Abstract
Rationale:
Intravascular leiomyomatosis (IVL) is a rare nonmalignant tumor that can be fatal if untreated.
Patient concerns:
A 49-year-old nulliparous Asian woman who underwent hysterectomy and left salpingo-oophorectomy for multiple uterine leiomyomas 18 months prior presented complaining of intermittent palpitation and chest tightness for approximately 1 month. Echocardiography revealed a large mobile tumor mass extending from the inferior vena cava (IVC) to the right atrium that partially obstructed IVC flow and tricuspid inflow. Thoracicabdominopelvic computed tomography revealed a left adnexal tumor (4.8 × 2.5 cm) causing intravascular obstruction extending from the left internal iliac vein to the IVC, right atrium, and right ventricle.
Diagnosis:
IVL with right heart involvement
Interventions:
Under cardiopulmonary bypass, a one-stage surgery combining sternotomy and laparotomy was performed. The tumor was approached and extracted via sternotomy, and tumor detachment and removal of residual tumors was accomplished via laparotomy.
Outcomes:
A firm, smooth, and regularly shape tumor 15.5 × 5.5 × 2.5 in size was completely removed and histopathologically confirmed as IVL. The patient tolerated the surgical procedure well and no postoperative complication was noted.
Lessons:
We describe a one-stage surgical approach to completely remove an IVL extending to the right ventricle.
Keywords: intracardiac tumor, intracaval tumor, intravascular leiomyomatosis, uterine leiomyoma
1. Introduction
Benign uterine leiomyomas are the most common pelvic tumors in women.[1] Intravascular leiomyomatosis (IVL) is a variant of leiomyoma characterized by intravascular proliferation of a histologically benign smooth muscle tumor extending beyond the uterus into distant great vessels or the heart. Although histologically benign, the condition may lead to heart failure or death if left untreated. Currently, complete surgical removal is the treatment of choice.[2] In the case presented herein, we successfully removed both intravascular and intracardiac components of an IVL utilizing a one-stage surgery combining sternotomy and laparotomy.
2. Case presentation
A 49-year-old nulliparous Asian woman presented at our cardiovascular center in March 2017 complaining of intermittent palpitation and chest tightness for approximately one month. She had undergone hysterectomy and left salpingo-oophorectomy for multiple uterine leiomyomas 18 months prior. She had no other history of major systemic disease. On evaluation of vital signs, her heart rate was 86 beats per minute, blood pressure was 122/84 mm Hg, respiratory rate was 18 breaths per minute, and body temperature was 36.9°C. Results of routine blood and urine laboratory tests were normal. Transthoracic and transesophageal echocardiography revealed a large mobile tumor mass in the right-heart chamber extending from the inferior vena cava (IVC) to the right atrium, partially obstructing IVC flow and tricuspid inflow. The intracardiac portion of the tumor mass was 4.0 × 1.8 cm in size. Thoracoabdominopelvic computed tomography revealed intravascular obstruction from the IVC to the right atrium and right ventricle (Fig. 1A–C). Computed tomography showed a 4.8 × 2.5 cm tumor at the left adnexa which completely occluded the left internal iliac vein and partially occluded the IVC (Fig. 1D–F).
Figure 1.
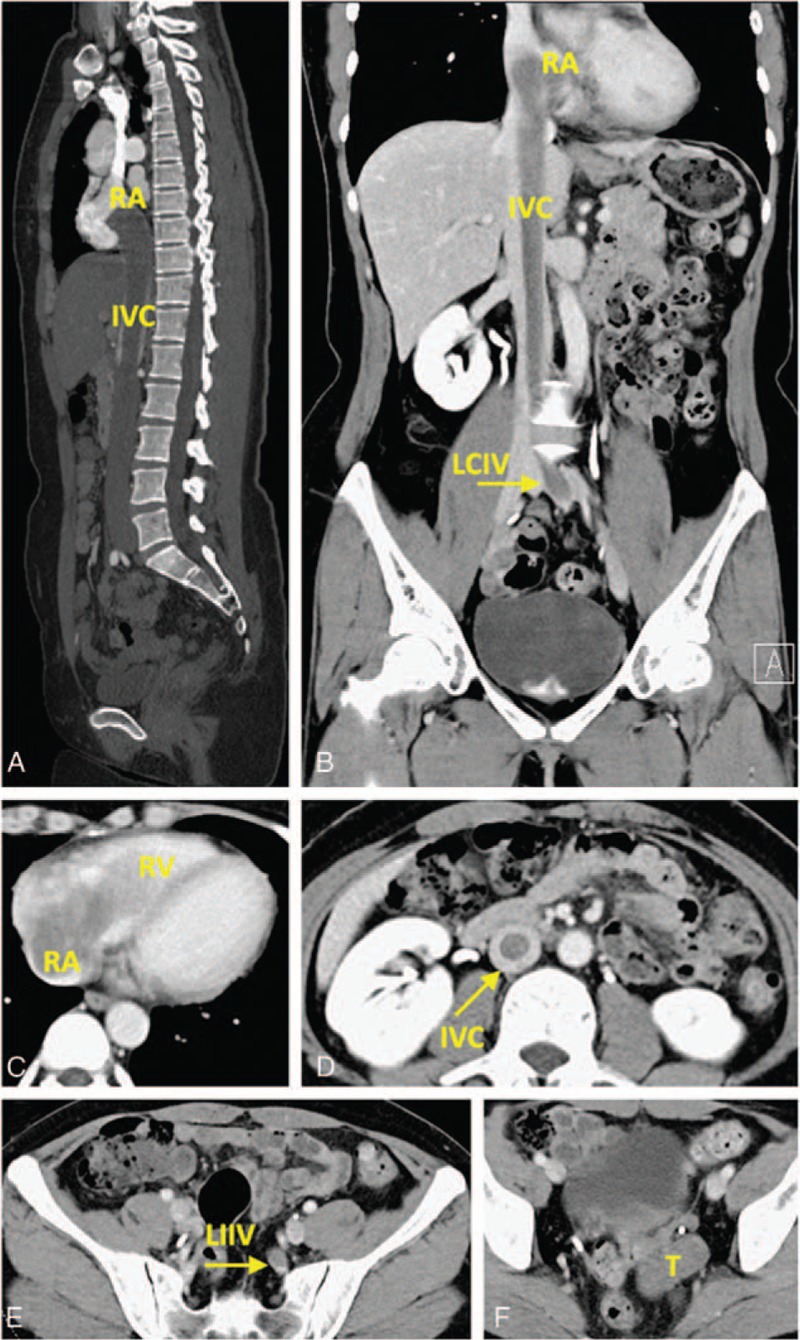
(A, B) Computed tomography showed a mass extending from left internal iliac vein to right ventricle. (C) The intracardiac tumor extended to right atrium and right ventricle. (D) The intracaval tumor. (E) The left internal iliac vein was totally occluded. (F) A tumor mass about 4.8 × 2.5 cm in size at the left adnexa. IVC = inferior vena cava, LCIV = left common iliac vein, LIIV = left internal iliac vein, RA = right atrium, RV = right ventricle, T = left adnexa tumor.
A one-stage surgery was performed to remove the intracardiac and intravascular portions of the mass concurrently. First, the right atrium and right ventricle were exposed via sternotomy, and the IVC was exposed via laparotomy (Fig. 2A). Cardiopulmonary bypass was established by cannulating the ascending aorta with venous drainage through the right atrium and superior vena cava (SVC, Fig. 2B). The right atrium was then opened to reveal the intracardiac part of the tumor mass (Fig. 2B) and the IVC was longitudinally incised at the iliac bifurcation to reveal the intravascular portion (Fig. 2C). After the proximal and distal parts of the tumor mass were controlled, the intravascular part of the mass was detached through the inferior cava venotomy and the entire tumor was extracted from the right atriotomy. Finally, the left common iliac vein was incised to excise the residual tumor.
Figure 2.
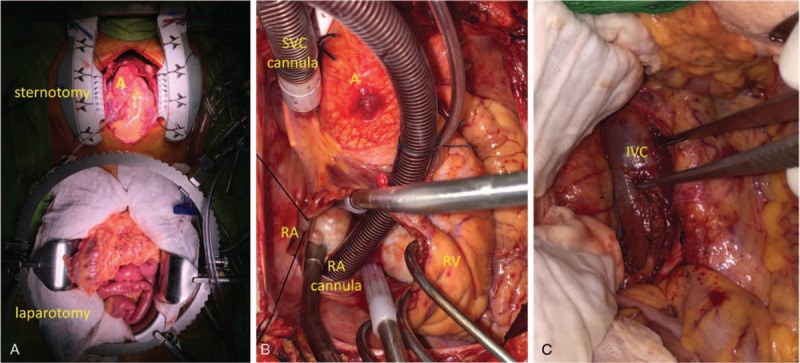
(A) Sternotomy and laparotomy were performed to expose the right atrium, right ventricle, and inferior vena cava. (B) Atriotomy was performed and the intracardiac part of the tumor mass was exposed. (C) The intracaval part of the tumor mass was detached through an inferior cava venotomy. A = aorta, IVC = inferior vena cava, RA = right atrium, RV = right ventricle, SVC = superior vena cava.
The patient tolerated the procedure well, and the postoperative course was uneventful without complications or need for additional treatment. Grossly, the tumor mass was firm, smooth, regularly shaped, and 15.5 × 5.5 × 2.5 cm in size. The mass originated from the left common iliac vein and extended to the IVC, right atrium, and right ventricle (Fig. 3). Histopathological examination revealed proliferating smooth muscle fibers with no abnormal mitotic activity, which is consistent with IVL. The patient provided written informed consent for publication of this report and all accompanying images.
Figure 3.

A firm, smooth, regularly shaped tumor 15.5 × 5.5 × 2.5 in size, originated from left internal iliac vein and extended to inferior vena cava, right atrium, and right ventricle. IVC = inferior vena cava, RA = right atrium, RV = right ventricle.
3. Discussion
IVL typically affects premenopausal women, particularly those who have undergone hysterectomy or myomectomy for uterine leiomyomas. Previous reports indicate that IVL develops in only 0.1% of uterine leiomyomas and that 10% to 40% of IVL cases exhibit intracardiac involvement.[3–5] IVL with intracardiac extension was first reported in 1907,[6] and since then, fewer than 300 cases have been documented in the literature. Although histologically and cytopathologically benign, IVL may behave in a malignant manner and may be fatal due to involvement of distant organs or great vessels.
Currently, complete surgical resection is the treatment of choice for IVL,[2] and the surgical strategy should be tailored to anatomic characteristics. In our patient, the maximum diameter of the intracardiac part of the IVL was larger than the diameter of the IVC. Thus, removal of both intracardiac and intravascular parts of the IVL via right atriotomy was initially planned. However, as IVL is usually attached to the pelvic veins due to origination from previous uterine leiomyoma,[7] blindly pulling out the tumor would be dangerous; therefore, the intravascular portion of the IVL was detached through the inferior cava venotomy. Similar to previously reported cases, in our case, the distal part of the IVL was the most strongly attached, whereas the intracardiac part was freely movable and not attached to adjacent endocardial surface. The middle region of the IVC was also entirely freely floating.[4,7,8] In summary, in this patient, IVL was successfully resected utilizing a one-stage surgical approach that combined sternotomy to approach and extract the IVL with laparotomy for IVL detachment and removal of the residual tumor. In addition, circulatory arrest was not required as cardiopulmonary bypass was established through cannulation of the SVC and the ascending aorta, further reducing operative and anesthetic risks.
Although patients with IVL often present with nonspecific symptoms, advances in imaging technology allow prompt diagnosis of the condition.[9] In addition, a precise surgical plan should be customized based on IVL features and individual patient characteristics.
4. Conclusion
In this case report, we describe a one-stage surgical approach to completely remove an IVL with right ventricle involvement.
Footnotes
Abbreviations: IVC = inferior vena cava, IVL = intravascular leiomyomatosis, SVC = superior vena cava.
Ethics approval and consent to participate:
Though ethical approval was not required for this case report, the patient provided written informed consent for publication and use of all accompanying images.
Consent for publication: The patient provided written informed consent for publication of this report and use of all accompanying images.
The authors have no funding and no conflicts of interest to disclose.
References
- [1].Buttram VC, Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril 1981;36:433–45. [DOI] [PubMed] [Google Scholar]
- [2].Castelli P, Caronno R, Piffaretti G, et al. Intravenous uterine leiomyomatosis with right heart extension: successful two-stage surgical removal. Ann Vasc Surg 2006;20:405–7. [DOI] [PubMed] [Google Scholar]
- [3].Andrade LA, Torresan RZ, Sales JF, Jr, et al. Intravenous leiomyomatosis of the uterus. A report of three cases. Pathol Oncol Res 1998;4:44–7. [DOI] [PubMed] [Google Scholar]
- [4].Du J, Zhao X, Guo D, et al. Intravenous leiomyomatosis of the uterus: a clinicopathologic study of 18 cases, with emphasis on early diagnosis and appropriate treatment strategies. Hum Pathol 2011;42:1240–6. [DOI] [PubMed] [Google Scholar]
- [5].Kocica MJ, Vranes MR, Kostic D, et al. Intravenous leiomyomatosis with extension to the heart: rare or underestimated? J Thorac Cardiovasc Surg 2005;130:1724–6. [DOI] [PubMed] [Google Scholar]
- [6].Durck H. Über ein kontinuierlich durch die untere Hohlvene in das Herz vorwachsendes: Fibromyom des Uterus. Münch Med Wochenschr 1907;54:1154. [Google Scholar]
- [7].Schafer HM, Isaak A, Gurke L. Case report of an intracaval leiomyomatosis 10 months after complete hysterectomy. Int J Surg Case Rep 2017;35:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Simon AJ, Parry-Smith WR, Redman CW, et al. Intravascular leiomyomatosis: a case report and review of the literature. J Obstet Gynaecol 2015;35:539–40. [DOI] [PubMed] [Google Scholar]
- [9].Valdes Devesa V, Conley CR, Stone WM, et al. Update on intravenous leiomyomatosis: report of five patients and literature review. Eur J Obstet Gynecol Reprod Biol 2013;171:209–13. [DOI] [PubMed] [Google Scholar]


