Abstract
Rationale:
Glycyrrhizin is the main active component of licorice. Licorice and glycyrrhizin induced hypertension has been widely reported, yet licorice and glycyrrhizin induced hypertensive crisis has been rarely known.
Patient concerns:
The case of this report was a 47-year-old woman, who took 225 mg of glycyrrhizin daily for 3 years due to primary biliary cholangitis. She was found to have a dramatically elevated blood pressure of about 230/110 mmHg without a history of hypertension and was referred to the emergency department.
Diagnoses:
Hypokalemia, hypertensive retinopathy, and nephropathy were found during the following work-up. Since no other risk factors of hypertension were identified, she was suspected to have glycyrrhizin induced pseudo-hyperaldosteronism.
Interventions:
Glycyrrhizin was discontinued. Intravenous sodium nitroprusside was used during the first few days. Nifedipine and irbesartan were taken after discharge, and the dosage was reduced gradually under supervision.
Outcomes:
She stopped all the anti-hypertensive drugs 6 months since glycyrrhizin was stopped. Her blood pressure was about 110/60 mmHg after repetitive measurement. Her serum potassium and urine albumin/creatinine ratio were also normalized.
Lessons:
Licorice and glycyrrhizin induced hypertension due to pseudo-hyperaldosteronism has been widely reported, yet only 3 cases reported that excessive consumption of licorice could lead to hypertensive emergencies. This is the first case that glycyrrhizin induced hypertensive crisis with target organ impairment. By presenting this case, we remind clinicians of glycyrrhizin induced hypertension, a condition which could lead to medical emergencies.
Keywords: case report, glycyrrhizin, hypertension, mineralocorticoids
1. Introduction
Licorice, also called Glycyrrhizae Radix, is popular as a natural sweetener and widely used drug in many areas, like the United States, Europe, and Asia, and has been regarded as a healthy natural substance without side effects in the traditional belief.[1] However, pseudo-hyperaldosteronism, featured by hypertension, hypokalemia, and alkalosis, should be a concern when licorice is taken excessively. As the main active component of licorice, glycyrrhizin has been proven effective for treating both acute and chronic hepatitis, but was also the main constituent that leads to pseudo-hyperaldosteronism.[2] Licorice and glycyrrhizin induced hypertension has been widely reported, yet only 3 cases reported that excessive consumption of licorice could lead to hypertensive emergencies, one of which identified hypertensive crisis with hypertensive retinopathy grade IV.[3–5] There were no reports of glycyrrhizin induced hypertensive crisis by far. We report a case of hypertensive crisis with target organ impairment (eye and kidney) induced by a long-term and full-dose of glycyrrhizin intake.
2. Case presentation
A 47-year-old woman presented to the emergency department with a history of increasingly frequent paroxysmal headache, ophthalmodynia, and nausea. These symptoms had started over the preceding 3 months. She had her blood pressure checked in a clinic by accident when she accompanied her family to see doctor, yet was told to have a dramatically elevated blood pressure of about 230/110 mmHg and was referred to the emergency department. On admission, physical examinations were unremarkable except for a blood pressure of 211/122 mmHg and enlarged left boarder of cardiac dullness. Her body mass index was 20.0 kg/m2. She had a medical history of primary biliary cholangitis confirmed by liver biopsy, and was otherwise well. She was on 1000 mg of ursodeoxycholic acid for about 3 years, yet did not achieve a good biochemical response. She also took glycyrrhizin from a Japanese pharmaceutical company to lower her elevated transaminases (225 mg of glycyrrhizin daily for 3 years). Besides, this patient had no history of hypertension, chronic kidney disease, or cardio- or cerebro-vascular diseases.
Initial examination revealed hypertensive retinopathy grade IV by ophthalmological fundoscopy. Urinary albumin was over 50 μg/mL (normal values: <10 μg/mL) although urine protein was negative in urinalysis. Therefore, hypertensive crisis with target organ impairment (eye and kidney) was considered. Laboratory testing showed that she had a mild hypokalaemia of 3.47 mmol/L (reference values: 3.5–5.3 mmol/L) with bicarbonate being 25.7 mmol/L (reference values: 22–29 mmol/L). Liver function revealed an alkaline phosphatase level of 362 U/L (normal values: 35–100 U/L), a gamma-glutamyl transpeptidase level of 266 U/L (normal values: 7–45 U/L), an aspartate transaminase level of 58 U/L (normal values: 13–35 U/L), and an alanine aminotransferase level of 64 U/L (normal values: 7–40 U/L). Full blood count and renal function were within normal limits. Endocrine testing, like thyroid function, lying level of renin-angiotension-aldosterone system (RAAS), and urine vanillyl mandelic acid were normal. Enhanced computed tomography did not show enlarged adrenal glands or renal artery stenosis. So common causes of secondary hypertension, like renoparenchymous and renovascular hypertension, endocrine hypertension due to hyperthyroidism, hyperaldosteronism, or pheocromocytoma, were excluded. It was unlikely to consider Cushing syndrome since the patient had no classic clinical symptoms or physical findings of hypercortisolism, although serum or urine cortisol level was not tested.
Further evaluation disclosed that the patient was on compound glycyrrhizin tablets 3 tablets 3 times daily for the past 3 years. Since this drug was considered to be likely related to the patient's hypertension, the compound glycyrrhizin tablet was discontinued.
While in hospital, the patient's highest blood pressure was about 262/163 mmHg. She was treated with intravenous sodium nitroprusside to lower blood pressure, which got gradually improved several days later. When discharged, her blood pressure was about 170/100 mmHg. After discharge, she took nifedipine sustained-release tablet 20 mg 2 times daily and irbesartan 150 mg once a day. Her blood pressure decreased gradually during the follow-up, and she reduced dosage of anti-hypertensive drugs under supervision. Six months later, she stopped all the anti-hypertensive drugs, and her blood pressure were about 110/60 mmHg after repetitive measurement. Urine test revealed that her albumin/creatinine ratio was 18 mg/g (normal values: <30 mg/g), which revealed that her kidney damage was reversed. Serum sodium, potassium, and creatinine were normal. Ophthalmological fundoscopy was not tested again, yet she had no signs of ophthalmodynia or vision loss.
2.1. Ethics approval and consent to participate
This research was reviewed by Institutional Review Board of West China Hospital and waived due to the nature of this case report. Informed consent was obtained from this patient.
3. Discussion
We present a case of hypertensive crisis with hypertensive retinopathy and nephropathy induced by a long-term and full-dose of glycyrrhizin intake. Although several cases have been reported that licorice could lead to hypertensive emergency when taking excessively, this is the first case as far as we know that glycyrrhizin induced hypertensive crisis with target organ impairment. By presenting this case, we remind clinicians of glycyrrhizin induced hypertension, a condition which could lead to medical emergencies, especially in subjects with long-term intake.
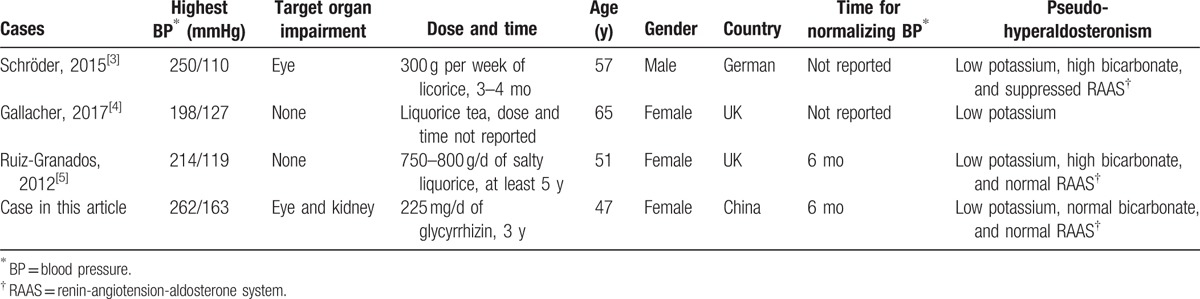
As far as we know, there were only 3 cases showing that excessive consumption of licorice could lead to hypertensive emergencies as shown in Table 1.[3–5] Among them, 1 case presented a Caucasian male developed hypertensive retinopathy grade IV and a blood pressure of 250/110 mmHg after a weekly consumption of at least 900 g of licorice for at least 3 months.[3] This is the only case with target organ impairment and an elevated blood pressure similar to that in ours. As far as we know, there were no reports of glycyrrhizin induced hypertensive crisis by far.
Table 1.
A summary of cases of licorice or glycyrrhizin induced hypertension emergencies.
For over several decades, glycyrrhizin has been widely used as a flavoring agent worldwide and an effective hepatoprotective drug for both acute and chronic hepatitis in countries like China, Japan, Indonesia, and Korea.[6,7] With high prevalence of chronic viral hepatitis and increasing prevalence of alcoholic and non-alcoholic steatosis hepatitis, drugs containing glycyrrhizin have been widely prescribed in clinical practice.[8,9] For example, a study investigating hepatoprotective drug utilization in 34 hospitals in China showed that glycyrrhizin ranked first in frequency of drug use.[10] Therefore, the adverse effects of glycyrrhizin should be a big concern with its widespread use.
Although not well defined, it is worth noting that pseudo-hyperaldosteronism, the main adverse effect of glycyrrhizin, is not rare. The main mechanism of pseudo-hyperaldosteronism is increased activity of cortisol through blocking 11-beta-hydroxysteroid dehydrogenase enzyme by glycyrrhizin, which binds to the mineralocorticoid receptor and then leads to water-sodium retention, potassium loss, and consequently suppressed RAAS through negative feed-back regulation.[1] Therefore, subjects with pseudo-hyperaldosteronism are characterized by hypertension, hypokalaemia, and low serum concentration of renin and aldosterone. In our case, the patient developed sustained hypertension and mild hypokalemia, but her serum renin and aldosterone were in the normal limits instead of being suppressed. The patient's serum level of renin and aldosterone were tested after her high blood pressure was improved, which may be the reason that her RAAS was not suppressed.
Experimental studies have shown that licorice raises blood pressure in a linear dose–response manner. Consuming as low as 75 mg of glycyrrhetinic acid daily for 2 weeks can cause a significant rise in systolic blood pressure.[11] Several administrations have issued advice on the dose of glycyrrhizin to increase the awareness of health hazards associated with excessive intake.[12] For example, the European Scientific Committee on Food advises a safe average daily intake of glycyrrhizin should not be >10 mg daily, and believes that regular intake of 100 mg of glycyrrhizin daily have potential health hazards. The Food Standards Agency in the UK requires a warning stating potential harms on any beverage with >50 mg/L of glycyrrhizin. Our patient was taking daily dose of 225 mg of glycyrrhizin daily, which is well in excess of the recommended limit for as long as 3 years.
4. Conclusions
The side effect of licorice on blood pressure has been previously reported and getting more attention. We think, however, that this case was important to remind clinicians that things with glycyrrhizin, like beverage and drug, may cause hypertension and even hypertensive crisis, especially in areas with wide use of glycyrrhizin. Blood pressure and serum potassium should be monitored among patients who take glycyrrhizin in a large dose for a significant period of time.
Acknowledgments
The authors thank Arjudeb Mukherjee for his help in language assistance.
Footnotes
Abbreviation: RAAS = renin-angiotension-aldosterone system.
The authors report no conflicts of interest.
References
- [1].Omar HR, Komarova I, El-Ghonemi M, et al. Licorice abuse: time to send a warning message. Ther Adv Endocrinol Metab 2012;3:125–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Li JY, Cao HY, Liu P, et al. Glycyrrhizic acid in the treatment of liver diseases: literature review. Biomed Res Int 2014;2014:872139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Schröder T, Hubold C, Muck P, et al. A hypertensive emergency with acute visual impairment due to excessive liquorice consumption. Neth J Med 2015;73:82–5. [PubMed] [Google Scholar]
- [4].Gallacher SD, Tsokolas G, Dimitropoulos I. Liquorice-induced apparent mineralocorticoid excess presenting in the emergency department. Clin Med (Lond) 2017;17:43–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ruiz-Granados ES, Shouls G, Sainsbury C, et al. A salty cause of severe hypertension. BMJ Case Rep 2012;2012:bcr1220115336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Isbrucker RA, Burdock GA. Risk and safety assessment on the consumption of Licorice root (Glycyrrhiza sp.), its extract and powder as a food ingredient, with emphasis on the pharmacology and toxicology of glycyrrhizin. Regul Toxicol Pharmacol 2006;46:167–92. [DOI] [PubMed] [Google Scholar]
- [7].Kumada H. Long-term treatment of chronic Hepatitis C with glycyrrhizin [stronger neo-minophagen C (SNMC)] for preventing liver cirrhosis and hepatocellular carcinoma. Oncology 2002;62(Suppl):94–100. [DOI] [PubMed] [Google Scholar]
- [8].Cui Y, Jia JD. Update on epidemiology of hepatitis B and C in China. J Gastroenterol Hepatol 2013;28(Suppl):7–10. [DOI] [PubMed] [Google Scholar]
- [9].Fan JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol 2013;28(Suppl):11–7. [DOI] [PubMed] [Google Scholar]
- [10].Liu JY, Zhang CL, Li XP, et al. Utilization analysis of hepatoprotecitve drugs of 34 hospitals in Wuhan area during 2012–2014 (Chinese). Chin J Pharmacoepidemiol 2016;25:113–8. [Google Scholar]
- [11].Sigurjónsdóttir HA, Franzson L, Manhem K, et al. Liquorice-induced rise in blood pressure: a linear dose-response relationship. J Hum Hypertens 2001;15:549–52. [DOI] [PubMed] [Google Scholar]
- [12].Allcock E, Cowdery J. Hypertension induced by liquorice tea. BMJ Case Rep 2015;2015:bcr2015209926. [DOI] [PMC free article] [PubMed] [Google Scholar]


