Abstract
Immunoglobulin G4-related diseases (IgG4-RD) are systemic inflammatory conditions, characterized by high serum IgG4 concentrations, and pathologically IgG4-positive plasmacytes infiltrations and storiform fibrosis. We described IgG4-related inflammatory abdominal aortic aneurysm in 2008, and revealed the existence of vascular lesions. IgG4-related vascular lesions frequently occur in the aorta and branching medium-sized arteries with or without aneurysmal change. The inflammatory lesion mainly involves in the adventitia, indicating remarkable adventitial fibrous thickening with infiltration of inflammatory cells. Clinical symptoms associated with IgG4-related vascular lesions might be fever, abdominal pain, hydronephrosis, or few subjective symptoms. Comprehensive diagnostic criteria is applied according to image findings of thickening lesions, high serum IgG4 levels, and histopathological findings. As a treatment, open surgical repair or endovascular aneurysm repair is performed for the aneurysmal cases, and steroid administration is used for the cases with strong inflammation. This disease can lead to a lethal situation due to the rupture following aneurysmal formation, thus special attention is needed unlike IgG4-RD occupying in the other organs. (This is a translation of Jpn J Vasc Surg 2017; 26: 129–134.)
Keywords: inflammatory abdominal aortic aneurysm, aortitis, arteritis, inflammation
Introduction
IgG4-related disease (immunoglobulin G4-related disease; IgG4-RD) is a systemic disease characterized by high serum IgG4 levels and marked IgG4-positive plasma cell infiltration and fibrosis in the affected tissues.1,2) IgG4-RD is characterized by common among elderly men, the disease affects multiple organs synchronously and metachronously and responds well to steroids. Its etiology remains unknown. It was selected as a designated intractable disease in 2015. Since Hamano et al. reported IgG4-RD in autoimmune pancreatitis in 2001,3) IgG4-RD has been found in various systemic organs, such as Mikulicz’s disease, sclerosing cholangitis, pulmonary inflammatory pseudotumor, and retroperitoneal fibrosis.1,2) In 2008, we revealed that some inflammatory abdominal aortic aneurysms (IAAAs) are IgG4-RDs (IgG4-related IAAAs)4) and that IgG4-RD could occur in blood vessels. Since then, the spectrum of vascular lesions has expanded to include the thoracic aorta5) and medium-sized arteries.6,7) Given that IgG4-related vascular lesions can cause fatal situations through aneurysm formation with rupture, unlike IgG4-RD in other organs, particular attention is required in medical care. In this study, we describe what is currently known about IgG4-related vascular lesions, including clinical and pathological features and diagnostic criteria, and also discuss treatment and prognosis of this disease including those from our own experiences.
Disease Concept
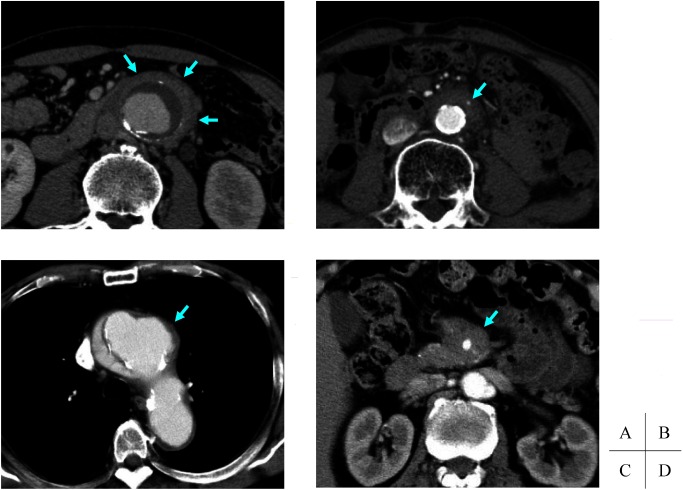
The most frequently affected site of IgG4-related vascular lesions is the abdominal aorta, which often presents as an IAAA (Fig. 1A). IAAA is a special subtype of abdominal aortic aneurysm (AAA) characterized by marked thickening of the aortic wall, particularly fibrosis of the adventitia and numerous inflammatory cell infiltration.8) Our study has shown that IgG4-RD (IgG4-related IAAA) accounts for about half of IAAAs.9) In addition, similar lesions but without increased vascular diameter (i.e., aneurysm is not involved) are referred to as IgG4-related periaortitis (IgG4-related periaortitis) (Fig. 1B). The two conditions differ only in the presence or absence of aneurysms and are considered similar in terms of pathogenic/pathological terms. While regular vasculitis affects the intima and media, the primary locus of the inflammation in the adventitia is a major characteristic of IgG4-related vascular lesions.
Fig. 1 Contrast-enhanced computed tomography (CT). (A) IgG4-related inflammatory abdominal aortic aneurysm. The aneurysmal wall shows severe thickening, and it looks like a soft tissue mass surrounding the aorta. An enhanced thickening of the adventitia forms ‘mantle sign’ (arrows). (B) IgG4-related periaortitis. Marked thickening of the aortic wall without aneurysmal change is shown. The inferior mesenteric artery penetrates the lesion without stenosis (arrow). (C) IgG4-related disease of the thoracic aorta. CT shows a saccular aneurysm with a mild wall thickening (arrow). (D) IgG4-related disease of the superior mesenteric artery. CT shows a soft tissue mass surrounding the artery (arrow).
In addition to aortic aneurysms, IgG4-RD in the thoracic aorta shows various features, such as aortic dissection, lymphoplasmacytic aortitis, and isolated aortitis5,10) (Fig. 1C). Wall thickening is relatively mild compared with abdominal lesions. Intense inflammation is also characteristically found in the media, and the condition is also referred to as IgG4-related aortitis.
IgG4-RD of medium-sized arteries occurs in the 1st and 2nd branches of the aortas, such as the coronary artery, superior mesenteric artery, and iliac artery.6,7) While lesions in the iliac artery resemble those in the abdominal aorta, many cases with lesions in the coronary artery and superior mesenteric artery show periarteritis characterized by mass formation around the artery without expansion of the arterial lumen (Fig. 1D). In peripheral arteries, IgG4-related femoral/popliteal artery aneurysm has been reported, in which saccular aneurysms are common and thickening of the arterial wall is insignificant.
Epidemiology
IgG4-related arterial lesions, like those in other organs, are common in elderly men. Given that IAAAs account for 3%–10% of AAAs11) and about half of IAAA cases are IgG4-related, 1%–5% of AAA cases are estimated to be IgG4-RD. Since lesions of the thoracic aorta are less common and show various pathologies, details are unclear. In Stone et al.’s analysis of 638 thoracic aortic resection specimens, however, 0.5% of all specimens and 9% of noninfectious aortitis were IgG4-RD.10) Among our cases, IgG4-RD was found in 4% of 125 patients who underwent surgery for thoracic aortic disease.5) Although the frequency is unknown for medium-sized arterial lesions, it is believed to be even lower.
Inoue et al. studied 235 patients with IgG4-RD and found aortic lesions in 20% and arterial lesions in 4% of all patients.12) In addition, Perugino et al. reported that macrovascular lesions were found in 22.5% of 165 patients with IgG4-RD.13) In the nationwide survey in 2011, the number of patients with IgG4-RD was approximately 10,000–20,000, which suggested that 2,000–4,000 patients had IgG4-related arterial lesions.
Etiology
The etiology of IgG4-RD remains unknown. The helper T cell (Th) balance has attracted attention, and various cytokines released from increased regulatory T cells under a Th2-dominant immune environment have been suggested to induce fibrosis and IgG4-positive plasma cell infiltration.1,2) For arterial lesions with aneurysm, the time sequence of aneurysm formation and development of IgG4-RD are not clear, but it seems reasonable to speculate that intensive inflammatory cell infiltration with primary focus in the adventitia results in weakened wall to cause aneurysm. In fact, Inoue et al. have reported images of the destructed elastic fibers in the media due to the effects of inflammation in the adventitia.14)
Clinical Features
Cases with strong inflammatory fibrous hypertrophy, such as IgG4-related IAAAs, are often associated with symptoms such as fever, abdominal pain/lower backache, and weight loss, and hydronephrosis and intestinal obstruction can occur due to involution of surrounding internal organs, including the ureter and gastrointestinal tract. On the contrary, subjective symptoms are rarely noted in cases of arterial (aortic) aneurysm and periarteritis (periaortitis) with mild wall thickening. The complication by allergic diseases is frequently observed, and the rate of complication by autoimmune diseases is also high.4,9) The complications by IgG4-RD in other organs are also found.12) Serologically, immunoglobulin E (IgE) is also often elevated in addition to high IgG4 levels. C-reactive protein level is also often elevated, but relatively mildly. Complements are normal or mildly decreased, and the positive rate of antinuclear antibodies is high.
Image Findings
On computed tomography, a lesion is depicted as circumferential thickening of the adventitia of the artery (aorta) or as a uniform soft mass spreading around it14) (Figs. 1A–1D). The so-called mantle sign, which is contrasted in the late post-contrast phase, is often seen (Fig. 1A), but is not a finding unique to this disease as it is also observed for non-IgG4-related lesions. In addition, the finding that the lumbar artery or inferior mesenteric artery penetrates through the lesion without undergoing stenosis is occasionally obtained (Fig. 1B). Fluorodeoxyglucose-positron emission tomography has been reported to have superior sensitivity in the detection of organ lesions of IgG4-RD and correlate with lesion activity.15)
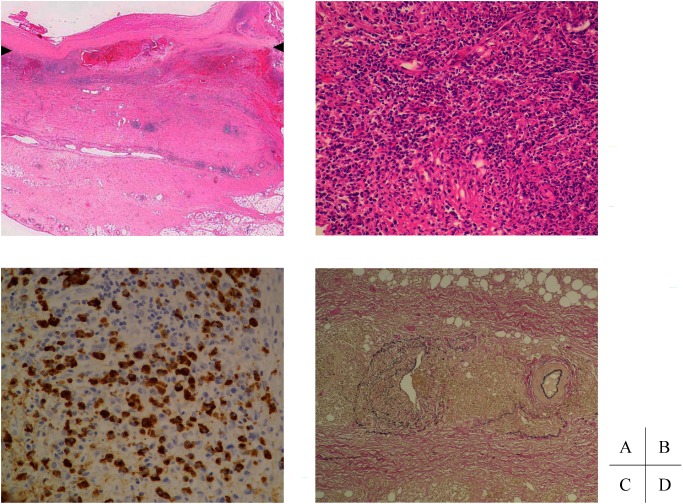
Histopathological Features
Histologically, severe fibrosis from the adventitia to the adipose tissue is observed4,9) (Fig. 2A). With the adventitia as the primary focus, a high degree of lymphoplasmacytic infiltration (Fig. 2B) and many lymphoid follicles are found, and IgG4-positive plasma cells are distributed diffusively and extensively in the entire connective tissue outgrowth (Fig. 2C). General histological features characteristic to IgG4-RD are also seen, such as storiform fibrosis, eosinophil infiltration, and obliterative phlebitis (Fig. 2D). Lymphoplasmacytic infiltration around the nerve bundle is also frequently observed in the adventitia. Neutrophil infiltration and granuloma formation are rarely seen.
Fig. 2 Histological findings of IgG4-related inflammatory abdominal aortic aneurysm. (A) HE-staining. Arrowheads indicate the lower end of the media. The adventitia is markedly thickened due to inflammatory cell infiltration accompanied by fibrous proliferation. (B) HE-staining. Dense lymphoplasmacytic infiltration with fibrosis is observed. (C) Immunostaining of IgG4. Diffuse infiltration by a large number of IgG4-positive cells is noted. (D) EVG staining. Obstructive phlebitis is observed (left).
Diagnosis and Differential Diagnosis
Currently, organ-specific diagnostic criteria for IgG4-related vascular lesions are being prepared, and comprehensive diagnostic criteria16) are used for diagnosis (Table 1). Specific criteria are (1) image findings (hypertrophic lesions of the arterial wall), (2) hyper IgG4emia (≥135 mg/dL), and (3) histopathological findings. A definitive diagnosis is made when 1+2+3 are all met; meanwhile, a semi-definitive diagnosis is made when only 1+3 are met, and patients are suspected if only 1+2 are met. Thus, histopathological examinations are essential for semi-definitive or stronger diagnosis, which requires observing marked lymphoplasmacytic infiltration and fibrosis, an IgG4/IgG positive cell ratio of ≥40%, and an IgG4 positive plasma cell count exceeding 10/high power field. In recent years, endovascular therapy has been the mainstream treatment for aortic aneurysms, and since resected specimens are often unavailable and performing biopsies at the affected site is difficult, diagnosis has become increasingly difficult. In many cases, the diagnosis is made comprehensively based on the presence of lesions in other organs in addition to imaging and serological findings. Note that the sensitivity for hyper IgG4emia has been reported to be approximately 90%.17)
Table 1 Comprehensive clinical diagnostic criteria for IgG4-related disease.
| 1. Clinical examination showing characteristic diffuse/localized swelling or masses in single or multiple organs |
| 2. Hematological examination shows elevated serum IgG4 concentrations (135 mg/dL) |
| 3. Histopathologic examination shows: |
| (1) Marked lymphocyte and plasmacyte infiltration and fibrosis. |
| (2) Infiltration of IgG4+ plasma cells: ratio of IgG4+/IgG+cells >40% and >10 IgG4+ plasma cells/HPF |
| Definite: 1)+2)+3) |
| Probable: 1)+3) |
| Possible: 1)+2) |
| However, it is important to differentiate IgG4-RD from malignant tumors of each organ (e.g., cancer, lymphoma) and similar diseases (e.g., Sjögren’s syndrome, primary sclerosing cholangitis, Castleman’s disease, secondary retroperitoneal fibrosis, Wegener’s granulomatosis, sarcoidosis, Churg–Strauss syndrome) by additional histopathological examination. |
| Even when patients cannot be diagnosed using the CCD criteria, they may be diagnosed using organ-specific diagnostic criteria for IgG4-RD. |
HPF: high power field; CCD: comprehensive clinical diagnostic
Non-IgG4-related IAAAs and periarteritis (periaortitis) needed to be differentiated; however, this is difficult based on clinical symptoms and image findings, and serological data and histopathological findings are necessary. In addition, differentiation from infectious aortic aneurysm may be required when findings indicate severe inflammation, and this can be achieved based on image findings such as irregular saccular aneurysms and rapid enlargement, blood culturing, and infectious disease markers. Differential features include the frequency of aortitis syndrome among young women and visualization of transmural wall thickening on images as well as the presence of stenosis, occlusion, and calcification. Differentiation of malignant lymphomas as tumor-forming lesions around the artery may be required, and attention should be paid to clinical symptoms and lymph node enlargement; biopsy of the affected site is required where differentiation is difficult.
Treatment and Prognosis
Some patients with IgG4-RD are known to improve spontaneously, and follow-up observation may be sufficient if arterial lesions are asymptomatic and no aneurysms are formed. Since steroids are effective for IgG4-RD, steroid therapy is used at the discretion of the attending physician for symptomatic relief when the patient has inflammatory symptoms, such as fever and abdominal pain/lower backache or passage obstruction due to involution of surrounding organs. According to the treatment of autoimmune pancreatitis, prednisolone at a starting dose of 0.6 mg/kg/day, which is gradually reduced to a maintenance dose of approximately 5 mg/day, is often used18); however the optimum dose for vascular lesions has not been fully investigated. In addition, there is no consensus regarding the duration of administration, and the disease may relapse after stopping medication. Note that steroid therapy could not prevent arterial aneurysm formation or rupture. Previous reports stated that 96% of perivascular lesions of periarteritis (periaortitis) shrunk by steroid therapy19); however, when lumen enlargement or aneurysm formation is observed before treatment, the blood vessel diameter also increased. Moreover, studies reported on periaortitis where rupture occurred due to rapid thinning of the aortic wall,20,21) and steroids should be carefully used. Rituximab is tested as an alternative to steroid therapy.22)
IgG4-related vascular disease with aneurysm formation have risks of rupture. They are treated with surgery, such as arterial graft replacement and stent grafting depending on the aneurysm diameter and growth rate according to the standard of treatment indication for usual aneurysms. Postoperative steroid combination therapy has also been reported for cases of persistent inflammation findings with abdominal pain and hydronephrosis. Among our cases, patients with IgG4-related IAAA who underwent graft replacement follow a relatively favorable postoperative course. In recent years, stent grafting has advantages of not requiring detachment of adhesion to the surroundings and has been used increasingly. However, whether the adequate efficacy can be obtained for both rupture prevention and improving inflammation findings is currently under investigation.
Conclusion
IgG4-related vascular lesions were outlined. This disease differs from other organ lesions in that aneurysm formation and rupture can cause a fatal complication, which appears to have a serious effect on the prognosis of this disease. While steroids are effective for improving inflammation, they can weaken arterial walls; thus, requiring adequate caution when they are used. Another characteristic of IgG4-RD is frequent relapses, and long-term close observation is considered necessary even for patients who spontaneously improved or underwent surgical treatment. We believe that our understanding of the pathology and clinical course of this disease can advance and the prognosis can be improved by accumulating and analyzing more cases.
Disclosure Statement
All authors and co-authors have no conflict of interest related to this article.
This is a translation of Jpn J Vasc Surg 2017; 26: 129–134.
Additional Remarks
The work was presented at the 24th Educational Seminar of the Japanese Society for Vascular Surgery (2016, Nara).
References
- 1).Kamisawa T, Zen Y, Pillai S, et al. IgG4-related disease. Lancet 2015; 385: 1460-71. [DOI] [PubMed] [Google Scholar]
- 2).Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med 2012; 366: 539-51. [DOI] [PubMed] [Google Scholar]
- 3).Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med 2001; 344: 732-8. [DOI] [PubMed] [Google Scholar]
- 4).Kasashima S, Zen Y, Kawashima A, et al. Inflammatory abdominal aortic aneurysm: close relationship to IgG4-related periaortitis. Am J Surg Pathol 2008; 32: 197-204. [DOI] [PubMed] [Google Scholar]
- 5).Kasashima S, Zen Y, Kawashima A, et al. A clinicopathologic study of immunoglobulin G4-related sclerosing disease of the thoracic aorta. J Vasc Surg 2010; 52: 1587-95. [DOI] [PubMed] [Google Scholar]
- 6).Kasashima S, Kawashima A, Endo M, et al. A clinicopathologic study of immunoglobulin G4-related disease of the femoral and popliteal arteries in the spectrum of immunoglobulin G4-related periarteritis. J Vasc Surg 2013; 57: 816-22. [DOI] [PubMed] [Google Scholar]
- 7).Matsumoto Y, Kasashima S, Kawashima A, et al. A case of multiple immunoglobulin G4-related periarteritis: a tumorous lesion of the coronary artery and abdominal aortic aneurysm. Hum Pathol 2008; 39: 975-80. [DOI] [PubMed] [Google Scholar]
- 8).Walker DI, Bloor K, Williams G, et al. Inflammatory aneurysms of the abdominal aorta. Br J Surg 1972; 59: 609-14. [DOI] [PubMed] [Google Scholar]
- 9).Kasashima S, Zen Y, Kawashima A, et al. A new clinicopathological entity of IgG4-related inflammatory abdominal aortic aneurysm. J Vasc Surg 2009; 49: 1264-71; discussion, 1271. [DOI] [PubMed] [Google Scholar]
- 10).Stone JH, Khosroshahi A, Deshpande V, et al. IgG4-related systemic disease accounts for a significant proportion of thoracic lymphoplasmacytic aortitis cases. Arthritis Care Res (Hoboken) 2010; 62: 316-22. [DOI] [PubMed] [Google Scholar]
- 11).Rasmussen TE, Hallett JW Jr. Inflammatory aortic aneurysms. A clinical review with new perspectives in pathogenesis. Ann Surg 1997; 225: 155-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Inoue D, Yoshida K, Yoneda N, et al. IgG4-related disease: dataset of 235 consecutive patients. Medicine 2015; 94: e680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Perugino CA, Wallace ZS, Meyersohn N, et al. Large vessel involvement by IgG4-related disease. Medicine 2016; 95: e3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Inoue D, Zen Y, Abo H, et al. Immunoglobulin G4-related periaortitis and periarteritis: CT findings in 17 patients. Radiology 2011; 261: 625-33. [DOI] [PubMed] [Google Scholar]
- 15).Zhang J, Chen H, Ma Y, et al. Characterizing IgG4-related disease with 18F-FDG PET/CT: a prospective cohort study. Eur J Nucl Med Mol Imaging 2014; 41: 1624-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol 2012; 22: 21-30. [DOI] [PubMed] [Google Scholar]
- 17).Carruthers MN, Khosroshahi A, Augustin T, et al. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis 2015; 74: 14-8. [DOI] [PubMed] [Google Scholar]
- 18).Kamisawa T, Shimosegawa T, Okazaki K, et al. Standard steroid treatment for autoimmune pancreatitis. Gut 2009; 58: 1504-7. [DOI] [PubMed] [Google Scholar]
- 19).Mizushima I, Inoue D, Yamamoto M, et al. Clinical course after corticosteroid therapy in IgG4-related aortitis/periaortitis and periarteritis: a retrospective multicenter study. Arthritis Res Ther 2014; 16: R156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Kasashima S, Kawashima A, Kasashima F, et al. Immunoglobulin G4-related periaortitis complicated by aortic rupture and aortoduodenal fistula after endovascular AAA repair. J Endovasc Ther 2014; 21: 589-97. [DOI] [PubMed] [Google Scholar]
- 21).Tajima M, Hiroi Y, Takazawa Y, et al. Immunoglobulin G4-related multiple systemic aneurysms and splenic aneurysm rupture during steroid therapy. Hum Pathol 2014; 45: 175-9. [DOI] [PubMed] [Google Scholar]
- 22).Carruthers MN, Topazian MD, Khosroshahi A, et al. Rituximab for IgG4-related disease: a prospective, open-label trial. Ann Rheum Dis 2015; 74: 1171-7. [DOI] [PubMed] [Google Scholar]