Abstract
As resident acuity levels increase for those who reside in assisted living (AL), states allow for hospice care provision in AL. End-of-life care training for staff can potentially increase the awareness of benefits of hospice care for AL residents. This study examined the association between AL staff trained in end-of-life care and hospice utilization in a sample of ALs (n = 45) in Florida. The sample included ALs (n = 21) with a low percentage (≤59%) and ALs (n = 24) with a high percentage (≥60%) of staff trained in end-of-life care as reported by AL directors. Zero-inflated negative binomial regression (ZINB) indicated that ALs in the high percentage of staff trained group were associated with a 3.64% greater utilization of hospice than ALs in the low percentage of staff trained group. Implementation of required staff training specific to care for the terminally ill as required in some states could potentially improve resident access to hospice care.
Keywords: assisted living, staff training, end-of-life care, hospice use
Background
Assisted living (AL) communities are sought out by many older adults who do not require a medical setting, but are in need of 24-hr supervision and assistance with activities of daily living (Wilson, 1996). Close to one third of AL residents remain until death in these settings, (Munn, Hanson, Zimmerman, Sloane, & Mitchell, 2006; Sloane et al., 2003). ALs have begun to utilize resources, such as hospice and direct care staff training, to maintain quality end-of-life care for residents who wish to age-in-place (Cartwright, Miller, & Volpin, 2009; Munn et al., 2006). Four states (Iowa, South Dakota, Texas, and Wyoming) currently require direct care staff to attend training within 30 days of employment and annually specific to the care for terminally ill residents and a competency evaluation by a nurse or hospice nurse agency (Carder, O’Keeffe, & O’Keeffe, 2015).
Hospice is well known for its goal of improving quality-of-life during end-of-life through comfort care (Torpy, Burke, & Golub, 2012). The approximate 3,400 hospice programs throughout the United States are growing with 50% of all decedents receiving hospice care (National Hospice and Palliative Care Organization, 2017). This has resulted in an increase in the use of hospice in ALs. National hospice figures show that of the one million persons who received hospice care in 2015, 10% received it in residential care settings such as ALs (National Hospice and Palliative Care Organization, 2017). Some studies have shown that hospice care in ALs has improved quality outcomes such as shorter hospital stays, lower nursing home admission rates (Meng, Dobbs, Wang, Hyer, 2013), and increased family satisfaction (Munn et al., 2008; Sloane et al., 2003).
End-of-life care training has been shown to improve a resident’s transition to hospice care and the quality of care during the dying process (Cartwright et al., 2009; Keay, Alexander, McNally, Crusse, & Eger, 2003; Munn et al., 2006). Despite these quality improvements, more AL residents are transferred to nursing homes than referred to hospice (Zimmerman et al., 2005). Although there has not been empirical evidence in ALs to show whether direct care staff end-of-life care training would increase the utilization of hospice, this has been evidenced in nursing homes (Hanson, Reynolds, Henderson, & Pickard, 2005).
One of the top three largest barriers to hospice use is knowing when the appropriate time is to refer someone for care (Knapp & Thompson, 2012). End-of-life care education provides the necessary skills for direct care staff to identify residents in need of hospice and other forms of palliative care, and to provide quality end-of-life care (Goddard, Stewart, Thomson, & Hall, 2013). Munn et al. (2006) showed that hospice was utilized in 93% of the cases where direct care staff anticipated a resident was dying versus 55% of cases in which they did not (p < .001). The purpose of this pilot study was to examine the relationship between the percentage of direct care staff trained on how to provide care at the end of life and hospice utilization. It was hypothesized that a higher percentage of direct care staff trained on how to provide care at the end of life was associated with greater hospice utilization in ALs, while controlling for key organizational characteristics (AL capacity, profit-status).
Method
Facility Sample Population
The pilot study sample consisted of a subset of 45 large ALs (>16 bed) selected from a larger cross-sectional survey study (N = 76) conducted about palliative and hospice care practices in Florida ALs and adult family care homes (Dobbs, 2011). The parent study was conducted between May 2009 and April 2010. For more details about the parent study see Holup, Dobbs, Temple, & Hyer, 2014. For this study, ALs were deemed eligible (n = 45) if both of the following two conditions were met at the time of the survey: (a) AL directors reported training data and (b) the AL was licensed for 17 beds or more. As previously stated, ALs are defined as community-based facilities, which provide 24-hr supervision and assistance (Wilson, 1996). This minimum number of beds was chosen because Florida ALs licensed for 17 or more beds are required by state regulations to schedule alert direct care staff 24 hr per day (Dobbs, 2011), a key factor in whether a resident who is hospice eligible could remain in the setting. Figure 1 outlines the process of determining eligibility for this study from the initial pilot study sample (N = 76). The eligible facilities were divided by the percentage of trained direct care staff, low (less than 59%, n = 21) and high (60% or more, n = 24). The eligible facilities reported that hospice was used in 28 ALs by at least one resident. Detailed AL organizational characteristics of the eligible ALs by both high and low percentages of direct care staff trained are shown in Table 1.
Figure 1.
Eligibility determination for this study for assisted living facility EOL trained and untrained direct care staff.
Note. EOL = end of life; RN = registered nurse.
Table 1.
Characteristics of Eligible Assisted Living Facilities.
| Percentage of direct care staff trained in end-of-life care |
||||
|---|---|---|---|---|
| AL Facility Characteristics | Low (n = 21) |
High (n = 24) |
||
| M | SD | M | SD | |
| Census | 75.95 | 38.46 | 56.92 | 27.56 |
| Capacity | 85.43 | 39.82 | 68.33 | 32.78 |
| n | % | n | % | |
| ALs with hospice residents | 11 | 52.38 | 17 | 70.83 |
| Frequency of hospice use | ||||
| 0 residents | 10 | 47.6 | 7 | 29.2 |
| 1-5 resident | 4 | 19.0 | 2 | 8.3 |
| 6 or more residents | 7 | 33.4 | 15 | 62.5 |
Note. Direct care staff training attendance was collected in six categories: 0%, 1% to 19%, 20% to 39%, 40% to 59%, 60% to 79%, and 80% to 100% and then split into two groups, high = 60% to 100% and low = 0% to 59%; 13 facilities were assigned a rate of 0% attendance as they reported that they do not offer training. Resident hospice use data are for the 3 months prior to data collection; AL census and capacity data are from the time of data collection. AL = assisted living.
The facilities deemed ineligible (n = 31) consisted of three adult care facilities, four ALs that were missing data on percentage of staff trained and 24 ALs that were licensed for less than 17 beds. The census of ineligible facilities ranged from no residents through 100 residents (M = 11.58, SD = 24.93) and a range in capacity from four through 100 resident beds (M = 17.32, SD = 26.37).
Measures
The pilot study data were obtained from the cross-sectional survey completed by AL directors (n = 45) on relevant measures for this current study. The survey question relevant to AL resident hospice use outcome in the pilot study questionnaire was measured using the question: “In the last 3 months, how many times was hospice brought in specifically so a resident would not have to be transferred?” The values were calculated as a continuous variable. The percentage of direct care staff trained in end-of-life care was measured using the following question: “Do you offer training for direct care staff on caring for terminally ill or dying residents?” and “If yes, in the last year, what percentage of your current staff has received training for terminally ill or dying residents?” The percentage of trained direct care staff was collected through the survey as a choice of six categories: 0%, 1% to 19%, 20% to 39%, 40% to 59%, 60% to 79%, and 80% to 100%. There was 0% attendance for 13 facilities that indicated that they did not offer end-of-life training for their direct care staff, but did not answer the latter question. The percentage groups were collapsed into two groups representing low (0 ≤ 59%) and high (60 ≤ 100%) percentages of direct care staff trained in end-of-life care.
AL capacity was reported through the question, “How many residential care/AL beds does this AL have overall, and how many are occupied today?” Profit status was reported according to the question, “Is your AL facility’s ownership for profit, not-for-profit, or government?”
Analyses
First, descriptive statistics were conducted. Second, chi-square tests and t tests were conducted to compare the AL organizational size and profit status by the dichotomous groups of high and low percentage of direct care staff trained in end-of-life care. Finally, zero-inflated negative binomial regression (ZINB) was used to examine the relationship between the counts of resident utilization of hospice care and the percentage of direct care staff trained in end-of-life care while controlling for AL capacity and profit status. All statistical analyses were performed using IBM SPSS Statistics 22.
Results
ZINB regression analysis proved to be an appropriate test for these data, β = 1.493, confidence interval (95% CI) = 0.811, 2.748. The likelihood ratio for the ZINB model was significant indicating the overall model is statistically significant, χ2(3) = 8.778, p = .032. The ZINB regression model was significant, χ2(1) = 8.344, p = .004. The percentage of AL direct care staff trained in end-of-life care can be used to predict the number of residents who utilize hospice. ZINB regression indicated that ALs with ≥60% direct care staff trained in end-of-life care are associated with 3.64% greater utilization of hospice by their residents than in ALs with a low percentage of trained direct care staff. Figure 2 depicts the mean number of AL residents who utilized hospice, and the ZINB regression analysis predicted mean values according to the percentage of direct care staff trained in end-of-life care.
Figure 2.
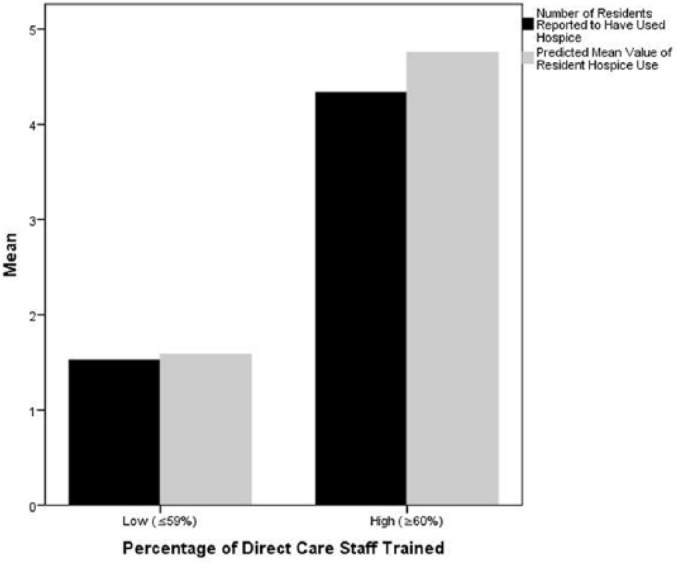
Contrast in resident hospice utilization of the mean reported number and the mean predicted number of assisted living residents who utilized hospice and the percentage of direct care staff trained in end-of-life care.
Discussion
This study contributes to the limited knowledge of empirical studies in the area of AL end-of-life care and staff training. The analyses in this study showed that AL resident hospice use was associated with the percentage of direct care staff trained in end-of-life care. These study findings suggest that ALs who have a higher percentage of staff who participated in an end-of-life training programs potentially could increase the use of hospice care by their residents. Hospice services are considered by most experts in the field of palliative care as the gold standard of end-of-life care services. The findings in this study are consistent with other research that has shown a relationship between direct care staff training and improved end-of-life care with the use of hospice (Meier, 2011). Munn et al. (2006) also showed that with end-of-life care training, AL direct care staff will be able to better recognize and report residents who could benefit from a referral to hospice.
Limitations
There were some study limitations. The 45 sample ALs from one state (Florida) is not generalizable to the larger U.S. population. Florida is unique in the delivery of hospice with its use of the Certificate of Need requirement, therefore, the state has large hospices, some as large as 1,000 patients per day for a daily census. There is also lack of information about the content of the training. Future studies should consider the collection of multistate data on training delivery, length, frequency, curriculum, and outcome measures over time to develop best practices for equivalent training requirements throughout the country . Conducting a more inclusive multistate longitudinal study would be most beneficial as it is important to states with different guidelines and practices. Another limitation would be due to administrator report of hospice use over a 3-month period. One possibility to best account for hospice utilization is to merge Medicare hospice claims data with selected state sources of AL data as it has been done in other studies (Meng et al., 2013).
Conclusion
The Institute of Medicine’s report on Dying In America recommends nonphysician direct care workers to have evidence-based educational programs available to them so as to be equipped to provide quality of end-of-life care (Institute of Medicine, 2014). The results from this small pilot study data are encouraging related to end-of-life care training and the increase in hospice use. AL communities will continue to serve an increasingly large portion of the older adult population in need of end-of-life care. The direct care workforce who cares for this older adult population needs to be prepared to provide end-of-life and palliative care. Given the growing demand for end-of-life care in ALs, the regulation of requiring some type of educational program related to providing care for the terminally ill for direct care staff as is done in some states with competency evaluations by a nurse or hospice agency should become a common practice for all states (Carder et al., 2015). Because hospice care is widely accepted as the gold standard for end-of-life care for dying persons, any end-of-life educational program should incorporate information about hospice as a key resource for residents in need of this type of care.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a University of South Florida New Researcher Award (Dobbs, PI).
References
- Carder P., O’Keeffe J., O’Keeffe C. (2015). Compendium of residential care and assisted living regulations and policy. Washington, DC: U.S. Department Health and Human Services. [Google Scholar]
- Cartwright J. C., Miller L., Volpin M. (2009). Hospice in assisted living: Promoting good quality care at end of life. The Gerontologist, 49, 508-516. doi: 10.1093/geront/gnp038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbs D. (2011). Hospice and palliative care practices in residential care facilities in Florida. Tampa, FL: University of South Florida: Florida Policy Exchange Center on Aging. [Google Scholar]
- Goddard C., Stewart F., Thomson G., Hall S. (2013). Providing end-of-life care in care homes for older people: A qualitative study of the views of care home staff and community nurses. The Journal of Applied Gerontology, 32, 76-95. doi: 10.1177/0733464811405047 [DOI] [PubMed] [Google Scholar]
- Hanson L. C., Reynolds K. S., Henderson M., Pickard C. G. (2005). A quality improvement intervention to increase palliative care in nursing homes. Journal of Palliative Medicine, 8, 576-584. doi: 10.1089/jpm.2005.8.576 [DOI] [PubMed] [Google Scholar]
- Holup A., Dobbs D., Temple A., Hyer K. (2014). Going digital: adoption of electronic health records in assisted living facilities. The Journal of Applied Gerontology, 33(4), 494-504. doi: 10.1177/0733464812454009 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Keay T. J., Alexander C., McNally K., Crusse E., Eger R. E. (2003). Nursing home physician educational intervention improves end-of-life outcomes. Journal of Palliative Medicine, 6(2), 205-213. doi: 10.1089/109662103764978452 [DOI] [PubMed] [Google Scholar]
- Knapp C., Thompson L. (2012). Factors associated with perceived barriers to pediatric palliative care: A survey of pediatricians in Florida and California. Palliative Medicine, 26, 268-274. doi: 10.1177/0269216311409085 [DOI] [PubMed] [Google Scholar]
- Meier D. E. (2011). Increased access to palliative care and hospice services: Opportunities to improve value in health care. Milbank Quarterly, 89, 343-380. doi: 10.1111/j.1468-0009.2011.00632.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng H., Dobbs D., Wang S., Hyer K. (2013). Hospice use and public expenditures at the end of life in assisted living residents in a Florida Medicaid waiver program. Journal of the American Geriatrics Society, 61(10), 1777-1781. doi: 10.1111/jgs.12459 [DOI] [PubMed] [Google Scholar]
- Munn J. C., Hanson L. C., Zimmerman S., Sloane P. D., Mitchell C. M. (2006). Is hospice associated with improved end-of-life care in nursing homes and assisted living facilities? Journal of the American Geriatrics Society, 54, 490-495. doi: 10.1111/j.1532-5415.2005.00636.x [DOI] [PubMed] [Google Scholar]
- Munn J. C., Dobbs D., Meier A., Williams C. S., Biola H., Zimmerman S. (2008). The end-of-life experience in long-term care: Five themes identified from focus groups with residents, family members, and staff. The Gerontologist, 48(4), 485-494. doi: 10.1093/geront/48.4.485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHPCO Facts and Figures: Hospice Care in America National Hospice and Palliative Care Organization. (2017). Alexandria, VA: National Hospice and Palliative Care Organization. [Google Scholar]
- Sloane P. D., Zimmerman S., Hanson L. C., Mitchell C. M., Riedel-Leo C., Custis-Buie V. (2003). End-of-life care in assisted living and related residential care settings: Comparison with nursing homes. Journal of the American Geriatrics Society, 51, 1587-1594. doi: 10.1046/j.1532-5415.2003.51511.x [DOI] [PubMed] [Google Scholar]
- Torpy J. M., Burke A., Golub R. M. (2012). Hospice care. The Journal of the American Medical Association, 308(2), 200. doi: 10.1001/jama.2012.6210 [DOI] [PubMed] [Google Scholar]
- Wilson K. B. (1996). Assisted living: Reconceptualizing regulation to meet consumers’ needs and preferences. Washington, DC: American Association of Retired Persons. [Google Scholar]
- Zimmerman S., Sloane P. D., Eckert J. K., Gruber-Baldini A. L., Morgan L. A., Hebel J. R., . . . Chen C. K. (2005). How good is assisted living? Findings and implications from an outcomes study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60(4), S195-S204. doi: 10.1093/geronb/60.4.S195 [DOI] [PubMed] [Google Scholar]



