Abstract
Primary iliac venous aneurysm is an exceedingly rare abnormality that can be complicated by pulmonary embolism, thrombosis, and rupture. Here we report the case of an otherwise healthy 40-year-old man with a unilateral external iliac vein aneurysm without any evidence of an arteriovenous fistula, proximal stenosis, or obstruction, as reported on computed tomography. Pulmonary embolism was diagnosed using 99mTc-macroaggregated albumin scintigraphy. To prevent life-threatening complications, we treated the patient with anticoagulant therapy and performed aneurysmectomy with reconstruction using a saphenous vein graft patch. Although postoperative venography showed obstruction of the external iliac vein, the patient remained asymptomatic.
Keywords: primary venous aneurysm, iliac vein, treatment
Introduction
Iliac venous aneurysm is an uncommon abnormality. Primary venous aneurysm, which is defined as a condition without an arteriovenous fistula, proximal stenosis, or obstruction, is particularly rare.1) The aneurysm may be associated with life-threatening complications, such as pulmonary thromboembolism, thrombosis, and rupture, followed by shock or cardiopulmonary arrest. Prior reports have shown several treatments, including anticoagulants, resection with venorrhaphy or patch plasty, and percutaneous coil embolization, were required for patients with primary venous aneurysm. In this report, we describe the case of a patient with a primary venous aneurysm of the right external vein; he was treated with tangential aneurysmectomy and reconstruction using a saphenous vein graft patch.
Case Report
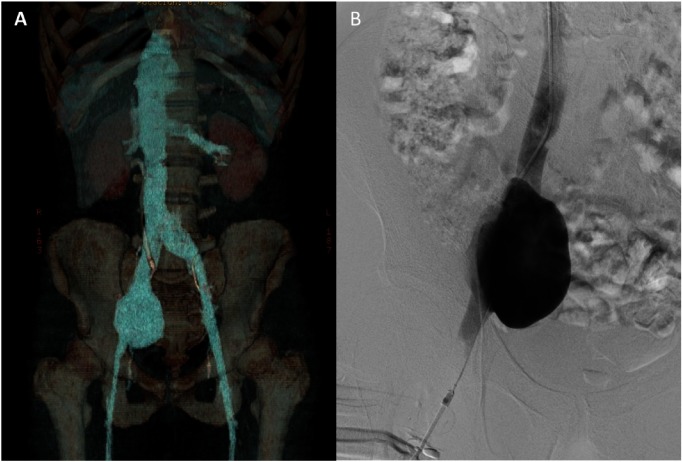
A 40-year-old male who complained of pain in the right inguinal region underwent abdominal ultrasonography, which revealed a 6-cm sacciform tumor in the right lower abdomen. The patient had no medical history including surgery, trauma, or inflammatory disease, and he was referred to our hospital for further evaluation. Enhanced computed tomography (CT) showed continuity between the cystic tumor, which measured 66 mm×72 mm, and the right external iliac vein (EIV) (Fig. 1A). Further, vascular ultrasonography indicated that the mass was a section of the ectatic vein. The mass was diagnosed as a right EIV aneurysm without stenosis or obstruction of the proximal flow. Although the patient did not present with any symptoms, 99mTc-macroaggregated albumin scintigraphy revealed a pulmonary thromboembolism in the inferior lobe of the right lung. Venography revealed a large saccular aneurysm of the EIV with flow stagnation (Fig. 1B), whereas arteriography of the common iliac artery did not indicate any sign of an arteriovenous fistula. Preoperative anticoagulant treatment with warfarin was initiated, and aneurysmectomy was recommended to prevent disastrous complications, such as massive pulmonary embolism and rupture.
Fig. 1 Preoperative imaging in a 40-year-old male with a unilateral EIV aneurysm. (A) A 3D-reconstructed computed tomography angiogram shows an aneurysm of the right EIV, with a maximal diameter of 66 mm×72 mm. (B) An ascending venogram reveals a large saccular aneurysm of the right EIV. EIV: external iliac vein.
One month after the aneurysm was diagnosed the patient underwent resection to treat the right EIV aneurysm. With the patient under general anesthesia, the aneurysm was exposed via a retroperitoneal incision in the right lower quadrant (Fig. 2A). The aneurysm did not adhere to the surrounding tissue and did not have feeding vessels. The border between the normal venous wall and the aneurysm was easily detectable. An abnormal venous wall occupied more than one-third of the circumference of the vein; therefore, compared to venorrhaphy, patch plasty was considered suitable to preserve the lumen. Following the intravenous administration of heparin (7,000 U), the proximal and distal portions of the aneurysmal sac were clamped, and longitudinal venotomy was performed. The excess vein wall was resected and did not show an adherent mural thrombus. The vessel wall was reconstructed using a saphenous vein graft patch taken from the opposite side, and sutured with continuous Nespylen 6-0 thread using the parachute technique. After the clamps were released, the patch was wrapped in the remaining wall of the aneurysmal vein (Fig. 2B). On histopathological examination, the three layers of resected venous wall were preserved and did not display signs of inflammation or fibrosis.
Fig. 2 Intraoperative findings of the external iliac venous aneurysm. (A) The venous aneurysm (white arrow), which was exposed through a retroperitoneal incision in the right lower quadrant, did not have feeding vessels. (B) After the excess vein wall was resected, the vessel wall was reconstructed using a saphenous vein graft patch that was taken from the opposite side. The patch was wrapped in the remaining wall of the aneurysmal vein.
After the 8-h surgery, anticoagulation was started with intravenous heparin: 15,000 U/day, with activated partial thromboplastin time (APTT) of 36.2 s. However, on postoperative day (POD) 1, bleeding from the retroperitoneal drain was aggravated, and anticoagulation therapy was stopped. After a 2-day intermission period, on POD 3, heparin was re-started along with warfarin. Ascending venography, which was performed on POD 6, revealed that the right EIV was completely occluded and there was good collateral flow into the common iliac vein without thrombosis in the vein below the inguinal ligament. On POD 13, venous ultrasonography revealed a hyperechoic thrombus of the EIV alone, which indicated organization and a lower risk of thromboembolism. The patient remained asymptomatic and was discharged on POD 14. Throughout the hospitalization period, the patient did not use either elastic compression stockings or an intermittent pneumatic compression device because we were apprehensive about promoting bleeding due to increased venous pressure.
At the 1-month follow-up interval, the patient appeared to be in good condition, ultrasonography did not show the development of a thrombosis, and there was no change regarding thrombotic obstruction in the right EIV. The patient performed manual labor and requested that the anticoagulant therapy be discontinued due to apprehension about trauma. Subsequently, anticoagulant therapy with warfarin was stopped because the risk of thromboembolism was considered to be low.
Discussion
To the best of our knowledge, only 16 cases of primary venous aneurysms of the iliac vein have been reported2–17) (Table 1). In these previously described patients, aneurysms did not seem to be prevalent in one particular sex, and the age of these patients ranged from 14 to 70 years (average age: 38 years). This demographic suggests that compared to other vascular diseases, primary venous aneurysm tends to manifest in younger patients. Aneurysms of the EIV occurred in 56% (9/16) of patients, whereas aneurysms of the common iliac vein and internal iliac vein were rare, occurring in 31% (5/16) and 13% (2/16) of patients, respectively.
Table 1 Published cases of primary aneurysms of the iliac vein.
| Author | Year | Age | Sex | Symptom | Location | Size (mm) | Thromboembolic complication | Operative procedure | Anticoagulant therapy |
|---|---|---|---|---|---|---|---|---|---|
| Postma2) | 1989 | 33 | M | Exercise intolerance, episodic hemoptysis | Lt. IIV | 30×120 | PTE | Ligation | + |
| Alatri4) | 1997 | 39 | F | None | Bilateral CIVs | 39×42×60 | — | No described | |
| 43×55×73 | |||||||||
| Petrunić3) | 1997 | 19 | M | Abdominal pain | Lt. CIV | 89×45 | Thrombosed aneurysm | Resection with lateral venorrhaphy | |
| Fourneau5) | 1998 | 21 | F | None | Lt. EIV | 50×100 | — | Resection with reconstruction with the SFV of the opposite side | |
| Alonso-Pérez6) | 2002 | 67 | M | Limb swelling and pain | Bilateral CIVs | 50 | DVT | Resection below the renal veins and ligation of the CIVs | + |
| Banno7) | 2004 | 20 | F | None | Lt. EIV | 80×60 | — | Resection with lateral venorrhaphy | + |
| Cañibano-Domínguez8) | 2007 | 70 | M | Limb swelling | Lt. CIV-EIV | 42 | DVT | No surgery | + |
| Kotsis9) | 2009 | 31 | F | None | Rt. EIV | 36 | — | Tangential aneurysmatectomy with lateral venorrhaphy | + |
| Ysa10) | 2010 | 30 | M | Limb swelling | Rt. IIV | 45 | DVT | No surgery | + |
| Humphries12) | 2010 | 32 | F | Left-sided abdominal pain | Bilateral EIV | 21×20 | — | No surgery | — |
| 38×41 | |||||||||
| Zou11) | 2011 | 14 | F | Dyspnea, syncope | Lt. EIV | Thrombosed aneurysm PTE | No surgery, IVC filter, mechanical fragmentation | + | |
| Ghidirim13) | 2011 | 59 | M | Abdominal pain, limb edema | Rt. CIV | Resection with lateral venorrhaphy | |||
| Hosaka14) | 2014 | 22 | F | Dyspnea | Lt. EIV | Thrombosed aneurysm PTE | Resection with reconstruction with the SFV | + | |
| Lucas15) | 2015 | 25 | M | Limb swelling and pain | Lt. EIV | 38 | — | Resection with lateral venorrhaphy | + |
| Park16) | 2016 | 63 | F | Right-sided abdominal pain, syncope, dyspnea | Rt. EIV | 40×50 | Rupture | Tangential aneurysmatectomy with lateral venorrhaphy | + |
| Audu17) | 2017 | 63 | M | Left testicular and inguinal pain | Lt. IIV | 31×22 | — | Percutaneous embolization | |
| Taki (current case) | 2017 | 40 | M | Right-sided abdominal pain | Rt. EIV | 66×72 | PTE | Resection with reconstruction with the GSV of the opposite side | + |
IIV: internal iliac vein; CIV: common iliac vein; EIV: external iliac vein; PTE: pulmonary thromboembolism; DVT: deep venous thrombosis; SFV: superficial femoral vein; IVC: inferior vena cava; GSV: great saphenous vein
Venous aneurysm is best described as a solitary area of venous dilatation that communicates with the main venous structure by a single channel, and which is not associated with arteriovenous communication or a pseudoaneurysm. Abbott et al. clearly defined a primary venous aneurysm as a fusiform or saccular lesion with no associated abnormality that increases blood flow or elevates venous pressure. The authors mentioned trauma, obstruction, and adjacent neoplasms as the causes of secondary venous aneurysms.18) Ysa et al. reported that arteriovenous fistulas, which commonly occur due to prior trauma, were the most common cause (41%) of iliac venous aneurysms; primary venous aneurysm being less frequent than other types (33%).1)
The most frequent clinical presentation of an iliac venous aneurysm is venous thrombosis (41%) followed by chronic venous insufficiency (32%).1) Our review of available literature revealed that most patients presented with abdominal pain or limb swelling, whereas only four patients had a diagnosis without exhibiting any symptoms. Seven patients (44%) developed thromboembolic complications such as deep venous thrombosis and pulmonary thromboembolism, and at least 10 patients (63%) were treated with anticoagulants. Rupture of the primary iliac venous aneurysm was reported in only one patient who was successfully treated with an operation. Among the 16 cases that were described in the literature, surgery was performed in ten cases (63%), resection with venorrhaphy or patch plasty was performed in nine, and ligation was performed in only two. Audu et al. demonstrated the efficacy of percutaneous coil embolization for primary venous aneurysms.17)
As few cases have been reported in the literature, no standard therapy or guideline for the management of pelvic primary venous aneurysms has been established. The therapeutic procedure should be decided in consideration of key aspects such as the aneurysm size, presence of thromboembolic complications, and the possibility of using anticoagulant therapy. In our case, 99mTc-macroaggregated albumin scintigraphy revealed a pulmonary thromboembolism, and ultrasonography revealed blood flow stagnation inside the aneurysm. Because these examinations indicated an imminent, life-threatening thromboembolic complication, it was essential to start anticoagulant therapy and perform aneurysmectomy.
Our review of the literature showed that the most popular treatment for a primary venous aneurysm was surgery; however, two reports demonstrated the efficacy of endovascular treatment of secondary venous aneurysms.17,19) Endovascular treatment includes coil embolization, inserting a bare metal stent into proximal venous stenosis, and deployment of a covered stent in the aneurysm.20) In our case, a stent grafting procedure may have been more effective and safer than conventional surgery in terms of bleeding and thrombotic events.
Postoperative thrombotic occlusion is believed to have occurred in our patient because of the interruption of heparin therapy. Ideally, postoperative anticoagulant therapy should be resumed as soon as possible to avoid postoperative thrombus formation. Elastic compression stockings or an intermittent pneumatic compression device should be used, especially in patients in whom anticoagulant therapy is suspended. In the current case, the EIV obstruction that occurred postoperatively may have been due to our decision not to use elastic compression stockings or an intermittent pneumatic compression device. Elastic compression stockings should have been used in the current case, even if there was a risk of bleeding.
Conclusion
To our knowledge, few cases of primary iliac venous aneurysms have been reported. We describe a case of primary venous aneurysm in the EIV that was treated with aneurysmal resection followed by reconstructive patch plasty. To prevent thromboembolic complications or rupture, anticoagulant treatment and surgical or percutaneous therapy should be considered in patients with primary iliac venous aneurysms, even if the patient is asymptomatic.
Disclosure Statement
The authors declare no conflict of interest.
Author Contributions
Writing: MT, TM
Critical review and revision: TM, TK, TK, TM, MH, YM, FY
Final approval of the article: all authors
Accountability for all aspects of the work: TM
References
- 1).Ysa A, Bustabad MR, Arruabarrena A, et al. Thrombosed iliac venous aneurysm: a rare form of presentation of a congenital anomaly of the inferior vena cava. J Vasc Surg 2008; 48: 218-22. [DOI] [PubMed] [Google Scholar]
- 2).Postma MP, McLellan GL, Northup HM, et al. Aneurysm of the internal iliac vein as a rare source of pulmonary thromboembolism. South Med J 1989; 82: 390-2. [DOI] [PubMed] [Google Scholar]
- 3).Petrunić M, Kruzić Z, Tonković I, et al. Large iliac venous aneurysm simulating a retroperitoneal soft tissue tumour. Eur J Vasc Endovasc Surg 1997; 13: 221-2. [DOI] [PubMed] [Google Scholar]
- 4).Alatri A, Radicchia S. Bilateral aneurysm of the common iliac vein: a case report. Ann Ital Med Int 1997; 12: 92-3. (in Italian) [PubMed] [Google Scholar]
- 5).Fourneau I, Reynders-Frederix V, Lacroix H, et al. Aneurysm of the iliofemoral vein. Ann Vasc Surg 1998; 12: 605-8. [DOI] [PubMed] [Google Scholar]
- 6).Alonso-Pérez M, Segura RJ, Vidal ED. Thrombosed aneurysm of the infrarenal vena cava: diagnosis and treatment. J Cardiovasc Surg (Torino) 2002; 43: 507-10. [PubMed] [Google Scholar]
- 7).Banno H, Yamanouchi D, Fujita H, et al. External iliac venous aneurysm in a pregnant woman: a case report. J Vasc Surg 2004; 40: 174-8. [DOI] [PubMed] [Google Scholar]
- 8).Cañibano-Domínguez C, Acín F, Martinez-Aguilar E, et al. Primary iliac venous aneurysm: a case report and review of the literature. Angiología 2007; 59: 277-82. (in Spanish) [Google Scholar]
- 9).Kotsis T, Mylonas S, Katsenis K, et al. External iliac venous aneurysm treated with tangential aneurysmatectomy and lateral venorrhaphy: a case report and review of the literature. Vasc Endovascular Surg 2009; 42: 615-9. [DOI] [PubMed] [Google Scholar]
- 10).Ysa A, Gainza E, Bustabad MR, et al. Primary venous aneurysm of the internal iliac vein. J Vasc Surg 2010; 51: 735. [DOI] [PubMed] [Google Scholar]
- 11).Zou J, Yang H, Ma H, et al. Pulmonary embolism caused by a thrombosed external iliac venous aneurysm. Ann Vasc Surg 2011; 25: 982.e15-8. [DOI] [PubMed] [Google Scholar]
- 12).Humphries MD, Dawson DL. Asymptomatic bilateral external iliac vein aneurysms in a young athlete: case report and literature review. Vasc Endovascular Surg 2010; 44: 594-6. [DOI] [PubMed] [Google Scholar]
- 13).Ghidirim G, Mişin I, Gagauz I, et al. Anevrism al venei iliace comune drepte: prezentare de caz și revista literaturii. [Iliac venous aneurysm: a case report and review of literature.] Chirurgia (Bucur) 2011; 106: 269-72. (in Romanian) [PubMed] [Google Scholar]
- 14).Hosaka A, Miyata T, Hoshina K, et al. Surgical management of a primary external iliac venous aneurysm causing pulmonary thromboembolism: report of a case. Surg Today 2014; 44: 1771-3. [DOI] [PubMed] [Google Scholar]
- 15).Lucas ML, Martins TB, Aerts N. Tratamento cirúrgico de um aneurisma primário de veia ilíaca externa. [Surgical treatment of a primary external iliac vein aneurysm.] J Vasc Bras 2015; 14: 267-70. (in Portuguese) [Google Scholar]
- 16).Park JS, Kim JY, Kim M, et al. Ruptured aneurysm of the external iliac vein. J Vasc Surg Venous Lymphat Disord 2016; 4: 92-4. [DOI] [PubMed] [Google Scholar]
- 17).Audu CO, Boniakowski AE, Robinson S, et al. Internal iliac venous aneurysm associated with pelvic venous insufficiency. J Vasc Surg Venous Lymphat Disord 2017; 5: 257-60. [DOI] [PubMed] [Google Scholar]
- 18).Abott OA, Leigh TF. Aneurysmal dilatations of the superior vena caval system. Ann Surg 1964; 159: 858-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Stewart JK, Miller MJ, Semmel DJ, et al. Endovascular treatment of May–Thurner syndrome-related symptomatic venous aneurysm. J Vasc Interv Radiol 2017; 28: 1330-2. [DOI] [PubMed] [Google Scholar]
- 20).Favelier S, Estivalet L, Pottecher P, et al. Successful endovascular treatment of a large azygos vein aneurysm with stent-graft implantation. Ann Thorac Surg 2015; 99: 1455. [DOI] [PubMed] [Google Scholar]