Abstract
Shigella represents one of the major diarrhea-inducing pathogens threatening public health, but its prevalence and antimicrobial resistance profile in Xinjiang Uygur Autonomous region, China, remains unclear. We conducted comprehensive investigation of Shigella serotype distribution and antimicrobial resistance pattern in Xinjiang, identifying 458 Shigella isolates between 2008 to 2014. Shigella flexneri was identified as predominant species, and several S. flexneri serotypes were isolated, including atypical serotypes 1c, 2c, and 4s. Dominant S. flexneri serotypes were 2a, 1b, 2b, and Xv, different from those generally dominant in China. A hybrid serotype pattern was observed, which included the major Chinese serotypes (2a, Xv) and those predominant in Pakistan (1b, 2b). Shigella sonnei was shown to have a lower frequency compared with that generally observed in China, but an increasing trend of infections associated with this pathogen was observed. Furthermore, a high frequency of drug resistance and different Shigella antimicrobial resistance patterns were demonstrated as well, including very severe resistance phenotypes, such as multidrug resistance and resistance to frontline antibiotics. Seventy-five cephalosporin-resistant Shigella isolates were frequently identified with the resistance determinants that can undergo horizontal transfer, such as blaOXA, blaTEM, blaCTX-M, and integrons, facilitating the development of cephalosporin resistance among Shigella subtypes. Additionally, genetic analyses demonstrated that all 86 quinolone-resistant S. flexneri isolates possess 3–4 mutation sites in quinolone resistance-determining regions, primarily contributing to their resistance to quinolone. However, S. sonnei isolates were not shown to be quinolone resistant. Co-resistance to cephalosporins and quinolones was detected in 17 S. flexneri isolates, and these isolates were additionally multidrug resistant and carried β-lactamase genes and quinolone-resistance determinants. As is demonstrated in this study, dominant serotypes of Shigella were distributed in unique trend with dangerous drug resistance patterns. Novel strategies are urgently required to prevent the development of drug resistance among diarrhea-inducing pathogens.
Introduction
Shigella spp. are recognized as important causative agents of diarrheal diseases in humans [1–4]. Shigella infections are considered the major public health burden worldwide, especially in the undeveloped and developing countries, and regions with poor sanitary conditions, with an estimated 167 million cases and about 1 million deaths annually; [5], and children under five are the most affected group [6]. Despite the improvements in economic and health conditions, shigellosis remains one of the top four notifiable infectious diseases, with half a million cases in China [7–9].
Shigella genus comprises four species, including Shigella flexneri, Shigella dysenteriae, Shigella boydii, and Shigella sonnei [10], and the distribution of these species and their serotypes shows distinct regional variations. S. flexneri has primarily been the epidemic species, caused diarrhea in developing countries, while S. sonnei has been prevalent in the developed countries [11]. However, S. sonnei prevalence has demonstrated an increasing trend in some Asian countries recently [12–15], together with the economic development. Furthermore, several serologically atypical isolates of S. flexneri were identified in recent studies [16–18], and these Shigella subgroup and serotype variations may lead to difficulties in the prevention and treatment of Shigella infection. The emergence and dissemination of antimicrobial resistance (AMR) aggravate Shigella prevalence. A trimethoprim/sulfamethoxazole-resistant Shigella isolate was first reported in Japan [19,20], followed by the emergence of diverse resistant Shigella types [21,22]. Previous studies reported a frequent resistance to some of the commonly used antibiotics, such as ampicillin and tetracyclines, worldwide [23–25]. Recently, the resistance to quinolones and cephalosporins was reported as well [12,26]. China is currently facing an increased risk of AMR dissemination among different types of intestinal pathogens. The antibiotic-resistant Shigella isolates have been identified throughout China [1,7,16,26], aggravating the challenges associated with the treatment and prevention of shigellosis.
As a region located in northwestern China, Xinjiang is bordered by eight countries. Historically, an important trading route, the ancient Silk Road, passed through Xinjiang, leading to the trans-regional migration of different populations. Today, increased contacts between China and other Asian or European countries, due to the proposed development of the Belt and Road, will occur through Xinjiang once more (http://hkmb.hktdc.com/en/1X0A5D5S/hktdc-research/Xinjiang-A-Core-Component-of-Belt-and-Road). The increase in the human economic activity may allow faster dissemination of infectious diarrhea pathogens and AMR. Additionally, a comprehensive survey of locally-present infectious pathogens is important to maintain the biosecurity of fast-growing economies. However, the prevalence and characterization of Shigella in Xinjiang has not been thoroughly analyzed before [27,28]. To improve the prevention and treatment of potential future Shigella epidemics, we performed detailed analyses of the prevalence and AMR patterns of Shigella isolates in Xinjiang, China. We analyzed the variations in Shigella species and serotype trends, characterized the AMR profile of these strains, and identified dominant antibiotic-resistant determinants of these isolates.
Material and methods
Bacterial isolation and Shigella serotyping
During routine surveillance of bacillary dysentery, fecal samples were collected from patients with diarrhea between 2008 and 2014 in Xinjiang. To isolate Shigella strains, the samples were directly streaked on Salmonella-Shigella agar (SS agar) (Beijing Land Bridge Technology CO., LTD, China) and incubated at 37°C for 16–22 h. The resultant Shigella-like colonies were steaked on the SS agar again and continually incubated at 37°C for 16–22 h. Following the second incubation, Shigella colonies were picked and streaked on Luria-Bertani agar plates, followed by incubation at 37°C for 16–22 h, after which these isolates were identified with API 20E test strips (bioMérieux SA, Marcy l’Etoile, France), according to the manufacturer’s instructions. The serotyping of Shigella isolates was performed using Shigella Antisera (Denka Seiken, Tokyo, Japan) and monoclonal antibody reagents (MASF IV-1 and MASF IV-2, Reagensia AB, Stockholm, Sweden). Written informed consents were obtained from patients or their guardians. All experiments were approved and authorized by the Ethics Committees of the Institute of Disease Prevention and Control, People’s Liberation Army, China.
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was performed using the automated broth microdilution (Sensititre; Thermo Fisher Scientific, USA). Minimum inhibitory concentrations (MICs) of 21 antimicrobial agents were determined, including those of piperacillin, ampicillin, ticarcillin, ticarcillin/clavulanic acid, ceftazidime, ceftriaxone, cefepime, cefoperazone, cefazolin, cefoxitin, imipenem, nitrofurantoin, levofloxacin, norfloxacin, tetracycline, tobramycin, gentamicin, amikacin, aztreonam, chloramphenicol, and trimethoprim/sulfamethoxazole. Each isolate was identified as resistant or susceptible to each antibiotic, according to the cut-offs defined by the Clinical and Laboratory Standards Institute (CLSI 2017) [29]. Escherichia coli ATCC 25922 strain was used as the susceptible control strain.
Detection of AMR determinants and integrons
Total DNA was extracted from all Shigella isolate using the TIANamp Bacterial DNA kit (Tiangen Biotech, Beijing, China). β-lactamase genes (blaCTX-M, blaTEM, blaOXA, blaVIM and blaNDM) [30–32], quinolone resistance-determining regions (QRDRs) (gyrA, gyrB, parC, and parE) [32], plasmid-mediated quinolone resistance (PMQR) genes (qnrA, qnrB, qnrD, qnrS, and aac(6’)-Ib-cr) [31–33], and the variable regions of class 1 and class 2 integrons [34,35] were screened using PCR and the primers listed in S1 Table. The resulting PCR products were sequenced by BGI, Beijing, China, and the obtained data were edited using DNAstar (DNAstar Inc., Madison, WI, USA) and analyzed using Basic Local Alignment Search Tool in NCBI.
Statistical analysis
Differences in the AMR rates and the frequency of AMR determinants between Shigella species were analyzed using χ2 test. Variations in Shigella prevalence with time were analyzed using linear regression. All statistical analyses were performed using Graph Pad 7.0 software, and P < 0.05 was considered statistically significant.
Results
Identification of isolates and distribution of Shigella spp
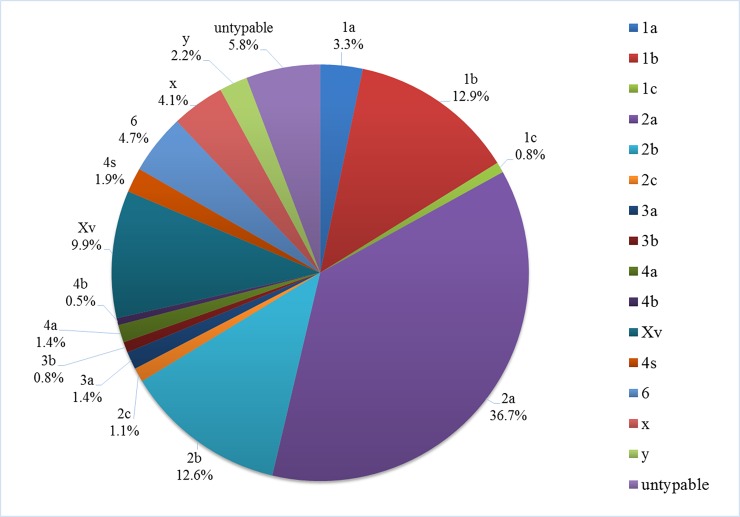
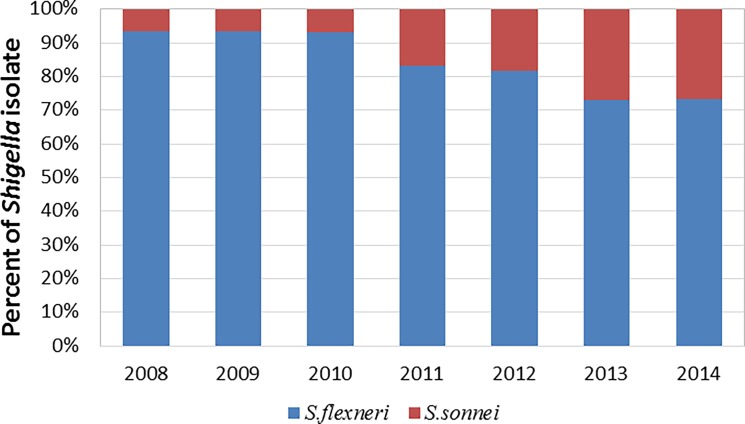
All Shigella isolates in our study were collected from sentinel hospitals in 12 cities or prefectures (Urumqi, Karamay, Kashgar Prefecture, Aksu Prefecture, Hotan Prefecture, Turpan Prefecture, Hami Prefecture, Tacheng Prefecture, Altay Prefecture, Bortala Mongol Autonomous Prefecture, Changji hui autonomous prefecture, Bayingolin Mongol Autonomous Prefecture, Ili Kazakh Autonomous Prefecture). Among all cases, male patient accounted for 55.0%, female accounted for 45.0%; children or teenagers under 18 accounted for 32.9%, adult accounted for 67.1%. In total, we collected 458 Shigella isolates between 2008 and 2014 (Table 1). Of these, 365 (79.7%) were identified as S. flexneri isolates, and 93 (20.3%) were identified as S. sonnei isolates. S. boydii and S. dysenteriae presence was not detected. All collected S. flexneri isolates belonged to one of at least 16 serotypes (Fig 1), while serotype 2a (134, 36.7%) was identified as the major S. flexneri serotype detected during 7 years of surveillance, followed by 1b (47, 12.9%), 2b (46, 12.6%), and Xv (36, 9.9%) (Fig 1). Some atypical serotypes were identified, including three 1c isolates, four 2c isolates, and seven 4s isolates. Consistently, S. flexneri was shown to be the dominant Shigella species every year, while S. sonnei isolates accounted for less than 30% of samples (Fig 2). However, we observed a change in this trend, with the percentage of S. sonnei among the isolates showing the tendency to increase with time (linear regression analysis, P < 0.05) (S1 Fig). S. sonnei species, together with the dominant S. flexneri serotypes (2a, 1b, 2b, and Xv), were shown to constitute the majority of Shigella isolates in Xinjiang, with the frequency of above 70% each year (Table 1).
Table 1. The prevalence of Shigella in Xinjiang between 2008 and 2014.
| Species/ serotype | Number (%) of isolates | |||||||
|---|---|---|---|---|---|---|---|---|
| 2008 (n = 15) |
2009 (n = 46) |
2010 (n = 30) |
2011 (n = 41) |
2012 (n = 91) |
2013 (n = 150) |
2014 (n = 85) |
Total (n = 458) |
|
| S. flexneri | 14 (93.3%) | 43 (93.5%) | 28 (93.3%) | 34 (82.9%) | 75 (82.4%) | 109 (72.7%) | 62 (72.9%) | 365 (79.7%) |
| 1a | 0 | 0 | 2 (6.7%) | 1 (2.4%) | 3 (3.3%) | 5 (3.3%) | 1 (1.2%) | 12 (2.6%) |
| 1b | 3 (2) | 3 (6.5%) | 7 (23.3%) | 7 (17.1%) | 6 (6.6%) | 13 (8.7%) | 8 (9.4%) | 47 (10.3%) |
| 1c | 0 | 1 (2.2%) | 2 (6.7%) | 0 | 0 | 0 | 0 | 3 (0.7%) |
| 2a | 5 (33.3%) | 26 (56.5%) | 6 (20%) | 15 (36.6%) | 22 (24.2%) | 37 (24.7%) | 23 (27.1%) | 134 (29.3%) |
| 2b | 2 (13.3%) | 4 (8.7%) | 5 (16.7%) | 7 (17.1%) | 8 (8.8%) | 15 (10%) | 5 (5.9%) | 46 (10.0%) |
| 2c | 0 | 0 | 0 | 1 (2.4%) | 1 (1.1%) | 2 (1.3%) | 0 | 4 (0.9%) |
| 3a | 1 (6.7%) | 1 (2.2%) | 0 | 2 (4.9%) | 0 | 0 | 1 (1.2%) | 5 (1.1%) |
| 3b | 0 | 0 | 0 | 0 | 1 (1.1%) | 1 (0.7%) | 1 (1.2%) | 3 (0.7%) |
| 4a | 0 | 0 | 0 | 0 | 1 (1.1%) | 2 (1.3%) | 2 (2.4%) | 5 (1.1%) |
| 4b | 0 | 0 | 0 | 0 | 0 | 2 (1.3%) | 0 | 2 (0.4%) |
| Xv | 2 (13.3%) | 0 | 2 (6.7%) | 1 (2.4%) | 13 (14.3%) | 9 (6.0%) | 9 (10.6%) | 36 (7.9%) |
| 4s | 0 | 0 | 0 | 0 | 0 | 7 (4.7%) | 0 | 7 (1.5%) |
| 6 | 0 | 1 (2.2%) | 1 (3.3%) | 0 | 3 (3.3%) | 7 (4.7%) | 5 (5.9%) | 17 (3.7%) |
| x | 1 (6.7%) | 1 (2.2%) | 1 (3.3%) | 0 | 4 (4.4%) | 6 (4.0%) | 2 (2.4%) | 15 (3.3%) |
| y | 0 | 1 (2.2%) | 0 | 0 | 5 (5.5%) | 1 (0.7%) | 1 (1.2%) | 8 (1.7%) |
| Untypable | 0 | 5 (10.9%) | 2 (6.7%) | 0 | 8 (8.8%) | 2 (1.3%) | 4 (4.7%) | 21 (4.6%) |
| S. flexneri 2a, 1b, 2b and Xv | 12 (80.0%) | 33 (71.7%) | 20 (66.7%) | 30 (73.2%) | 49 (53.8%) | 74 (49.3%) | 45 (52.9%) | 263 (57.4%) |
| S. sonnei | 1 (6.7%) | 3 (6.5%) | 2 (6.7%) | 7 (17.1%) | 16 (17.6%) | 41 (27.3%) | 23 (27.1%) | 93 (20.3%) |
| S. sonnei+ S. flexneri 2a, 1b, 2b and Xv | 13 (86.7%) | 36 (78.3%) | 22 (73.3%) | 37 (90.2%) | 65 (71.4%) | 115 (76.7%) | 68 (80.0%) | 356 (77.7%) |
Fig 1. S. flexneri serotype distribution.
Our analyses showed that 2a serotype was the most frequent among 19 identified serotypes. Serotype 2a, 2b, 1b, Xv represent the dominant serotypes, while others were rarely detected.
Fig 2. Trends in Shigella prevalence in isolates collected in Xinjiang between 2008 and 2014.
Variations in the frequencies of S. flexneri and S. sonnei with time are presented. In each column, frequencies of S. flexneri and S. sonnei are shown.
Shigella AMR in Xinjiang
Antimicrobial susceptibility testing demonstrated that S. flexneri isolates are frequently resistant to ampicillin (94.0%), followed by the resistance to ticarcillin (92.9%), tetracycline (88.8%), chloramphenicol (87.7%), and trimethoprim/sulfamethoxazole (44.4%) (Table 2). Additionally, S. flexneri isolates showed a significantly higher resistance to several antimicrobials, including ceftazidime, levofloxacin, norfloxacin, ampicillin, ticarcillin, chloramphenicol, and ticarcillin/clavulanic acid, compared with that observed for the S. sonnei strains (χ2 analysis, P < 0.05). Furthermore, 57 (15.6%) S. flexneri isolates were shown to be resistant to cephalosporins, including cefazolin (15.3%), ceftriaxone (14.5%), cefoperazone (12.3%), ceftazidime (2.2%), and cefoxitin (0.5%). Moreover, 86 (23.6%) quinolone-resistant S. flexneri isolates (norfloxacin, 23.6%; levofloxacin, 8.5%) were detected in Xinjiang.
Table 2. Antimicrobial resistance of Shigella isolates recovered from patients with diarrhea in Xinjiang, China between 2008 and 2014.
| Antimicrobial agents | Total (n = 458) |
S. flexneri (n = 365) |
S. sonnei (n = 93) |
χ2 | P | |||
|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | |||
| Cephems | ||||||||
| FEP | 0 | 0 | 0 | 0 | 0 | 0 | / | / |
| FOX | 2 | 0.4 | 2 | 0.5 | 0 | 0 | 0.5118 | P = 0.4744 |
| CAZ | 8 | 1.7 | 8 | 2.2 | 0 | 0 | 8.601, | P = 0.0034 |
| CFP | 63 | 13.8 | 45 | 12.3 | 18 | 19.4 | 3.084 | P = 0.0791 |
| CRO | 53 | 11.6 | 53 | 14.5 | 18 | 19.4 | 1.322 | P = 0.2502 |
| CFZ | 74 | 16.2 | 56 | 15.3 | 18 | 19.4 | 0.8808 | P = 0.3480 |
| Fluoroquinolones | ||||||||
| LEV | 31 | 6.8 | 31 | 8.5 | 0 | 0 | 8.472 | P = 0.0036 |
| NOR | 86 | 18.8 | 86 | 23.6 | 0 | 0 | 26.98 | P < 0.0001 |
| Carbapenems | ||||||||
| IMP | 0 | 0.0 | 0 | 0 | 0 | 0 | / | / |
| Penicillins | ||||||||
| PIP | 66 | 14.4 | 45 | 12.3 | 21 | 22.6 | 6.316 | P = 0.0120 |
| TIC | 399 | 87.1 | 339 | 92.9 | 60 | 64.5 | 53.12 | P < 0.0001 |
| AMP | 403 | 88.0 | 343 | 94 | 60 | 64.5 | 60.86 | P < 0.0001 |
| Aminoglycosides | ||||||||
| AK | 1 | 0.2 | 1 | 0.3 | 0 | 0 | 0.2554 | P = 0.6133 |
| TO | 11 | 2.4 | 9 | 2.5 | 2 | 2.1 | 0.03142 | P = 0.8593 |
| GN | 57 | 12.4 | 16 | 4.4 | 41 | 44.1 | 107.2 | P < 0.0001 |
| Monobactams | ||||||||
| ATM | 33 | 7.2 | 18 | 4.9 | 15 | 16.1 | 13.9 | P = 0.0002 |
| Nitrofurans | ||||||||
| NIT | 0 | 0.0 | 0 | 0 | 0 | 0 | / | / |
| Tetracyclines | ||||||||
| TE | 407 | 88.9 | 324 | 88.8 | 83 | 89.2 | 0.01727 | P = 0.8954 |
| Phenicols | ||||||||
| C | 322 | 70.3 | 320 | 87.7 | 2 | 2.1 | 259.7 | P < 0.0001 |
| β-Lactam/β-lactamase inhibitor combinations | ||||||||
| TIM | 35 | 7.6 | 34 | 9.3 | 1 | 1.1 | 7.13 | P = 0.0076 |
| Folate pathway inhibitors | ||||||||
| SXT | 249 | 54.4 | 162 | 44.4 | 87 | 93.5 | 72.21 | P < 0.0001 |
AK, amikacin; AMP, ampicillin; ATM, aztreonam; CFZ, cefazolin; FEP, cefepime; CFP, cefoperazone; FOX, cefoxitin; CAZ, ceftazidime; CRO, ceftriaxone; C, chloramphenicol; GEN, gentamicin; IPM, imipenem; LEV, levofloxacin; NIT, nitrofurantoin; NOR, norfloxacin; PIP, piperacillin; SXT, trimethoprim/sulfamethoxazole; TE, tetracycline; TIC, ticarcillin; TIM, ticarcillin/clavulanic acid; TO, tobramycin.
In contrast, S. sonnei species was shown to be the most resistant to trimethoprim/sulfamethoxazole (93.5%), followed by the resistance to tetracycline (89.2%), ticarcillin (64.5%), ampicillin (64.5%), gentamicin (44.1%) (Table 2). Furthermore, S. sonnei showed a significantly higher resistance rates to some antibiotics, including piperacillin, gentamicin, aztreonam, and trimethoprim/sulfamethoxazole, compared with those obtained for S. flexneri isolates (χ2, P < 0.05). Additionally, S. sonnei isolates showed resistance to cephalosporins, including cefazolin (19.4%), ceftriaxone (19.4%), and cefoperazone (19.4%). None of these isolates was resistant to other cephalosporins, such as cefepime, cefoxitin, and ceftazidime, and to quinolones (levofloxacin and norfloxacin; Table 2).
Furthermore, 330 (90.4%) of 365 S. flexneri isolates and 59 (63.4%) of 93 S. sonnei isolates were shown to be multidrug resistant (MDR, resistant to three or more CLSI classes of antimicrobials) (Table 3 and S2 Table). S. flexneri species showed a significantly higher frequency of MDR than S. sonnei species (χ2, P < 0.05). S. flexneri exhibited MDR to at most 7 classes of antimicrobial and S. sonnei showed MDR to at most 5 classes of antimicrobials. Besides, there were some S. flexneri isolates with important MDR phenotypes, including 136 (37.3%) S. flexneri isolates resistant to at least ampicillin, chloramphenicol, tetracycline and trimethoprim/sulfamethoxazole; 38 (10.4%) S. flexneri isolates resistant to at least ampicillin, chloramphenicol, tetracycline, trimethoprim/sulfamethoxazole and norfloxacin; 22 (6%) S. flexneri isolates resistant to at least ampicillin, chloramphenicol, tetracycline, trimethoprim/sulfamethoxazole and ceftriaxone; 9 (2.5%) S. flexneri isolates resistant to at least ampicillin, chloramphenicol, tetracycline, trimethoprim/sulfamethoxazole, norfloxacin and ceftriaxone. Notably, these important MDR phenotypes have not been observed in S. sonnei isolates.
Table 3. Antimicrobial resistance profiles of Shigella isolates in Xinjiang between 2008 and 2014.
| Antibiotic* | Number of isolates (%) | |
|---|---|---|
| S. flexneri (n = 365) | S. sonnei (n = 93) | |
| No resistance detected | 12 (3.3) | 3 (3.2) |
| Resistant ≥ 1 CLSI class | 353 (96.7) | 90 (96.8) |
| Resistant ≥ 2 CLSI classes | 349 (95.6) | 90 (96.8) |
| Resistant ≥ 3 CLSI classes | 330 (90.4) | 59 (63.4) |
| Resistant ≥ 4 CLSI classes | 200 (54.8) | 53 (57.0) |
| Resistant ≥ 5 CLSI classes | 62 (17.0) | 14 (15.1) |
| Resistant ≥ 6 CLSI classes | 21 (5.8) | 0 |
| Resistant = 7 CLSI classes | 8 (2.2) | 0 |
| Cephalosporin | 57 (15.6) | 18 (19.4) |
| Quinolones | 86 (23.6) | 0 |
| Cephalosporin and quinolones | 17 (4.7) | 0 |
| At least ACTT/S | 136 (37.3) | 0 |
| At least ACTT/SNOR | 38 (10.4) | 0 |
| At least ACTT/SCRO | 22 (6.0) | 0 |
| At least ACTT/SCRONOR | 9 (2.5) | 0 |
*A, ampicillin; C, chloramphenicol; CRO, ceftriaxone; NOR, norfloxacin; T, tetracycline; T/S, trimethoprim/sulfamethoxazole.
Detection of AMR determinants and integrons
A total of 57 (15.6%) S. flexneri and 18 (19.4%) S. sonnei isolates showing high-level resistance to cephalosporin were selected to detect the presence of antibiotic-resistance determinant genes and integrons (Table 4). Rates of blaOXA-1, blaTEM-1, and blaCTX-M expression among the selected S. flexneri isolates were 82.5%, 61.4%, and 89.5%, respectively. Moreover, 48 S. flexneri isolates contained the CTX-M gene, including 23 (40.4%) isolates containing CTX-M-1 group genes, 29 (50.9%) isolates with CTX-M-9 group genes, and 4 (7.0%) isolates containing both group genes. No expression of blaVIM and blaNDM was observed in the tested isolates. Furthermore, the majority of tested S. flexneri isolates was shown to harbor integrons, including 49 (86.0%) isolates that were shown to harbor class 1 integrons and 51 (89.4%) that harbored class 2 integrons (Table 4). In contrast to the S. flexneri isolates, all selected S. sonnei isolates were negative for blaOXA-1 expression, while only 38.9% expressed blaTEM (Table 4). The expression rate of class 1 integrons detected in S. sonnei isolates (5.6%) was considerably lower than that in the S. flexneri isolates (86.0%), while the rate of isolates expressing class 2 integrons reached 83.3%. All 18 tested cephalosporin-resistant S. sonnei isolates were demonstrated to harbor blaCTX-M genes, including 14 (77.8%) isolates with CTX-M-1 group genes, nine (50%) isolates containing CTX-M-9 group genes, and six (33.3%) isolates carrying genes from both of these groups (Table 4). Among cephalosporin-resistant isolates, a higher frequency of isolates carrying both CTX-M-1 and CTX-M-9 group genes was detected among S. sonnei isolates, compared with that observed among S. flexneri isolates (χ2 analysis, P < 0.05).
Table 4. Antimicrobial resistance determinants in 75 cephalosporin-resistant Shigella isolates and 86 quinolone-resistant Shigella isolates.
| Resistant determinant | Number of isolates (%) | ||
|---|---|---|---|
| Determinants of cephalosporin resistance | S. flexneri (n = 57) | S. sonnei (n = 18) | Total (n = 75) |
| blaVIM | 0 | 0 | 0 |
| blaNDM | 0 | 0 | 0 |
| blaOXA | 47 (82.5) | 0 | 47 (62.7) |
| blaTEM | 35 (61.4) | 7 (38.9) | 42 (56.0) |
| blaCTX-M | 51 (89.5) | 18 (100%) | 69 (92.0) |
| CTX-M-1 group | 23 (40.4) | 14 (77.8) | 37 (49.3) |
| blaCTX-M-3 | 3 (5.3) | 0 (0) | 3 (4.0) |
| blaCTX-M-15 | 10 (17.5) | 7 (38.9) | 17 (22.7) |
| blaCTX-M-28 | 2 (3.5) | 0 (0) | 2 (2.7) |
| blaCTX-M-55 | 6 (10.5) | 7 (38.9) | 13 (17.3) |
| blaCTX-M-64 | 2 (3.5) | 0 (0) | 2 (2.7) |
| CTX-M-9 group | 29 (50.9) | 4 (22.2) | 33 (44.0) |
| blaCTX-M-14 | 26 (45.6) | 4 (22.2) | 30 (40.0) |
| blaCTX-M-24 | 3 (5.3) | 0 (0) | 3 (4.0) |
| Both CTX-M-1 and CTX-M-9 group | 4 (7.0) | 6 (33.3) | 10 (13.3) |
| intl1 | 49 (86.0) | 1 (5.6) | 50 (66.7) |
| intl2 | 51 (89.5) | 15 (83.3) | 66 (88.0) |
| hep74-51 | 49 (86.0) | 17 (94.4) | 66 (88.0) |
| Determinants of resistance to quinolones | S. flexneri (n = 86) | S. sonnei (n = 0) | Total (n = 86) |
| QRDRs mutations | 86 (100) | 0 | 86 (100) |
| gyrA | 86 (100) | 0 | 86 (100) |
| Ser83Leu | 86 (100) | 0 | 86 (100) |
| Asp87Asn | 62 (72.1) | 0 | 62 (72.1) |
| Asp87Gly | 16 (18.6) | 0 | 16 (18.6) |
| His211Tyr | 82 (95.3) | 0 | 82 (95.3) |
| gyrB | 0 | 0 | 0 |
| parE | 0 | 0 | 0 |
| parC | 86 (100) | 0 | 86 (100) |
| Ser80Ile | 86 (100) | 0 | 86 (100) |
| Triple (or more) mutations | 86 (100) | 0 | 86 (100) |
| Four mutations | 74 (86.0) | 0 | 74 (86.0) |
| PMQR genes | 3 (3.5) | 0 | 3 (3.5) |
| qnrB | 1 (1.2) | 0 | 1 (1.2) |
| qnrS | 2 (2.3) | 0 | 2 (2.3) |
| acc (6’)-Ib-cr | 0 | 0 | 0 |
Moreover, in this study, we identified 86 S. flexneri isolates resistant to quinolones (levofloxacin or norfloxacin) (Table 4). QRDR mutations were detected in three amino acids of the gyrA gene (Ser83Leu, Asp87Asn/Gly, His211Tyr) and one amino acid of the parC gene (Ser80Ile). All 86 isolates were shown to harbor Ser83Leu mutations in the gyrA and Ser80Ile in the parC genes. Additionally, 62 isolates were shown to carry Asp87Asn mutation in the gyrA gene, 16 isolates had Asp87Gly mutation in the gyrA and 82 isolates had His211Tyr mutation in the gyrA gene. No point mutations in the gyrB and parE genes were observed. All 86 quinolone-resistant isolates were identified to carry at least three types of QRDR mutations, and 74 (86.0%) isolates were shown to harbor four types of QRDR mutations. In contrast, only three isolates were shown to harbor PMQR gene mutations (one in qnrB, two in qnrS), and no isolates were positive for acc(6′)-Ib-cr.
Notably, 17 Shigella isolates were resistant to cephalosporins and quinolones simultaneously (Table 5), and these were the MDR S. flexneri strains. Other than the resistance to cephalosporins and quinolones, the resistance to penicillins (17, 100%) was one of the most frequent types of resistance, followed by the resistance to tetracyclines (16, 94.1%), amphenicols (15, 88.2%), folate pathway inhibitors (13, 76.5%), and monobactams (6, 35.3%). Molecular analysis of the resistance determinants in 17 isolates, demonstrated the expression of blaOXA-1 in 16 isolates, blaTEM-1 in 14 isolates, and blaCTX-M in 15 isolates. Quinolone resistance of all 17 isolates was shown to be mediated by the mutations in QRDRs of gyrA and parC, since no isolate was shown to have PMQR gene mutations. Integrons and gene cassette arrays were identified in a number of isolates, including 17 isolates shown to carry integrons, 16 isolates with class 1 integrons, and 16 with class 2 integrons.
Table 5. Antimicrobial resistance profiles and resistance determinants of 17 Shigella isolates co-resistant to cephalosporin and quinolone.
| Isolate | Antimicrobial resistance profile | β-Lactamases gene | QRDRs mutation | PMQR gene | Integron | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| blaOXA-1 | blaTEM-1 | blaCTX-M | gyrA | parC | qnrB/qnrS | IntI1 | IntI2 | hep74-51 | ||
| XJSF20 | CRO/CFZ/TIC/AMP/NOR/TE/C/STX | + | + | blaCTX-M-15 | S83L, D87N, H211Y | S80I | - | + | + | + |
| XJSF22 | CRO/CFP/CFZ/TIC/AMP/PIP/NOR/TE/ATM/C/STX | + | + | blaCTX-M-55 | S83L, D87G, H211Y | S80I | - | + | + | + |
| 2010048 | CRO/CFP/CFZ/TIC/AMP/PIP/NOR/TE/ATM/C/STX | + | + | blaCTX-M-55 | S83L, D87N, H211Y | S80I | - | + | + | + |
| 2011109 | CRO/CFP/CFZ/TIC/TIM/AMP/PIP/NOR/GN/TE/ATM/C/STX | + | + | blaCTX-M-55 | S83L, D87G, H211Y | S80I | - | + | + | + |
| 2012064 | CAZ/CRO/CFP/CFZ/TIC/AMP/NOR/TE/C | + | + | blaCTX-M-15 | S83L, D87G, H211Y | S80I | - | + | + | + |
| 2012076 | CRO/CFP/CFZ/TIC/TIM/AMP/PIP/LEV/NOR/TE/ATM/C/STX | + | + | blaCTX-M-15 | S83L, H211Y | S80I | - | + | + | + |
| 2012085 | CFZ/TIC/TIM/AMP/NOR/TE/C/STX | + | + | - | S83L, D87N, H211Y | S80I | - | + | + | + |
| 2012131 | CRO/CFP/CFZ/TIC/AMP/PIP/NOR/TE/ATM/C | + | + | blaCTX-M-55 | S83L, D87G, H211Y | S80I | - | + | + | + |
| 2012136 | CRO/CFP/CFZ/TIC/TIM/AMP/PIP/LEV/NOR/C | + | + | blaCTX-M-14 | S83L, D87N, H211Y | S80I | - | + | + | + |
| 2012262 | CRO/CFP/CFZ/TIC/TIM/AMP/PIP/NOR/TE/C | + | + | - | S83L, D87G, H211Y | S80I | - | + | + | + |
| 2013269 | CAZ/CRO/CFP/CFZ/TIC/TIM/AMP/PIP/LEV/NOR/TE/ATM/C/STX | + | + | blaCTX-M-15 | S83L, D87N, H211Y | S80I | - | + | + | + |
| 2013398 | CRO/CFP/CFZ/TIC/TIM/AMP/PIP/LEV/NOR/GN/TE/C/STX | + | + | blaCTX-M-14 | S83L, H211Y | S80I | - | + | + | + |
| 2013416 | CRO/CFP/CFZ/TIC/AMP/PIP/NOR/TE/ATM/C/STX | + | + | blaCTX-M-14, 64 | S83L, D87N, H211Y | S80I | - | + | + | + |
| 2014104 | CRO/CFP/CFZ/TIC/AMP/PIP/LEV/NOR/GN/TE/ATM/STX | - | - | blaCTX-M-15 | S83L, D87N, H211Y | S80I | - | + | - | - |
| 2014331 | CRO/CFP/CFZ/TIC/AMP/PIP/NOR/TE/ATM/C/STX | + | + | blaCTX-M-15 | S83L, D87N, H211Y | S80I | - | + | + | + |
| 2014351 | CRO/CFZ/TIC/AMP/LEV/NOR/TE/C/STX | + | - | blaCTX-M-14 | S83L, H211Y | S80I | - | - | + | + |
| 2014366 | CRO/CFZ/TIC/AMP/LEV/NOR/TE/C/STX | + | - | blaCTX-M-15 | S83L, D87N, H211Y | S80I | - | + | + | + |
AK, amikacin; AMP, ampicillin; ATM, aztreonam; CFZ, cefazolin; FEP, cefepime; CFP, cefoperazone; FOX, cefoxitin; CAZ, ceftazidime; CRO, ceftriaxone; C, chloramphenicol; GEN, gentamicin; IPM, imipenem; LEV, levofloxacin; NIT, nitrofurantoin; NOR, norfloxacin; PIP, piperacillin; SXT, trimethoprim/sulfamethoxazole; TE, tetracycline; TIC, ticarcillin; TIM, ticarcillin/clavulanic acid; TO, tobramycin.
Discussion
Here, we demonstrated that the most frequent species of Shigella genus in Xinjiang in all years of our study was S. flexneri. Recently, the S. sonnei has shown increasing prevalence in China and even become the dominant species in southeast and central parts of China [36]. Furthermore, together with the economic growth in Xinjiang, an obvious rising trend in S. sonnei infections can be observed. The frequency of identified S. sonnei isolates altered from 6.7% in 2008 to 27.1% in 2014, which was, even considering the increase, shown to be below the average frequency of S. sonnei infections registered in China, where it was the dominant Shigella species (58.2% in 2011–2013) [36]. Various studies have concluded that S. sonnei prevalence increase with economic development [37]. As Xinjiang will continue to enhance its level of economy and sanitation, it is likely that S. sonnei species would become even more of a local public health concern. The design of vaccine candidate and shigellosis prevention strategy should consider this change of Shigella epidemics.
Considering serotypes, 2a and Xv were reported to be dominant S. flexneri serotypes in China [36], and 2a was reported to be dominant S. flexneri serotype in Xinjiang [27]. However, the results of our study further demonstrated that 2a serotype was still the most prevalent in Xinjiang but Xv serotype accounted for a smaller proportion of S. flexneri isolates, while 2a, 1b, 2b, and Xv represent the dominant serotypes detected between 2008 and 2014. Serotypes 1b and 2b are less frequent in China [36], but common in Pakistan [38], a country bordering Xinjiang. Therefore, the dominant S. flexneri serotypes distributed in Xinjiang likely represent the mixture of the major serotypes in China and adjacent countries.
Furthermore, we detected atypical serotypes 1c, 2c, and 4s in Xinjiang. Serotype-based vaccines are currently under development, as a promising strategy against Shigella epidemics [39]. A future Shigella vaccine potentially applied in Xinjiang should be developed in accordance considering the characteristic Shigella serotypes in this region, and future surveillance studies in Xinjiang should pay close attention not only to the newly emerged serotypes but the predominant subgroups in surrounding regions as well, in order to prevent potential Shigella epidemics caused by bacteria with novel or imported O-antigen types.
Shigella isolates demonstrated high levels of resistance to antibiotics. Both S. flexneri and S. sonnei revealed high AMR rate to some common used antibiotics like penicillins and tetracyclines. Thus, these older-generation drugs should not be contained in empirical therapy of shigellosis. Notably, 330 of 365 S. flexneri isolates and 59 of 93 S. sonnei isolates collected from Xinjiang showed MDR profiles. The high-level MDR frequency further restrict the choice of antibiotics in the clinical treatment of bacterial infections. Since the efficacy of older-generation antibiotics decreased due to the development of resistant strains, in a previous study, quinolones and third-generation cephalosporins were recommended as frontline antimicrobials for the empiric treatment of diarrhea-inducing pathogens [40]. However, in our study, 75 (16.38%) isolates were resistant to cephalosporin and 86 (18.77%) were resistant to norfloxacin. Additionally, 17 (3.71%) isolates were resistant to both cephalosporins and quinolones. Considering the currently used frontline antimicrobials, these resistance phenotypes threaten the effectiveness of therapy [41,42]. The mobility and dissemination of the resistant strains may increase in Xinjiang as it becomes an increasingly crucial region connecting China and other countries. Surveillance to Shigella in China revealed its high MDR frequency [7,16,17,26,43,44]. The high-level resistant pathogen could migrate along with increasing trans-regional human activities. Therefore, novel preventive strategies are urgently required to prevent the spreading of AMR among Shigella strains. Clinicians prescribing anti-infective therapies should be more cautious, since the unreasonable use of antibiotics may further accelerate the accumulation and spread of AMR [45–47].
The AMR profile differed between S. flexneri and S. sonnei strains. Specifically, S. flexneri revealed higher MDR levels, demonstrating also some specific and important MDR phenotypes. A proportion of S. flexneri strains (37.3%) was shown to be resistant to the combination of commonly used antibiotics, including ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole, which was not observed among S. sonnei isolates. Quinolone resistance and even co-resistance to cephalosporin and quinolone emerged in S. flexneri strains, while S. sonnei demonstrated the sensitivity to quinolone. As a long-term predominant species in China [48], the traditional antibiotic-associated selection of S. flexneri has been underway for decades, and by frontline antibiotics in recent years, which led to the development of the MDR strains and the resistance to cephalosporin and quinolone. Therefore, our results imply that the antibiotic therapy of choice may differ between two Shigella species. Treatment of S. flexneri infections may be more complicated than that of S. sonnei, and a drug susceptibility test should be performed immediately after diagnosing a patient with S. flexneri infection. Antibiotic abuse should be more controlled, in order to reduce the selection pressure on S. flexneri strains, but the quinolone treatment may represent a safer antibiotic choice if the infective pathogens are identified as S. sonnei.
In this study, we further elucidated the genetic background and mechanisms underlying Shigella resistance to cephalosporins and quinolones. Cephalosporin-resistant S. flexneri were shown to frequently express blaCTX-M, blaOXA, and blaTEM, three main genes conferring the resistance to cephalosporin [49,50]. All cephalosporin-resistant S. sonnei expressed blaCTX-M as well. These genes were reported to be frequently encoded by plasmids [51–55], which facilitates the horizontal transfer of resistance to β-lactamase antibiotics [49,56]. Previous studies reported that class 1 and class 2 integrons may provide the resistance to other types of drugs and be responsible for the dissemination of AMR [35,57,58]. Almost 90% of the isolated S. flexneri strains were shown to harbor two integrons. The intl2 was also frequently identified in the S. sonnei isolates (83.3%). These results indicate that the cephalosporin resistance determinants can actively disseminate among Shigella cells or transferr within microflora. The PMQR genes were reported to be always located in mobile genetic elements such as plasmids [59]. Here, the presence of qnrS and qnrB genes was detected at a very low level in quinolone-resistant S. flexneri in Xinjiang, while a number of QRDR mutations were identified, indicating that the mutations in QRDRs primarily underlie the resistance to quinolone in Shigella isolates investigated here. Different QRDR mutations confer various levels of resistance [60–62]. Notably, all quinolone-resistant isolates were shown to harbor at least three QRDR mutations, showing that their simultaneous presence may underlie the observed increase in the resistance to quinolones.
We analyzed and presented here the prevalence of Shigella species and serotypes in Xinjiang, China. S. flexneri was shown to be the dominant Shigella species, with a unique dominant serotype pattern (2a, 1b, 2b, Xv), which represents a hybrid pattern comprising serotypes prevalent in adjacent regions. High levels of AMR were observed, especially by S. flexneri isolates. Emergence of frequently observed MDR and resistance to frontline antibiotics can severely restrict the choice of antibiotic therapy used for the treatment of Shigella infections. Since unsafe sanitation conditions remain present in this region, food-borne or water-borne shigellosis epidemic will remain a significant public health concern in future [63,64]. Therefore, the prevalence, trends, and AMR patterns of Shigella species and serotypes in Xinjiang should be closely monitored, and novel strategies are urgently required to prevent the spreading of the AMR among Shigella strains.
Supporting information
An increasing trend in S. sonnei frequency among the Shigella isolates was observed between 2008 and 2014.
(TIF)
(DOCX)
(DOCX)
Acknowledgments
We thank all patients for providing their consent to be included in this study and sentinel hospitals for facilitating the collection and delivery of diarrhea samples.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the National Key R&D Program of China (no. 2017YFC1600105) and the National Nature Science Foundation of China (nos. 81673237 and 81473023). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Zhang CL, Liu QZ, Wang J, Chu X, Shen LM, Guo YY. Epidemic and virulence characteristic of Shigella spp. with extended-spectrum cephalosporin resistance in Xiaoshan District, Hangzhou, China. BMC Infectious Diseases. 2014;14:260 doi: 10.1186/1471-2334-14-260 ; PubMed Central PMCID: PMC4229937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cristea D, Ceciu S, Chitoiu DT, Bleotu C, Lazar V, Chifiriuc MC. Comparative study of pathogenicity tests for Shigella spp. and enteroinvasive Escherichia coli strains. Roumanian Archives of Microbiology and Immunology. 2009;68(1):44–9. . [PubMed] [Google Scholar]
- 3.Pazhani GP, Ramamurthy T, Mitra U, Bhattacharya SK, Niyogi SK. Species diversity and antimicrobial resistance of Shigella spp. isolated between 2001 and 2004 from hospitalized children with diarrhoea in Kolkata (Calcutta), India. Epidemiology and Infection. 2005;133(6):1089–95. doi: 10.1017/S0950268805004498 ; PubMed Central PMCID: PMC2870343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parsot C. Shigella spp. and enteroinvasive Escherichia coli pathogenicity factors. FEMS Microbiology Letters. 2005;252(1):11–8. doi: 10.1016/j.femsle.2005.08.046 . [DOI] [PubMed] [Google Scholar]
- 5.Qu F, Bao C, Chen S, Cui E, Guo T, Wang H, et al. Genotypes and antimicrobial profiles of Shigella sonnei isolates from diarrheal patients circulating in Beijing between 2002 and 2007. Diagnostic Microbiology and Infectious Disease. 2012;74(2):166–70. doi: 10.1016/j.diagmicrobio.2012.06.026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. British Medical Bulletin. 2009;92:7–32. doi: 10.1093/bmb/ldp028 . [DOI] [PubMed] [Google Scholar]
- 7.Qiu S, Wang Y, Xu X, Li P, Hao R, Yang C, et al. Multidrug-resistant atypical variants of Shigella flexneri in China. Emerging Infectious Diseases. 2013;19(7):1147–50. doi: 10.3201/eid1907.111221 ; PubMed Central PMCID: PMC3713959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye C, Lan R, Xia S, Zhang J, Sun Q, Zhang S, et al. Emergence of a new multidrug-resistant serotype X variant in an epidemic clone of Shigella flexneri. Journal of Clinical Microbiology. 2010;48(2):419–26. doi: 10.1128/JCM.00614-09 ; PubMed Central PMCID: PMC2815595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ke X, Gu B, Pan S, Tong M. Epidemiology and molecular mechanism of integron-mediated antibiotic resistance in Shigella. Archives of Microbiology. 2011;193(11):767–74. doi: 10.1007/s00203-011-0744-3 . [DOI] [PubMed] [Google Scholar]
- 10.Kahsay AG, Muthupandian S. A review on Sero diversity and antimicrobial resistance patterns of Shigella species in Africa, Asia and South America, 2001–2014. BMC Research Notes. 2016;9(1):422 doi: 10.1186/s13104-016-2236-7 ; PubMed Central PMCID: PMC5004314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotloff KL, Winickoff JP, Ivanoff B, Clemens JD, Swerdlow DL, Sansonetti PJ, et al. Global burden of Shigella infections: implications for vaccine development and implementation of control strategies. Bulletin of the World Health Organization. 1999;77(8):651–66. ; PubMed Central PMCID: PMC2557719 on Shigella infection. [PMC free article] [PubMed] [Google Scholar]
- 12.Bhattacharya D, Bhattacharya H, Sayi DS, Bharadwaj AP, Singhania M, Sugunan AP, et al. Changing patterns and widening of antibiotic resistance in Shigella spp. over a decade (2000–2011), Andaman Islands, India. Epidemiology and Infection. 2015;143(3):470–7. doi: 10.1017/S0950268814000958 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung The H, Rabaa MA, Pham Thanh D, De Lappe N, Cormican M, Valcanis M, et al. South Asia as a Reservoir for the Global Spread of Ciprofloxacin-Resistant Shigella sonnei: A Cross-Sectional Study. PLoS Medicine. 2016;13(8):e1002055 doi: 10.1371/journal.pmed.1002055 ; PubMed Central PMCID: PMC4970813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bodhidatta L, Pitisuttithum P, Chamnanchanant S, Chang KT, Islam D, Bussaratid V, et al. Establishment of a Shigella sonnei human challenge model in Thailand. Vaccine. 2012;30(49):7040–5. doi: 10.1016/j.vaccine.2012.09.061 ; PubMed Central PMCID: PMC3732056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ud-Din AI, Wahid SU, Latif HA, Shahnaij M, Akter M, Azmi IJ, et al. Changing trends in the prevalence of Shigella species: emergence of multi-drug resistant Shigella sonnei biotype g in Bangladesh. PloS ONE. 2013;8(12):e82601 doi: 10.1371/journal.pone.0082601 ; PubMed Central PMCID: PMC3867351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cui X, Wang J, Yang C, Liang B, Ma Q, Yi S, et al. Prevalence and antimicrobial resistance of Shigella flexneri serotype 2 variant in China. Frontiers in Microbiology. 2015;6:435 doi: 10.3389/fmicb.2015.00435 ; PubMed Central PMCID: PMC4423435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu S, Wang Z, Chen C, Liu N, Jia L, Liu W, et al. Emergence of a novel Shigella flexneri serotype 4s strain that evolved from a serotype X variant in China. Journal of Clinical Microbiology. 2011;49(3):1148–50. doi: 10.1128/JCM.01946-10 ; PubMed Central PMCID: PMC3067715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed SF, Klena J, Husain T, Monestersky J, Naguib A, Wasfy MO. Genetic characterization of antimicrobial resistance of Shigella flexneri 1c isolates from patients in Egypt and Pakistan. Annals of Clinical Microbiology and Antimicrobials. 2013;12:9 doi: 10.1186/1476-0711-12-9 ; PubMed Central PMCID: PMC3661368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aoki Y. Colicin type, biochemical type and drug-resistance pattern of Shigella sonnei isolated in Japan and its neighboring countries. Archivum Immunologiae et Therapiae Experimentalis. 1968;16(2):303–13. . [PubMed] [Google Scholar]
- 20.Mitsuhashi S, Harada K, Hashimoto H, Egawa R. On the drug-resistance of enteric bacteria. 4. Drug-resistance of Shigella prevalent in Japan. The Japanese Journal of Experimental Medicine. 1961;31:47–52. . [PubMed] [Google Scholar]
- 21.Puzari M, Sharma M, Chetia P. Emergence of antibiotic resistant Shigella species: A matter of concern. Journal of Infection and Public Health. 2017. doi: 10.1016/j.jiph.2017.09.025 . [DOI] [PubMed] [Google Scholar]
- 22.Klontz KC, Singh N. Treatment of drug-resistant Shigella infections. Expert Review of Anti-infective Therapy. 2015;13(1):69–80. doi: 10.1586/14787210.2015.983902 . [DOI] [PubMed] [Google Scholar]
- 23.Lindsey RL, Batra D, Rowe L, NL V, Juieng P, Garcia-Toledo L, et al. High-Quality Draft Genome Sequences for Four Drug-Resistant or Outbreak-Associated Shigella sonnei Strains Generated with PacBio Sequencing and Whole-Genome Maps. Genome Announcements. 2017;5(35). doi: 10.1128/genomeA.00906-17 ; PubMed Central PMCID: PMC5578855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffmann C, Sahly H, Jessen A, Ingiliz P, Stellbrink HJ, Neifer S, et al. High rates of quinolone-resistant strains of Shigella sonnei in HIV-infected MSM. Infection. 2013;41(5):999–1003. doi: 10.1007/s15010-013-0501-4 . [DOI] [PubMed] [Google Scholar]
- 25.Zhu JY, Duan GC, Yang HY, Fan QT, Xi YL. Atypical class 1 integron coexists with class 1 and class 2 integrons in multi-drug resistant Shigella flexneri isolates from China. Current Microbiology. 2011;62(3):802–6. doi: 10.1007/s00284-010-9790-3 . [DOI] [PubMed] [Google Scholar]
- 26.Cui X, Yang C, Wang J, Liang B, Yi S, Li H, et al. Antimicrobial Resistance of Shigella flexneri Serotype 1b Isolates in China. PloS one. 2015;10(6):e0129009 doi: 10.1371/journal.pone.0129009 ; PubMed Central PMCID: PMC4454585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahemuti W, Li X, Li F, Husaiyin M, Gu B, Zhang Jian S, et al. Analysis on groups and serotypes of Shigella in Xinjiang, 2003–2013. Chinese journal of preventive medicine. 2015;49(5):447–9. Epub 2015/09/02. . [PubMed] [Google Scholar]
- 28.Zhang J, Mahemuti M, Xia YD, Mutalifu M, Muheyati M, Li F, et al. Epidemiology and etiology of bacillary dysentery in Xinjiang Uigur Autonomous Region, 2004–2014. Chinese Journal of Epidemiology. 2016;37(11):1526–30. Epub 2017/01/11. doi: 10.3760/cma.j.issn.0254-6450.2016.11.018 . [DOI] [PubMed] [Google Scholar]
- 29.Institute. CaLS. Performance standards for antimicrobial susceptibility testing, 27th ed. CLSI document M100. 2018.
- 30.Ahmed AM, Furuta K, Shimomura K, Kasama Y, Shimamoto T. Genetic characterization of multidrug resistance in Shigella spp. from Japan. Journal of Medical Microbiology. 2006;55(Pt 12):1685–91. doi: 10.1099/jmm.0.46725-0 . [DOI] [PubMed] [Google Scholar]
- 31.Galani I, Souli M, Mitchell N, Chryssouli Z, Giamarellou H. Presence of plasmid-mediated quinolone resistance in Klebsiella pneumoniae and Escherichia coli isolates possessing blaVIM-1 in Greece. International Journal of Antimicrobial Agents. 2010;36(3):252–4. doi: 10.1016/j.ijantimicag.2010.05.004 . [DOI] [PubMed] [Google Scholar]
- 32.Tariq A, Haque A, Ali A, Bashir S, Habeeb MA, Salman M, et al. Molecular profiling of antimicrobial resistance and integron association of multidrug-resistant clinical isolates of Shigella species from Faisalabad, Pakistan. Canadian Journal of Microbiology. 2012;58(9):1047–54. doi: 10.1139/w2012-085 . [DOI] [PubMed] [Google Scholar]
- 33.Hu LF, Li JB, Ye Y, Li X. Mutations in the GyrA subunit of DNA gyrase and the ParC subunit of topoisomerase IV in clinical strains of fluoroquinolone-resistant Shigella in Anhui, China. Journal of Microbiology. 2007;45(2):168–70. . [PubMed] [Google Scholar]
- 34.Li R, Xie M, Lv J, Wai-Chi Chan E, Chen S. Complete genetic analysis of plasmids carrying mcr-1 and other resistance genes in an Escherichia coli isolate of animal origin. The Journal of Antimicrobial Chemotherapy. 2017;72(3):696–9. doi: 10.1093/jac/dkw509 . [DOI] [PubMed] [Google Scholar]
- 35.Pan JC, Ye R, Meng DM, Zhang W, Wang HQ, Liu KZ. Molecular characteristics of class 1 and class 2 integrons and their relationships to antibiotic resistance in clinical isolates of Shigella sonnei and Shigella flexneri. The Journal of Antimicrobial Chemotherapy. 2006;58(2):288–96. doi: 10.1093/jac/dkl228 . [DOI] [PubMed] [Google Scholar]
- 36.Qiu S, Xu X, Yang C, Wang J, Liang B, Li P, et al. Shift in serotype distribution of Shigella species in China, 2003–2013. Clinical Microbiology and Infection: the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2015;21(3):252 e5-8. doi: 10.1016/j.cmi.2014.10.019 . [DOI] [PubMed] [Google Scholar]
- 37.Anderson M, Sansonetti PJ, Marteyn BS. Shigella Diversity and Changing Landscape: Insights for the Twenty-First Century. Frontiers in Cellular and Infection Microbiology. 2016;6:45 doi: 10.3389/fcimb.2016.00045 ; PubMed Central PMCID: PMC4835486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zafar A, Hasan R, Nizami SQ, von Seidlein L, Soofi S, Ahsan T, et al. Frequency of isolation of various subtypes and antimicrobial resistance of Shigella from urban slums of Karachi, Pakistan. International Journal of Infectious Diseases. 2009;13(6):668–72. doi: 10.1016/j.ijid.2008.10.005 . [DOI] [PubMed] [Google Scholar]
- 39.Livio S, Strockbine NA, Panchalingam S, Tennant SM, Barry EM, Marohn ME, et al. Shigella isolates from the global enteric multicenter study inform vaccine development. Clinical Infectious Diseases. 2014;59(7):933–41. doi: 10.1093/cid/ciu468 ; PubMed Central PMCID: PMC4166982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guarino A, Albano F, Ashkenazi S, Gendrel D, Hoekstra JH, Shamir R, et al. European Society for Paediatric Gastroenterology, Hepatology, and Nutrition/European Society for Paediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe. Journal of Pediatric Gastroenterology and Nutrition. 2008;46 Suppl 2:S81–122. doi: 10.1097/MPG.0b013e31816f7b16 . [DOI] [PubMed] [Google Scholar]
- 41.Pouwels KB, Van Kleef E, Vansteelandt S, Batra R, Edgeworth JD, Smieszek T, et al. Does appropriate empiric antibiotic therapy modify intensive care unit-acquired Enterobacteriaceae bacteraemia mortality and discharge? The Journal of Hospital Infection. 2017;96(1):23–8. doi: 10.1016/j.jhin.2017.03.016 . [DOI] [PubMed] [Google Scholar]
- 42.Collatz E. Selecting empiric antibiotic therapy in an era of multi-drug resistance—is the cupboard really bare? Introduction. Clinical Microbiology and Infection. 2008;14 Suppl 6:1 doi: 10.1111/j.1469-0691.2008.02127.x . [DOI] [PubMed] [Google Scholar]
- 43.Gu B, Xu T, Kang H, Xu Y, Liu G, Pan S, et al. A 10-year surveillance of antimicrobial susceptibility patterns in Shigella sonnei isolates circulating in Jiangsu Province, China. Journal of global Antimicrobial Resistance. 2017;10:29–34. doi: 10.1016/j.jgar.2017.03.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang J, Qiu S, Xu X, Su W, Li P, Liang B, et al. Emergence of ONPG-negative Shigella sonnei in Shanghai, China. Diagnostic Microbiology and Infectious Disease. 2015;83(4):338–40. doi: 10.1016/j.diagmicrobio.2015.08.010 . [DOI] [PubMed] [Google Scholar]
- 45.Wang Z, Zhang H, Han J, Xing H, Wu MC, Yang T. Deadly Sins of Antibiotic Abuse in China. Infection Control and Hospital Epidemiology. 2017;38(6):758–9. doi: 10.1017/ice.2017.60 . [DOI] [PubMed] [Google Scholar]
- 46.Wang X, Ryu D, Houtkooper RH, Auwerx J. Antibiotic use and abuse: a threat to mitochondria and chloroplasts with impact on research, health, and environment. BioEssays. 2015;37(10):1045–53. doi: 10.1002/bies.201500071 ; PubMed Central PMCID: PMC4698130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.English BK, Gaur AH. The use and abuse of antibiotics and the development of antibiotic resistance. Advances in Experimental Medicine and Biology. 2010;659:73–82. doi: 10.1007/978-1-4419-0981-7_6 . [DOI] [PubMed] [Google Scholar]
- 48.Wang XY, Tao F, Xiao D, Lee H, Deen J, Gong J, et al. Trend and disease burden of bacillary dysentery in China (1991–2000). Bulletin of the World Health Organization. 2006;84(7):561–8. ; PubMed Central PMCID: PMC2627389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moore JE, Watabe M, Millar BC, Loughrey A, McCalmont M, Goldsmith CE, et al. Screening of clinical, food, water and animal isolates of Escherichia coli for the presence of blaCTX-M extended spectrum beta-lactamase (ESBL) antibiotic resistance gene loci. The Ulster Medical Journal. 2010;79(2):85–8. ; PubMed Central PMCID: PMC2993149. [PMC free article] [PubMed] [Google Scholar]
- 50.Smet A, Martel A, Persoons D, Dewulf J, Heyndrickx M, Cloeckaert A, et al. Comparative analysis of extended-spectrum-β-lactamase-carrying plasmids from different members of Enterobacteriaceae isolated from poultry, pigs and humans: evidence for a shared β-lactam resistance gene pool? The Journal of Antimicrobial Chemotherapy. 2009;63(6):1286–8. doi: 10.1093/jac/dkp101 ; PubMed Central PMCID: PMC2680344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tong P, Sun Y, Ji X, Du X, Guo X, Liu J, et al. Characterization of antimicrobial resistance and extended-spectrum beta-lactamase genes in Escherichia coli isolated from chickens. Foodborne Pathogens and Disease. 2015;12(4):345–52. doi: 10.1089/fpd.2014.1857 . [DOI] [PubMed] [Google Scholar]
- 52.Oduro-Mensah D, Obeng-Nkrumah N, Bonney EY, Oduro-Mensah E, Twum-Danso K, Osei YD, et al. Genetic characterization of TEM-type ESBL-associated antibacterial resistance in Enterobacteriaceae in a tertiary hospital in Ghana. Annals of Clinical Microbiology and Antimicrobials. 2016;15:29 doi: 10.1186/s12941-016-0144-2 ; PubMed Central PMCID: PMC4857374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Solgi H, Badmasti F, Giske CG, Aghamohammad S, Shahcheraghi F. Molecular epidemiology of NDM-1- and OXA-48-producing Klebsiella pneumoniae in an Iranian hospital: clonal dissemination of ST11 and ST893. The Journal of Antimicrobial Chemotherapy. 2018. doi: 10.1093/jac/dky081 . [DOI] [PubMed] [Google Scholar]
- 54.Flores-Carrero A, Labrador I, Paniz-Mondolfi A, Peaper DR, Towle D, Araque M. Nosocomial outbreak of extended-spectrum beta-lactamase-producing Enterobacter ludwigii co-harbouring CTX-M-8, SHV-12 and TEM-15 in a neonatal intensive care unit in Venezuela. Journal of Global Antimicrobial Resistance. 2016;7:114–8. doi: 10.1016/j.jgar.2016.08.006 . [DOI] [PubMed] [Google Scholar]
- 55.Nguyen NT, Ha V, Tran NV, Stabler R, Pham DT, Le TM, et al. The sudden dominance of blaCTX-M harbouring plasmids in Shigella spp. Circulating in Southern Vietnam. PLoS Neglected Tropical Diseases. 2010;4(6):e702 doi: 10.1371/journal.pntd.0000702 ; PubMed Central PMCID: PMC2882334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Matar GM, Jaafar R, Sabra A, Hart CA, Corkill JE, Dbaibo GS, et al. First detection and sequence analysis of the bla-CTX-M-15 gene in Lebanese isolates of extended-spectrum-beta-lactamase-producing Shigella sonnei. Annals of Tropical Medicine and Parasitology. 2007;101(6):511–7. doi: 10.1179/136485907X193860 . [DOI] [PubMed] [Google Scholar]
- 57.Madiyarov RS, Bektemirov AM, Ibadova GA, Abdukhalilova GK, Khodiev AV, Bodhidatta L, et al. Antimicrobial resistance patterns and prevalence of class 1 and 2 integrons in Shigella flexneri and Shigella sonnei isolated in Uzbekistan. Gut Pathogens. 2010;2(1):18 doi: 10.1186/1757-4749-2-18 ; PubMed Central PMCID: PMC3017001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gassama Sow A, Aidara-Kane A, Barraud O, Gatet M, Denis F, Ploy MC. High prevalence of trimethoprim-resistance cassettes in class 1 and 2 integrons in Senegalese Shigella spp isolates. Journal of Infection in Developing Countries. 2010;4(4):207–12. . [DOI] [PubMed] [Google Scholar]
- 59.Folster JP, Pecic G, Bowen A, Rickert R, Carattoli A, Whichard JM. Decreased susceptibility to ciprofloxacin among Shigella isolates in the United States, 2006 to 2009. Antimicrobial Agents and Chemotherapy. 2011;55(4):1758–60. doi: 10.1128/AAC.01463-10 ; PubMed Central PMCID: PMC3067149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alekshun MN, Levy SB. Molecular mechanisms of antibacterial multidrug resistance. Cell. 2007;128(6):1037–50. doi: 10.1016/j.cell.2007.03.004 . [DOI] [PubMed] [Google Scholar]
- 61.Qin T, Bi R, Fan W, Kang H, Ma P, Gu B. Novel mutations in quinolone resistance-determining regions of gyrA, gyrB, parC and parE in Shigella flexneri clinical isolates from eastern Chinese populations between 2001 and 2011. European Journal of Clinical Microbiology & Infectious Diseases. 2016;35(12):2037–45. doi: 10.1007/s10096-016-2761-2 . [DOI] [PubMed] [Google Scholar]
- 62.Tatay-Dualde J, Prats-van der Ham M, de la Fe C, Paterna A, Sanchez A, Corrales JC, et al. Mutations in the quinolone resistance determining region conferring resistance to fluoroquinolones in Mycoplasma agalactiae. Veterinary Microbiology. 2017;207:63–8. doi: 10.1016/j.vetmic.2017.06.003 . [DOI] [PubMed] [Google Scholar]
- 63.Nandy S, Dutta S, Ghosh S, Ganai A, Rajahamsan J, Theodore RB, et al. Foodborne-associated Shigella sonnei, India, 2009 and 2010. Emerging Infectious Diseases. 2011;17(11):2072–4. doi: 10.3201/eid1711.110403 ; PubMed Central PMCID: PMC3310563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kuo HW, Kasper S, Jelovcan S, Hoger G, Lederer I, Konig C, et al. A food-borne outbreak of Shigella sonnei gastroenteritis, Austria, 2008. Wiener Klinische Wochenschrift. 2009;121(3–4):157–63. doi: 10.1007/s00508-008-1141-7 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An increasing trend in S. sonnei frequency among the Shigella isolates was observed between 2008 and 2014.
(TIF)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.