Abstract
Objectives
Using a social learning model, the aim of the Sleep Smart Program was to primarily improve sleep health behaviors and secondarily improve academic performance and behavioral well-being.
Design
Randomized control trial for a social learning-based preventive intervention program.
Participants
A diverse group of seventh graders from 2 urban, middle schools were randomly assigned, according to school, to an 8-session Sleep Smart Program (SS = 70) or a comparison group (comparison = 73).
Measurements
Sleep patterns, sleep hygiene, and sleep health efficacy; academic performance; and behavioral well-being were assessed at 4 times of measure (baseline, postintervention, 2 follow-up times in eighth grade).
Results
SS seventh graders experienced significantly greater sleep health efficacy, improved physiological and emotional sleep hygiene, more time in bed, and earlier bedtimes vs comparison group. SS (vs comparison) participants also reported a significant decrease in internalizing behavior problems and sustained academic performance. Finally, although not maintained at time 4, SS participants continued to report improved sleep health efficacy at time 3, whereas the comparison group participants' sleep health efficacy declined.
Conclusion
The Sleep Smart preventive intervention was effective in improving sleep health efficacy, sleep hygiene, time in bed, and bedtimes; in maintaining grades; and in reducing internalizing behavior problems, yet these changes were not sustained at follow-up.
Keywords: Adolescence, Intervention, Sleep hygiene, Sleep-health efficacy
Introduction
Over the last 30 years, researchers, educators, and health care providers have recognized early adolescence as a developmental time that is unique and distinct from late childhood and later adolescence, usually defined as ages 10 to 15 years.1,2 In particular, a nuanced understanding of adolescents' sleep requirements, schedules, and regulatory processes has emerged.3–7 Laboratory and self-report data have demonstrated that adolescents sleep need of about 9 hours does not change from ages 10 to 17 years and, with the onset of puberty, they experience a circadian phase delay.3–5,8,9
Despite this stable or increased need, studies indicate that as early as age 12 (ie, sixth or seventh grade), adolescents obtain less sleep, experience increased daytime sleepiness, and report poor sleep hygiene, including using greater amounts of caffeine close to bedtime (BT) and engaging in screen-based activities that delay sleep.10–13 School schedules, extracurricular hours, and other environmental constraints are not beneficial to middle school– and high school–aged adolescents' sleep schedules and requirements.5,8,14,15 In fact, over the course of early to late adolescence, teens develop a sleep debt by getting a minimal amount of sleep on school nights and then delaying, as well as oversleeping, on weekends.3,5,14,15 The result is that even early adolescents are frequently absent or late for school, sleepy and moody during school hours, inattentive during class time, and struggle academically.14,16–18 Furthermore, early adolescents with poor sleep hygiene practices such as consuming caffeine close to BT and/or engaging in physiologically arousing activities (eg, cell phone use, playing video/iPad games) report later BTs, more disturbed sleep throughout the night, and increased daytime sleepiness.10,19–23 A recent systematic literature review concluded that studies consistently report a significant association between screen time and reduced sleep duration and increased sleep problems for children and adolescents.10 Similarly, a recent meta-analysis documented that good sleep hygiene (eg, regular BTs, decreased technology use) and physical activity function as protective factors, largely under adolescents' control, and are associated with earlier BTs for 12- to 18-year-olds.23 In comparison, a negative home environment and evening light, which is less likely to be under early adolescents' control, lead to later BTs. Despite the resounding agreement among health professionals that health habits need to be taught early in life,23–25 only some school districts have started to include sleep hygiene as part of their numerous health education standards (eg, California, Michigan, and Virginia).26–28 It is unclear, however, as to whether the focus is on teaching about sleep health vs working with adolescents to change their sleep health behaviors.
An increasing number of sleep education programs have been developed with the aim of improving adolescents' sleep practices by providing knowledge on the importance of sleep and strategies by which this change can be achieved. Cortesi et al29 evaluated the effects of a 2-hour sleep educational program on a sample of Italian high school students. The targeted students and a comparison group were evaluated using a sleep knowledge test before the program, immediately after the program, and during a 3-month follow-up to assess the intervention's effectiveness. Both groups had poor baseline knowledge of sleep; but compared with the control group, the sleep education group showed an average 50% gain in the number of correct answers immediately after the course and good retention of information three months later. De Sousa et al30 evaluated the effects of a 1-week school-based sleep hygiene program on sleep quality and daytime sleepiness in a small sample of high school–aged students in Brazil. Participants showed improved sleep-wake schedules and shorter sleep latencies reflecting promising behavioral changes; however, sleep quality and daytime sleepiness did not improve.
Moseley and Gradisar31 developed a school-based sleep intervention program for high school–aged adolescents using a cognitive-behavioral therapy framework with four 50-minute classes over a 4-week period. To evaluate the program's effectiveness, a randomized controlled trial featured 2 groups (program class and control group) assessed at 3 time points. Moseley and Gradisar's31 program successfully increased sleep knowledge; however, compared to the control group, sleep patterns did not improve. In a follow-up study, the researchers evaluated a motivational-based school intervention for improving adolescents' sleep.32 Again, the intervention group (vs control) increased their sleep knowledge and their motivation to regularize their sleep schedules. Although the adolescents in the motivation-oriented program did not improve their sleep patterns or daytime functioning, the program participants showed a marked retention rate in sustained sleep knowledge, which may be a precursor to behavioral change. More recently, they evaluated school-based sleep education programs using adjunct bright light therapy and/or parental involvement within a motivational interviewing framework.33 Contrary to their earlier studies, students reported decreased sleep onset latency and better mood ratings in addition to improved sleep knowledge in comparison to the control group. At a 6-week follow-up, improved sleep knowledge, mood, and decreased sleep onset latency were maintained. Nonetheless, bright light devices and parental involvement did not enhance the adolescents' behavioral changes, and it is not clear if the high school–aged participants maintained their knowledge or sleep changes beyond 6 weeks.
Taken together, these programs illustrate possible avenues to decreasing sleep restriction, improving sleep hygiene, and subsequent behavioral consequences for adolescents and demonstrate the value in raising healthy sleep-related behaviors for older adolescents. Few studies, however, have evaluated the effectiveness of sleep health programs for early adolescents.31–33
The current study examined the efficacy of the Sleep Smart Program (SS), a school-based sleep hygiene education program for improving early adolescents' sleep health efficacy, sleep hygiene practices, and patterns to ultimately improve academic performance and behavioral well-being. The program assumes 3-way dynamic interaction among personal/developmental factors (eg, sleep need), environmental influences (eg, sleep arrangements), and behavior (eg, caffeine, screen use). It was developed based on social learning theory: informative instructions, participatory classroom activities (eg, role playing, age-appropriate games), personal goal setting (utilization of sleep goal charts and diaries), feedback, and reinforcement (relevant rewards and specific recommendations each session). The program used some of the social learning aspects of the Slice of Life program, designed to promote healthy eating and physical activity patterns for adolescents34, as well as the Great Sensations Program.35 Students who participated in the Slice of Life program reported a significant improvement in knowledge and awareness regarding their eating habits and increased appropriate exercising.34 Similarly, the Great Sensations Program, a nutrition-education project, was effective in decreasing consumption of salty snacks and in increasing the consumption of target or healthy snack foods.35 The studies' outcomes suggested that school programs developed using social learning principles can be effective in facilitating important behavior changes for early adolescents. In addition, some aspects of the SS were influenced by the skill training model by Botvin et al,36 which provides adolescents with the necessary knowledge, skills, and personal sleep health efficacy for resisting social influences to smoke or, in this case, drink caffeine and/or stay up late.
Thus, it was hypothesized that students who participated in the program (SS) would obtain more sleep, develop better physiological sleep hygiene practices, and report a greater sense of efficacy regarding their sleep habits than a comparison group that did not participate in the program. In addition, it was hypothesized that those in the SS group might perform better academically and evidence fewer behavioral problems.
Methods
Study design and participants
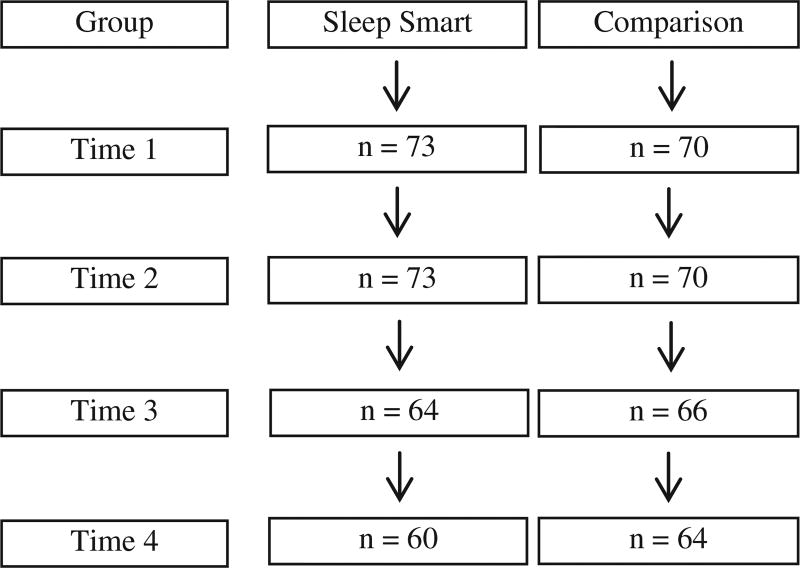
Seventh graders and their parents were recruited to participate from health classes in 2 urban, New England, public middle schools with delayed school start times of 8:37 am. The schools were randomly assigned to either the SS or the comparison conditions before families were recruited for the study, with condition assigned by school rather than by individual classrooms to avoid cross-classroom contamination. Of approximately 300 seventh graders in 12 health classes across the 2 schools, 48% (143 seventh graders) consented to participate (parental consent, seventh grader assent). There was a 100% retention rate between times 1 and 2, whereas some participants left the study at times 3 and 4 largely due to leaving the school or the district (Ns reported in Figure). Of note, of those participants who left the study between times 2 and 3 or 3 and 4, there were no significant differences on any of the dependent variables. Participant characteristics are displayed in Table 1.
Figure.
Ns across the program.
Table 1.
Participant characteristics.
| Comparison, n=73 |
Sleep Smart, n=70 |
|
|---|---|---|
| Age | 12.58 (0.48) | 12.50 (0.56) |
| Sex | 43 f. 30 m | 42 f. 28 m |
| aFamily income*** | ||
| <$30,000 | 21 (30%) | 28 (45%) |
| aRace/ethnicity (% underrepresented minority)* | 28b (38%) | 42c (64%) |
| Pubertal status | ||
| Pre/early | 17 (23%) | 12 (18%) |
| Mid | 30 (41%) | 22 (33%) |
| Late/post | 27 (36%) | 32 (48%) |
| BMI** | M = 19.83 (4.32) | M = 23.46 (5.78) |
| Overweight | 5 (7%) | 15 (22%) |
P ≤ .05.
P ≤ .01.
P ≤ .001.
Race/ethnicity characteristics of the participants in each school are similar to the district data for the 2 schools; however, 38% of the students' families at the comparison school vs 53% at the Sleep Smart school met the criteria for low income, defined as meeting the criteria for free or reduced lunch.37
Comparison: 4% Black/African American, 20% Hispanic, 7% Asian, 7% multiracial.
Sleep Smart: 15% Black/African American, 33% Hispanic, 8% Asian, 8% multiracial.
Procedures
After November recruitment, baseline (time 1) assessment occurred during January of seventh grade for both the SS and comparison group participants. Then, during February to March, students in the SS condition participated in the 4-week (8 total sessions, twice a week) sleep hygiene program held at the same time and length as their regularly scheduled health class (ie, 40 minutes). Postsession (time 2) assessments for the SS and comparison groups took place 1-week after the end of the program. Sleep Smart booster sessions were held to review and reinforce the sleep smart strategies taught in the initial 8 sessions. The first booster session was held in May of seventh grade with the time 3 follow-up assessment for both groups in October to November of eighth grade. The second booster session was held in February of eighth grade with the time 4 follow-up assessment in April/May of eighth grade. Attendance for the 8 initial sessions and the 4 booster sessions was 100%, excluding participants who were no longer in the study for times 3 and 4. At each time point, participants completed the same set of measures to assess sleep time, sleep hygiene, behavior problems, pubertal status, and self-efficacy, described in more detail in the Measures section. SS and comparison participants and their parents were given gift cards for participating in the study.
Sleep smart curriculum
Students in the SS condition learned about healthy sleep behaviors through a preventive health curriculum, which sought to improve specific sleep practices. Participants met in small groups (9–11 students) cofacilitated by 2 trained, BA-level leaders (supervised by a licensed clinical psychologist) over the eight 40-minute sessions. In an effort to monitor treatment fidelity, each group had the same 2 co-leaders for all 8 sessions, and only 4 pairs of co-facilitators taught the sessions over the course of the study. Seventh graders were provided with didactic information on adolescent sleep and specific strategies for establishing healthy sleep hygiene practices and obtaining sufficient sleep. Session-specific topics are summarized in Table 2. SS leaders used goal setting, modeling, role playing, educational games, and self-monitoring throughout the program, and the participants received session-relevant rewards after each session (eg, water bottle for caffeine session, laminated, wallet-size cards with sleep hygiene principles, sleep-smart pen to record their BT/wake time [WT]). SS participants' parents received a weekly newsletter that reviewed session information so that parents could reinforce the Sleep Smart strategies.
Table 2.
Sleep Smart session specific topics.
| Session number |
Topic | Session content |
|---|---|---|
| 1 | What is sleep? Why is it important? The basics | Sleep quiz, education on sleep cycles, and sleep needs for adolescents |
| 2 | Learn “Cool” sleep habits | Red/green light game, role playing to learn healthy sleep habits, and hygiene |
| 3 | Where and how much sleep is in your schedule? | Importance of sufficient sleep (8.5–9.5 h/night) for daytime functioning, exercise/game to reinforce |
| 4 | Consistent sleep/wake cycles | Emphasis on consistent sleep-wake habits, hygiene; relay race to review/reinforce hygiene strategies |
| 5 | BT routines | Skits created to role play helpful BT routines |
| 6 | Monitoring sleep patterns and sleep health efficacy for obtaining goals | Learn to self-assess/monitor sleep patterns through graphing activity |
| 7 | Effects of caffeine | Caffeine education, observations of caffeine advertising, creation of ads to promote healthy, noncaffeinated drinks |
| 8 | Wrap up: review, evaluation, and sleep smart commencement | Review 8 sessions and goal setting |
The comparison condition was described as research on the development of adolescents' sleep patterns and largely controlled for contact with the participants. This group met for approximately 30–40 minutes for each of their 4 sessions. Researchers maintained contact with comparison participants and their parents or guardians over the same period as the SS group through telephone follow-up. These points of contact focused on observing and reporting sleep patterns at the time 1 and time 2 assessments and did not approach ways to improve current sleep habits. Comparison group participants, like SS participants, completed all measures during the school day.
Measures
Background variables
Parents/guardians provided information about family income on the background information form. Income was measured with a checklist of dollar ranges reflecting $10,000 increments, and parents marked the option that included their total household income. Because of low frequency of responses in some options, responses were coded into 3 ordinal levels: lower income (<$30,000), middle income ($30,000–$60,000), and higher income (>$60,000).38 Participants reported their race/ethnicity along with height and weight on a revised School Sleep Habits Questionnaire. Based on this information, body mass index (BMI) was calculated using the Center for Disease Control recommended BMI for age, which takes into account age and sex.14,39 Pubertal status was measured with the child's self-ratings on the Pubertal Development Scale,9,40 which yields a categorical classification of pubertal status (eg, prepubertal, early, mid, late, and postpubertal).
Sleep outcome variables
Using Bandura's concept of self-efficacy and the recommendations for developing self-efficacy scales, sleep health efficacy was measured using the situation-specific measure, Adolescent Health and Sleep Efficacy Scale.41–43 The scale consisted of 6 sleep hygiene behaviors (eg, establishing healthy bed routine, getting at least 8.5 hours, healthy sleep habits, avoiding energetic activities, avoiding caffeine, establishing regular BT schedule), jointly considered to measure sleep health efficacy, or one's potential competency in their ability to make changes to these referenced behaviors (ie, sleep health). Participants rated each sleep-related question according to how sure they were that they could handle each activity using 100-point % scale.41–43 Cronbach α for the 6 sleep items was .84 for the 2 pilot samples taken before this program41,42 and .83 for the current study.
Sleep hygiene was examined using the Adolescent Sleep Hygiene Scale, a 28-item self-report measure that assesses sleep-facilitating and sleep-inhibiting practices in 12- to 18-year-old adolescents along different conceptual domains.21,44 Six domains were focused on for this study: physiological (5 items), cognitive (6 items), emotional (3 items), sleep environment (4 items), BT routine (1 item), and sleep stability (4 items). For example, the physiological domain queries about frequency of behaviors relating to exercise, activity before BT, and feelings of hunger (after 6:00 in the evening, I have drinks with caffeine; during the hour before bedtime, I am very active; during the 1 hour before bedtime, I drink more than 4 glasses of water; I go to bed with a stomach ache; I go to bed feeling hungry) and the emotional domain looks at frequency of behaviors tied to strong or upsetting emotions before BT. Participants reported how often these sleep-related behaviors occurred during the past month along a 6-point scale (“always,” “frequently-if not always,” “quite often,” “sometimes,” “once in a while,” and “never”), with higher scores indicative of better sleep hygiene. Reliability estimates of internal consistency for the subscales ranged from Cronbach α of .60 to .82.
School and weekend night BT and wake time (WT) were reported on the revised School Sleep Habits Questionnaire (adapted from Wolfson and Carskadon14), which asks about usual sleep and wake behaviors over the past 2 weeks (ie, what time do you usually go to bed/wake up?). School and weekend night time in bed (TIB) were calculated by using the self-report BT and WT for school and weekend nights.
PM Caffeine use (caffeine consumption from noon until BT), another aspect of sleep hygiene, was assessed based on the participants' self-reported afternoon/evening caffeine use (type and amount) on a daily sleep-wake diary. Total caffeine consumption was summed to get total daily caffeine use (milligrams per ounce). Afternoon and evening caffeine use was assessed, as previous studies suggest that dose-dependent caffeine use close to BT negatively affects sleep maintenance in adults and adolescents.45,46
Bedtime screen time use (eg, television, video games, and computer) was calculated based on the participants' self-reported screen time use in the hour before bed (reported in minutes).
Academic performance and behavioral outcome variables
Average English grades and average Math grades were based on students' school transcripts, which were reported on a 100-point grading scale. Transcripts from quarters 2 and 3 corresponded to academic performance for time 1 and time 2, respectively. English and Math grades were used as an indication of academic performance, with higher scores indicating better academic performance. Behavioral well-being was assessed using the Internalizing and Externalizing Behavior Problem scores, derived from the Youth Self Report (YSR) and the parent report Child Behavior Checklist (internalizing and externalizing behavior problem scales).47 The scores are based on the 112 items, each rated on a 3-point scale (0, not true; 1, somewhat/sometimes true; 2, very true/often true) of how truly each behavior reflected the adolescent's behavior. Lower scores indicate better well-being. Analyses are based on the YSR, as cross-informant correlations for the YSR and CBCL were .33 for internalizing and .46 for externalizing, similar to other studies.48
Statistical analyses
The analyses presented here focus on changes from baseline (T1) to each postintervention time point (T2, T3, and T4). For all postintervention outcome or dependent variables, difference scores were calculated separately for each follow-up using T1 as the reference point. Four multivariate analyses of covariance (MANCOVA) were conducted to assess the effects of the program on the adolescents' changes in sleep health efficacy; sleep hygiene practices; school and weekend night BT, WT, and TIB; academic performance; and behavioral well-being. An initial MANCOVA assessed the program's effect on itemized sleep health efficacy. A second MANCOVA evaluated the changes in 6 sleep hygiene domains, BT screen use, and pm caffeine use. A third MANCOVA assessed differences in school and weekend night sleep patterns, specifically, BT, WT, and TIB. A final MANCOVA assessed the secondary effects of the program on internalizing and externalizing problem behaviors and academic performance based on English and Math grades. Covariates for each model included background variables (family income, BMI, pubertal status, race/ethnicity, and sex) and the T1 dependent variables.
Results
Background characteristics
As shown in Table 1, significant differences between conditions were noted at baseline in income, race/ethnicity, BMI, and pubertal status, with SS participants from families with lower incomes (<$30,000/year), further along in pubertal development, and more overweight/obese than comparison participants. As previously mentioned, these variables were controlled for in all analyses.
Sleep health efficacy, sleep hygiene, and sleep-wake patterns
Pearson correlations were examined for the sleep variables. Sleep health efficacy and school night sleep patterns (BT and TIB) were significantly correlated (rs = 0.18–0.23; Ps < .04). Likewise, earlier weekend WTs were associated with higher sleep health efficacy (rs = −0.19 to −0.21; Ps < .04). Lower caffeine and screen use were associated with higher sleep health efficacy for avoiding caffeine and avoiding energetic activities (rs = −0.17 to−0.21; Ps < .05). Furthermore, the 6 different sleep hygiene domains were also significantly correlated with sleep health efficacy (rs = 0.26–0.38; Ps < .01).
Table 3 displays the difference scores, means, and SDs for the sleep health efficacy variables for T1 and T2. The SS prompted significant changes in sleep health efficacy (multivariate F (6, 135) = 2.42; P = .03) as explained by univariate differences in 5 of 6 sleep health efficacy items (avoiding energetic activities was not significant). SS participants reported an improvement in their sleep health efficacy over BT-specific behaviors. In addition, the SS participants maintained overall sleep health efficacy from time 1 to time 3 (F (6, 77) = 2.29; P = .04). This significance is explained entirely by the participants' sleep health efficacy that they can obtain at least 8.5 hours of sleep each night. The SS participants reported increased percentage of sleep health efficacy from T1 to T3 (62%-64%), whereas the comparison group participants reported decreased sleep health efficacy percentage (73%-57%). This difference was not significant from T1 to T4.
Table 3.
Means and SDs for sleep health efficacy variables at time 1, time 2, and difference scores.
| Sleep health efficacy | Condition | DS | T1 | T2 | |
|---|---|---|---|---|---|
| Healthy bed routine* | Sleep Smart group | M (SD) | .10 (.39) | .51 (.30) | .62 (.28) |
| Comparison group | M (SD) | −.02 (.31) | .61 (.32) | .59 (.35) | |
| At least 8.5 hours** | Sleep Smart group | M (SD) | .06 (.35) | .63 (.32) | .69 (.31) |
| Comparison group | M (SD) | −.10 (.26) | .72 (.30) | .62 (.33) | |
| Healthy sleep habits* | Sleep Smart group | M (SD) | .04 (.28) | .63 (.28) | .67 (.27) |
| Comparison group | M (SD) | −.06 (.32) | .74 (.27) | .67 (.31) | |
| Avoid energetic activities | Sleep Smart group | M (SD) | .04 (.37) | .33 (.32) | .37 (.34) |
| Comparison group | M (SD) | −.02 (.34) | .42 (.35) | .40 (.35) | |
| Avoid caffeine** | Sleep Smart group | M (SD) | .09 (.45) | .46 (.34) | .55 (.36) |
| Comparison group | M (SD) | −.09 (.39) | .63 (.31) | .54 (.37) | |
| Regular BT schedule** | Sleep Smart group | M (SD) | .10 (.39) | .59 (.31) | .68 (.27) |
| Comparison group | M (SD) | −.06 (.35) | .70 (.33) | .64 (.34) |
Abbreviation: DS, difference score from T1 to T2.
Note: Variables represent how participants rated each sleep health efficacy question according to how sure they were that they could handle each behavior on 100% scale. This difference was not significant from T1 to T4.
P ≤ .05.
P ≤ .01.
As seen in Table 4, overall, SS group participants significantly improved their sleep hygiene practices as compared to the comparison group, multivariate F (8, 87) = 2.82; P = .05. Specifically, SS participants decreased BT screen use by nearly 5 minutes, whereas the comparison group increased BT screen use by over 6 minutes (P = .07); SS participants decreased PM caffeine use by 8.80 mg/oz, whereas comparison group only decreased caffeine use by 2.39 mg/oz (P = .02); and SS participants improved physiological and emotional sleep hygiene scores by 0.53 and 0.43, respectively, whereas comparison group improved by less than 0.20 (Ps ≤ .05). There were no significant differences reported from T1 to T3 and from T1 to T4.
Table 4.
Means and SDs for sleep hygiene variables at time 1, time 2, and difference scores.
| Sleep hygiene | Condition | DS | T1 | T2 | |
|---|---|---|---|---|---|
| Physiological*** | Sleep Smart | M (SD) | 0.50 (0.83) | 4.04 (0.75) | 4.54 (0.77) |
| Comparison | M (SD) | 0.20 (0.75) | 4.17 (0.99) | 4.37 (0.84) | |
| Cognitive | Sleep Smart | M (SD) | 0.29 (0.91) | 3.81 (0.94) | 4.12 (0.98) |
| Comparison | M (SD) | 0.18 (1.14) | 3.85 (1.13) | 4.03 (1.11) | |
| Emotional* | Sleep Smart | M (SD) | 0.43 (1.04) | 4.71 (1.05) | 5.14 (0.88) |
| Comparison | M (SD) | 0.16 (1.14) | 4.94 (1.07) | 5.11 (1.03) | |
| Sleep environment | Sleep Smart | M (SD) | 0.37(1.15) | 4.69 (1.07) | 5.06 (0.90) |
| Comparison | M (SD) | 0.20 (1.02) | 5.00 (1.13) | 5.16 (0.99) | |
| BT routine | Sleep Smart | M (SD) | 0.13 (2.20) | 3.37 (1.75) | 3.52 (1.63) |
| Comparison | M (SD) | 0.08 (1.94) | 3.63 (1.96) | 3.71 (1.84) | |
| Sleep stability | Sleep Smart | M (SD) | 0.57 (1.35) | 3.42 (1.22) | 4.00 (1.15) |
| Comparison | M (SD) | 0.45 (1.07) | 3.41 (1.17) | 3.86 (1.11) | |
| PM Caffeine use (mg/oz)* | Sleep Smart | M (SD) | −8.80 (16.05) | 13.49 (15.78) | 4.89 (8.52) |
| Comparison | M (SD) | −2.39 (10.25) | 8.09 (12.13) | 5.92 (12.20) | |
| BT screen time (min)** | Sleep Smart | M (SD) | −4.91 (26.55) | 33.41 (21.32) | 28.01 (21.06) |
| Comparison | M (SD) | 6.48 (19.18) | 20.27 (18.78) | 26.91 (20.13) |
Note: Physiological, cognitive, emotional, sleep environment, daytime sleepiness, BT routine, and sleep stability: variables from Adolescent Sleep Hygiene Scale. PM Caffeine use was based on participants' self-reported afternoon/evening caffeine use (milligrams per ounce) on sleep-wake diary. BT screen time use (eg, television, video games, computer) calculated based on participants' self-reported screen time use in hour before bed (minutes). No significant differences reported from T1 to T3 or T1 to T4 for these variables.
P ≤ .10.
P ≤ .05.
P ≤ .01.
Overall, SS participants reported increased TIB and earlier BTs on school and weekend nights (multivariate F (3, 94) = 3.31; P = .005) relative to their comparison peers (see Table 5). On average, participants reported a 13-minute increase in school night TIB, whereas their comparison group peers reported a 12-minute decrease in school night TIB (P = .034). In addition on weekends, SS participants reported that they were getting 42 more minutes in bed, whereas the comparison group reported that they decreased their weekend night TIB by 17 minutes (P = .009). Increased TIB on school and weekend nights for the SS group corresponded with significantly earlier BTs for the SS vs comparison participants (school night BT, P = .013; weekend night BT, P = .008), whereas WTs did not change for the 2 groups from T1 to T2 and there were no significant differences reported from T1 to T3 and from T1 to T4 for any of these sleep pattern variables.
Table 5.
Means and SDs for school and weekend sleep pattern variables at time 1 and time 2 and difference scores.
| TIB | Condition | DS (min) | T1 | T2 | |
|---|---|---|---|---|---|
| School night TIB* | Sleep Smart group | M (SD) | 13 (58) | 8.98 (67) | 9.20 (55) |
| Comparison group | M (SD) | −12 (43) | 9.43 (54) | 9.23 (51) | |
| Weekend TIB (min)** | Sleep Smart group | M (SD) | 42 (133) | 9.80 (126) | 10.50 (174) |
| Comparison group | M (SD) | −17 (95) | 10.50 (107) | 10.22 (96) | |
| School BT (hour:min)** | Sleep Smart group | M (SD) | −0:12 (0:55) | 21:56 (1:10) | 21:44 (0:55) |
| Comparison group | M (SD) | 0:11 (0:38) | 21:28 (0:54) | 21:39 (0:47) | |
| School WT (hour:min) | Sleep Smart group | M (SD) | −0:01 (0:20) | 6:53 (0:26) | 6:52 (0:25) |
| Comparison group | M (SD) | −0:09 (0:35) | 6.55 (0:34) | 6:46 (0:43) | |
| Weekend BT (hour:min)** | Sleep Smart group | M (SD) | −0:58 (1:38) | 24:12 (1:58) | 23:20 (1:34) |
| Comparison group | M (SD) | −0:03 (1:02) | 23:22 (1:29) | 23.25 (1:28) | |
| Weekend WT (hour:min) | Sleep Smart group | M (SD) | −0:10 (1:51) | 9:59 (1:57) | 9:49 (1:50) |
| Comparison group | M (SD) | −0:14 (1:15) | 9:51 (1:48) | 9:37 (1:44) |
Abbreviation: DS, difference score from T1 to T2.
Note: School and weekend wake and bed times were reported on the School Sleep Habits Questionnaire. School and weekend night TIB was computed using self-reported school and weekend night BT and WT. There were no significant differences reported from T1 to T3 or from T1 to T4 for these variables.
P ≤ .05.
P ≤ .01.
Academic performance and behavioral well-being
Table 6 displays the difference scores, means, and SDs for the SS and comparison groups' transcript reported English and Math grades and internalizing and externalizing behavior problem scores. Behavioral well-being and academic performance significantly changed with the SS, multivariate F (4, 83) = 2.71; P = .036. Univariate analyses revealed that the SS vs comparison participants reported a moderately significant decrease in internalizing behavior problems (P = .06). In addition, SS participants maintained their English academic performance from quarters 2 to 3 (ie, times corresponding to before and after the Sleep Smart intervention), whereas the comparison participants experienced a significant decline in their academic performance based on average English course grades showing minimal decline in English grade (P = .04). There were no significant differences from T1 to T3 and from T1 to T4.
Table 6.
Means and SDs for academic performance and behavioral well-being outcome variables at time 1, time 2, and difference scores.
| Outcome variables | Condition | DS | T1 | T2 | |
|---|---|---|---|---|---|
| Average English grade** (100%) | Sleep Smart group | M (SD) | 0.05 (13.81) | 78.10 (14.82) | 78.15 (14.40) |
| Comparison group | M (SD) | −6.10 (12.51) | 84.56 (10.64) | 78.68 (16.75) | |
| Average Math grade (100%) | Sleep Smart group | M (SD) | 0.65 (8.03) | 80.17 (13.68) | 80.83 (10.71) |
| Comparison group | M (SD) | −1.65 (10.34) | 80.35 (14.08) | 79.97 (12.35) | |
| YSR —internalizing behavior* | Sleep Smart group | M (SD) | −3.72 (11.38) | 52.56 (9.20) | 49.03 (8.24) |
| Comparison group | M (SD) | −2.40 (10.62) | 49.84 (9.94) | 47.44 (10.27) | |
| YSR—externalizing behavior | Sleep Smart group | M (SD) | −0.77 (6.88) | 50.82 (9.00) | 50.12 (9.00) |
| Comparison group | M (SD) | −1.74 (9.52) | 49.47 (10.09) | 47.73 (10.78) |
Abbreviation: DS, difference score from T1 to T2.
Note: Average English grades were based on student transcripts, which were reported on a 100-point grading scale. Behavioral well-being was assessed using internalizing and externalizing behavior problem scores, derived from the YSR. There were no significant differences reported from T1 to T3 or T1 to T4 for these variables.
P ≤ .10.
P ≤ .05.
Discussion
The purpose of this study was to evaluate the impact of the SS on early adolescents' sleep patterns and hygiene, including caffeine use, along with academic and behavioral well-being. Findings demonstrate that this preventive intervention was effective in helping the seventh graders in an urban school environment feel more competent in their ability to manage certain aspects of their sleep habits; establish better sleep hygiene practices; increase school and weekend TIB, advance BTs, particularly weekend nights; and use less caffeine in comparison to their peers who did not participate in the program. With regard to sleep patterns, it is particularly noteworthy that the SS early adolescents reported that they were going to bed almost an hour earlier on weekend nights after the intervention, whereas their peers had more delayed BTs.
Clinical significance is also important in a preventive intervention study. For adolescents, studies have shown for example that adolescents who get As and Bs obtain at least 20 minutes more sleep and/ or go to bed 20 minutes earlier than their peers who are performing poorly in school.13,14 Therefore, from a clinical perspective, it is noteworthy that the SS adolescents reported an average increase of 13minutes school night and 42 minutes weekend night sleep after the intervention.
Based on the social learning model, the SS focused on sleep health efficacy along with sleep patterns and sleep hygiene practices as a model for promoting behavioral change in adolescents.49 Results demonstrate that the program helped adolescents develop a greater sense of efficacy in their ability to manage aspects of their sleep. In particular, 5 of the 6 sleep health efficacy behaviors changed significantly from time 1 to time 2, suggesting that SS adolescents acknowledged that they were more efficacious post-program from baseline in their ability to establish a BT routine, maintain a regular sleep schedule, monitor their sleep habits, and decrease their caffeine use. Moreover, sleep health efficacy was significantly associated with healthier sleep patterns and hygiene practices and the early adolescents who participated in the SS maintained their self-efficacy regarding their ability to obtain at least 8.5 hours of sleep each night from time 1 to time 3 in comparison to their peers who reported decreased sleep health efficacy on the same variable, suggesting that improving one's sleep health efficacy might be linked to improving sleep habits and hygiene. The aspects of the adolescents' sleep that changed after the program were topics that were centrally focused on throughout the program such as caffeine use, quantity of sleep, and sleep hygiene practices. It should be noted, however, that a causal relationship cannot be established and that other models of behavior exist. Other explanations suggest that adolescents may alter their behaviors even when they are not necessarily connected to primary changes in efficacy, including motivational, self-regulation, or other cognitive-behavioral change models.50,51
Stability in academic performance for the SS group suggests that gains from the program may have helped to maintain academic performance, as the SS participants' grades were consistent over the academic year, whereas their comparison group peers' grades worsened. During the time 2 assessment, participants were well into their third quarter of seventh grade, which should have allowed for adjustment to the school year and workload. Comparing the SS groups' consistent academic performance vs the comparison adolescents' declining academic performance suggests that cumulative sleep loss might negatively affect grades, whereas the tools learned in the SS may have helped to buffer the young adolescents against the risk of academic difficulties over the first year of middle school.13
Although we are encouraged by our findings, certain caveats and limitations pertain. The schools were randomly assigned as SS or comparison; however, baseline differences between the groups may have affected the program. SS adolescents came from lower income families, had higher BMIs, and were further along in pubertal development. The evident socioeconomic disadvantage of the SS group may have created stressful environments that negatively impacted sleep health.52 In addition, increased BMI is associated with less sleep and more sleep problems in adolescents.53 Finally, more advanced pubertal development is often associated with a delayed sleep phase preference.9 After controlling for baseline differences, however, the intervention was still effective in improving sleep behaviors for SS participants, suggesting that without these baseline differences, the effects may have been even greater. Moreover, the contact with the comparison participants, although not purposefully educational, may have highlighted important aspects of sleep without overtly addressing these issues. For example, although the comparison condition sessions focused on collecting the data, the nature of focusing on one's sleep patterns and hygiene may affect how they think about their sleep. In essence, these sessions may have unintentionally influenced behavioral changes. Another caveat of the study was that the 4-week, 8-session program and 4 review sessions may not have been sufficient for more lasting behavioral change. Without regular booster interventions, adolescents, in particular, may not be able to maintain program benefits and lasting behavioral changes. Lastly, the results of this study are based on self-report and parent report other than the transcript-based grades. Self-reported sleep patterns, in particular, are less reliable than actigraphy and diary estimated sleep patterns, especially for weekend sleep.54
The SS and comparison schools used in this study both had delayed school start times (ie, 8:37 am),which might explain the participants' estimated adequate sleep at the outset of the study (ie, <8.5 hours).3,8 A prior study conducted in the same school district along with other research has shown that middle school– and high school–aged adolescents who attend later starting schools obtain more school night sleep and have later WTs; less sleepiness; decreased tardiness; and, in some instances, better academic performance.55 As a result, it is striking that the SS seventh graders further increased their TIB, advanced their BTs, and improved their sleep hygiene strategies. In other words, in addition to delaying school start times, middle schools may want to consider sleep hygiene education as a way of helping their adolescents obtain sufficient sleep and, in turn, improve academic performance and related behaviors.
This field is still in its “adolescence,” and there are many avenues for future research. Although our study shows that BA-level educators can provide effective support, sleep health education, and practical sleep hygiene change strategies to early adolescents in an urban school setting, other school environments and adolescent populations should be included in the future. The preventive intervention was reinforced with a parent newsletter; however, an integrated parent/ guardian preventive intervention may have led to more significant gains. Future work on social learning–based interventions may need to consider additional intervention time so that sleep hygiene gains are more sustainable. Likewise, future studies should examine the nuances (eg, sleep logs, role playing, sleep knowledge, self efficacy, etc) of the SS program? to determine which aspects of the intervention are most likely to lead to significant and lasting behavioral change.
Conclusion
Findings suggest that this social learning–based program focused on sleep patterns and sleep hygiene has clear potential for successfully helping early adolescents in an urban school environment improve their sleep health efficacy and change and maintain important sleep behaviors and academic performance. In particular, the Sleep Smart preventive intervention was effective in: improving sleep health efficacy, sleep hygiene, TIB, and BTs; maintaining grades; and reducing internalizing behavior problems; yet, these changes were not sustained at follow-up.
Acknowledgments
This research was funded by the following grant: NIH, NICH5, 5 R01 HD047928-06 from the National Institutes of Health and conducted while the first author was at the Department of Psychology, College of the Holy Cross, Worcester, MA. The authors wish to thank the many research assistants, including Michaela Sparling, Andrea Azuaje, Kelly Naku, Kathleen Barry, Christina Kyriakos, Jillian Canton, Melissa Richards, and Marissa Lown.
Footnotes
Sleep-Smart curriculum materials are available upon request from the first author.
Conflict of interest: All authors report that there are no competing financial interests regarding this paper.
References
- 1.Urdan T, Klein S. Early adolescence: a review of the literature. In: National Association of Secondary School Principals, editor. Collected papers from the OERI Conference on Adolescence: designing developmentally appropriate middle schools. Washington, D. C.: 1999. pp. 19–52. [Google Scholar]
- 2.Steinberg L, Silverberg SB. The vicissitudes of autonomy in early adolescence. Child Dev. 1986;57(4):841–851. doi: 10.1111/j.1467-8624.1986.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 3.Carskadon MA, Acebo C. Regulation of sleepiness in adolescents: update, insights, and speculation. Sleep. 2002;25:606–614. doi: 10.1093/sleep/25.6.606. [DOI] [PubMed] [Google Scholar]
- 4.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021(1):276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 5.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21(8):871–881. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 6.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–612. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Jenni OG, Achermann P, Carskadon MA. Homeostatic sleep regulation in adolescents. Sleep. 2005;28(11):1446–1454. doi: 10.1093/sleep/28.11.1446. [DOI] [PubMed] [Google Scholar]
- 8.Carskadon MA, Harvey K, Duke P, Anders TF, Dement WC. Pubertal changes in daytime sleepiness. Sleep. 1980;2:453–460. doi: 10.1093/sleep/2.4.453. [DOI] [PubMed] [Google Scholar]
- 9.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16(3):258–262. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 10.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;12(21):50–58. doi: 10.1016/j.smrv.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollack CP, Bright D. Caffeine consumption and weekly sleep patterns in US seventh, eighth, and ninth graders. Pediatrics. 2003;111(1):42–46. doi: 10.1542/peds.111.1.42. [DOI] [PubMed] [Google Scholar]
- 12.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000;36(3):291–301. doi: 10.1037//0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- 13.Wolfson AR, Carskadon MA. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7(6):491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 14.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescence. Child Dev. 1998;69(4):875–887. [PubMed] [Google Scholar]
- 15.Wolfson AR, Acebo C, Fallone G, Carskadon MA. Actigraphically-estimated sleep patterns of middle school students. Sleep. 2003;26(Abstract Suppl):A126–A127. [Google Scholar]
- 16.Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 17.Comstock G. Television and the American Child. San Diego, CA: Academic Press; 1991. [Google Scholar]
- 18.Wahlstrom K. Accommodating the sleep patterns of adolescents within current educational structures: an uncharted path. In: Carskadon M, editor. Adolescent Sleep Patterns: Biological, Sociological, and Psychological Influences. Cambridge, United Kingdom: Cambridge University Press; 2002. [Google Scholar]
- 19.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med Rev. 2010;11(8):735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123(6):1005–1010. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 21.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson A, Harsh J. The relationship between sleep hygiene and sleep quality in Italian and American adolescents. Pediatrics. 2005;115:257–265. doi: 10.1542/peds.2004-0815H. [Supplement] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seifert SM, Schaechter JL, Hershorin ER, Lipshultz SE. Health effects of energy drinks on children, adolescents, and young adults. Pediatrics. 2011;127(3):511–528. doi: 10.1542/peds.2009-3592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 24.Hawkins JD, Catalano RF, Kosterman R, Abbot R, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Arch Pediatr Adolesc Med. 1999;153(3):226–234. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- 25.Nicklas TA, Johnson CC, Webber LS, Berenson GS. School-based programs for health-risk reduction. Ann N Y Acad Sci. 1997;817:208–224. doi: 10.1111/j.1749-6632.1997.tb48208.x. [DOI] [PubMed] [Google Scholar]
- 26.California State Board of Education. Health Education Content Standards for California Public Schools: Kindergarten through Grade Twelve. 2008 [Google Scholar]
- 27.Michigan Department of Education. Michigan Merit Curriculum Credit Guidelines: Health Education. 2007 [Google Scholar]
- 28.Board of Education, Commonwealth of Virginia. Health Education Standards of Learning for Virginia Public Schools. 2015 [Google Scholar]
- 29.Cortesi F, Giannotti F, Sebastiani T, Bruni O, Ottaviano S. Knowledge of sleep in Italian high school students: pilot test of a school-based sleep education program. J Adolesc Health. 2004;34(4):344–351. doi: 10.1016/j.jadohealth.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 30.De Sousa IC, Araujo JF, de Azevedo CVM. The effect of a sleep hygiene education program on the sleep–wake cycle of Brazilian adolescent students. Sleep Biol Rhythms. 2007;5(4):251–258. [Google Scholar]
- 31.Moseley L, Gradisar M. Evaluation of a school-based intervention for adolescent sleep problems. Sleep. 2009;32(3):334–341. doi: 10.1093/sleep/32.3.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cain N, Gradisar M, Moseley L. A motivational school-based intervention for adolescent sleep problems. Sleep Med Rev. 2011;12(3):246–251. doi: 10.1016/j.sleep.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 33.Bonnar D, Gradisar M, Moseley L, Coughlin A, Cain N, Short M. Evaluation of novel school-based interventions for adolescent sleep problems: does parental involvement and bright light improve outcomes? Sleep Health. 2015;1(1):66–74. doi: 10.1016/j.sleh.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 34.Perry CL, Klepp KI, Halper A, et al. Promoting healthy eating and physical activity patterns among adolescents: a pilot study of "Slice of Life". Health Educ Res. 1987;2(2):93–103. [Google Scholar]
- 35.Coates T, Barofsky I, Saylor KE. Modifying the snack consumption patterns of inner city high school students: the great sensation study. Prev Med. 1985;14(2):234–247. doi: 10.1016/0091-7435(85)90039-8. [DOI] [PubMed] [Google Scholar]
- 36.Botvin G, Dusenbury L, Baker E, Botvin EM, Diaz T. A skills training approach to smoking prevention among Hispanic youth. J Behav Med. 1989;12(3):279–296. doi: 10.1007/BF00844872. [DOI] [PubMed] [Google Scholar]
- 37.Massachusetts Department of Elementary and Secondary Education. 2006 http://profiles.doe.mass.edu/state_report/selectedpopulations.aspx?mode=school&year=2006&Continue.x=0&Continue.y=0.
- 38.Marco CA, Wolfson AR, Sparling M, Azuaje A. Family socioeconomic status and sleep patterns of young adolescents. Behav Sleep Med. 2012;10(1):70–80. doi: 10.1080/15402002.2012.636298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. 2015 Retrieved from http://www.cdc.gov/healthyweight/assessing/bmi/childrens_BMI/about_childrens_BMI.html#HowIsBMICalculated.
- 40.Petersen A, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc. 1988;17(2):117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- 41.Rossi CM, Campbell AL, Vo OT, Marco CA, Wolfson AR. Middle school sleep-smart program: a pilot evaluation. Sleep. 2002;25:A279. [Supplement] [Google Scholar]
- 42.Vo OT, LeChasseur K, Wolfson A, Marco C. Sleepy pre-teens: second pilot of sleep-smart program in 7th graders. Sleep. 2003;26:1036. [Supplement] [Google Scholar]
- 43.Bandura A. Self-Efficacy: The Exercise of Control. New York, New York: Freeman; 1997. [Google Scholar]
- 44.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115(1):257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hughes JR, Hale KL. Behavioural effects of caffeine and other methylxanthines on children. Exp Clin Psychopharmacol. 1998;6(1):87–95. doi: 10.1037//1064-1297.6.1.87. [DOI] [PubMed] [Google Scholar]
- 46.Roehrs T, Roth T. Caffeine: sleep and daytime sleepiness. Sleep Med Rev. 2008;12(2):153–162. doi: 10.1016/j.smrv.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 47.Achenbach TM, Rescorla LA. Child Behavior Checklist: Youth Self-Report for Ages 11–18 (YSR 11–18) Manual for the ASEBA school-age forms and profiles. 2001 [Google Scholar]
- 48.Van der Ende J, Verhulst F, Tiemeier H. Agreement of informants on emotional and behavioral problems from childhood to adulthood. Psychol Assess. 2012;24(2):293–300. doi: 10.1037/a0025500. [DOI] [PubMed] [Google Scholar]
- 49.Schwarzer R, Luszczynska A. Self-efficacy and adolescent's risk taking and health. In: Pajares F, Urdan T, editors. Self-efficacy beliefs of adolescents. Adolescence and EducationGreenwich, CT: Information Age Publishing; 2005. pp. 139–159. [Google Scholar]
- 50.Peters LW, Kok G, Ten Dam GT, Buijs GJ, Paulussen TG. Effective elements of school health promotion across behavioral domains: a systematic review of reviews. BMC Public Health. 2009;9:182–195. doi: 10.1186/1471-2458-9-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Prev Med. 2008;46(3):181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children's socioemotional adjustment. Psychol Sci. 2005;16(7):560–565. doi: 10.1111/j.0956-7976.2005.01575.x. [DOI] [PubMed] [Google Scholar]
- 53.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78(1):309–323. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 54.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 55.Wolfson AR, Spaulding N, Dandrow C, Baroni E. Early versus late starting middle schools: the importance of a good night's sleep for young adolescents. Behav Sleep Med. 2007;5(3):194–209. doi: 10.1080/15402000701263809. [DOI] [PubMed] [Google Scholar]