-expectations and health typically examined bivariate correlations. We further tested whether associations were significant after adjusting for demographic, social, and health covariates. Age-expectations were associated with mental-health-related quality of life and minutes of physical activity; however, age-expectations were no longer associated with physical-health-related quality of life after adjusting for covariates.
Interestingly, we found that after adjusting for covariates, the link between age-expectations and depression differed by race/ethnicity. Age-expectations were only significantly associated with depression severity for Latino participants, not Chinese, Korean, or African American participants. Fung (2013) suggested that although optimism appears adaptive for older adults in Western contexts, negative expectations about the future may be adaptive for East Asian older adults’ wellbeing. This may explain the null association between negative age-expectations and depression among the Chinese and Korean Americans; however, it is unclear why age-expectations are not linked to depression among African American participants. Moreover, given the correlational design, we cannot conclude that age-expectations influence depression in Latino participants; Latino participants’ depression may undermine expectations about aging. Our results suggest most findings from less diverse, published samples generalized to participants from African American, Latino, Chinese, and Korean backgrounds. Yet, some health outcomes may be linked to age-expectations only in certain racial/ethnic groups.
The identified racial/ethnic differences in age-expectations are novel and important contributions to our understanding of the relationship between race/ethnicity and perceptions of aging, but we could not directly test why these differences exist. The study was designed to test a stroke-reduction intervention and we lacked measures of individualism/collectivism (which can vary within racial/ethnic groups). Moreover, immigrants can differ from non-immigrants, which may limit generalizability. Yet, aging immigrants are understudied and by identifying intra-national racial/ethnic differences in age-expectations we lay foundation for future research elucidating nuances and possible cultural mechanisms.
Confounds also exist in the dataset. Race/ethnicity is confounded with language of survey administration so it is possible that, despite rigorous front and back-translation methods, some ethnic differences could be translation artifacts. Validating translations with bi-lingual, older participants could rule out this alternative explanation. Also, different racial/ethnic groups were recruited from near different senior centers, so there could be unmeasured community variables that are distinct from, but confounded with, race/ethnicity that contribute to age-expectations.
Implications for Policy and Practice
The U.S. population of non-white older adults is growing. Understanding age-expectations is a key part of providing culturally competent health care, as understanding older patients’ mental models can facilitate clinician-patient communication (e.g., addressing fatalism). If there is a causal relationship between perceptions of aging and healthy aging (such as hypothesized by Levy, 2009), racial/ethnic differences in age-expectations may help identify at-risk groups for interventions to improve perceptions of aging and subsequently improve health (e.g., targeting Latino age-expectations to reduce depression). Conversely, unrealistically high expectations can backfire, and Korean and Chinese American older adults’ lower expectations may actually be adaptive for future wellbeing (e.g., Cheng, Fung, & Chan, 2009). Thus programs promoting positive views of aging must be sensitive to cultural context.
Funding
This work was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (1-U54NS081764); the National Institute on Aging of the National Institutes of Health (1K24AG047899-02, P30-AG021684, and P30AG028748); and AARP. This paper was published as part of a supplement sponsored and funded by AARP. The statements and opinions expressed herein by the authors are for information, debate, and discussion, and do not necessarily represent official policies of AARP.
Acknowledgments
The authors would like to acknowledge the critically important contributions of our community partner staff without whose partnership the “Worth the Walk” project could not have been completed: Charlayne Browe and Paul Magee from Watts Labor Community Action Committee/Theresa Lindsay Senior Center; Andres Gonzalez, Helen Hong, Jaeun Joo, and Fabiola Torres from St. Barnabas Senior Services; Elaine Chen from Chinatown Service Center; and Maria Sanchez from Mexican American Opportunity Foundation. We are also thankful to Theodore Robles who commented on versions of this manuscript and to Bryanna and Brennan Lee for volunteering their time to help with data cleaning and literature searches.
References
- Beyene Y., Becker G., & Mayen N (2002). Perception of aging and sense of well-being among Latino elderly. Journal of Cross-Cultural Gerontology, 17, 155–172. doi:10.1023/A:1015886816483 [DOI] [PubMed] [Google Scholar]
- Boduroglu A., Yoon C., Luo T., & Park D. C (2006). Age-related stereotypes: a comparison of American and Chinese cultures. Gerontology, 52, 324–333. doi:10.1159/000094614 [DOI] [PubMed] [Google Scholar]
- Campos B. & Kim H. S (2017). Incorporating the cultural diversity of family and close relationships into the study of health. American Psychologist. [DOI] [PubMed] [Google Scholar]
- Cheng S. T., Fung H. H., & Chan A. C (2009). Self-perception and psychological well-being: the benefits of foreseeing a worse future. Psychology and Aging, 24, 623–633. doi:10.1037/a0016410 [DOI] [PubMed] [Google Scholar]
- Cohen S., & Hoberman H. M (1983). Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology, 13, 99–125. doi:10.1111/j.1559–1816.1983.tb02325.x [Google Scholar]
- Craig C. L., Marshall A. L., Sjöström M., Bauman A. E., Booth M. L., Ainsworth B. E.,…Oja P (2003). International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise, 35, 1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- Fung H. H. (2013). Aging in culture. Gerontologist, 53, 369–377. doi:10.1093/geront/gnt024 [DOI] [PubMed] [Google Scholar]
- Gill T. M., McGloin J. M., Gahbauer E. A., Shepard D. M., & Bianco L. M (2001). Two recruitment strategies for a clinical trial of physically frail community-living older persons. Journal of the American Geriatrics Society, 49, 1039–1045. doi:10.1046/j.1532-5415.2001.49206.x [DOI] [PubMed] [Google Scholar]
- Harwood J., Giles H., McCann R. M., Cai D., Somera L. P., Ng S. H.,…Noels K (2001). Older adults’ trait ratings of three age-groups around the Pacific rim. Journal of Cross-Cultural Gerontology, 16, 157–171. doi:10.1023/A:1010616316082 [DOI] [PubMed] [Google Scholar]
- Hofstede G., Hofstede G. J., & Minkov M (2010). Cultures and organizations: Software of the mind (3rd ed.). New York, NY: McGraw-Hill. [Google Scholar]
- Joshi V. D., Malhotra R., Lim J. F., Østbye T., & Wong M (2010). Validity and reliability of the expectations regarding aging (ERA-12) instrument among middle-aged Singaporeans. Annals of the Academy of Medicine, Singapore, 39, 394–398. [PubMed] [Google Scholar]
- Katz J. N., Chang L. C., Sangha O., Fossel A. H., & Bates D. W (1996). Can comorbidity be measured by questionnaire rather than medical record review?Medical Care, 34, 73–84. doi:10.1097/00005650-199601000-00006 [DOI] [PubMed] [Google Scholar]
- Kim G., Jang Y., & Chiriboga D. A (2012). Personal views about aging among Korean American older adults: the role of physical health, social network, and acculturation. Journal of Cross-Cultural Gerontology, 27, 139–148. doi:10.1007/s10823-012-9165-2 [DOI] [PubMed] [Google Scholar]
- Kim S. H. (2009). Older people’s expectations regarding ageing, health-promoting behaviour and health status. Journal of Advanced Nursing, 65, 84–91. doi:10.1111/j.1365-2648.2008.04841.x [DOI] [PubMed] [Google Scholar]
- Kornadt A. E. & Rothermund K (2015). Views on aging: Domain-specific approaches and implications for developmental regulation. Annual Review of Gerontology and Geriatrics, 35, 121–144. doi:10.1891/0198-8794.35.121 [Google Scholar]
- Kroenke K., & Spitzer R. L (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, 509–515. doi:10.3928/0048-5713-20020901-06 [Google Scholar]
- Kwon I., Choi S., Mittman B., Bharmal N., Liu H., Vickrey B., … Sarkisian C (2015). Study protocol of “Worth the Walk”: a randomized controlled trial of a stroke risk reduction walking intervention among racial/ethnic minority older adults with hypertension in community senior centers. BMC Neurology, 15, 91. doi:10.1186/s12883-015-0346-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332–336. doi:10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B., & Langer E (1994). Aging free from negative stereotypes: successful memory in China and among the American deaf. Journal of Personality and Social Psychology, 66, 989–997. doi:10.1037//0022-3514.66.6.989 [DOI] [PubMed] [Google Scholar]
- Levy B. R., Zonderman A. B., Slade M. D., & Ferrucci L (2012). Memory shaped by age stereotypes over time. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 67, 432–436. doi:10.1093/geronb/gbr120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löckenhoff C. E., De Fruyt F., Terracciano A., McCrae R. R., De Bolle M., Costa P. T. Jr,…Yik M (2009). Perceptions of aging across 26 cultures and their culture-level associates. Psychology and Aging, 24, 941–954. doi:10.1037/a0016901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisner B. A., Weir P. L., & Baker J (2013). The relationship between aging expectations and various modes of physical activity among aging adults. Psychology of Sport and Exercise, 14, 569–576. doi:10.1016/j.psychsport.2013.02.007 [Google Scholar]
- Menkin J. A., Robles T. F., Gruenewald T. L., Tanner E. K., & Seeman T. E (2016). Positive expectations regarding aging linked to more new friends in later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- North M. S., & Fiske S. T (2015). Modern attitudes toward older adults in the aging world: a cross-cultural meta-analysis. Psychological Bulletin, 141, 993–1021. doi:10.1037/a0039469 [DOI] [PubMed] [Google Scholar]
- Oyserman D., Coon H. M., & Kemmelmeier M (2002). Rethinking individualism and collectivism: evaluation of theoretical assumptions and meta-analyses. Psychological Bulletin, 128, 3–72. doi:10.1037//0033-2909.128.1.3 [PubMed] [Google Scholar]
- Ryder A. G., Alden L. E., & Paulhus D. L (2000). Is acculturation unidimensional or bidimensional? A head-to-head comparison in the prediction of personality, self-identity, and adjustment. Journal of Personality and Social Psychology, 79, 49–65. doi:10.1037//0022-3514.79.1.49 [DOI] [PubMed] [Google Scholar]
- Sarkisian C. A., Hays R. D., Berry S., & Mangione C. M (2002). Development, reliability, and validity of the expectations regarding aging (ERA-38) survey. Gerontologist, 42, 534–542. doi:10.1093/geront/42.4.534 [DOI] [PubMed] [Google Scholar]
- Sarkisian C. A., Hays R. D., & Mangione C. M (2002). Do older adults expect to age successfully? The association between expectations regarding aging and beliefs regarding healthcare seeking among older adults. Journal of the American Geriatrics Society, 50, 1837–1843. doi:10.1046/j.1532-5415.2002.50513.x [DOI] [PubMed] [Google Scholar]
- Sarkisian C. A., Prohaska T. R., Wong M. D., Hirsch S., & Mangione C. M (2005a). The relationship between expectations for aging and physical activity among older adults. Journal of General Internal Medicine, 20, 911–915. doi:10.1111/j.1525-1497.2005.0204.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkisian C. A., Shunkwiler S. M., Aguilar I., & Moore A. A (2006). Ethnic differences in expectations for aging among older adults. Journal of the American Geriatrics Society, 54, 1277–1282. doi:10.1111/j.1532-5415.2006.00834.x [DOI] [PubMed] [Google Scholar]
- Sarkisian C. A., Steers W. N., Hays R. D., & Mangione C. M (2005). Development of the 12-item expectations regarding aging survey. Gerontologist, 45, 240–248. doi:10.1093/geront/45.2.240 [DOI] [PubMed] [Google Scholar]
- Tien-Hyatt J. L. (1986). Self perceptions of aging across cultures: Myth or reality? International Journal of Aging and Human Development, 24, 129–48. doi:10.2190/MCF9-22DM-8HPA-P3F4 [DOI] [PubMed] [Google Scholar]
- Ware J. Jr, Kosinski M., & Keller S. D (1996). A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220–233. doi:10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- Wong S. T., Nordstokke D., Gregorich S., & Pérez-Stable E. J. (2010). Measurement of social support across women from four ethnic groups: Evidence of factorial invariance. Journal of Cross Cultural Gerontology, 25, 45–58. doi:10.1007/s10823-010-9111-0 [DOI] [PMC free article] [PubMed] [Google Scholar]